Xu et al. provide the first study in patients with intractable epilepsy showing a direct correlation between the phenotype, activation state, cytokine profiles, and ability to cause neuronal apoptosis of brain-infiltrating peripherally derived immune cells with seizure severity using an unbiased flow cytometric approach.
Abstract
The pathophysiology of drug-resistant pediatric epilepsy is unknown. Flow cytometric analysis of inflammatory leukocytes in resected brain tissues from 29 pediatric patients with genetic (focal cortical dysplasia) or acquired (encephalomalacia) epilepsy demonstrated significant brain infiltration of blood-borne inflammatory myeloid cells and memory CD4+ and CD8+ T cells. Significantly, proinflammatory (IL-17– and GM-CSF–producing) γδ T cells were concentrated in epileptogenic lesions, and their numbers positively correlated with disease severity. Conversely, numbers of regulatory T (T reg) cells inversely correlated with disease severity. Correspondingly, using the kainic acid model of status epilepticus, we show ameliorated seizure activity in both γδ T cell– and IL-17RA–deficient mice and in recipients of T reg cells, whereas T reg cell depletion heightened seizure severity. Moreover, both IL-17 and GM-CSF induced neuronal hyperexcitability in brain slice cultures. These studies support a major pathological role for peripherally derived innate and adaptive proinflammatory immune responses in the pathogenesis of intractable epilepsy and suggest testing of immunomodulatory therapies.
Introduction
The pathogenesis and progression of treatment-resistant epilepsy are poorly understood (Xu et al., 2013). Spontaneous seizures associated with epilepsy affect up to 1% of the world’s population with more than half of the cases in children (Hauser et al., 1996; Banerjee et al., 2009; Nelson et al., 2011). About one-third of these patients develop drug-resistant epilepsy defined as therapeutic failure of at least two anticonvulsants (Kwan and Brodie, 2000; Berg and Kelly, 2006; Kwan and Sperling, 2009; Kwan et al., 2010), which provide symptomatic seizure control without addressing the underlying pathophysiology (Guerrini, 2006).
Drug-resistant epilepsy often starts with an isolated prolonged convulsion in early life, a remission period, followed by recurring intractable seizures (Sagar and Oxbury, 1987; Harvey et al., 1995; Koh et al., 1999; Berg and Rychlik, 2015). Recent evidence suggests a link between neuroinflammation and epileptogenesis (Fabene et al., 2008; Vezzani et al., 2011; Xu et al., 2013). Several commonly prescribed anticonvulsants have antiinflammatory effects (Goto et al., 2003; Bibolini et al., 2011; Chuang et al., 2014). Additionally, corticosteroids have shown promising results in refractory epilepsy cases and in select epilepsy syndromes (Chutorian et al., 1968; Gayatri et al., 2007; Grosso et al., 2008; Xu et al., 2013). A small fraction of patients with drug-resistant epilepsy undergo resective brain surgery as a final attempt to reduce seizure burden (Téllez-Zenteno et al., 2005).
Human studies substantiating the contribution of blood-borne leukocytes in epilepsy development and progression to support the use of antiinflammatory therapies are lacking. To gain a better understanding of the immunopathogenesis of epilepsy, we performed flow cytometric characterization of brain-infiltrating and brain-resident immune cells in surgically resected brain tissues from pediatric patients diagnosed with two leading causes of intractable epilepsies: focal cortical dysplasia (FCD; ∼50%) presumably caused by somatic mutation and encephalomalacia (EM; ∼20%) caused by brain injury (Kabat and Król, 2012).
We demonstrate significant infiltration of the brain parenchyma by activated memory CD4+ helper and CD8+ cytotoxic T lymphocytes, as well as blood-borne inflammatory myeloid cells. Moreover, we demonstrate for the first time that proinflammatory IL-17–producing γδ T lymphocytes are concentrated in the epileptogenic zone, and their numbers positively correlate with seizure severity, whereas the numbers of brain-infiltrating regulatory T cells (T reg cells) inversely correlate with disease severity. These findings are corroborated by animal experiments demonstrating similar activation of innate and adaptive immune responses in the brains of a mouse model of status epilepticus induced by the chemoconvulsant, kainic acid (KA). In line with our human data, we show that both IL-17RA– and γδ T cell–deficient mice display less severe seizures, whereas autologous natural T reg (nT reg) cell depletion worsens and T reg cell supplementation dampens seizure susceptibility. Moreover, we show that IL-17 causes enhanced neuronal hyperexcitability in hippocampal pyramidal neurons. Uniquely, our data support an important pathological role for blood-derived leukocytes in epileptogenesis and provide evidence for the development and testing of novel and safe disease-modifying treatments targeting brain infiltration of peripheral immune cells.
Results
Activated infiltrating peripheral myeloid cells, not microglia, correlate with seizure frequency
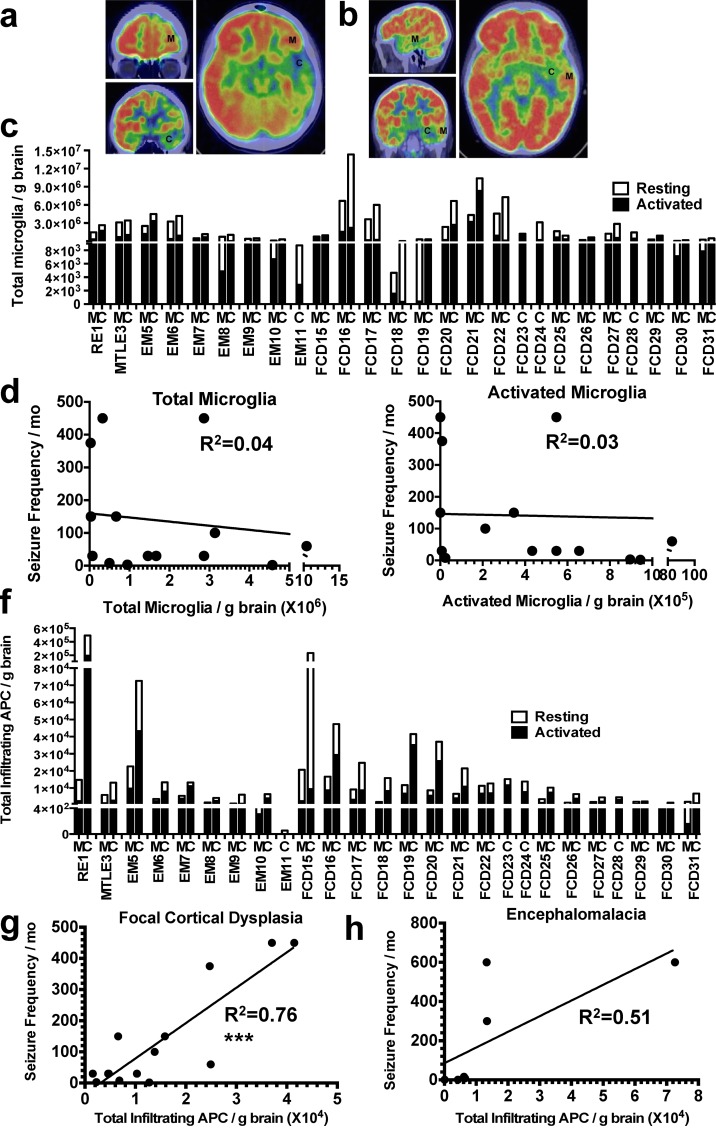
Apart from Rasmussen’s encephalitis (RE; Rogers et al., 1994; Atkins et al., 1995; Bien et al., 2002; Varadkar et al., 2014), other intractable pediatric epilepsy syndromes have rarely been associated with brain infiltration of peripheral leukocytes (Choi and Koh, 2008; Xu et al., 2013). Using an unbiased flow cytometric analysis of leukocyte infiltrates in 33 resected brains of pediatric RE, mesial temporal lobe epilepsy (MTLE), EM, or FCD patients (Table S1), we initially analyzed the numbers and activation states of brain-resident microglia and brain-infiltrating peripheral myeloid APCs, including inflammatory monocytes, macrophages, and dendritic cells (DCs) from the lesion margin and epileptogenic center in the same patient. The demarcation of lesion margin and epileptogenic center was defined as a hypometabolic zone by fluorodeoxyglucose-positron emission tomography (FDG-PET; Fig. 1, a and b) and verified by intraoperative corticography. The heterogeneity of the human population and the plasticity of young developing brains make it highly challenging to compare between healthy adult controls from autopsy, which were what previous adult studies used, and pediatric epilepsy populations (Iyer et al., 2010; He et al., 2016). We therefore used a lesion margin with near-normal metabolic function as an internal control to help control for patient individuality, as an autologous blood sample and the marginal zone of the resected brain from the same patient are the most relevant controls that were available to us. Microglia have long been considered the major driving force of brain inflammation in epilepsy (Walker and Sills, 2012; Vezzani et al., 2013; Vezzani, 2014). Several studies have suggested a possible correlation between microglia activation and seizure in both human and murine models of chronic seizure induced by KA (Boer et al., 2006; Amhaoul et al., 2015). To better understand the contribution of microglia versus blood-borne APCs to seizure burden, we quantified the number of microglia and brain-infiltrating APCs from the blood using a well-established flow cytometric panel composed of a combination of antibodies against CD39, CD11c, and CD45 to distinguish these two cell populations. Microglia are CD39hi/CD45int/CD11clow, whereas the infiltrating APCs are CD11chi/CD39low-int/CD45hi. In humans, CD11c is a panmyeloid cell marker expressed by monocytes, macrophages, neutrophils, myeloid DCs, and microglia, much like its counterpart CD11b, the panmyeloid cell marker in mice (Cobbold and Waldmann, 1987; Kim et al., 2015). We have also verified the specificity of the CD39/CD11c/CD45 antibody cocktail to distinguish microglia and peripherally derived APCs using an antibody to TMEM119, a newly identified microglia-specific marker for both humans and mice, which stains the same population of cells in the brain as the antibody cocktail (Fig. 5 e and Fig. S1; Bennett et al., 2016; Satoh et al., 2016). Interestingly, the correlation between microglia activation and seizure was lacking in our pediatric cohort. There was no difference between the absolute numbers of microglia per gram of brain when comparing an RE patient (RE1) with frequent seizures and an MTLE patient (MTLE3) with much less frequent seizures (Fig. 1 c and Fig. S1). Similarly, almost all EM (EM5–11) and FCD (FCD15–31) patients showed comparable numbers of microglia in the epileptogenic center, with no differences noted when compared with the epileptogenic margin, irrespective of the disease etiology (Fig. 1 c). Neither the absolute numbers of microglia (Fig. 1 d; R2 = 0.04 and P = 0.47) nor the numbers of activated microglia displaying up-regulated levels of MHC II and the costimulatory molecules CD80/CD86 (Fig. 1 e; R2 = 0.03 and P = 0.53) correlated with electroencephalography (EEG)-confirmed seizure frequency (Table S1). In contrast, there was a nearly 40-fold difference in the number of total and activated infiltrating APCs in the epileptogenic center between patients with severe (RE1) and milder seizures (MTLE3; Fig. 1 f). Remarkably, the total numbers of infiltrating peripheral APCs (>80% activated; Fig. 1 f) significantly correlated with seizure frequency for FCD patients (P < 0.001; Fig. 1 g), and a strong trend existed for correlation for EM patients (P = 0.07; Fig. 1 h). Although we acknowledge previous studies reporting the important role of glia, including astrocytes and microglia, in epileptogenesis caused by their unique anatomical locations and physiological support for neurons, the APC correlation data indicate that the contribution of peripheral immune cells to epilepsy development early on should not be neglected (Boer et al., 2006; Amhaoul et al., 2015) This finding challenges the widely held view that RE is the unique immune-related epilepsy syndrome.
Figure 1.
Clinical relevance of brain-resident microglia and brain-infiltrating APCs in epileptic brains. (a and b) PET scan demarcates the epileptogenic center (C), and the lesion margin (M) served as internal control for patients RE1 (a) and MTLE3 (b). (c) Number of resting and activated microglia in the epileptogenic center and the lesion margin of patients diagnosed with RE (n = 1), MTLE (n = 1), EM (n = 7), and FCD (n = 17). (d and e) Correlation of seizure frequency with quantity of total (d) or activated microglia (e) in the epileptogenic center of FCD 2 patients. (f) Quantity of resting and activated infiltrating myeloid APCs in the epileptogenic center and the lesion margin of patients diagnosed with RE (n = 1), MTLE (n = 1), EM (n = 7), and FCD (n = 17). (g and h) Correlation of seizure frequency with quantity of total APCs in the epileptogenic center of FCD II (g) and EM (h) patients. ***, P < 0.001. P-values calculated using Student’s t test. R2 determined using Pearson’s correlation analysis.
