This cost-effectiveness analysis evaluates the use of magnetic resonance imaging vs no follow-up after a normal computed tomographic finding in a model of obtunded blunt trauma.
Key Points
Question
What is the optimal follow-up strategy to clear the cervical spine in patients with obtunded blunt trauma after a normal computed tomographic finding?
Findings
In this cost-effectiveness analysis, magnetic resonance imaging had a lower health benefit (24.02 quality-adjusted life-years) and a higher cost ($14 185) compared with no follow-up (24.11 quality-adjusted life-years and $1059) after a normal computed tomographic finding in patients with obtunded blunt trauma to the cervical spine. The conclusion was robust in probabilistic sensitivity analysis and multiple 1- and 2-way sensitivity analyses.
Meaning
Magnetic resonance imaging may have a lower health benefit and a higher cost compared with no follow-up after a normal computed tomographic finding in patients with obtunded blunt trauma of the cervical spine.
Abstract
Importance
Magnetic resonance imaging (MRI) continues to be performed for cervical clearance of obtunded blunt trauma, despite poor evidence regarding its utility after a normal computed tomographic (CT) finding.
Objective
To evaluate the utility and cost-effectiveness of MRI vs no follow-up after a normal cervical CT finding in patients with obtunded blunt trauma.
Design, Setting and Participants
This cost-effectiveness analysis evaluated an average patient aged 40 years with blunt trauma from an institutional practice. The analysis used a Markov decision model over a lifetime horizon from a societal perspective with variables from systematic reviews and meta-analyses and reimbursement rates from the Centers for Medicare & Medicaid Services, National Spinal Cord Injury Database, and other large published studies. Data were collected from the most recent literature available.
Interventions
No follow-up vs MRI follow-up after a normal cervical CT finding.
Results
In the base case of a 40-year-old patient, the cost of MRI follow-up was $14 185 with a health benefit of 24.02 quality-adjusted life-years (QALY); the cost of no follow-up was $1059 with a health benefit of 24.11 QALY, and thus no follow-up was the dominant strategy. Probabilistic sensitivity analysis showed no follow-up to be the better strategy in all 10 000 iterations. No follow-up was the better strategy when the negative predictive value of the initial CT was relatively high (>98%) or the risk of an injury treated with a cervical collar turning into a permanent neurologic deficit was higher than 25% or when the risk of a missed injury turning into a neurologic deficit was less than 58%. The sensitivity and specificity of MRI were varied simultaneously in a 2-way sensitivity analysis, and no follow-up remained the optimal strategy.
Conclusions and Relevance
Magnetic resonance imaging had a lower health benefit and a higher cost compared with no follow-up after a normal CT finding in patients with obtunded blunt trauma to the cervical spine, a finding that does not support the use of MRI in this group of patients. The conclusion is robust in sensitivity analyses varying key variables in the model. More literature on these key variables is needed before MRI can be considered to be beneficial in the evaluation of obtunded blunt trauma.
Introduction
Cervical spine injuries occur in as many as 4% of patients with blunt trauma, and unstable injury can result in neurologic sequelae if the patient is not immobilized in a timely fashion.1,2,3,4 The optimal mechanism for spinal clearance has not been without controversy, especially in unevaluable patients with obtunded injury. Computed tomographic (CT) 64-section scans have been proposed to be sufficient to clear significant cervical spine injury5; however, the methods of such studies have been questioned.6 Follow-up magnetic resonance imaging (MRI) is frequently used in patients with normal CT findings and is being advocated for further assessment of soft-tissue (ligamentous) injury owing to its superior contrast resolution.5,7 This support comes despite the limited availability, prolonged scan time, risk of complications during transportation, the need for safety screening, and the relatively high cost of MRI.
Multiple studies8,9,10,11,12,13,14 have been published evaluating the utility of MRI for assessing stability in the context of blunt trauma after a normal CT finding in the cervical spine; opposing conclusions have led to uncertainty in the current literature. A previous meta-analysis15 quantified the rate of unstable injuries detected by MRI that were missed on initial CT and found the utility of MRI to be low. The pooled incidence of reported, unstable, missed injury on CT was only 0.017% among patients with obtunded trauma.16 Significant heterogeneity exists in the literature regarding the selection criteria for MRI, sensitivity and specificity of MRI, incidence of unstable injury, and incidence of unstable injury resulting in spinal cord injury.16 However, the high cost of missed unstable injuries and its potential neurologic sequelae are often the clinical justification for performing an MRI examination after a normal finding on CT of the cervical spine. A comprehensive analysis in 199617 concluded that the estimated total annual cost of all cervical spinal cord injuries in the United States was $9.7 billion per year. This cost includes initial cost of care in the first year, recurring cost of direct care, and indirect costs owing to loss of economic activity. In a more recent study from Canada,18 the estimated lifetime economic burden per individual ranged from $1.5 million for incomplete paraplegia to $3.0 million for complete tetraplegia.
