Abstract
Objective
Little is known about positive emotion communication (PEC) in end-of-life care. This study aims to identify types and patterns of PEC among hospice nurses, caregivers, and patients.
Methods
A coding system based on positive psychology theory was applied as a secondary analysis to audio recordings of hospice nurse home visits with cancer patients and family caregivers, collected as part of a prospective longitudinal study. Eighty recordings (4 visits from 20 triads) were coded for humor, connection, praise, positive focus, gratitude, taking joy/savoring, and perfunctory statements.
Results
Descriptive statistics revealed the greatest proportion of PEC was made by nurses. Humor was most frequently used across all speakers. Cluster analysis revealed four PEC visit types: Savor/Take Joy; Humor; Perfunctory; and Other-focused Expressions of Positive Emotions. Linear mixed effect regression was used to estimate the trajectory of PEC over time, but no significant change was found.
Conclusion
We found that positive emotions are common in nurse, caregiver and patient communication at end-of-life and do not decline closer to death.
Practice Implication
This study is among the first to explore PEC at end-of-life, and offers a way to bring strengths-based approaches into end of life communication research.
Keywords: Caregiver, cancer, expressed emotion, hospice care, communication
1. Introduction
As the proportion of the aging population grows so does the need for end-of-life care [1]. Hospice services provide holistic care to patients with life-limiting illness and their family members. In the U.S., about 1.7 million patients receive hospice services, the majority within their home or place of residence [2]. Hospice is made available to patients of any age with a life-limiting diagnosis and a life expectancy of less than 6 months. Care, in the U.S., is made available through Medicare or other health insurance providers. Typically, a family member serves as the primary caregiver with members of the hospice team (e.g., social worker, chaplain, nurse) making regular visits to provide care and other services. The unit of care is considered to be patient and family. Over a third of U.S. hospice patients have advanced cancer which is associated with a rapid, yet highly variable, decline [3]. This places unique stress on the hospice care team and indicates a need for attention to home hospice communication. Family caregivers are a vital member of the hospice care team, and as the patients’ health declines the caregiver role expands, often placing them at significant negative psychological, physical, social, and financial risk [4–8]. The increased engagement by caregivers in hospice care is in contrast to earlier in the cancer care trajectory where the caregiver’s voice is largely absent and much of the communication is between the patient and clinician [9–11]. It is important for hospice care team members to use communication strategies that strengthen relationships and positively engage all family members.
Little is known about positive emotions at end-of-life care. Positive and negative emotions are independent constructs (e.g., [12]) and can be experienced at the same time. Because positive and negative emotions have different implications for health and well-being, it is important to learn about risks associated with negative emotion as well as potential benefits of positive emotion for patients and caregivers. Cancer patient positive emotion has been associated with lower symptom reports, less functional impairment, and fewer cancer-related medical appointments [13–15]. Research available on caregiver positive emotion suggests that caregiving “uplifts” are associated with well-being [16], and experiencing positive emotion is associated with greater post-traumatic growth [17, 18].
Positive emotions are associated with better health and longevity, thus serving a protective function [19, 20]. Similarly, positive emotions are associated with enhanced coping, meaning-making, and building resilience to stressful events [21–23]. Meaning-making or benefit-finding might be particularly relevant to cancer patients and caregivers, as it is associated with more positive emotion, less distress, and better mental health [24]. The Broaden-and-Build Theory [25] may explain some of these associations as it posits that positive emotions broaden an individual’s thought-action repertoire and build physical, intellectual, and social resources, thereby promoting resilience. In contrast to negative emotions, which carry direct and immediate adaptive benefits by prompting a specific threat response (e.g., fear prompts fleeing), positive emotions carry more indirect and long-term adaptive benefits because broadening builds enduring resources to manage future threats. In the short term, positive emotions counteract negative emotion and enhance stress recovery [26]. When shared, positive emotions create mutual enjoyment and social bonds.
1.1 Positive Emotion Communication
Effective communication is a key component of healthcare interactions and serves many functions, including information exchange and relationship-building [27]. Beyond the required information exchange in nurse-patient-caregiver interactions, high quality relationships that encompass trust and support are important and contribute to better care and improved health and well-being [28]. One way to build high quality relationships is through positive emotion. Due to the intimate and intensive nature of home hospice care, nurses, patients, and families can quickly develop relationships built on trust and support that assist caregivers and patients to navigate end-of-life care.
Positive emotion can be a shared experience, and is frequently communicated verbally. This is also the case in nurse-patient-caregiver communication. Alpert and Womble [29] examined how caregivers used communication as a coping strategy when caring for a family member in an analysis of over 150 caregiver stories, and found that stories using emotion-based techniques—such as humor and positive framing—fostered meaningful bonds between caregivers and family members, and may help with coping. Humor, in particular, has received the most attention as a coping strategy, as it represents a safe way to share challenging, frustrating, and/or upsetting experiences [30]. Using positive emotion words has been associated with better overall health [31]. These effects have been replicated in written and verbal expressive disclosure paradigms in chronically stressed caregivers of older adults [32]. There is relatively little research on positive emotion expression in patients at end-of-life; however, a study comparing blog posts of terminally ill cancer patients to posts from healthy participants who imagined they were terminally ill found that the patients used similar amounts of positive words and far more positive than negative emotion words overall than those who imagined being terminally ill [33].