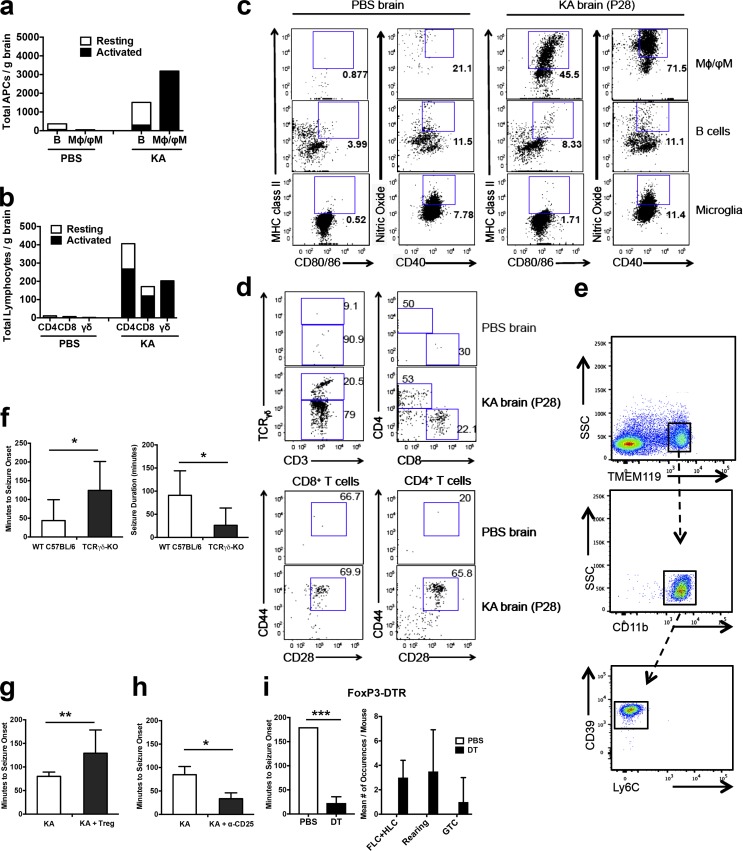
Figure 5.
Characterization of innate and adaptive immune effector and regulatory T cells in the mouse model of KA-SE. (a–d) Numbers (a and b) and frequencies (c and d) of resting and activated brain-infiltrating APCs (a and c) and T cells (b and d) in single-hit KA injected WT C57BL/6 mice (pooled from six mice). Three independent repeats were performed. (e) CD11b+Ly6C−CD39+ microglia costained for TMEM119, a novel microglia-specific marker for both human and mouse. Three independent repeats were performed. (f) Seizure onset latency and duration measured in single-hit KA injected wt C57BL/6 versus γδ T cell KO mice. Data represents a total of eight mice of each strain pooled from three separate experiments. (g) Seizure onset measured immediately after the second-hit of KA in unmanipulated (KA) and T reg cells supplemented (KA + T reg) C57BL/6 mice (n = 11 each) pooled from two separate experiments. (h) Unmanipulated (KA) and T reg cell–depleted (KA + α-CD25; n = 6 each) C57BL/6 mice 14 d after the first-hit of KA pooled from two separate experiments. (i) Seizure onset and frequency of seizure behavior measured immediately after the second-hit of KA in DT-injected (n = 4) and control (PBS, n = 3) FoxP3-DTR-eGFP mice. Data were pooled from two separate experiments. HLC, hind-limb clonus; FLC, fore-limb clonus; GTC, general tonic-clonic seizure, Mφ, macrophage; ϕM, inflammatory monocytes. Data are represented as means ± SD. *, P < 0.05; **, P < 0.01; ***, P < 0.001. P-values calculated using Student’s t test.
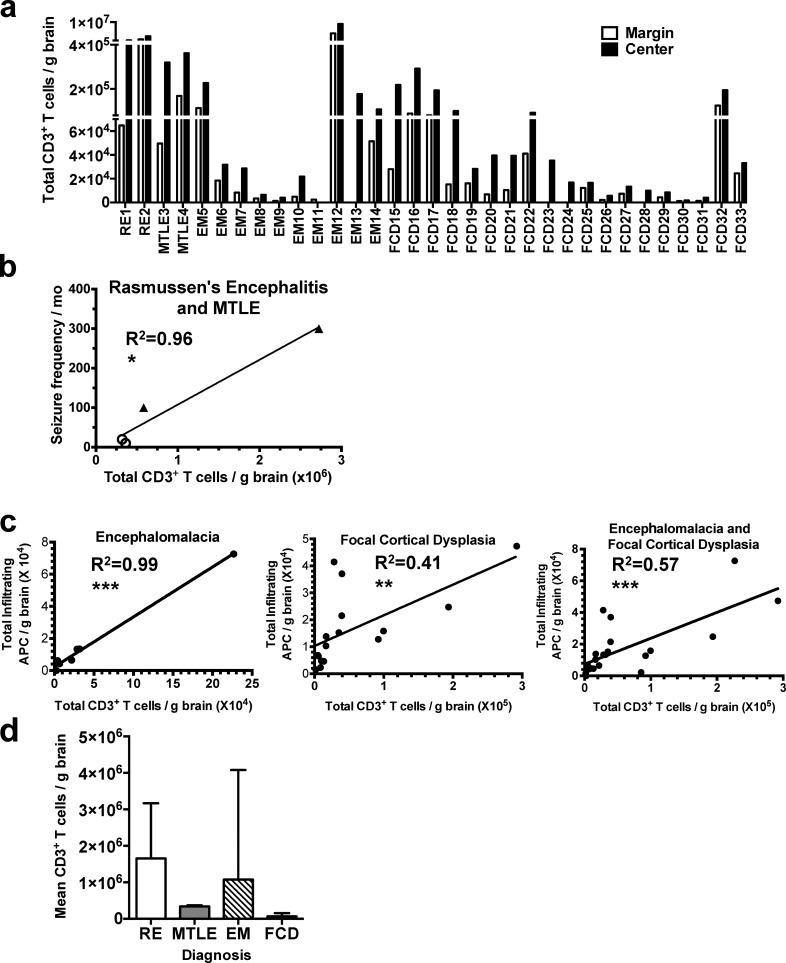
Identification of activated conventional αβ T cells in the epileptogenic center
Activated innate immune cells initiate and sustain central nervous system (CNS)–adaptive immune responses (McMahon et al., 2005). CD3+ T cells, natural killer (NK) cells, and B cells were observed in the epileptogenic center (Fig. 2 a and Figs. S1, S2 and S3). The absolute numbers of infiltrating CD3+ T lymphocytes strongly correlated (R2 = 0.96 and P = 0.02) with EEG-confirmed seizure frequency in RE and MTLE patients, even with the limited number of subjects with these diagnoses available to us (Fig. 2 b). RE represents a more severe form of epilepsy, whereas MTLE represents a milder form. Although not significantly different as a result of low patient numbers for the RE and MTLE diagnoses, this trend supports the finding that the mean total number of CD3+ T cells for patients in each diagnostic category is proportional to the general disease severity in addition to seizure frequency. Surprisingly, the absolute numbers of infiltrating CD3+ T lymphocytes also correlated with the numbers of blood-borne infiltrating APCs, but not activated microglia, in FCD and EM patients (Fig. 2 c). Total CD3 counts positively correlated with seizure frequency similarly to the numbers of infiltrating APCs (not depicted). Destructive lesions as seen in EM and RE that cause cortical atrophy, cognitive deficit, and motor weakness as well as frequent seizures displayed a trend of higher numbers of CD3+ T cells compared with MTLE and FCD (Fig. 2 d).
Figure 2.
Clinical significance of brain-infiltrating CD3+ T cells. (a) Numbers of brain-infiltrating CD3+ T cells in the lesion margin and lesion center of patients diagnosed with RE (n = 2), MTLE (n = 2), EM (n = 10), and FCD (n = 19). (b) Correlation between seizure frequency and CD3+ T cell count in two RE (shaded triangles) and two MTLE (open circles) patients. (c) Correlation of brain-infiltrating CD3+ T cells with total APC counts detected in the epileptogenic center of EM and FCD patients. (d) Mean CD3+ T cell count by diagnosis (RE, n = 2; MTLE, n = 2; EM, n = 10; and FCD, n = 19). Data in d represent means ± SD. We have included all the subjects, except those treated with steroid that may compromise immune readout, with data available for each subset of cells being interrogated in the correlation study. *, P < 0.05; **, P < 0.01; ***, P < 0.001. P-values calculated using Student’s t test. R2 determined using Pearson’s correlation analysis.
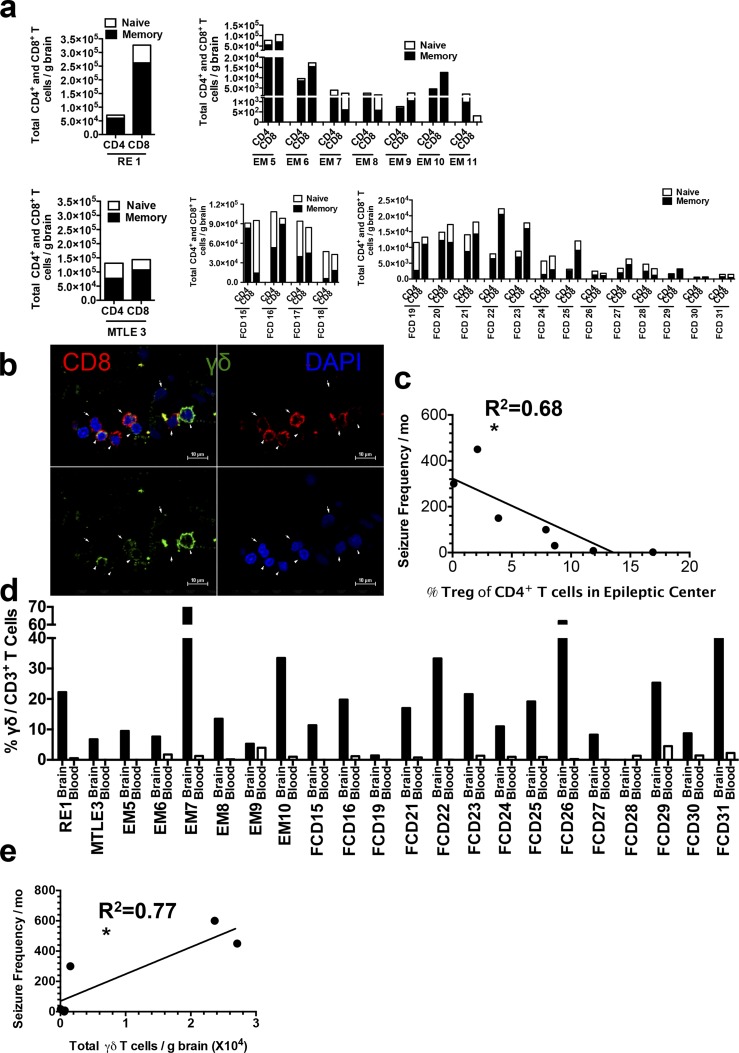
Among conventional αβ T cells, CD8+ T cells were the dominant population detected in patients’ brains. The blood CD8/CD4 T cell ratio was the normal value of 1:3, but was reversed to values between 1:1 to 7:1 in the brain, indicating their enrichment (Fig. 3 a and Fig. S3 c). The CD8+ and γδ T cells (Fig. 3 b) were localized in the epileptogenic center as shown by immunohistochemical (IHC) staining. The vast majority of CD4+ and CD8+ T cells were antigen-experienced memory cells, as indicated by surface expression of CD45RO and IL-7 receptor α chain (CD127) in the absence of CD62L and CD45RA (Fig. 3 a and Fig. S2), suggesting potential reactivity to brain antigens. Both brain-infiltrating CD4+ and CD8+ T cells highly expressed integrins (very late antigen-4 [VLA-4] and lymphocyte function–associated antigen-1 [LFA-1]) essential for transmigration across the intact blood–brain barrier (BBB; Fig. 3 d and S2). We also detected T reg cells (CD4+Foxp3+CD25+) in the brains of RE, EM, and FCD patients, which made various levels of IL-10, and remarkably, their abundance inversely correlated (R2 = 0.68 and P < 0.02) with seizure frequency (Fig. 3 c). This correlation analysis includes all of the patients examined for T reg cell numbers. The limited number of patients analyzed for T reg cell profile and function was a result of the restricted amount of the tissue that was available and, more importantly, the development of the study as we only started focusing on T reg cell for their role in epileptogenesis toward the advanced stage of the study.
