Abstract
Purpose of the Study:
This study determined whether self-reports of unmet need for help with activities of daily living (ADL) disabilities are prognostic of emergency department (ED) utilization.
Design and Methods:
This prospective cohort study of 2,194 community-living, ADL-disabled subjects combined 2004 National Long-Term Care Survey responses with linked Medicare data through 2005. A negative binomial count model was computed to assess the association between unmet ADL need and number of subsequent ED admissions while statistically adjusting for predisposing, enabling, and need characteristics associated with ED admissions among older adults.
Results:
The adjusted annual incidence rate (IR) for ED admissions was 19% higher for unmet versus met need (IR = 1.19; 95% confidence interval [CI] = 1.00–1.40; p = .047). The IR for ED admissions for falls and injuries was higher for those with unmet ADL versus met ADL need (IR = 1.43; 95% CI = 1.10–1.86), and trended toward significance for ED admissions for skin breakdown (IR = 2.02; 95% CI = 0.97–2.88), but was not significant for ED admissions for dehydration (IR = 1.13; 95% CI= 0.79–1.63).
Implications:
Unmet ADL need is prognostic of ED admissions, especially for falls and injuries. Future research is needed to determine whether resolution of unmet ADL need reduces ED utilization.
Keywords: Disabilities, Medicaid/Medicare, Home and Community based care and services
One in five community-living older adults with activity of daily living (ADL) disabilities report they do not have sufficient care for their ADL disabilities (Allen, Piette, & Mor, 2014; Kennedy, 2001). Self-reported health consequences of unmet ADL need include: skin breakdown due to lack of help with toileting and bathing; going hungry or thirsty because of lack of help with eating, and injuries attributed to lack of help with getting around (LaPlante, Kaye, Kang, & Harrington, 2004). Whether or not these self-reported consequences portend future emergency department (ED) utilization has not been determined. However, a cross-sectional study found that older adults with unmet ADL reported more ED visits in the prior year than older adults with met ADL need (Allen & Mor, 1997). That study assessed unmet ADL need and prior utilization at the same time. Consequently, it is unknown whether self-reports of unmet ADL need have predictive validity for risk identification and resource planning of older adults’ future ED utilization.
Community-living older adults have more than 17 million admissions to the ED annually (Pines, Mullins, Cooper, Feng, & Roth, 2013). Older adults at greatest risk for frequent ED admissions have multiple comorbidities and functional disabilities (Fan, Shah, Veazie, & Friedman, 2011; Gray et al., 2013), characteristics that are also associated with unmet ADL need (Newcomer, Kang, LaPlante, & Kaye, 2005). A study of older adults admitted to EDs concluded that nearly 40% of ED visits are potentially preventable including visits for injuries or skin breakdown (Caffrey, 2010). These reasons for ED utilization are similar to older adults’ self-reported consequences of unmet ADL need. These trends highlight the need for further research into future health outcomes of older adults with unmet ADL need.
A framework provided by Andersen (Andersen & Newman, 2005) guides our methodology for determining whether unmet ADL need increases risk for ED admissions in the context of characteristics that predispose, enable, and create need for medical care. Age is a predisposing characteristic that increases risk for ED utilization (Pallin, Allen, Espinola, Camargo, & Bohan, 2013). Chronic diseases such as heart disease and diabetes create need for emergency care (McCusker, Cardin, Bellavance, & Belzile, 2000). Unmet need for ADL assistance is considered an enabling characteristic that increases risk for future health care utilization. In summation, the primary hypothesis is that older adults who report unmet ADL need have more future ED admissions than older adults who report their ADL needs are met. Secondary hypotheses are that future ED admissions for falls, skin disorders, and dehydration occur with greater frequency among older adults who report unmet versus met ADL need.
Methods
Data are from the 2004 community interviews of the National Long-Term Care Survey (NLTCS) and linked Medicare claims data from 2004 to 2005. The NLTCS community sample is a nationally representative sample of community-living Medicare recipients aged 65 and older. The overall response rate to the community interview was over 90%. Medicare data provided information about the number of, and diagnostic codes for, ED admissions that occurred the year after the subject’s interview date.
Among the 5,201 respondents to the 2004 community survey, 2,449 without an ADL disability were excluded because presumably one cannot have unmet ADL need unless one has at least one ADL disability. An additional 390 subjects enrolled in a Health Maintenance Organization were excluded because HMOs used capitated rather than fee for service billing. Consequently it wasn’t possible to detect ED utilization for HMO enrollees. We also excluded 168 subjects whose disability began less than three months prior to the interview because this study is focused on older adults with long-term disability, rather than those with short-term episodes of disability. The final analytic sample included 2,194 subjects.
