Abstract
Objective
The purpose of this study was to evaluate the intraexaminer and interexaminer reliability of image assessment of infrared thermography of the plantar surface of people with diabetes mellitus.
Methods
Fifty-one participants with diabetes were included. The interexaminer reliability (test) consisted of measuring the temperature of the plantar surface by 2 evaluators who separately performed the analysis of thermographic images. The intraexaminer reliability (retest) consisted of the revaluation of the images by a single evaluator 10 days after the first analysis.
Results
The analysis of intrareliability and interreliability indicated excellent levels of correlation (intraclass correlation coefficient >0.75, 95% confidence interval >0.70) in the plantar surface points analyzed.
Conclusion
Infrared thermography image evaluation identified intrareliability and interreliability for temperature analysis of the plantar surface of people with diabetes mellitus. However, further studies need to be conducted to assess validity and its application in health care.
Key Indexing Terms: Body Temperature, Diabetic Foot, Lower Limbs, Reproducibility of Results
Introduction
Infrared thermography is based on the emission of infrared radiation from a particular object or region as seen through a thermographic camera.1, 2, 3 This instrument enables the detection of the heat distribution on the surface and at the same time allows the measurement of peripheral temperature.2, 3, 4 After capturing the image, one can obtain a record of temperature gradients in colorful hues and enable the computational analysis of the quantification and interpretation of the image.3 This method allows the measurement of the average temperature, the temperature difference and thermal recovery rate.5 Researchers interested in investigating the use of infrared thermography in health care have reported the benefit of the method in the evaluation of musculoskeletal disorders, diabetic neuropathy, and vasculopathy.1, 3, 4, 6, 7, 8, 9, 10 Other studies have been conducted to test the use of thermography in detecting problems related to gynecology and obstetrics, neonatology, cardiology, nephrology, neurology, and dermatology.4, 6, 7, 11, 12, 13 This method has been used to diagnose disease and monitor various clinical conditions.1, 4, 10 The detection of small changes in temperature in specific regions may suggest corresponding changes in the physiology, which contributes to the screening, diagnosis, and treatment of various diseases.1, 6, 7, 8, 9, 10
Body temperature, mediated by sensory innervation and peripheral circulation, is directly influenced by room temperature.11 In the presence of local lesions, impairment occurs in perception and thermal regulation, which promotes metabolic and physiological changes in an organism.11, 12 In this sense, a person with diabetes mellitus presents with damage in peripheral nerves and blood vessels and has a reduction in lower limb temperature.12, 13 This can be explained by the involvement of regulatory mechanisms: neurovegetative and motor mechanisms of blood vessels, resulting in the reduction of vasomotor function and lifting or lowering the temperature of the feet.14 Acquired neuropathy exposes the individual to a higher probability of complications in different body regions, especially in the extremities, and increased risk of developing skin lesions, resulting in high costs of hospitalization and medical expenses.15
Infrared thermography, as a noninvasive method, measures changes in the peripheral body temperature,8, 10, 16 maps body temperature,11 and tracks changes that decrease or increase body temperature.1, 2, 3, 8 However, because it is a new methodology in health care, its applicability and effectiveness as a method of evaluation need further testing.4 Few studies have reported the intrarater and interrater reliability of this instrument.
Therefore, the purpose of this study was to assess the intrarater and interrater reliability of infrared thermography in the analysis of the plantar surface temperature of people with diabetes mellitus.
Methods
This was a cross-sectional study. A test–retest design was used to evaluate the intraexaminer and interexaminer reliability of the temperature measured by the infrared thermography. This study was part of a larger project titled “The Use of Reflexology Feet as Treatment for Patients With Diabetes Mellitus.” This was approved by the Ethics Committee of the Federal University of Alfenas, Minas Gerais, Brazil (CAAE: 07183512.1.00005142).
Population and Sample
Fifty-one participants with type 2 diabetes mellitus from 2 primary health care units participated. The following were inclusion criteria: diagnosis of the disease for at least 5 years, minimum age of 18 years old, both sexes, infrequent medical monitoring for diabetes control in 2 primary health care units. Exclusion criteria were presence of ulcers, presence of amputations of the lower limbs, uncontrolled hypertension, thrombosis, presence of burns, and fever.
