Abstract
Objectives
To investigate the association between epilepsy and antiepileptic drugs and serious transport accidents requiring emergency care or resulting in death.
Methods
We identified 29,220 individuals 18 years or older with epilepsy without cerebral palsy or intellectual disability and 267,637 matched controls using Swedish registers. This nationwide cohort was followed from 2006 to 2013 for serious transport accidents. We used Cox regression to analyze the risk of serious transport accidents between individuals with epilepsy and matched controls, and then stratified Cox regression to compare the risk during periods of medication with the risk during nonmedication period within the same individual with epilepsy. We adjusted for civil status, employment, education, living area, psychiatric disorders prior to the start of follow-up, and psychotropic medication.
Results
Compared to matched controls, individuals with epilepsy were at increased risk of serious transport accidents (hazard ratio [HR] 1.37; 95% confidence interval [CI] 1.29–1.46). There were increased risks of pedestrian accidents (HR 2.24, 95% CI 1.69–2.97), bicycle accidents (HR 1.68, 95% CI 1.49–1.89) and car accidents (HR 1.31, 95% CI 1.19–1.44). However, among patients with a diagnosis of epilepsy, use of antiepileptic drugs did not influence the risk of serious transport accidents in population-level comparisons (HR 0.97; 95% CI 0.85–1.11) or within-individual comparisons (HR 0.99; 95% CI 0.69–1.42).
Conclusion
Serious transportation accidents were more common in individuals with epilepsy, but this risk was independent of use of antiepileptic drugs.
Epileptic seizures can be associated with impaired awareness and uncontrolled motor activity affecting the ability to drive safely,1 and also imposing risks for bicycle, motorcycle, or pedestrian accidents.2 Restrictions for motor vehicle driving, which vary between countries, have been imposed on individuals with epilepsy, leading to important effects on everyday life.3 Treatment with antiepileptic drugs (AEDs)4,5 is for many a prerequisite for meeting the regulatory requirements for seizure control needed for driving, while on the other hand adverse effects of AEDs may impair driving abilities.6,7 Adding to the complexity, individuals with epilepsy often have comorbidities, which can affect the ability to handle traffic.8–10
Most studies regarding epilepsy and risks associated with driving rely on self-reported car crashes, leading to inconsistent and inconclusive results.11,12 Previous studies have focused on motor vehicle accidents, while data on accident risks for persons with epilepsy traveling on bicycle or other non-car-related accidents are scarce.
For the purpose of patient counseling and as a basis for recommendations on reasonable restrictions, there is an urgent need for more accurate and representative data on risks of traffic accidents in people with epilepsy. We have therefore carried out a nationwide cohort study of serious transport accidents (STA) in people with epilepsy utilizing Swedish health care registries, including motor vehicle as well as bicycle and pedestrian accidents. We have also assessed the effect of AEDs on STA.
Methods
Through Sweden's National Patient Register (NPR),13 we identified all individuals born between 1960 and 1992 with ≥2 inpatient or outpatient diagnoses of epilepsy, according to the ICD-8 to ICD-10 (table e-1, links.lww.com/WNL/A286). Status epilepticus and febrile convulsions were not included in our definition of epilepsy (table e-1). Patients with a lifetime diagnosis of either cerebral palsy or intellectual disability (table e-1) were excluded, as these disorders pose an additional burden of comorbidity.
Study participants were followed between the second diagnosis of epilepsy, age 18 years, or July 1, 2006, whichever came last, and December 31, 2013, emigration, or death, whichever occurred first.
The main outcome measure was STA, defined as having an ICD-10 code of V01-V99 (table e-2, links.lww.com/WNL/A286) in the NPR or the Cause of Death Register, hence “serious” is defined as having an emergency visit at a hospital or death. The accidents were divided into the following groups: car (the coding does not distinguish between driver or passenger), motorcycle, bicycle, and pedestrian, all involving collision with a vehicle, or for pedestrian, accidents during transport (for a detailed description, see table e-2). We restricted traffic accidents to “emergency” (unplanned) hospital visits to rule out that a visit was due to rehabilitation for a previous traffic accident.
We obtained data on sociodemographic factors (marriage or registered partner, employment, education) and living area (urban vs countryside) from the Integrated Database for Labour Market Research (LISA).
Data on pharmacologic treatment were obtained through the Swedish Prescribed Drug Registry, which includes information on all dispensed medications since July 1, 2005, registered as Anatomical Therapeutic Chemical Classification (ACT) codes.14 AEDs and psychotropic medication according to ACT codes are described in table e-3 (links.lww.com/WNL/A286). For the main analysis, all AEDs registered in Sweden were used. Information on psychiatric disorders was collected from the NPR.
