Abstract
Mindfulness-based intervention has become increasingly popular to address disinhibited eating in obesity and type 2 diabetes (T2D). Theoretically, present-moment attention promotes the ability to recognize and respond to internal hunger cues and to differentiate physiological hunger from other stimuli. Yet, there is limited research describing the relationship of mindfulness with disinhibited eating patterns in adolescents. In this study, we evaluated the relationship of dispositional mindfulness to laboratory eating in 107 adolescent (12–17 years) girls at risk for T2D. Adolescents reported dispositional mindfulness, were evaluated for recent loss-of-control-eating (LOC-eating) by interview, and participated in two successive, standardized laboratory test meals to assess eating when hungry as well as eating in the absence of hunger (EAH). Adolescents rated state appetite throughout the test meal paradigms. In analyses adjusting for body composition and other possible confounds, mindfulness was inversely related to caloric intake during the EAH paradigm. Mindfulness did not relate to energy intake when hungry. Instead, there was a significant interaction of reported LOC-eating by state hunger, such that girls with recent, reported LOC-eating and high state hunger consumed more calories when hungry, regardless of mindfulness. Findings suggest that in girls at risk for T2D, mindfulness may play a role in disinhibited eating. A propensity for LOC-eating may be most salient for overeating in a high hunger state.
Keywords: Adolescent, Mindfulness, Type 2 Diabetes, Loss-of-control, Eating in the Absence of Hunger, Disinhibited Eating
1. Introduction
Mindfulness refers to a non-judgmental state of purposeful awareness that brings attention to the present moment and allows for the recognition and consideration of internal and external experiences without the pressure to alter the moment or take immediate action (Kabat-Zinn, 1991). Mindfulness has dispositional or trait-like characteristics, but also may be learned and developed through training (Shapiro, Carlson, Astin, & Freedman, 2006). Mounting empirical evidence suggests that mindfulness promotes psychological and physical health through adaptive self-regulation, such as improved emotion regulation and fostering healthy eating (Creswell, 2017). In adults, mindfulness-based interventions have gained popularity as a therapeutic modality to address disinhibited eating patterns that contribute to obesity and type 2 diabetes (T2D) (Godfrey, Gallo, & Afari, 2015; Godsey, 2013). However, there is limited information expressly describing the relationship of dispositional mindfulness to disinhibited eating in adolescents at risk for adverse weight and metabolic outcomes.
Disinhibited eating refers to a lack of self-regulation over food consumption, including behaviors such as eating in the absence of hunger (EAH) and loss-of-control-eating (LOC-eating) (Shomaker, Tanofsky-Kraff, & Yanovski, 2011). EAH is the intake of palatable food in the absence of physiological hunger, in response to emotional and/or external cues such as the availability of highly palatable food (Kral & Faith, 2007), and EAH is a common form of disinhibited eating in youth with overweight and obesity (Shomaker, Tanofsky-Kraff, & Yanovski, 2011). Externality theory suggests that individuals prone to obesity are less sensitive to internal cues and highly sensitive to external cues to eat (Schachter & Rodin, 1974). In early studies, youth with obesity ate significantly more when presented with snacks (Costanzo & Woody, 1979) and were more influenced by external cues such as the availability or composition of food (Schachter, 1971; Schachter & Rodin, 1974) than youth who were lean. More recent studies also have demonstrated a positive cross-sectional association between EAH, as assessed by survey and test meal intake, with body mass index (BMI) in adolescents (Fisher et al., 2007; Shomaker et al., 2010).
Another prevalent form of disinhibited eating is LOC-eating, referring to perceived overeating accompanied by a subjective sense of not being able to control what or how much one is eating (American Psychiatric Association, 2013). The experience of LOC is frequently reported in adolescents with overweight and obesity (Tanofsky-Kraff, 2008; Tanofsky-Kraff et al., 2004; Vannucci et al., 2013) and in adolescents with obesity-related comorbidities including T2D (Wilfley et al., 2011). Youth who endorse LOC are more likely to gain excess weight and body fat over time (Field et al., 2012; Sonneville et al., 2013; Tanofsky-Kraff et al., 2009) and to show a worsening in components of metabolic health that elevate T2D risk (Kelly et al., 2015; Tanofsky-Kraff et al., 2012).
In theory, mindfulness is anticipated to relate inversely to disinhibited eating because present-moment attention should promote an individual’s ability to recognize and respond effectively to internal appetitive cues of hunger and satiety (Brown, Ryan, & Creswell, 2007). Moreover, attention to the present moment should support the differentiation between physiological hunger signals and other internal or external stimuli for eating, such as negative emotions or food availability (Brown et al., 2007; Olson & Emery, 2015). Nearly all existing studies characterizing the cross-sectional relationship of dispositional mindfulness with disinhibited eating have been conducted in adults. In healthy adult women, dispositional mindfulness was negatively related to a self-reported tendency to engage in disinhibited eating patterns, including eating in response to external food cues and negative affect (Lattimore, Fisher, & Malinowski, 2011). Likewise, in adults with T2D, mindfulness was inversely associated with self-reported eating in response to emotions or external cues (Tak et al., 2015). In other studies of non-clinical samples of adults using self-report surveys, dispositional mindfulness also has been inversely associated with reported eating in response to emotions (Pidgeon, Lacota, & Champion, 2013), disordered eating symptoms (Masuda, Price, & Latzman, 2012), and fewer symptoms of disinhibited-type eating disorders such as bulimia nervosa (Lavender, Jardin, & Anderson, 2009). In a prior cross-sectional study of overweight and obese adolescent girls, dispositional mindfulness was related to a lower odds of reported binge-eating, less frequent reported-EAH in response to fatigue or boredom, and less reinforcing value of food (Pivarunas et al., 2015). Although existing data have primarily relied upon self-reports of disinhibited eating, one previous study of college students found that an experimental mindfulness induction led to greater enjoyment of eating paired with less energy intake from unhealthy “junk” foods in the laboratory (Arch et al., 2016). These preliminary findings support a relationship between dispositional mindfulness and eating behavior, yet more evidence in adolescents using objective measurement of food intake is needed.