The following guidelines were given to the participants before the examination: Avoid alcohol 24 hours before the examination, caffeine and cigarettes 2 hours before the examination, vigorous sports activities on examination day, and the use of lotions or powders on your feet on examination day.17, 18 All participants gave consent to participate.
Photographic Record
For thermographic recording, the participants were positioned supine with bare feet and held that position for 15 minutes. This amount of time was used because it is the time required for the body heat to come into balance with the environment and produce stable recordings.19 During this period, participants avoided touching their feet, and all electronics that could compromise the evaluation were removed. The testing environment was thermally controlled at a constant temperature of 23°C.17, 20 To obtain stable interpretations of plantar temperature and to prevent that the temperature of other parts of the body interfering on the photographic record, the feet were thermally insulated by a uniform backdrop.18 This uniform backdrop consisted in a box with 2 openings for the feet.
All participants had their feet photographed with an infrared thermal camera (FLIR, model E60, Wilsonville, Oregon), with emissivity set to 0.98.4 According to the manufacturer, this device enables measurement of temperatures ranging from –120°C to 650°C. The equipment was positioned on a tripod at a standardized height of 0.95 m from the ground and at a distance of 0.98 m from the participants’ feet, which provided a picture without distortion. All photographic records were performed by a single observer who was familiar with the camera.
Reliability of Infrared Thermography
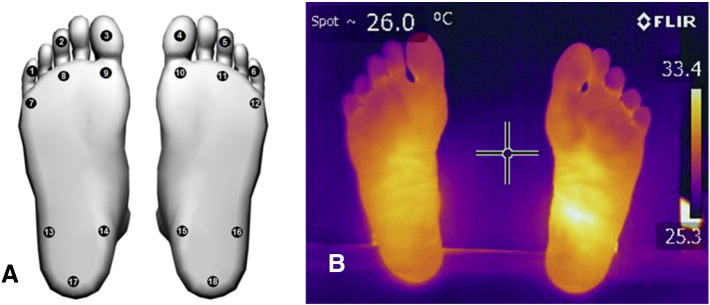
To assess intraexaminer reliability, a single evaluator analyzed thermographic images of the 18 points shown in Figures 1A and 1B on 2 different occasions. Respecting an interval of time for the data storage was not possible. The first evaluation was conducted on the day the images were captured by the thermographic camera, and the second evaluation was conducted after 10 days. The Quick Report Software Version 1.1 (FLIR Systems) that was provided by the camera’s manufacturer was used for these analyses.
Fig 1.
(A) The 18 points used for the study. (B) A sample thermographic image.
To assess interrater reliability, the image analysis was performed by 2 different evaluators in different locations and with different computers. Therefore, there was no exchange of information between examiners that could interfere with the assessments. Results were recorded separately to avoid the comparison of data during the analysis.
Statistical Analysis
We calculated sample size using G*Power Software Version 3.1.7 (Christian-Albrechts-Universität Kiel, Kiel, Germany) that estimated the need for 12 participants for a power of 0.80. The intraexaminer result concordance was analyzed by means of the intraclass correlation coefficient (ICC), assessing the measure consistency by each rater in 2 evaluations, whereas the interexaminer result concordance was analyzed by means of ICC, considering the between-rater concordance at the 2 time intervals for 1 measure assessed. The interpretation of the ICC was according to Fleiss (<0.40, poor correlation; 0.40-0.75, moderate correlation; >0.75, excellent correlation).21 The 95% confidence interval (CI) was calculated, with values >0.70 being considered excellent.22, 23 The calculation of the standard error of measurement (SEM) was performed using the following formula: SEM = SD × √(1 – ICC), wherein SD corresponds to the standard deviation.24 Minimum detectable change (MDC) was calculated with the following formula: MDC = z score level of confidence × SD baseline × √(2[1 – test-retest]). In this study, CI = 95%; z = 1.96.23 Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) Version 19.0 (IBM Corp., Armonk, New York). A significance level (α) of .05 was used for all tests.
Results
The sample consisted of 51 people with diabetes mellitus (mean time since diagnosis of diabetes 10 years [SD = 6, 16]), with a mean age of 61.5 years (SD = 9.8), mean weight of 75.11 kg (SD = 13.05), mean height of 1.63 m (SD = 0.2), and 63.5% women and 36.5% men. Other patient characteristics are described in Table 1.