We analyzed risks of STA in individuals with epilepsy using stratified Cox regression to calculate hazard ratios (HRs). Each patient with epilepsy was matched to up to 10 controls for sex and age at the year of diagnosis. Controls were selected from the Total Population Register.15 Analyses were adjusted for sociodemographic factors, earlier psychiatric medication, and psychotropic medication. Study participants with missing values on sociodemographic factors and living area were excluded (309 patients with epilepsy and 26,358 controls) from the adjusted analysis. We estimated the excess number of accidents in patients with epilepsy. We analyzed individuals without any psychiatric disorders prior to the start of follow-up separately.
To investigate the association between AED and STA among individuals with epilepsy, we first used between-individual Cox regression and then stratified Cox regression with each individual entering as a separate stratum (within-individual analyses).16 In the later approach, each patient served as his or her own control, and the rate of accidents during AED was compared to the same individual while untreated. AED treatment was included as a time-varying exposure.
Patients were defined as on treatment with AED if the interval between 2 dispensed AED prescriptions was ≤12 months. In case 2 prescriptions were more than 12 months apart, active treatment was defined as the first 12 months after withdrawal of medication from the pharmacy.
In our sensitivity analysis, we compared 2 older AEDs (carbamazepine and oxcarbazepine) with 2 newer AEDs (levetiracetam and lamotrigine) as monotherapy. Further, we performed sensitivity analyses for the association between AEDs and STA in patients without any earlier psychiatric disorders prior to the start of follow-up.
In one of the sensitivity analyses, we used the 6 months cutoff to define treatment interval (instead of 12 months cutoff in the main analyses) to test whether the results were influenced by the choice of exposure (AED medication) definition.
Statistical analyses were conducted using SAS (SAS Institute, Cary, NC) software. HRs with 95% confidence intervals (CIs) that did not include 1.0 were regarded as statistically significant.
Standard protocol approvals, registrations, and patient consents
The study was approved by the Regional Ethics Review Board (2013/5:8), Stockholm, which adjudicated that individual informed consent was not required.17
Results
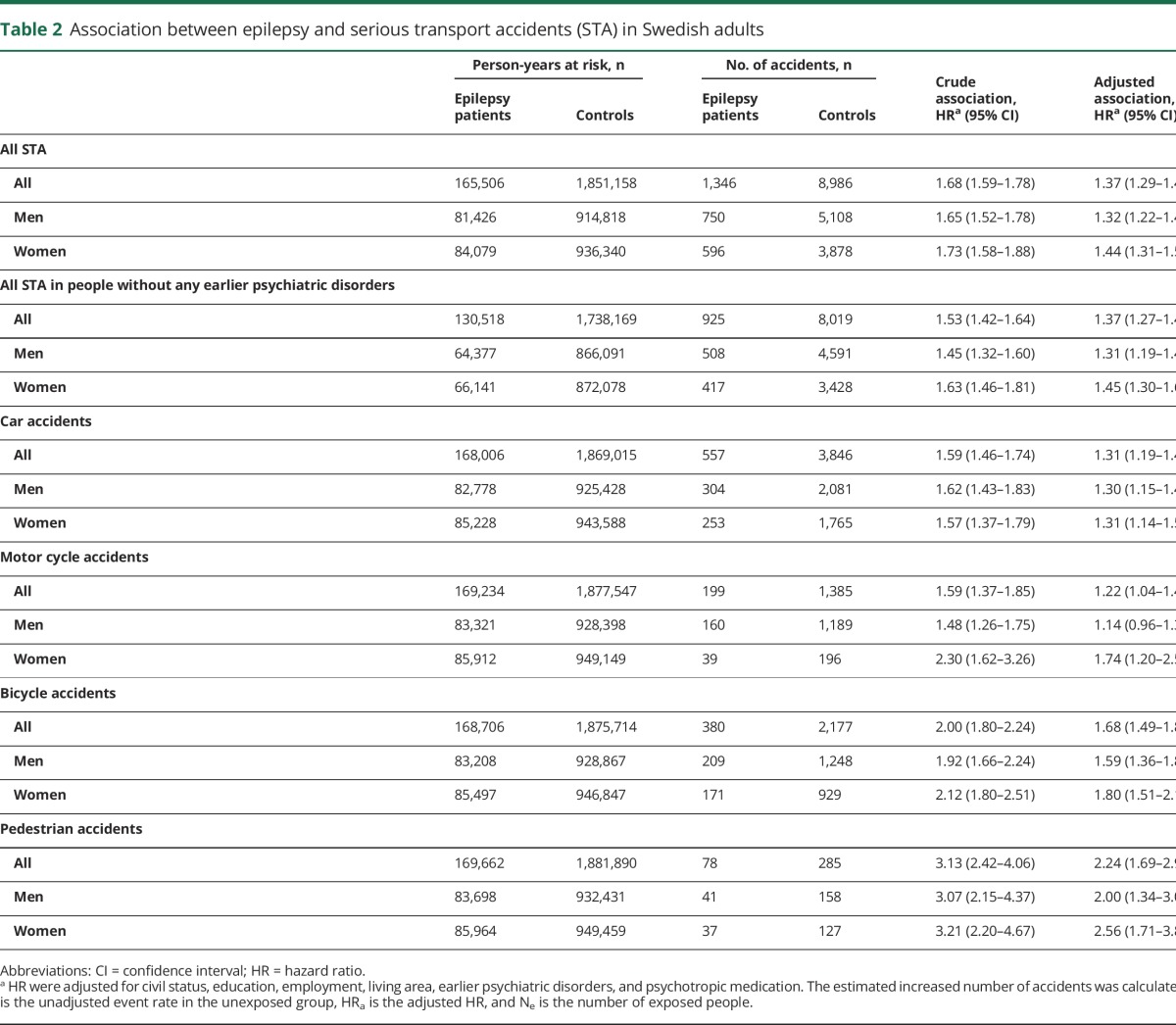
The study population consisted of 29,220 individuals with epilepsy and 267,637 controls (table 1). Among individuals with epilepsy, 24.1% had an earlier psychiatric disorder, compared to 6.3% of the controls (table 1). Antidepressants were the most common group of psychotropic medications (17.6%), followed by hypnotics/anxiolytics (15.0%), among individuals with epilepsy, compared to 5.6% and 3.0%, respectively, among controls (table 1). Of