Adolescence is an important age span for understanding the association between mindfulness and disinhibited eating, particularly in girls. This period is frequently marked by the emergence of and worsening of disinhibited eating (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011; Stice, Shaw, & Marti, 2006). Girls, as compared to boys, are also more likely to endorse disinhibited eating behaviors in some studies (Ackard, Neumark-Sztainer, Story, & Perry, 2003; Neumark-Sztainer et al., 2011) and to have a greater risk for youth-onset T2D (Dabelea et al., 2014). Thus, understanding the relationship of mindfulness to disinhibited eating, especially in adolescent girls at high risk for T2D, has the potential to inform prevention efforts for T2D.
In the current study, we evaluated the association of mindfulness with laboratory eating behavior using two successive standardized, laboratory test meals that assess eating when hungry and EAH. Laboratory test meal studies avoid many of the confounding variables found within self-report, such as under-reporting (Goran, 1998; Lanctot, Klesges, Stockton, & Klesges, 2008; Tanofsky-Kraff, Haynos, Kotler, Yanovski, & Yanovski, 2007; Waling & Larsson, 2009). We anticipated that there would be an inverse relationship between mindfulness and EAH based on the notion that mindfulness encourages noticing, accepting, and differentiating among internal and external experiences (Hill et al., 2015), which may translate to an increased ability to self-regulate eating. Because mindfulness is related to reported LOC-eating patterns (Pivarunas et al., 2015), we sought to determine the relationship of mindfulness to EAH after accounting for LOC-eating, in order to ensure that any identified findings indicated a unique association of mindfulness with EAH. As a secondary objective, we explored the interaction of mindfulness and LOC in the prediction of laboratory eating behavior. Based on previous findings of other variables associated with eating and weight (Kelly et al., 2016; Shank et al., 2015; Stojek et al., 2017), we expected that reported LOC-eating status would exacerbate the inverse association of mindfulness with energy intake, such that being prone to uncontrolled eating in combination with less present-moment awareness would have the strongest effect on EAH. Finally, because attention (or lack of attention) to hunger cues is a key aspect of the conceptual model through which mindfulness regulates eating behavior (Brown et al., 2007; Schachter & Rodin, 1974), we adjusted for hunger state in all models and tested its interactions with mindfulness and LOC-eating.
2. Methods
2.1 Study sample
Participants in this cohort were healthy adolescent (12–17 years) girls recruited through the National Institutes of Health’s clinical trials website, local community postings in libraries and supermarkets, direct mailings to area families, and through notices to school parents’ listservs in Washington, DC and the greater metropolitan area. Recruitment materials targeted parents of adolescent girls who were concerned about their daughter being at risk for diabetes. All girls were determined to be at risk for T2D by having overweight or obesity (BMI ≥85th percentile) and having one or more first- or second-degree relative with prediabetes, T2D, or gestational diabetes. Other criteria for study inclusion were mild to moderately elevated depressive symptoms defined as a total score ≥16 on the Center for Epidemiologic Studies-Depression Scale (Radloff, 1977) and English-speaking. Exclusion criteria included current major depressive disorder or psychiatric symptoms requiring treatment; T2D (fasting glucose >126 mg/dL, 2-hour OGTT glucose >200 mg/dL); medication that could affect insulin resistance, body weight, or mood (such as antidepressants, stimulants, or insulin sensitizers); pregnancy; and current participation in weight loss or psychotherapy treatment programs. Adolescents provided written assent and their parents or guardians gave written consent for participation. The study was approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Adolescents were financially compensated for their time and inconvenience.
2.2 Study design
The current study represents a secondary data analysis of baseline data collected from 107 adolescent girls taking part in a randomized controlled trial addressing depressive symptoms as a contributor to worsening insulin resistance and T2D risk (Shomaker et al., 2016; Shomaker, Tanofsky-Kraff, Stern, et al., 2011). Primary results from the trial have been published elsewhere (Shomaker et al., 2016; Shomaker, Kelly, et al., 2017). This paper represents the first and only analysis of mindfulness in relationship to laboratory eating behavior in this cohort. Adolescents were seen at the National Institutes of Health Mark O. Hatfield Clinical Research Center following an overnight fast. All participants completed a medical history and a physical examination conducted by an endocrinologist or a nurse practitioner. Adolescents completed measurements of body composition, an interview to assess recent, reported LOC-eating behavior, questionnaires to evaluate dispositional mindfulness and depressive symptoms, and they participated in two successive test meals to objectively characterize eating when hungry and EAH.
2.3 Measures
2.3.1 Body composition
Height was measured to the nearest millimeter three times by stadiometer and fasting weight was measured to the nearest 0.1 kg on a calibrated scale. BMI was calculated as weight (kg) divided by the square of height (m) and BMI z scores were determined according to the Centers for Disease Control and Prevention 2000 standards (Kuczmarski et al., 2000). Percentage of body fat (fat mass/total body mass × 100) and lean mass (kg) were assessed with dual-energy X-ray absorptiometry (iDXA, GE Healthcare, Madison, WI).
2.3.2 Loss-of-control-eating (LOC-eating)
The reported presence of recent (past month) LOC-eating episodes were evaluated by trained interviewers with the Eating Disorder Examination (EDE) Overeating Section version 12.0D (Fairburn & Cooper, 1993). The EDE has shown good discriminant validity, internal consistency, and concurrent validity (Cooper, Cooper, & Fairburn, 1989) and has demonstrated good test-retest reliability (Rizvi, Peterson, Crow, & Agras, 2000). All interviews were audio-recorded and randomly selected EDEs were co-rated to verify inter-rater reliability for LOC-eating presence. For this study, participants reporting at least 1 episode in the past month of objective and/or subjective binge episodes were considered to have presence of LOC-eating.
2.3.3 Trait mindfulness
Dispositional mindfulness was assessed with the reliable and validated 15-item Mindful Attention and Awareness Scale (Brown & Ryan, 2003). In a recent systematic review, the MAAS has been shown to have adequate validity, internal consistency, and test-retest reliability in adolescents (Pallozzi, Wertheim, Paxton, & Ong, 2017). Using a Likert scale ranging from 1 (almost always) to 6 (almost never), participants answered items such as “I find myself doing things without paying attention.” The total score is calculated as the sum of all items; higher scores indicate more dispositional mindfulness.
