Abstract
Background
Healthcare providers and law enforcement (LE) officers are among the most common first responders to injuring events. Despite frequent interface between the health system (HS) and LE sectors, the published evidence that supports their collaboration in injury surveillance, control and prevention has not been comprehensively reviewed.
Methods
We conducted a scoping review of literature published from 1990 to 2016 that focused on local and regional HS and LE collaborations in injury surveillance, control and prevention. Our aim was to describe what is known and what remains unexplored about these cross-sector efforts.
Results
128 articles were included in the final review. These were categorised by their focus on either surveillance activities or partnerships in injury control and prevention programmes. The majority of surveillance articles focused on road traffic injuries. Conversely, articles describing partnerships and programme evaluations primarily targeted the prevention of interpersonal violence.
Discussion
This review yielded two major findings: overall, the combination of HS and LE injury data added value to surveillance systems, especially as HS data augmented LE data; and HS and LE partnerships have been developed to improve injury control and prevention. However, there are few studies that have evaluated the impact and sustainability of these partnerships.
Conclusions
The current evidence to support HS and LE collaboration in injury surveillance and control and prevention programmes is heterogeneous. Notable gaps suggest ample opportunity for further research and programme evaluation across all types of injury.
INTRODUCTION
Injury, both intentional (eg, interpersonal violence) and unintentional (eg, MVCs), is among the top 10 causes of morbidity and mortality worldwide. A recent global estimate suggests that on a yearly basis, 973 million people sustain injuries requiring medical treatment.1 Assessing the impact of injury and the enactment of effective injury prevention programmes and policies is not possible without quality surveillance.2 Yet, there is rarely a single sector that can provide the totality of accurate and reliable injury surveillance data or respond to it effectively.3
Health systems (HS), where the injured are cared for, and public safety agencies like law enforcement (LE) are typically the first responders to injuring events and supply a first line of injury surveillance data. Partnerships between HS and LE (HS-LE) may improve injury surveillance and enable multisector injury control and prevention efforts.4 Indeed, both HS and LE stakeholders ‘share a common goal… to have safer communities.’4 Moreover, injury prevention, if achieved, reduces burdens on both health and LE systems.
Multisector injury surveillance partnerships that include the HS, LE and other health and safety agencies create the opportunity to link injury data from different sources to identify where and to whom injuries are occurring. Foremost multisector injury surveillance partnerships in the US are the National Violent Death Reporting System (NVDRS) and Crash Outcome Data Evaluation System (CODES). NVDRS, created in 2002 and implemented in 40 states, centralises data on violent deaths collected from local medical examiners, coroners and LE agencies, as well as toxicology and vital statistics reports. This repository provides a clearer understanding of the incidence and prevalence of fatal violence which has been used to guide local, regional and national prevention efforts.5 CODES was developed through a partnership between the US National Highway Traffic Safety Administration and individual states to integrate data on crash, vehicular and driver characteristics (collected as part of the Fatality Analysis Reporting System or FARS) with medical and economic outcomes. This has yielded a more comprehensive surveillance system as well as evidence of the benefit of linked data to guide and improve highway and traffic safety.6
Despite the evidence that supports multisector systems and the day-to-day interface of HS employees like physicians and nurses in the Emergency Department (ED) and LE officers,7 the body of evidence that supports direct HS-LE collaboration in injury surveillance and response has not been comprehensively reviewed. The scope of these ‘bilateral’ efforts may yield under-recognised local and regional improvements in injury surveillance and prevention. These collaborations may also be less resource and logistically intensive when compared with large, national, multisector systems. We therefore reviewed the published evidence that has focused on joint HS-LE injury surveillance and response to describe what is known and what remains unexplored about these collaborations.
METHODS
Using Arskey and O’Malley’s framework, we conducted a scoping review8 of published literature from 1990 to 2016. To identify the extent, range and nature of relevant studies, we searched three primary databases that capture publications across biomedicine, public health and criminal justice. These included: Scopus (which catalogues 100% of Medline content), Embase with Medline suppressed to limit duplication and the National Criminal Justice Reference Service (NCJRS). Each database was queried for the following terms that were chosen for relevancy to the unique intersection between HS and LE data for injury surveillance and control: ‘police hospital partnership,’ ‘medical police partnership,’ ‘hospital law enforcement partnership,’ ‘hospital police injury prevention,’ ‘hospital law enforcement injury prevention,’ ‘emergency department police,’ ‘emergency department law enforcement,’ ‘medical police data injury,’ ‘medical law enforcement data injury’ and ‘cops and docs.’