There is limited research on positive emotion communication (PEC) between patients, nurses, and caregivers at end-of-life. The nature of the emotional experience in hospice care is tremendously complex, and includes positive and negative emotions across the continuum from admission, to caregiving, and bereavement. Hospice nurses have been shown to use PEC to elicit caregiver and patient concerns [34]. Patients have been shown to use humor and positive emotion when discussing sensitive topics such as end-of-life discussions or embarrassing moments to lighten the mood [18]. Generally speaking, PEC is also associated with less caregiver distress during palliative home care and greater resilience during bereavement (e.g., [35–38]). For example, recently bereaved caregivers who were genuinely smiling and laughing while discussing their recent loss adjusted better over time compared with other bereaved individuals [39, 40].
1.2 Objective
In a large study of palliative nurse-caregiver-patient communication [41], we were surprised to find a significant proportion of PEC at end-of-life [42]. More surprising, during nurse visits, positive emotion occurred more frequently than distress for caregivers, and in equal amounts for patients. In other research, hospice nurses were found to use PEC as a strategy to elicit caregiver and patient concerns that they may otherwise have been reluctant to express [34]. These findings prompted a closer look at the occurrence of PEC during in-home palliative care. The purpose of this study was to conduct a secondary analysis of nurse-caregiver-patient communication to explore PEC in hospice, and to identify types and patterns of PEC at end-of-life.
2. Methods
2.1 Study Design, Participants and Setting
The data for this study were derived from a large prospective observational project described in detail elsewhere [41, 42]. The study was approved by the University’s Institutional Review Board and participating hospice agencies. Study participants included hospice nurses and family caregivers of hospice cancer patients at seven home hospice agencies located in two different geographic locations in the U.S. (intermountain West, urban East coast). All caregiver and hospice nurse participants completed demographic surveys at baseline. Hospice nurses who agreed to participate recorded their home visits with consenting family caregivers of cancer hospice patients. Visits from the larger study were coded using the Roter Interactional Analysis System (RIAS) [43], followed by secondary coding for PEC. Because we wanted to examine communication over the course of home hospice visits, we chose cases with at least four recorded home visits. Sampling four time points allowed us to assess for patterns of change and variability in positive emotion across a patient’s end-of-life trajectory by capturing both “good and bad days” as the patient declined. Choosing more time points would have limited our sample size as many patients had limited number of home visits. Twenty cases were randomly selected from a larger group of cases that had one visit recording in each of the four quartiles of time from study consent to death, resulting in a total of 80 recorded home visits. A home visit was randomly selected if there was more than one recorded visit in that quartile.
2.2 Data Collection
Nurses were invited to participate at a staff meeting. Those who agreed completed informed consent and questionnaires. Research staff assessed for eligibility at each hospice to identify family caregivers of cancer patients 45 years or older, were English-speaking, and cognitively able to participate. Family caregivers were contacted by phone and, if interested, a home meeting was scheduled to obtain consent from caregivers and to complete questionnaires. Patients were invited to consent when able, and if not, caregivers served as proxy. Nurses wore digital recorders around their neck during home visits. This allowed nurses to capture the entire visit as they moved throughout the home. Upon entering the home, nurses reminded those present they were recording that day. Finally, research staff abstracted patient data from hospice records.
2.3 Measures
2.3.1 Baseline measures: Nurses
Participating hospice nurses completed demographics and questions on professional characteristics; e.g., years in practice as a hospice nurse and nursing degree. Caregivers: Consenting family caregivers completed demographic questionnaires including nature and length of relationship with patient.
2.3.2 Case characteristics
From hospice records, research staff extracted patient age, gender, and cancer type. They also documented the number of nurse home visits and length of home hospice care (enrollment to patient death) for each case.
2.3.3 Coding PEC
As part of the larger study, digitally recorded home hospice visits were analyzed using RIAS (Kappa >.0.65), which has demonstrated applicability in the home hospice setting [44, 45]. Details on RIAS coding of the parent study are provided elsewhere [42]. Codes were applied using direct-entry data software (Noldus Observer XT Version 11.5). An advantage of using a coding system like RIAS is marking communication that can be revisited for second level coding to derive a more focused, conceptually driven examination.
The focus of our secondary data analyses was on PEC. First, we combined the following RIAS codes to create a general positive emotion category: laughs/tells jokes, reassurance/optimism, shows approval and compliments. Next, we used concepts associated with Seligman’s positive psychology pillars to conduct a directed content analysis of the RIAS positive affect codes [46]. Through an iterative process of weekly meetings with coders, two investigators (A.T., L.E.) identified seven categories and created theoretically-based operational definitions for PEC within interpersonal exchanges. Six categories were used to further code the combined RIAS codes (see Table 1). The seventh code category was added for communication that was determined to be perfunctory through interpretation of content and tone (e.g., “good,” “nice,” “thanks”). These PEC categories were used to capture content and emotional intensity. The connection code trumped all other codes because it reflected a deep expression of feeling towards the other person. For example, a caregiver might say to the nurse “I’m glad you’re here today” to greet the nurse entering the home to reflect gratitude and appreciation. However, if the family is gathered around the patient who is near death and the caregiver says to the nurse in a heartfelt manner “I’m glad you’re here today” it would be interpreted as connection.
Table 1.