individuals with epilepsy, 75.3% received AEDs and 4.6% experienced at least one STA during follow-up compared to 3.4% of the controls (table 1). For further characteristics of the cohort, see table 1. Fewer than 0.1% of epilepsy patients and their controls died from STA during follow-up (table 1).
Table 1.
Sample characteristics of patients with epilepsy and controls at baseline
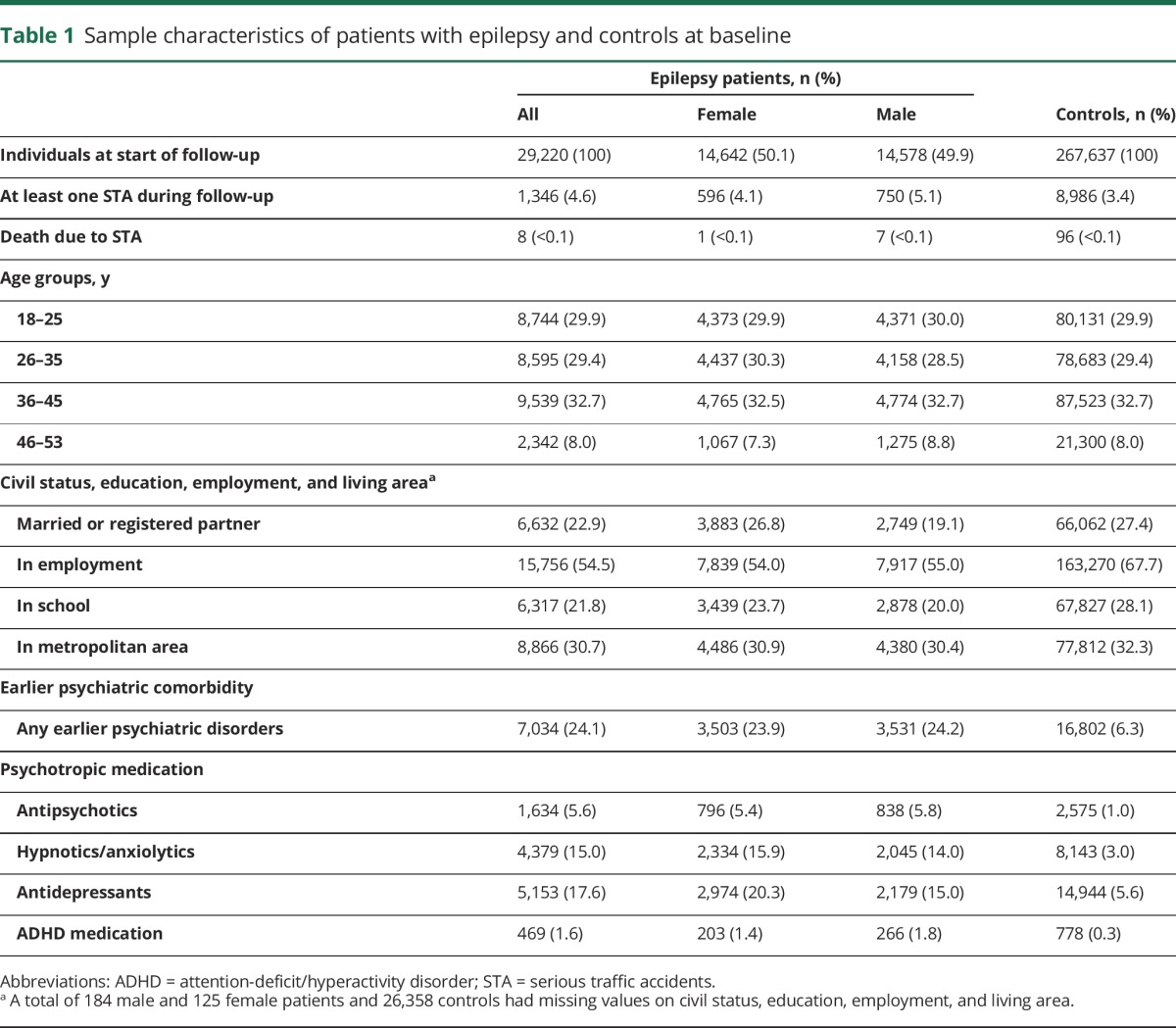
Individuals with epilepsy showed significantly higher rates of STA than those without epilepsy (table 2); the unadjusted HR was 1.68 (95% CI 1.59–1.78). Adjusting for confounders, the HR was 1.37 (95% CI 1.29–1.46), with no difference between men and women (table 2).
Table 2.
Association between epilepsy and serious transport accidents (STA) in Swedish adults
Epilepsy was linked to a 2.2-fold increased risk of pedestrian accidents (HR 2.24, 95% CI 1.69–2.97), a 1.7-fold risk of bicycle accidents (HR 1.68, 95% CI 1.49–1.89), and finally a 1.3-fold increased risk of car accidents (HR 1.31, 95% CI 1.19–1.44) (table 2). The increased number of accidents per year in individuals with epilepsy was 297.3 (95% CI 233.0–369.6) (table 2). Table 2 presents additional data.
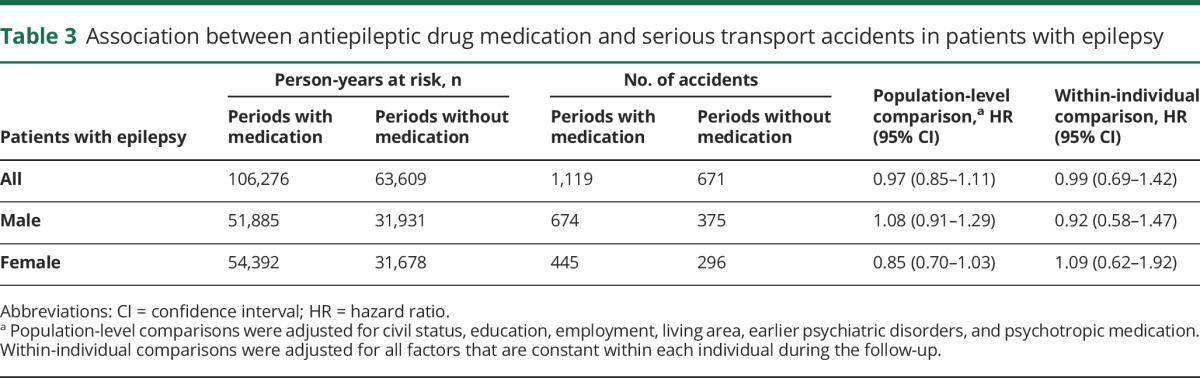
We found no significant differences in accidents rates among individuals with epilepsy during periods with AED medication compared to periods without, in the within-individual comparison or in the population-level comparison (table 3).
Table 3.
