Abstract
BACKGROUND:
In the past several decades, the increasing frequency of overweight and obese children and adolescents in the world has become a public health problem. It has contributed significantly to the already high tide of diabetes, cardiovascular and cerebrovascular diseases.
AIM:
To investigate the frequency of insulin resistance and to evaluate the metabolic profile of insulin resistant and non-insulin resistant obese children and adolescents.
SUBJECTS AND METHODS:
The study included 96 (45 boys, 51 girls) obese children and adolescents aged 4-17 years old (10.50 ± 2.87 years). Only participants with Body Mass Index ≥ 95 percentile were included. We analysed sera for fasting insulin levels (FI), fasting serum triglycerides (TG), total serum cholesterol (TC), fasting plasma glucose (FPG) and plasma glucose 2 hours after the performance of the oral glucose tolerance test (2-h G). Homeostatic model assessment for insulin resistance (HOMA-IR) index was calculated as fasting insulin concentration (microunits per millilitre) x fasting glucose concentration (millimolar)/22.5. The value of HOMA-IR above 3.16 was used as a cut-off value for both genders.
RESULTS:
Insulin resistance was determined in 58.33% of study participants. Insulin resistant participants had significantly higher level of 2-h G (p = 0.02), FI level (p = 0.000) as well as TG levels (p = 0.01), compared to non-insulin resistant group. Strikingly, 70.73% of the pubertal adolescents were insulin resistant in comparison to 49.09% of the preadolescents (p = 0.03). Significantly higher percentage of insulin-resistant participants were girls (p = 0.009). Moreover, a higher percentage of the girls (70.59%) than boys (44.44%) had HOMA-IR above 3.16 and had elevated FI levels (70.59% vs 48.89%). The difference in the frequency of insulin resistance among obese versus severely obese children and adolescents was not significant (p = 0.73, p > 0.05). Our study results also showed positive, but weak, correlation of HOMA-IR with age, FPG, TG and BMI of the participants (p < 0.05).
CONCLUSION:
Higher percentage of insulin-resistant participants was of female gender and was adolescents. In general, insulin resistant obese children and adolescents tend to have a worse metabolic profile in comparison to individuals without insulin resistance. It is of note that the highest insulin resistance was also linked with the highest concentrations of triglycerides.
Keywords: Childhood obesity, Obesity in adolescents, Insulin resistance, Homeostatic model assessment of insulin resistance, Metabolic parameters
Introduction
Obesity is a chronic medical condition where increased adipose tissue growth impairs metabolic health, increases the risk for type 2 diabetes mellitus, cardiovascular diseases, dyslipidemia, hypertension and insulin resistance [1] [2] [3] [4] [5].
Obesity rates are constantly rising globally, in line with growing prevalence of obesity and overweight in pediatric patients. This prevalence has risen by 47.1% between 1980 and 2013 [6]. One in 3 children in the US is overweight or obese [7]. In Europe, the highest rates of obese children are observed in the south-eastern European countries [8]. Also, the rise in obesity is occurring in earlier ages [9] [10]. It is of note there has been plateauing in the prevalence of obesity in developed countries [11].
Insulin resistance is a key component of the metabolic syndrome [12]. Childhood insulin resistance could impair metabolic health and is associated with metabolic syndrome, prediabetes, type 2 diabetes mellitus and several other cardiometabolic risk factors [13][5]. One of the earliest complications, as a consequence of insulin resistance in childhood obesity, is the impairment of glucose metabolism [14]. However, it should be mentioned that insulin resistance may not always be present in obese individuals [13].
There are several methods that could be used for assessing insulin resistance: hyperinsulinemic euglycemic clamp and intravenous glucose tolerance test, homeostasis model assessment (HOMA), quantitative insulin sensitivity check index (QUICKI), McAuley index, Matsuda index, Belfioreindex, Cederholm index, Avignonindex, Stumvollindex. Although hyperinsulinaemic-euglycaemic clamp test is the gold-standard for the measurement of insulin sensitivity, homeostatic model assessment has been considered as a useful, cost-effective, and most widely used tool for the assessment of insulin resistance [15] [16]. The interaction between HOMA-IR and BMI in preadolescence predicts the likelihood of having metabolic syndrome in late adolescence. Therefore reducing insulin resistance in children at the age of 9-10 years could lead to metabolic syndrome prevention at the age of 18-19 years [17]. Moreover, both metabolic syndrome and type 2 diabetes mellitus in adulthood could be predicted form the existence of pediatric metabolic syndrome [18]. Impaired fasting glucose, type 2 diabetes mellitus in early adulthood could also be predicted using the HOMA-IR index for insulin resistance in the preadolescent age [19]. However, it is the HOMA-IR threshold levels for defining insulin resistance have been varying greatly hampering the interpretation of the results [20].
Our study aimed to investigate the frequency of insulin resistance and to evaluate the metabolic profile of insulin resistant and non-insulin resistant obese children and adolescents.
Methods
This cross-sectional study included a total of 96 obese children and adolescents referred to the University Clinic of Child Diseases – Skopje between 2009 and 2017 for investigation and treatment for obesity. The cohort included 45 boys and 51 girls aged 4-17 years (10.50 ± 2.87). Study participants were classified as preadolescents if they were between 4 and 11 years old and adolescents if they were between 12 and 18 years old [21]. Obesity was the only inclusion criteria, as defined from the sex- and age-specific growth charts provided by the Centers of Disease Control and Prevention (CDC) – Body Mass Index ≥ 95th percentile [22]. As severely obese participants were classified those whose BMI was 120% of the 95th percentile for age and sex [23]. Study participants with secondary obesity syndromes, syndromal obesity, primary hyperinsulinemia, hypothyroidism, long-term corticosteroid use, primary hyperlipidemia, diabetes mellitus type 1, or other weight affecting disorders as well as chronic, hereditary, endocrine, infectious and inflammatory disorders were excluded. This study was approved by the Ethical Committee of the Faculty of Medicine of the University “Ss. Cyril and Methodius” – Skopje, Macedonia and was carried out by the Declaration of Helsinki.
Participants’ height (to the nearest millimetre) and weight (to the nearest decimal fraction of kg) were measured according to the standard procedures while participants’ were barefoot and dressed only in light underwear. Body Mass Index was calculated as weight in kilograms divided by height in square meters. An oral glucose tolerance test was performed with a dose of 1.75 g glucose/kg body weight (up to a maximum of 75 grams) by the World Health Organization (WHO) recommendations [24]. Blood samples were collected in at 0 minutes and in several intervals, at 30, 60, 90, 120, 150, 240 minutes, after the glucose load. All study participants fasted for 12 hours after which venous sampling was done. The levels of plasma glucose, serum triglycerides, and total serum cholesterol were determined using clinical chemistry analyser ARCHITECT c4000 (Abbott Diagnostics). Insulin levels were measured in an analyser IMMULITE® 2000 immunoassay system (SimensHealthcareDiagnostics). Homeostatic model assessment for insulin resistance (HOMA-IR) index was calculated: fasting insulin concentration (microunits per millilitre) x fasting glucose concentration (millimolar)/22.5 [25].
