Abstract
Purpose of the Study
Driving is important for older adults’ health and well-being, yet little research has examined interventions to maintain driving mobility. As fluid cognitive abilities are strongly linked to driving, targeted cognitive training interventions may impact driving mobility longitudinally. This study assessed the effects of three different cognitive training programs (reasoning, speed of processing, and memory) on driving cessation in older adults across 10 years (n = 2,390).
Design and Methods
Cox regression analyses evaluated the impact of each program relative to a no-contact control group with intent-to-treat (ITT) analyses. The effects of randomization to additional booster sessions were also examined. Subsample analyses repeated these models in participants who were at-risk for driving mobility declines.
Results
There were no training (n = 2,390) or booster training (n = 1,540) effects on driving cessation with ITT analyses. Individuals at-risk for future mobility declines were 49% (Hazard Ratio (HR) = 0.51, 95% confidence interval [CI]: 0.28, 0.94; n = 336) less likely to cease driving after speed of processing training and 55% (HR = 0.45, 95% CI: 0.24, 0.86; n = 324) less likely to quit driving subsequent to reasoning training. Additional booster sessions for speed of processing training resulted in a 70% reduction of driving cessation (HR = 0.30, 95% CI: 0.11, 0.82; n = 252) in the subsample analyses. There were no significant effects of memory training.
Implications
Some cognitive interventions transfer to maintained driving among those at-risk for mobility declines due to cognitive impairment. Future research should identify moderators and mediators of training and transfer effects.
Keywords: Cognitive intervention, Speed of processing training, Reasoning training, Memory training, Everyday functioning
Maintaining safe driving mobility is an important skill of great concern to older adults and their families. Older adults who cease driving are at greater risk for numerous negative outcomes ranging from depression (Marottoli et al., 1997; Ragland, Satariano, & MacLeod, 2005) and decreased engagement (Mezuk & Rebok, 2008), to greater health declines (Edwards, Lunsman, Perkins, Rebok, & Roth, 2009), increased risk for entry into a long-term care facility, and mortality (Edwards, Perkins, Ross, & Reynolds, 2009; Freeman, Gange, Muñoz, & West, 2006). Older adults with poor fluid cognitive abilities, such as reasoning (Anstey, Windsor, Luszcz, & Andrews, 2006; O’Connor, Edwards, Small, & Andel, 2012) or speed of processing (Anstey et al., 2006; Edwards, Bart, O’Connor, & Cissell, 2009; Emerson et al., 2012; Ross et al., 2009; Vance et al., 2006) are at greater risk for adverse mobility outcomes including driving cessation. Our previous research demonstrated that a cognitive training program (i.e., speed of processing training) transferred to enhanced driving safety and mobility over 5 years (Ball, Edwards, Ross, & McGwin, 2010; Edwards, Delahunt, & Mahncke, 2009; Edwards, Myers, et al., 2009; Roenker, Cissell, Ball, Wadley, & Edwards, 2003; Ross et al., 2016). Given this prior work, as well as the robust associations between cognition and driving, this study examined the effects of three different cognitive training programs (reasoning, speed of processing, and memory training) on driving cessation across 10 years, thus addressing a critical gap in the knowledge of the long-term effects of different types of cognitive training on everyday function (Kelly et al., 2014).
Over the last 30 years, several cognitive training programs have been developed to improve specific fluid abilities. Although these training programs typically demonstrate improvement of the cognitive abilities targeted, transfer to broader cognitive abilities has been limited (Edwards et al., 2005; Peng, Wen, Wang, & Gao, 2012; Simpson, Camfield, Pipingas, Macpherson, & Stough, 2012), which has led to debates about the value of such interventions. The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study was the first randomized controlled trial to compare the effects of three cognitive training programs (reasoning training, speed of processing training, and memory training) on cognitive and everyday functional outcomes across 10 years. Each intervention improved performance on the targeted cognitive abilities, but effects varied by training type, approach, and participant characteristics (Ball, Ross, Roth, & Edwards, 2013; Rebok et al., 2014; Rebok et al., 2013; Willis & Caskie, 2013). Participants randomized to speed of processing training reported maintained health-related quality of life at 5 years (Wolinsky et al., 2006), and participants randomized to any of the three types of training reported less difficulty with Instrumental Activities of Daily Living (IADL) performance across 10 years (Rebok et al., 2014). Those randomized to speed of processing training showed better self-ratings of health (Wolinsky et al., 2010), protection against depressive symptoms (Wolinsky, Vander Weg, et al., 2009), and less predicted medical expenditures (Wolinsky, Mahncke, et al., 2009) across 3 to 5 years. Similarly, other randomized trials have shown transfer of speed of processing training to improved IADL performance (Edwards et al., 2002; Edwards et al., 2005), as well as safer and prolonged driving mobility (Ball et al., 2013; Roenker et al., 2003; Ross et al., 2016). Thus, despite the ongoing debate regarding the potential efficacy of cognitive training, there is evidence that some programs transfer more broadly to positively affect older adults’ well-being and everyday functioning.