Figure 3.
Clinical significance of T reg and γδ T cells detected in the epileptic lesion center. (a) Quantity of resting and activated CD4+ and CD8+ T cells in the epileptic center of patients grouped by diagnosis. (b) Single channel and merged confocal micrographs of a brain section of a representative patient (EM13) showing CD8 T cells, γδ T cells, and nuclei. The true signals are circular and in close proximity to the blue DAPI stained nuclei. Arrows indicate locations of CD8+ and γδ T cells. (c) Correlation of seizure frequency with the percentage of T reg cells in the epileptic center of all the patients (RE1; EM6; and FCD15, 16, 19, 22, and 25) analyzed for the T reg cell subset by flow cytometry. (d) Percentage of γδ T cells in the total CD3+ T cell population in the brain and blood. (e) Correlation of seizure frequency with quantity of γδ T cells in the epileptic center of all the EM patients (5, 6, 7, 9, and 10) analyzed for the γδ subset by flow cytometry. (R2 = 0.77). We have included all the subjects, except those treated with steroid that may compromise immune readout, with data available for each subset of cells being interrogated in the correlation study. *, P < 0.05. P-values calculated using Student’s t test. R2 determined using Pearson’s correlation analysis.
γδ T cells infiltrate the brains of non-RE patients
A subset of CD3+ T cells using unconventional γδ TCRs were detected at a surprisingly high frequency in EM and FCD patients, as well as in RE patients, as previously described (Owens et al., 2015). γδ T cells are commonly found with high abundance at epithelial and mucosal surfaces, but comprise <0.7% of the circulating leukocytes. In the majority of the non-RE patients, >10% of CD3+ T cells in the brain parenchyma were γδ+ (Fig. 3, d and b). The mean percentage for the 20 non-RE patients was 21.9%, comparable to the RE patient level of 22.2%. Notably, >25% of CD3+ T cells in the epileptogenic zone in 6/20 patients with EM or FCD were γδ+, with the highest frequency being 75% (Fig. 3 d). Thus, infiltration of γδ T cells in the epileptogenic zone is a common feature of intractable epilepsy, and the brain γδ T cell numbers correlated (R2 = 0.77 and P = 0.02) with seizure frequency in EM patients (Fig. 3 e) and exhibited a strong trend of correlation that is not statistically significant for the FCD patients (not depicted).
Potential immune-mediated mechanisms of neuronal loss
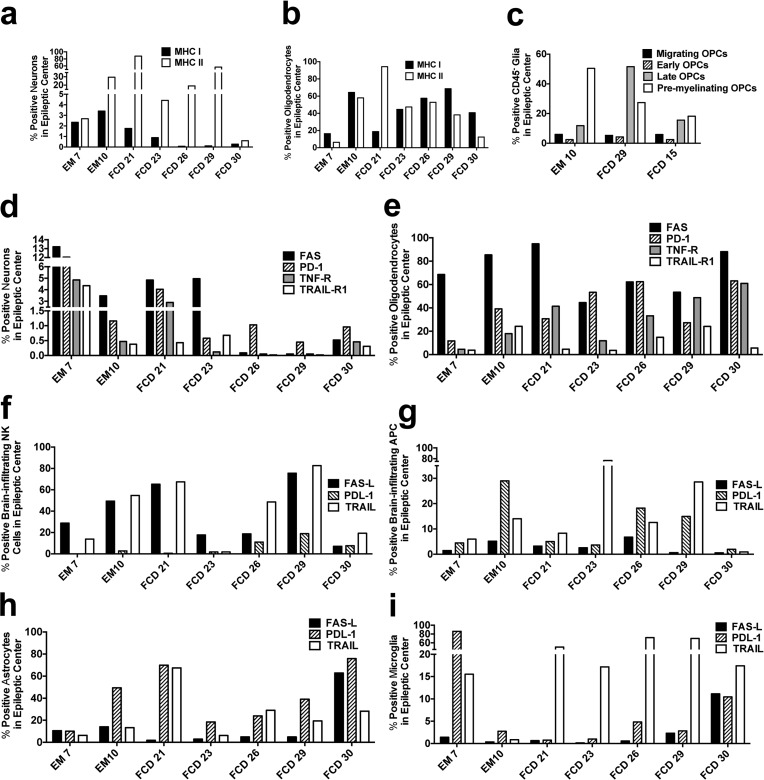
Based on the immune subsets identified, multiple potential mechanisms of immune-mediated neuronal loss and glial damage are possible. Related to MHC-restricted pathogenic mechanisms mediated by CD8+ and CD4+ αβ T cells in EM and FCD patients, we found varied percentages of neurons expressing MHC class I, averaging 1.3% (highest value = 3.4%; Fig. 4 a and Fig. S4). Surprisingly, the neuronal expression of MHC class II exceeded that of MHC class I with a mean of 28.7% (maximum = 87.9%; Fig. 4 a), suggesting that neurons in the epileptic brain may be capable of presenting antigenic peptides to both CD8+ and CD4+ T cells and, hence, be susceptible to lymphocyte-mediated killing. MHC expression was also unexpectedly found in mature oligodendrocytes with mean expression levels for MHC I and II similar at 44.4% and 44.2%, respectively (Fig. 4 b). Demyelination has been associated with seizures in epilepsy (Libenson et al., 1994; Hoffmann et al., 2008; Totolian et al., 2011), and loss of myelin sheaths can lead to neuronal loss. In the epileptogenic centers of both selected EM and FCD patients expressing the highest levels of MHC class I and II, late oligodendrocyte progenitor cells (OPC) and the premyelinating oligodendrocytes were the predominant subsets observed (Fig. 4 c).
Figure 4.
Frequencies of apoptotic receptors and ligands in brain-resident and brain-infiltrating cells. (a and b) Percentages of MHC class I and II–expressing neurons (a) and oligodendrocytes (b). (c) Ratio of OPCs at various developmental stages. (d and e) Frequencies of neurons (d) and oligodendrocytes (e) expressing apoptotic receptors. (f–i) Percentages of NK cells (f), brain-infiltrating APCs (g), astrocytes (h), and microglia (i) expressing apoptotic ligands.
Neuronal apoptosis is a hallmark of epilepsy. We therefore examined surface expression of known apoptotic receptors (apoptosis-stimulating fragment [FAS], programed cell death protein 1 [PD-1], TNF receptor [TNF-R], and receptor 1 for TNF-related apoptosis-inducing ligand [TRAIL-R1]) that lead to cell death in neurons and oligodendrocytes (Martin-Villalba et al., 2001; Dörr et al., 2002; Morrison et al., 2003; Hövelmeyer et al., 2005). FAS and PD-1 were predominantly expressed by neurons, whereas oligodendrocytes also expressed TNF-R (Fig. 4, d and e). In contrast, TRAIL-R1 was expressed at basal levels on both neurons and oligodendrocytes. Apoptotic ligands for these receptors were differentially expressed by glia and infiltrating leukocytes. FAS ligand (FAS-L) was primarily expressed by NK cells, and PD-L1 by infiltrating APCs and astrocytes (Fig. 4, f–h), whereas microglia expressed little of either (Fig. 4 i). TRAIL was expressed ubiquitously by both glia and infiltrating leukocytes. Collectively, these results suggest that NK cells may induce apoptosis in neurons and mature oligodendrocytes via the FAS–FAS-L pathway, whereas infiltrating APCs and astrocytes may use the PD-1–PD-L1 pathway. Interestingly, microglia would appear to contribute little to neuronal or oligodendrocyte loss via any of these apoptotic pathways.
Cytokines produced by inflammatory cells in epileptogenic lesions
We used intracellular cytokine staining to enumerate the numbers of cytokine-producing, brain-resident microglia and astrocytes, as well as infiltrating APCs and T cells. Conventional TCRαβ CD4+ T cells directly ex vivo produced predominantly IFN-γ, TNF-α, GM-CSF, and IL-17, and the frequencies for all cytokines increased to ∼40% after PMA/ionomycin stimulation (Fig. S5, a and b). Cytokine production by CD8+ T cells directly ex vivo was variable in all patients, with patient RE1 producing mainly IFN-γ, whereas the EM and FCD patients produced a combination of proinflammatory cytokines, which were greatly enhanced upon PMA/ionomycin stimulation (Fig. S5, c and d). APCs from several FCD patients produced primarily IL-12 directly ex vivo, whereas astrocytes mainly produced IL-1β. (Fig. S5, e and f). IL-6 and TNF-α were produced at similar frequencies by infiltrating APCs and astrocytes. Microglia had the lowest frequencies of cytokine-producing cells. Upon LPS stimulation, only marginal increases in frequencies of cytokine-producing microglia, infiltrating APCs, and astrocytes were noted.
Functional roles for γδ T cells and T reg cells in animal models of status epilepticus
To support a potential functional role for brain-infiltrating immune cells in the induction and regulation of epileptogenesis, we used the mouse model of KA-induced status epilepticus (KA-SE; Hampson and Manalo, 1998). Our time course study on brain-infiltrating immune cells in the single-hit KA-SE model showed that brain-infiltration by peripheral APCs gradually increases from day 1 to day 3, followed by lymphocyte infiltration, and indicated that the best time point to examine diverse innate and adaptive immune cell types is day 7 after KA injection, even though seizure onset is generally observed within 1 h after intraperitoneal delivery of KA, dependent on the dose of KA. We hypothesize that infiltration of peripheral effector immune cells, but not T reg cells, evoked by the first seizure precipitates subsequent ictal events in humans and mice. We thus first examined the immune activation status of an acute seizure induced by a single hit of KA. Compatible with our clinical epilepsy findings, even a single hit of KA-induced status epilepticus resulted in cortical infiltration of activated APCs and memory αβ and γδ T cells in postnatal day 28 (P28) mice, which is considered comparable to 6 mo of age in humans with minimal hormonal influence on seizure (Dutta and Sengupta, 2016; Fig. 5, a and b). The majority of the brain-infiltrating APCs in KA-SE mice were highly activated, expressing costimulatory molecules (CD40, CD80, and CD86), MHC class II, and nitric oxide, compared with microglia, which were mildly activated with a much lower frequency of cells positive for these activation markers (Fig. 5, a and c). Microglia and infiltrating APCs were distinguished using the combination of antibodies against CD39/CD11b/CD45 and confirmed by TMEM119 staining, similar to the staining performed for the human samples (Fig. 5 e). >65% of the brain-infiltrating CD4+ and CD8+ T cells exhibited a memory phenotype (CD44high) with elevated expression of activation markers (CD69+/CD28+/CD25+; Fig. 5, b and d) and integrins known to facilitate crossing of the BBB (not depicted). Significantly, >20% of the CD3+ T cells were γδ T cells (Fig. 5 b). The immune profile identified in the brain of acute KA-SE model was corroborated in a chronic epilepsy model using intrahippocampal injection of KA in C57BL/6 mice at weeks 1, 2, and 4 after KA delivery with infiltration limited mostly to the hippocampus (not depicted). To determine the functional pathogenicity of infiltrating γδ T cells, we compared latency to clinical seizure onset and total seizure duration in sex-, age-, and background-matched WT control and γδ T cell–deficient C57BL/6 mice. γδ KO mice displayed significantly delayed clinical seizure onset (P = 0.03) and reduced duration (P = 0.01; Fig. 5 f), suggesting an important role for γδ T cells in seizure induction, even in an acute seizure model. This is consistent with the positive correlation of γδ T cell numbers with seizure frequency in EM patients (Fig. 3 e). Lastly, we tested the effects of autologous CD4+CD25+Foxp3+ nT reg cells in the “two-hit” KA-SE model. To understand the influence of early seizures on subsequent seizures, we used a two-hit KA mouse model to measure the effect of immune modulation after induction of the first seizure on the subsequent second hit seizure. Remarkably, recipient mice with prior KA-SE receiving two i.v. infusions of nT reg cells displayed significantly decreased seizure susceptibility and severity upon a second administration of a KA in a two-hit model of epileptogenesis (Fig. 5 g), and conversely, T reg cell inactivation/depletion with anti-CD25 (Fig. 5 h) or using diphtheria toxin (DP) in FoxP3-DTR transgenic mice (Fig. 5 i) augmented clinical seizure severity, supporting the inverse correlation of T reg cell numbers with seizure frequency in epileptogenic human brains (Fig. 3 c). We did not perform EEG recording because the procedure significantly damages the BBB and leads to inflammatory responses and thus bias when examining the immune responses in the brain.