The purpose of this study was to perform a cost-effectiveness analysis of MRI in patients with obtunded (Glasgow Coma Scale score, <13 of a possible 15 [lower scores indicate more severe injury]) blunt trauma after a normal finding on CT of the cervical spine to assess stability. The primary reason for performing MRI in patients with blunt trauma is to look for instability that may need a cervical collar or surgical fixation for immobilization. We conducted this study to assess pertinent factors that might affect decision making regarding the role of MRI and its cost implications by comparing the 2 follow-up strategies.
Methods
We performed a modeling-based economic decision analysis from a societal perspective. By using computational simulation, decision analytic modeling can be considered as an alternative to performing a large-cohort randomized clinical trial. The advantages include being able to compare several strategies and to estimate the optimal imaging based on the most favorable ratio of benefits to costs. A Markov model design represents the clinical pathways in patients with blunt cervical trauma with the anticipated implications of the imaging results on downstream processes of directing clinical care and using health care resources, patient outcomes, and health care costs. The model was programmed using TreeAge Pro software (version 2017; TreeAge Software, Inc) with a branching structure in the chronological order of the imaging, treatment, and outcome events that occur in the clinical pathway (Figure 1). Because no actual patients were involved in this study, approval by an institutional review board was not required.
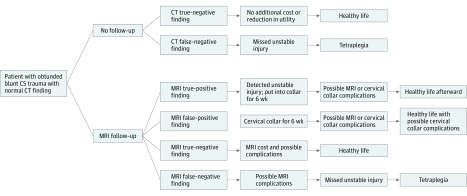
Figure 1. Simplified Flowchart of the Decision Tree.
CS indicates cervical spine; CT, computed tomography; and MRI, magnetic resonance imaging.
The 2 strategies being compared were no follow-up after a normal CT finding and follow-up with MRI. A hybrid Markov model with an annual 3% discount rate was used, with Bayesian probability leading to patient outcomes and a subsequent Markov model assessing lifetime effect of the outcome on health benefits and costs. The number of Markov cycles depends on a 40-year-old patient’s life expectancy at a particular health state. The life expectancies were derived from the National Spinal Cord Injury Database.19
Model Design
The base case scenario of the model was a 40-year-old patient with obtunded (Glasgow Coma Scale score, <13) blunt cervical trauma and a normal finding on initial non–contrast-enhanced CT of the cervical spine. In the strategy with no follow-up, true- and false-negative initial CT findings were considered. In the true-negative case, the patient was assumed to live a healthy life with no additional cost or reduction in utility. In the false-negative case, we assumed the patient might develop a spinal cord injury (SCI), incurring significant cost and disutility. Spinal cord injury can result in a spectrum of neurologic outcomes, with tetraplegia being the worst.19
The following 4 possible scenarios were considered on follow-up MRI: true-positive, false-positive, true-negative, and false-negative results. In the true-negative arm, the patient would be cleared from cervical spine injury and have the additional cost of MRI but no reduction in utility. In the true- and false-positive cases, the patient would be put into a semirigid cervical collar for 6 weeks, with temporary disutility and risk of having a collar-associated pressure ulcer. The true-positive case may still have a permanent neurologic deficit from the SCI. A false-negative case would carry the risk of missed injury that develops into SCI and subsequently tetraplegia. Patients with detected unstable injury could recover fully after collar immobilization or still develop permanent neurologic deficits. The complications from collar immobilization and intubations included pressure ulcer, venous thromboembolism, and catheter-associated complications. We also included the probability of ventilator-associated pneumonia owing to MRI positioning and secondary brain injury during MRI transportation.
Clinical Variables
Most of the clinical variables were derived from the best evidence in the current literature. According to the National Spinal Cord Injury Database,19 the life expectancy after SCI with low-level tetraplegia in an individual aged 40 years is 24 years, whereas life expectancy in a similar healthy patient is 40 years. We similarly ran the model for patients with SCI at 20 years of age (life expectancy is 59 years without SCI and 40 years with SCI) and at 60 years of age (life expectancy is 23 years without SCI and 10 years with SCI).19 The numbers of the Markov cycle were thus assigned accordingly. The negative predictive value (NPV) of the initial CT finding was assigned based on the reported unstable injury missed by the initial CT but detected on MRI follow-up from the pooling of 23 studies. Of the 3370 patients with obtunded trauma, only 4 unstable injuries were reported, for an NPV of 99.88%.15 The major complications of collar and intubation included pressure ulcer at a reported rate of 5.2% by Como et al,20 catheter-associated complications at a rate of 5.7%,20 and venous thromboembolism at a rate of 7.9% reported by Stelfox et al.21
In the MRI arm, we used a 79.6% sensitivity and 60.0% to 75.0% specificity for MRI in detecting SCI, as reported by Martínez-Pérez et al22 and Muchow et al,8 respectively. We also included possible complications of MRI positioning and transportation among patients with obtunded trauma, with a 34.3% risk of ventilator-associated pneumonia reported by Stelfox et al21 and a 9.3% risk of secondary brain injury reported by Dunham et al.23
Davis et al24 found that of 32 117 patients with trauma, 740 (2.3%) had cervical spine injuries and 34 of these (4.6%) had a delayed or a missed diagnosis based on cervical spine CT. Of the 34 patients, 10 (29.4%) developed a permanent neurologic deficit as a result of these delays.