Positive emotion communication category codes
| Positive Emotion Codes | Examples |
|---|---|
| Humor: intension to be amusing or comical; making a joke. This can include: nervous humor (i.e., break tension about behavior); conversation filler; sharing a funny story to fill the void; supportive humor; dark humor (e.g., jokes about dying); using humor to ease tension/emotion in the room; using humor to normalize. | Nurse to caregiver: When I was on the phone it sounded like a goose honk. Caregiver to nurse: Thought I would give it to him (pill) while you are here so if he chokes you will be here. (Said jokingly) |
| Praise or support: complimenting, providing support for, or affirming another person; positive reinforcement; validation | Nurse to caregiver: You are doing a 300% fantastic job! Nurse to patient: You look beautiful always, wearing nice clothes and your family keeps you looking so well all the time. |
| Positive focus: focusing on the positive, being optimistic or having a positive outlook; encouraging others to be positive or be hopeful | Caregiver to nurse: We can be miserable or we can make the best of it, get back on our feet and make the best we can with whatever the day is. Caregiver to nurse: I’m hopeful he (patient) feel better tomorrow. |
| Appreciation or gratitude: counting blessings; appreciation of life circumstances; gratitude towards others; thanking someone | Caregiver to nurse: You are wonderful. Patient to nurse: We appreciate all that you do to help us. |
| Savoring or experiencing joy: taking delight or joy in a moment; replaying life’s pleasures and wonders; open expression of finding beauty; relishing in ordinary experiences, and savoring those experiences with others. Many of these expressions need to be interpreted within the context of a very limited lifespan. | Caregiver to nurse: We (she and her husband (patient)) would drink a coffee every afternoon out on our deck. Patient to nurse: Aren’t these socks awesome? Nurse to patient: They (socks) are like little blankets. Patient to nurse: They keep my feet so warm and cozy. |
| Connection: fostering relationships and connecting with another person; endearment, affection; emotional greetings and goodbyes can fall under this code provided there is a clearly expressed strong emotional connection (intensity); often reciprocated. | Nurse to caregiver: It takes a special person to do what you do. Patient to nurse: Come over here so I can give you a hug. Nurse to patient: You know I love you. |
| Perfunctory: social etiquette; perfunctory, automatic or statements reflecting habitual responses. | Nurse to caregiver: Thanks. (in response to caregiver opening the door and allowing the nurse to walk into the room first) Caregiver: Good. (in response to nurse bringing more pads for the patient’s bed) |
Using Observer software, research assistants trained in coding listened to the interactions surrounding each previously-identified RIAS positive emotion code within a visit to accurately interpret communication within the interpersonal context. Trained coders and investigators (A. T., L. E.) met weekly. Eight randomly selected visits (10%) were used to establish and refine the codebook and were consensus coded by the group. The remaining visits were randomly assigned to coders with eight visits serving as reliability checks (kappa = 0.75).
2.4 Analysis
This is an exploratory prospective longitudinal observational study using various analytic approaches to better understand how and when positive emotion is expressed at end-of-life among patients, caregivers, and hospice nurses. We used descriptive statistics to describe sample characteristics, visit length, and PEC categories. To provide the broader context of home visits for the 20 cases, we examined the PEC code in relation to the other RIAS codes from the parent study by examining mean and median frequency and ratios. We also compared the seven PEC codes to each other using descriptive statistics. Next we conducted cluster analysis using Gaussian finite mixture modeling to assign visits to clusters by common patterns of utterance types. Model based clustering allows for selecting number of clusters and covariance parameterization based on likelihood ratio statistic, Bayesian information criterion (BIC) or ad hoc decision [47]. We used linear mixed effect regression to estimate the trajectory of utterance proportions over time for each PEC category, adjusting for random intercepts at the dyad level.
3. Results
3.1 Participant and Visit Characteristics
There were a total of 20 patients, 20 partner caregivers, and 20 nurses in this sample with recordings of 80 hospice visits (4 visits per case). The average visit was 44.7 minutes in length. Nurses were employed at seven different hospices, and had been working in hospice on average for 5.3 years. See Table 2 for participant characteristics.
Table 2.
Participant Characteristics
| Patient | Caregiver | Nurse | |
|---|---|---|---|
| N=20 | N=20 | N=20 | |
| Age, mean (SD) | 64.95 (9.8) | 63.05 (11.3) | 45.15 (10.1) |
|
| |||
| Sex, % (n) | 70 (14) | 30 (6) | 0 (0) |
| Male | |||
|
| |||
| Marital Status, % (n) | 85 (17) | 85 (17) | -- |
| Married | |||
|
| |||
| Length of hospice stay in days, mean (SD) | 104.45 (71.9) | -- | -- |
|
| |||
| Type of cancer, % (n) | |||
| brain | 5 (1) | -- | -- |
| breast | 10 (2) | -- | -- |
| lung | 10 (2) | -- | -- |
| lymphoma/leukemia | 10 (2) | -- | -- |
| melanoma | 15 (3) | -- | -- |
| other GI/GU | 25 (5) | -- | -- |
| reproductive | 25 (5) | -- | -- |
|
| |||
| Race, % (n) | |||
| White | 90 (18) | 100 (20) | 95 (19) |
|
| |||
| Education, % (n) | |||
| High school | 15 (3) | 15 (3) | |
| Some college | 45 (9) | 45 (9) | |
| 4 year college | 20 (4) | 20 (4) | |
| Graduate school | 20 (4) | 20 (4) | |
| Nursing diploma | -- | -- | 5 (1) |
| Nursing associate | -- | -- | 70 (14) |
| Nursing bachelors | -- | -- | 25 (5) |
|
| |||
| Religion, % (n) | |||
| Catholic | 5 (1) | 15 (3) | 15.8 (3) |
| Jewish | 5 (1) | 0 (0) | 0 (0) |
| Latter-day Saints | 50 (10) | 50 (10) | 36.8 (7) |
| Protestant | 10 (2) | 5 (1) | 5.3 (1) |
| Other | 20 (4) | 15 (3) | 5.3 (1) |
| No religious affiliation | 10 (2) | 10 (2) | 36.8 (7) |
|
| |||
| Income, % (n) | |||
| < 10,000 | 5 (1) | 5 (1) | |
| 10,000 24,999 | 15 (3) | 15 (3) | |
| 25,000 39,999 | 5 (1) | 5 (1) | |
| 40,000 49,999 | 10 (2) | 10 (2) | |
| 50,000 74,999 | 15 (3) | 15 (3) | |
| 75,000 or more | 45 (9) | 45 (9) | |
|
| |||
| Nursing certificate, % (n) | -- | -- | |
| CHPN | 29.4 (5) | ||
3.2 PEC Descriptives
Across all visit utterances, PEC represents a median of 5.87% of the total visit utterances (M = 12.30, SD = 23.16). Table 3 provides mean, standard deviation, median, range of responses, and proportion (%) of statements for each category and speaker. Nurses made the most PEC statements. For nurses, praise (23%), humor (22%) and perfunctory statements (22%) are equally represented and make up the majority of nurse PEC. In contrast, humor represents by far the most predominant type of PEC for caregivers (31%) and patients (34%) relative to each of their total PEC.