2.3.4 Laboratory eating behavior: Eating while hungry and eating in the absence of hunger (EAH)
As part of a validated laboratory procedure to assess disinhibited eating in adolescents (Shomaker et al., 2010), individual participants were given a buffet lunch meal at approximately 12:00 pm and instructed to eat until no longer hungry. A lab staff member timed the meal with a stopwatch while the participant ate alone. The buffet lunch meal consisted of approximately 11,000 kcal and had multiple lunch food items, such as sandwich fixings, fruits, vegetables, and snack foods (e.g. pretzels, chips, and candy). Sixty minutes after the initiation of the lunch meal, participants were presented with a 4,055-kcal array of generous proportions of highly palatable, novel snack foods (e.g. popcorn, chips, candy, and ice cream). Participants were given the audio-recorded instructions to taste the foods, rate their liking/disliking for the foods on a brief rating form, and to eat as much of the foods as they would like. The examiner left the room for the 15-minute snack period. During this time, activities were made available including hand-held computer games, drawing, playing cards, and magazines.
Each food and drink item consumed from the lunch buffet meal and from the snack array was measured using the difference in weight (g) of each item before and after the meal. Energy (kcal) consumption was calculated using the US Department of Agriculture National Nutrient Database for Standard Reference and from the manufacturer labels on packaged food items. Eating while hungry was evaluated based on total energy (kcal) consumed at the lunch meal. EAH was assessed based on total energy (kcal) consumed during the snack array.
2.3.5 State hunger ratings
Adolescents completed brief state ratings of hunger directly before the lunch meal, directly after the lunch meal (and prior to the snacks), and directly after the snacks. They rated their subjective feelings of hunger on a visual analog scale ranging from 1 = “not at all” to 100 = “extremely.”
2.3.6. Depressive symptoms
The Center for Epidemiologic Studies-Depression Scales (Radloff, 1977) was used to determine inclusion eligibility (score ≥16) for the parent study, a randomized controlled trial examining depressive symptoms as a contributor to worsening insulin resistance and T2D risk (Shomaker et al., 2016; Shomaker, Tanofsky-Kraff, Stern, et al., 2011).
2.4 Data analysis
All analyses were conducted using IBM SPSS Statistics 23. Feasible outliers were winsorized in order to fall inside 1.5 times the interquartile range above the 75th percentile or below the 25th percentile, as is standard in Tukey’s boxplot (Tukey, 1977). For descriptive purposes, independent samples t-tests and chi-square statistics were conducted to compare adolescents with and without reported LOC-eating on key variables. State hunger was described before the meal and after the meal/before EAH for a validity check of the test meal paradigm. To address the primary objective of evaluating the association of dispositional mindfulness with EAH, hierarchical multiple regression models were performed with the dependent variable of EAH (snack energy intake, kcal). As a secondary outcome, we also evaluated eating while hungry (buffet meal energy intake, kcal) as a dependent variable. The covariates of age (years), race/ethnicity, body composition (percent body fat, lean mass, and height), and depressive symptoms were entered in the first step. We controlled for depressive symptoms to ensure that any relationships of mindfulness with eating behavior were not explained by depression (Mooreville et al., 2014). When evaluating EAH, buffet meal intake also was included as a covariate. In the second step of the models, reported hunger just prior to eating (meal or snacks) was included. In level three, the main effects of mindfulness and LOC-eating were entered. Finally, the two-way interactions among mindfulness, LOC-eating, and state hunger were entered as the fourth step. Following standard recommendations (Aiken & West, 1991), the continuous variables of mindfulness and state hunger were centered before being entered as main effects into the models and prior to computing interaction terms. Based on a sample size of 107 and the analytic strategy, post-hoc power analyses revealed adequate ability to detect medium (1-β =.93) to large (1-β > .99) effects, but not small effects (Faul, Erdfelder, Lang, & Buchner, 2007).
3. Results
3.1 Participant characteristics and preliminary analyses
One-hundred seven adolescent girls (M ± SD, age 14.53 ± 1.63 years) were studied. Characteristics of adolescents with and without reported LOC-eating are presented in Table 1. Statistical comparisons of these variables by LOC-eating status revealed several unadjusted between-group differences. Adolescents with reported LOC-eating were more likely to have obesity, versus overweight, than adolescents without LOC-eating (p < .05). Adolescents who reported LOC-eating, on average, also had significantly higher BMI percentile (p < .01) and tended to consume more energy during the EAH paradigm (p = .05) as compared to adolescents without LOC-eating. In unadjusted analyses, adolescents with reported LOC-eating had a non-significant tendency towards poorer mindfulness than those without reported LOC-eating (p=.07).
Table 1.
Demographic, anthropometric, psychological, and eating characteristics for adolescent girls with and without loss-of-control-eating (LOC-eating)
| Characteristica | No LOC-Eating | LOC-Eating | p | t |
|---|---|---|---|---|
| n | 65 | 42 | ||
| Age (years) | 14.51 ± 1.69, 12–17 | 14.57 ± 1.55, 12–17 | .84 | .20 |
| BMIb (kg/m2) | 32.13 ± 7.35, 23–51 | 33.79 ± 5.04, 26–46 | .17 | 1.30 |
| BMI (percentile) | 94.77 ± 4.08, 85–99 | 96.86 ± 2.68, 87–99 | .002 | 3.13 |
| Body fat (%) | 42.19 ± 6.12, 31–57 | 43.47 ± 4.93, 32.4–51 | .26 | 1.16 |
| Depressive symptoms | 24.92 ± 7.17, 16–46 | 25.20 ± 7.23, 17–46.5 | .85 | .43 |
| Trait mindfulness | 59.91 ± 12.31, 32–85 | 55.36 ± 12.63, 28–84 | .07 | −1.82 |
| Pre-meal state hunger | 68.20 ± 24.34, 16–100 | 65.48 ± 27.96, 9–100 | .60 | −.64 |
| Post-meal/pre-snack state hunger | .67 ± 1.04, 0–2.5 | .60 ± .97, 0–2.5 | .71 | −.10 |
| Meal intake (kcal) | 1466.41 ± 531.71, 688–3032 | 1634.78 ± 630.28, 447–3032 | .14 | 1.47 |
| EAHc (kcal) | 357.96 ± 158.39, 100–809 | 419.37 ± 149.08, 122–678 | .05 | 2.08 |
|
|
||||
| p | χ2 | |||
|
|
||||
| Non-Hispanic Black (%) | 61.2% | 62.2% | .91 | .01 |
| Obesity (% with BMI ≥95% percentile) | 64.2% | 82.2% | .04 | 4.29 |
Values are Mean ± SD, range, unless otherwise noted as percentage.