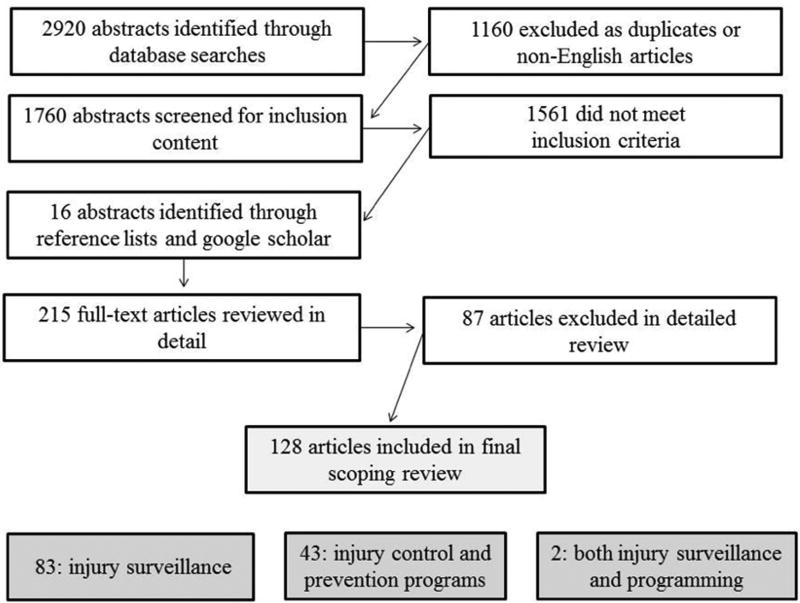
This published literature search was conducted in November 2015 and updated in June 2016 with additional confirmation and grey literature data capture achieved through review of the reference lists of included articles and a web search using Google Scholar. A total of 2920 publications were identified across all sources (figure 1). Duplicate, non-English language and articles concerning mental health interventions, psychiatric care, mental health referrals, suicide, substance abuse only (inclusive of drug and/or alcohol abuse), occupational health of LE professionals, police partnerships with non-HS partners, broad multisector systems (data linkage at a broad national or multistate level) and disaster response were excluded. A total of 1760 abstracts were reviewed to assess the extent to which articles met inclusion criteria which required report of original content and focus on joint HS-LE data for surveillance activities or programmatic partnership in injury prevention and control. From this abstract review, 215 full text articles were identified for detailed review.
Figure 1.
Health system-law enforcement literature review.
Two research team members reviewed articles to: confirm inclusion criteria, code for geographic context and injury focus (type or mechanism) and categorise how each article’s content conveyed evidence related to HS-LE collaboration in injury surveillance and partnership. Any discrepancies in this detailed review were resolved through consensus. After detailed abstract and article text assessment, 128 articles were included in this scoping review (figure 1). Count data were analysed and mapped using R V.3.1.1.
RESULTS
Geographic distribution and content focus
The publications included in this review described injury research that has been conducted worldwide (figure 2). This includes research from nine global regions (using the Stern regional classification system) and 32 individual countries. The majority of research was concentrated in the US (n=43), UK (n=40) and Australia (n=12). Across all settings, the most common study focus (figure 3) was road traffic injuries (n=62), followed by interpersonal violence (n=40), substance abuse-involved injuries (n=11), multiple mechanisms of injury (n=7), other aspects of HS-LE collaboration (eg, logistics of partnerships; n=5) and emergency response (n=3).
Figure 2.
Published health system-law enforcement collaboration articles by world region Note: Darker shading indicates a greater number of articles published. Some articles included data from more than one country and are counted multiple times. Countries represented include (in order of most published articles to least): US, UK, Australia, Hong Kong, Pakistan, Canada, France, New Zealand, China, Finland, Iran, Netherlands, Norway, Austria, Bangladesh, Czech Republic, Ethiopia, Germany, Ghana, Greece, Hungary, India, Israel, Italy, Mali, Mexico, Nicaragua, Portugal, Spain, Sri Lanka, Switzerland and Vietnam.
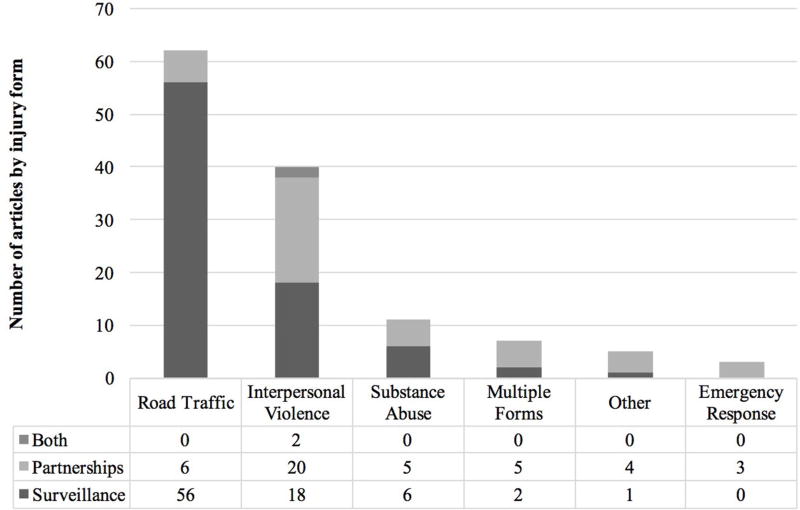
Figure 3.