The probability of having an SCI after a patient with an unstable injury received a collar was assigned to be 55% according to Parashari et al.25 A simplified flowchart for the decision tree is included in Figure 1.
Cost and Health States
All cost variables were derived from the 2015 Medicare national reimbursement values26 whenever possible. The values were assigned a normal distribution with an SD of 10% to reflect regional variability in the sensitivity analysis. The costs of collar complication and SCI were obtained from the literature, adjusted to the 2015 purchasing power.19,27 They were assigned to have a gamma distribution to allow for a wider range.
The utilities of different health states were measured in quality-adjusted life- years (QALY), a multifactorial measure that considers life expectancy and quality of life. The healthy state had a value of 1.00 per year; having a detected unstable injury with full recovery was assumed to have utility of 0.75 for the first 6 months and 1.00 for the next 6 months.28 After recovery, the patient was assumed to have the full QALY in each subsequent year. Cervical collar use would last for 6 weeks and result in half of the current health state during that time. Patients with tetraplegia would have 0.39 QALY in each Markov cycle.29 Temporary disutility was also assigned to all cervical collar– and MRI-related complications for 1 year and would have no effect on the patient’s subsequent quality of life. If the patient was to experience more than 1 complication or condition, the costs would be cumulative and the lowest utility among the conditions would be assigned. A complete list of variables is presented in the Table.30,31,32,33
Table. List of All Model Variables.
| Variable | Value | Distribution (Distribution Variable) | Source |
|---|---|---|---|
| Clinical probability | |||
| Life expectancy without spinal cord injury, y | 40 (mean) | NA | Spinal Cord Injury Model System,19 2014 |
| Life expectancy with spinal cord injury, y | 21 (mean) | NA | Spinal Cord Injury Model System,19 2014 |
| NPV of initial CT scan, % | 99.88 | Beta (3366, 4) | Malhotra et al,15 2017 |
| Missed unstable injuries that develop into SCI, % | 29 | NA | Davis et al,24 1993 |
| Patients with SCI who develop tetraplegia, % | 55 | Beta (48, 92) | Dunham et al,23 2008 |
| Sensitivity of MRI, % | 79.6 | NA | Martínez-Pérez et al,22 2014 |
| False-positive rate of MRI (1 – specificity), % | 25-40 | Uniform | Muchow et al,8 2008 |
| Probability of developing pressure ulcer, % | 5.2 | Beta (6, 109) | Como et al,20 2007 |
| Probability of developing catheter-associated complications, % | 5.7 | Beta (8, 132) | Stelfox et al,21 2007 |
| Probability of developing VTE, % | 7.9 | Beta (11, 129) | Stelfox et al,21 2007 |
| Probability of developing VAP, % | 34.3 | Beta (48, 92) | Dunham et al,23 2008 |
| Probability of developing secondary brain injury, % | 9.3 | NA | Stelfox et al,21 2007; Dunham et al,23 2008 |
| Cost, $ US | |||
| MRI | 371.85a | Normal (SD, 10%) | Medicare reimbursement |
| Cervical collar | 76.39b | Normal (SD, 10%) | Medicare reimbursement |
| Pressure ulcer | 2928c | Gamma (SD, 10%) | Padula et al,27 2011 |
| Catheter-associated complications | 29 156 | Gamma (SD, 10%) | Ertel et al,30 2016 |
| VTE | 12 381 | Gamma (SD, 10%) | Ertel et al,30 2016 |
| VAP | 28 508 | Gamma (SD, 10%) | Ertel et al,30 2016 |
| Secondary brain injury | 42 574 | Gamma (SD, 10%) | Ertel et al,30 2016 |
| Tetraplegia in first year | 771 000c | Gamma (SD, 10%) | Spinal Cord Injury Model System,19 2014 |
| Tetraplegia in subsequent year | 114 000c | Gamma (SD, 10%) | Spinal Cord Injury Model System,19 2014 |
| Loss of productivity due to tetraplegia | 20 898c | Gamma (SD, 10%) | Berkowitz et al,17 1998 |
| Discount, % | 3 | NA | NA |
| Utility value | |||
| Healthy without SCI | 1.00 | NA | Reference standard |
| SCI first year | 0.88d | NA | Lin et al,28 2012; Garcia et al,29 2014 |
| Cervical collar use | 0.95 | NA | Ertel et al,30 2016 |
| Pressure ulcer | 0.68 | NA | Fleurence,31 2005 |
| Catheter-associated complications | 0.53 | NA | Ertel et al,30 2016 |
| VTE | 0.88 | NA | Locadia et al,32 2004 |
| VAP | 0.88 | NA | Hamel et al,33 2000 |
| Secondary brain injury | 0.20 | NA | Dunham et al,23 2008 |
| Persistent neurologic sequelae | 0.39 | NA | Lin et al,28 2012; Garcia et al,29 2014 |
Abbreviations: CPT, Current Procedural Terminology; CT, computed tomographic; MRI, magnetic resonance imaging; NA, not applicable; NPV, negative predictive value; SCI, spinal cord injury; VAP, ventilator-associated pneumonia; VTE, venous thromboembolism.