The primary outcome variable is the number of ED admissions in the year following the community interview. Revenue center codes 0450-0459, 0981 from both inpatient and outpatient Medicare claims data indicated an ED admission (Merriman & Caldwell, 2012). Secondary outcome variables were number of ED admissions associated with three categories of diagnoses: falls and injuries (ICD-9 codes 800.00–996.99), skin disease (ICD-9 codes 680.00–708.99), and dehydration including disorders of fluid, electrolyte, and acid-base balance (ICD-9 codes 276.00–276.99).
Presence of ADL disability was defined as requiring help, standby help, or using equipment to complete an ADL task (bathing, dressing, eating, toileting, and either getting out of bed or moving around a room). Unmet ADL need was defined as not receiving any help in the prior week, or receiving insufficient help, or having to wait to do the ADL task because there was not enough help for one or more ADL disability.
Choice of covariates were informed by prior research on predictors of ED use among older adults. Predisposing risks for ED admission included: age, sex, race, and living alone (Fan et al., 2011; Pallin et al., 2013; Shah, Rathouz, & Chin, 2001). Enabling characteristics include having a primary care provider and an adult child at home (Shah et al., 2001). Need characteristics included cancer, heart disease, stroke, chronic obstructive pulmonary disease, diabetes, Medicaid status, level of ADL disability, and cognitive impairment defined as reporting the presence of dementia or scoring 5 or above on the Short Portable Mental Status Questionnaire (Fan et al., 2011; McCusker et al., 2000; Pfeiffer, 1975; Pines et al., 2011).
Adjusted annual incidence ratios (IR) were computed using a negative binomial count model that incorporated sampling weights and covariates to control for predisposing, enabling and need characteristics that in preliminary analyses showed marginal significance (p < .2) with the dependent variable. Separately, for each of the secondary outcomes (ED admissions for falls and injuries, skin breakdown, and dehydration) IRs were computed using negative binomial models with sampling weights and covariates that had a p-value of .05 or less in the primary model for ED admissions.
Results
There were 1,986 total ED admissions. Table 1 shows that the annual average number of ED admissions was 1.19 for those with unmet ADL need compared with 0.87 for with met need. Table 2 presents IRs associated with unmet ADL need as well as other subject characteristics estimated from the negative binomial model. The following characteristics were associated with higher incidence for ED admissions: age 75 and older, Medicaid eligible, cognitive impairment, heart disease, and diabetes. The adjusted IR for unmet ADL need was 1.19 (95% confidence interval [CI] = 1.00–1.40).
Table 1.
Sample Characteristics
| Variable | Count weighted (%) | Population count | Weighted annual average number ED visits |
|---|---|---|---|
| Age | |||
| ≥75 | 463 (26.7) | 974,012 | 0.82 |
| <75 | 1,731 (73.3) | 2,676,029 | 0.99 |
| Sex | |||
| Men | 637 (31.9) | 1,163,312 | 0.97 |
| Women | 1,557 (68.1) | 2,486,729 | 0.93 |
| Race | |||
| White | 1,922 (85.9) | 3,134,584 | 0.92 |
| Other | 272 (14.1) | 515,457 | 1.09 |
| Living | |||
| Alone | 930 (39.0) | 1,424,356 | 0.93 |
| Not alone | 1,264 (61.0) | 2,225,685 | 0.95 |
| Medicaid | |||
| Yes | 484 (22.7) | 826,697 | 1.24 |
| No | 1,710 (77.4) | 2,823,344 | 0.85 |
| PCP | |||
| Yes | 2,069 (96.5) | 3,437,845 | 0.94 |
| No | 75 (3.5) | 116,712 | 1.06 |
| Adult child | |||
| In home | 403 (18.4) | 625,171 | 1.10 |
| Not in home | 1,791 (81.6) | 3,024,869 | 0.91 |
| Cancer | |||
| Yes | 293 (9.2) | 334,754 | 1.03 |
| No | 1,996 (90.8) | 3,303,159 | 0.93 |
| Heart disease | |||
| Yes | 1,167 (55.8) | 1,593,793 | 1.09 |
| No | 997 (44.2) | 2,015,269 | 0.76 |
| Stroke | |||
| Yes | 201 (9.5) | 344,467 | 1.05 |
| No | 1,981 (90.5) | 3,286,174 | 0.92 |
| COPD | |||
| Yes | 179 (9.3) | 338,282 | 1.12 |
| No | 2,009 (90.7) | 3,299,410 | 0.92 |
| Cognitive impairment | |||
| Yes | 695 (29.8) | 1,088,784 | 1.16 |
| No | 1,499 (70.2) | 2,561,256 | 0.85 |
| Diabetes | |||
| Yes | 527 (28.0) | 1,018,314 | 1.13 |
| No | 1,661 (72.0) | 2,620,443 | 0.87 |
| ADL | |||
| 1–2 | 1,545 (69.8) | 2,547,649 | 0.84 |
| 3–5 | 649 (30.2) | 1,102,392 | 1.18 |
| Unmet need | |||
| Yes | 472 (22.5) | 822,391 | 1.19 |
| No | 1,722 (77.5) | 2,827,649 | 0.87 |
ADL = activity of daily living; COPD = chronic obstructive pulmonary disease; ED = emergency department; PCP = primary care provider.