Association between antiepileptic drug medication and serious transport accidents in patients with epilepsy
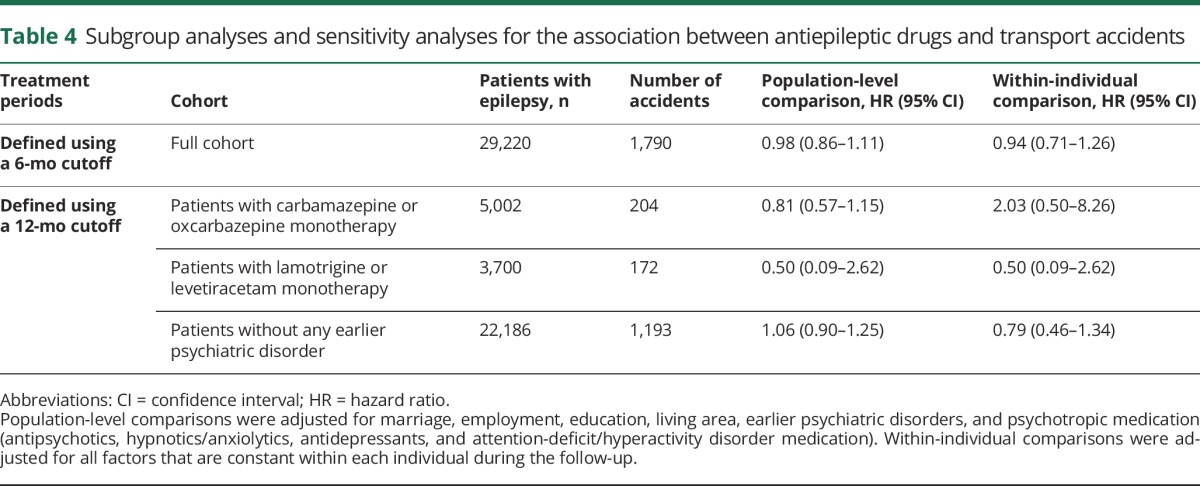
The HRs of STA in patients with levetiracetam/lamotrigine monotherapy or on oxcarbazepine/carbamazepine monotherapy were not different from the main analysis (table 4).
Table 4.
Subgroup analyses and sensitivity analyses for the association between antiepileptic drugs and transport accidents
Discussion
In this nationwide cohort study of over 29,000 individuals with epilepsy, we found a 37% increased risk of STA. The risk increase was especially high in cyclists and pedestrians. We found no association between AED treatment and risk of STA.
Our findings of an excess risk of car accidents are in line with earlier data, including a Danish study that found that drivers with epilepsy are more often treated at an emergency department after a motor vehicle accident.18 A French study based on national databases found that drivers exposed to AEDs (n = 251) had an increased risk of being responsible for a crash (OR 1.74, 95% CI 1.29–2.34) and concluded that the increased risk was more likely related to seizures than the effect of AEDs.19 Another record linkage study on long-term chronic disease and transportation accidents, including 80 individuals with epilepsy, found a 2.5-fold increased risk for crash responsibility in patients with epilepsy.20 However, contradictory data exist (no association with accidents) based on self-reported3,11,12,21 and register-based data.22 One reason for the lack of association in the Canadian article could be lack of study power, as their adjusted OR was 1.38 (95% CI 0.97–1.96).22 Their study included 10,240 individuals with epilepsy as compared to almost 3 times as many in our study.22
In the current study, the risk of STA was similar in men and women with epilepsy. This is in line with the increased risk of accidents in patients with diabetes, where sex has no significant influence on the collision risk,23 even though male drivers in general have an increased risk of accidents.24 The frequency of female drivers varies considerably between different countries and cultures. In Sweden, sex differences are small, which reinforces our result that there is no biological effect of sex when it comes to STA for individuals with epilepsy.
The associations between epilepsy and STA could not be fully explained by comorbid psychiatric disorders; hence it is probably epilepsy as such that is the main reason for the increased risk.
We found a 2.2-fold risk of pedestrian STA among epilepsy patients, which is consistent with a previous study that found a more than 2-fold risk of injuries in street accidents as well as an overall increased risk of accidents in epilepsy patients.2
In our study, approximately 25% of individuals with epilepsy were not on medication during follow-up. This likely represents, to a large extent, patients whose epilepsy is in remission or resolved, and for whom medication has been withdrawn. Another explanation might be nonadherence to AED treatment, as this is common (between 26% and 50% in one study).25,26
Both scenarios could explain why we did not find any association between STA and medication status, not even in the within-patient analysis, where each individual with epilepsy served as his or her own control. We did not find any difference in the comparison between carbamazepine/oxcarbazepine and levetiracetam/lamotrigine; nor did Orriols et al.19 find any difference in STA risk according to AED class.