Serum fasting triglyceride levels ≥ 100 (mg/dL) for children aged 0-9 years and > 130 for children aged 10-19 years old defined the abnormally elevated level of serum triglycerides. Total serum cholesterol ≥ 200 mg/dL was considered abnormal [26]. To convert mg/dL to mmol/L values of total cholesterol and triglycerides were multiplied by 0.0259 and 0.0113, respectively;
Impaired fasting glucose was defined if the fasting plasma glucose level was ≥ 5.6 but < 7 mmol/L, impaired glucose tolerance if two-hours of plasma glucose after OGTT performance was ≥ 7.8 but < 11.1 mmol/L. Type 2 diabetes mellitus was defined if the fasting plasma glucose level was ≥ 7 mmol/L, or two -hours of plasma glucose after OGTT performance was ≥ 11.1 mmol/L [27]. Fasting insulin levels ≥ 15 mU/ml were considered hyperinsulinemic levels [28]. Insulin resistance was defined as HOMA-IR index > 3.16 [29].
Continuous data were expressed as mean ± SE. Categorical data were expressed as frequencies and percentages. All continuous variables were first tested for distribution normality using Smirnov -Kolmogorov and Shapiro-Wilk normality tests. Depending on the normality of the distribution parametric and non-parametric statistical tests were conducted. For the analysis of normally distributed data t-test was performed and Pearson correlation coefficients were calculated. In cases where data were not normally distributed Man Whitney U test was conducted, and Spearman correlation coefficients were calculated. The Pearson Chi-square was used to analyse differences in categorical variables. Data were analyzed by using statistical package STATISTICA 8.0. P values < 0.05 were considered statistically significant.
Results
Our study comprised of 96 obese children and adolescents (45 boys and 51 girls), aged between 4 -17 years (Table 1). Girls had significantly higher BMI, fasting insulin levels and HOMA-IR compared to boys (p < 0.005). Other metabolic parameters (fasting plasma glucose, plasma glucose 2 hours post the glucose load after the OGTT, total cholesterol and triglyceride level) did not differ significantly between genders (Table 1).
Table 1.
Clinical and metabolic characteristics of obese children and adolescents according to gender
| All | Boys | Girls | |||||
|---|---|---|---|---|---|---|---|
| Variable | Participants No. | % or mean ± SE | Participants No. | % or mean ± SE | Participants No. | % or mean ± SE | p-value |
| Degree of obesity* | 96 | - | 45 | - | 51 | - | 0.451 |
| Obese | 27 | 28.13 | 11 | 24.44 | 16 | 31.37 | |
| Severely obese | 69 | 71.88 | 34 | 75.56 | 35 | 68.63 | |
| Preadolescents vs. adolescents* | 96 | - | 45 | - | 51 | - | 0.032 |
| Preadolescents | 55 | 57.29 | 31 | 68.89 | 24 | 47.06 | |
| Adolescents | 41 | 42.71 | 14 | 31.11 | 27 | 52.94 | |
| Age (years)†† | 96 | 10.50 ± 0.29 | 45 | 10.17 ± 0.40 | 51 | 10.79 ± 0.42 | 0.18 |
| Wieght (kg)†† | 96 | 74.97 ± 2.39 | 45 | 72.86 ± 3.73 | 51 | 76.84 ± 3.08 | 0.18 |
| Height (cm)†† | 96 | 150.52 ± 1.63 | 45 | 149.20 ±2.68 | 51 | 151.69 ± 2.03 | 0.45 |
| BMI (kg/m2)†† | 96 | 31.68 ± 0.49 | 45 | 30.63 ± 0.58 | 51 | 32.62 ± 0.74 | 0.03 |
| FPG (mmol/L)† | 96 | 4.18 ± 0.04 | 45 | 4.16 ± 0.07 | 51 | 4.20 ± 0.06 | 0.65 |
| 2-h G (mmol/L)† | 93 | 5.67 ± 0.12 | 45 | 5.70 ± 0.18 | 48 | 5.64 ± 0.16 | 0.79 |
| FI (uU/mL)†† | 96 | 20.35 ± 1.09 | 45 | 16.93 ± 1.46 | 51 | 23.37 ± 1.47 | 0.000 |
| HOMA-IR†† | 96 | 3.80 ± 0.21 | 45 | 3.14 ± 0.29 | 51 | 4.37 ± 0.29 | 0.000 |
| TC (mmol/L)† | 88 | 4.05 ± 0.08 | 41 | 4.04 ± 0.12 | 47 | 4.06 ± 0.10 | 0.89 |
| TG (mmol/L)†† | 88 | 1.20 ± 0.06 | 41 | 1.11 ± 0.09 | 47 | 1.27 ± 0.07 | 0.07 |
Obtained from χ2 test for comparison of categorical variables;
Group comparison was examined using Mann-Whitney U test for continuous data;
Group comparison was examined using t test for continuous data; 1Pearson χ2 = 0.57, df=1; 2Pearson χ2 = 4.66, df=1; BMI, Body Mass Index; FPG, fasting plasma glucose; 2-h G, plasma glucose two hours post the glucose load during the oral glucose tolerance test; FI, fasting insulin level; HOMA-IR, homeostatic model assessment of insulin resistance; TC, total cholesterol; TG, triglycerides.
The second table shows characteristics of insulin resistant and non-insulin resistant obese children and adolescents. Adolescents had a statistically significant higher frequency of insulin resistance (p = 0.03). Also, the significantly higher percentage of participants with insulin resistance were girls compared to boys (64.29% vs 35.71%, p = 0.009). The mean age, as well as BMI, was significantly higher in the insulin-resistant group (p < 0.05). Study participants who had insulin resistance had significantly higher values of some of the metabolic parameters (plasma glucose 2 hours post the glucose load after the OGTT, fasting insulin, level of triglycerides) compared to participants in the non-resistant group. The values of fasting plasma glucose and total serum cholesterol showed no statistically significant difference between the two tested groups.