Total number of health system-law enforcement articles by mechanism of injury or partnership intent. Note: Substance abuse category includes partnerships that include substance abuse-involved unintentional or intentional injury (eg, alcohol-related MVCs). Multiple forms category includes both unintentional and intentional injuries.
HS-LE in injury surveillance, control and prevention
We identified two overarching categories of published literature in our scoping review: (1) joint HS-LE data for injury surveillance activities (n=83) and (2) HS-LE partnerships for injury control and prevention (n=43). Two articles fell into both categories. Articles included in the surveillance category (online supplementary table 1) describe differences and complementing factors between HS and LE data and explore methodological advancements in data linkage using these sources. Articles included in the partnerships category (online supplementary table 2) explore the development and implementation of joint HS-LE injury control and prevention programmes and cross-sectoral relationships at the local and regional level.
HS-LE data in injury surveillance activities
There were 85 published articles that examined outcomes, methodology and comparative accuracy of HS and LE data sources in injury surveillance (figure 3). The majority of these articles (n=56) use HS and LE data to illustrate the epidemiology of road traffic injuries, including bicycle and pedestrian injuries. A smaller number (n=18) engaged HS and LE data sources for violent injury surveillance.
Differences identified between HS and LE data sources
HS and LE data generated different epidemiological profiles of road traffic injuries across the same population. For example, Gill et al found that the reduction in road traffic fatalities that had been identified through LE data in England was likely due to missing data and not a true decline. Hospital admission records for the same time period demonstrated a higher rate of injury that more closely matched previous years.9 In fact, all but one study10 found that when compared with HS records, LE records underestimated the incidence of road traffic injuries.
Differences in how, when and to whom a road traffic injury occurred changed the likelihood that it was captured in HS and/or LE records. Injuries associated with clinical presentations subject to legal statutes (eg, high blood alcohol levels) were most likely to appear in both HS and LE records.11 Temporal factors like hospital length of stay, the month of the year or the day of week also changed the likelihood of record overlap. In a New Zealand study, for example, the month in which a crash took place predicted the likelihood that HS records would correspond to LE reports for the same injury.12 Record capture was also shown to vary by the demographic characteristics (age, race and ethnicity) of the injured. In a study of paediatric RTC injuries in Long Beach California, injuries in younger children, Asian children and Hispanic children were more likely to be captured solely in HS records when compared with older children or White and African American children.13 Finally, by comparing HS and LE data, researchers identified that LE records tended to overestimate road traffic injury severity when compared with formal clinical evaluations in the hospital.11,14
The studies that compared HS data and LE data for violent injuries similarly identified important differences between the data captured by each source. Through a firearm injury database that combined ED, LE, Medical Examiner (ME) and emergency call system data in Atlanta, Georgia, researchers identified that all fatal gunshot injuries were known to LE. LE records, however, underestimated the rate of non-fatal gunshot injuries when compared with HS records.15 The demographic characteristics of those injured by violence also changed the likelihood of capture in HS or LE records. In one study, assaults in men were more likely to be exclusively recorded in HS records whereas assaults in women were more likely to be exclusively recorded in LE records.16
Linking HS-LE data
Researchers compensated for the relative ‘blind spots’ in HS and LE injury data by developing linked databases. In general, these linked databases offered more robust estimates of injury rates when compared with either HS or LE data alone. However, inconsistencies in the quality or availability of either HS or LE records were shown to limit the accuracy and reliability of linked data.9,17–19
In the earliest published linkage evaluation, Rosman and Knuiman reported that 64% of Australian road traffic injury records could be linked using HS-LE data.14 The ability to link data was significantly lower for injuries of lesser severity and for motorcycle crash injuries (compared with four-wheel MVC injuries).20 The type of HS has also been associated with the ability to link injury data. In one study, private hospitals had the lowest percentage of HS-LE record overlap (31%), followed by county hospitals (57%) and public metropolitan hospitals (62%). The highest percentage of linked records was found when comparing LE and teaching hospitals, where the most severe injuries were treated (72%).20 Another study found that HS records were less likely to be linked to LE reports when only one vehicle was involved, hospital length of stay was shorter or when passengers were younger than 20 years of age.18
Methodological approaches for improving the yield of linked HS-LE data were also identified in studies in this review. Specifically, capture-recapture methods are described as a way to improve HS-LE injury surveillance. Capture-recapture is a method in which two independent samples (HS and LE) of injured individuals are used to estimate the true burden of injury across a specific geography. All studies that used this method noted its limitations when the completeness and independence of HS and LE records were unknown.11,13,21,22 Other methodological evaluations addressed the relative sensitivity and specificity14 and influence of sample selection bias on the predictive value of HS and LE data for estimating of injury rates.23
Identifying injury risk factors
Two publications included in this review described how well HS and LE data identified select risk factors for injuries. Orsay et al found that despite being able to link over 70% of hospital admission records to LE records at a major trauma centre in Chicago, Illinois, LE had identified only 31.2% of injured motorists with blood alcohol concentrations above the legal limit and 15% of injured motorists with a positive drug screen.24 In New South Wales, Australia, using linked HS and LE records, Brown and Bilson identified the increased risk of severe injuries to rear seat passengers when compared with front seat drivers and passengers.25
HS-LE in injury control and prevention partnerships
There were 45 published articles that described and/or evaluated HS-LE programmes for injury control and prevention. These articles focused on partnerships that were formed to: prevent or respond to violence (n=22), road traffic injuries (n=6), substance abuse-related injuries (n=5) and multiple mechanisms of injuries (n=5), or described the logistics of HS-LE collaborations (n=4) and HS-LE emergency response activities (n=3).