CPT code 72141 with technical component.
CPT code L0140.
Adjusted to 2015 purchasing power.
For first 6 months, 0.75; for next 6 months, 1.00.
Statistical Analysis
The primary measure used in this study was net monetary benefit, which is defined as expected utility × willingness to pay – cost. The measure was used to determine the optimal strategy in sensitivity analyses, because a strategy with higher net monetary benefit is more desirable.
We performed the base case calculation using the mean value for each variable. We performed probabilistic sensitivity analysis simulating 10 000 iterations by varying all input variables in the model, thus modeling 10 000 patients, to assess the stability of the model results. In addition, key variables, including the NPV of the initial CT finding, the percentage of missed SCIs developing into tetraplegia, the percentage of patients with cervical collars who developed tetraplegia, and the risk of MRI complications were varied for a wide range in sensitivity analyses. Threshold values of these variables that could potentially affect the results of the model were reported. Two-way sensitivity analysis was performed by varying the sensitivity and specificity of MRI.
Results
Base Case Calculation
In the base case calculation for a patient aged 40 years, the mean values for each variable are used. The MRI follow-up was strictly dominated by no follow-up with a higher cost and a lower health benefit. The results showed that the cost of MRI follow-up was $14 185 with a utility of 24.02 QALY; the cost of no follow-up was $1059 with a utility of 24.11 QALY. For a 20-year-old patient with SCI, the cost of MRI follow-up was $14 703 with a utility of 28.41 QALY; the cost of no follow-up was $1361 with a utility of 28.50 QALY. For a 60-year-old patient with SCI, the cost of MRI follow-up was $13 529 with a utility of 17.35 QALY; the cost of no follow-up was $676 with a utility of 17.44 QALY. The higher cost and lower utility of MRI were primarily driven by the complications of prolonged cervical collar use and the limited benefit of MRI after a normal cervical CT finding. We used the 40-year age group for all the subsequent sensitivity analyses.
Probabilistic Sensitivity Analysis
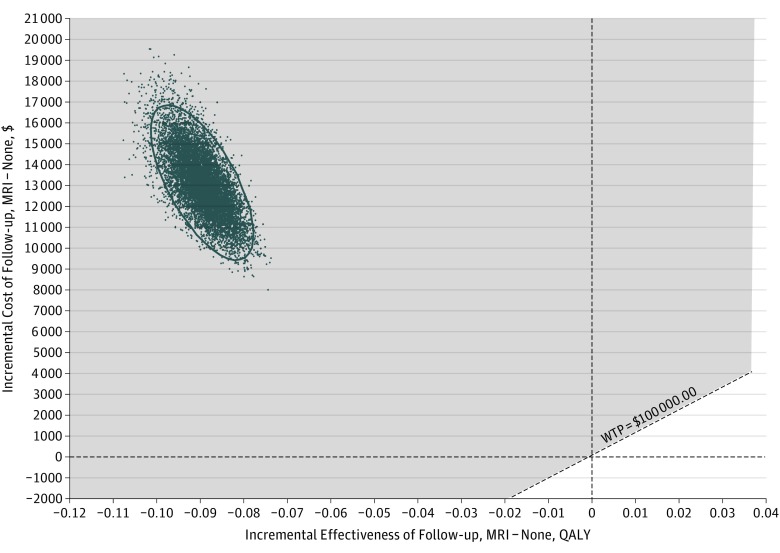
We performed probabilistic sensitivity analysis simulation with 10 000 iterations. The mean (SD) cost for MRI follow-up was $14 174 ($1788). The utility was 24.02 (0.01) QALY. The mean cost for no follow-up was $1063 ($539). The utility was 24.11 (0.003) QALY. No follow-up was a better strategy in all 10 000 iterations (Figure 2).
Figure 2. Incremental Cost-effectiveness for Magnetic Resonance Imaging (MRI) vs No Follow-up.
The scatterplot depicts 10 000 iterations in the probabilistic sensitivity analysis. No follow-up is the better strategy in all iterations. The shaded area corresponds to cases in which no follow-up is a better strategy than MRI. QALY indicates quality-adjusted life-year; WTP, willingness to pay.