Maintaining mobility is vital to preserving quality of life across the lifespan. Although public transportation and other forms of transit such as walking and cycling may be viable modes of travel for some, driving an automobile serves as a means of independence and the primary or only source of transportation for many Americans. This is particularly evident in rural and suburban areas where there are limited transportation alternatives and greater distances to access goods, services, and social networks. Consequently, safe driving mobility is important to older adults’ health and well-being (Edwards, Lunsman, et al., 2009; Edwards, Perkins, et al., 2009; Freeman et al., 2006; Marottoli et al., 1997). The first randomized clinical trial of speed of processing training among older adults with poor baseline Useful Field of View (UFOV®) test performance, a measure of processing speed, divided attention, and selective attention (including inhibition), demonstrated transfer to safer on-road driving performance relative to driver-simulator training (Roenker et al., 2003). The ACTIVE study showed that both speed of processing and reasoning training enhanced older drivers’ safety as indicated by a ≥48% reduction in at-fault crash involvement over 6 years (Ball et al., 2010). The ACTIVE study and a third randomized clinical trial further demonstrated that relative to active- and no-contact controls, speed of processing training transferred to maintained driving mobility across 3 and 5 years (Edwards, Delahunt, et al., 2009; Ross et al., 2016), and lower rates of driving cessation across 3 years (Edwards, Delahunt, et al., 2009). Across multiple clinical trials, the transfer effects of speed of processing training vary according to the baseline characteristics of the sample, the number of sessions, and the training technique (Ball, Edwards, & Ross, 2007; Ball et al., 2013).
Specifically, previous research indicates that those with particular baseline cognitive difficulties (i.e., poor UFOV® performance) are more likely to benefit, that more sessions of training result in greater benefits, and that adaptive training techniques are most effective (Ball et al., 2007; Ball et al., 2013; Lövdén, Backman, Lindenberger, Schaefer, & Schmiedek, 2010; Ross et al., 2016). Further, a growing body of work has indicated that individuals with poor UFOV® performance are at greater risk for future mobility declines including driving cessation (Edwards et al., 2008; Edwards, Bart, et al., 2009; Ross et al., 2009).
This is the first study to examine the impact of reasoning, speed of processing, and memory training, as well as related booster training sessions, on driving mobility across 10 years. As reasoning and speed of processing are strongly related to driving outcomes (Anstey et al., 2006; Edwards, Bart, et al., 2009; Emerson et al., 2012; Ross et al., 2009; Vance et al., 2006), it was hypothesized that both of these training types, but not memory training, would transfer to maintained driving mobility. Second, in line with previous work (Ball et al., 2007; Ross et al., 2016), effects were examined among a subsample of participants with poor baseline UFOV® performance as this subsample was at greater risk for future mobility declines (Edwards et al., 2008; Edwards, Bart, et al., 2009; Ross et al., 2009). It was expected that this more impaired subsample would demonstrate the largest effects. Finally, this study examined the effects of additional booster sessions within each respective training group on driving cessation across 10 years. In line with previous work demonstrating that additional speed of processing booster sessions result in larger training and transfer effects (Ball et al., 2010; Ross et al., 2016; Willis et al., 2006), it was hypothesized that booster training would strengthen effects.
Design and Methods
Participants
Analyses were conducted among older drivers from the ACTIVE study. Briefly, the ACTIVE study was a single-blind (i.e., assessors), randomized, controlled trial across six U.S. field sites (Birmingham, AL; State College, PA; Cumberland, MD; Detroit, MI; Boston, MA; Indianapolis, IN) that investigated the impact of three cognitive interventions, compared to a no-contact control group, on long-term cognition, health, and everyday functioning (n = 2,802). Recruitment strategies varied by field site and included recruitment from senior centers and state driver/nondriver identification card databases as examples (see Jobe et al., 2001 for further details). Eligibility criteria resulted in a healthy sample of community-dwelling adults aged 65 and older without substantial cognitive impairment (Mini-Mental State Exam score of 23 or higher); unremarkable physical health (no reported stroke within the last year, no report of certain types of cancer, or no recent chemotherapy/radiation treatment); intact functional abilities (reported ability to perform activities of daily living); intact vision (20/50 far visual acuity or better); and ability to verbally communicate. Further details on procedures are elsewhere (Jobe et al., 2001). The current analyses included participants who self-identified as drivers at baseline (n = 2,402). Participants in the analytic sample reported an average age of 73 years (SD = 5.70, range 65–91), education of 13.75 years (SD = 2.68, range 4–20), and drove 5.59 (SD = 1.78, range = 1–7) days per week. The majority (73.2%) of participants were women. Table 1 displays sample demographic characteristics by study arm.
Table 1.
Demographic Characteristics of Study Sample Across Four Study Arms (n = 2,402)
| Reasoning | Speed of processing | Memory | Control | |
|---|---|---|---|---|
| Age in years, mean (SD) | 73.16 (5.60) | 73.13 (5.55) | 73.21 (5.87) | 73.60 (5.78) |
| Education in years, mean (SD) | 13.70 (2.65) | 13.84 (2.70) | 13.80 (2.72) | 13.63 (2.68) |
| Gender (% female) | 73.50 | 73.60 | 74.30 | 71.40 |
| Cessation events, n | 50 | 52 | 53 | 54 |
| Total n | 596 | 598 | 610 | 598 |
Note: ANOVA and Chi-square analyses revealed no group differences at baseline.
Procedure and Materials
Eligible participants completed in-person baseline assessments and were equally allocated to one of four parallel study arms via a computerized randomization sequence conducted by an independent organization. Participants were randomized to either reasoning training (n = 596), speed of processing training (n = 598), memory training (n = 610), or no-contact control arms (n = 598). Between 1998 and 2000, each training arm received ten 60–75min sessions of training. All training sessions were led by certified trainers and conducted in small groups of three to four participants. Feedback was provided. The first five initial training sessions for all training arms were standardized (i.e., exercises were the same across all participants within each condition), whereas the last five initial sessions focused on practice of skills learned in the first five sessions. Further detail on intervention procedures are elsewhere (Jobe et al., 2001). 90.2% of the participants completed at least eight or more sessions and compliance did not differ by training group (p > .05). Half of the compliant participants (i.e., those who completed eight or more of the initial 10 reasoning-, speed of processing-, or memory- training sessions) were further randomized to additional “booster” training. Booster training included four additional training sessions prior to Year 1 and four more sessions again prior to Year 3. Those not randomized to the booster groups were not offered additional training. All participants were re-assessed at post-test (immediately after initial training), Years 1 through 3, 5, and 10. The trial was registered at ClinicalTrials.gov, No: NCT00298558.