Partnerships for violence control and prevention
The vast majority of articles (n=23) in this category focused on the Cardiff Violence Prevention Program (Cardiff Model). This programme has been adopted by the National Health System across the UK and replicated in other countries.26 The Cardiff Model uses injury data collected in hospital EDs to enhance records of assaults to LE. Data from each source are shared and compared to generate hotspot maps that can be used by violence prevention working groups to build local policies and programmes to reduce violence and injuries.27–30 Evaluation of this model has demonstrated that it reduces the rate of violence-related injury and is cost-effective.31,32
Other articles on HS-LE partnerships for violence control and prevention examined a single, unreplicated programme. The initiative ‘Operation Blade’ in Scotland was established to reduce knife-related assaults. This programme consisted of a media campaign, knife amnesty collections, stop and search campaigns, increased safety at public venues and educational outreach to knife retailers and secondary school students. Programme evaluation revealed that stabbings decreased for 10 months following Operation Blade, but returned to preintervention rates 1 year later.33
All remaining publications on HS-LE partnerships for violence and violent injury control were descriptive and did not evaluate the injury prevention impact of partnerships efforts. The Harstad Injury Prevention Study conducted in Harstad and Trondheim, Norway outlined the development of an injury prevention working group with representation from a hospital and public and private organisations.34 An article highlighting the Consortium of Law Enforcement and Private Security (CLEPS) in El Paso, Texas described how a hospital security team and LE formed a partnership through the development of enhanced reporting procedures, crime briefings and consortium bylaws.35 Karchmer et al described a programme through which police chiefs reached out to public health organisations to address issues involving deaths and mass casualties so that LE-public health organisations (eg, hospitals, health departments) could work together to develop prevention plans.36
Two articles describe the role of ED nurses in partnered HS-LE injury control initiatives. In the ‘Cops-Docs Handcuff-in-Glove’ programme, ED nurses facilitated comprehensive screening and data collection to assist forensic investigations for victims of violent assault.37 Another coalition in New Hampshire in the US improved communication and safety of hospital staff through collaborative nurse-LE development of occupational safety policy to reduce hospital staff assaults.38
Physician training programmes are also described as an opportunity to build HS-LE partnerships for injury control and prevention. Within the department of Emergency Medicine at the University of New Mexico, a medical resident used analysis of unintentional gunshot fatalities and their associated risk factors to inform the work of the New Mexico Zero Tolerance Team. This community action team which included HS, LE, medical and other stakeholders used a map of childhood firearm deaths to focus community resources on addressing youth firearm fatality prevention.39 Doezema similarly described how a medical resident’s participation in a death review team for domestic violence-related homicide victims resulted in more complete case reports.40
Finally, a handful of articles review the key components that authors discovered in the development of HS-LE partnerships. Petch outlines best practices identified during implementation of UK’s Safety Matters programme which brought together multiple agencies including the HS and LE to address violent injuries.41 In their experience, developing a multiagency programme required attention to: communication and information sharing, organisational cultures and the development of explicit roles and responsibilities. Additionally, Hunt and van der Arend conducted a small exploratory qualitative study in the UK and Netherlands that identified ethical considerations in HS-LE partnerships including information sharing and medical confidentiality/client consent, public safety and organisational accountability.42
Partnerships for road traffic injury control and prevention
The published literature also included descriptions of HS-LE partnerships for road traffic injury control and prevention.39,43–46 In Pakistan, LE and physicians collaborated to create and implement a LE-led Emergency Medical Systems (EMS) programme called Rescue 15.46 A different Pakistani programme, in the city of Karachi, established a partnership between hospitals, LE agencies, industry and media and developed a road traffic injury surveillance system and safety-focused road design.39 In addition, HS-LE partnerships are described that expanded to include other stakeholder groups (eg, businesses, insurance providers)39,43 in efforts to develop road traffic injury surveillance partnerships,45 as well as to address injury risk factors like teen driving44 and alcohol consumption.45
Partnerships for emergency response
Three studies described how coalitions centred around HS-LE partnerships can help prepare communities for coordinated emergency response.47–49 Two studies explored the inclusion of a surgeon in emergency response teams: Metzger described the effectiveness of integrating a physician in an LE special operations team to provide immediate medical support50 and Kaplan examined the cost-effectiveness of a tactical police surgeon (TPS) on a Special Weapons and Tactics (SWAT) team, concluding that TPS was a cost-effective for both LE and the hospital.51 A similar report examined feasibility and efficiency of tactical emergency medicine support (TEMS) integration within LE teams.52
Emerging models for HS-LE injury prevention partnerships