Strengths
This is the largest study on epilepsy and STA so far, and with increased statistical power we were able to demonstrate small risk differences. We used the NPR to ascertain epilepsy; this register has been used before to define epilepsy.27,28 Hence this population-based study includes all individuals with epilepsy 18 years or older, except for those with comorbid cerebral palsy and intellectual disability, in Sweden. In this way, all types and severities of epilepsy are included, reflecting their occurrence in the population. Several previous studies may potentially suffer from selection bias as only certain subgroups of epilepsy patients have been included.11,12 Different methods have been used to report accidents in individuals with epilepsy, from reporting over shorter time intervals to lifetime accident rates.11,12 In our approach, we calculated the risk in comparison to matched controls and also reported adjusted results. Our within-individual analyses regarding medication with AED, or not, allowed us to adjust for potential unmeasured but important confounders such as type and severity of epilepsy, mental and motor abilities, genetic predisposition, and somatic comorbidities. To our knowledge, our study is the first to examine all types of STA.
Limitations
Our study had some limitations. None of the registers used had information on driver's license ownership, if the epilepsy patients were actually driving, and whether they were actually responsible for the accident. These circumstances were the same for individuals with epilepsy and our controls. Previous studies regarding epilepsy and driving have shown that 73% of individuals with epilepsy have a driver's license, compared to 94% of the general adult population.3 However, through excluding individuals with comorbid cerebral palsy and intellectual disability, the proportion of driver's license holders probably increased. Still, the lower proportion of potential drivers among epilepsy patients may have diluted the association between epilepsy and STA.
A further limitation of the study is the lack of information on seizure control among the epilepsy patients, which also complicates the interpretation of associations with AED treatment. Those who are off medication may be so because their epilepsy is resolved and thus less exposed to risks imposed by seizures.
As our outcome was transport accidents that resulted in emergency hospital visits or death, minor accidents were not included. We cannot rule out that patients with epilepsy who regularly visit hospitals for their chronic disease are more prone to seek care for accidents and if so, this would drive up our risk estimates.
As our findings are based on a cohort living in Sweden, a country with small costs for health care, reduced costs for medication, and a rather low general rate of transport accidents, generalizations across cultures/countries should be made with caution, also taking into account the Swedish requirements for driver's licenses.
Interpretations
Individuals with epilepsy are at a moderately increased risk of STA, and AED medication does not seem to influence that risk. We cannot determine to what extent the increased risk is seizure-related, but other studies have shown that the majority of car crashes in individuals with epilepsy are not caused by a seizure,29,30 although accidents in general seem to be.2 In comparison to individuals with diabetes, where the only link to an increased risk of collisions is hypoglycemia23 (introduced by medication), the increased risk in epilepsy patients does not seem to be associated with medication or earlier psychiatric comorbidity.
To regulate driving is not easy as such regulations aim to maximize public safety while preserving individual freedom as much as possible.31 Studies have shown that the length of seizure freedom is important, yet the shortening of these periods has not led to more accidents.32 In Sweden, individuals with epilepsy must have been seizure-free the last 12 months, following the regulations being implemented in the European union.33 Many individuals with epilepsy are driving regardless of whether they are allowed to, and the reporting of these patients is low.34,35 However, mandatory reporting of patients by their physician has not been shown to reduce the risk of accidents.3
Bicycle accidents in the general population are a growing problem as cycling becomes increasingly popular,36 which is probably true also for individuals with epilepsy. The increased risk of 70% should have implications both for implementations of safety measures and counseling of individuals with epilepsy. Our results raise the same concern for pedestrians with epilepsy.
There is a significantly increased risk for STA in individuals with epilepsy. This increased risk does not seem to be influenced by sex. It is of importance to further investigate the circumstances that contribute to this increased risk of STA among individuals with epilepsy. With that knowledge, it might be possible to educate individuals with epilepsy about preventive measures rather than implement stricter regulations.
Glossary
- ACT
Anatomical Therapeutic Chemical Classification
- AED
antiepileptic drug
- CI
confidence interval
- HR
hazard ratio
- ICD
International Classification of Diseases
- NPR
National Patient Register
- STA
serious transport accidents
Footnotes
Editorial, page 583
Patient Page: NPub.org/patient
Author contributions
Heléne E.K. Sundelin: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval. Zheng Chang: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval, statistical analysis. Henrik Larsson: drafting/revising the manuscript, accepts responsibility for conduct of research and final approval, acquisition of data, study supervision, obtaining funding. Paul Lichtenstein: drafting/revising the manuscript, study concept or design, accepts responsibility for conduct of research and final approval, acquisition of data, obtaining funding. Catarina Almqvist: drafting/revising the manuscript, accepts responsibility for conduct of research and final approval, acquisition of data, obtaining funding. Torjörn Tomson: drafting/revising the manuscript, analysis or interpretation of data, accepts responsibility for conduct of research and final approval. Jonas F. Ludvigsson: drafting/revising the manuscript, study concept or design, analysis or interpretation of data, accepts responsibility for conduct of research and final approval.