Training Arms
Reasoning training was strategy-based and used paper-and-pencil tasks designed to improve linear problem solving. Training involved practice identifying patterns or sequences, such as finding the pattern in a series of repeating letters or identifying dosage patterns of medications (Willis & Caskie, 2013). This training was partially adaptive with two levels offered based on the individual participant that differed in difficulty and pacing.
Speed of processing training was process-based, computerized training, involving perceptual-practice exercises focused on improving the speed at which participants could correctly identify increasingly complex displays of visual information. The exercises focused on visual stimulus detection, identification, and discrimination alone and along with localization of peripheral targets (i.e., divided attention) with and without distractors (i.e., selective attention). The primary adaptation was display speed (Ball et al., 2007; Jobe et al., 2001). Exercises in the first five sessions were standardized across participants and all remaining sessions (including all booster sessions) involved exercises adaptive in difficulty to the individual trainee.
Memory training was strategy-based and conducted using paper-and-pencil tasks designed to teach mnemonic strategies focused on verbal episodic memory. The training involved practice organizing materials into meaningful categories that would promote transfer to everyday functioning (e.g., remembering lists of errands, grocery shopping, etc.; Rebok et al., 2013).
No-contact control: No intervention was conducted with this arm.
Materials
Main Outcome Measure
Driving status was assessed at each time-point using a validated questionnaire (Owsley, Stalvey, Wells, & Sloane, 1999). Drivers were defined as those who reported “having driven within the previous 12 months or who would drive today, if needed” (Owsley et al., 1999). A dichotomous variable was created with participants who ceased driving at any point during the 10-year study period coded as 1 and those who did not quit driving coded as 0.
Covariates
Driving Frequency
Baseline driving frequency is a well-established predictor of future driving cessation (Edwards, Bart, et al., 2009; Emerson et al., 2012). Baseline days driven per week (0–7), derived by a validated questionnaire (Owsley et al., 1999), was used as a covariate to account for driving mobility.
Study Site
ACTIVE study sites differed in terms of demographics (age, gender, and education), as well as metropolitan density, socio-economic status, and access to alternative transportation, all of which can affect driving behaviors (Santos, McGuckin, Nakamoto, Gray, & Liss, 2011). Site was included in all regression models as a covariate to adjust for these factors.
Gender
Women are more likely to cease driving earlier than men (Dugan & Lee, 2013; Edwards, Bart, et al., 2009) and are over-represented in the ACTIVE study (74%). Gender was included as a covariate (women = 0, men = 1).
Baseline Cognition
The UFOV® is a well-established measure of speed of processing, divided attention, and selective attention that reliably and longitudinally predicts driving behaviors such as avoidance, mobility, and cessation (Edwards et al., 2008; Ross et al., 2009). Individuals with poor UFOV® performance are at increased risk for subsequent mobility declines due to difficulties managing the demands of driving (e.g., processing a large amount of information in a constantly changing environment; Edwards et al., 2008; Ross et al., 2009). Such individuals show larger training gains and broader transfer of training to driving outcomes (Ball et al., 2007; Ball et al., 2013; Ross et al., 2016). As in prior research (Edwards, Delahunt, et al., 2009; Edwards, Myers, et al., 2009; Roenker et al., 2003; Ross et al., 2016), UFOV® performance was used to define the subsample with baseline cognitive difficulties. Using the standardized scoring protocol (Ball & Roenker, 2014), participants with poor baseline performance (i.e., UFOV® categories 3–5) were included in the subsample analyses (n = 663).
Analyses
First, Chi-square and ANOVA analyses examined if demographics, baseline driving frequency, or baseline UFOV® scores differed by study arm. Then, Cox regression analyses examined the effects of each cognitive training program (as compared to the no-contact control condition) on driving cessation across 10 years after controlling for study site, baseline driving frequency, and gender. For participants who quit driving, months between baseline and driving cessation was calculated. For nonevents (i.e., did not quit driving), time was right censored at the last assessment. A small percentage of participants were excluded from these analyses due to missing baseline data resulting in a total analytic sample of 2,390 for the ITT analyses and 656 for the subsample analyses. Analyses were performed with SPSS 22.
Each training arm (1) was dummy coded for comparison to the no-contact control arm (0) resulting in three main group comparisons: reasoning training versus no-contact control, speed of processing training versus no-contact control, and memory training versus no-contact control. Cox regression models were conducted for each training versus control group comparison. First, separate intent-to-treat (ITT) models compared participants randomized to each intervention to the no-contact control group, regardless of training adherence. Second, the impact of booster training was assessed for each intervention by comparing participants in each training arm who were randomized to booster training to the participants in the control group. Lastly, two additional sets of models focused on participants who were at-risk for driving mobility declines due to poor baseline UFOV® performance (Edwards, Myers, et al., 2009; Ross et al., 2009). Within this subsample, analyses investigating the impact of randomization to training and booster training were repeated.
Results
Chi-square and ANOVAs revealed that the four study arms did not differ on demographics (age, gender, and education), baseline driving frequency, or baseline UFOV® (ps > .05).