On Table 3 are demonstrated percentages of abnormal metabolic parameters among study participants by gender and insulin resistance status according to HOMA-IR. The frequency of elevated fasting insulin levels was significantly higher in girls (p = 0.03). The distribution of other metabolic parameters between boys and girls did not reveal any statistical significance. The percentage of abnormal level of fasting insulin was significantly higher in obese insulin-resistant children and adolescents. Also, the elevated triglycerides level was more prevalent in the insulin-resistant group. However, the differences in the distribution of other abnormal laboratory parameters among study participants showed no statistical significance.
Table 2.
Clinical and metabolic characteristics of obese children and adolescents according to insulin resistance
| Non-insulin resistant (non-IR) | Insulin resistant (IR) | |||||
|---|---|---|---|---|---|---|
| Variable | Participants No. | Participants No. | % or mean ± SE | Participants No. | % or mean ± SE | p-value |
| Degree of obesity* | 96 | 40 | - | 56 | - | 0.731 |
| Obese | 27 | 12 | 30.00 | 15 | 26.79 | |
| Severely obese | 69 | 28 | 70.00 | 41 | 73.21 | |
| Preadolescents vs. adolescents* | 96 | 40 | - | 56 | - | 0.032 |
| Preadolescents | 55 | 28 | 70.00 | 27 | 48.21 | |
| Adolescents | 42 | 12 | 30.00 | 29 | 51.79 | |
| Gender | 0.0093 | |||||
| Boys | 45 | 25 | 62.5 | 20 | 35.71 | |
| Girls | 51 | 15 | 37.5 | 36 | 64.29 | |
| Age (years)†† | 96 | 40 | 9.79 ± 0.50 | 56 | 11.00 ± 0.34 | 0.04 |
| Wieght (kg)†† | 96 | 40 | 67.05 ± 3.21 | 56 | 80.63 ± 3.21 | 0.005 |
| Height (cm)†† | 96 | 40 | 146.76 ± 2.64 | 56 | 153.21 ± 2.02 | 0.03 |
| BMI (kg/m2)†† | 96 | 40 | 30.35 ± 0.63 | 56 | 32.64 ± 0.68 | 0.02 |
| FPG (mmol/L)† | 96 | 40 | 4.09 ± 0.07 | 56 | 4.25 ± 0.06 | 0.07 |
| 2-h G (mmol/L)† | 93 | 39 | 5.35 ± 0.19 | 54 | 5.89 ± 0.15 | 0.02 |
| FI (uU/mL)†† | 96 | 40 | 11.81 ± 0.59 | 56 | 26.45 ± 1.30 | 0.000 |
| TC (mmol/L)† | 88 | 35 | 3.88 ± 0.11 | 53 | 4.15 ± 0.10 | 0.08 |
| TG (mmol/L)†† | 88 | 35 | 0.99 ± 0.07 | 53 | 1.33 ± 0.08 | 0.005 |
Obtained from χ2 test for comparison of categorical variables;
Group comparison was examined using Mann-Whitney U test for continuous data;
Group comparison was examined using t-test for continuous data;
Pearson χ 2 = 0.12, df=1;
Pearson χ 2 = 4.53, df=1;
Pearson χ 2 = 6.72, df=1; BMI, Body Mass Index; FPG, fasting plasma glucose; 2-h G, plasma glucose two hours post the glucose load during the oral glucose tolerance test; FI, fasting insulin level; TC, total cholesterol; TG, triglycerides.
Table 3.
Frequency (%) of abnormal laboratory parameters among study participants
| Gender | HOMA-IR | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Participants No. | All | Boys | Girls | p-value* | Non-insulin resistant (non-IR) | Insulin resistant (IR) | p-value* | ||||
| n (%) | Participants No. | n (%) | Participants No. | n (%) | Participants No. | n (%) | Participants No. | n (%) | ||||
| FPG (mmol/L) | 96 | 1 (1.04) | 45 | 1 (2.22) | 51 | 0 (0.00) | 0.281 | 40 | 0 (0.00) | 56 | 1 (1.79) | 0.407 |
| 2-h G (mmol/L) | 93 | 3 (3.23) | 45 | 1 (2.22) | 48 | 2 (4.17) | 0.602 | 39 | 2 (5.13) | 54 | 1 (1.85) | 0.388 |
| FI (uU/ml) | 96 | 58 (60.42) | 45 | 22 (48.89) | 51 | 36 (70.59) | 0.033 | 40 | 5 (12.5) | 56 | 53 (96.64) | 0.0009 |
| TC (mmol/L) | 88 | 5 (5.68) | 41 | 3 (7.32) | 47 | 2 (4.26) | 0.754 | 35 | 2 (5.71) | 53 | 3 (5.66) | 0.2710 |
| TG (mmol/L) | 88 | 30 (34.09) | 41 | 13 (31.71) | 47 | 17 (36.17) | 0.105 | 35 | 9 (25.71) | 53 | 21 (39.62) | 0.0111 |
| HOMA-IR | 96 | 56 (58.33) | 45 | 20 (44.44) | 51 | 36 (70.59) | 0.0096 | - | - | - | - | - |
Obtained from χ2 test for comparison of categorical variables;
Pearson χ2 = 1.15, df=1;
Pearson χ2 = 0.28, df=1;
Pearson χ2 = 4.71, df=1;
Pearson χ2 = 0.57, df=2;
Pearson χ2 = 4.57, df=2;
Pearson χ2 = 6.72, df=1;
Pearson χ2 = 0.72, df=1;
Pearson χ2 = 0.78, df=1;
Pearson χ2 = 65.83, df=1;
Pearson χ2 = 2.60, df=2;
Pearson χ2 = 8.75, df=2; FPG, fasting plasma glucose; 2-h G, plasma glucose two hours post the glucose load during the oral glucose tolerance test; FI, fasting insulin level; TC, total cholesterol; TG, triglycerides; HOMA-IR, homeostatic model assessment of insulin resistance.
On Figure 1 the differences and the frequency of abnormal metabolic parameters between participants in two age groups (preadolescents: 4-12; adolescents: ≥ 12-18 years) are presented. There was a higher percentage of plasma glucose 2 hours post the glucose load after the OGTT, elevated fasting insulin and HOMA-IR among adolescents in comparison to preadolescents. All adolescents have undergone puberty, in contrast to only 15% of the preadolescents.
Figure 1.
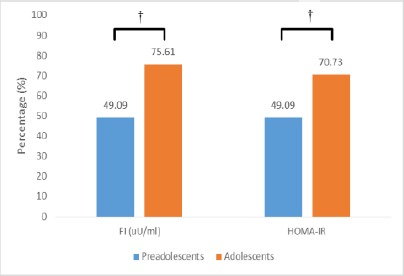
Distribution of abnormal parameters among study participants according to age group. FI, fasting insulin level; HOMA-IR, homeostatic model assessment for insulin resistance. †p value < 0.05, preadolescents vs. adolescents
As shown in Figure 2, the comparison of HOMA-IR comparing the degree of obesity did not reveal any statistical significance (p > 0.05).