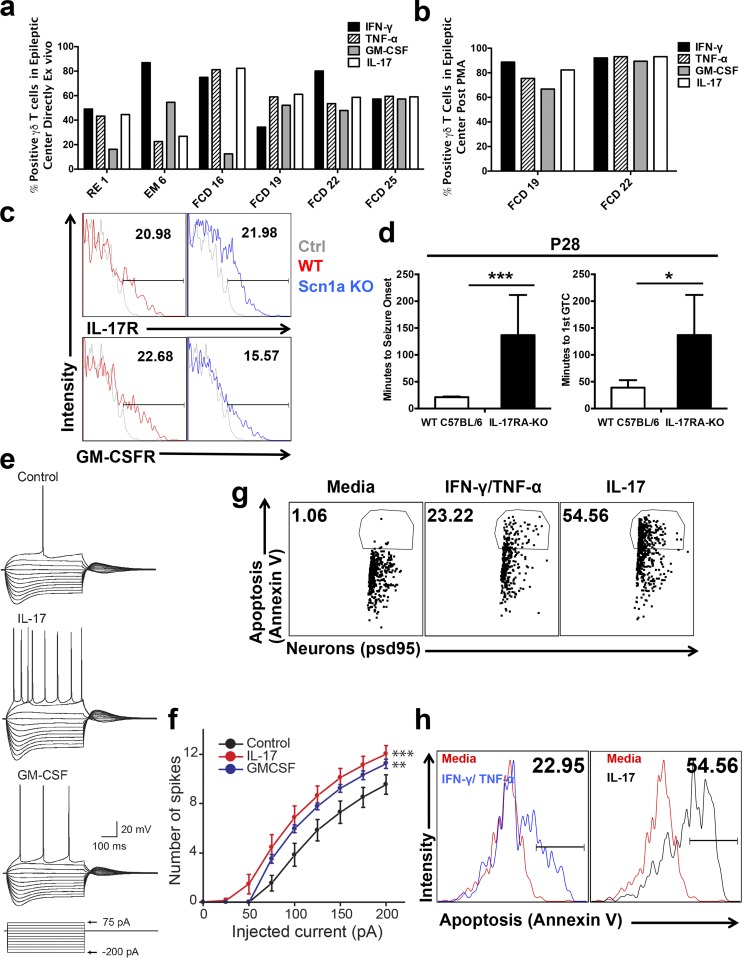
Direct effect of IL-17 and GM-CSF on the neuronal excitability and viability
>50% of γδ T cells directly ex vivo from human brain produced IL-17, GM-CSF, IFN -γ, and TNF-α, and the frequency increased to ∼80% after stimulation with the T cell mitogens, PMA, and ionomycin (Fig. 6, a and b; and Fig. S5 g). Potential direct influences of these cytokines on neurons was first assessed by examining neurons for the presence of receptors for IL-17 (IL-17R) and GM-CSF (GM-CSFR). >20% of neurons in naive C57BL/6 mice showed surface expression of IL-17R and GM-CSFR, as measured by flow cytometry (Fig. 6 c). This frequency was similar in mice deficient in voltage-gated sodium channel 1a (Scn1a-KO), which spontaneously develop epilepsy (Fig. 6 c; Miller et al., 2014). To determine the potential functional pathogenicity of these proinflammatory cytokines, we first compared latency to seizure onset and to the first general tonic-clonic (GTC) seizure in sex- and age-matched WT control and IL-17RA–deficient C57BL/6 mice. We chose receptor subunit A because it is by far the largest member of IL17 receptor family and is a common signaling subunit as part of the heterodimeric receptor used by multiple IL-17 ligands. IL-17RA KO mice displayed significantly delayed seizure onset (P < 0.0001) and first appearance of GTC (P = 0.025; Fig. 6 d), suggesting an important role for IL-17 in seizure induction. To directly assess the potential functional role of these cytokines in epileptogenesis, we tested whether IL-17 and GM-CSF directly altered neuronal excitability, consistent with their modification of seizure threshold, by measuring action potential generation in hippocampal CA1 pyramidal neurons in acute mouse brain slices after being exposed to PBS, recombinant IL-17, or GM-CSF for 4–11 h. The dose of cytokines used were previously titrated by us (Rodgers et al., 2015). Whole-cell current clamp recordings were performed after the incubation, and action potentials were measured in response to 500-ms injections of currents of varying amplitudes. Neurons recorded from IL-17 and GM-CSF–treated slices exhibited significantly enhanced excitability; we observed more spikes elicited by a range of current injections compared with the PBS control (repeated measures ANOVA; Fig. 6, e and f). Resting membrane potentials and input resistances were not different between the three treatment groups (not depicted). Longer exposures (>65 h) of neurons to recombinant IL-17 resulted in apoptosis as determined by annexin V staining using organotypic brain slices (Fig. 6, g and h). A 50-fold increase of neuronal apoptosis was observed when brain slices were treated with recombinant IL-17 compared with PBS. Such a frequency even exceeded those slices treated with IFN-γ and TNF-α, which served as a positive control. Collectively, the data indicate that exposure of neurons to IL-17 or GM-CSF in the context of other brain-resident glial cells resulted in hyperexcitability in the short term and compromised cell viability in an extended time period. These pathological effects of IL-17 and GM-CSF on neurons strongly support our findings that there is a positive correlation of γδ T cells, which actively produce IL-17 and GM-CSF, with seizure frequency in epileptogenic human brains (Fig. 3 e). Conversely, T reg cells that dampen immune response by suppressing the release of proinflammatory cytokines, such as IL-17 and GM-CSF, reduce neuronal excitability, consistent with the observed inverse correlation of T reg cell numbers with seizure frequency in epileptogenic human brains (Fig. 3 c).
Figure 6.
Effect of IL-17 and GM-CSF on neuronal excitability, viability, and seizure susceptibility. (a and b) Production of IL-17, GM-CSF, IFN-γ, and TNF-α by γδ T cells ex vivo from human brains in the absence (a) and presence (b) of PMA and ionomycin. (c) Surface expression of IL-17R and GM-CSFR by neurons from naive C57BL/6 (WT) and Scn1a-KO mice. Fluorescent-minus-one samples serve as negative controls (gray). (d) Seizure onset latency and first GTC latency measured in single-hit KA injected WT C57BL/6 versus IL-17RA KO mice. Data represent a total of nine mice of each strain pooled from three separate experiments. (e and f) Whole-cell current clamp recordings from hippocampal CA1 neurons in acute brain slices treated with PBS, IL-17, or GM-CSF for 4–11 h. Voltage responses were measured while injecting currents that changed in amplitude in 25 pA increments from −200 to 200 pA. P-values were calculated using repeated measures ANOVA. The number of recordings were 8 (control), 9 (GM-CSF), and 11 (IL-17). Four mice were used per group. Data are represented as means ± SEM. (g and h) Dot plots (g) and histograms (h) of Annexin V staining on neurons expressing psd95 in organotypic brain slices treated with PBS, IFN-γ/TNF-α, or IL-17 for 65 h. Data represent slices pooled from 10 mice. Two independent repeats were performed. Data are represented as means ± SD. P-values calculated using Student’s t test. *, P < 0.05; ** P < 0.01; ***, P < 0.001. Numbers in the flow plots indicate the frequencies of positive cell populations.
Discussion
Children 5 yr or younger have the highest incidence of epilepsy (Shinnar and Pellock, 2002; Raspall-Chaure et al., 2007). Up to 40% of children with epilepsy continue to have seizures despite treatment with anticonvulsants, which target symptoms without addressing the underlying pathophysiology (Xu et al., 2013). Using a flow cytometric approach to define inflammatory populations in resected brain tissues from pediatric patients diagnosed with EM and FCD, the most common cause of drug-resistant childhood epilepsy (Kabat and Król, 2012), we demonstrate the presence of significant numbers of activated myeloid cells, antigen-experienced CD8+ and CD4+ T cells, γδ T cells, and T reg cells. Importantly, a positive correlation with clinical seizure frequency was established for brain-infiltrating myeloid APCs and T cells, but not for activated microglia, which have historically been considered the main drivers of epileptogenic inflammation (Devinsky et al., 2013). Uniquely, we also show that disease severity correlates with the numbers of infiltrating γδ T cells, supported by our demonstration of significantly less seizure activity in γδ T cell–deficient mice in the KA-SE model. Additionally, we show the numbers of brain-infiltrating T reg cells inversely correlate with seizure burden in children with intractable epilepsy, supported by the amelioration of seizures by T reg cell transfer in the two-hit KA-SE model.
The presence of perivascular CD8+ T cells in the dysplastic brain region of type II FCD patients has been previously described using IHC staining (Iyer et al., 2010). 85% of our FCD cases were also type II, but our data suggest that the majority of leukocytes are in the epileptogenic brain parenchyma. The enrichment of CD8+ T cells in the brain and their memory phenotype may have a critical impact on neurons and oligodendrocytes. As is shown in Fig. 4 (a and b), neurons and oligodendrocytes express various levels of MHC class I and class II, potentially making them vulnerable for attack by activated CD8+ and CD4+ T cells. Neurons do not normally express MHC molecules. However, under inflammatory conditions, we and others have detected expression of MHC class I/II by neurons (Neumann et al., 1995), making them a possible target for T cell recognition. We found that the T cells detected in the epilepsy brain are mostly memory cells, which do not require costimulatory molecules for reactivation (Harris and Ronchese, 1999). Thus, neurons are potentially vulnerable targets of memory T cells irrespective of the expression of costimulatory molecules. This finding suggests the possibility that neuronal expression of MHC II may be partially responsible for the pathogenesis of epilepsy, but further studies are required to make definitive conclusions.
At least three findings indicate a lack of blood contamination for the brain samples. First, <1% of leukocytes isolated from the resected brains are neutrophils (Fig. S1), which normally comprise 40∼60% of PBMC. Second, the inverse CD8+/CD4+ T cell ratio in the brain compared with the blood argues strongly against contamination of circulating leukocytes (Fig. S3 c). Third, the vast majority (∼85%) of the brain-isolated CD4+ and CD8+ T cells were antigen-experienced cells, in contrast to <10% in the blood. Failure to detect brain parenchymal immune-cell infiltration in other studies may be a result of the heterogeneous adult-dominant subject pool, as opposed to pediatric subjects examined in our study.
Seizure frequency in pediatric patients positively correlated with the numbers of activated CD3+ T cells and blood-borne myeloid cells, but not activated microglia, in the epileptogenic lesions. This is in stark contrast to previous studies (Boer et al., 2006; Amhaoul et al., 2015). This discrepancy may be attributed to the age of patient cohorts and methods used to analyze immune cells in the brain. The mean ages of patients in Iyer et al. (2010) were 27.8 (FCD1) and 26.2 yr age of (FCD2), whereas our subjects had a mean onset of 3.8 and 8.7 yr of age at the time of surgery. This may significantly impact the immune profile in the brain. Additionally, other studies mostly used formalin-fixed and paraffin-embedded tissue for IHC to detect CD3+ T cells and APC subtypes. IHC using paraffin-embedded tissues are very insensitive compared with multicolor flow cytometry analysis on fresh brain samples, which we used. The correlation reported for activated microglia in previous studies used CD68 and HLA-DR by IHC to identify microglia. It is well accepted that CD68 by IHC cannot discriminate between microglia and brain-infiltrating APCs, especially after activation in an inflamed brain. Therefore, the correlation reported by others was likely contributed by peripherally derived APCs in the epileptogenic focus, supporting our findings using flow cytometry, which clearly distinguish microglia from infiltrating monocytes/macrophages. Therefore, we hypothesize that the timing of immune phenotyping relative to the epilepsy development and the detection method used are critical in deciphering the role of peripheral immune cells at difference stages of epileptogenesis. We suggest that similar flow analysis should be performed on adult patients with the same etiologies and severe pharmacoresistant seizures to compare and confirm this phenomenon observed in pediatric cohorts.