Research identified in this review also explored how new kinds of injury surveillance data can be integrated in HS-LE injury prevention efforts. In Hong Kong, geographic information system (GIS) data were used in conjunction with HS-LE data to identify ‘hot zones’ where there were hazardous road conditions that would benefit from low-cost remedial, and injury prevention, measures.53 Schuch et al analysed school transport pathways and child injury data through GIS to better understand the environmental context in which risk for injury was highest.54 In two Australian cities, a project targeted alcohol-related injuries reviewed HS-LE data, observation of alcohol-serving establishments and interview data from key community members to inform alcohol-related injury harm reduction interventions.55 Finally, in another Australian study, evaluation of a pilot model to use ED data to enhance alcohol-related injury surveillance and cross-sector prevention programme integrated closed-circuit television data within the suite of data used to inform programme activities.56
DISCUSSION
This scoping review of 25 years of published evidence suggests that HS-LE collaborations offer promising approaches for injury surveillance, control and prevention at the local and regional level. HS-LE data linkage improved injury surveillance, and the creation of HS-LE partnerships resulted in new and expanded injury control and prevention programmes. Nonetheless, there are notable gaps in the current body of literature. The majority of evidence on HS-LS surveillance focused on road traffic injuries. Conversely, articles on HS-LE collaborations primarily described programmes that targeted the reduction of interpersonal violence. This suggests ample opportunity for further research across mechanisms of injury. Other than studies of the Cardiff Model and broad multisector systems (eg, NVDRS and CODES; excluded from this review), we were unable to find evaluations of how well HS-LE data linkage and injury prevention partnerships sustain the impact of their collaboration over time. In addition, there are no studies, beyond the Cardiff Model, that have evaluated the benefits of HS-LE partnerships in the context of their required financial investments.
Current evidence is also largely focused on urban settings and in the US, UK and Australia. This is likely because the availability of data systems for HS and LE surveillance can be costly and resource intensive, and that the concentration of injury is highest in cities. The process and benefit of HS-LE collaboration warrant further study in rural communities and settings where there are limited resources for emergency medical care and LE work. Consequently, it is in these contexts that HS-LE partnerships for injury surveillance and prevention may offer the most cost-effectiveness and strengthen the capacity for injury response due to leveraging efforts from both the HS and LE sectors. Additionally, rural areas may benefit from greater surveillance of access to HS-LE services and the potential for under-reporting of injury in rural areas.
The results of this scoping review should be interpreted within the context of its limitations. The published literature included in the review is based on select search terms which may not have captured all that has been published to describe HS-LE sector collaborations for injury surveillance, control and prevention. We also are limited to publications available in the English language and catalogued within Scopus, Embase and NCJRS. These databases have wide and interdisciplinary capture but it is possible that there are HS-LE related publications published in other languages or not included in these sources. In particular, evaluations for programmes that are emerging in practice may be documented in white papers and other grey literature that are more challenging to identify. For example, the value added from linked HS-LE for the surveillance and programmatic response to the epidemic of opioid overdose was not captured in this review.57 Nonetheless, such published sources outside of the formal literature are generally less detailed in the description of evaluation and outcome methodology and may have some limitation in its comparability to published research. Furthermore, this review did not assess US national and broad multisector systems such as NVDRS and CODES, of which HS and LE partners may be listed among several partners. In spite of these limitations, to our knowledge, this is the first review to broadly describe injury-related evidence for HS-LE collaborations.
This review suggests that there are often blind spots in LE and HS data and that even linked databases can contain incomplete information. Extension of current data sources and methods that can advance the technical efficacy of data linkage will undoubtedly enhance the field. The inclusion of new sources such as EMS and ME data may create more robust injury surveillance databanks.58,59 However, even with multiple sources, missing data challenges the ability to link cases and identify accurate estimates. Therefore, the development and evaluation of imputation and data linkage methods continue to be essential for HS-LE collaboration in injury surveillance and response. Other research materials from population-based or patient surveys60 can improve the appraisal of the accuracy and reliability of HS-LE data. Continued use and development of injury surveillance research may lead to improved data quality and provide more informative data to guide prevention programming. Further description and evaluation of HS-LE partnerships that have built effective cross-sectoral relationships is also needed to replicate and extend the evidence that supports HS-LE partnerships for injury control and prevention. With this evidence, HS-LE programmes, implemented worldwide, have the potential to build more comprehensive injury surveillance data and enable the most effective cross-sectoral opportunities to improve public health.
Supplementary Material
What is already known on the subject
-
►
Partnerships between health systems and law enforcement have the potential to improve injury surveillance and enable multisector injury control and prevention efforts.
-
►
The evidence to support health system and law enforcement collaboration at the local and regional level has not been subject to comprehensive review.