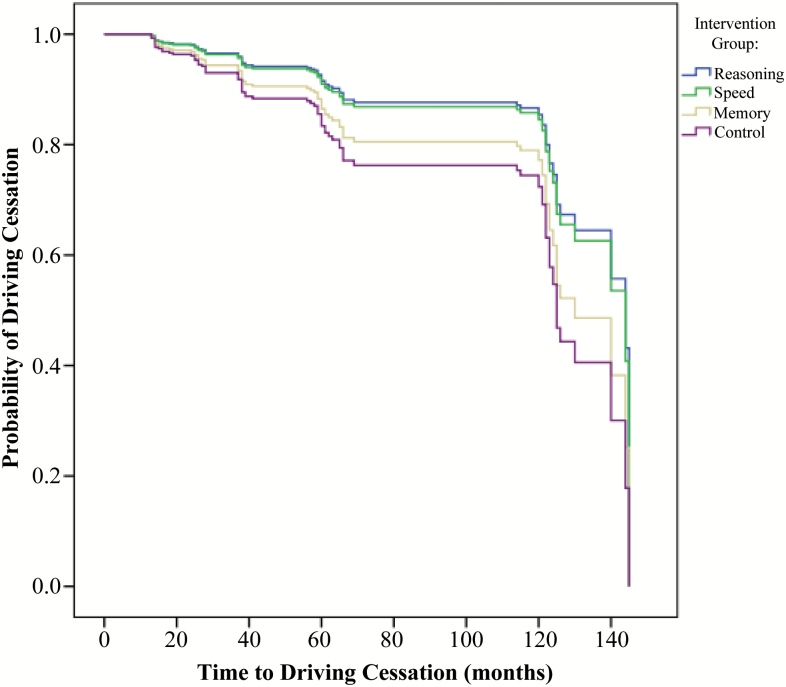
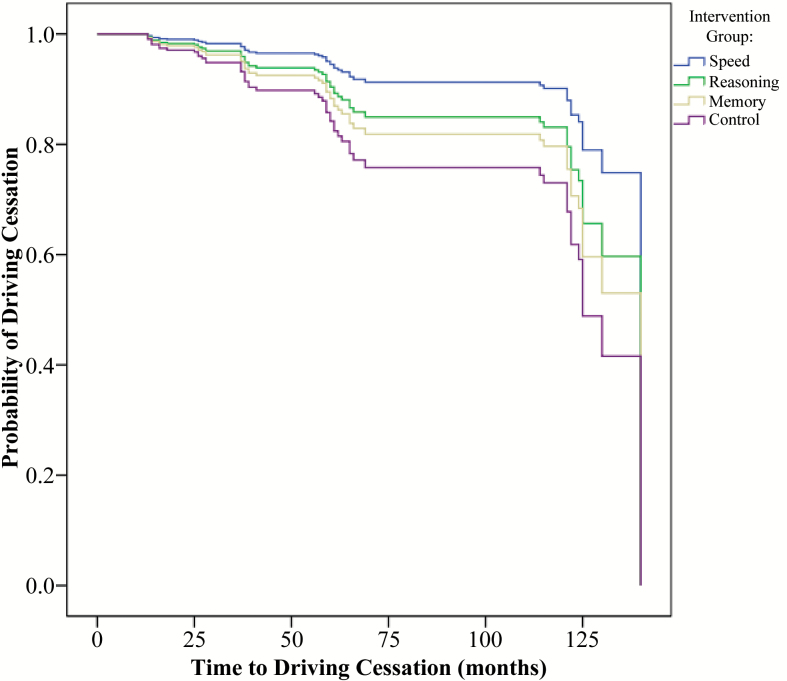
Across training arms, 209 participants ceased driving (8.7%) and 2,193 did not quit driving (91.3%). Cox regression models revealed that training did not affect rates of driving cessation within the full sample ITT (n = 2,390) or booster session (n = 1,540) analyses (Hazard Ratios (HR) = 0.74–0.94, ps > .05). However, transfer effects were observed for the subsample of individuals with poor UFOV® at baseline (n = 656; see Table 2 and Figure 1). In this subsample, the percentage of participants who ceased driving were 11%, 11.9%, 14.8%, and 16.4% for participants randomized to the reasoning training, speed of processing training, memory training, and control arms respectively. Results revealed that reasoning and speed of processing training reduced the likelihood of driving cessation by 55% and 49% across 10 years, respectively in this subsample. Speed of processing booster training, but not reasoning booster training, further reduced the likelihood of driving cessation by 70% across 10 years in the subsample (see Table 2 and Figure 2). Memory training did not reduce the rates of driving cessation within any analyses. Greater driving frequency at baseline was associated with a lower likelihood of driving cessation across the study period, with HRs ranging between 0.63 and 0.76. Table 2 and Figures 1 and 2 depict the probabilities of driving cessation by study arm.
Table 2.