BMI=body mass index
EAH=eating in the absence of hunger.
Prior to the laboratory test meal, adolescents endorsed moderate-to-high levels of hunger (67.1 ± 25.7, possible range 0–100), supporting the notion that meal energy intake represented eating when hungry. Conversely, after the meal and prior to the snack period, adolescents reported very low levels of state hunger (0.6 ± 1.0), validating the paradigm that snack intake represented EAH.
3.2 Predictors of meal intake when hungry
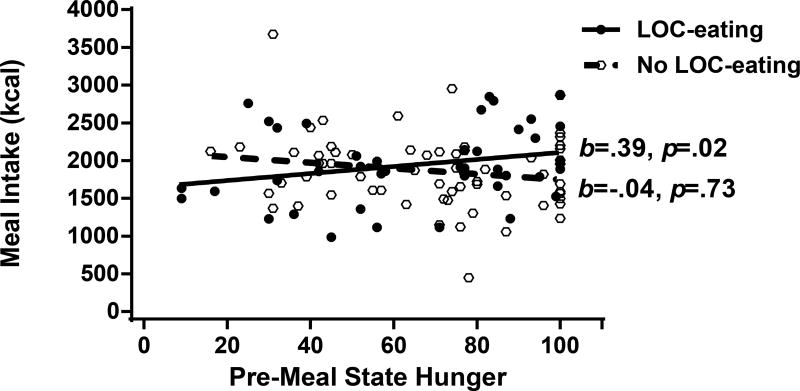
A summary of results from the hierarchical regression modeling examining predictors of meal energy intake when participants were hungry is presented in Table 2. In level 1, covariates accounted for a combined 22.7% of the variance in meal intake. The main effect of pre-meal state hunger entered at level 2 was non-significant (p = .10), and the main effects of mindfulness and LOC-eating entered at level 3 also were non-significant (all ps > .05). At level 4, the addition of the interaction terms among mindfulness, LOC, and hunger explained an additional, non-significant combined 4.7% of the variance in meal intake (p = .10). If the non-significant interaction terms of mindfulness by reported LOC-eating (p = .72) and mindfulness by hunger (p =.64) were not included in the model, the reported LOC-eating by state hunger interaction added a significant, additional 4.4% of explained variance in meal intake (p = .02). There was a significant two-way interaction between adolescents’ reported LOC-eating status and pre-meal state hunger on meal energy intake (p = .02); however, a cautious interpretation of these results is necessary based on the non-significant variance explained when all possible interaction terms were included. As depicted in Figure 1, there was a significant positive relationship between pre-meal state hunger and meal intake only in adolescents with reported LOC-eating (b = .39, p = .02), whereas there was no relationship between state hunger and meal intake in adolescents without LOC (b = −.02, p = .73). Among adolescents with reported LOC-eating, every 1-unit increase on a visual analog scale for pre-meal hunger (range: 0 – 100) was associated with eating 10 more kcal; said differently, every 10-unit increase in hunger (e.g. moving from a little hungry to slightly hungry) was related to consuming 100 kcal more.
Table 2.
Multiple hierarchical regressions predicting adolescent girls’ total energy meal intake when hungry (kcal)
| Level | Variable entered | βa | SE | bb | R2c | ΔR2 |
|---|---|---|---|---|---|---|
| Level 1 | Race (Black) | 85.38 | 107.09 | .07 | .227*** | .227*** |
| Age (years) | −44.17 | 32.63 | −1.30 | |||
| Body fat (%) | −.69 | 9.69 | −.01 | |||
| Lean body mass (kg) | 38.71*** | 8.81 | .55*** | |||
| Height (cm) | −21.05* | 9.66 | −.24* | |||
| Depressive symptoms | 4.67 | 7.59 | .06 | |||
| Level 2 | Pre-meal state hunger | 3.36 | 2.02 | .15 | .248 | .021 |
| Level 3 | Mindfulness | −4.35 | 4.73 | −.10 | .262 | .014 |
| LOC-eatingd (presence) | 86.27 | 106.22 | .07 | |||
| Level 4 | Mindfulness × pre-meal state hunger | −.08 | .16 | −.04 | .309 | .047 |
| LOC-eating × pre-meal state hunger | 9.97* | 4.18 | .30* | |||
| Mindfulness × LOC-eating | 3.03 | 8.35 | .04 |
β = unstandardized regression coefficient at each step.
b = standardized regression coefficient at each step.
R2= proportion of variability in the dependent variable accounted for by model.
LOC-eating = loss-of-control-eating
p < .001.
p < .05
Figure 1.
Reported loss-of-control-eating (LOC-eating) status moderated the relationship between pre-meal state hunger and meal energy intake (kcal; β = .30, p = .02), accounting for age, race/ethnicity, body composition (percent body fat, lean mass, and height), and depressive symptoms; only among adolescent girls with reported LOC-eating, state hunger was positively related to meal intake (β = .39, p = .02), but not among girls without LOC (p = .73).