Infiltration of the brain parenchyma by peripheral immune cells may occur secondary to BBB breakdown, a known hallmark of epilepsy (Oby and Janigro, 2006). Indeed, protection of BBB integrity diminishes seizure occurrence (Fabene et al., 2008). It is also possible that activated leukocytes expressing VLA-4 and LFA-1 integrins may cross the intact BBB (Fig. S3 d; Male et al., 1994; Greenwood et al., 1995). Blockade of leukocyte adhesion to the BBB reduces seizure severity and chronic recurrence (Fabene et al., 2008). However, the use of FDA-approved drugs (e.g., Tysabri [Yaldizli and Putzki, 2009; Planas et al., 2014] or Gilenya [Kappos et al., 2015]) to prevent leukocyte transmigration into the brain as potential therapies for childhood epilepsy are problematic because of potential severe side effects. If these CNS-infiltrating T cells prove to be autoreactive, specific tolerance immunotherapy for epilepsy may prove useful in the future.
nT reg cells comprise ∼5–10% of the circulating CD4+ T cells and play crucial roles in the maintenance of immunological self-tolerance and regulation of immune responses (Sakaguchi et al., 2007; Sojka et al., 2008; Schmidt et al., 2012). T reg cell numbers inversely correlated with seizure severity in pediatric epilepsy patients. Highlighting the potential clinical significance of our findings, we show that supplementation of nT reg cells in the KA-SE mouse model significantly ameliorates seizure susceptibility, whereas inactivating/depleting T reg cells with either anti-CD25 antibodies (Kohm et al., 2006; Setiady et al., 2010) or DT injection (Kim et al., 2007) heightens seizure severity. These results indicate that infiltration of certain immune cell subsets in epilepsy may be protective/regenerative rather than destructive. The efficacy of T reg cell infusion has been well established by our laboratory and others in several mouse models of autoimmune diseases, as well as clinical trials of autoimmune diseases and lymphoma. After T reg cell infusion, we detected an increase of T reg cells both in the periphery and the brain (unpublished data). Such an increase of T reg cells is accompanied by a reduction of T effectors (T eff) cells in the brain, consistent with our hypothesis that T reg cells regulate the trafficking pattern and function of T eff cells, thereby affecting brain inflammation and seizure severity. The dose and efficacy of anti–mouse CD25 antibody infusion has been reported by our group and others in several mouse models of autoimmune disease to deplete or inactivate the T reg cell population without activating CD4+Foxp3− effector cells. It is possible, although unlikely, that the anti-CD25 treatment could affect recently activated effector T cells. However, the shortened seizure latency and prolonged duration of seizures after the treatment suggested that the antibody mostly affected T reg cells. In addition, the T reg cell depletion data using DTR-FoxP3-GFP transgenic mice supports the conclusion that the enhanced clinical symptoms of epilepsy after anti-CD25 treatment is likely a result of T reg cell depletion. T reg cells highly express CD25 to scavenge IL-2, thereby restricting its availability to T eff cells. Therefore, at the dose we used, the anti-CD25 mainly impacts T reg cells rather than other T eff cells (Kohm et al., 2006). It is worth pointing out that the clone of anti-CD25 that we used here does not deplete CD4+FoxP3+CD25+ T reg cells, but instead functionally inactivates T reg cells by down-regulating CD25 for a period of 7–10 d (Kohm et al., 2006). Previous studies examining patient samples reported detection of CD3+ T cells and macrophages in the brain by IHC staining without characterizing their cellular subtypes. CD3+ T reg cells and M2 macrophages can have reparative functions in the brain (Gensel and Zhang, 2015; Hu et al., 2015). Our preliminary finding that treatment with T reg cells immediately after acute seizure in the KA-SE model boosted the number of CD206 expressing M2 macrophages in the brain (unpublished data) supports a potential protective/regenerative role of immune regulatory cells.
Our finding of a positive correlation of increased frequencies of γδ T cells with clinical seizure severity is the first description of these cells within pediatric populations with FCD and EM. Brain-infiltrating γδ T cells were recently described by another group in RE (Owens et al., 2015). γδ T cells are known to respond to stress-induced self-proteins, such as heat shock proteins and lipid moieties bound to CD1 (Born et al., 2013; Chien et al., 2014). It is conceivable that they are activated after stress or triggered by alarm signals up-regulated in the epileptogenic brain (Vezzani et al., 2013). Unlike αβ T cells, γδ T cells are not dependent on antigen presentation by classical MHC molecules, rendering neurons, which normally do not express MHC molecules, a potential target. Upon activation, they secrete a broad spectrum of proinflammatory cytokines (e.g., IL-17 and GM-CSF), which we show for the first time contribute to neuronal excitability, dysfunction, and death. It is possible that these cytokines can also be released by cells other than immune cells, for instance, brain endothelial cells, dysmorphic neurons, glia, and endothelial cells of blood vessels in human malformations of cortical development including FCD (He et al., 2013a), and the excitotoxic effect of GM-CSF and IL-17 could be indirect through glia (Trajkovic et al., 2001). Nevertheless, the level of these cytokine produced by infiltrating γδ T cells measured directly ex vivo using fresh patient samples is strong and consistent for all diagnoses tested, suggesting an important pathogenic contribution of γδ T cells. The direct effect of IL-17 and GM-CSF on neuronal hyperexcitability and viability strongly support the finding of a positive correlation of γδ T cells producing proinflammatory cytokines with seizure frequency in epileptogenic human brains (Fig. 3 e). Consistent with an immunopathogenic role of γδ T cells in epileptogenesis, we show that γδ T cell–deficient mice display significantly less seizure activity in the KA-SE model. Significantly, the numbers of T reg cells that dampen immune response by suppressing the release of proinflammatory cytokines, such as IL-17 and GM-CSF, inversely correlated with seizure frequency in epileptogenic human brains (Fig. 3 c).
Previously, increased serum IL-17A levels were reported in adult epilepsy patients with mixed etiology during the interictal phase compared with healthy controls and elevated levels in the CSF postictally compared with the interictal phase (Mao et al., 2013; Wang et al., 2015). Elevated IL-17A, measured by histology and Western blot, was also found in the brain of an adult cohort diagnosed with MTLE (He et al., 2016). More relevant to our study, a cohort of pediatric patients with intractable epilepsy, including tuberous sclerosis complex and FCD, was also reported to express increased IL-17 levels in the brain (He et al., 2013a,b). Interestingly, up-regulated serum levels of IL-17 were reduced after ketogenic diet, which partially controlled seizures in some pediatric patients with intractable epilepsy. A concomitant increase of circulating T reg cells in the blood was noted in these patients, suggesting a balance between Th17 and T reg cell cells in the regulation of seizure (Ni et al., 2016). To our knowledge, there have been no studies that provide an association of GM-CSF with epilepsy. Collectively, these findings strongly suggest the potential of repurposing for the treatment of epilepsy existing antiinflammatory strategies, such as GM-CSF receptor antagonistic monoclonal antibodies to specifically block GM-CSF signaling (Ifergan et al., 2017) and IL-12/23p40–neutralizing antibodies (ustekinumab), found useful for the treatment of autoimmune CNS disease (Segal et al., 2008). The influence of these antibodies on the activation and trafficking of peripherally derived immune cells can prevent their infiltration into the brain, circumventing the necessity of penetrating the BBB to achieve efficacy. Additionally, we have used a novel immunoregulatory therapy using biodegradable PLG nanoparticles to restrict peripheral inflammatory monocytes from entering the CNS (Getts et al., 2014) and have preliminarily shown efficacy in both acute and chronic models of epilepsy (unpublished data). Although it is nearly impossible to definitively ascribe a causal relationship of inflammation with seizures in epilepsy patients, our data showing the ability of IL-17 and GM-CSF to trigger hyperexcitability of neurons in brain slices importantly supports the possibility that inflammation can cause seizures. We thus conclude that inflammation plays a critical role in epileptogenesis regardless of whether it is a cause or consequence. Our data also indicate that modulating inflammation could lessen seizure severity. Thus, targeting a specific subset of immune cells may present a potential target for a novel epilepsy therapy.
Based on the array of proinflammatory leukocytes identified in epileptogenic lesions, there are multiple potential mechanisms of immune-mediated neuronal loss and glial damage. Recent studies have described the presence of damaged oligodendrocytes and myelinated fibers in patients with TLE (Rodríguez-Cruces and Concha, 2015); however, the consequence of these effects on the pathogenesis of epilepsy is uncertain. A unique preliminary finding is our demonstration of immune-mediated death of oligodendrocytes and potential effects of brain-infiltrating myeloid and NK cells on OPC development. Migrating and early OPCs were at significantly lower frequencies than later stage oligodendrocytes in patients expressing the highest levels of MHC on oligodendrocyte lineage cells, perhaps suggesting that OPCs are pushed to differentiate in the epileptogenic center where oligodendrocyte loss is prominent.
In summary, our unbiased flow cytometric approach interrogating the number, phenotype, and activation state of both peripherally derived and brain-resident inflammatory cells in the epileptogenic brain supports a potential pathological role for peripherally derived innate and adaptive immune responses in pediatric epilepsy. Demonstration of αβ, γδ T cells, and T reg cells in the brain parenchyma of FCD and EM patients provides unique insight into the potential role of these autoreactive effector and immunoregulatory responses in neuronal hyperexcitability, viability, and the process of epileptogenesis. We are currently investigating the mechanistic basis of multiple immunomodulatory therapies in murine epilepsy models. Results from these studies will likely contribute to the identification of new biomarkers useful for disease prognosis and to the development of novel therapeutics.
Materials and methods
Human subjects
33 children (RE 1 and 2, MTLE 3 and 4, EM 5–14, and FCD 15–33) with chronic intractable epilepsy who underwent resective brain surgery from January 2010 to August 2015 were recruited from the Epilepsy Center at Ann & Robert H. Lurie Children’s Hospital of Chicago (Table S1). Preoperation and follow-up visits were conducted at the same location. Extensive presurgical evaluation included video EEG monitoring, brain magnetic resonance imaging (3 Tesla), fluorodeoxyglucose-positron emission tomography imaging, functional magnetic resonance imaging, and intraoperative corticography.
Preparation of fresh brain samples for flow cytometric analysis
Freshly dissected brain tissues were immediately washed with cold PBS, dissociated from loosely attached blood vessels, weighed, and minced with razor blades. At least 5 ml Accutase (Millipore) was added to 1 g of brain and incubated for a 1 h at 37°C before being passed through 100-µm cell strainers using syringe plungers in 30 ml RMPI 1640 with 10% fetal calf serum. To purify single cell suspensions devoid of myelin debris, cells were then washed once with PBS, resuspended in 30% Percoll, and centrifuged in 30% over 70% Percoll gradients at 650 g without brake for 25 min at room temperature. The interface containing cells was aspirated, washed once in RMPI 1640 with 10% fetal calf serum, and counted on hemocytometers in the presence of 4% trypan blue. Half of the cells were then stained for flow cytometric analyses, and the other half were cultured with GolgiStop and GolgiPlug (BD Biosciences) for 8 h at 37°C in preparation for intracellular cytokine staining.
Flow cytometry
Cells were incubated with human or mouse Fc-block (564220 and 553142, respectively; BD Biosciences) followed by appropriate antibody cocktails. Live/dead fixable blue (L-23105; Invitrogen) was added to the cells thereafter to label dead cells before cell fixation with 1% formaldehyde diluted with PBS. Each incubation step was performed at 4°C for 30 min in the dark. Human antibodies used are listed below with the antigen, conjugated fluorophore, and catalog number specified. Antibodies were purchased from BD Biosciences (CD45 V500, 560777; CD3 V450, 560365; TCRγδ PE, 555717; HLA-ABC PE-Cy7, 561349; CD279 BV605, 563245; CD274 PE-Cy7, 558017; and CD25 V450, 560356), BioLegend (CD4 APC-Cy7, 317418; CD8 Alexa Fluor 700, 300920; CD11c PE-Cy7, 337216; CD45RO PerCP-Cy5.5, 304222; CD11a FITC, 301206; CD18 FITC, 302106; CD49d APC, 304308; CD29 APC, 303008; CD62L BV605, 304834; CD39 PE, 328208; CD14 Alexa Fluor 700, 301822; CD19 APC-Cy7, 302218; CD83 PerCP-Cy5.5, 305320; CD66b V450, 561649; CD80 APC, 305220; CD86 APC, 305412; HLA-DR FITC, 327006; HLA-DR BV421, 307636; CD120b APC, 350406; CD261 PE, 307206; CD95 PerCP-Cy5.5, 305630; CD11c BV605, 301636; CD56 PerCP-Cy5.5, 318322; CD39 FITC, 328206; CD253 BV421, 564243; CD178 PE, 306407; CD45RA APC, 304112; CD127 PE, 351304; CD197 PerCP-Cy5.5, 353220; CD45RA FITC, 304106; CD45RO APC, 304210; and CD45RO PerCP-Cy5.5, 304222), or eBiosciences (CD20 APC–Alexa Fluor 780, 47-0209). Mouse antibodies (anti-MOG APC-Cy7, MAB5680; EMD Millipore and anti GLAST APC, 130-095-814; Miltenyi Biotec) that cross react with human have previously been tested. Anti–human PSD95 FITC (ab150241), was purchased from Abcam. A six-laser Fortessa flow cytometer (BD Biosciences) was used to enumerate cell populations, and the data were analyzed using FlowJo software (TreeStar).