What this study adds
-
►
Review of 128 articles published between 1990 and 2016 resulted in two major findings: health system and law enforcement data linkage improved injury surveillance and health system and law enforcement partnerships resulted in the implementation of injury control and prevention programmes.
-
►
This review revealed the heterogeneous focus and methodology of the current body of evidence suggesting opportunity for further research and programme evaluation.
Acknowledgments
Funding Support for this research was provided by the Piloting the Cardiff Model for Violence Prevention Program, a joint project of the CDC Foundation and the Robert Wood Johnson Foundation, in colloboration with the Centers for Disease Control and Prevention and the University of Pennsylvania.
Footnotes
Contributors SFJ and LMMK shared the role of lead author. All authors have made substantive contributions to the conceptualisation, methodological approach and manuscript development for this review.
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allegrante JP, Mitchell RJ, Taylor JA, et al. Injury surveillance: the next generation. Inj Prev. 2016;22(Suppl 1):i63–5. doi: 10.1136/injuryprev-2015-041943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kellermann AL, Bartolomeos KK. Firearm injury surveillance at the local level from data to action. Am J Prev Med. 1998;15(3 Suppl):109. doi: 10.1016/s0749-3797(98)00061-0. [DOI] [PubMed] [Google Scholar]
- 4.Hargarten SW, Waeckerle JF. Docs and cops: a collaborating or colliding partnership? Ann Emerg Med. 2001;38:438–40. doi: 10.1067/mem.2001.118615. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. [accessed 11 May 2016];National violence death reporting system. 2016 http://www.cdc.gov/violenceprevention/nvdrs/publications.html.
- 6.National Highway Traffic Safety Administration. [accessed 11 May 2016];Crash outcome data evaluation system publications. 2015 https://crashstats.nhtsa.dot.gov/#/PublicationList/27.
- 7.Jones PM, Appelbaum PS, Siegel DM Massachusetts Work Group on Law Enforcement Access to Hospital Patients. Law enforcement interviews of hospital patients: a conundrum for clinicians. JAMA. 2006;295:822. doi: 10.1001/jama.295.7.822. [DOI] [PubMed] [Google Scholar]
- 8.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 9.Gill M, Goldacre MJ, Yeates DG. Changes in safety on England’s roads: analysis of hospital statistics. BMJ. 2006;333:73. doi: 10.1136/bmj.38883.593831.4F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant RJ, Gregor MA, Maio RF, et al. The accuracy of medical records and police reports in determining motor vehicle crash characteristics. Prehosp Emerg Care. 1998;2:23–8. doi: 10.1080/10903129808958835. [DOI] [PubMed] [Google Scholar]
- 11.Aptel I, Salmi LR, Masson F, et al. Road accident statistics: discrepancies between police and hospital data in a French island. Accid Anal Prev. 1999;31:101–8. doi: 10.1016/s0001-4575(98)00051-7. [DOI] [PubMed] [Google Scholar]
- 12.Alsop J, Langley J. Under-reporting of motor vehicle traffic crash victims in New Zealand. Accid Anal Prev. 2001;33:353–9. doi: 10.1016/s0001-4575(00)00049-x. [DOI] [PubMed] [Google Scholar]
- 13.Dhillon PK, Lightstone AS, Peek-Asa C, et al. Assessment of hospital and police ascertainment of automobile versus childhood pedestrian and bicyclist collisions. Accid Anal Prev. 2001;33:529–37. doi: 10.1016/s0001-4575(00)00066-x. [DOI] [PubMed] [Google Scholar]
- 14.Sciortino S, Vassar M, Radetsky M, et al. San Francisco pedestrian injury surveillance: mapping, under-reporting, and injury severity in police and hospital records. Accid Anal Prev. 2005;37:1102–13. doi: 10.1016/j.aap.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Kellermann AL, Bartolomeos K, Fuqua-Whitley D, et al. Community-level firearm injury surveillance: local data for local action. Ann Emerg Med. 2001;38:423–9. doi: 10.1067/mem.2001.117273. [DOI] [PubMed] [Google Scholar]
- 16.Sutherland I, Sivarajasingam V, Shepherd JP. Recording of community violence by medical and police services. Inj Prev. 2002;8:246–7. doi: 10.1136/ip.8.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cryer PC, Westrup S, Cook AC, et al. Investigation of bias after data linkage of hospital admissions data to police road traffic crash reports. Inj Prev. 2001;7:234–41. doi: 10.1136/ip.7.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson SJ, Begg DJ, Samaranayaka A. Validity of using linked hospital and police traffic crash records to analyse motorcycle injury crash characteristics. Accid Anal Prev. 2012;49:30–5. doi: 10.1016/j.aap.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Tin Tin S, Woodward A, Ameratunga S. Completeness and accuracy of crash outcome data in a cohort of cyclists: a validation study. BMC Public Health. 2013;13:420. doi: 10.1186/1471-2458-13-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosman DL, Knuiman MW. A comparison of hospital and police road injury data. Accid Anal Prev. 1994;26:215–22. doi: 10.1016/0001-4575(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 21.Amoros E, Martin JL, Lafont S, et al. Actual incidences of road casualties, and their injury severity, modelled from police and hospital data, France. Eur J Public Health. 2008;18:360–5. doi: 10.1093/eurpub/ckn018. [DOI] [PubMed] [Google Scholar]