Figure 2.
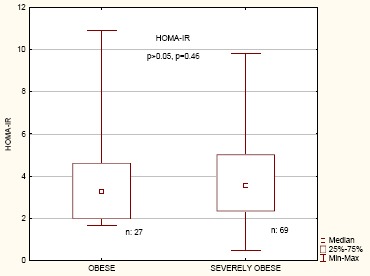
Homeostatic model assessment of insulin resistance comparison between obese and severely obese children and adolescents
Figure 3 shows differences in the frequency of insulin resistance (HOMA – IR > 3.16) among obese and severely obese participants. There was no statistical significance in the distribution of insulin resistance between two examined groups (p = 0.73, Pearson χ2 = 0.12, df = 1).
Figure 3.
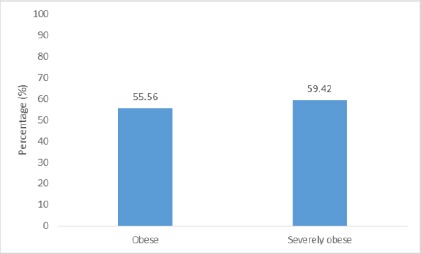
Frequency (%) of elevated HOMA-IR according to the degree of obesity. HOMA-IR, homeostatic model assessment for insulin resistance. p-value > 0.05, obese vs. severely obese
Correlation analysis between the BMI and HOMA-IR of the participants with age and other investigated metabolic parameters is presented in Table 4. BMI was positively correlated with age, FI and HOMA IR of the participants, while HOMA-IR showed a positive correlation with age, fasting plasma glucose, fasting insulin, triglycerides, and BMI.
Table 4.
Correlation between Body Mass Index and HOMA-IR with various parameters studied
| Body Mass Index | HOMA-IR | ||||
|---|---|---|---|---|---|
| Variable | n | Correlation coefficient | p-value | Correlation coefficient | p-value |
| Age (years)†† | 96 | 0.62 | 0.000 | 0.29 | 0.005 |
| FPG (mmol/L)† | 96 | 0.02 | 0.80 | 0.24 | 0.02 |
| 2-h G (mmol/L)† | 93 | 0.13 | 0.22 | 0.20 | 0.06 |
| FI (uU/mL)†† | 96 | 0.34 | 0.000 | 0.98 | 0.00 |
| TC (mmol/L)† | 88 | -0.003 | 0.98 | 0.17 | 0.12 |
| TG (mmol/L)†† | 88 | 0.16 | 0.14 | 0.38 | 0.000 |
| BMI (kg/m2)†† | 96 | - | - | 0.33 | 0.001 |
| HOMA-IR†† | 96 | 0.33 | 0.001 | - | - |
Correlation examined using Pearson correlation,
Correlation examined using Spearman correlation; FPG, fasting plasma glucose; 2-h G, plasma glucose two hours post the glucose load during the oral glucose tolerance test; FI, fasting insulin level; TC, total cholesterol; TG, triglycerides; BMI, Body Mass Index; HOMA-IR, homeostatic model assessment of insulin resistance.
Discussion
Studies have shown an association of excess adipose tissue with insulin resistance [30]. In the present study, 58.13% of all participants were insulin resistant. Significantly higher percentage of girls (70.59%) was insulin resistant in comparison with boys (44.44%). A high percentage of insulin resistance among children and adolescents is also evident in other studies [31] [32]. Others have also reported that there is a significantly higher percentage of girls with insulin resistance [33]. The concentrations of plasma insulin and HOMA-IR indicating insulin resistance were not significantly higher in girls [34]. A study that aimed to evaluate possible predictors for fasting insulin levels in overweight and obese adolescents concluded that gender, BMI and waist circumference were predictors of fasting insulin and HOMA-IR. In the same study, girls were considered to have higher fasting insulin levels compared to boys [32], which is by our study results. Similarly, the level of serum insulin showed high association with female gender in a study conducted by Hrafnkelsson et al. [35]. Results from another study from the United Kingdom revealed that 5 years old girls were more prone to be insulin resistant compared to their peers of the opposite gender [36]. A study conducted on 3,203 children and adolescents from China showed that those participants with the highest number of metabolic abnormalities had significantly higher HOMA-IR [31]. Insulin resistance was significantly higher in girls [37].
We found a significant difference in gender distribution between IR and non-IR group. Namely, 64.29% of the IR group were girls, and 35.71% were boys, while 37.5% and 62.5% of the non-IR group were girls and boys, respectively. Thus, the percentage of girls was higher in the group of children and adolescents with insulin resistance. In the current study, obese girls were not found to have significantly higher values of triglycerides. Also, the frequency of abnormal triglyceride level was not significantly different compared to obese boys. Different studies have shown that insulin resistance could lead to various abnormalities affecting lipid and lipoprotein levels [2]. Contrary to our study, triglyceride levels were highly associated with female gender and were significantly higher in girls [35]. The study conducted on 151 overweight youths found that triglycerides level, as a cardiovascular risk factor, increased with the increase of fasting insulin as well as with the increase of 2 hours insulin [38]. A significant positive correlation between the level of triglycerides and fasting insulin and HOMA-IR has been confirmed in a study on overweight and obese adolescents [32]. Children who had insulin levels in the highest quartile showed increased levels of various cardiovascular risk factors such as triglycerides, systolic and diastolic blood pressure, LDL-cholesterol, VLDL cholesterol, glucose, and decreased the level of HDL-cholesterol. These children also showed higher BMI [39].
