Abstract
Background
Despite the effectiveness of 12-step groups, most people reporting a prior alcohol use disorder (AUD) do not sustain involvement in such groups at beneficial levels. This highlights the need for research on other mutual help groups that address alcohol problems and may attract those who avoid 12-step groups. The current study addresses this need, offering outcome data from the first longitudinal, comparative study of 12-step groups and their alternatives: The Peer ALlternatives for Addiction (PAL) Study.
Methods
Adults with a lifetime AUD were surveyed at baseline (N=647), 6 months (81% response rate) and 12 months (83% response rate). Members of the largest known secular mutual help alternatives, namely Women for Sobriety (WFS), LifeRing, and SMART, were recruited in collaboration with group directors; current 12-step attendees were recruited from an online meeting hub. Online surveys assessed demographic and clinical variables; mutual help involvement; and alcohol and drug use and severity. Analyses involved multivariate logistic GEEs separately modelling alcohol abstinence, alcohol problems, and total abstinence across 6 and 12 months. Key predictors were baseline primary group affiliation (PGA); primary group involvement (PGI) at both baseline and 6 months; and the interaction between baseline PGA and 6-month PGI. The critical effects of interest were the interactions, expressing whether associations between changes in PGI from baseline to 6 months and substance use outcomes differed by primary group.
Results
None of the interactions between baseline PGA and 6-month PGI were significant, suggesting no differences in the efficacy of WFS, LifeRing, or SMART, vs. 12-step groups. Nevertheless, some PGA main effects emerged. Compared to 12-step members, those identifying SMART as their primary group at baseline fared worse across outcomes, and those affiliating with LifeRing showed lower odds of total abstinence. Still, these effects became nonsignificant when controlling for baseline alcohol recovery goal, suggesting that any group differences may be explained by selection of those with weaker abstinence motivation into LifeRing and (especially) SMART.
Conclusions
This study makes a valuable contribution in view of the extremely limited evidence on mutual help alternatives. Results tentatively suggest that WFS, LifeRing, and SMART are as effective as 12-step groups for those with AUDs, and that this population has the best odds of success when committing to lifetime total abstinence. An optimal care plan may thus involve facilitating involvement in a broad array of mutual help groups and supporting abstinence motivation.
1. Introduction
1.1. Research on Mutual Help Group Alternatives for those with Alcohol Use Disorders (AUDs)
Mutual help groups are an important resource for those unable or unwilling to attend formal treatment and a powerful source of support during and after treatment. Twelve-step groups, such as Alcoholics Anonymous (AA), are by far the most widely available mutual help groups for addiction, and they appear to be effective: A large slate of observational and quasi-experimental studies has consistently supported associations between participation in 12-step groups and better substance use outcomes and psychosocial functioning (Kaskutas, 2009; J. F. Kelly, Magill, & Stout, 2009; Timko, 2008; Tonigan, Toscova, & Miller, 1996) (Project MATCH Research Group, 1997, 1998). Nevertheless, many people find 12-step groups unappealing. Most people receiving treatment for an alcohol or drug use disorder do not sustain involvement in 12-step groups at levels where benefits can be expected (Cloud & Kingree, 2008; J. F. Kelly & Moos, 2003), even where encouraging 12-step involvement is the primary focus of treatment (Timko & Debenedetti, 2007; Timko, DeBenedetti, & Billow, 2006; Tonigan, Connors, & Miller, 2003). This suggests that 12-step groups are not an ideal match for many of those with substance use disorders. Twelve-step involvement tends to be particularly limited among those identifying as atheist, agnostic, or unsure (compared to spiritual or religious) (Kaskutas, Turk, Bond, & Weisner, 2003; Tonigan, Miller, & Schermer, 2002), and lower religiosity strongly predicts drop-out from 12-step groups (J. F. Kelly & Moos, 2003). Thus, secular mutual help alternatives may have potential to attract, and help, some of those who avoid or drop out of 12-step groups.
Unfortunately, research on the nature and effectiveness of the many alternatives to 12-step groups remains underdeveloped. AA now has a number of active, predominantly secular, abstinence-focused counterparts in the U.S., including Women for Sobriety (WFS), LifeRing Secular Recovery (LifeRing), and SMART Recovery (Self-Management and Recovery Training, or SMART); older alternatives include the largely defunct Secular Organization for Sobriety (SOS) and Rational Recovery (RR), no longer offering groups. A national survey targeting those in recovery from an alcohol problem (Kaskutas et al., 2014) found that 19–25% of those recruited from Craigslist, a treatment program, or a recovery organization had attended WFS, LifeRing, SOS, or SMART. Yet, research on these groups is extremely sparse, and there are no known longitudinal, comparative studies. Additional research on 12-step alternatives—and particularly secular alternatives—is sorely needed to provide professionals and the public with clear, evidence-based recommendations regarding which groups are effective.(Peele, Bufe, & Brodsky, 2000)
A few cross-sectional studies have separately described the memberships of WFS (Kaskutas, 1989, 1992, 1994, 1996a, 1996b, 1996c), SMART (Beck et al., 2017; P. J. Kelly, Deane, & Baker, 2015; O’Sullivan, Blum, Watts, & Bates, 2015), SOS (Connors & Dermen, 1996), and RR (Galanter, Egelko, & Edwards, 1993). These studies have helped to confirm that participants are indeed attracted to these groups by their more secular approaches (Connors & Dermen, 1996; Kaskutas, 1994), though results have provided limited information on efficacy Meanwhile, just one known observational study has examined associations between mutual help group involvement and substance use outcomes in a sample including both 12-step members and participants of at least one mutual help alternative. This cross-sectional study, led by Atkins and Hawdon (2007), sampled attendees of WFS (n=236), SMART (n=324), SOS (n=104), and 12-step groups (n=161). Results of controlled analyses revealed that greater group participation was associated with greater length of sobriety, while primary group choice was not. Results also showed that, while lower participant religiosity related to lower mutual help participation among 12-step and WFS attendees, religiosity was unrelated to participation among SMART attendees and negatively related to participation among SOS attendees. These findings speak again to the potential for alternative groups such as SMART and SOS to appeal to those low on religiosity, though the cross-sectional design clearly limits inferences regarding efficacy.