Study funding
Z.C.: the Swedish Research Council for Health, Working Life and Welfare (2014-2780). H.L.: the Swedish Research Council (2014-3831) and the Swedish Initiative for Research on Microdata in the Social and Medical Sciences (SIMSAM), framework grant no. 340-2013-5867. P.L.: the Swedish Research Council for Health, Working Life and Welfare (project 2012-1678) and the Swedish Research Council (2011-2492). C.A.: the Swedish Research Council through the Swedish Initiative for Research on Microdata in the Social and Medical Sciences (SIMSAM) framework grant no 340-2013-5867TT: Stockholm County Council (ALF). J.F.L.: None.
Disclosure
H. Sundelin and Z. Chang report no disclosures relevant to the manuscript. H. Larsson has served as a speaker for Eli Lilly and has received a research grant from Shire (both outside the submitted work). P. Lichtenstein and C. Almqvist report no disclosures relevant to the manuscript. T. Tomson is a full-time employee of Karolinska Institutet, has been associate editor of Epilepsia and is currently the same for Epileptic Disorders, has received speaker's honoraria to his institution from Eisai, UCB, and Actavis, and received research support from Stockholm County Council, CURE, GSK, UCB, Eisai, Bial, and Novartis (outside the submitted work). J. Ludvigsson reports no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Aschkenasy MT, Drescher MJ, Ratzan RM. Physician reporting of medically impaired drivers. J Emerg Med 2006;30:29–39. [DOI] [PubMed] [Google Scholar]
- 2.van den Broek M, Beghi E; RESt-1 Group. Accidents in patients with epilepsy: types, circumstances, and complications: a European cohort study. Epilepsia 2004;45:667–672. [DOI] [PubMed] [Google Scholar]
- 3.McLachlan RS, Starreveld E, Lee MA. Impact of mandatory physician reporting on accident risk in epilepsy. Epilepsia 2007;48:1500–1505. [DOI] [PubMed] [Google Scholar]
- 4.Brodie MJ. Outcomes in newly diagnosed epilepsy in adolescents and adults: insights across a generation in Scotland. Seizure 2017;44:206–210. [DOI] [PubMed] [Google Scholar]
- 5.Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med 2000;342:314–319. [DOI] [PubMed] [Google Scholar]
- 6.Brunbech L, Sabers A. Effect of antiepileptic drugs on cognitive function in individuals with epilepsy: a comparative review of newer versus older agents. Drugs 2002;62:593–604. [DOI] [PubMed] [Google Scholar]
- 7.Witt JA, Elger CE, Helmstaedter C. Adverse cognitive effects of antiepileptic pharmacotherapy: each additional drug matters. Eur Neuropsychopharmacol 2015;25:1954–1959. [DOI] [PubMed] [Google Scholar]
- 8.Selassie AW, Wilson DA, Martz GU, Smith GG, Wagner JL, Wannamaker BB. Epilepsy beyond seizure: a population-based study of comorbidities. Epilepsy Res 2014;108:305–315. [DOI] [PubMed] [Google Scholar]
- 9.Lin JJ, Mula M, Hermann BP. Uncovering the neurobehavioural comorbidities of epilepsy over the lifespan. Lancet 2012;380:1180–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rai D, Kerr MP, McManus S, Jordanova V, Lewis G, Brugha TS. Epilepsy and psychiatric comorbidity: a nationally representative population-based study. Epilepsia 2012;53:1095–1103. [DOI] [PubMed] [Google Scholar]
- 11.Classen S, Crizzle AM, Winter SM, Silver W, Eisenschenk S. Evidence-based review on epilepsy and driving. Epilepsy Behav 2012;23:103–112. [DOI] [PubMed] [Google Scholar]
- 12.Naik PA, Fleming ME, Bhatia P, Harden CL. Do drivers with epilepsy have higher rates of motor vehicle accidents than those without epilepsy? Epilepsy Behav 2015;47:111–114. [DOI] [PubMed] [Google Scholar]
- 13.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register: opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 2007;16:726–735. [DOI] [PubMed] [Google Scholar]
- 15.Ludvigsson JF, Almqvist C, Bonamy AE, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol 2016;31:125–136. [DOI] [PubMed] [Google Scholar]