Because 52.94% of the girls were in the adolescent age, while 68.89% of the boys were in the preadolescent age, these differences in the insulin resistance status in girls might be related to the age of the participants. Namely, significantly higher percentage (51.79%) of the study participants with insulin resistance were adolescents and 70% of the non-IR group were preadolescents. Our study indicated that insulin-resistant participants had higher BMI and were older. Similarly, the mean age and BMI of study participants with IR were found to be higher compared to those without IR in a study conducted by Romualdo et al. [33]. One study on 196 obese children and adolescents from Turkey revealed that the frequency of cases with insulin resistance differs significantly between the prepubertal and pubertal group and that it is higher among obese adolescents [40]. This is also our observation. One of the most relevant longitudinal studies that was investigating insulin resistance in different stages of puberty on 357 normal children and adolescents found that up to the Tanner stage 2 insulin resistance increases, while during Tanner stages 2, 3 and 4 is constant, followed by a decrease in the prepubertal level at the Tanner stage 5 [37]. Similarly, another recent study suggests that insulin resistance is under the influence of puberty only in Tanner Stage (TS) 1, while during TS 2-4, insulin resistance did not reveal such association. Authors discuss that it could be a result of the degree of obesity, as a contributor to the development of insulin resistance, during adolescence. Therefore, screening for IR is highly recommended in children with early puberty onset, as well as, in adolescents with obesity [41]. However, the suggested insulin sensitivity recovery phenomenon in lean children at the end of puberty could not be seen in obese individuals [42] [43]. Insulin resistance during puberty in obese children is even higher than normal -weight controls [43]. Furthermore, the above-discussed decrease in insulin sensitivity has been shown to start before the pubertal transition in children with morbid obesity, and this could not be explained by total adiposity status [44]. Others have demonstrated that metabolically healthy obese children tend to change to metabolically unhealthy when growing from pre-pubertal to pubertal stage. The metabolic set up in girls could be under the influence of hormonal changes during puberty and adolescence or due to gender-specific body fat distribution [32]. It has been discussed that insulin resistance is not always a consequence of obesity, but it could also be a contributing factor that leads to its development [31]. In the USA more than 50% of the adolescents with obesity are insulin resistant [45]. In girls, insulin resistance occurring during puberty could be worsening as a result of existing obesity [46].
In the current study, an obvious unfavourable metabolic profile was noticed among insulin-resistant participants compared to the non-insulin resistant group. More precisely, participants in the IR group had higher values of all investigated laboratory parameters such as: fasting plasma glucose, 2-h plasma glucose, fasting insulin, and total serum cholesterol and triglyceride level. However, significant differences were only seen in 2-h plasma glucose, fasting insulin and triglyceride levels. Moreover, the frequency of abnormal fasting insulin and triglycerides was higher among insulin-resistant participants. Strikingly, 96.64% and 39.62% of insulin-resistant participants tend to have elevated levels of fasting insulin and serum triglycerides, respectively. Only for comparison, the percentage of abnormal fasting insulin and serum triglycerides in the non-insulin resistant group was 12.5% and 25.71% respectively. In one study it has been shown that glucose and insulin levels among obese participants with elevated HOMA-IR (> 2.5) were significantly higher compared to the obese children with HOMA-IR below 2.5. Interestingly, these same differences were found in the non-obese participants with HOMA-IR > 2.5 and HOMA-IR < 2.5. In contrary to our results, in obese and non - an obese group with HOMA-IR < 2.5 or HOMA-IR > 2.5 participants’ BMI values did not differ significantly [47]. Our study results are similar to those of Atabek et al. [40] whereas insulin resistant group of obese children have significantly higher mean age, higher BMI, fasting glucose, fasting insulin levels and HOMA-R. Triglyceride levels and total cholesterol levels were not found to differ significantly between these two groups. In Another study, triglyceride levels were significantly higher in participants with insulin resistance [33]. The differences between triglyceride levels were significantly higher in the groups of obese children and adolescents with insulin resistance compared to non-insulin resistant groups [41] [48].
The present study indicates that, although weakly, the HOMA-IR was positively correlated with the age, fasting plasma glucose levels, triglyceride levels, and BMI of the participants. Similarly, a study conducted by Esteghamati et al. [49], showed a positive correlation between HOMA-IR and BMI in all subjects as well as in different study groups considering the degree of obesity. Our study revealed the strong positive correlation between HOMA-IR and fasting insulin levels in study participants. A study that evaluated the correlation of insulin resistance assessed by different indices such as McAuley, HOMA and QUICKI, came to a conclusion that fasting insulin is sensitive and could be used as a simple test for the detection of insulin resistance in obese individuals [50]. Thus, it could be concluded that obese insulin-resistant individuals show significantly worse metabolic profile compared to non-insulin resistant ones.
Interestingly, 2.22% of boys from our study had impaired fasting glucose, while girls were not affected. On the contrary, impaired glucose tolerance was detected in 4.17% of girls, while the percentage of boys remained unchanged 2.22%. The study of Valerio et al. [51], did not detect any case of impaired fasting plasma glucose, presenting this laboratory parameter as insensitive. However, this same study found 4% prevalence of impaired glucose tolerance among the study population of obese children and adolescents. Our results are consistent with a study in which impaired fasting glucose was detected only in boys (3%), while no cases were detected in girls. Similarly, the percentage of impaired glucose tolerance among girls increased dramatically and was equal to the one among boys (11%) [52].
Hagman et al. in her studies pointed out those regional differences in glucose levels exist. A study that compared the plasma glucose level between Swedish and Polish children concluded that obese Swedish children have higher glucose levels in comparison to obese children from Poland [53]. Also, the risk of having impaired plasma glucose is higher in obese children from Sweden compared to obese children in Germany [54]. Another study conducted on 54 obese children confirmed that obese children with insulin resistance have higher blood sugar level compared to those obese children without insulin resistance [55]. Interestingly, it has been suggested that the risk of having impaired glucose tolerance is higher in obese children who have high fasting blood glucose level, but still in the range of the reference values [56].
Data from our study showed that the frequency of impaired fasting glucose, as well as impaired glucose tolerance 2 hours post oral glucose tolerance test performance, in both IR and non-IR group, were low. Only 1.79% insulin-resistant participants showed impaired fasting glucose. Similarly, 1.85% and 5.13% had impaired glucose tolerance in IR and non-IR study group, respectively. There were no cases of type 2 diabetes mellitus detected. Our results did not reveal a significant difference between plasma glucose level between IR and non-IR group. Although the prevalence of type 2 diabetes is low, studies have shown that there is a significant increase in recent years, especially with the increase in the prevalence of obesity [57].
Considering the degree of obesity, HOMA-IR values, as well as all other metabolic parameters, did not differ significantly between severely obese and obese participants. However, although differences between these two categories of obesity regarding insulin resistance did not reveal significance, it is worth mentioning that insulin resistance is high among obese and severely obese participants. Namely, 55.56% of obese and 59.42% of severely obese children and adolescents in our study were insulin resistant. The high percentage of insulin resistance among obese children is also seen in studies from the literature. Insulin resistance was found in 44.3% [52], 40.8% in obese children and 41.2% in obese adolescents [51]. A study on forty obese patients revealed that the degree of omental white adipose tissue fibrosis in severe obesity might be the explanation for the degree of insulin resistance in severely obese individuals [58]. A study found that serum insulin levels were higher among overweight children compared to normal weight children [35]. Importantly, the metabolic profile between overweight and obese subjects might not always lead to significant differences, indicating that metabolic disturbances are already present in the overweight state [59].