Additionally, one randomized trial offers some information on relationships between participation in SMART and substance use outcomes, though this trial was not designed to test the efficacy of SMART per se. In this study, Hester and colleagues (2013) examined the efficacy of a web-based intervention drawing on SMART principles (i.e., Overcoming Addictions) alone and in the context of SMART in-person meeting attendance: Participants were thus randomized to one of three conditions, including SMART (In-Person Meetings) Only, Overcoming Addictions Only, and SMART Plus Overcoming Addictions. Results showed positive relationships between SMART in-person meeting attendance and better substance use outcomes in the first condition. However, the study did not report on effects for SMART in-person meetings in the second condition, and associations with substance use outcomes were nonsignificant in the third. These inconclusive results highlight the need for further research on SMART and other alternatives.
1.2. The Current Study
The Peer Alternatives in Addiction (PAL) study aimed to address the research gap surrounding mutual help alternatives by offering the first longitudinal, comparative survey study of 12-step groups and the largest known secular, abstinence-based alternatives to AA now available in the U.S.: WFS, SMART, and LifeRing. Similar to AA, these groups all provide free, regular, in-person meetings. Each alternative has its own literature and protocol for change, but all three place some emphasis on experiential knowledge, devoting substantial portions of each meeting to discussion, and all three address both alcohol and drugs—with SMART also welcoming those with other addictions. Nationally, there are about 62 peer-led WFS meetings, 163 LifeRing meetings, and 874 SMART meetings (Humphreys, 2004; J. F. Kelly & White, 2012; LifeRing: Secular Recovery, 2016; SMART Recovery - Self Management for Addiction Recovery, 2016; Women for Sobriety, 2016); see Zemore et al. (2017) for complete descriptions of each. The PAL study sampled participants of each group longitudinally over a one-year period (baseline, 6 months, and 12 months) to examine membership characteristics and relationships between group involvement and substance use outcomes.
The current paper builds on published analyses of the baseline data, which compared respondents identifying WFS, LifeRing, SMART, and a 12-step group as their primary group (hereafter “members” of those groups) on demographics, clinical severity, and mutual help group participation, satisfaction, and cohesion (Zemore et al., 2017). This paper extends these findings to examine substance use outcomes across all three survey waves. The paper’s primary aim is to examine the comparative efficacy of WFS, LifeRing, SMART, and 12-step groups: that is, whether the benefits of a given level of mutual help group involvement for substance use outcomes over time are equivalent regardless of the participant’s choice of groups.1 In other words, we are interested in whether participants get the same “bang for their buck” for a given level of involvement in each of the mutual help alternatives, compared to 12-step groups. The paper’s secondary aim is to explore whether differences in alcohol recovery goal across groups contributed to differences in outcomes. We focus on alcohol abstinence and alcohol problems as primary outcomes, given that our sampling targeted those with lifetime AUD. Total abstinence from alcohol and drugs is a secondary outcome.
Both aims are framed as exploratory given the mixed evidence base to date. On the one hand, prior studies have generally suggested benefits for involvement in mutual help alternatives to AA. Toward this point, analyses of the baseline PAL data actually showed higher satisfaction and cohesion among WFS, LifeRing, and SMART members, vs. 12-step members (Zemore et al., 2017). Moreover, as described, prior cross-sectional studies have reported positive associations between length/intensity of involvement and length of sobriety for various 12-step alternatives (Atkins & Hawdon, 2007; Galanter et al., 1993). Third, evidence suggests that the mechanisms of action of 12-step groups are largely general and not 12-step specific, with the most powerful mechanisms being changes in social support (measured as increased support for abstinence, decreased support for drinking, and increased overall support) and others including abstinence motivation, abstinence self-efficacy, and coping skills (J. F. Kelly, 2017; J. F. Kelly et al., 2009). On the other hand, analyses of our baseline PAL data also suggested that LifeRing and SMART members have less stringent alcohol recovery goals than 12-step members: While large majorities of 12-step (72%) and WFS (67%) members endorsed a recovery goal of lifetime total abstinence, endorsement rates for this same goal were significantly lower among LifeRing members (58%) and lowest of all among SMART members (40%) (Zemore et al., 2017). This could imply worse outcomes for LifeRing and SMART, given that lower abstinence motivation predicts lower odds of abstinence in recovery from AUD (J. F. Kelly & Greene, 2014; Morgenstern, Frey, McCrady, Labouvie, & Neighbors, 1996; Satre, Mertens, Arean, & Weisner, 2003; Witbrodt & Romelsjö, 2012) and that social support for abstinence and abstinence motivation help drive the benefits of 12-step participation (J. F. Kelly et al., 2009).
Because of the mixed findings above, we declined to offer specific hypotheses, but constructed our aims and analyses with special focus on a possible role for recovery goal in participant outcomes. Specifically, we used sequential regressions to examine associations between recovery outcomes and mutual help group affiliation, mutual help group involvement, and their interactions with and without accounting for recovery goal at baseline. This allowed us to examine whether differential selection into mutual help groups as a function of recovery goal contributed to any differences across groups in outcomes through the 12-month follow-up.