Table 2.
Incidence Ratios for ED Admissions
| Incidence ratio (95% CI) | p-Value | |
|---|---|---|
| Age 75+ | .013 | |
| Yes | 1.29 (1.06–1.27) | |
| No | — | |
| Sex | .648 | |
| Women | 0.96 (0.83–1.12) | |
| Men | — | |
| Race | .668 | |
| White | 0.93 (0.69–1.27) | |
| Other | — | |
| Living | .965 | |
| Alone | 1.00 (0.83–1.19) | |
| Other | — | |
| Medicaid | .004 | |
| Yes | 1.36 (1.11–1.66) | |
| No | — | |
| Adult child | .786 | |
| In home | 1.03 (0.83–1.29) | |
| Not in home | — | |
| Cancer | .481 | |
| Yes | 1.10 (0.85–1.43) | |
| No | — | |
| Heart disease | .001 | |
| Yes | 1.32 (1.13–1.55) | |
| No | — | |
| Stroke | .913 | |
| Yes | 0.99 (0.77–1.26) | |
| No | — | |
| COPD | .174 | |
| Yes | 1.17 (0.93–1.47) | |
| No | — | |
| Cognitive status | .022 | |
| Impaired | 1.27 (1.04–1.56) | |
| Not impaired | — | |
| Diabetes | .042 | |
| Yes | 1.22 (1.02–1.46) | |
| No | — | |
| ADL 3–5 | .155 | |
| Yes | 1.15 (0.95–1.39) | |
| No | — | |
| Unmet need | .047 | |
| Yes | 1.19 (1.00–1.40) | |
| No | — |
ADL = activity of daily living; CI = confidence interval; COPD = chronic obstructive pulmonary disease; ED = emergency department.
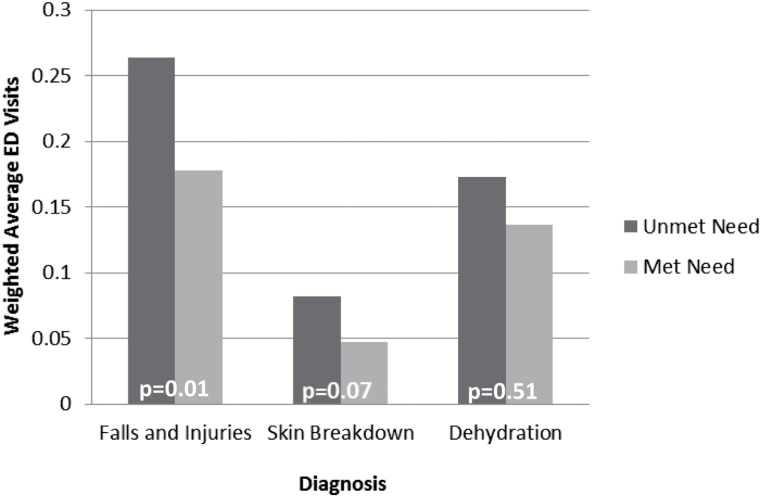
Among subjects with an ED admission, 15.9% of patients had at least one ED admission with an ICD9 code for a falls and injuries, 4.4% had at least one ED admission for skin breakdown, and 11.8% had at least one ED admission for dehydration. Figure 1 illustrates that patients with unmet ADL need had a population weighted annual average of 0.26 ED admissions for falls and injuries compared with 0.18 for those with met ADL need. The IR for an ED admission for a fall or injury was 1.43 (95% CI = 1.10–1.86) for those with unmet versus met need. Patients with unmet ADL need had a population weighted average of 0.08 ED admissions for skin breakdown per year compared with 0.05 for those who reported met need for ADL help. The IR for skin breakdown was 2.02 (95% CI = 0.97–2.88), revealing a nonsignificant trend for increased ED admissions for skin breakdown among those who reported unmet versus met ADL need. The population weighted average of 0.17 ED admissions for dehydration per year compared with 0.14 for those who did not report unmet need for ADL help was not statistically significant (p = .51: IR = 1.13; 95% CI = 0.79–1.63).