We found that obese children and adolescents have a high rate of insulin resistance and have altered biochemical metabolic parameters. Lack of control group and relatively small sample size were major drawbacks of this study, therefore imposing that these data need to be confirmed in a controlled trial in order more relevant clinical conclusions to be drawn.
In conclusion, insulin resistance is highly prevalent among obese children and adolescents. Interestingly, the degree of obesity does not seem to play an important factor. Significantly higher percentage of insulin-resistant participants was girls. Also, the frequency of insulin resistance was higher among adolescents. Obese individuals with insulin resistance show more unfavourable metabolic setup, with higher BMI, plasma glucose two-hour post glucose load during the OGTT and higher levels and frequency of abnormal serum triglycerides. It is of note that the more pronounced insulin resistance was also linked with the highest concentrations of triglycerides.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.McMorrow AM, Connaughton RM, Lithander FE, et al. Adipose tissue dysregulation and metabolic consequences in childhood and adolescent obesity: potential impact of dietary fat quality. Proc Nutr Soc. 2015;74(1):67–82. doi: 10.1017/S002966511400158X. https://doi.org/10.1017/S002966511400158X. PMid:25497038. [DOI] [PubMed] [Google Scholar]
- 2.Morandi A, Maffeis C. Predictors of metabolic risk in childhood obesity. Horm Res Paediatr. 2014;82(1):3–11. doi: 10.1159/000362237. https://doi.org/10.1159/000362237. PMid:24923289. [DOI] [PubMed] [Google Scholar]
- 3.Lewandowska E, Zieliński A. White adipose tissue dysfunction observed in obesity. Pol Merkur Lekarski. 2016;40(239):333–6. PMid:27234867. [PubMed] [Google Scholar]
- 4.Berenson GS. Obesity--a critical issue in preventive cardiology: the Bogalusa Heart Study. Prev Cardiol. 2005;8(4):234–41. doi: 10.1111/j.0197-3118.2005.04485.x. quiz 242. https://doi.org/10.1111/j.0197-3118.2005.04485.x. PMid:16230878. [DOI] [PubMed] [Google Scholar]
- 5.Marcovecchio ML, Mohn A, Chiarelli F. Obesity and insulin resistance in children. J Pediatr Gastroenterol Nutr. 2010;51(Suppl 3):S149–50. doi: 10.1097/MPG.0b013e3181f853f9. https://doi.org/10.1097/MPG.0b013e3181f853f9. PMid:21088543. [DOI] [PubMed] [Google Scholar]
- 6.Ng M, Fleming T, Robinson M, et al. Global, regional and national prevalence of overweight and obesity in children and adults 1980-2013: A systematic analysis. Lancet. 2014;30(384 (9945)):766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar S, Kelly AS. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. 2017;92:251–65. doi: 10.1016/j.mayocp.2016.09.017. https://doi.org/10.1016/j.mayocp.2016.09.017. PMid:28065514. [DOI] [PubMed] [Google Scholar]
- 8.Livingstone MBE. Epidemiology of childhood obesity in Europe. Eur J Pediatr. 2000;159(Suppl.1):S14–S34. doi: 10.1007/pl00014363. https://doi.org/10.1007/PL00014363. PMid:11011953. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(17):1660–1. doi: 10.1056/NEJMc1402397. https://doi.org/10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung PC, Cunningham SA, Naryan KMV, et al. Childhood Obesity Incidence in the United States: A Systematic Review. Childhood Obesity. 2016;12(1):1–11. doi: 10.1089/chi.2015.0055. https://doi.org/10.1089/chi.2015.0055. PMid:26618249. PMCid:PMC4753627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. https://doi.org/10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol. 2008;159(Suppl 1):S67–74. doi: 10.1530/EJE-08-0245. https://doi.org/10.1530/EJE-08-0245. PMid:18805916. [DOI] [PubMed] [Google Scholar]
- 13.Levy-Marchal C, Arslanian S, Cutfield W, et al. Insulin Resistance in Children: Consensus, Perspective, and Future Directions. J Clin Endocrinol Metab. 2010;95(12):5189–5198. doi: 10.1210/jc.2010-1047. https://doi.org/10.1210/jc.2010-1047. PMid:20829185. PMCid:PMC3206517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiss R, Kaufman FR. Metabolic complications of childhood obesity: identifying and mitigating the risk. Diabetes Care. 2008;31(Suppl 2):S310–6. doi: 10.2337/dc08-s273. https://doi.org/10.2337/dc08-s273. PMid:18227502. [DOI] [PubMed] [Google Scholar]
- 15.Antuna-Puente B, Disse E, Rabasa-Lhoret R, et al. How can we measure insulin sensitivity/resistance? Diabetes Metab. 2011;37(3):179–88. doi: 10.1016/j.diabet.2011.01.002. https://doi.org/10.1016/j.diabet.2011.01.002. PMid:21435930. [DOI] [PubMed] [Google Scholar]
- 16.Gutch M, Kumar S, Razi SM, et al. Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metab. 2015;19(1):160–164. doi: 10.4103/2230-8210.146874. https://doi.org/10.4103/2230-8210.146874. PMid:25593845. PMCid:PMC4287763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morrison JA, Glueck CJ, Horn PS, et al. Homeostasis model assessment of insulin resistance*body mass index interactions at ages 9 to 10 years predict metabolic syndrome risk factor aggregate score at ages 18 to 19 years: a 10-year prospective study of black and white girls. Metabolism. 2009;58(3):290–5. doi: 10.1016/j.metabol.2008.09.027. https://doi.org/10.1016/j.metabol.2008.09.027. PMid:19217441. [DOI] [PubMed] [Google Scholar]
- 18.Morrison JA, Friedman LA, Wang P, et al. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008;152(2):201–6. doi: 10.1016/j.jpeds.2007.09.010. https://doi.org/10.1016/j.jpeds.2007.09.010. PMid:18206689. [DOI] [PubMed] [Google Scholar]
- 19.Morrison JA, Glueck CJ, Horn PS, et al. Pre-teen insulin resistance predicts weight gain, impaired fasting glucose, and type 2 diabetes at age 18-19 y: a 10-y prospective study of black and white girls. Am J Clin Nutr. 2008;88(3):778–88. doi: 10.1093/ajcn/88.3.778. https://doi.org/10.1093/ajcn/88.3.778. PMid:18779296. [DOI] [PubMed] [Google Scholar]