3.3 Predictors of eating in the absence of hunger (EAH)
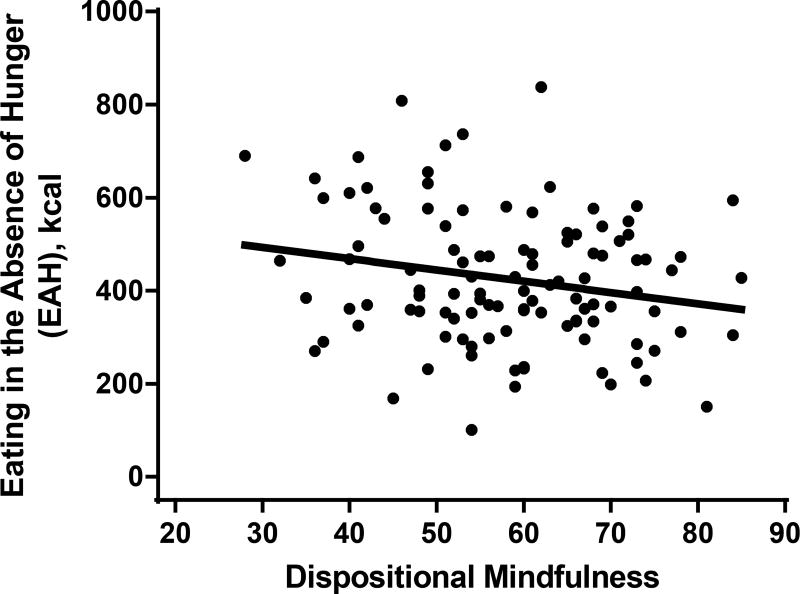
Results from the hierarchical regression modeling examining mindfulness as a predictor of EAH are summarized in Table 3. In level 1, covariates accounted for a combined 15.8% of the variance in snack energy intake (p = .01). Entered at level 2, the main effect of post-meal/pre-EAH state hunger was not significant (p = .59). The main effect of mindfulness entered at level 3 was a significant predictor of EAH (p = .03) and explained an additional 5.4% of the variance in EAH. As depicted in Figure 2, there was a significant inverse relationship between trait mindfulness and snack energy intake (b = −.24, p = .03), such that the more dispositionally mindful an adolescent was, the less snacks she ate in the absence of hunger. Adolescents ate 2.9 kcal less for every 1-unit increase on the MAAS scale (range 15 – 90); for every 10-unit increase in mindfulness, adolescents consumed approximately 30 fewer kcal. There were no significant interactions among mindfulness, LOC, and hunger as entered in level 4 (ps > .05). We also evaluated the three-way interaction of mindfulness, LOC, and state hunger, which was not significant for the prediction of either EAH or meal intake, and thus, was not reported in the presented analyses.
Table 3.
Multiple hierarchical regression predicting adolescent girls’ eating in the absence of hunger (EAH; kcal)
| Level | Variable entered | βa | SE | bb | R2c | ΔR2 |
|---|---|---|---|---|---|---|
| Level 1 | Meal intake when hungry (kcal) | .06 | .03 | .20 | .158* | .158* |
| Race (Non-Hispanic Black) | −30.92 | 30.73 | −.10 | |||
| Age (years) | −1.08 | 9.42 | −.01 | |||
| Body fat (%) | 5.04 | 2.77 | .18 | |||
| Lean body mass (kg) | .95 | 2.75 | .05 | |||
| Height (cm) | 4.38 | 2.83 | .19 | |||
| Depressive symptoms | .56 | 2.18 | .03 | |||
| Level 2 | Post-meal state hunger | −.65 | 1.17 | −.05 | .161 | .003 |
| Level 3 | Mindfulness | −2.94* | 1.37 | −.24* | .215* | .054* |
| LOC-eatingd (presence) | 28.46 | 30.33 | .09 | |||
| Level 4 | Mindfulness × post-meal state hunger | .15 | .18 | .24 | .262 | .047 |
| LOC-eating × post-meal state hunger | −12.54 | 7.66 | −.18 | |||
| Mindfulness × LOC-eating | 4.50 | 2.40 | .23 |
β = unstandardized regression coefficient at each step.
b = standardized regression coefficient at each step.
R2= proportion of variability in the dependent variable (EAH) accounted for by model.
LOC-eating = loss-of-control-eating
p < .05
Figure 2.
Dispositional mindfulness was inversely associated with eating in the absence of hunger (EAH; kcal; β = −.24, p = .03), after accounting for age, race/ethnicity, body composition (percent body fat, lean mass, and height), depressive symptoms, and buffet meal energy intake.
4. Discussion
Mindfulness-based interventions have shown promising preliminary results as a therapeutic modality for disinhibited eating in adults with overweight and obesity and those with T2D (Katterman, Kleinman, Hood, Nackers, & Corsica, 2014; Rogers, Ferrari, Mosely, Lang, & Brennan, 2017; Ruffault et al., 2017). Yet, despite the potential relevance for T2D prevention efforts, there is a paucity of descriptive work to explain how dispositional mindfulness relates to eating behavior, and even less research to understand the possible connection between mindfulness and disinhibited eating in adolescents. The primary objective of the current study was to evaluate, in adolescents at risk for T2D, the relationship of reported dispositional mindfulness with disinhibited eating, assessed with a standardized laboratory test meals paradigm.
In concordance with our hypothesis, there was an inverse association between mindfulness and EAH. Adolescents who endorsed higher levels of dispositional mindfulness consumed less energy in the absence of hunger. This effect remained significant after accounting for body composition, depressive symptoms, prior meal intake, hunger state, and reported LOC-eating, meaning that the relationship of mindfulness to EAH was independent of these potentially confounding factors. This finding is consistent with previous correlational studies supporting an inverse association between mindfulness and self-reported disinhibited eating in college-aged students and adults (Jordan, Wang, Donatoni, & Meier, 2014; Murphy, Mermelstein, Edwards, & Gidycz, 2012; Tak et al., 2015). Also in college students, an experimental mindfulness induction led to greater enjoyment of eating, while concurrently decreasing the total amount of calories consumed from unhealthy foods in the laboratory (Arch et al., 2016), suggesting that enjoyment of eating is a possible mechanism behind mindfulness-based work with eating. Of note, mindfulness was related to EAH, but not to eating when hungry, suggesting a particular application of mindlessness for self-regulation over eating in response to external cues in adolescents at risk for T2D. As mindfulness encompasses moment-by-moment awareness of the emotional experience without judgment and with acceptance (Kabat-Zinn, 1991), one possible explanation is that adolescents who are more dispositionally mindful may have the natural propensity to accept what they are experiencing in the moment without feeling pressured to take an action or “fix” an unpleasant feeling through coping mechanisms such as EAH or disinhibited eating (Caldwell, Baime, & Wolever, 2012). Another characteristic of mindfulness is attunement to internal and external environment; more mindful adolescents may also be more aware of and responsive to their physiological hunger and fullness signals. Mindfulness may have allowed adolescents to acknowledge the presence of highly palatable foods without acting on a desire to eat (Caldwell et al., 2012). In future work, the specific attentional mechanisms through which mindfulness may impact eating behavior merit investigation.