Sensitivity Analyses
To evaluate the robustness of the conclusions against some key variables and assumptions, we performed multiple 1-way and 2-way sensitivity analyses. The NPV of the initial CT was assigned as 99.88% based on the previous meta-analysis in the base case calculation.15
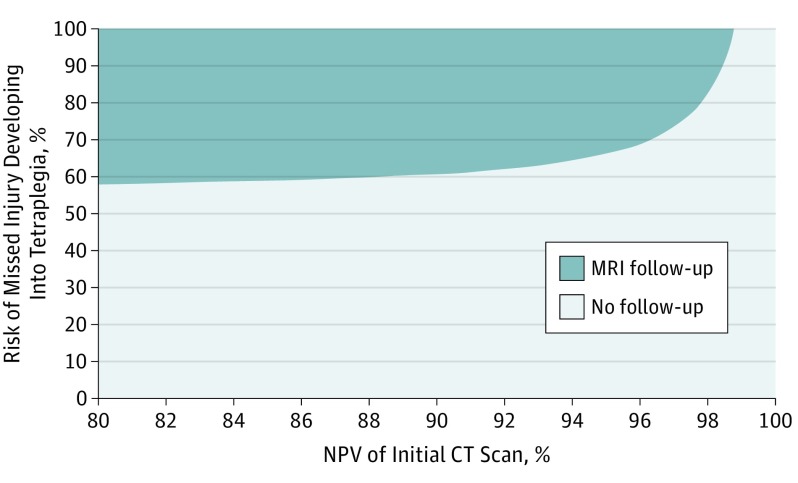
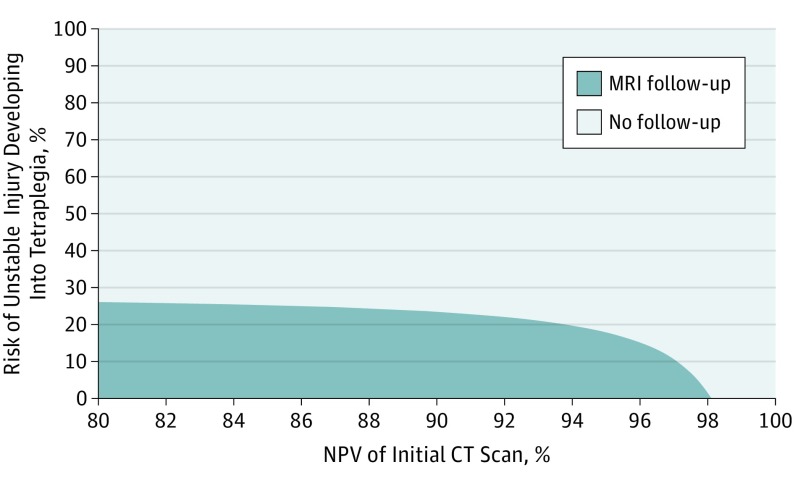
The percentage of missed unstable injuries on initial CT findings that developed into permanent neurologic injuries (tetraplegia in this case) was assigned as 29% according to Davis et al.24 In the 2-way sensitivity analysis, the probability of a missed unstable injury turning into tetraplegia varied from 0 to 100%, and the NPV of the initial CT varied from 80% to 100%. When the NPV of the initial CT was greater than 98%, no follow-up was the better strategy regardless of the risk of missed unstable injuries developing to tetraplegia. When the risk was higher than 60% and the NPV was lower than 94%, MRI follow-up should be performed (Figure 3). The probability of an unstable injury treated with a cervical collar still developing SCI also varied from 0 to 100%, along with the NPV of the initial CT. Again, when the NPV was higher than 98%, no follow-up remained the more cost-effective strategy regardless of the risk of an unstable injury treated with a cervical collar developing into tetraplegia. When the NPV was lower than 90% and the risk was lower than 25%, MRI follow-up was more cost-effective (Figure 4).
Figure 3. Two-Way Sensitivity Analysis Varying the Negative Predictive Value (NPV) of the Initial Computed Tomographic (CT) Scan and the Percentage of Missed Unstable Injuries Turning Into Spinal Cord Injuries.
The colors on the graph represent the areas where the corresponding strategy is better (higher net monetary benefit defined as utility × willingness to pay – cost, where willingness to pay is $100 000.00). MRI indicates magnetic resonance imaging.
Figure 4. Two-Way Sensitivity Analysis Varying the Negative Predictive Value (NPV) of the Initial Computed Tomographic (CT) Scan and the Percentage of Collared Unstable Injuries Turning Into Spinal Cord Injuries.
The colors on the graph represent the areas where the corresponding strategy is better (higher net monetary benefit defined as utility × willingness to pay – cost, where willingness to pay is $100 000.00). MRI indicates magnetic resonance imaging.
The sensitivity of MRI was set to be 79.6%, and the specificity was a uniform distribution from 60% to 75%. Both values were varied simultaneously in a 2-way sensitivity analysis, and no follow-up remained the optimal strategy, assuming an NPV of initial CT of 99.88%.
A relative paucity of literature exists regarding complications due to MRI transportation and positioning in patients with blunt trauma. Stelfox et al21 reported a 34.3% risk of ventilator-associated pneumonia, and Dunham et al23 reported a 9.3% risk of secondary brain injury. We varied the incidence of ventilator-associated pneumonia across an appropriate range of values from 0 to 50% and of secondary brain injury due to MRI transportation from 0 to 20%. The conclusions remained robust despite the variability in the risk of complications (eFigures 1 and 2 in the Supplement).
Discussion
The current decision tree model reported a lower cost of no follow-up compared with the cost of the MRI follow-up strategy. In the base case calculation, MRI follow-up had an expected cost of $14 185 and utility of 24.02 QALY per patient, whereas no follow-up had an expected cost of $1059 and utility of 24.11 QALY per patient. The difference in utility is equivalent to a mean (SD) of 32.85 (3.81) additional days in a fully healthy state.