Figure 1.
Weighted average emergency department visits for given diagnoses by unmet need status.
Discussion
Self-reports of unmet ADL need predict future ED utilization, particularly for falls and injuries. Prior studies have described the prevalence of self-reported consequences of unmet need (Allen et al., 2014; Freedman & Spillman, 2014; LaPlante et al., 2004) but this study is the first to assess the prognostic validity of reports of unmet ADL need using Medicare claims data. Policy makers rely on Medicare claims data to inform need for quality improvement in health care delivery. Because unmet ADL need, falls, and injuries are potentially preventable; the results from this study motivate the development of care practices that reduce unmet ADL need and its costly health consequences.
Despite the high prevalence of unmet ADL need, there is no system that ensures screening of community-living disabled older adults about their ADL needs. Hospital discharge planning that includes assessments of unmet ADL need is a potential solution. However, many older adults report new unmet ADL need after hospital discharge, and those who return home with new unmet ADL need have twice the risk for readmission as those with met ADL need (DePalma et al., 2013). EDs provide another opportunity for recognition and referral. Although a study found that one in five older ED patients who reported they did not have sufficient care at home were nonetheless discharged home (Wilber, Blanda, & Gerson, 2006). Clearly, there is a need for improved screening for unmet ADL need, especially in clinical settings frequented by vulnerable older adults.
The findings from this study underscore the importance of coordinating primary care, acute care, and long-term services. Coordination of care could reduce costly consequences of unmet ADL need. Acute care admissions significantly declined after enrollment in the Program of All Inclusive Care (PACE) among enrollees who did not have a caregiver to help with their ADL disabilities (Sands et al., 2006). PACE provides primary care, acute care, and community based services and supports. Recent efforts in developing systems of coordinated care for frail elders include the MediCaring Model of care (Lynn & Montgomery, 2015). Key elements include longitudinal patient-centered care plans that incorporate health, social and supportive services. The Affordable Care Act encourages the creation of programs that improve quality of patient care while simultaneously reducing Medicare spending.
The results must be interpreted in the context of the study limitations. We depended upon ICD-9 codes to detect ED admissions for potentially preventable events. ICD-9 codes are for billing purposes and are not designed to describe causal mechanisms for ED admissions. Also, data for this study were collected 10 years ago, but the phenomenon of unmet need and its consequences appears to be consistent in the past 2 decades. Multiple national studies estimate that unmet ADL need affects 20–25% of community-living older adults (Allen et al., 2014; LaPlante et al., 2004; Sands et al., 2006; Xu, Covinsky, Stallard, Thomas, & Sands, 2012). Further, multiple studies report that falls and skin discomfort are the most common self-reported consequences of unmet ADL need (Allen & Mor, 1997; LaPlante et al., 2004). To our knowledge, this study is the first to link survey data with prospective Medicare data to demonstrate that self-reports of unmet ADL need predict future ED utilization. More comprehensive research is needed to develop care pathways that reduce unmet ADL need and associated health consequences.
Funding
This research was funded by a grant from the National Institutes of Health (R01AG034160 to L.P.S.).