Table 3.
Positive Emotion Communication Codes by Speakers per Visit
| PEC Code | Caregiver | Patient | Nurse | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Med | Range | % | Mean (SD) | Med | Range | % | Mean (SD) | Med | Range | % | |
| Connection | 1.18 (2.00) | 0 | 0–11 | 10 | 0.33 (.90) | 0 | 0–5 | 6 | 1.85 (2.64) | 1 | 0–13 | 8 |
| Savor/Take Joy | 1.38 (2.40) | 0 | 0–11 | 12 | 0.71 (1.96) | 0 | 0–14 | 13 | 1.50 (2.32) | 1 | 0–11 | 7 |
| Gratitude | 1.30 (1.61) | 1 | 0–9 | 11 | 0.65 (1.03) | 0 | 0–5 | 12 | 1.91 (1.98) | 1 | 0–10 | 9 |
| Positive focus | 0.56 (1.33) | 0 | 0–8 | 5 | 0.33 (0.85) | 0 | 0–4 | 6 | 1.98 (2.66) | 1 | 0–14 | 9 |
| Praise | 1.24 (1.67) | 1 | 0–9 | 11 | 0.54 (1.07) | 0 | 0–5 | 10 | 5.20 (4.08) | 4.5 | 0–18 | 23 |
| Humor | 3.51 (5.10) | 2 | 0–29 | 31 | 1.85 (3.31) | 0.5 | 0–16 | 34 | 4.90 (4.24) | 4 | 0–18 | 22 |
| Perfunctory | 2.24 (4.06) | 1 | 0–26 | 20 | 1.05 (1.83) | 0 | 0–10 | 19 | 4.91 (5.39) | 4 | 0–28 | 22 |
| Total PEC Statements | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Med | Range | % | Mean (SD) | Med | Range | % | Mean (SD) | Med | Range | % | ||
| All Codes | PEC | 11.40 (12.71) | 7 | 0–61 | 29 | 5.45 (7.20) | 2.5 | 0–38 | 14 | 22.26 (12.77) | 19 | 2–60 | 57 |
3.3 Cluster Analysis
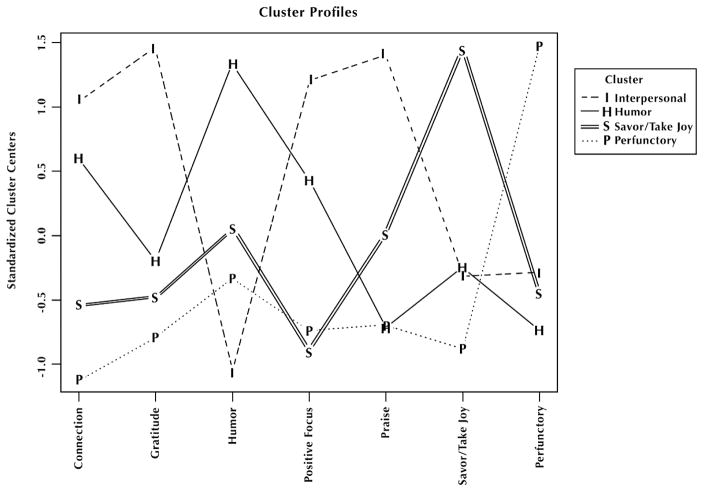
To determine whether there was a pattern to PEC types occurring together during visits, cluster analysis was conducted using Gaussian finite mixture modeling to assign visits into clusters that share a common utterance type pattern. We selected a four cluster solution based on conceptual and statistical fit. We then chose the covariance parameterization based on optimal BIC subject to the four cluster constraint. The optimal between-cluster covariance structure was spherical variances with varying volume. This corresponds to a diagonal covariance matrix. Three types of visits can be characterized by a larger number of utterances from a single category: Savoring/Taking Joy, Humor, and Perfunctory statements. The fourth visit type can be characterized by a larger number of PEC codes, which tend to be more other- or relationship-oriented: Connection, Gratitude, Positive Focus, and Praise (see Figure 1).
Figure 1.
Cluster Analysis of Positive Emotion Expression Codes Occurring Together in Visits
3.4 Trajectory Analysis
We used linear mixed effect regression to estimate the utterance proportion trajectory over time for each PEC category, adjusting for random intercepts at the case level. We did not detect a time effect on the amount of connection, gratitude, positive focus, praise, or perfunctory categories (t < 0.95). We found humor declines at a rate of −0.242 (se = 0.08, t = −2.984) per visit and Savoring declines at a rate of −0.112 (se = 0.037, t = −2.994) per visit. Because of the small increment in decline, these changes are unlikely to be clinically relevant.
4. Discussion
This secondary analysis of nurse-caregiver-patient communication explored PEC prospectively in home hospice. We developed a coding approach based on positive psychology theory in order to identify types and patterns of PEC at end-of-life. Although this is not the first study to capture positive psychology-related constructs at end-of-life, other commonly used approaches rely primarily on self-report measures to capture constructs such as positive emotion (e.g., [48, 49]).