Table 1.
Patient Characteristics (N = 51)
| Patient Characteristics | Yes (%) | No (%) | ||
|---|---|---|---|---|
| Smoker | 15.55 | 84.44 | ||
| Hypertension | 82.22 | 17.77 | ||
| Practices physical activity | 33.34 | 66.66 | ||
| Feet assessment by a health professional | 20.00 | 80.00 | ||
| Counseling on self-care for the feet | 35.56 | 64.44 | ||
| Risk rating analysis | Low | Moderate | High | 55.55 |
| 24.44 | 15.55 | 4.44 | ||
| Glycemic control | Oral hypoglycemic | Insulin | ||
| 91.11 | 8.88 | |||
Rows may not equal 100% due to rounding.
Reliability of Infrared Thermography
The assessment of the 18 points indicated excellent correlation in both the intraexaminer and interexaminer analysis (ICC >0.75; 95% CI >0.70; P < .01). This analysis may be due to the results obtained and the MDC, which represents good stability through repeated testing.23 All values obtained in the intra-analyses and interanalyses are described in Table 2.
Table 2.
Analysis of Intraexaminer and Interexaminer Reliability of Infrared Thermography
| Points | Temperature (°C) |
Intraexaminer |
Interexaminer |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1st Examiner | 2nd Examiner | Retest 1st Examiner | ICC | Level | SEM | 95% CI | MDD | ICC | Level | SEM | 95% CI | MDD | |
| 1 | 29.40 ± 3.41 | 29.35 ± 3.43 | 29.39 ± 3.42 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.10 | 0.99-0.99 | 0.30 |
| 2 | 29.47 ± 3.70 | 29.46 ± 3.76 | 29.39 ± 3.66 | 0.99 | Excellent | 0.23 | 0.99-0.99 | 0.64 | 0.99 | Excellent | 0.11 | 0.99-1.00 | 0.33 |
| 3 | 30.21 ± 3.38 | 30.21 ± 3.39 | 30.20 ± 3.38 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.10 | 0.99-0.99 | 0.29 |
| 4 | 30.03 ± 3.33 | 30.03 ± 3.37 | 30.03 ± 3.33 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.10 | 0.99-1.00 | 0.29 |
| 5 | 29.38 ± 3.70 | 29.32 ± 3.73 | 29.37 ± 3.70 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.11 | 0.99-1.00 | 0.32 |
| 6 | 29.51 ± 3.36 | 29.46 ± 3.37 | 29.51 ± 3.36 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.10 | 0.99-1.00 | 0.29 |
| 7 | 29.90 ± 3.36 | 30.20 ± 2.88 | 29.90 ± 3.02 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.94 | Excellent | 0.73 | 0.89-0.96 | 2.05 |
| 8 | 30.55 ± 2.83 | 30.55 ± 2.81 | 30.56 ± 2.84 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.15 | 0.99-0.99 | 0.43 |
| 9 | 30.83 ± 2.71 | 30.88 ± 2.71 | 30.81 ± 2.71 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.08 | 0.99-0.99 | 0.23 |
| 10 | 30.73 ± 2.70 | 30.78 ± 2.70 | 30.74 ± 2.69 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.12 | 0.99-0.99 | 0.33 |
| 11 | 30.55 ± 2.74 | 30.56 ± 2.73 | 30.55 ± 2.75 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.08 | 0.99-0.99 | 0.24 |
| 12 | 30.22 ± 2.71 | 30.28 ± 2.77 | 30.22 ± 2.70 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.15 | 0.99-0.99 | 0.42 |
| 13 | 30.40 ± 2.41 | 30.53 ± 2.44 | 30.39 ± 2.39 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.98 | Excellent | 0.31 | 0.97-0.99 | 0.88 |
| 14 | 30.56 ± 2.32 | 31.45 ± 1.82 | 30.56 ± 2.32 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.94 | Excellent | 0.53 | 0.90-0.96 | 1.49 |
| 15 | 30.38 ± 2.47 | 31.30 ± 1.82 | 30.34 ± 2.45 | 0.99 | Excellent | 0.15 | 0.99-0.99 | 0.43 | 0.94 | Excellent | 0.58 | 0.89-0.96 | 1.63 |
| 16 | 30.29 ± 2.49 | 30.38 ± 2.36 | 30.29 ± 2.48 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.98 | Excellent | 0.34 | 0.96-0.98 | 0.95 |
| 17 | 29.97 ± 2.58 | 30.48 ± 2.57 | 29.96 ± 2.57 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.24 | 0.98-0.99 | 0.67 |
| 18 | 29.80 ± 2.65 | 30.31 ± 2.56 | 29.81 ± 2.63 | 1.00 | Excellent | 0.00 | 1.00-1.00 | 0.00 | 0.99 | Excellent | 0.22 | 0.98-0.99 | 0.61 |
The table presents the result consistency for each rater. The mean as well as standard deviation of the values obtained in each assessment session and by each rater are presented, in addition to the intraclass correlation coefficient (ICC3), confidence interval (CI), standard error of measurement (SEM), and minimal detectable change (MDC).17, 18
Discussion