Rates of Driving Cessation for Cognitive Training vs. No-contact Control Conditions Across 10 Years in Older Adults At-risk for Driving Mobility Declines
| Reasoning vs. control | Speed of processing vs. control | Memory vs. control | ||||
|---|---|---|---|---|---|---|
| Model | HR | 95% CI | HR | 95% CI | HR | 95% CI |
| Randomization to training | ||||||
| Training group | 0.45* | 0.24, 0.86 | 0.51* | 0.28, 0.94 | 0.81 | 0.47, 1.41 |
| Study site | 0.92 | 0.77, 1.09 | 0.99 | 0.84, 1.17 | 0.91 | 0.78, 1.07 |
| Baseline driving frequency | 0.68*** | 0.58, 0.79 | 0.72*** | 0.62, 0.82 | 0.76* | 0.66, 0.87 |
| Gender | 1.78 | 0.88, 3.60 | 1.98* | 1.06, 3.72 | 1.56 | 0.81, 3.02 |
| Randomization to booster training | ||||||
| Training group | 0.61 | 0.31, 1.22 | 0.30* | 0.11, 0.82 | 0.69 | 0.34, 1.40 |
| Study site | 0.89 | 0.74, 1.07 | 0.93 | 0.76, 1.13 | 0.91 | 0.76, 1.11 |
| Baseline driving frequency | 0.63*** | 0.53, 0.76 | 0.74** | 0.62, 0.88 | 0.73** | 0.61, 0.88 |
| Gender | 1.17 | 0.83, 3.66 | 2.20* | 1.03, 4.73 | 2.16* | 1.05, 4.44 |
Notes: Sample sizes for initial training analyses were: reasoning trained (n = 154), speed of processing trained (n = 166), memory trained (n = 166), no-contact control (n = 170). Sample sizes for booster analyses were: reasoning trained (n = 87), speed of processing trained (n = 82), memory trained (n = 97), and no-contact control (n = 170). CI = confidence interval.
*p < .05. **p < .01. ***p < .001.
Figure 1.
Risk of driving cessation by study arm across 10 years in participants with poor baseline Useful Field of View performance. Note: Covariates included study site, gender, and baseline driving frequency. Sample sizes were: reasoning trained (n = 154), speed of processing trained (n = 166), memory trained (n = 166), and no-contact control (n = 170).
Figure 2.
Risk of driving cessation by study arm across 10 years in participants with poor baseline Useful Field of View performance who received booster training. Note: Covariates included study site, gender, and baseline driving frequency. Booster training occurred at Years 1 and 3. Sample sizes for booster analyses were: reasoning trained (n = 87), speed of processing trained (n = 82), memory trained (n = 97), and no-contact control (n = 170).
Discussion
These analyses are the first to compare the effects of three cognitive training programs on driving cessation across a 10-year period. Our hypotheses were partially supported. Although reasoning, speed of processing, and memory training did not impact driving cessation within the ITT analyses, there were significant effects of training among the subsample of adults with baseline UFOV® difficulties, which are indicative of risk for future mobility declines. This subsample of older adults who were randomized to reasoning training were 55% less likely to quit driving across 10 years. Similarly, older adults with baseline UFOV® difficulties randomized to speed of processing training were 49% less likely to cease driving and 70% less likely to cease driving with additional booster training. This training transfer among older adults with baseline cognitive difficulties is noteworthy, particularly given the large and lasting effects across 10 years. To our knowledge, this is the first study to demonstrate that cognitive training transfers to maintained driving across a decade. Previous research similarly indicated that among older adults with poor baseline UFOV®, speed of processing training prolonged driving mobility and decreased rates of driving cessation across 3 to 5 years (Edwards, Delahunt, et al., 2009; Edwards, Myers, et al., 2009; Ross et al., 2016).
Of course maintained driving mobility does not equate to safe driving nor is it a desired outcome for those who do not drive safely. However, prior research has also demonstrated that speed of processing training enhances on-road driving safety (Roenker et al., 2003). Additionally, both reasoning training and speed of processing training resulted in fewer at-fault crashes compared to no training for up to 6 years (Ball et al., 2010). Taken together, these results indicate that cognitive reasoning or speed of processing training can positively affect both driving safety and mobility among older adults who are at risk for mobility declines due to cognitive difficulties.
Clearly, there is heterogeneity of treatment effects for cognitive training. Patterns of training transfer differed by cognitive training approach and participant baseline cognitive abilities. Significant transfer effects to driving mobility across 10 years were limited to those with poor UFOV® performance at baseline. This is in line with previous research (Ball et al., 2007; Ross et al., 2016) that has found the greatest training gains and transfer among at-risk individuals when using process-based cognitive training approaches. This pattern of training gains and transfer is likely due to greater room for improvements in cognitive and everyday functional abilities. Significant declines in the everyday performance outcome of interest must be evident for training transfer effects to be detected (Willis et al., 2006).
Our results, as well as previous work, indicate that those with baseline cognitive difficulties are more likely to longitudinally experience transfer of training to improved everyday functional outcomes such as driving. In contrast, other research indicates that individuals with better baseline cognitive function tend to benefit more from strategy-based memory training (Bissig & Lustig, 2007). Thus, baseline cognitive status is likely a moderator of training gains and transfer, but effects vary by training approach. Interpretation of cognitive training gains and transfer across studies should be made in consideration of the samples’ baseline cognitive abilities as well as the training approach used (Edwards, Myers, et al., 2009). These heterogeneity of treatment effects are likely contributing to the ongoing debate as to whether or not cognitive training is effective. Different approaches have varying effects that are also dependent upon the sample characteristics.
Interestingly, only speed of processing booster sessions resulted in additional benefit for transfer to reducing rates of driving cessation. In ACTIVE, a key difference of speed of processing training, as compared to the reasoning or memory training, was that the last five training sessions and all booster sessions included exercises that were fully adaptive in difficulty to individual participant performance. In fact, ACTIVE results indicated far transfer of speed of processing training to improved IADL performance after nine sessions of adaptive training, with performance gains enduring at 5 years (Willis et al., 2006). Other studies of speed of processing training using only adaptive techniques among samples with poor baseline UFOV® performance showed immediate transfer to improved IADL performance and driving safety (Edwards et al., 2005; Roenker et al., 2003). It is increasingly clear that a key feature of effective cognitive training interventions is the use of adaptive techniques (Kelly et al., 2014; Lövdén et al., 2010). These techniques ensure that task difficulty is maintained at an intensity that is sufficiently challenging, but not so difficult that it becomes frustrating (Kelly et al., 2014; Lövdén et al., 2010).