Altogether, our findings suggest that PEC occurs in various forms and frequencies in patients, caregivers, and nurses at end-of-life, up to day of death. Importantly, PEC does not decline closer to day of death. Because positive emotions are thought to be a mechanism to enhance resilience and foster connections with other people [25], they could help promote well-being during palliative care and end-of-life. Prospective studies that systematically investigate the potential benefit of PEC at end-of-life represent an important area of future research.
4.1 PEC Across Nurses, Patients, and Caregivers
Our findings provide evidence of all types of PEC by all stakeholders (nurses, caregivers, and patients). The greatest proportion of PEC was initiated by nurses, who had twice as many expressions per visit as caregivers and four times as many as patients. Although humor was the most frequent PEC overall (e.g., “You’re tougher than an old rattle snake”), nurses most frequently used praise and support during each visit. Typically, this was an expression of encouragement (“you’re doing a great job”) or compliment (e.g., telling the caregiver that her dress looks beautiful on her). This is consistent with previous findings that PEC is a way nurses develop rapport with families [34]; humor, praise and support can all be effectively used to build and maintain relationships in healthcare settings.
Patients had the fewest overall PEC, frequently having no PEC during a visit which was expected given their physical decline. Humor was the most common PEC, and often appeared to function as a means for patients to mitigate others’ discomfort and maintain personal dignity. For example, a patient asked her husband to the leave the room while the nurse did bandaging, and she jokes to the nurse “He just wants to see this incredible operation here.” Savoring or taking joy was the second most frequent patient-initiated PEC. Often this would occur in the form of a memory about food they enjoyed, which is remarkable given that for many people at end-of-life, food is not always enjoyable. Other examples included savoring the warmth of a pair of socks and sharing a description of the sunshine outside. These experiences are made more meaningful given the context of a person who has limited number of days left to take pleasure in the simple things. Joining a patient in reflecting on and savoring an enjoyable moment could be a way to facilitate and strengthen the experience of positive emotion in this setting.
Caregivers initiated twice as much PEC as patients; their most common PEC types per visit were humor followed by savoring. Humor may have been used as a coping strategy to keep caregivers’ feelings of frustration, fear, and uncertainty at bay. It was common for families to joke about the patient living longer than expected (e.g., “He is stubborn”). Caregivers were also most likely to express gratitude and connection relative to their overall PEC. This typically occurred in caregiver-nurse exchanges, where the caregiver expressed gratitude toward the nurse’s support. A central function of gratitude in a social exchange is thought to assist individuals with bonding and maintaining relationships [50, 51]. In the context of end-of-life, expressing gratitude to the nurse may facilitate the therapeutic alliance. Research suggests that those who express gratitude to another person are happier and less depressed [52], and have less caregiver burden [53]. Although the predictive role of PEC on caregiver adjustment is beyond the scope of this manuscript, future research should explore the relationship of PEC such as gratitude with outcomes such as caregiver depression and strain. Our findings about caregiver gratitude expression are similar to findings of a qualitative analysis of family caregivers expressing gratitude for the humane attitude, professional treatment, and emotional support that loved ones received from the palliative care team [54].
4.2 PEC Across Visits
We did not find a systematic variation of proportion or types of PEC across visits. There is a common belief that as death approaches, PEC from families, providers, and patients in hospice decreases and is replaced by grief and distress. However, our data indicate that the relationship between PEC and proximity to patient death is more complicated. It is likely that variation in hospice emotion expression is context- or situation-based. For example, PEC might change as patient symptoms worsen or improve at any point in time, or the quality may shift, e.g. from humor to gratitude. Other influencing factors could include different beliefs about death, changing family situations, or presence of different people (family, friends, other caregivers or healthcare providers) at a visit. Altogether, the lack of systematic variation reflects the variability of the dying process in home hospice.
We identified four visit clusters: other-oriented visits, which included connection, gratitude, praise, and focusing on the positive; humor; savoring; and perfunctory. This latter cluster reflects visits that were largely lacking deep positive emotion, with exchanges being consistent with social etiquette (e.g., “good,” “thanks”). Humor, which was the most common PEC type, has received some attention in healthcare, cancer, and palliative care literature as a means to remedy, cope with, and buffer a wide range of sensitive, embarrassing, fearful, anxious, or abnormal situations (e.g., [55–59]). Studies have shown that humor is valued by patients in hospice (e.g., [59]). It can also facilitate caregiver adjustment during bereavement, and can be a powerful therapeutic asset when used by healthcare providers in a caring, sensitive way [59, 60]. Finally, humor may be the shared language used by patients and their families to regain autonomy and agency amid serious illness [61]. Savoring involves reflecting on an enjoyable moment or special memory, and has received far less attention in the caregiving and palliative care and communication literature. However, some research has shown that savoring positive moments could have a role in ameliorating anxiety and depression in cancer caregivers [62]. More generally, savoring has been associated with greater well-being and could promote resilience in older adults [63].
4.3 Limitations and Future Directions
By basing this project on audio recordings coded with RIAS to capture PEC, we may have missed some positive emotion expressions (e.g., non-verbal expressions, such as facial expressions or touch could convey humor or connection). In addition, using RIAS codes to identify positive emotion could miss more holistic expressions of emotion that may have been better identified through a broader qualitative analysis. In other work [64], we identified an example of a caregiver developing strength and pride in her ability to provide care for her husband. RIAS coding captured statements of positive affect but missed the process of moving from feelings of loss and abandonment to a position of resilience. Furthermore, this study does not address whether PEC by one speaker prompted the experience of positive emotion in another.