IHC staining
Paraformaldehyde-fixed 8-µm brain sections were blocked with 10% goat serum in 1× PBS for 30 min in a humid chamber at room temperature, followed by primary antibodies specific for CD8 (1:250 dilution, rabbit anti–human, clone SP16; Thermo Fisher Scientific) and TCRγδ (1:100 dilution, mouse anti–human, clone 5A6.E9; Thermo Fisher Scientific) in 3% goat serum overnight at 4°C. Secondary antibodies, goat anti–rabbit Cy3 (1:1,000 dilution, 111-165-144; Jackson ImmunoResearch) and goat anti–mouse Alexa Fluor 488 (1:1,000 dilution; 115-545-166; Jackson ImmunoResearch), were then incubated for 30 min at room temperature after washing the tissue sections seven times with 0.05% Tween. Tissue sections were then incubated with 1% Triton X-100 for 10 min at room temperature and mounted on coverslips with SlowFADE Diamond mounting media with DAPI (S36964; Invitrogen). All images were acquired on a laser-scanning confocal microscope (A1R; Nikon) and analyzed with NIS-Elements software (Nikon). Representative data were shown in Fig. 3 b from at least three individuals.
Animals, KA administration, semiology recording, and cell isolation
C57BL/6 female mice (age specified in the Results section for each experiment) used in this study were bred and housed under specific pathogen-free conditions in the barrier facility at Northwestern University Center for Comparative Medicine. The mice were housed at five or less per cage in a room with a 12 h light/dark cycle. γδ T cell KO breeder mice (B6.129P2-Tcrdtm1Mom/J; stock 002120) were purchased from Jackson Laboratory and bred in house for at least five generations. IL-17RA KO, FoxP3-DTR-eGFP transgenic, and Scn1atm1Kea (Scn1a-KO) mice were bred in house. The Northwestern University Institutional Animal Care and Use Committee approved all animal experiments. Two doses of KA (K-1013; A.G. Scientific) were injected intraperitoneally at 16 mg/kg in <100 µl sterile saline into C57BsL/6, γδ T cell KO mice, or IL-17RA KO mice at 0 and 1 h. Seizure semiology was recorded as follows during light cycle: forelimb clonic jerks, hindlimb clonic jerks, rearing/falling, general tonic clonic jerks, and status epilepticus. Seizure onset was scored as the first appearance of any of the motor seizures listed above. 7 d after seizure induction, mice were perfused with cold phosphate-buffered saline via cardiac puncture. Brain devoid of the olfactory bulb and cerebellum was harvested and digested with Accutase (Millipore) for 1 h at 37°C, triturated, and forced through a 100-µM cell strainer and centrifuged on a 30% over 70% Percoll gradient to enrich single cell suspension devoid of fat.
Supplementation and depletion of nT reg cells
On P28, two doses of KA as the first hit were injected intraperitoneally at 16 mg/kg in <100 µl sterile saline into C57BL/6 female mice (P28) at 0 and 1 h. In the nT reg cell supplementation study, 9.5 million CD4+CD25+FoxP3+ nT reg cells isolated from naive littermates using MACS cell separation column (Regulatory T Cell Isolation kit, 130-091-041; Miltenyi Biotec) or PBS as control were transferred into recipient mice via tail vein at 5 and 48 h after first dose of KA delivery. nT reg cell depletion was performed in two ways. First, anti-CD25 (0.5 mg/mouse, clone PC-61.5.3; BioXCell) or control IgG1 (HRPN, rat; BioXCell) antibodies were injected intraperitoneally into recipient or control mice on days 1, 3, and 7 after first dose of KA delivery. A second hit of KA was injected intraperitoneally into treatment and control mice P42 for both the supplementation and depletion experiments. Seizure semiology was similarly recorded as described above. Second, FoxP3-DTR-eGFP C57BL/6 mice were bred in house and were injected with KA intraperitoneally at P28, followed by two consecutive doses (0.25 µg per mouse in 250 µl PBS) of DT at P29 and P30. This dose of DT is sufficient to deplete >99% of FoxP3+ T reg cells, as previously reported (Kim et al., 2007). Mice were injected with a second hit of KA intraperitoneally at P33 to be monitored for seizure semiology using the Racine scale.
Organotypic cortical slice culture preparation
Slices were made using the interface culture method adapted from Kristensen et al. (1999). In brief, P10 C57BL/6 mice were euthanized by instant decapitation. Whole brain was quickly removed and coronally sectioned at 350 µm by a McIlwain tissue chopper (Mickle Laboratory) with the chopping blade prewetted using glucose-supplemented Gey’s balanced salt solution (GBSS; adding 1 ml 45% d-(+)-glucose solution [8769; Sigma-Aldrich] to 100 ml GBSS [G9779; Sigma-Aldrich]). The slices brain was placed in a 60-mm cell culture dish and soaked in chilled glucose-supplemented GBSS. The slices were separated and trimmed for excess tissue under a stereo microscope (VM VMZ 1–4× stereo microscope; Olympus) and immediately placed on a membrane insert (PICM0RG50; Millipore) in a 6-well tissue culture dish filled with 1 ml/well culture medium, consisting of 25% inactivated horse serum (26050070; Thermo Fisher Scientific), 25% HBSS (14170; Invitrogen), 50% Opti-MEM I Reduced Serum Medium (31985070; Thermo Fisher Scientific), and 1% d-(+)-glucose 45% solution. Cultures were maintained for 4 d in a humidified incubator with 5% CO2 at 36°C. Culture medium was replaced at 24 and 72 h after explanation. After 3 d, the culture was relocated to a humidified incubator with 5% CO2 at 33°C, and the culture was maintained in neurobasal medium (21103049; Thermo Fisher Scientific) supplemented with 1× B-27 (Thermo Fisher Scientific, Cat. 17504) and 1 mM l-glutamine (Thermo Fisher Scientific, Cat. 25030). The medium was replaced every 3 d until it was ready to use. During this period, the slices were examined by ordinary and phase-contrast microscopy every day to ensure that only cultures with intact structures were exposed to cytokines for further experimentation. For apoptosis assay, slices were cultured in either medium containing 100 ng/ml IL-17 or IFN-γ/TNF-α for 60 h before harvested for flow cytometric staining. Medium alone was used as negative control.
Hippocampal slice preparation
For electrophysiological recordings, acute hippocampal slices were prepared from juvenile (P21–P25) C57BL/6J mice of either sex, in accordance with Institutional Animal Care and Use Committee–approved protocols. In all of the comparative physiological studies, experimenters were blinded to pharmacological treatment until data analysis was completed. Mice were trans-cardially perfused with ice-cold, sucrose-rich slicing artificial cerebral spinal fluid (aCSF) containing 85 mM NaCl, 2.5 mM KCl, 1.25 mM NaH2PO4, 25 mM NaHCO3, 75 mM sucrose, 25 mM glucose, 10 µM DL-APV, 100 µM kynurenate, 0.5 mM Na l-ascorbate, 0.5 mM CaCl2, and 4 mM MgCl2, and oxygenated and equilibrated with 95% O2/5% CO2. After perfusion, mice were decapitated and brains were sliced in sucrose-aCSF. 350-µm horizontal slices preserving the ventral hippocampus were prepared using a vibratome (VT1200S; Leica Biosystems), warmed to 30°C in oxygenated sucrose-aCSF, and returned to room temperature. They were then transferred to oxygenated aCSF containing 125 mM NaCl, 2.4 mM KCl, 1.2 mM NaH2PO4, 25 mM NaHCO3, 25 mM glucose, 2 mM CaCl2, and 1 mM MgCl2, and maintained under these incubation conditions for at least 4 h before recording with 100 ng/ml IL-17, 100 ng/ml GM-CSF, or PBS (control). After incubation, individual slices were transferred to a recording chamber and continuously perfused with oxygenated aCSF at room temperature (25°C). Hippocampal CA1 pyramidal neurons were visually identified using a fixed-stage upright microscope (BX51WI; Olympus) and subsequently used for whole cell patch clamp recordings with a MultiClamp 700A amplifier (Molecular Devices).
Electrophysiological recordings
For cell-attached recordings, aCSF was used as the internal pipette solution. No additional drugs were applied in the external solution. The recording were done in I = 0 mode for >1 min. In current clamp recordings, a potassium gluconate internal solution containing 130 mM K-gluconate, 20 mM KCl, 1 mM K-Hepes, 0.2 mM EGTA, 0.3 mM Na-GTP, and 4 mM Mg-ATP, pH 7.3, was loaded into recording electrodes. After whole-cell break-in, CA1 neurons were equilibrated with the internal solution for 5 min and maintained in aCSF containing GABAA receptor antagonists bicuculline (10 µM) and picrotoxin (50 µM), the NMDA receptor antagonist d-APV (50 µM), and the AMPA and kainate receptor antagonist NBQX (10 µM). To record input–output relationships, membrane potential was held initially at −70 mV before injecting −200 to 200 pA current in 25-pA increments. Traces that contained action potentials were excluded. Recordings also were excluded if the pipette potential was less than −2.0 mV or larger than 0.5 mV or if the membrane capacitance was >70 pF. Inclusion criteria were applied to each dataset before the experimenter was unblinded. Analyses were performed with pClamp10 (Molecular Devices).
Statistics
GraphPad Prism 6 software was used for all statistical analyses. Statistical comparisons were made using Student’s two-tailed t test and the Pearson’s correlation coefficient was used to study the relationships between variables shown in scatterplots. Coefficient of determination (R2) was used to denote the strength of the linear association between the variables. We have included all the subjects, except those treated with steroid that may compromise immune readout, with data available for each subset of cells being interrogated in the correlation study. For the physiology data, a repeated measure ANOVA was used to compare the three experimental groups.
Study approval
Institutional review boards at Ann & Robert H. Lurie Children’s Hospital of Chicago approved this study. Informed consent was obtained for all subjects. All the animal procedures were approved by the Northwestern University Institutional Animal Care and Use Committee.
Online supplemental material
Fig. S1 shows the gating strategy for microglia and brain-infiltrating APCs. Fig. S2 shows the gating strategy for T cells. Fig. S3 shows the numbers of NK cells and B cells in epileptogenic lesions, the ratio of CD8+/CD4+ T cells in the epileptogenic center, and peripheral blood, as well as the visualization of integrin molecule expression by T cells in the epileptogenic center. Fig. S4 shows the gating strategy for brain-resident cells. Fig. S5 shows the cytokine profile of brain-infiltrating T cells. Table S1 shows the characteristics of clinical findings in patients used in this study.
Supplementary Material
Acknowledgments
We acknowledge S. Swaminathan, P. Mehl, and C. Ostiguin at Robert H. Lurie Comprehensive Cancer Center Flow Cytometry Core Facility for the assistance of data acquisition. We thank J. Rappoport and C. Arvanitis at Northwestern University Center for Advanced Microscopy for their support in data acquisition. We acknowledge the important contribution of the patients and their guardians who have donated resected brain and blood samples for our study. We thank Miller laboratory members for all the support and insightful comments.
This work was supported by National Institutes of Health grants R01 NS073768 and R21 NS094999 to S.D. Miller and S. Koh and Epilepsy Foundation fellowships 262243 to D. Xu and 1K22 AI118421 to P. Penaloza-MacMaster.
The authors declare no competing financial interests.
Author contributions: D. Xu designed research studies, conducted experiments, acquired data, analyzed data, and wrote the manuscript. A.P. Robinson, T. Ishii, and D.S. Duncan designed research studies, conducted experiments, acquired data. T.D. Alden provided patient samples. G.E. Goings conducted experiments and acquired data. I. Ifergan and J.R. Podojil designed research studies. J.A. Kearney and P. Penaloza-MacMaster provided reagents and mouse strains. G.T. Swanson, S.D. Miller, and S. Koh designed research studies and wrote the manuscript.