Given previous research supporting LOC-eating as an individual vulnerability factor in exacerbating the effects of emotional eating on excess weight gain in adolescents (Stojek et al., 2017), we explored the interaction of reported LOC-eating with mindfulness in the prediction of eating behavior. Contrary to our hypothesis, LOC-eating and mindfulness did not show a significant interaction in the prediction of meal intake when hungry or EAH. Instead, there was an interaction of LOC-eating and state hunger in the prediction of meal intake such that state hunger was related to eating significantly more at the buffet meal only when adolescents reported LOC-eating. One potential explanation is that hunger sensations are a precipitant to overeating in adolescents who are prone to feeling a lack of control over eating. Indeed, previous data demonstrate that disinhibition or losing control over eating may be triggered by hunger sensations (Tanofsky-Kraff, Goossens, et al., 2007), that youth with LOC-eating patterns experience hunger earlier after eating than youth without LOC (Hilbert, Tuschen-Caffier, & Czaja, 2010; Mirch et al., 2006), and that managing hunger levels may attenuate the incidence of overeating and LOC episodes in adults with binge eating disorder (Masheb & Grilo, 2006; Masheb, Grilo, & White, 2011). Given these findings, it follows that higher levels of hunger may trigger LOC-eating. However, the cross-sectional nature of our data inhibits the ability to determine directionality; it is also possible that LOC may trigger feeling greater hunger. Further exploration of how hunger relates to disinhibited eating episodes is needed. Although these findings were exploratory and require replication, they have potential applied and clinical significance; interventions that include a combination of teaching attention to hunger signals, how to restructure eating to avoid extreme levels of both hunger and fullness, and mindfulness training might be valuable to youth with LOC-eating.
4.1 Considerations and future directions
The current descriptive data supplement a small but growing body of literature supporting the possible utility of mindfulness-based interventions for weight management and metabolic outcomes in adults (Godfrey et al., 2015; Godsey, 2013; Raja-Khan et al., 2017). Preliminary data also support the potential utility of mindfulness-based training for psychological health and lessening T2D risk in adolescents at risk for T2D (Shomaker, Bruggink, et al., 2017). Although the current study may contribute to understanding the relationship of mindfulness and disinhibited eating in adolescents, the data were cross-sectional, resulting in an inability to determine a cause and effect relationship. It could be that increased dispositional mindfulness leads to fewer instances of disinhibited eating, but it is also possible that engaging in fewer episodes of disinhibited eating leads an adolescent to report higher levels of mindfulness. Future research utilizing an experimental induction of state mindfulness in adolescents would allow for stronger conclusions about directionality. Longitudinal studies are also necessary to evaluate mindfulness as a prospective risk factor for changes in disinhibited eating. The MAAS is a unifactor measure that may not capture the multi-faceted nature of mindfulness. New measures examining the many aspects of mindfulness, particularly in youth, will aid in the ability to explore the role of mindfulness in disinhibited eating behavior (Johnson, Burke, Brinkman, & Wade, 2017). Further, we acknowledge the exploratory nature of the interactions among mindfulness, LOC-eating, and state hunger on eating behavior. Although the findings were consistent with prior data on the role of hunger and LOC-eating (Hilbert et al., 2010; Mirch et al., 2006; Tanofsky-Kraff, Goossens, et al., 2007), the extent to which we can interpret these findings depends upon replication in additional studies. Also, to what degree the findings from the current study may be generalizable to populations outside of adolescent girls at risk for T2D with depressive symptoms is unknown, given the specific characteristics of the sample in addition to the possibility that laboratory eating paradigms may not replicate day-to-day eating. Future ecological momentary assessment studies of mindfulness and eating behavior would add to our knowledge base.
Despite these limitations, the current study has important strengths. To our knowledge, there has been limited investigation on the relationship between mindfulness and laboratory EAH in adolescents. Strengths of the current study include objective measurements of body composition using DXA, in addition to the objective measurement of eating behavior in the laboratory as opposed to relying on self-report measures of energy intake, which generally show very poor concurrent or predictive validity (Goran, 1998). We accounted for several important, potentially confounding factors in our analyses, including body composition and depression symptoms, indicating that the reported relationships existed above and beyond these covariates. Moreover, the sample was racially/ethnically diverse and represented a population at high risk for excess weight gain and T2D. Given the exponential rise of T2D in adolescents (Dabelea et al., 2014), our study contributes to the literature on mindfulness and associated eating behavior.
In summary, using laboratory test meals, we found evidence for a link between dispositional mindfulness and EAH in adolescents at risk for developing T2D; however, dispositional mindfulness was not associated with eating when hungry. Instead, exploratory analysis revealed a significant interaction between reported LOC-eating and state hunger on meal intake such that teens prone to uncontrolled eating ate the most in a state of high hunger. These findings suggest that future experiments should test if interventions to increase mindfulness are useful in decreasing disinhibited eating in adolescents at risk for T2D. Mindfulness-based training to foster interoceptive awareness and recognition of hunger cues may be important for helping at risk youth to develop long-term healthy eating behavior.
Acknowledgments
Funding: This study was supported by K99/R00HD069516 (to LBS) and 1ZIAHD000641 (to JAY) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development with supplemental support from the National Institutes of Health Bench to Bedside Program, the Office of Behavioral and Social Sciences Research, and the National Institutes of Health Office of Disease Prevention.
Footnotes
ClinicalTrials.gov identifier: NCT01425905
Conflict of interest: All authors report no conflicts of interest. J. A. Yanovski is a commissioned officer in the U.S. Public Health Service. The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the Public Health Service, the Department of Health and Human Services, the Uniformed Services University of the Health Sciences, or the U.S. Department of Defense.