2. Materials and Methods
2.1. Sample Recruitment and Characteristics
The Peer Alternatives in Addiction (PAL) Study is a longitudinal study with three waves of data collection (i.e., baseline, 6-month follow-up, and 12-month follow-up) incorporating online surveys of those reporting past-30-day in-person attendance at a 12-step group, WFS, LifeRing, or SMART at baseline. Surveys measured mutual help participation; substance use; psychiatric and clinical variables; and demographics, among other variables. Sample characteristics have been found to be generally similar to those of samples obtained via groups’ membership surveys (Zemore et al., 2017). A detailed description of the baseline recruitment methods, data cleaning, and sample is provided in Zemore et al. (2017).
Baseline respondents were recruited in the fall of 2015 via collaboration with the Executive Directors of WFS, LifeRing, and SMART; LifeRing’s Board Chair; and SMART’s President. These collaborators emailed meeting conveners and individual members directly; emailed flyers to conveners to distribute at meetings; and publicized the study via their webpages, social media (e.g., Facebook, Twitter), and at national conferences. A comparison sample of 12-step attendees was recruited by publicizing the study via paid advertisements on IntheRooms, an online meeting hub for those in recovery with a 12-step focus. IntheRooms has over 400,000 users across all U.S. states, with most (79%) reporting membership in AA, NA, and/or CA (In the Rooms: A Global Recovery Community, 2016). Study announcements included a brief study description and link to the study webpage. Interested parties who accessed the study webpage were linked to the online consent form and then online screener. All participants were required to be at least 18; be a U.S. resident; report a lifetime AUD; and report attending at least one in-person 12-step, WFS, LifeRing, or SMART meeting for alcohol/drug use in the past 30 days. Only participants whose screeners indicated that they met these criteria were advanced to the baseline survey.
Baseline data collection yielded 1064 “complete cases” (i.e., cases showing completion through the questions just preceding or including the final income questions). Extensive cleaning procedures were implemented on these 1064 cases to address and eliminate suspicious cases, as indicated by duplicate information, shared IP addresses, returned incentives, and major inconsistencies in survey responses, resulting in an initial baseline N of 651. All 651 baseline cases were then contacted by email and, if nonresponsive, by telephone and letter to complete their 6-month and 12-month surveys. For each follow-up, participants were provided with a unique survey link. Follow-ups yielded initial N’s of 528 at 6 months and 538 at 12 months. Follow-up surveys were further inspected for major inconsistencies, which resulted in the elimination of a final 4 cases, all indicating male gender and WFS participation. This yielded a final N=647 at baseline (208 12-step, 175 WFS, 98 LifeRing, and 166 SMART members); final N’s were 526 at 6 months (81% response rate) and 536 at 12 months (83% response rate). (Because additional cleaning procedures were implemented with follow-up data, the current baseline N differs from that in Zemore et al., 2017, with N=651.) Surveys were about 20–25 minutes in length, and participants received gift certificates of $25 for the baseline and $30 for each follow-up.
We compared those lost to follow-up at both 6 and 12 months to those retained on baseline demographics (i.e., gender, age, marital status, race/ethnicity, education, employment status, income, and religious identification), substance use variables (i.e., lifetime and past-12-month alcohol and drug severity), and mutual help group variables (i.e., primary group affiliation and involvement). Only minor differences emerged. Those with lower lifetime AUD symptom counts were significantly more likely to be lost (vs. retained) at 6 months (p<.05). Meanwhile, Blacks were significantly more likely, and Latinos/Hispanics less likely, to be lost at 12 months, vs. Whites (p<.05); the unemployed were also more likely to be lost at 12 months, vs. those in other employment categories (p<.05).
2.2. Main Measures
Unless otherwise noted, all measures described below were assessed at all three time points. Cronbach’s alphas were similar across waves and are provided for baseline assessments.
2.2.1 Primary group affiliation and involvement
All surveys assessed past-30-day meeting attendance for each group under study. For those reporting attendance at only one group, that group was coded as their “primary group;” for those attending multiple groups, surveys requested that participants identify a primary group. Subsequently, respondents completed 4 yes/no questions measuring other aspects of involvement with their primary groups. Items used different wording for 12-step groups and their alternatives: Participants were asked if they had 1) a “home group” (12-step) or “regular group” (alternative), defined as “a meeting that you usually attend weekly and where you know many of the people,” 2) at least one “sponsor” (12-step) or “close friend” (alternative) in the group “whose number you have and who you can call on for help when you need it”, 3) “led” (12-step) or “convened or facilitated” (alternative) any group meetings in the past 30 days, and 4) done “service” (12-step) or “volunteer work” (alternative) at a group meeting; examples provided included “helping newcomers, setting up chairs, making coffee, or cleaning up after a meeting.” Items were adapted from 4 items used in a standard scale of 12-step involvement (Humphreys, Kaskutas, & Weisner, 1998) and selected because they have been strongly associated with substance use outcomes (Zemore, Subbaraman, & Tonigan, 2013) and are appropriate for all groups. An aggregate, 5-item measure of primary group involvement was created by averaging across activities (recoding yes=1 and no=0) and meeting attendance. Meeting attendance was recoded using group-specific quartile splits, where cut-points were drawn from the attendance distribution for those indicating that group as their primary group (baseline α’s=.90-.93 across groups).