Although our sample characteristics for patients and caregivers (e.g. sex, income, and education) are similar to US national statistics available for informal caregivers [65] and hospice [66], there are some differences that should be considered when generalizing our findings to the target population. Caregivers tended to be a bit older (63 years compared to 49) and patients a bit younger than national averages, which likely reflects that our sample consisted of cancer patients married to their caregivers. The majority of primary family caregivers are either spouse/partners or adult children and the relationship dynamic is likely to be different between partners as compared to parent-child, which may influence PEC. Length of hospice stay was twice as long in our sample as the national average for individuals with cancer [66]. Finally, Latter-day Saints were overrepresented in our sample due to the location of one of our data collection sites.
Because this study was exploratory and descriptive, findings should be interpreted with caution; generalizability is limited, and considerations of cultural interpretations of positive emotions should be taken into account. Future prospective studies need to be conducted to better understand potential benefits of positive emotion, particularly in the face of patient variable symptoms at end-of-life, and how PEC could be utilized in nurse-caregiver-patient exchanges to facilitate coping and promote resilience for both patients and caregivers.
4.3 Practice Implications
Focusing on PEC offers a way to bring strengths-based approaches into end-of-life communication research. Previous research has mainly focused on how to identify and reduce caregiver and patient distress. Specifically, health communication research has focused on improving provider communication skills to address and alleviate caregiver and patient negative emotion expression [34, 67]. Equally important is building communication skills to scaffold and build a sense of strength, connection, and joy despite facing loss and life-limiting illness. This may be especially important for caregivers whose difficult task is often not acknowledged by providers [68, 69]. Clearly the expression of both positive and negative emotions is important, particularly at end-of-life when time is limited. Due to the exploratory and novel nature of this study, implications for practice are preliminary.
Highlights.
Developed a coding system for positive emotion communication research
Nurses initiated the most positive emotion communication
End-of-life positive emotion communication occurs in various forms and frequencies
The most frequently used positive emotion code across all speakers was humor
Focusing on positive emotion brings strengths-based approaches into end-of-life care
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award number P01CA138317 (PI Mooney; Project Leader Ellington), and the American Cancer Society under award number ACS MRSG 13-234-01-PCSM (PI Reblin). The co-author Xu was supported by NINR T32 NR 013456-03 (PIs Beck and Pepper). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the American Cancer Society. The authors would like to thank the research staff and participants who make this research possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.He W, Goodkind D, Kowal P U.S. Census Bureau. International Population Reports, P95/16-1, An Aging World: 2015. U.S. Government Publishing Office; Washington, DC: 2016. [Google Scholar]
- 2.NHPCO. [accessed 10.04.17];NHPCO Facts and figures: Hospice care in America. 2015 http://www.nhpco.org/sites/default/files/public/Statistics_Research/2014_Facts_Figures.pdf.
- 3.National Academies of Sciences, Engineering, and Medicine. Families Caring for an Aging America. The National Academies Press; Washington, DC: 2016. [PubMed] [Google Scholar]
- 4.Roth DL, Friedman L, Haley WE. Informal caregiving and its impact on health: a reappraisal from population based studies. Gerontologist. 2015;55:309–19. doi: 10.1093/geront/gnu177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferrario SR, Cardillo V, Vicario F, Balzarini E, Zotti AM. Advanced cancer at home: caregiving and bereavement. Palliat Med. 2004;18:129–36. doi: 10.1191/0269216304pm870oa. [DOI] [PubMed] [Google Scholar]
- 6.Gotze H, Brahler E, Gansera L, Schnabel A, Gottschalk-Fleischer A, Kohler N. Anxiety, depression and quality of life in family caregivers of palliative cancer patients during home care and after the patient's death. Euro J Cancer Care. 2016 doi: 10.1111/ecc.12606. (Ahead of print) [DOI] [PubMed] [Google Scholar]
- 7.Parker Oliver D, Washington K, Smith J, Uraizee A, Demiris G. The prevalence and risks for depression and anxiety in hospice caregivers. J Palliat Med. 2016;20:366–71. doi: 10.1089/jpm.2016.0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pottie CG, Burch KA, Thomas LPM, Irwin SA. Informal caregiving of hospice patients. J Palliat Med. 2014;17:845–856. doi: 10.1089/jpm.2013.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emanuel EJ, Fairclough DL, Slutsman J, Alpert H, Baldwin D, Emanuel LL. Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients. N Eng J Med. 1999;341:956–63. doi: 10.1056/NEJM199909233411306. [DOI] [PubMed] [Google Scholar]
- 10.McPherson CJ, Wilson KG, Murray MA. Feeling like a burden: exploring the perspectives of patients at the end of life. Soc Sci Med. 2007;64:417–27. doi: 10.1016/j.socscimed.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Tang ST, Liu TW, Tsai CM, Wang CH, Chang GC, Liu LN. Patient awareness of prognosis, patient-family caregiver congruence on the preferred place of death, and caregiving burden of families contribute to the quality of life for terminally ill cancer patients in Taiwan. Psychooncology. 2008;17:1202–9. doi: 10.1002/pon.1343. [DOI] [PubMed] [Google Scholar]