Although strategy-based reasoning training transfered to maintained driving mobility in the at-risk subsample, additional reasoning training through booster sessions did not demonstrate such transfer. There were no benefits derived from strategy-based memory training. Thus, in addition to the effects of baseline cognitive status varying by intervention approach, the amount and technique of training necessary to derive benefits varies by training approach.
A main limitation of the current study is the healthy sample. ACTIVE purposely recruited healthy adults to increase the likelihood that participants would be available for follow-up assessments. Thus, the sample may not be representative of older adults overall. This is particularly important given that training benefit was conferred to the subsample of participants with poor baseline UFOV® performance (which equated to 28% of the total sample). Such individuals may be more prevalent in the general population. Given the healthy sample, another limitation of these analyses is the relatively low driving cessation rate, which limited statistical power.
The underlying mechanisms of training transfer are not known. To the best of our knowledge, there are no studies examining the mechanisms of reasoning training. Three studies have examined the mechanisms of speed of processing training through mediation analyses and by measuring neurophysiological effects. O’Brien and colleagues found that speed of processing training may be effective by enhancing attention 2013. Training effects were not explained by improvements in self-efficacy (Sharpe et al., 2014). Interestingly, although the debate about cognitive training stems from lack of transfer to broader cognitive abilities, improvements in the divided attention subtest of the UFOV® completely accounted for the transfer to improved IADL performance (Edwards et al., 2013). Future work should determine mediators of training transfer.
Clearly, there are different patterns of transfer from cognitive training approaches. The amount and timing of training needed to derive benefits may differ by intervention type. The individuals who benefit from such approaches may also vary. Future research should investigate the common and unique mechanisms and moderators of successful cognitive interventions. A better understanding of these important factors will allow for refinement of effective cognitive interventions.
In summary, this is the first study to compare the effects of three different cognitive training programs on rates of driving cessation across 10 years. Results revealed that two cognitive training programs reduced driving cessation among individuals at-risk for driving mobility declines. These results add evidence of long-lasting cognitive training transfer effects. Although the field of cognitive training is often critiqued due to lack of transfer to everyday function, most studies have not assessed the longitudinal effects on functional outcomes (Kelly et al., 2014). These results add to evidence that process-based cognitive speed of processing training and strategy-based reasoning training transfers to several indices of driving safety and mobility (Ball et al., 2010; Edwards, Delahunt, et al., 2009; Edwards, Myers, et al., 2009; Roenker et al., 2003; Ross et al., 2016), particularly among at-risk subsamples and with use of adaptive techniques. Furthermore, increasing evidence that reasoning training also longitudinally transfers to improved driving safety and mobility is emerging (Ball et al., 2010). There is mounting evidence that some types of cognitive training transfer to improved health, well-being (Wolinsky, Mahncke, et al., 2009; Wolinsky, Vander Weg, et al., 2009) and everyday function (i.e., IADL performance; Ball et al., 2010; Edwards et al., 2005; Rebok et al., 2014; Ross et al., 2016). The potential for these cognitive interventions to prolong driving mobility of older adults most susceptible to decline has significant societal and quality of life implications. Thus, the reasoning and speed of processing training used in these analyses should be recommended to older adults at risk for mobility decline due to cognitive difficulties.
Funding
This work was supported by the National Institute on Aging and the National Institute of Nursing Research to Hebrew Senior Life (U01 NR04507); Indiana University School of Medicine (U01 NR04508); Johns Hopkins University (U01AG14260); New England Research Institutes (U01 AG14282); Pennsylvania State University (U01 AG14263); University of Alabama at Birmingham (U01 AG14289); and University of Florida (U01AG14276). These analyses were supported by the National Institute on Aging, Cognitive Training Gains and Mobility Outcomes in ACTIVE (5 R03 AG23078-02).
Acknowledgments
The authors would like to acknowledge the entire ACTIVE team. The ACTIVE principal investigators included: Karlene Ball, PhD; Richard N. Jones, ScD; Jonathan W. King, PhD; Michael Marsiske, PhD; John Morris, PhD; George Rebok, PhD; Sharon Tennstedt, PhD; Frederick W. Unverzagt, PhD; and Sherry Willis, PhD. K. Ball owns stock in the Visual Awareness Research Group (formerly Visual Awareness, Inc.), and Posit Science, Inc., the companies that market the Useful Field of View Test and speed of processing training software. Posit Science acquired Visual Awareness, and K. Ball continues to collaborate on the design and testing of these assessment and training programs as a member of the Posit Science Scientific Advisory Board. J. D. Edwards has worked as a limited consultant to Posit Science, Inc. and currently serves on Data Safety Monitoring Boards for Posit Science investigators. No other authors have a financial disclosure or conflict of interest.