- 20.Gayoso-Diz P, Otero-González A, Rodriguez-Alvarez MX, et al. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study. BMC Endocr Disord. 2013;13:47. doi: 10.1186/1472-6823-13-47. https://doi.org/10.1186/1472-6823-13-47. PMid:24131857. PMCid:PMC4016563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel DA, Srinivasan SR, Chen W, et al. Serum Alanine Aminotransferase and Its Association with Metabolic Syndrome in Children: The Bogalusa Heart Study. Metabolic Syndrome and Related Disorders. 2011;9(3):211–216. doi: 10.1089/met.2010.0086. https://doi.org/10.1089/met.2010.0086. PMid:21476865. PMCid:PMC3125570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. https://doi.org/10.1542/peds.2007-2329C. PMid:18055651. [DOI] [PubMed] [Google Scholar]
- 23.Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–712. doi: 10.1161/CIR.0b013e3182a5cfb3. https://doi.org/10.1161/CIR.0b013e3182a5cfb3. PMid:24016455. [DOI] [PubMed] [Google Scholar]
- 24.Alberti KG, Zimmet PZ. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications Part 1: Diagnosis and Classification of Diabetes Mellitus Provisional Report of a WHO Consultation. 1998;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 25.Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. https://doi.org/10.1007/BF00280883. PMid:3899825. [DOI] [PubMed] [Google Scholar]
- 26.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–S256. doi: 10.1542/peds.2009-2107C. https://doi.org/10.1542/peds.2009-2107C. PMid:22084329. PMCid:PMC4536582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Diabetes Association. Classification and Diagnosis of Diabetes. Diabetes Care. 2016;39(Suppl 1):S13–22. doi: 10.2337/dc16-S005. https://doi.org/10.2337/dc16-S005. PMid:26696675. [DOI] [PubMed] [Google Scholar]
- 28.Reaven GM, Brand RJ, Chen YD, et al. Insulin resistance and insulin secretion are determinants of oral glucose tolerance in normal individuals. Diabetes. 1993;42(9):1324–32. doi: 10.2337/diab.42.9.1324. https://doi.org/10.2337/diab.42.9.1324. PMid:8349044. [DOI] [PubMed] [Google Scholar]
- 29.Keskin M, Kurtoglu S, Kendirci M, et al. Homeostasis Model Assessment Is More Reliable Than the Fasting Glucose / Insulin Ratio and Quantitative Insulin Sensitivity Check Index for Assessing Insulin Resistance Among Obese Children and Adolescents. Pediatrics. 2005;115(4):500–503. doi: 10.1542/peds.2004-1921. https://doi.org/10.1542/peds.2004-1921. PMid:15741351. [DOI] [PubMed] [Google Scholar]
- 30.Thota P, Perez-Lopez FR, Benites-Zapata VA, et al. Obesity-related insulin resistance in adolescents: a systematic review and meta-analysis of observational studies. Gynecol Endocrinol. 2017;33(3):179–184. doi: 10.1080/09513590.2016.1273897. https://doi.org/10.1080/09513590.2016.1273897. PMid:28102091. [DOI] [PubMed] [Google Scholar]
- 31.Yin J, Li M, Xu L, et al. Insulin resistance determined by Homeostasis Model Assessment (HOMA) and associations with metabolic syndrome among Chinese children and teenagers. Diabetology & Metabolic Syndrome. 2013;5:71. doi: 10.1186/1758-5996-5-71. https://doi.org/10.1186/1758-5996-5-71 PMid:24228769. PMCid:PMC3833654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ling JCY, Mohamed MNA, Jalaludin MY, et al. Determinants of High Fasting Insulin and Insulin Resistance Among Overweight/Obese Adolescents. Sci Rep. 2016;6:36270. doi: 10.1038/srep36270. https://doi.org/10.1038/srep36270. PMid:27824069. PMCid:PMC5099955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Romualdo MC, Nóbrega FJ, Escrivão MA. Insulin resistance in obese children and adolescents. J Pediatr (Rio J) 2014;90(6):600–7. doi: 10.1016/j.jped.2014.03.005. https://doi.org/10.1016/j.jped.2014.03.005. PMid:25019650. [DOI] [PubMed] [Google Scholar]
- 34.Nogueira-de-Almeida CA, Mello ED. Correlation of BMI Z-scores with glucose and lipid profiles among overweightand obese children and adolescents. J Pediatr (Rio J) 2017 doi: 10.1016/j.jped.2017.06.012. https://doi.org/10.1016/j.jped.2017.06.012. PMid:28881179. [DOI] [PubMed] [Google Scholar]
- 35.Hrafnkelsson H, Magnusson KT, Sigurdsson EL, et al. Association of BMI and fasting insulin with cardiovascular disease risk factors in seven-year-old Icelandic children. Scand J Prim Health Care. 2009;27(3):186–191. doi: 10.1080/02813430903155028. https://doi.org/10.1080/02813430903155028. PMid:19731182. PMCid:PMC3413192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy MJ, Metcalf BS, Voss LD, Jeffery, et al. Girls at five are intrinsically more insulin resistant than boys: The Programming Hypotheses Revisited –The EarlyBird Study (EarlyBird 6) Pediatrics. 2004;113(1):82–86. doi: 10.1542/peds.113.1.82. https://doi.org/10.1542/peds.113.1.82. PMid:14702453. [DOI] [PubMed] [Google Scholar]
- 37.Moran A, Jacobs DR, Jr, Steinberger J, et al. Insulin resistance during puberty: results from clamp studies in 357 children. Diabetes. 1999;48(10):2039–44. doi: 10.2337/diabetes.48.10.2039. https://doi.org/10.2337/diabetes.48.10.2039. PMid:10512371. [DOI] [PubMed] [Google Scholar]
- 38.Libman IM, Barinas-Mitchell E, Bartucci A, et al. Fasting and 2-Hour Plasma Glucose and Insulin: Relationship with risk factors for cardiovascular disease in overweight nondiabetic children. Diabetes Care. 2010;33(12):2674–2676. doi: 10.2337/dc10-0085. https://doi.org/10.2337/dc10-0085. PMid:21115769. PMCid:PMC2992211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bao W, Srinivasan SR, Berenson GS. Persistant elevation of plasma insulin levels is associated with increased cardiovascular risk in children and young adults. The Bogalusa Heart Study. Circulation. 1996;93:54–9. doi: 10.1161/01.cir.93.1.54. https://doi.org/10.1161/01.CIR.93.1.54. PMid:8616941. [DOI] [PubMed] [Google Scholar]