- 12.Diener E, Emmons RA. The independence of positive and negative affect. J Pers Soc Psychol. 1984;47:1105–17. doi: 10.1037//0022-3514.47.5.1105. [DOI] [PubMed] [Google Scholar]
- 13.Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley AA, Kirk SB, Austenfeld JL. Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. J Clin Oncol. 2002;20:4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- 14.Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol. 2005;73:212–20. doi: 10.1037/0022-006X.73.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caprara GV, Castellani V, Alessandri G, Mazzuca F, La Torre M, Barbaranelli C, Colaiaco F, Gerbino M, Pasquali V, D'Amelio R, Marchetti P, Ziparo V. Being positive despite illness: The contribution of positivity to the quality of life of cancer patients. Psychol Health. 2016;31:524–34. doi: 10.1080/08870446.2015.1117081. [DOI] [PubMed] [Google Scholar]
- 16.Pinquart M, Sörensen S. Associations of caregiver stressors and uplifts with subjective well-being and depressive mood: a meta-analytic comparison. Aging Ment Health. 20044;8:38–49. doi: 10.1080/13607860410001725036. [DOI] [PubMed] [Google Scholar]
- 17.Hamama L, Sharon M. Posttraumatic growth and subjective well-being among caregivers of chronic patients: A preliminary study. J Happiness Stud. 2013;14:1717–37. [Google Scholar]
- 18.Olver IN, Eliott JA. The use of humor and laughter in research about end-of-life discussions. J Nurs Ed Prac. 2014;4:80–7. [Google Scholar]
- 19.Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 20.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 21.Aspinwall LG, Richter L, Hoffman RR. Understanding how optimism works: An examination of optimists’ adaptive moderation of belief and behavior. Optimism and Pessimism: Implications for Theory, Research, and Practice. 2001:217–38. [Google Scholar]
- 22.Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. 2000;55:647. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- 23.Tugade MM, Fredrickson BL. Regulation of positive emotions: Emotion regulation strategies that promote resilience. J Happiness Stud. 2007;8:311–33. [Google Scholar]
- 24.Park CL. Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychol Bull. 2010;136:257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- 25.Fredrickson BL. What good are positive emotions? RevGen Psychol. 1998;2:300. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol. 2008;95:1045. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Epstein RM, Street RL., Jr . Patient-centered communication in cancer care: Promoting healing and reducing suffering. National Cancer Institute; Bethesda, MD: 2007. [Google Scholar]
- 28.Wiechula R, Conroy T, Kitson AL, Marshall RJ, Whitaker N, Rasmussen P. Umbrella review of the evidence: What factors influence the caring relationship between nurse and patient? J Adv Nurs. 2016;72:723–4. doi: 10.1111/jan.12862. [DOI] [PubMed] [Google Scholar]
- 29.Alpert JM, Womble FE. Coping as a caregiver for an elderly family member. Health Commun. 2015;30:714–721. doi: 10.1080/10410236.2013.879560. [DOI] [PubMed] [Google Scholar]
- 30.Peacock S, Forbes D, Markle-Reid M, Hawranik P, Morgan D, Jansen L, Leipert BD, Henderson SR. The positive aspects of the caregiving journey with dementia: Using a strengths-based perspective to reveal opportunities. J Appl Gerontol. 2010;29:640–59. [Google Scholar]
- 31.Pennebaker WJ. Writing about emotional experiences as a therapeutic process. Psychol Sci. 1997;8:162–6. [Google Scholar]
- 32.Mackenzie CS, Wiprzycka UJ, Hasher L, Goldstein D. Seeing the glass half full: Optimistic expressive writing improves mental health among chronically stressed caregivers. Br J Health Psychol. 2008;13:73–6. doi: 10.1348/135910707X251153. [DOI] [PubMed] [Google Scholar]
- 33.Goranson A, Ritter RS, Waytz A, Norton MI, Gray K. Dying is unexpectedly positive. Psychol Sci. 2017;28:988–99. doi: 10.1177/0956797617701186. [DOI] [PubMed] [Google Scholar]
- 34.Clayton MF, Reblin M, Carlisle M, Ellington L. Communication behaviors used to elicit and address cancer patient/caregiver emotional concerns: A description of home hospice communication. Oncol Nurs Forum. 2014;4:311–21. doi: 10.1188/14.ONF.311-321. [DOI] [PubMed] [Google Scholar]
- 35.Bonanno GA, Moskowitz JT, Papa A, Folkman S. Resilience to loss in bereaved spouses, bereaved parents, and bereaved gay men. J Pers Soc Psychol. 2005;88:827–43. doi: 10.1037/0022-3514.88.5.827. [DOI] [PubMed] [Google Scholar]
- 36.Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med. 1997;45:1207–21. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- 37.Hirdes JP, Freeman S, Smith TF, Stolee P. Predictors of caregiver distress among palliative home care clients in Ontario: Evidence based on the interRAI Palliative Care. Palliat Support Care. 2012;10:155–63. doi: 10.1017/S1478951511000824. [DOI] [PubMed] [Google Scholar]
- 38.Lund DA, Utz R, Caserta MS, de Vries B. Humor, laughter, and happiness in the daily lives of recently bereaved spouses. Omega (Westport) 2008;58:87–105. doi: 10.2190/om.58.2.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bonanno GA, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. J Abnorm Psychol. 1997;106:126. doi: 10.1037//0021-843x.106.1.126. [DOI] [PubMed] [Google Scholar]
- 40.Keltner D, Bonanno GA. A study of laughter and dissociation: distinct correlates of laughter and smiling during bereavement. J Pers Soc Psychol. 1997;73:687. doi: 10.1037//0022-3514.73.4.687. [DOI] [PubMed] [Google Scholar]