References
- Anstey K. J. Windsor T. D. Luszcz M. A., & Andrews G. R (2006). Predicting driving cessation over 5 years in older adults: Psychological well-being and cognitive competence are stronger predictors than physical health. Journal of the American Geriatrics Society, 54, 121–126. doi:10.1111/j.1532-5415.2005.00471.x [DOI] [PubMed] [Google Scholar]
- Ball K. Edwards J. D., & Ross L. A (2007). The impact of speed of processing training on cognitive and everyday functions. The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 62 (Spec No 1), 19–31. [DOI] [PubMed] [Google Scholar]
- Ball K. Edwards J. D. Ross L. A., & McGwin G. Jr (2010). Cognitive training decreases motor vehicle collision involvement of older drivers. Journal of the American Geriatrics Society, 58, 2107–2113. doi:10.1111/j.1532-5415.2010.03138.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K. K., & Roenker D. L (2014). The useful field of view user’s manual (7.1.0 ed.). Punta Gorda, FL: Visual Awareness Research Group, Inc. [Google Scholar]
- Ball K. K. Ross L. A. Roth D. L., & Edwards J. D (2013). Speed of processing training in the ACTIVE study: How much is needed and who benefits? Journal of Aging and Health, 25(8 Suppl), 65S–84S. doi:10.1177/0898264312470167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissig D., & Lustig C (2007). Who benefits from memory training? Psychological Science, 18, 720–726. doi:10.1111/j.1467-9280.2007.01966.x [DOI] [PubMed] [Google Scholar]
- Dugan E., & Lee C. M (2013). Biopsychosocial risk factors for driving cessation: Findings from the Health and Retirement Study. Journal of Aging and Health, 25, 1313–1328. doi:10.1177/0898264313503493 [DOI] [PubMed] [Google Scholar]
- Edwards J. D. Bart E. O’Connor M. L., & Cissell G (2009). Ten years down the road: Predictors of driving cessation. The Gerontologist, 50, 393–399. doi:10.1093/geront/gnp127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Delahunt P. B., & Mahncke H. W (2009). Cognitive speed of processing training delays driving cessation. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 64, 1262–1267. doi:10.1093/gerona/glp131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Lunsman M. Perkins M. Rebok G. W., & Roth D. L (2009). Driving cessation and health trajectories in older adults. Journals of Gerontology: Series A, Medical Science, 64, 1290–1295. doi:10.1093/gerona/glp114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Myers C. Ross L. A. Roenker D. L. Cissell G. M. McLaughlin A. M., & Ball K. K (2009). The longitudinal impact of cognitive speed of processing training on driving mobility. The Gerontologist, 49, 485–494. doi:10.1093/geront/gnp042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Perkins M. Ross L. A., & Reynolds S. L (2009). Driving status and three-year mortality among community-dwelling older adults. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 64, 300–305. doi:10.1093/gerona/gln019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Ross L. A. Ackerman M. L. Small B. J. Ball K. K. Bradley S., & Dodson J. E (2008). Longitudinal predictors of driving cessation among older adults from the ACTIVE clinical trial. Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 63, P6-P12. doi:10.1093/geronb/63.1.P6 [DOI] [PubMed] [Google Scholar]
- Edwards J. D. Ruva C. L. O’Brien J. L. Haley C. B., & Lister J. J (2013). An examination of mediators of the transfer of cognitive speed of processing training to everyday functional performance. Psychology and Aging, 28, 314–321. doi:10.1037/a0030474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D. Wadley V. G. Myers R. S. Roenker D. L. Cissell G. M., & Ball K. K (2002). Transfer of a speed of processing intervention to near and far cognitive functions. Gerontology, 48, 329–340. doi:10.1159/000065259 [DOI] [PubMed] [Google Scholar]
- Edwards J. D. Wadley V. G. Vance D. E. Wood K. Roenker D. L., & Ball K. K (2005). The impact of speed of processing training on cognitive and everyday performance. Aging & Mental Health, 9, 262–271. doi:10.1080/13607860412331336788 [DOI] [PubMed] [Google Scholar]
- Emerson J. L. Johnson A. M. Dawson J. D. Uc E. Y. Anderson S. W., & Rizzo M (2012). Predictors of driving outcomes in advancing age. Psychology and Aging, 27, 550–559. doi:10.1037/a0026359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman E. E. Gange S. J. Muñoz B., & West S. K (2006). Driving status and risk of entry into long-term care in older adults. American Journal of Public Health, 96, 1254–1259. doi:10.2105/AJPH.2005.069146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobe J. B. Smith D. M. Ball K. Tennstedt S. L. Marsiske M. Willis S. L.,…Kleinman K (2001). ACTIVE: A cognitive intervention trial to promote independence in older adults. Controlled Clinical Trials, 22, 453–479. doi:10.1016/S0197-2456(01)00139-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly M. E. Loughrey D. Lawlor B. A. Robertson I. H. Walsh C., & Brennan S (2014). The impact of cognitive training and mental stimulation on cognitive and everyday functioning of healthy older adults: A systematic review and meta-analysis. Ageing Research Reviews, 15, 28–43. doi:10.1016/j.arr.2014.02.004 [DOI] [PubMed] [Google Scholar]
- Lövdén M. Backman L. Lindenberger U. Schaefer S., & Schmiedek F (2010). A theoretical framework for the study of adult cognitive plasticity. Psychological Bulletin, 136, 659–676. doi:10.1037/a0020080 [DOI] [PubMed] [Google Scholar]
- Marottoli R. A. Mendes de Leon C. F. Glass T. A. Williams C. S. Cooney L. M. Berkman L. F., & Tinetti M. E (1997). Driving cessation and increased depressive symptoms: Prospective evidence from the New Haven EPESE. Journal of the American Geriatrics Society, 45, 202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x [DOI] [PubMed] [Google Scholar]