Scale structure and scoring closely mirrored those of a gold-standard and well-validated 12-step involvement scale—the AA Affiliation Scale (Humphreys et al., 1998)—which sums across 9 items and uses just one item to capture meeting attendance. Both the original and adapted versions of the AAAS strongly predict better substance use outcomes (Humphreys et al., 1998; Kaskutas, Bond, & Humphreys, 2002; Zemore & Kaskutas, 2008), and composition of the AAAS and our scale reflect the fact that meeting attendance is just one among many important aspects of involvement (Zemore et al., 2013). Participants who did not have a primary group because of lack of meeting attendance were coded 0 on this measure.
2.2.2. Alcohol severity
Baseline surveys assessed past-12-month and lifetime AUD using an adaptation of the Alcohol Section of the CIDI (World Health Organization, 1993) comprised of 18 items selected to address the 11 criteria for a DSM-5 AUD diagnosis (American Psychiatric Association, 2013). The DSM-5 assumes a single, unidimensional construct. Scores of 2–3 symptoms indicate mild AUD, 4–5 moderate AUD, and 6+ severe AUD. The lifetime measure was used to determine study eligibility. All surveys also assessed recency of last alcohol use, used to code abstinence since last survey (i.e., the past 6 months) at 6 and 12 months. For those not abstinent in these periods, surveys also assessed alcohol problem severity using the Short Index of Alcohol Problems (SIP) (Alterman, Cacciola, Ivey, Habing, & Lynch, 2009; Miller, Tonigan, & Longabaugh, 1995). The SIP is a unidimensional index that was derived from the Drinker Inventory of Consequences (DrInc) assessing physical, intrapersonal, interpersonal, social role, and impulse control problems, and was found to be well-correlated with Addiction Severity Index (ASI) alcohol severity scores (Alterman et al., 2009; Miller et al., 1995). We used the full 15-item measure at baseline (α=.88) and a 5-item version at 6 and 12 months, with these 5 items being selected based on their coverage of all 5 domains and high factor loadings in prior work (Alterman et al., 2009; Miller et al., 1995). Items showed excellent reliability among those reporting drinking in the assessment period (6-month α=.81, 12-month α=.84). SIP scores were coded as 0 for those reporting no drinking.
2.2.3. Drug severity
Baseline surveys similarly assessed past-12-month and lifetime drug problems, using 2 yes/no items asking whether there were “times in your life when you were often under the influence of drugs in situations where you could get hurt, for example when riding a bicycle, driving, operating a machine, or anything else?” and “times in your life when you tried to stop or cut down on your drug use and found that you were not able to do so?” Items were drawn from prior scale analyses of items assessing DSM-5 criteria, and were selected in favor of the full scale due to space constraints (Borges et al.; Saha et al., 2012) (baseline 12-month Pearson r=.81). Items were summed and dichotomized to differentiate those experiencing 2+ drug problems vs. 1 or none at each time point. Paralleling the alcohol assessment, all surveys assessed recency of last use of all illegal drugs, legal drugs not taken as prescribed, and marijuana, used to code past-6-month abstinence at 6 and 12 months.
2.2.4. Recovery goal
Current alcohol recovery goal was assessed at all surveys using a single item (Hall, Havassy, & Wasserman, 1991) asking respondents to select the one recovery goal among 5 that was most true for them at that time, ranging from total lifetime abstinence to controlled use. Responses have been related to lower risk of relapse (Hall et al., 1991) and versions are often used in clinical assessment (see Supplementary Material for wording). Based on preliminary analyses and considering low power, we dichotomized this item into two categories: endorsement of total lifetime abstinence (i.e., “I want to quit using alcohol once and for all, to be totally abstinent, and never use alcohol ever again for the rest of my life”) or another goal.
2.3. Additional Baseline Measures
2.3.1. Demographic characteristics
Baseline surveys assessed gender, age, race/ethnicity, marital status, and socioeconomic status (i.e., education, employment status, and annual household income).
2.3.2. Psychiatric severity
Baseline surveys included 4 items measuring lifetime psychiatric severity, including whether the respondent was ever diagnosed with a mental health disorder; ever received counseling, psychotherapy, or psychiatric visits for a mental health problem; was ever prescribed medication for a mental health problem; and had ever been hospitalized for a mental health problem. An aggregate measure of lifetime severity was created by recoding responses (yes=1, no=0) and averaging (α=.76). At baseline, respondents were also asked about the number of days they experienced mental health problems in the past 30 days (continuous).
2.3.3. Receipt of specialty substance use treatment
Baseline surveys additionally inquired whether participants had “ever received inpatient or outpatient treatment for an alcohol or drug problem?”, and whether any of this treatment had occurred in the past 12 months. Responses were recoded into categorical variables indicating lifetime treatment receipt (yes/no) and past-12-month treatment receipt (yes/no).
2.4. Analysis
Our two primary outcomes were alcohol abstinence and absence of alcohol problems; a secondary outcome was total abstinence from alcohol and drugs. All outcomes used a past-6-month timeframe. Given that outcomes were assessed at both 6 and 12 months, we used a generalized estimating equation (GEE) framework (Fitzmaurice, Laird, & Ware, 2004) to model effects for primary group affiliation (PGA) and primary group involvement (PGI) on outcomes over time. For all analyses, 12-step groups (i.e., Alcoholics Anonymous, Narcotics Anonymous, Cocaine Anonymous, Marijuana Anonymous, and Methadone Anonymous) were aggregated to maximize power.