- 41.Reblin M, Clayton MF, John KK, Ellington L. Addressing methodological challenges in large communication datasets: Collecting and coding longitudinal interactions in home hospice cancer care. Health Commun. 2015;18:1–9. doi: 10.1080/10410236.2014.1000480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ellington L, Clayton MF, Reblin M, Donaldson G, Latimer S. Communication among cancer patients, caregivers, and hospice nurses: Content, process, and change over time. Patient Ed Couns. doi: 10.1016/j.pec.2017.09.013. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roter D, Larson S. The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46:243–51. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 44.Ellington L, Reblin M, Clayton MF, Berry P, Mooney K. Hospice nurse communication with cancer patients and their family caregivers. J Palliat Med. 2012;15:262–8. doi: 10.1089/jpm.2011.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ellington L, Clayton MF, Reblin M, Donaldson G, Latimer S. Assessing triadic home hospice communication among cancer patients, caregivers, and nurses. doi: 10.1016/j.pec.2017.09.013. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seligman MEP. Authentic Happiness. Simon and Schuster; New York: 2009. [Google Scholar]
- 47.Fraley C, Raftery AE. Model-based clustering, discriminant analysis and deny estimation. JASA. 2002;97:611–31. [Google Scholar]
- 48.Rabkin JG, McElhiney M, Moran P, Acree M, Folkman S. Depression, distress and positive mood in late-stage cancer: a longitudinal study. Psychooncology. 2009;18:79–86. doi: 10.1002/pon.1386. [DOI] [PubMed] [Google Scholar]
- 49.Van der Lee ML, Swarte NB, Van der Bom JG, Van den Bout J, Heintz AP. Positive feelings among terminally ill cancer patients. Euro J Cancer Care. 2006;15:51–5. doi: 10.1111/j.1365-2354.2005.00619.x. [DOI] [PubMed] [Google Scholar]
- 50.Lambert NM, Fincham FD. Expressing gratitude to a partner leads to more relationship maintenance behavior. Emotion. 2011;11:52. doi: 10.1037/a0021557. [DOI] [PubMed] [Google Scholar]
- 51.Watkins PC, Van Gelder M, Frias A. Furthering the science of gratitude. Oxford Handbook of Positive Psychology. 2009;41:437. [Google Scholar]
- 52.Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: Empirical validation of interventions. Am Psychol. 2005;60:410. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 53.Amaro LM. Dyadic effects of gratitude on burden, conflict, and contribution in the family caregiver and sibling relationship. J Appl Commun Res. 2017;45:61–78. [Google Scholar]
- 54.Centeno C, Arantzamendi M, Rodríguez B, Tavares M. Letters from relatives: A source of information providing rich insight into the experience of the family in palliative care. J Palliat Care. 2010;26:167–75. [PubMed] [Google Scholar]
- 55.Beach WA, Prickett E. Laughter, humor, and cancer: Delicate moments and poignant interactional circumstances. Health Commun. 2016:1–12. doi: 10.1080/10410236.2016.1172291. [DOI] [PubMed] [Google Scholar]
- 56.du Pré A. Humor and the healing arts: A multimethod analysis of humor use in health care. Lawrence Erlbaum Associates; Mahwah, NJ: 1998. [Google Scholar]
- 57.Haakana M. Laughter in medical interaction: From quantification to analysis, and back. J Socioling. 2002;6:207–35. [Google Scholar]
- 58.McCreaddie M, Payne S. Humour in healthcare interactions: A risk worth taking. Health Expect. 2014;17:332–44. doi: 10.1111/j.1369-7625.2011.00758.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ridley J, Dance D, Pare D. The acceptability of humor between palliative care patients and health care providers. J Palliat Med. 2014;17:472–4. doi: 10.1089/jpm.2013.0354. [DOI] [PubMed] [Google Scholar]
- 60.Dean RAK, Gregory DM. More than trivial: Strategies for using humor in palliative care. Cancer Nurs. 2005;28:292–300. doi: 10.1097/00002820-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 61.Gramling D, Gramling R. Laughing at the dark: tactical humor for autonomous decision making in serious illness. J Palliat Med. 2012;15:1170–2. doi: 10.1089/jpm.2012.0279. [DOI] [PubMed] [Google Scholar]
- 62.Hou WK, Lau KM, Ng SM, Lee TMC, Cheung HYS, Shum TCY, Cheng ACK. Psychological detachment and savoring in adaptation to cancer caregiving. Psychooncology. 2016;25:839–47. doi: 10.1002/pon.4019. [DOI] [PubMed] [Google Scholar]
- 63.Smith JL, Hollinger-Smith L. Savoring, resilience, and psychological well-being in older adults. Aging Ment Health. 2015;19:192–200. doi: 10.1080/13607863.2014.986647. [DOI] [PubMed] [Google Scholar]
- 64.Reblin M, Otis-Green S, Ellington L, Clayton MF. Strategies to support spirituality in health care: An example from a home hospice cancer caregiver. J Holist Nurs. 2014;32:269–77. doi: 10.1177/0898010114531856. [DOI] [PubMed] [Google Scholar]
- 65.National Alliance for Caregiving and AARP. Caregiving in the US. 2015 Nov; ( www.aarp.org)
- 66.NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization; Sep, 2017. [Google Scholar]
- 67.Clayton MF, Hulett J, Kaur K, Reblin M, Wilson A, Ellington L. Nursing support of home hospice caregivers on the day of cancer patient death. Oncol Nurs Forum. 2016 doi: 10.1188/17.ONF.457-464. In press. scheduled for print July 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.National Academies of Sciences, Engineering, and Medicine. Families Caring for an Aging America. The National Academies Press; Washington, DC: 2016. [PubMed] [Google Scholar]
- 69.Boehmer KR, Egginton JS, Branda ME, Kryworuchko J, Bodde A, Montori VM, Leblanc A. Missed opportunity? Caregiver participation in the clinical encounter, A videographic analysis. Patient Educ Couns. 2014;96:302–7. doi: 10.1016/j.pec.2014.05.016. [DOI] [PubMed] [Google Scholar]