The results of this study indicate that infrared thermography, when used by the same person at different times and by another examiner, is a reliable method for assessing images of plantar surface temperature of people with diabetes mellitus. The MDC and the minimum clinically important changes it aims to measure include the effects and cost of treatments, clinical relevance, and tolerability of treatment choices.25 In the present study, the interpretation of MDC indicates that the results are clinically significant because of the low values identfied.23, 26
These findings may inform the selection of interventions or contribute to reduction of financial expenses with the clinical evaluation process.23 Some studies have used infrared thermography as an evaluation method19, 27, 28 and relate its reliability and validation to certain clinical conditions.5, 28, 29
For analysis of foot temperature of people diagnosed with diabetes mellitus, only 1 study investigated the thermal recovery of the feet after cooling was identified. Another study pointed out that thermography was reliable, suitable for the evaluation of peripheral circulation, and could be used to monitor the treatment of people with diabetes mellitus.19 Thermography has been used to study the variation of plantar temperatures in patients with diabetes and those without diabetes27 and for the early evaluation of neuropathy. However, not all studies perform reliability analyses or instrument validation.13 Thermographic imaging could possibly be used to assess infections in people with diabetic foot, facilitate early evaluation of the feet, and observe for signs of infection.16, 30 Moreover, it can be an additional tool for the diagnosis of diabetic neuropathy and several other pathologic conditions.13, 14 Infrared thermography may be a reliable instrument for measuring signs of temperature increase or decrease as well as for signal evaluation of inflammation.5, 29, 31
For reliability analysis and validation of infrared thermography, it is important to use adequate instruments.32 Professionals responsible for thermographic analyses should be properly trained, and recommendations issued by the literature should be followed with the utmost rigor possible.32, 33, 34 Further requirements include the presence of a thermally controlled environment, the proper preparation and orientation of the person who will undergo analysis, and the standardization of the technique with respect to the intervals of analysis, and completion of independent instruments by investigators.13, 17, 20
Limitations
We did not control for the menstrual cycle period with female volunteers, and this may have influenced the findings. It is known that there is influence of menstruation on the surface skin temperature. Infrared thermography has yet to be reported as a valid instrument to detect the surface temperature of the skin on the feet of people with type 2 diabetes mellitus. This study did not correlate results with clinical data and physical examination or other tests; thus, clinical relevance has yet to be proven.
Conclusion
According to the results of this study, intraexaminer and interexaminer reliability was good for the analysis of infrared thermography images of the plantar surface temperature of people with diabetes mellitus.
Funding Sources and Conflicts of Interest
This work was carried out with the financial support of The National Council of Technological and Scientific Development (Process nos. 477383/2012-2), the Oncology Network of the State of Minas Gerais–FAPEMIG, under RED-11-14 and Tutorial Education Program MEC–SESu. No conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): N.C.M.S., H.A.C., L.C.C., E.C.L.C., L.O.R., D.H.I.
Design (planned the methods to generate the results): N.C.M.S., H.A.C., L.C.C., E.C.L.C., L.O.R., D.H.I.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): N.C.M.S., H.A.C., L.C.C., D.H.I.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): N.C.M.S., H.A.C., D.H.I.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): N.C.M.S., H.A.C., L.C.C., D.H.I.
Literature search (performed the literature search): N.C.M.S., H.A.C., L.C.C., E.C.L.C., L.O.R., D.H.I.