The primary aim of clearing the cervical spine after blunt trauma remains the detection of unstable injury and the prevention of adverse neurologic sequelae from cord injury. The National Emergency X-Radiography Utilization Study (NEXUS)34 and the Canadian C-Spine Rule Study35,36 have previously demonstrated that imaging is unnecessary in awake and alert patients who are neurologically intact and without distracting injury.
Hadley et al37 have advocated MRI for further imaging in patients with obtunded trauma or those who are clinically unevaluable. The Eastern Association for the Surgery of Trauma guidelines38 were recently revised to recommend the removal of the cervical collar in patients with obtunded trauma after a normal high-quality CT finding alone. Although this recommendation is based on level III evidence, the clinical use of MRI in this patient population remains widespread.38 A recent cost-effectiveness analysis30 found MRI not to be cost-effective for cervical spine clearance in patients with obtunded blunt trauma. However, these investigators did not consider the MRI sensitivity, specificity, and risk of unstable injury resulting in cord injury.
A previous meta-analysis15 concluded that the utility of MRI in detecting unstable cervical injury after a normal CT finding was relatively limited and that additional studies are needed, including cost-effectiveness analysis. In the present study, we attempted to identify the key variables and their influence on the cost-effectiveness of MRI follow-up.
The literature is relatively lacking on the incidence of SCI turning into permanent neurologic deficits, which can be a spectrum of outcomes with tetraplegia as the worst. For this model, tetraplegia was used as the outcome of SCI, because a less severe outcome would favor no follow-up more. The lifetime cost of missed SCI was extracted from the National Spinal Cord Injury Database,19 which includes yearly health care and living expenses for disability. The detailed calculations to reach these values were not available on the website but reflect costs adjusted to 2015 purchasing power. The cost assigned to a patient with tetraplegia was $771 000 in the first year and $114 000 in every subsequent year.19 In contrast, in the MRI strategy, all cost variables except for the cost of complications due to cervical collars were Medicare reimbursement values, which represent a lower bound for estimated costs. The cost of MRI was only $372 in the model, and the cost of a cervical collar was $76, both of which are disproportionate to the actual incurred costs. As a result, the model results are likely an underestimation of the cost difference between the 2 strategies.
Magnetic resonance imaging has been reported to have a false-positive rate for ligamentous injury ranging from 25% to 40%, and patients could subsequently be given cervical collars or undergo surgery, which would incur additional costs, disutility, and risks of complications.8,39 The proportion of patients undergoing surgery after a false-positive MRI finding could be challenging to estimate accurately; thus, we assumed that all patients would only be given cervical collars in the model, with lower cost and mild disutility. The cost of the MRI strategy would be significantly higher, and effectiveness lower if operations were taken into account in place of cervical collar immobilization.
Some studies have assumed MRI to have perfect sensitivity. However, several false-negative MRI cases have been reported, and the limited literature on validation with anatomical and surgical studies shows poor correlation with MRI findings.40,41 Martínez-Pérez et al22 reported a sensitivity of 79.6% for MRI. Our sensitivity analysis showed a limited influence of MRI performance (sensitivity and specificity) on the final model results.
Limitations
Although guidelines recommend performing MRI within 48 to 72 hours, they are not supported by the literature.42 Such recommendations frequently result in patients undergoing urgent MRIs in the emergency department, often at an additional cost. Limited availability of MRI in many hospitals also potentially delays discharge until the MRI is performed and, in our experience, this delay is often used as a reason to expedite the MRI. Patients with soft-tissue injuries detected on MRI have also been shown to undergo early surgical stabilization more frequently and have a longer hospital length of stay.43 All these factors have not been included in the current model but are likely to adversely affect the MRI follow-up strategy.
Detection of incidental findings on additional imaging (MRI in this study) is known to cause increases in subsequent costs. This fact was not factored into the model because it would be difficult to incorporate. However, detection of incidental findings is likely to make the MRI follow-up strategy less cost-effective.
Conclusions
Our cost-effectiveness analysis showed MRI to have a lower health benefit and a higher cost compared with no follow-up after a normal finding of a CT scan for spine instability in patients with obtunded blunt cervical spine trauma. The conclusion was robust in sensitivity analyses varying key variables in the model (ie, NPV of CT, sensitivity and specificity of MRI, complication rate due to MRI, percentages of missed and unstable injury turning into SCI). More literature on these key variables is needed before MRI can be considered to be beneficial in evaluation of patients with obtunded, blunt trauma. As the Choosing Wisely Campaign is taking root among clinicians, increased awareness and discussion of the risks vs benefits of MRI in blunt trauma will lead to a more objective evaluation of its utility.