- 22.Tercero F, Andersson R. Measuring transport injuries in a developing country: an application of the capture-recapture method. Accid Anal Prev. 2004;36:13–20. doi: 10.1016/s0001-4575(02)00109-4. [DOI] [PubMed] [Google Scholar]
- 23.Tarko A, Azam MS. Pedestrian injury analysis with consideration of the selectivity bias in linked police-hospital data. Accid Anal Prev. 2011;43:1689–95. doi: 10.1016/j.aap.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 24.Orsay EM, Doan-Wiggins L, Lewis R, et al. The impaired driver: hospital and police detection of alcohol and other drugs of abuse in motor vehicle crashes. Ann Emerg Med. 1994;24:51–5. doi: 10.1016/s0196-0644(94)70162-8. [DOI] [PubMed] [Google Scholar]
- 25.Brown J, Bilston LE. The scope and nature of injuries to rear seat passengers in NSW using linked hospital admission and police data. Traffic Inj Prev. 2014;15:462–9. doi: 10.1080/15389588.2013.833662. [DOI] [PubMed] [Google Scholar]
- 26.Quigg Z, Hughes K, Bellis MA. Data sharing for prevention: a case study in the development of a comprehensive emergency department injury surveillance system and its use in preventing violence and alcohol-related harms. Inj Prev. 2012;18:315–20. doi: 10.1136/injuryprev-2011-040159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodwin V, Shepherd JP. The development of an assault patient questionnaire to allow accident and emergency departments to contribute to Crime and Disorder Act local crime audits. J Accid Emerg Med. 2000;17:196–8. doi: 10.1136/emj.17.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shepherd J, Lisles C. Towards multi-agency violence prevention and victim support: an investigation of police-accident and emergency service liaison. Br J Criminol. 1998;38:351–70. [Google Scholar]
- 29.Warburton AL, Shepherd JP. Development, utilisation, and importance of accident and emergency department derived assault data in violence management. Emerg Med J. 2004;21:473–7. [PMC free article] [PubMed] [Google Scholar]
- 30.Young CA, Douglass JP. Use of, and outputs from, an assault patient questionnaire within accident and emergency departments on Merseyside. Emerg Med J. 2003;20:232–7. doi: 10.1136/emj.20.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Florence C, Shepherd J, Brennan I, et al. An economic evaluation of anonymised information sharing in a partnership between health services, police and local government for preventing violence-related injury. Inj Prev. 2014;20:108–14. doi: 10.1136/injuryprev-2012-040622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kmietowicz Z. Sharing information on violence saved Cardiff 7m in health, legal, and social costs in 2007. BMJ. 2013;347:f5668. doi: 10.1136/bmj.f5668. [DOI] [PubMed] [Google Scholar]
- 33.Bleetman A, Perry CH, Crawford R, et al. Effect of Strathclyde police initiative “Operation Blade” on accident and emergency attendances due to assault. J Accid Emerg Med. 1997;14:153–6. doi: 10.1136/emj.14.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ytterstad B, Wasmuth HH. The Harstad Injury Prevention Study: evaluation of hospital-based injury recording and community-based intervention for traffic injury prevention. Accid Anal Prev. 1995;27:111–23. doi: 10.1016/0001-4575(94)00036-l. [DOI] [PubMed] [Google Scholar]
- 35.Cottrell PA, DeAngelis G. CLEPS: how police and hospital security work together in a large city. J Healthc Prot Manage. 1999;15:18–23. [PubMed] [Google Scholar]
- 36.Karchmer C, Tully P, Devlin L, et al. New pressures/new partnerships: public health and law enforcement. J Law Med Ethics. 2003;31(4 Suppl):52–3. doi: 10.1111/j.1748-720x.2003.tb00750.x. [DOI] [PubMed] [Google Scholar]
- 37.McCue C. Cops and Docs program brings police and ED staff together to address the cycle of violence. J Emerg Nurs. 2001;27:578–80. doi: 10.1067/men.2001.118760. [DOI] [PubMed] [Google Scholar]
- 38.Allen DE, Harris FN, de Nesnera A. Nurse-police coalition: improves safety in acute psychiatric hospital. J Psychosoc Nurs Ment Health Serv. 2014;52:27–31. doi: 10.3928/02793695-20140709-01. [DOI] [PubMed] [Google Scholar]