Writing (responsible for writing a substantive part of the manuscript): N.C.M.S., H.A.C., L.C.C., D.H.I.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): N.C.M.S., H.A.C., L.C.C., E.C.L.C., L.O.R., D.H.I.
Practical Applications
-
•
The analysis of intrareliability and interreliability indicated excellent levels of correlation (ICC >0.75, 95% CI >0.70) in the plantar surface points analyzed.
-
•
Further studies should be conducted to ensure validity and greater reliability of the method and its application in health care.
Alt-text: Image 1
References
- 1.Hernandez-Contreras D, Peregrina-Barreto H, Rangel-Magdaleno JJ, Gonzalez JA. Narrative review: diabetic foot and infrared thermography. Infrared Phys Technol. 2016;78:105–117. [Google Scholar]
- 2.Weerd L, Mercer JB, Weum S. Dynamic infrared thermography. Clin Plast Surg. 2011;28(2):277–292. doi: 10.1016/j.cps.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Irace A. Infrared thermography application to functional and failure analysis of electron devices and circuits. Microel Reliab. 2012;52(1):2019–2023. [Google Scholar]
- 4.Lahiri BB, Bagavathiappan S, Jayakumar T, Philip J. Medical applications of infrared thermography: a review. Infrared Phys Technol. 2012;55(1):221–235. doi: 10.1016/j.infrared.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Bigaton D, Filho AVD, Costa ACS, Packer AC, Castro EM. Accuracy and reliability of infrared thermography in the diagnosis of arthralgia in women with temporomandibular disorder. J Manipulative Physiol Ther. 2013;36(4):253–258. doi: 10.1016/j.jmpt.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 6.Brioschi ML, Yeng LT, Pastor EMH, Teixeira MJ. Infrared imaging use in rheumatology. Rev Bras Reumatol. 2007;47(9):42–51. [Google Scholar]
- 7.Sivanandam S, Anburajan M, Venkatraman B, Menaka M, Sharath D. Medical thermography: a diagnostic approach for type 2 diabetes based on non-contact infrared thermal imaging. Endocrine. 2012;42(2):343–351. doi: 10.1007/s12020-012-9645-8. [DOI] [PubMed] [Google Scholar]
- 8.Staffa E, Bernard V, Kubíček L. Using noncontact infrared thermography for long-term monitoring of foot temperatures in a patient with diabetes mellitus. Ostomy Wound Manage. 2016;62(4):54–61. [PubMed] [Google Scholar]
- 9.Ring F. Thermal imaging today and its relevance to diabetes. J Diabetes Sci Technol. 2010;4(4):857–862. doi: 10.1177/193229681000400414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sousa P, Felizardo V, Oliveira D, Couto R, Garcia NM. A review of thermal methods and technologies for diabetic foot assessment. Expert Rev Med Devices. 2015;12(4):439–448. doi: 10.1586/17434440.2015.1032251. [DOI] [PubMed] [Google Scholar]
- 11.Lavery LA, Higgins KR, Lanctot DR. Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring a self-assessment tool. Diabetes Care. 2007;30(1):14–20. doi: 10.2337/dc06-1600. [DOI] [PubMed] [Google Scholar]
- 12.Najafi B, Wrobel JS, Grewal G. Plantar temperature response to walking in diabetes with and without acute Charcot: The Charcot activity response test. J Aging Res. 2012;2012:1–5. doi: 10.1155/2012/140968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balbinot LF, Canani LH, Robinson CC, Achaval M, Zaro MA. Plantar thermography is useful in the early diagnosis of diabetic neuropathy. Clinics (São Paulo) 2012;67(12):1419–1425. doi: 10.6061/clinics/2012(12)12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balbinot LF, Robinson CC, Achaval M, Zaro MA, Brioschi ML. Repeatability of infrared plantar thermography in diabetes patients: a pilot study. J Diabetes Sci Technol. 2013;7(5):1130–1137. doi: 10.1177/193229681300700505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bagavathiappan S, Philip J, Jayakumar T. Correlation between plantar foot temperature and diabetic neuropathy: a case study by using an infrared thermal imaging technique. J Diabetes Sci Technol. 2010;4(6):1386–1392. doi: 10.1177/193229681000400613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hazenberg CEVB, Netten JJV, Baal SGV, Bus SA. Assessment of signs of foot infection in diabetes patients using photographic foot imaging and infrared thermography. Diabetes Technol Ther. 2014;16(6):370–377. doi: 10.1089/dia.2013.0251. [DOI] [PubMed] [Google Scholar]