References
- Ackard DM, Neumark-Sztainer D, Story M, Perry C. Overeating among adolescents: Prevalence and associations with weight-related characteristics and psychological health. Pediatrics. 2003;111:67–74. doi: 10.1542/peds.111.1.67. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association, Inc.; 2013. [Google Scholar]
- Arch JJ, Brown KW, Goodman RJ, Della Porta MD, Kiken LG, Tillman S. Enjoying food without caloric cost: The impact of brief mindfulness on laboratory eating outcomes. Behaviour Research and Therapy. 2016;79:23–34. doi: 10.1016/j.brat.2016.02.002. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18:211–237. doi: 10.1080/10478400701598298. [DOI] [Google Scholar]
- Caldwell KL, Baime MJ, Wolever RQ. Mindfulness based approaches to obesity and weight loss maintenance. Journal of Mental Health Counseling. 2012;34:269–282. doi: 10.17744/mehc.34.3.t016616717774643. [DOI] [Google Scholar]
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Costanzo PR, Woody EZ. Externality as a function of obesity in children: Pervasive style or eating-specific attribute? Journal of Personality and Social Psychology. 1979;37:2286–2296. doi: 10.1037/0022-3514.37.12.2286. [DOI] [PubMed] [Google Scholar]
- Creswell JD. Mindfulness interventions. Annual Review of Psychology. 2017;68:491–516. doi: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, Hamman RF. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. Journal of the American Medical Association. 2014;311:1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, Horton NJ. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130:e289–e295. doi: 10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Cai G, Jaramillo SJ, Cole SA, Comuzzie AG, Butte NF. Heritability of hyperphagic eating behavior and appetite-related hormones among Hispanic children. Obesity. 2007;15:1484–1495. doi: 10.1038/oby.2007.177. [DOI] [PubMed] [Google Scholar]
- Godfrey KM, Gallo LC, Afari N. Mindfulness-based interventions for binge eating: A systematic review and meta-analysis. Journal of Behavioral Medicine. 2015;38:348–362. doi: 10.1007/s10865-014-9610-5. [DOI] [PubMed] [Google Scholar]
- Godsey J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: An integrative review. Complementary Therapies in Medicine. 2013;21:430–439. doi: 10.1016/j.ctim.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Goran MI. Measurement issues related to studies of childhood obesity: assessment of body composition, body fat distribution, physical activity, and food intake. Pediatrics. 1998;101:505–518. [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B, Czaja J. Familial interactions and mealtime behavior of children with binge eating: A laboratory test meal study. American Journal of Clinical Nutrition. 2010;91:510–518. doi: 10.3945/ajcn.2009.28843. [DOI] [PubMed] [Google Scholar]
- Johnson C, Burke C, Brinkman S, Wade T. Development and validation of a multifactor mindfulness scale in youth: The Comprehensive Inventory of Mindfulness Experiences–Adolescents (CHIME-A) Psychological Assessment. 2017;29:264–281. doi: 10.1037/pas0000342. [DOI] [PubMed] [Google Scholar]
- Jordan CH, Wang W, Donatoni L, Meier BP. Mindful eating: Trait and state mindfulness predict healthier eating behavior. Personality and Individual Differences. 2014;68:107–111. doi: 10.1016/j.paid.2014.04.013. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Dell Publishing; 1991. [Google Scholar]
- Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eating Behaviors. 2014;15:197–204. doi: 10.1016/j.eatbeh.2014.01.005. [DOI] [PubMed] [Google Scholar]
- Kelly NR, Shomaker LB, Pickworth CK, Grygorenko MV, Radin RM, Vannucci A, Yanovski JA. Depressed affect and dietary restraint in adolescent boys' and girls' eating in the absence of hunger. Appetite. 2015;91:343–350. doi: 10.1016/j.appet.2015.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly NR, Tanofsky-Kraff M, Vannucci A, Ranzenhofer LM, Altschul AM, Schvey NA, Yanovski JA. Emotion dysregulation and loss-of-control eating in children and adolescents. Health Psychology. 2016;35:1110–1119. doi: 10.1037/hea0000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TV, Faith MS. Child eating patterns and weight regulation: a developmental behaviour genetics framework. Acta Paediatr. 2007;96:29–34. doi: 10.1111/j.1651-2227.2007.00167.x. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Johnson CL. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- Lanctot JQ, Klesges RC, Stockton MB, Klesges LM. Prevalence and characteristics of energy underreporting in African-American girls. Obesity (Silver Spring) 2008;16:1407–1412. doi: 10.1038/oby.2008.222. [DOI] [PubMed] [Google Scholar]
- Lattimore P, Fisher N, Malinowski P. A cross-sectional investigation of trait disinhibition and its association with mindfulness and impulsivity. Appetite. 2011;56:241–248. doi: 10.1016/j.appet.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Jardin BF, Anderson DA. Bulimic symptoms in undergraduate men and women: Contributions of mindfulness and thought suppression. Eating Behaviors. 2009;10:228–231. doi: 10.1016/j.eatbeh.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. International Journal of Eating Disorders. 2006;39:141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM, White MA. An examination of eating patterns in community women with bulimia nervosa and binge eating disorder. International Journal of Eating Disorders. 2011;44:618–624. doi: 10.1002/eat.20853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuda A, Price M, Latzman RD. Mindfulness moderates the relationship between disordered eating cognitions and disordered eating behaviors in a non-clinical college sample. Journal of Psychopathology and Behavioral Assessment. 2012;34:107–115. doi: 10.1007/s10862-011-9252-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirch MC, McDuffie JR, Yanovski SZ, Schollnberger M, Tanofsky-Kraff M, Theim KR, Yanovski JA. Effects of binge eating on satiation, satiety, and energy intake of overweight children. American Journal of Clinical Nutrition. 2006;84:732–738. doi: 10.1097/WAD.0b013e3181aba588.MRI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooreville M, Shomaker LB, Reina SA, Hannallah LM, Adelyn Cohen L, Courville AB, Yanovski JA. Depressive symptoms and observed eating in youth. Appetite. 2014;75:141–149. doi: 10.1016/j.appet.2013.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MJ, Mermelstein LC, Edwards KM, Gidycz CA. The benefits of dispositional mindfulness in physical health: A longitudinal study of female college students. Journal of American College Health. 2012;60:341–348. doi: 10.1080/07448481.2011.629260. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association. 2011;111:1004–1011. doi: 10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson KL, Emery CF. Mindfulness and weight loss. Psychosomatic Medicine. 2015;77:59–67. doi: 10.1097/PSY.0000000000000127. [DOI] [PubMed] [Google Scholar]