- 40.Atabek ME, Pirgon O, Kurtoglu S. Assessment of abnormal glucose homeostasis and insulin resistance in Turkish obese children and adolescents. Diabetes Obes Metab. 2007;9(3):304–10. doi: 10.1111/j.1463-1326.2006.00601.x. https://doi.org/10.1111/j.1463-1326.2006.00601.x. PMid:17391156. [DOI] [PubMed] [Google Scholar]
- 41.Lentferink YE, Elst MAJ, Knibbe CAJ, et al. Predictors of Insulin Resistance in Children versus Adolescents with Obesity. J Obes. 2017;2017:3793868. doi: 10.1155/2017/3793868. https://doi.org/10.1155/2017/3793868. PMid:29375912. PMCid:PMC5742469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kelsey MM, Zeitler PS. Insulin Resistance of Puberty. Curr Diab Rep. 2016;16(7):64. doi: 10.1007/s11892-016-0751-5. https://doi.org/10.1007/s11892-016-0751-5. PMid:27179965. [DOI] [PubMed] [Google Scholar]
- 43.Pilia S, Casini MR, Foschini ML, et al. The effect of puberty on insulin resistance in obese children. J Endocrinol Invest. 2009;32(5):401–5. doi: 10.1007/BF03346475. https://doi.org/10.1007/BF03346475. PMid:19794287. [DOI] [PubMed] [Google Scholar]
- 44.Manco M, Spreghini MR, Luciano R, et al. Insulin Sensitivity from Preschool to School Age in Patients with Severe Obesity. PLoS ONE. 2013;8(7):e68628. doi: 10.1371/journal.pone.0068628. https://doi.org/10.1371/journal.pone.0068628. PMid:23935878. PMCid:PMC3729946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee JM. Insulin resistance in children and adolescents. Rev Endocr Metab Disord. 2006;7(3):141–7. doi: 10.1007/s11154-006-9019-8. https://doi.org/10.1007/s11154-006-9019-8. PMid:17165145. [DOI] [PubMed] [Google Scholar]
- 46.Burt SCM, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010;140(3):399–410. doi: 10.1530/REP-10-0119. https://doi.org/10.1530/REP-10-0119. PMid:20802107. PMCid:PMC2931339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Onal ZE, Atasayan V, Gürbüz T, et al. Association of glycosylated hemoglobin (HbA1c) levels with Iinsulin resistance in obese children. Afr Health Sci. 2014;14(3):533–8. doi: 10.4314/ahs.v14i3.6. https://doi.org/10.4314/ahs.v14i3.6. PMid:25352869. PMCid:PMC4209635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guerrero-Romero F, Aradillas-García C, Simental-Mendía LE, et al. Biochemical characteristics and risk factors for insulin resistance at different levels of obesity. Pediatrics. 2013;131(4):e1211–7. doi: 10.1542/peds.2012-1421. https://doi.org/10.1542/peds.2012-1421. PMid:23478864. [DOI] [PubMed] [Google Scholar]
- 49.Esteghamati A, Khalilzadeh O, Anvari M, et al. Metabolic syndrome and insulin resistance significantly correlate with body mass index. Arch Med Res. 2008;39(8):803–8. doi: 10.1016/j.arcmed.2008.08.004. https://doi.org/10.1016/j.arcmed.2008.08.004. PMid:18996295. [DOI] [PubMed] [Google Scholar]
- 50.Panag KMDS, Kaur N, Goyal G. Correlation of insulin resistance by various methods with fasting insulin in obese. Int J Appl Basic Med Res. 2014;4(Suppl 1):S41–S45. doi: 10.4103/2229-516X.140733. https://doi.org/10.4103/2229-516X.140733. PMid:25298942. PMCid:PMC4181131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Valerio G, Licenziati MR, Iannuzzi A, et al. Insulin resistance and impaired glucose tolerance in obese children and adolescents from Southern Italy. Nutr Metab Cardiovasc Dis. 2006;16(4):279–84. doi: 10.1016/j.numecd.2005.12.007. https://doi.org/10.1016/j.numecd.2005.12.007. PMid:16679220. [DOI] [PubMed] [Google Scholar]
- 52.Viner R, Segal T, Lichtarowicz-Krynska E, Hindmarsh P. Prevalence of the insulin resistance syndrome in obesity. Arch Dis Child. 2005;90(1):10–14. doi: 10.1136/adc.2003.036467. https://doi.org/10.1136/adc.2003.036467. PMid:15613503. PMCid:PMC1720077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hagman E, Arani PI, Fischer M, et al. Blood sugar levels are higher in obese young children in Sweden than in Poland. Acta Paediatr. 2014;103(11):1174–8. doi: 10.1111/apa.12760. https://doi.org/10.1111/apa.12760. PMid:25060480. [DOI] [PubMed] [Google Scholar]
- 54.Hagman E, Reinehr T, J Kowalski J, et al. Impaired fasting glucose prevalence in two nationwide cohorts of obese children and adolescents. Int J Obes (Lond) 2014;38(1):40–45. doi: 10.1038/ijo.2013.124. https://doi.org/10.1038/ijo.2013.124. PMid:23828099. PMCid:PMC3884136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yuri YPM, Pateda V, Tirtamulya K, et al. Profile of fasting blood glucose in obese children with insulin resistance. International Journal of Pediatric Endocrinology 2013. 2013;(Suppl 1):P100. https://doi.org/10.1186/1687-9856-2013-S1-P100. PMCid:PMC3890975. [Google Scholar]
- 56.Grandone A, Amato A, Luongo C, et al. High-normal fasting glucose levels are associated with increased prevalence of impaired glucose tolerance in obese children. J Endocrinol Invest. 2008;31(12):1098–102. doi: 10.1007/BF03345659. https://doi.org/10.1007/BF03345659. PMid:19246977. [DOI] [PubMed] [Google Scholar]
- 57.Pulgaron ER, Delamater AM. Obesity and Type 2 Diabetes in Children: Epidemiology and Treatment. Curr Diab Rep. 2014;14(8):508. doi: 10.1007/s11892-014-0508-y. https://doi.org/10.1007/s11892-014-0508-y. PMid:24919749. PMCid:PMC4099943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guglielmi V, Cardellini M, Cinti F, et al. Omental adipose tissue fibrosis and insulin resistance in severe obesity. Nutr Diabetes. 2015;10(5):e175. doi: 10.1038/nutd.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ricco RC, Ricco RG, Almeida CA, et al. Comparative study of risk factors among children and adolescents with an anthropometric diagnosis of overweight or obesity. Rev Paul Pediatr. 2010;28(4):320–5. https://doi.org/10.1590/S0103-05822010000400006. [Google Scholar]