To gain a general impression of the data, we first examined bivariate associations between study outcomes and baseline demographics, clinical variables, PGA, and PGI. These preliminary GEE’s were designed to help identify those demographic and clinical variables that should be targeted as covariates and to investigate the basic pattern of effects for our main variables of interest.
To directly address our questions regarding the comparative efficacy of our four mutual help groups, we then conducted multivariate logistic GEE’s predicting each of the three substance use outcomes across 6 and 12 months from PGA at baseline (with 12-step as the referent), PGI at baseline, PGI at 6 months, and the interaction between PGA at baseline and PGI at 6 months. The key effects of interest were then the main effects for PGA at baseline (expressing any baseline affiliation effects on outcomes independent of involvement), the main effects for PGI at 6 months (expressing the effect of increases in PGI from baseline to 6 months on outcomes) and the interactions between PGA at baseline and PGI at 6 months (expressing any differences in the relationships between changes in PGI and substance use outcomes across group membership as defined at baseline; that is, the comparative efficacy of each mutual help alternative vs. 12-step). We emphasize that the baseline PGA by 6-month PGI interactions addresses our central interest in comparative efficacy, as they reveal whether the effects of changes in involvement over time on substance use outcomes differed across groups (i.e., the “bang for the buck” question). Nonsignificant interaction terms were dropped in the final models. In preliminary models, we incorporated a main effect for time (6 vs. 12 months) as well as all 2-way and 3-way interactions with time. However, because only one of the 15 interaction terms involving time was significant at p<.05 and because power was limited, we dropped these interactions from all equations and entered time exclusively as a covariate for the final models. This decision was supported by the results of separate multivariate regressions predicting outcomes at 6 and 12 months, which yielded very similar effects.
Models incorporated a comprehensive set of controls for baseline clinical severity, including past-12-month AUD symptoms, past-12-month multiple drug problems, past-12-month specialty substance abuse treatment, and lifetime psychiatric severity. In general, any demographic or clinical variable that was significantly associated (p<.05) with one of the three outcomes in preliminary analyses was also included as a covariate. However, some covariates that were significant in bivariate analyses were dropped from the final models because they contributed little when more proximal or conceptually similar variables were also in the model. Such variables included lifetime measures of AUD symptoms, drug problems, and specialty substance abuse treatment, which added little when past-12-month measures were entered, as well as past-month psychiatric severity, which added little when the lifetime psychiatric severity was used. Similarly, education and income were dropped because of redundancy with employment status. Finally, although bivariate analyses showed some associations between worse outcomes and Hispanic and Other (vs. White) race/ethnicity, we did not include race/ethnicity in the final models because of the low representation of minorities: Only ~8% of respondents in total identified as Black, Hispanic, or Other race/ethnicity.
All models were implemented as sequential regressions. In Model 1, we entered all primary group variables, time, their interactions, and all baseline covariates except recovery goal; in Model 2, we added recovery goal. Recovery goal was entered as a second step to determine whether any effects for primary group variables might be attributable to differences in baseline recovery goal. We chose controlled analyses instead of mediation analyses because our aim was to test for confounding rather than mediation. That is, we wished to test whether differential selection into groups as a function of recovery goal might contribute to the effects of primary group choice on outcomes. Tests of the many potential mechanisms driving benefits of participation in each group are beyond the scope of this paper. All preliminary and main analyses were conducted using respondents with data on all model covariates as well as outcome data at 6 and/or 12 months (N=503). Finally, as a sensitivity analysis, we replicated the models without including participants who indicated changing primary group across the 12-month study period (i.e., with N=440 of 503). This helps address the fact that tests of comparative efficacy could be distorted by participants’ changing affiliations during the follow-up period.
3. Results
3.1. Preliminary Analyses
In bivariate analyses, substance use outcomes at 6 and 12 months were significantly associated with numerous baseline demographics, clinical variables, and mutual help variables (see Table 1 and Figures 1 and 2). Baseline predictors of better outcomes across all dependent variables included older age, married (vs. other) status, fewer past-12-month AUD symptoms, 1 or fewer (vs. 2+) past-12-month drug problems, no (vs. any) past-12-month substance abuse treatment, fewer past-month psychiatric symptoms, and lower lifetime psychiatric severity. Thus, in general, indicators of higher functioning tended to be associated with better outcomes. Less consistent predictors of better outcomes included male (vs. female) gender, White (vs. Hispanic and Other) race/ethnicity, some college (vs. less) education, employed or other (vs. unemployed) status, higher lifetime AUD symptoms, and no (vs. any) lifetime substance abuse treatment.
Table 1.
Bivariate associations between baseline variables and outcomes across 6 and 12 months in GEE logistic regressions (N=503).