References
- Amhaoul H., Hamaide J., Bertoglio D., Reichel S.N., Verhaeghe J., Geerts E., Van Dam D., De Deyn P.P., Kumar-Singh S., Katsifis A., et al. . 2015. Brain inflammation in a chronic epilepsy model: Evolving pattern of the translocator protein during epileptogenesis. Neurobiol. Dis. 82:526–539. 10.1016/j.nbd.2015.09.004 [DOI] [PubMed] [Google Scholar]
- Atkins M.R., Terrell W., and Hulette C.M.. 1995. Rasmussen’s syndrome: a study of potential viral etiology. Clin. Neuropathol. 14:7–12. [PubMed] [Google Scholar]
- Banerjee P.N., Filippi D., and Allen Hauser W.. 2009. The descriptive epidemiology of epilepsy-a review. Epilepsy Res. 85:31–45. 10.1016/j.eplepsyres.2009.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett M.L., Bennett F.C., Liddelow S.A., Ajami B., Zamanian J.L., Fernhoff N.B., Mulinyawe S.B., Bohlen C.J., Adil A., Tucker A., et al. . 2016. New tools for studying microglia in the mouse and human CNS. Proc. Natl. Acad. Sci. USA. 113:E1738–E1746. 10.1073/pnas.1525528113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg A.T., and Kelly M.M.. 2006. Defining intractability: comparisons among published definitions. Epilepsia. 47:431–436. 10.1111/j.1528-1167.2006.00440.x [DOI] [PubMed] [Google Scholar]
- Berg A.T., and Rychlik K.. 2015. The course of childhood-onset epilepsy over the first two decades: a prospective, longitudinal study. Epilepsia. 56:40–48. 10.1111/epi.12862 [DOI] [PubMed] [Google Scholar]
- Bibolini M.J., Chanaday N.L., Báez N.S., Degano A.L., Monferran C.G., and Roth G.A.. 2011. Inhibitory role of diazepam on autoimmune inflammation in rats with experimental autoimmune encephalomyelitis. Neuroscience. 199:421–428. 10.1016/j.neuroscience.2011.08.076 [DOI] [PubMed] [Google Scholar]
- Bien C.G., Bauer J., Deckwerth T.L., Wiendl H., Deckert M., Wiestler O.D., Schramm J., Elger C.E., and Lassmann H.. 2002. Destruction of neurons by cytotoxic T cells: a new pathogenic mechanism in Rasmussen’s encephalitis. Ann. Neurol. 51:311–318. 10.1002/ana.10100 [DOI] [PubMed] [Google Scholar]
- Boer K., Spliet W.G., van Rijen P.C., Redeker S., Troost D., and Aronica E.. 2006. Evidence of activated microglia in focal cortical dysplasia. J. Neuroimmunol. 173:188–195. 10.1016/j.jneuroim.2006.01.002 [DOI] [PubMed] [Google Scholar]
- Born W.K., Kemal Aydintug M., and O’Brien R.L.. 2013. Diversity of γδ T-cell antigens. Cell. Mol. Immunol. 10:13–20. 10.1038/cmi.2012.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien Y.H., Meyer C., and Bonneville M.. 2014. γδ T cells: first line of defense and beyond. Annu. Rev. Immunol. 32:121–155. 10.1146/annurev-immunol-032713-120216 [DOI] [PubMed] [Google Scholar]
- Choi J., and Koh S.. 2008. Role of brain inflammation in epileptogenesis. Yonsei Med. J. 49:1–18. 10.3349/ymj.2008.49.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang Y.F., Yang H.Y., Ko T.L., Hsu Y.F., Sheu J.R., Ou G., and Hsu M.J.. 2014. Valproic acid suppresses lipopolysaccharide-induced cyclooxygenase-2 expression via MKP-1 in murine brain microvascular endothelial cells. Biochem. Pharmacol. 88:372–383. 10.1016/j.bcp.2014.02.004 [DOI] [PubMed] [Google Scholar]
- Chutorian A.M., Gold A.P., and Low N.L.. 1968. Steroid therapy of non-infantile (childhood) myoclonic epilepsy. Neurology. 18:304–305. [PubMed] [Google Scholar]
- Cobbold S.H.G., and Waldmann H.. 1987. Non-lineage, LFA-1 family, and leucocyte common antigens: New and previously defined clusters. In Leucocyte Typing III. White Cell Differentiation Antigens. Mc-Michael A.J., editor. Oxford University Press, Oxford: pp. 788–803. [Google Scholar]
- Devinsky O., Vezzani A., Najjar S., De Lanerolle N.C., and Rogawski M.A.. 2013. Glia and epilepsy: excitability and inflammation. Trends Neurosci. 36:174–184. 10.1016/j.tins.2012.11.008 [DOI] [PubMed] [Google Scholar]
- Dörr J., Bechmann I., Waiczies S., Aktas O., Walczak H., Krammer P.H., Nitsch R., and Zipp F.. 2002. Lack of tumor necrosis factor-related apoptosis-inducing ligand but presence of its receptors in the human brain. J. Neurosci. 22:RC209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta S., and Sengupta P.. 2016. Men and mice: Relating their ages. Life Sci. 152:244–248. 10.1016/j.lfs.2015.10.025 [DOI] [PubMed] [Google Scholar]
- Fabene P.F., Navarro Mora G., Martinello M., Rossi B., Merigo F., Ottoboni L., Bach S., Angiari S., Benati D., Chakir A., et al. . 2008. A role for leukocyte-endothelial adhesion mechanisms in epilepsy. Nat. Med. 14:1377–1383. 10.1038/nm.1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayatri N.A., Ferrie C.D., and Cross H.. 2007. Corticosteroids including ACTH for childhood epilepsy other than epileptic spasms. Cochrane Database Syst. Rev. CD005222 10.1002/14651858.CD005222.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gensel J.C., and Zhang B.. 2015. Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res. 1619:1–11. 10.1016/j.brainres.2014.12.045 [DOI] [PubMed] [Google Scholar]
- Getts D.R., Terry R.L., Getts M.T., Deffrasnes C., Müller M., van Vreden C., Ashhurst T.M., Chami B., McCarthy D., Wu H., et al. . 2014. Therapeutic inflammatory monocyte modulation using immune-modifying microparticles. Sci. Transl. Med. 6:219ra7 10.1126/scitranslmed.3007563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto Y., O’Malley C., Fanning N.F., Wang J., Redmond H.P., and Shorten G.D.. 2003. Benzodiazepines inhibit the rate of neutrophil apoptosis. Ir. J. Med. Sci. 172:191–194. 10.1007/BF02915288 [DOI] [PubMed] [Google Scholar]
- Greenwood J., Wang Y., and Calder V.L.. 1995. Lymphocyte adhesion and transendothelial migration in the central nervous system: the role of LFA-1, ICAM-1, VLA-4 and VCAM-1. off. Immunology. 86:408–415. [PMC free article] [PubMed] [Google Scholar]
- Grosso S., Farnetani M., Mostardini R., Cordelli D., Berardi R., and Balestri P.. 2008. A comparative study of hydrocortisone versus deflazacort in drug-resistant epilepsy of childhood. Epilepsy Res. 81:80–85. 10.1016/j.eplepsyres.2008.04.016 [DOI] [PubMed] [Google Scholar]
- Guerrini R. 2006. Epilepsy in children. Lancet. 367:499–524. 10.1016/S0140-6736(06)68182-8 [DOI] [PubMed] [Google Scholar]
- Hampson D.R., and Manalo J.L.. 1998. The activation of glutamate receptors by kainic acid and domoic acid. Nat. Toxins. 6:153–158. [DOI] [PubMed] [Google Scholar]
- Harris N.L., and Ronchese F.. 1999. The role of B7 costimulation in T-cell immunity. Immunol. Cell Biol. 77:304–311. 10.1046/j.1440-1711.1999.00835.x [DOI] [PubMed] [Google Scholar]
- Harvey A.S., Grattan-Smith J.D., Desmond P.M., Chow C.W., and Berkovic S.F.. 1995. Febrile seizures and hippocampal sclerosis: frequent and related findings in intractable temporal lobe epilepsy of childhood. Pediatr. Neurol. 12:201–206. 10.1016/0887-8994(95)00022-8 [DOI] [PubMed] [Google Scholar]
- Hauser W.A., Annegers J.F., and Rocca W.A.. 1996. Descriptive epidemiology of epilepsy: contributions of population-based studies from Rochester, Minnesota. Mayo Clin. Proc. 71:576–586. 10.4065/71.6.576 [DOI] [PubMed] [Google Scholar]
- He J.J., Li S., Shu H.F., Yu S.X., Liu S.Y., Yin Q., and Yang H.. 2013a The interleukin 17 system in cortical lesions in focal cortical dysplasias. J. Neuropathol. Exp. Neurol. 72:152–163. 10.1097/NEN.0b013e318281262e [DOI] [PubMed] [Google Scholar]
- He J.J., Wu K.F., Li S., Shu H.F., Zhang C.Q., Liu S.Y., Yang M.H., Yin Q., and Yang H.. 2013b Expression of the interleukin 17 in cortical tubers of the tuberous sclerosis complex. J. Neuroimmunol. 262:85–91. 10.1016/j.jneuroim.2013.05.007 [DOI] [PubMed] [Google Scholar]
- He J.J., Sun F.J., Wang Y., Luo X.Q., Lei P., Zhou J., Zhu D., Li Z.Y., and Yang H.. 2016. Increased expression of interleukin 17 in the cortex and hippocampus from patients with mesial temporal lobe epilepsy. J. Neuroimmunol. 298:153–159. 10.1016/j.jneuroim.2016.07.017 [DOI] [PubMed] [Google Scholar]
- Hoffmann K., Lindner M., Gröticke I., Stangel M., and Löscher W.. 2008. Epileptic seizures and hippocampal damage after cuprizone-induced demyelination in C57BL/6 mice. Exp. Neurol. 210:308–321. 10.1016/j.expneurol.2007.11.005 [DOI] [PubMed] [Google Scholar]
- Hövelmeyer N., Hao Z., Kranidioti K., Kassiotis G., Buch T., Frommer F., von Hoch L., Kramer D., Minichiello L., Kollias G., et al. . 2005. Apoptosis of oligodendrocytes via Fas and TNF-R1 is a key event in the induction of experimental autoimmune encephalomyelitis. J. Immunol. 175:5875–5884. 10.4049/jimmunol.175.9.5875 [DOI] [PubMed] [Google Scholar]
- Hu X., Leak R.K., Shi Y., Suenaga J., Gao Y., Zheng P., and Chen J.. 2015. Microglial and macrophage polarization—new prospects for brain repair. Nat. Rev. Neurol. 11:56–64. 10.1038/nrneurol.2014.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ifergan I., Davidson T.S., Kebir H., Xu D., Palacios-Macapagal D., Cann J., Rodgers J.M., Hunter Z.N., Pittet C.L., Beddow S., et al. . 2017. Targeting the GM-CSF receptor for the treatment of CNS autoimmunity. J. Autoimmun. 84:1–11. 10.1016/j.jaut.2017.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer A., Zurolo E., Spliet W.G., van Rijen P.C., Baayen J.C., Gorter J.A., and Aronica E.. 2010. Evaluation of the innate and adaptive immunity in type I and type II focal cortical dysplasias. Epilepsia. 51:1763–1773. 10.1111/j.1528-1167.2010.02547.x [DOI] [PubMed] [Google Scholar]
- Kabat J., and Król P.. 2012. Focal cortical dysplasia - review. Pol. J. Radiol. 77:35–43. 10.12659/PJR.882968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kappos L., O’Connor P., Radue E.W., Polman C., Hohlfeld R., Selmaj K., Ritter S., Schlosshauer R., von Rosenstiel P., Zhang-Auberson L., and Francis G.. 2015. Long-term effects of fingolimod in multiple sclerosis: the randomized FREEDOMS extension trial. Neurology. 84:1582–1591. 10.1212/WNL.0000000000001462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim I., Mlsna L.M., Yoon S., Le B., Yu S., Xu D., and Koh S.. 2015. A postnatal peak in microglial development in the mouse hippocampus is correlated with heightened sensitivity to seizure triggers. Brain Behav. 5:e00403 10.1002/brb3.403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.M., Rasmussen J.P., and Rudensky A.Y.. 2007. Regulatory T cells prevent catastrophic autoimmunity throughout the lifespan of mice. Nat. Immunol. 8:191–197. 10.1038/ni1428 [DOI] [PubMed] [Google Scholar]