- Mezuk B., & Rebok G. W (2008). Social integration and social support among older adults following driving cessation. Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 63B, S298–S303. doi:10.1093/geronb/63.5.S298 [DOI] [PubMed] [Google Scholar]
- O’Brien J. L. Edwards J. D. Maxfield N. D. Peronto C. L. Williams V. A., & Lister J. J (2013). Cognitive training and selective attention in the aging brain: An electrophysiological study. Clinical Neurophysiology, 124, 2198–2208. doi:10.1016/j.clinph.2013.05.012 [DOI] [PubMed] [Google Scholar]
- O’Connor M. L. Edwards J. D. Small B. J., & Andel R (2012). Patterns of level and change in self-reported driving behaviors among older adults: Who self-regulates? J Gerontol B Psychol Sci Soc Sci, 67, 437–446. doi:10.1093/geronb/gbr122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owsley C. Stalvey D. Wells J., & Sloane M. E (1999). Older drivers and cataract: Driving habits and crash risk. Journals of Gerontology: Medical Sciences, 54A, M203–M211. doi:10.1093/gerona/54.4.M203 [DOI] [PubMed] [Google Scholar]
- Peng H. Wen J. Wang D., & Gao Y (2012). The impact of processing speed training on working memory in old adults. J Adult Dev, 19, 150–157. doi:10.1007/s10804-012-9142-6 [Google Scholar]
- Ragland D. R. Satariano W. A., & MacLeod K. E (2005). Driving cessation and increased depressive symptoms. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 60A, 399–403. doi:10.1093/gerona/60.3.399 [DOI] [PubMed] [Google Scholar]
- Rebok G. W. Ball K. K. Guey L. T. Jones R. N. Kim H.-Y. King J. W.,…Willis S. L (2014). Ten year effects of the Advanced Cognitive Training for Independent and Vital Elderly cognitive training trial on cognition and everyday functioning in older adults. Journal of the American Geriatrics Society, 62, 16–24. doi:10.1111/jgs.12607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebok G. W. Langbaum J. B. Jones R. N. Gross A. L. Parisi J. M. Spira A. P.,…Brandt J (2013). Memory training in the ACTIVE study: How much is needed and who benefits? Journal of Aging and Health, 25(8 Suppl), 21S–42S. doi:10.1177/0898264312461937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenker D. L. Cissell G. M. Ball K. K. Wadley V. G., & Edwards J. D (2003). Speed-of-processing and driving simulator training result in improved driving performance. Human Factors, 45, 218–233. [DOI] [PubMed] [Google Scholar]
- Ross L. A. Clay O. J. Edwards J. D. Ball K. K. Wadley V. G. Vance D. E.,…Joyce J. J (2009). Do older drivers at-risk for crashes modify their driving over time? The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 64, 163–170. doi:10.1093/geronb/gbn034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L. A. Edwards J. D. O’Connor M. L. Ball K. K. Wadley V. G., & Vance D. E (2016). The transfer of cognitive speed of processing training to older adults’ driving mobility across 5 years. The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 71, 87–97. doi:10.1093/geronb/gbv022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A. McGuckin N. Nakamoto H. Y. Gray D., & Liss S (2011). Summary of Travel Trends: 2009 National Household Travel Survey. Washington, DC: U.S. Department of Transportation Federal Highway Administration. [Google Scholar]
- Sharpe C. Holup A. A. Hansen K. E., & Edwards J. D (2014). Does self-efficacy affect responsiveness to cognitive speed of processing training? Journal of Aging and Health, 26, 786–806. doi:10.1177/0898264314531615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson T. Camfield D. Pipingas A. Macpherson H., & Stough C (2012). Improved processing speed: Online computer-based cognitive training in older adults. Educational Gerontology, 38, 445–458. doi:10.1080/03601277.2011.559858 [Google Scholar]
- Vance D. E. Roenker D. L. Cissell G. M. Edwards J. D. Wadley V. G., & Ball K. K (2006). Predictors of driving exposure and avoidance in a field study of older drivers from the state of Maryland. Accident Analysis and Prevention, 38, 823–831. doi:10.1016/j.aap.2006.02.008 [DOI] [PubMed] [Google Scholar]
- Willis S. L., & Caskie G. I (2013). Reasoning training in the ACTIVE study: How much is needed and who benefits? Journal of Aging and Health, 25(8 Suppl), 43S–64S. doi:10.1177/0898264313503987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis S. L. Tennstedt S. Marsiske M. Ball K. K. Elias J. Koepke K. M.,…Wright E (2006). Long-term effects of cognitive training on everyday functional outcomes in older adults. Journal of the American Medical Association, 296, 2805–2814. doi:10.1001/jama.296.23.2805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D. Mahncke H. Vander Weg M. W. Martin R. Unverzagt F. W. Ball K.,…Tennstedt S (2010). Speed of processing training protects self-rated health in older adults: Enduring effects observed in the multi-site ACTIVE randomized controlled trial. International Psychogeriatrics, 22, 470–478. doi:http://dx.doi.org/10.1017/S1041610209991281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D. Mahncke H. W. Kosinski M. Unverzagt F. W. Smith D. M. Jones R. N.,…Tennstedt S. L (2009). The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Services Research, 9, 109. doi:10.1186/1472-6963-9-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D. Unverzagt F. W. Smith D. M. Jones R. Stoddard A., & Tennstedt S. L (2006). The ACTIVE cognitive training trial and health-related quality of life: Protection that lasts for 5 years. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 61, 1324–1329. [DOI] [PubMed] [Google Scholar]
- Wolinsky F. D. Vander Weg M. W. Martin R. Unverzagt F. W. Ball K. K. Jones R. N., & Tennstedt S. L (2009). The effect of speed-of-processing training on depressive symptoms in ACTIVE. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 64, 468–472. doi:10.1093/gerona/gln044 [DOI] [PMC free article] [PubMed] [Google Scholar]