eFigure 1. Sensitivity Analysis Varying the Risk of Ventilator-Associated Pneumonia
eFigure 2. Sensitivity Analysis Varying the Risk of Secondary Brain Injury
References
- 1.Goldberg W, Mueller C, Panacek E, Tigges S, Hoffman JR, Mower WR; NEXUS Group . Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. 2001;38(1):17-21. [DOI] [PubMed] [Google Scholar]
- 2.Grossman MD, Reilly PM, Gillett T, Gillett D. National survey of the incidence of cervical spine injury and approach to cervical spine clearance in US trauma centers. J Trauma. 1999;47(4):684-690. [DOI] [PubMed] [Google Scholar]
- 3.Hasler RM, Exadaktylos AK, Bouamra O, et al. . Epidemiology and predictors of cervical spine injury in adult major trauma patients: a multicenter cohort study. J Trauma Acute Care Surg. 2012;72(4):975-981. [DOI] [PubMed] [Google Scholar]
- 4.Lowery DW, Wald MM, Browne BJ, Tigges S, Hoffman JR, Mower WR; NEXUS Group . Epidemiology of cervical spine injury victims. Ann Emerg Med. 2001;38(1):12-16. [DOI] [PubMed] [Google Scholar]
- 5.Daffner RH, Weissman BN, Wippold FJ, et al; Expert Panels on Musculoskeletal and Neurologic Imaging. American College of Radiology Appropriateness Criteria: Suscepted Spine Trauma. https://acsearch.acr.org/list. Reviewed 2012. Accessed July 17, 2015.
- 6.Wu X, Forman HP, Kalra VB, Malhotra A. Letter to the Editor regarding “sixty-four-slice computed tomographic scanner to clear traumatic cervical spine injury: systematic review of the literature”. J Crit Care. 2015;30(5):1141-1142. [DOI] [PubMed] [Google Scholar]
- 7.Resnick DK. Updated guidelines for the management of acute cervical spine and spinal cord injury. Neurosurgery. 2013;72(suppl 2):1. [DOI] [PubMed] [Google Scholar]
- 8.Muchow RD, Resnick DK, Abdel MP, Munoz A, Anderson PA. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma. 2008;64(1):179-189. [DOI] [PubMed] [Google Scholar]
- 9.Russin JJ, Attenello FJ, Amar AP, Liu CY, Apuzzo ML, Hsieh PC. Computed tomography for clearance of cervical spine injury in the unevaluable patient. World Neurosurg. 2013;80(3-4):405-413. [DOI] [PubMed] [Google Scholar]
- 10.Schoenfeld AJ, Bono CM, McGuire KJ, Warholic N, Harris MB. Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma. 2010;68(1):109-113. [DOI] [PubMed] [Google Scholar]
- 11.James IAO, Moukalled A, Yu E, et al. . A systematic review of the need for MRI for the clearance of cervical spine injury in obtunded blunt trauma patients after normal cervical spine CT. J Emerg Trauma Shock. 2014;7(4):251-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raza M, Elkhodair S, Zaheer A, Yousaf S. Safe cervical spine clearance in adult obtunded blunt trauma patients on the basis of a normal multidetector CT scan: a meta-analysis and cohort study. Injury. 2013;44(11):1589-1595. [DOI] [PubMed] [Google Scholar]
- 13.Badhiwala JH, Lai CK, Alhazzani W, et al. . Cervical spine clearance in obtunded patients after blunt traumatic injury: a systematic review. Ann Intern Med. 2015;162(6):429-437. [DOI] [PubMed] [Google Scholar]
- 14.Wu X, Kalra VB, Forman HP, Malhotra A. Letter to the Editor regarding “is magnetic resonance imaging in addition to a computed tomographic scan necessary to identify clinically significant cervical spine injuries in obtunded blunt trauma patients?”. Am J Surg. 2016;211(4):825-826. [DOI] [PubMed] [Google Scholar]
- 15.Malhotra A, Wu X, Kalra VB, et al. . Utility of MRI for cervical spine clearance after blunt traumatic injury: a meta-analysis. Eur Radiol. 2017;27(3):1148-1160. [DOI] [PubMed] [Google Scholar]
- 16.Malhotra A, Wu X, Kalra VB, Schindler J, Forman HP. Cost-effectiveness analysis of follow-up strategies for thunderclap headache patients with negative non–contrast CT. Acad Emerg Med. 2016;23(3):243-250. [DOI] [PubMed] [Google Scholar]
- 17.Berkowitz M, O’Leary P, Kruse DL, Harvey C. Spinal Cord Injury: An Analysis of Medical and Social Costs. New York, NY: Demos Medical Publishing; 1998. [Google Scholar]
- 18.Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33(3):113-122. [PubMed] [Google Scholar]
- 19.Spinal Cord Injury Model System Spinal cord injury (SCI) facts and figures at a glance. https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202014.pdf. August 2014. Accessed June 24, 2015.