- 39.Razzak JA, Shamim MS, Mehmood A, et al. A successful model of road traffic injury surveillance in a developing country: process and lessons learnt. BMC Public Health. 2012;12:357. doi: 10.1186/1471-2458-12-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doezema D, McLaughlin S, Sklar DP. An approach to fulfilling the systems-based practice competency requirement. Acad Emerg Med. 2002;9:1355–9. doi: 10.1111/j.1553-2712.2002.tb01601.x. [DOI] [PubMed] [Google Scholar]
- 41.Petch A. Safety Matters: The role of partnership working in safeguarding adults. J Integr Care. 2008;16:39–40. [Google Scholar]
- 42.Hunt G, van der Arend A. Treatment, custody, support: an exploratory qualitative dialogue to map the ethics of interagency co-operation in hospital emergency departments in the UK and the Netherlands. J Interprof Care. 2002;16:211–20. doi: 10.1080/13561820220146658. [DOI] [PubMed] [Google Scholar]
- 43.Farrow J, Pham T. CHP:reducing traffic fatalities and injuries through cooperation and partnership. Law and Order. 2006;54:112–20. [Google Scholar]
- 44.Galey TM, Smith G. Recidivism rates of teen driving trauma prevention program in birmingham, alabama. J Invest Med. 2010;58:474. [Google Scholar]
- 45.Roeper P, Voas R, Padilla-Sanchez L, et al. A Long-term community-wide intervention to reduce alcohol-related traffic injuries Salinas, California. Drugs. 2000;7:51–60. [Google Scholar]
- 46.Ali M, Miyoshi C, Ushijima H. Emergency medical services in Islamabad, Pakistan: a public-private partnership. Public Health. 2006;120:50–7. doi: 10.1016/j.puhe.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Glick DF, Jerome-D’Emilia B, Nolan MA, et al. Emergency preparedness: one community’s response. Fam Community Health. 2004;27:266–73. doi: 10.1097/00003727-200407000-00014. [DOI] [PubMed] [Google Scholar]
- 48.Glow SD, Colucci VJ, Allington DR, et al. Managing multiple-casualty incidents: a rural medical preparedness training assessment. Prehosp Disaster Med. 2013;28:334–41. doi: 10.1017/S1049023X13000423. [DOI] [PubMed] [Google Scholar]
- 49.Jennings-Bey T, Lane SD, Rubinstein RA, et al. The trauma response team: a community intervention for gang violence. J Urban Health. 2015;92:947–54. doi: 10.1007/s11524-015-9978-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Metzger JC, Eastman AL, Benitez FL, et al. The lifesaving potential of specialized on-scene medical support for urban tactical operations. Prehosp Emerg Care. 2009;13:528–31. doi: 10.1080/10903120903144940. [DOI] [PubMed] [Google Scholar]
- 51.Kaplan LJ, Glenn KJ, Maung A, et al. Embedding a surgeon in a civilian tactical team reduces resource utilization and is cost effective. Am J Disaster Med. 2014;9:121–5. doi: 10.5055/ajdm.2014.0148. [DOI] [PubMed] [Google Scholar]
- 52.Vainionpää T, Peräjoki K, Hiltunen T, et al. Integrated model for providing tactical emergency medicine support (TEMS): analysis of 120 tactical situations. Acta Anaesthesiol Scand. 2012;56:158–63. doi: 10.1111/j.1399-6576.2011.02565.x. [DOI] [PubMed] [Google Scholar]
- 53.Loo BP, Chow CB, Leung M, et al. Multidisciplinary efforts toward sustained road safety benefits: integrating place-based and people-based safety analyses. Inj Prev. 2013;19:58–63. doi: 10.1136/injuryprev-2012-040400. [DOI] [PubMed] [Google Scholar]
- 54.Schuch L, Curtis JW, Curtis A, et al. Breaking out of surveillance silos: integrative geospatial data collection for child injury risk and active school transport. J Urban Health. 2016;93:36–52. doi: 10.1007/s11524-015-0006-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Miller P, Palmer D, Droste N, et al. Dealing with alcohol-related problems in the night-time economy: a study protocol for mapping trends in harm and stakeholder views surrounding local community level interventions. BMC Res Notes. 2011;4:204. doi: 10.1186/1756-0500-4-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Clough AR, Hayes-Jonkers CS, Pointing ES. Assault and licensed premises in inner-city areas. 2013 [Google Scholar]
- 57.Ohio Department of Health. [accessed 29 Jan 2017];2015 Ohio drug overdoes data: general findings. https://www.odh.ohio.gov/-/media/ODH/ASSETS/Files/health/injury-prevention/2015-Overdose-Data/2015-Ohio-Drug-Overdose-Data-Report-FINAL.pdf.
- 58.Spivak HR, Prothrow-Stith D. Addressing violence in the emergency department. Clin Pediatr Emerg Med. 2003;4:135–40. [Google Scholar]
- 59.Clark DE. Practical introduction to record linkage for injury research. Inj Prev. 2004;10:186–91. doi: 10.1136/ip.2003.004580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meuleners LB, Lee AH, Haworth C. Emergency presentations by vulnerable road users: implications for injury prevention. Inj Prev. 2006;12:12–14. doi: 10.1136/ip.2005.010389. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.