| Alcohol Abstinence | No Alcohol Problems | Total Abstinence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| Demographics | |||||||||
| Male (vs. female) | 1.22 | (0.85, 1.75) | 1.62 | * | (1.08, 2.43) | 1.09 | (0.78, 1.52) | ||
| Age | 1.04 | *** | (1.02, 1.05) | 1.04 | *** | (1.02, 1.05) | 1.03 | *** | (1.02, 1.05) |
| Race (Ref: White) | |||||||||
| Black | 0.77 | (0.21, 2.91) | 0.91 | (0.21, 4.06) | 0.90 | (0.25, 3.22) | |||
| Hispanic | 0.52 | (0.24, 1.11) | 0.46 | * | (0.21, 0.99) | 0.57 | (0.27, 1.20) | ||
| Other | 0.41 | (0.14, 1.20) | 0.51 | (0.17, 1.57) | 0.26 | * | (0.08, 0.84) | ||
| Married (vs. other) | 1.48 | * | (1.05, 2.09) | 1.60 | * | (1.11, 2.33) | 1.39 | * | (1.01, 1.91) |
| Education (Ref: HS degree or less) | |||||||||
| Some college | 2.01 | (0.97, 4.17) | 2.82 | ** | (1.30, 6.10) | 1.24 | (0.63, 2.47) | ||
| College degree | 1.26 | (0.65, 2.45) | 1.52 | (0.77, 2.97) | 1.01 | (0.53, 1.92) | |||
| Post-graduate school/degree | 1.23 | (0.63, 2.42) | 1.75 | (0.87, 3.51) | 1.03 | (0.54, 1.99) | |||
| Employment Status (Ref: unemployed) | |||||||||
| Other | 2.16 | * | (1.09, 4.25) | 2.78 | ** | (1.37, 5.65) | 1.61 | (0.83, 3.12) | |
| Employed | 1.86 | (0.98, 3.52) | 1.91 | * | (1.00, 3.67) | 1.31 | (0.70, 2.46) | ||
| Income (Ref: <$30,001) | |||||||||
| $30,001–$60,000 | 0.75 | (0.47, 1.22) | 0.99 | (0.59, 1.66) | 0.85 | (0.54, 1.33) | |||
| $60,001–$100,000 | 0.92 | (0.55, 1.53) | 1.25 | (0.71, 2.18) | 1.12 | (0.70, 1.81) | |||
| $100,001 or more | 1.28 | (0.79, 2.09) | 1.21 | (0.73, 2.02) | 1.31 | (0.84, 2.03) | |||
| Clinical Variables | |||||||||
| Past-12-month AUD symptoms (continuous) | 0.81 | *** | (0.77, 0.84) | 0.77 | *** | (0.74, 0.81) | 0.82 | *** | (0.79, 0.86) |
| Lifetime AUD symptoms (continuous) | 1.08 | (0.99, 1.17) | 0.97 | (0.88, 1.07) | 1.07 | (0.99, 1.16) | |||
| Past-12-month 2+ drug problems (vs. fewer/none) | 0.39 | ** | (0.25, 0.55) | 0.33 | *** | (0.19, 0.57) | 0.28 | *** | (0.16, 0.49) |
| Lifetime 2+ drug problems (vs. fewer/none) | 1.41 | * | (1.00, 1.99) | 1.58 | * | (1.09, 2.31) | 1.12 | (0.82, 1.54) | |
| Past-12-month specialty substance abuse treatment (vs. none) | 0.37 | *** | (0.25, 0.55) | 0.39 | *** | (0.26, 0.59) | 0.39 | *** | (0.27, 0.58) |
| Lifetime specialty substance abuse treatment (vs. none) | 1.03 | (0.71, 1.49) | 0.92 | (0.61, 1.39) | 1.03 | (0.73, 1.45) | |||
| Past-30-day psychiatric severity (continuous) | 0.97 | *** | (0.95, 0.98) | 0.96 | *** | (0.94, 0.98) | 0.96 | *** | (0.95, 0.98) |
| Lifetime psychiatric severity (continuous) | 0.83 | ** | (0.73, 0.95) | 0.84 | * | (0.72, 0.97) | 0.85 | * | (0.76, 0.97) |
| Current alcohol recovery goal of total abstinence (vs. other) | 7.13 | *** | (4.90, 10.36) | 4.60 | *** | (3.11, 6.81) | 5.52 | *** | (3.91, 7.80) |
| Mutual Help Group Involvement | |||||||||
| Primary group involvement (continuous) | 9.08 | *** | (4.81, 17.15) | 11.87 | *** | (6.02, 23.44) | 7.97 | *** | (4.35, 14.60) |
Notes.
p<0.05,
p<0.01,
p<.001.
Figure 1.
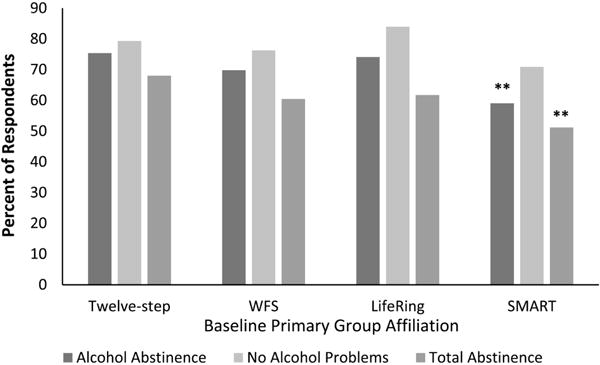
Bivariate associations between baseline primary group affiliation and 6-month outcomes (N=503).
Notes. *p<0.05, **p<0.01, ***p<.001.
Figure indicates statistical significance in comparison to 12-step group.
Figure 2.
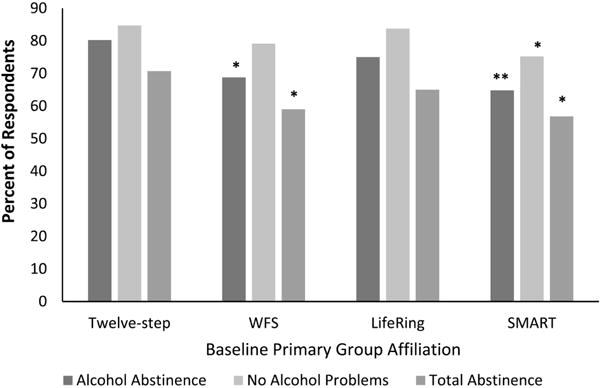
Bivariate associations between baseline primary group affiliation and 12-month outcomes (N=503).