- 20.Como JJ, Thompson MA, Anderson JS, et al. . Is magnetic resonance imaging essential in clearing the cervical spine in obtunded patients with blunt trauma? J Trauma. 2007;63(3):544-549. [DOI] [PubMed] [Google Scholar]
- 21.Stelfox HT, Velmahos GC, Gettings E, Bigatello LM, Schmidt U. Computed tomography for early and safe discontinuation of cervical spine immobilization in obtunded multiply injured patients. J Trauma. 2007;63(3):630-636. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-Pérez R, Paredes I, Cepeda S, et al. . Spinal cord injury after blunt cervical spine trauma: correlation of soft-tissue damage and extension of lesion. AJNR Am J Neuroradiol. 2014;35(5):1029-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dunham CM, Brocker BP, Collier BD, Gemmel DJ. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12(4):R89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma. 1993;34(3):342-346. [DOI] [PubMed] [Google Scholar]
- 25.Parashari UC, Khanduri S, Bhadury S, et al. . Diagnostic and prognostic role of MRI in spinal trauma, its comparison and correlation with clinical profile and neurological outcome, according to ASIA impairment scale. J Craniovertebr Junction Spine. 2011;2(1):17-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Medicare & Medicaid Services. Physician Fee Schedule https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/index.html?redirect=/physicianFeeSched/. Modified November 2, 2017. Accessed November 6, 2015.
- 27.Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care. 2011;49(4):385-392. [DOI] [PubMed] [Google Scholar]
- 28.Lin M-R, Yu W-Y, Wang S-C. Examination of assumptions in using time tradeoff and standard gamble utilities in individuals with spinal cord injury. Arch Phys Med Rehabil. 2012;93(2):245-252. [DOI] [PubMed] [Google Scholar]
- 29.Garcia A, Liu TH, Victorino GP. Cost-utility analysis of prehospital spine immobilization recommendations for penetrating trauma. J Trauma Acute Care Surg. 2014;76(2):534-541. [DOI] [PubMed] [Google Scholar]
- 30.Ertel AE, Robinson BR, Eckman MH. Cost-effectiveness of cervical spine clearance interventions with litigation and long-term-care implications in obtunded adult patients following blunt injury. J Trauma Acute Care Surg. 2016;81(5):897-904. [DOI] [PubMed] [Google Scholar]
- 31.Fleurence RL. Cost-effectiveness of pressure-relieving devices for the prevention and treatment of pressure ulcers. Int J Technol Assess Health Care. 2005;21(3):334-341. [DOI] [PubMed] [Google Scholar]
- 32.Locadia M, Bossuyt PM, Stalmeier PF, et al. . Treatment of venous thromboembolism with vitamin K antagonists: patients’ health state valuations and treatment preferences. Thromb Haemost. 2004;92(6):1336-1341. [DOI] [PubMed] [Google Scholar]
- 33.Hamel MB, Phillips RS, Davis RB, et al. . Outcomes and cost-effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med. 2000;109(8):614-620. [DOI] [PubMed] [Google Scholar]
- 34.Griffith B, Bolton C, Goyal N, Brown ML, Jain R. Screening cervical spine CT in a level I trauma center: overutilization? AJR Am J Roentgenol. 2011;197(2):463-467. [DOI] [PubMed] [Google Scholar]
- 35.Duane TM, Wilson SP, Mayglothling J, et al. . Canadian Cervical Spine Rule compared with computed tomography: a prospective analysis. J Trauma. 2011;71(2):352-355. [DOI] [PubMed] [Google Scholar]
- 36.Paxton M, Heal CF, Drobetz H. Adherence to Canadian C-Spine Rule in a regional hospital: a retrospective study of 406 cases. J Med Imaging Radiat Oncol. 2012;56(5):514-518. [DOI] [PubMed] [Google Scholar]
- 37.Hadley MN, Walters BC, Grabb PA, et al. . Radiographic assessment of the cervical spine in asymptomatic trauma patients. Neurosurgery. 2002;50(3)(suppl 3):S30-S35. [DOI] [PubMed] [Google Scholar]
- 38.Patel MB, Humble SS, Cullinane DC, et al. . Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;78(2):430-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu X, Kalra VB, Forman HP, Malhotra A. Letter to the Editor regarding “adjacent level ligamentous injury associated with traumatic cervical spine fractures: indications for imaging and implications for treatment”. World Neurosurg. 2016;86:6. [DOI] [PubMed] [Google Scholar]
- 40.Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol. 2007;28(2):209-215. [PMC free article] [PubMed] [Google Scholar]
- 41.Wu X, Kalra VB, Forman HP, Malhotra A. Letter to the Editor regarding “systematic review of flexion/extension radiography of the cervical spine in trauma patients”. Eur J Radiol. 2015;84(12):2686-2687. [DOI] [PubMed] [Google Scholar]
- 42.Ryken TC, Hadley MN, Walters BC, et al. . Radiographic assessment. Neurosurgery. 2013;72(suppl 2):54-72. [DOI] [PubMed] [Google Scholar]
- 43.Awad BI, Carmody MA, Lubelski D, et al. . Adjacent level ligamentous injury associated with traumatic cervical spine fractures: indications for imaging and implications for treatment. World Neurosurg. 2015;84(1):69-75. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Sensitivity Analysis Varying the Risk of Ventilator-Associated Pneumonia
eFigure 2. Sensitivity Analysis Varying the Risk of Secondary Brain Injury