- Koh S., Storey T.W., Santos T.C., Mian A.Y., and Cole A.J.. 1999. Early-life seizures in rats increase susceptibility to seizure-induced brain injury in adulthood. Neurology. 53:915–921. 10.1212/WNL.53.5.915 [DOI] [PubMed] [Google Scholar]
- Kohm A.P., McMahon J.S., Podojil J.R., Begolka W.S., DeGutes M., Kasprowicz D.J., Ziegler S.F., and Miller S.D.. 2006. Cutting Edge: Anti-CD25 monoclonal antibody injection results in the functional inactivation, not depletion, of CD4+CD25+ T regulatory cells. J. Immunol. 176:3301–3305. 10.4049/jimmunol.176.6.3301 [DOI] [PubMed] [Google Scholar]
- Kristensen B.W., Noraberg J., Jakobsen B., Gramsbergen J.B., Ebert B., and Zimmer J.. 1999. Excitotoxic effects of non-NMDA receptor agonists in organotypic corticostriatal slice cultures. Brain Res. 841:143–159. 10.1016/S0006-8993(99)01833-8 [DOI] [PubMed] [Google Scholar]
- Kwan P., and Brodie M.J.. 2000. Early identification of refractory epilepsy. N. Engl. J. Med. 342:314–319. 10.1056/NEJM200002033420503 [DOI] [PubMed] [Google Scholar]
- Kwan P., and Sperling M.R.. 2009. Refractory seizures: try additional antiepileptic drugs (after two have failed) or go directly to early surgery evaluation? Epilepsia. 50(Suppl 8):57–62. 10.1111/j.1528-1167.2009.02237.x [DOI] [PubMed] [Google Scholar]
- Kwan P., Arzimanoglou A., Berg A.T., Brodie M.J., Allen Hauser W., Mathern G., Moshé S.L., Perucca E., Wiebe S., and French J.. 2010. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 51:1069–1077. 10.1111/j.1528-1167.2009.02397.x [DOI] [PubMed] [Google Scholar]
- Libenson M.H., Stafstrom C.E., and Rosman N.P.. 1994. Tonic “seizures” in a patient with brainstem demyelination: MRI study of brain and spinal cord. Pediatr. Neurol. 11:258–262. 10.1016/0887-8994(94)90114-7 [DOI] [PubMed] [Google Scholar]
- Male D., Rahman J., Pryce G., Tamatani T., and Miyasaka M.. 1994. Lymphocyte migration into the CNS modelled in vitro: roles of LFA-1, ICAM-1 and VLA-4. Immunology. 81:366–372. [PMC free article] [PubMed] [Google Scholar]
- Mao L.Y., Ding J., Peng W.F., Ma Y., Zhang Y.H., Fan W., and Wang X.. 2013. Interictal interleukin-17A levels are elevated and correlate with seizure severity of epilepsy patients. Epilepsia. 54:e142–e145. 10.1111/epi.12337 [DOI] [PubMed] [Google Scholar]
- Martin-Villalba A., Hahne M., Kleber S., Vogel J., Falk W., Schenkel J., and Krammer P.H.. 2001. Therapeutic neutralization of CD95-ligand and TNF attenuates brain damage in stroke. Cell Death Differ. 8:679–686. 10.1038/sj.cdd.4400882 [DOI] [PubMed] [Google Scholar]
- McMahon E.J., Bailey S.L., Castenada C.V., Waldner H., and Miller S.D.. 2005. Epitope spreading initiates in the CNS in two mouse models of multiple sclerosis. Nat. Med. 11:335–339. 10.1038/nm1202 [DOI] [PubMed] [Google Scholar]
- Miller A.R., Hawkins N.A., McCollom C.E., and Kearney J.A.. 2014. Mapping genetic modifiers of survival in a mouse model of Dravet syndrome. Genes Brain Behav. 13:163–172. 10.1111/gbb.12099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison R.S., Kinoshita Y., Johnson M.D., Ghatan S., Ho J.T., and Garden G.. 2003. Neuronal survival and cell death signaling pathways. Adv. Exp. Med. Biol. 513:41–86. 10.1007/978-1-4615-0123-7_2 [DOI] [PubMed] [Google Scholar]
- Nelson W.E., Kliegman R., and Nelson W.E.. 2011. Nelson textbook of pediatrics. Elsevier, Philadelphia. 2610 pp. [Google Scholar]
- Neumann H., Cavalié A., Jenne D.E., and Wekerle H.. 1995. Induction of MHC class I genes in neurons. Science. 269:549–552. 10.1126/science.7624779 [DOI] [PubMed] [Google Scholar]
- Ni F.F., Li C.R., Liao J.X., Wang G.B., Lin S.F., Xia Y., and Wen J.L.. 2016. The effects of ketogenic diet on the Th17/Treg cells imbalance in patients with intractable childhood epilepsy. Seizure. 38:17–22. 10.1016/j.seizure.2016.03.006 [DOI] [PubMed] [Google Scholar]
- Oby E., and Janigro D.. 2006. The blood-brain barrier and epilepsy. Epilepsia. 47:1761–1774. 10.1111/j.1528-1167.2006.00817.x [DOI] [PubMed] [Google Scholar]
- Owens G.C., Erickson K.L., Malone C.C., Pan C., Huynh M.N., Chang J.W., Chirwa T., Vinters H.V., Mathern G.W., and Kruse C.A.. 2015. Evidence for the involvement of gamma delta T cells in the immune response in Rasmussen encephalitis. J. Neuroinflammation. 12:134 10.1186/s12974-015-0352-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planas R., Martin R., and Sospedra M.. 2014. Long-term safety and efficacy of natalizumab in relapsing-remitting multiple sclerosis: impact on quality of life. Patient Relat. Outcome Meas. 5:25–33. 10.2147/PROM.S41768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raspall-Chaure M., Chin R.F.M., Neville B.G., Bedford H., and Scott R.C.. 2007. The epidemiology of convulsive status epilepticus in children: a critical review. Epilepsia. 48:1652–1663. 10.1111/j.1528-1167.2007.01175.x [DOI] [PubMed] [Google Scholar]
- Rodgers J.M., Robinson A.P., Rosler E.S., Lariosa-Willingham K., Persons R.E., Dugas J.C., and Miller S.D.. 2015. IL-17A activates ERK1/2 and enhances differentiation of oligodendrocyte progenitor cells. Glia. 63:768–779. 10.1002/glia.22783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Cruces R., and Concha L.. 2015. White matter in temporal lobe epilepsy: clinico-pathological correlates of water diffusion abnormalities. Quant. Imaging Med. Surg. 5:264–278. 10.3978/j.issn.2223-4292.2015.02.0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers S.W., Andrews P.I., Gahring L.C., Whisenand T., Cauley K., Crain B., Hughes T.E., Heinemann S.F., and McNamara J.O.. 1994. Autoantibodies to glutamate receptor GluR3 in Rasmussen’s encephalitis. Science. 265:648–651. 10.1126/science.8036512 [DOI] [PubMed] [Google Scholar]
- Sagar H.J., and Oxbury J.M.. 1987. Hippocampal neuron loss in temporal lobe epilepsy: correlation with early childhood convulsions. Ann. Neurol. 22:334–340. 10.1002/ana.410220309 [DOI] [PubMed] [Google Scholar]
- Sakaguchi S., Wing K., and Miyara M.. 2007. Regulatory T cells - a brief history and perspective. Eur. J. Immunol. 37(S1, Suppl 1):S116–S123. 10.1002/eji.200737593 [DOI] [PubMed] [Google Scholar]
- Satoh J., Kino Y., Asahina N., Takitani M., Miyoshi J., Ishida T., and Saito Y.. 2016. TMEM119 marks a subset of microglia in the human brain. Neuropathology. 36:39–49. 10.1111/neup.12235 [DOI] [PubMed] [Google Scholar]
- Schmidt A., Oberle N., and Krammer P.H.. 2012. Molecular mechanisms of treg-mediated T cell suppression. Front. Immunol. 3:51 10.3389/fimmu.2012.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal B.M., Constantinescu C.S., Raychaudhuri A., Kim L., Fidelus-Gort R., and Kasper L.H.. Ustekinumab MS Investigators . 2008. Repeated subcutaneous injections of IL12/23 p40 neutralising antibody, ustekinumab, in patients with relapsing-remitting multiple sclerosis: a phase II, double-blind, placebo-controlled, randomised, dose-ranging study. Lancet Neurol. 7:796–804. 10.1016/S1474-4422(08)70173-X [DOI] [PubMed] [Google Scholar]
- Setiady Y.Y., Coccia J.A., and Park P.U.. 2010. In vivo depletion of CD4+FOXP3+ Treg cells by the PC61 anti-CD25 monoclonal antibody is mediated by FcgammaRIII+ phagocytes. Eur. J. Immunol. 40:780–786. 10.1002/eji.200939613 [DOI] [PubMed] [Google Scholar]
- Shinnar S., and Pellock J.M.. 2002. Update on the epidemiology and prognosis of pediatric epilepsy. J. Child Neurol. 17(1_suppl, Suppl 1):S4–S17. 10.1177/08830738020170010201 [DOI] [PubMed] [Google Scholar]
- Sojka D.K., Huang Y.H., and Fowell D.J.. 2008. Mechanisms of regulatory T-cell suppression - a diverse arsenal for a moving target. Immunology. 124:13–22. 10.1111/j.1365-2567.2008.02813.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Téllez-Zenteno J.F., Dhar R., and Wiebe S.. 2005. Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain. 128:1188–1198. 10.1093/brain/awh449 [DOI] [PubMed] [Google Scholar]
- Totolian N.A., Borisova E.V., Totolian A.A., Miliukhina I.V., Lapin S.V., Kodzaeva A.Iu., Prakhova L.N., Evdoshenko E.P., Kairbekova E.I., and Skoromets A.A.. 2011. [Symptomatic epilepsy in inflammatory demyelinating diseases]. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova. 111:38–51. [PubMed] [Google Scholar]
- Trajkovic V., Markovic M., Samardzic T., Miljkovic D.J., Popadic D., and Mostarica Stojkovic M.. 2001. Amphotericin B potentiates the activation of inducible nitric oxide synthase and causes nitric oxide-dependent mitochondrial dysfunction in cytokine-treated rodent astrocytes. Glia. 35:180–188. 10.1002/glia.1083 [DOI] [PubMed] [Google Scholar]
- Varadkar S., Bien C.G., Kruse C.A., Jensen F.E., Bauer J., Pardo C.A., Vincent A., Mathern G.W., and Cross J.H.. 2014. Rasmussen’s encephalitis: clinical features, pathobiology, and treatment advances. Lancet Neurol. 13:195–205. 10.1016/S1474-4422(13)70260-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A. 2014. Epilepsy and inflammation in the brain: overview and pathophysiology. Epilepsy Curr. 14(s2, Suppl):3–7. 10.5698/1535-7511-14.s2.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A., French J., Bartfai T., and Baram T.Z.. 2011. The role of inflammation in epilepsy. Nat. Rev. Neurol. 7:31–40. 10.1038/nrneurol.2010.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A., Aronica E., Mazarati A., and Pittman Q.J.. 2013. Epilepsy and brain inflammation. Exp. Neurol. 244:11–21. 10.1016/j.expneurol.2011.09.033 [DOI] [PubMed] [Google Scholar]
- Walker L., and Sills G.J.. 2012. Inflammation and epilepsy: the foundations for a new therapeutic approach in epilepsy? Epilepsy Curr. 12:8–12. 10.5698/1535-7511-12.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Wang D., and Guo D.. 2015. Interictal cytokine levels were correlated to seizure severity of epileptic patients: a retrospective study on 1218 epileptic patients. J. Transl. Med. 13:378 10.1186/s12967-015-0742-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu D., Miller S.D., and Koh S.. 2013. Immune mechanisms in epileptogenesis. Front. Cell. Neurosci. 7:195 10.3389/fncel.2013.00195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaldizli O., and Putzki N.. 2009. Natalizumab in the treatment of multiple sclerosis. Ther. Adv. Neurol. Disorder. 2:115–128. 10.1177/1756285608101861 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.