Notes. *p<0.05, **p<0.01, ***p<.001.
Figure indicates statistical significance in comparison to 12-step group.
Regarding the main variables of interest, both having an alcohol goal of lifetime total abstinence (vs. another goal) and higher PGI at baseline were strongly associated with better outcomes. However, as shown in Figures 1 and 2, those identifying SMART as their primary group at baseline had lower odds of both alcohol abstinence and total abstinence at 6 and 12 months and lower odds of no alcohol problems at 12 months, vs. 12 step members. Further, those identifying WFS as their primary group at baseline had lower odds of both alcohol abstinence and total abstinence at 12 months, again vs. 12-step members.
3.2. Multivariate Analyses
The main analyses involved three multivariate, sequential GEE’s for the three substance use outcome across 6 and 12 months (Table 2). As noted, Model 1 entered baseline PGA, baseline PGI, 6-month PGI, the interaction between baseline PGA and 6-month PGI, and model covariates (i.e., gender, age, marital status, employment status, past-12-month AUD symptoms, past-12-month multiple drug problems, past-12-month specialty abuse treatment, and lifetime psychiatric severity); Model 2 added baseline alcohol goal to these models.
Table 2.
Multivariate, logistic GEE models of outcomes across 6 and 12 months by primary group affiliation and involvement (N=503).
| Alcohol Abstinence | No Alcohol Problems | Total Abstinence | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |||||||||||||
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| Baseline Primary Group Affiliation (PGA) | ||||||||||||||||||
| Twelve-step | Ref | Ref | Ref | Ref | Ref | Ref | ||||||||||||
| WFS | 0.67 | (0.37, 1.22) | 0.70 | (0.38, 1.30) | 0.86 | (0.46, 1.62) | 0.88 | (0.46, 1.68) | 0.64 | (0.37, 1.10) | 0.66 | (0.38, 1.14) | ||||||
| LifeRing | 0.53 | (0.27, 1.06) | 0.70 | (0.34, 1.45) | 0.63 | (0.29, 1.36) | 0.73 | (0.33, 1.61) | 0.52 | * | (0.28, 0.96) | 0.64 | (0.34, 1.21) | |||||
| SMART | 0.39 | ** | (0.22, 0.70) | 0.67 | (0.36, 1.24) | 0.44 | * | (0.24, 0.82) | 0.61 | (0.32, 1.16) | 0.53 | * | (0.31, 0.89) | 0.82 | (0.47, 1.42) | |||
| Primary Group Involvement (PGI) | ||||||||||||||||||
| Baseline PGI | 2.26 | (0.92, 5.52) | 1.65 | (0.66, 4.09) | 3.95 | ** | (1.51, 10.31) | 3.11 | * | (118, 8.21) | 1.95 | (0.84, 4.52) | 1.54 | (0.65, 3.64) | ||||
| 6-month PGI | 3.76 | *** | (1.89, 7.47) | 3.97 | *** | (196, 8.04) | 1.80 | (0.86, 3.78) | 1.79 | (0.85, 3.77) | 3.67 | *** | (193, 6.98) | 3.83 | *** | (1.97, 7.46) | ||
| Baseline PGA × 6-month PGI Interactions | — | — | — | — | — | — | ||||||||||||
| Goal of Total Alcohol Abstinence | ||||||||||||||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref | ||||||||||||
| Yes | 5.22 | *** | (3.32, 8.19) | 2.64 | *** | (164, 4.26) | 3.72 | *** | (2.47, 5.61) | |||||||||
Notes.
p<0.05,
p<0.01,
p<.001,
---dropped because nonsignificant.
All models control for time and baseline gender, age, marital status, employment status, past-12-month AUD symptoms, past-12-month multiple drug problems, past-12-month specialty substance abuse treatment, and lifetime psychiatric severity.
In Model 1, all baseline PGA × 6-month PGI interaction terms were nonsignificant for all outcomes (p’s>.17), suggesting no differences in the comparative efficacy of WFS, LifeRing, or SMART compared to 12-step groups. Hence, these interactions were dropped. Meanwhile, greater 6-month PGI was powerfully and positively related to both abstinence outcomes, suggesting beneficial effects for increases in PGI over time regardless of PGA. However, in the alcohol problems model, baseline PGI—but not 6-month PGI—was significant, indicating that changes in PGI over time did not contribute to alcohol problems beyond the contribution of baseline PGI.
Model 1 results also reveal some evidence for worse outcomes among those affiliating with an alternative (vs. 12-step) mutual help group when controlling for the PGI variables and other covariates. Compared to 12-step members, those identifying SMART as their primary group at baseline showed significantly lower odds of all three positive outcomes through follow-ups, while those affiliating with LifeRing showed significantly lower odds of total abstinence through follow-ups.
Nevertheless, Model 2 results show that adding baseline alcohol goal to the model rendered these PGA effects nonsignificant, while having an abstinence goal was strongly and consistently associated with better outcomes across equations. This suggests that baseline alcohol goal partially or fully accounted for the associations between baseline PGA and outcomes through follow-ups. Notably, the effects for PGI remain strong in Model 2.
As noted, we replicated the final models without including participants who indicated changing primary group across the 12-month study period. These analyses yielded nearly equivalent findings. Results showed no significant interactions between baseline PGA and 6-month PGI (p’s>.19) and the same pattern of effects for baseline PGA and recovery goal variables in Models 1 and 2, with one exception: In the alcohol problems model, 6-month but not baseline PGI was associated with better outcomes through follow-ups.