- 17.Brioschi ML, Teixeira MJ, Yeng LT, Silva FMRM. Andreoli; São Paulo, Brazil: 2012. Manual of Medical Thermography. [Google Scholar]
- 18.Gatt A, Formosa C, Cassar K. Thermographic patterns of the upper and lower limbs: baseline data. Int J Vasc Med. 2015;15:831369. doi: 10.1155/2015/831369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roy R, Boucher JP, Comtois AS. Validity of infrared thermal measurements of segmental paraspinal skin surface temperature. J Manipulative Physiol Ther. 2006;29(2):150–155. doi: 10.1016/j.jmpt.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Leemans V, Destain M, Kilundu B, Dehombreux P. Evaluation of the performance of infrared thermography for on-line condition monitoring of rotating machines. Engineering. 2011;3(10):1030–1039. [Google Scholar]
- 21.Fleiss JL. The Design and Analysis of Clinical Experiments. John Wiley & Sons; New York, NY: 1986. Reliability of measurement; pp. 1–32. [Google Scholar]
- 22.Lexell JE, Downham DY. How to assess the reliability of measurements in rehabilitation. Am J Phys Med Rehabil. 2005;84(9):719–723. doi: 10.1097/01.phm.0000176452.17771.20. [DOI] [PubMed] [Google Scholar]
- 23.Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther. 2006;86(5):735–743. [PubMed] [Google Scholar]
- 24.Portney LG, Watkins MP. 3rd ed. Upper Saddle River, NJ; Pearson/Prentice Hall: 2009. Foundations of Clinical Research: Applications to Practice. [Google Scholar]
- 25.Kovacs FM, Abraira V, Royuela A. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet Disord. 2008;9(43):1–9. doi: 10.1186/1471-2474-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spooner J, Dressing SA, Meals DW. Minimum detectable change analysis. Tech Notes 7; 2011. 2011. http://www.bae.ncsu.edu/programs/extension/wqg/319monitoring/TechNotes/technote7_MDC.pdf Available at: Accessed March 19, 2016.
- 27.Mori T, Nagase T, Takehara K. Morphological pattern classification system for plantar thermography of patients with diabetes. J Diabetes Sci Technol. 2013;7(5):1102–1112. doi: 10.1177/193229681300700502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Denoble AE, Hall N, Pieper CF, Kraus VB. Patellar skin surface temperature by thermography reflects knee osteoarthritis severity. Clin Med Insights Arthritis Musculoskelet Disord. 2010;3(1):69–75. doi: 10.4137/CMAMD.S5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan JH, Ng EYK, Rajendra Acharya U, Chee C. Infrared thermography on ocular surface temperature: a review. Infrared Phys Technol. 2009;52(4):97–108. [Google Scholar]
- 30.Bharara M, Schoess J, Armstrong DG. Coming events cast their shadows before: detecting inflammation in the acute diabetic foot and the foot in remission. Diabetes Metab Res Rev. 2012;28:15–20. doi: 10.1002/dmrr.2231. suppl. [DOI] [PubMed] [Google Scholar]
- 31.Bouzida N, Bendada A, Maldague XP. Visualization of body thermoregulation by infrared imaging. J Therm Biol. 2009;34(3):120–126. [Google Scholar]
- 32.Kosus N, Kosus A, Duran M, Simavli S, Turhan N. Comparison of standard mammography with digital mammography and digital infrared thermal imaging for breast cancer screening. J Turkish-German Gynecol Assoc. 2010;11(3):152–157. doi: 10.5152/jtgga.2010.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bagavathiappan S, Saravanan T, Philip J. Infrared thermal imaging for detection of peripheral vascular disorders. J Med Phys. 2009;34(1):43–47. doi: 10.4103/0971-6203.48720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ratovoson D, Jourdan F, Huon V. Influence of gravity on the skin thermal behavior: Experimental study using dynamic infrared thermography. Skin Res Technol. 2013;19(1):397–408. doi: 10.1111/j.1600-0846.2012.00657.x. [DOI] [PubMed] [Google Scholar]