- 16.Allison PD. Fixed Effects Regression Models. Thousand Oaks, CA: SAGE Publications; 2009. [Google Scholar]
- 17.Ludvigsson JF, Haberg SE, Knudsen GP, et al. Ethical aspects of registry-based research in the Nordic countries. Clin Epidemiol 2015;7:491–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lings S. Increased driving accident frequency in Danish patients with epilepsy. Neurology 2001;57:435–439. [DOI] [PubMed] [Google Scholar]
- 19.Orriols L, Foubert-Samier A, Gadegbeku B, et al. Prescription of antiepileptics and the risk of road traffic crash. J Clin Pharmacol 2013;53:339–344. [DOI] [PubMed] [Google Scholar]
- 20.Orriols L, Avalos-Fernandez M, Moore N, et al. Long-term chronic diseases and crash responsibility: a record linkage study. Accid Anal Prev 2014;71:137–143. [DOI] [PubMed] [Google Scholar]
- 21.Taylor J, Chadwick D, Johnson T. Risk of accidents in drivers with epilepsy. J Neurol Neurosurg Psychiatry 1996;60:621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwon C, Liu M, Quan H, Thoo V, Wiebe S, Jette N. Motor vehicle accidents, suicides, and assaults in epilepsy: a population-based study. Neurology 2011;76:801–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hostiuc S, Negoi I, Hostiuc M. Diabetes and collision risk: a meta-analysis and meta-regression. Int J Clin Pract 2016;70:554–568. [DOI] [PubMed] [Google Scholar]
- 24.Donnelly-Swift E, Kelly A. Factors associated with single-vehicle and multi-vehicle road traffic collision injuries in Ireland. Int J Inj Contr Saf Promot 2016;23:351–361. [DOI] [PubMed] [Google Scholar]
- 25.Faught E. Adherence to antiepilepsy drug therapy. Epilepsy Behav 2012;25:297–302. [DOI] [PubMed] [Google Scholar]
- 26.Chang Z, Lichtenstein P, D'Onofrio BM, Sjolander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry 2014;71:319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattsson P, Tomson T, Eriksson O, Brannstrom L, Weitoft GR. Sociodemographic differences in antiepileptic drug prescriptions to adult epilepsy patients. Neurology 2010;74:295–301. [DOI] [PubMed] [Google Scholar]
- 28.Nilsson L, Tomson T, Farahmand BY, Diwan V, Persson PG. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia 1997;38:1062–1068. [DOI] [PubMed] [Google Scholar]
- 29.Chen J, Yan B, Lu H, et al. Driving among patients with epilepsy in West China. Epilepsy Behav 2014;33:1–6. [DOI] [PubMed] [Google Scholar]
- 30.Bicalho MA, Sukys-Claudino L, Guarnieri R, Lin K, Walz R. Socio-demographic and clinical characteristics of Brazilian patients with epilepsy who drive and their association with traffic accidents. Epilepsy Behav 2012;24:216–220. [DOI] [PubMed] [Google Scholar]
- 31.Berg AT, Engel J Jr. Restricted driving for people with epilepsy. Neurology 1999;52:1306–1307. [DOI] [PubMed] [Google Scholar]
- 32.Drazkowski JF, Fisher RS, Sirven JI, et al. Seizure-related motor vehicle crashes in Arizona before and after reducing the driving restriction from 12 to 3 months. Mayo Clin Proc 2003;78:819–825. [DOI] [PubMed] [Google Scholar]
- 33.Winston GP, Jaiser SR. Western driving regulations for unprovoked first seizures and epilepsy. Seizure 2012;21:371–376. [DOI] [PubMed] [Google Scholar]
- 34.Berg AT, Vickrey BG, Sperling MR, et al. Driving in adults with refractory localization-related epilepsy: Multi-Center Study of Epilepsy Surgery. Neurology 2000;54:625–630. [DOI] [PubMed] [Google Scholar]
- 35.Krauss GL, Krumholz A, Carter RC, Li G, Kaplan P. Risk factors for seizure-related motor vehicle crashes in patients with epilepsy. Neurology 1999;52:1324–1329. [DOI] [PubMed] [Google Scholar]
- 36.Gopinath B, Jagnoor J, Craig A, et al. Describing and comparing the characteristics of injured bicyclists and other injured road users: a prospective cohort study. BMC Public Health 2016;16:324. [DOI] [PMC free article] [PubMed] [Google Scholar]