References
- Allen S. M., Mor V. (1997). The prevalence and consequences of unmet need. Contrasts between older and younger adults with disability. Medical Care, 35, 1132–1148. [DOI] [PubMed] [Google Scholar]
- Allen S. Piette E., & Mor V (2014). The adverse consequences of unmet need among older persons living in the community: Dual-eligible versus Medicare-only beneficiaries. Journal of Gerontology: Social Sciences, 69, S51–S58. doi:10.1093/geronb/gbu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R., & Newman J (2005). Societal and individual determinants of medical care utilization in the United States. The Millbank Quarterly, 83, 1–28. [PubMed] [Google Scholar]
- Caffrey C. (2010). Potentially preventable emergency department visits by nursing home residents: United States, 2004. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- DePalma G. Xu H. Covinsky K. E. Craig B. A. Stallard E. Thomas J. III, & Sands L. P (2013). Hospital readmission among older adults who return home with unmet need for ADL disability. The Gerontologist, 53, 454–461. doi:10.1093/geront/gns103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan L. Shah M. Veazie P., & Friedman B (2011). Factors associated with Emergency Department use among the rural elderly. Journal of Rural Health, 27, 39–49. doi:10.1111/j.1748-0361.2010.00313.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V., & Spillman B (2014). Disability and care needs among older Americans. Milbank Quarterly, 92, 509–541. doi:10.1111/1468-0009.12076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray L. Peel N. Costa A. Burkett E. Dey A. Jonsson P.,…Hirdes J (2013). Profiles of older patients in the emergency department: Findings from the interRAI Multinational Emergency Department Study. Annals of Emergency Medicine, 62, 467–474. doi:10.1016/j.annemergmed.2013.05.008 [DOI] [PubMed] [Google Scholar]
- Kennedy J. (2001). Unmet and undermet need for activities of daily living and instrumental activities of daily living assistance among adults with disabilities. Medical Care, 39, 1305–1312. [DOI] [PubMed] [Google Scholar]
- LaPlante M. Kaye S. Kang T., & Harrington C (2004). Unmet need for personal assistance services: Estimating the shortfall in hours of help and adverse consequences. Journal of Gerontology: Social Sciences, 59B, S98–S108. [DOI] [PubMed] [Google Scholar]
- Lynn J., Montgomery A. (2015). Creating a comprehensive care system for frail elders in "age boom" America. The Gerontologist, 55, 278–285. doi:10.1093/geront/gnu175 [DOI] [PubMed] [Google Scholar]
- McCusker J. Cardin S. Bellavance F., & Belzile E (2000). Return to the emergency department among elders: Patterns and predictors. Academic Emergency Medicine, 7, 249–259. [DOI] [PubMed] [Google Scholar]
- Merriman K., & Caldwell D (2012). How to identify emergency room services in the Medicare claims data. Retrieved February 4, 2014, from http://www.resdac.org/resconnect/articles/144 [Google Scholar]
- Newcomer R. Kang T. LaPlante M., & Kaye S (2005). Living quarters and unmet need for personal care assistance among adults with disabilities . Journal of Gerontology: Social Sciences, 60B, S205–S213. [DOI] [PubMed] [Google Scholar]
- Pallin D. Allen M. Espinola J. Camargo C., & Bohan J (2013). Population aging and emergency departments: Visits will not increase, lengths-of-stay and hospitalizations will. Health Affairs, 32, 1306–1312. doi:10.1377/hlthaff.2012.0951 [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. (1975). A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society, 23, 433–441. [DOI] [PubMed] [Google Scholar]
- Pines, J. M., Asplin, B. R., Kaji, A. H., Lowe, R. A., Magid, D. J., Raven, M., . . . Yealy, D. M. (2011). Frequent users of emergency department services: Gaps in knowledge and a proposed reserach agenda. Academic Emergency Medicine, 18, e64–e69. doi:10. 1111/j.1553-2712.2011.01086.x [DOI] [PubMed] [Google Scholar]
- Pines J. M., Mullins P. M., Cooper J. K., Feng L. B., Roth K. E. (2013). National trends in emergency department use, care patterns, and quality of care of older adults in the United States. Journal of the American Geriatrics Society, 61, 12–17. doi:10.1111/jgs.12072 [DOI] [PubMed] [Google Scholar]
- Sands L. Wang Y. McCabe G. Jennings K. Eng C., & Covinsky K (2006). Rates of acute care admissions for frail elders living with met versus unmet activity of daily living needs. Journal of the American Geriatrics Society, 54, 339–344. [DOI] [PubMed] [Google Scholar]
- Shah M. Rathouz P., & Chin M (2001). Emergency department utilization by noninstitutionalized elders. Academic Emergency Medicine, 8, 267–273. [DOI] [PubMed] [Google Scholar]
- Wilber S. Blanda M., & Gerson L (2006). Does functional decline prompt emergency department visits and admission in older patients? Academic Emergency Medicine, 13, 680–682. [DOI] [PubMed] [Google Scholar]
- Xu H. Covinsky K. Stallard E. Thomas J., & Sands L (2012). Insufficient help for ADL disabilities and risk for all-cause hospitalization. Journal of the American Geriatrics Society, 60, 927–933. doi:10.1111/j.1532-5415.2012.03926.x [DOI] [PMC free article] [PubMed] [Google Scholar]