- Pallozzi R, Wertheim E, Paxton S, Ong B. Trait mindfulness measures for use with adolescents: A systematic review. Mindfulness. 2017;8:110–125. doi: 10.1007/s12671-016-0567-z. [DOI] [Google Scholar]
- Pidgeon A, Lacota K, Champion J. The moderating effects of mindfulness on psychological distress and emotional eating behaviour. Australian Psychologist. 2013;48:262–269. doi: 10.1111/j.1742-9544.2012.00091.x. [DOI] [Google Scholar]
- Pivarunas B, Kelly NR, Pickworth CK, Cassidy O, Radin RM, Shank LM, Shomaker LB. Mindfulness and eating behavior in adolescent girls at risk for type 2 diabetes. International Journal of Eating Disorders. 2015;48:563–569. doi: 10.1002/eat.22435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Raja-Khan N, Agito K, Shah J, Stetter CM, Gustafson TS, Socolow H, Legro RS. Mindfulness-based stress reduction in women with overweight or obesity: A randomized clinical trial. Obesity (Silver Spring) 2017;25:1349–1359. doi: 10.1002/oby.21910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the Eating Disorder Examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108X(200011)28:3<311::AID-EAT8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Rogers JM, Ferrari M, Mosely K, Lang CP, Brennan L. Mindfulness-based interventions for adults who are overweight or obese: A meta-analysis of physical and psychological health outcomes. Obesity Reviews. 2017;18:51–67. doi: 10.1111/obr.12461. [DOI] [PubMed] [Google Scholar]
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Flahault C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obesity Research and Clinical Practice. 2017;11:90–111. doi: 10.1016/j.orcp.2016.09.002. [DOI] [PubMed] [Google Scholar]
- Schachter S. Some extraordinary facts about obese humans and rats. American Psychologist. 1971;26:129–144. doi: 10.1037/h0030817. [DOI] [PubMed] [Google Scholar]
- Schachter S, Rodin J. Obese humans and rats. Washington, D.C: Erlbaum/Halsted; 1974. [Google Scholar]
- Shank LM, Tanofsky-Kraff M, Nelson EE, Shomaker LB, Ranzenhofer LM, Hannallah LM, Yanovski JA. Attentional bias to food cues in youth with loss of control eating. Appetite. 2015;87:68–75. doi: 10.1016/j.appet.2014.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Shomaker LB, Bruggink S, Pivarunas B, Skoranski A, Foss J, Chaffin E, Bell C. Pilot randomized controlled trial of a mindfulness-based group intervention in adolescent girls at risk for type 2 diabetes with depressive symptoms. Complementary Therapies in Medicine. 2017;32:66–74. doi: 10.1016/j.ctim.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Kelly NR, Pickworth CK, Cassidy OL, Radin RM, Shank LM, Yanovski JA. A randomized controlled trial to prevent depression and ameliorate insulin resistance in adolescent girls at risk for type 2 diabetes. Annals of Behavioral Medicine. 2016;50:762–774. doi: 10.1007/s12160-016-9801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Kelly NR, Radin RM, Cassidy OL, Shank LM, Brady SM, Yanovski JA. Prevention of insulin resistance in adolescents at risk for type 2 diabetes with depressive symptoms: 1-year follow-up of a randomized trial. Depression and Anxiety. 2017;34:866–876. doi: 10.1002/da.22617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Stern EA, Miller R, Zocca JM, Field SE, Yanovski JA. Longitudinal study of depressive symptoms and progression of insulin resistance in youth at risk for adult obesity. Diabetes Care. 2011;34:2458–2463. doi: 10.2337/dc11-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Yanovski JA. Disinhibited eating and body weight in youth. In: Preedy VR, Watson RR, Martin CR, editors. Handbook of behavior, food and nutrition. New York, NY: Springer; 2011. pp. 2183–2200. [Google Scholar]
- Shomaker LB, Tanofsky-Kraff M, Zocca JM, Courville A, Kozlosky M, Columbo KM, Yanovski JA. Eating in the absence of hunger in adolescents: Intake after a large-array meal compared with that after a standardized meal. American Journal of Clinical Nutrition. 2010;92:697–703. doi: 10.3945/ajcn.2010.29812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, Field AE. Longitudinal associations between binge eating and overeating and adverse outcomes: Does LOC matter? 2013;167:149–155. doi: 10.1001/2013.jamapediatrics.12.Longitudinal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychological Bulletin. 2006;132:667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojek MMK, Tanofsky-Kraff M, Shomaker LB, Kelly NR, Thompson KA, Mehari RD, Yanovski JA. Associations of adolescent emotional and loss of control eating with 1-year changes in disordered eating, weight, and adiposity. International Journal of Eating Disorders. 2017;50:551–560. doi: 10.1002/eat.22636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tak SR, Hendrieckx C, Nefs G, Nyklíček I, Speight J, Pouwer F. The association between types of eating behaviour and dispositional mindfulness in adults with diabetes. Results from Diabetes MILES. The Netherlands. Appetite. 2015;87:288–295. doi: 10.1016/j.appet.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M. Binge eating among children and adolescents. In: Jelalian E, Steele RG, editors. Handbook of childhood and adolescent obesity. New York, NY: Springer Science + Business Media; 2008. pp. 43–59. [Google Scholar]
- Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, Yanovski JA. A multisite investigation of binge eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology. 2007;75:901–913. doi: 10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Haynos AF, Kotler LA, Yanovski SZ, Yanovski JA. Laboratory-based studies of eating among children and adolescents. Current Nutrition and Food Science. 2007;3:55–74. doi: 10.2174/1573401310703010055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, DellaValle D, Yanovski JA. Children's binge eating and development of metabolic syndrome. International Journal of Obesity. 2012;36:956–962. doi: 10.1038/ijo.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders. 2009;42:26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of Consulting and Clinical Psychology. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW. Exploratory data analysis. Reading, MA: Addison-Wesley Publishing Company; 1977. [Google Scholar]
- Vannucci A, Tanofsky-Kraff M, Crosby RD, Ranzenhofer LM, Shomaker LB, Field SE, Yanovski JA. Latent profile analysis to determine the typology of disinhibited eating behaviors in children and adolescents. Journal of Consulting and Clinical Psychology. 2013;81:494–507. doi: 10.1037/a0031209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waling MU, Larsson CL. Energy intake of Swedish overweight and obese children is underestimated using a diet history interview. Journal of Nutrition. 2009;139:522–527. doi: 10.3945/jn.108.101311. [DOI] [PubMed] [Google Scholar]
- Wilfley D, Berkowitz R, Goebel-Fabbri A, Hirst K, Ievers-Landis C, Lipman TH, Van Buren D. Binge eating, mood, and quality of life in youth with type 2 diabetes: Baseline data from the TODAY study. Diabetes Care. 2011;34:858–860. doi: 10.2337/dc10-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]