4. Discussion
4.1. Summary and Discussion of Main Results
The present study contributes the first longitudinal, comparative data on 12-step groups and the largest secular, abstinence-based alternatives available in the U.S.: WFS, SMART, and LifeRing. Results revealed strong, robust associations between higher primary group involvement and all three outcomes across 6- and 12-month follow-ups, along with no significant interactions between primary group affiliation at baseline and 6-month primary group involvement in any model. These results tentatively suggest equivalent efficacy for WFS, LifeRing, and SMART, compared to 12-step groups. They suggest that mutual help group involvement—measured as meeting attendance; having a regular or home group; having a close friend or sponsor in the group; leading, convening, or facilitating meetings; and doing volunteer or service work—offers equivalent benefits in relation to substance use and problems regardless of group choice. Findings are noteworthy given the almost total lack of evidence on the efficacy of alternatives to the 12-step model in recovery from alcohol and drug abuse. Though findings should be confirmed in larger samples, they do support referral to a range of abstinence-focused alternatives to AA.
A key strength of this study is its longitudinal design, which allowed us to show that changes in primary group involvement from baseline to 6 months were related to alcohol abstinence and total abstinence across follow-ups in lagged fashion and even accounting for baseline alcohol and drug severity and other clinical and demographic factors. Intriguingly, results did not show this same pattern in the main analyses of alcohol problems, where baseline, but not 6-month, primary group involvement predicted better outcomes. It is unclear why this finding for baseline PGI emerged, but it should be interpreted cautiously because it was not replicated in the sensitivity analyses, where 6-month but not baseline PGI was predictive (as in the other models). Additional research will be important to clarifying the effects of mutual help group involvement at different time points on alcohol problems.
Conclusions of comparative efficacy across the mutual help alternatives may be surprising in view of the significant main effects for baseline PGA on outcomes across 6 and 12 months in the initial models (i.e., Model 1): That is, the associations between SMART (vs. 12-step) affiliation and lower odds of all three positive outcomes through follow-ups, and the association between LifeRing (vs. 12-step) affiliation and lower odds of total abstinence through follow-ups. These baseline affiliation effects appear to be driven largely by group differences in alcohol recovery goal. As noted in the Introduction, both SMART and LifeRing members were less likely than 12-step members to endorse a recovery goal of lifetime total abstinence at baseline. Further, when the present models were adjusted for baseline alcohol recovery goal (as in Model 2), results yielded nonsignificant effects for baseline affiliation and very strong effects for recovery goal across all three substance use outcomes, whereby those with an alcohol recovery goal of lifetime total abstinence had 5.2 times the odds of alcohol abstinence, 3.7 times the odds of total abstinence, and 2.6 times the odds of no alcohol problems, vs. those with any other goal. Given both the substantial differences in recovery goals across groups and the apparent importance of recovery goal to outcomes, the reader may wonder how associations between mutual help involvement and better substance use outcomes could be as strong for SMART and LifeRing as they are for 12-step groups.
Involvement in SMART and LifeRing may yield benefits equivalent to those of 12-step involvement despite differences in recovery goal profiles for two reasons. First, perhaps social support for abstinence and abstinence motivation are not the strongest drivers of the benefits of participation in these groups. While such mechanisms are at least partially responsible for the benefits of 12-step participation (J. F. Kelly, 2017; J. F. Kelly et al., 2009), they may be less important to success in SMART and LifeRing. Second, it may be that social support for abstinence and abstinence motivation do contribute strongly to the benefits of SMART and LifeRing participation, but also that members who become heavily involved associate most with abstinent members and those who encourage abstinence, and/or that the group “cultures” encourage abstinence. This latter scenario seems more likely given the very powerful associations between having a goal of lifetime total abstinence and all three outcomes in the present study. Additional research on mechanisms of action is needed to fully resolve this question. Regardless, the current baseline primary group affiliation effects may be best thought of as selection effects operating independently of involvement effects. Other potential selection factors that may contribute to this pattern of baseline effects should be investigated systematically in further research.
Conclusions of comparative efficacy across the mutual help alternatives may also be surprising because WFS, LifeRing, and SMART do differ significantly from each other—and from 12-step groups—in their philosophies, meeting structures, and memberships. For example, WFS, LifeRing, and SMART diverge from AA in emphasizing personal empowerment over reliance on a Higher Power, and WFS was founded based in part on the idea that AA was not effective for women. SMART also differs from WFS and LifeRing in its unique emphasis on didactic instruction and frequent use of professionals (vs. peers) as meeting facilitators. As described previously, there are furthermore numerous demographic and clinical differences across groups. (For more, Kelly et al. (2012) and Zemore et al. (2017)). Findings for similar efficacy despite these differences may bode well for other abstinence-focused groups not studied here, such as Celebrate Recovery and Refuge Recovery. However, because so little is known about alternatives to 12-step groups in general, the present results should not be generalized incautiously to these groups. Future work on mechanisms of action within WFS, LifeRing, and SMART, as well as study of other mutual help groups, will be critical to better understanding which mutual help groups are effective and why.
4.2. Study Limitations and Future Directions
There are several important limitations associated with this paper. As discussed in the baseline paper (Zemore et al., 2017), an important limitation is that we cannot establish a baseline response rate and cannot completely ensure the representativeness of our mutual help group samples. None of the studied groups keeps a complete list of attendees at any given time-point, so it is impossible to establish a baseline denominator or to compare baseline responders to non-responders. As a result, we cannot rule out selection biases. In fact, our sample probably over-represents those who have participated in each group consistently and for longer time periods. Relatedly, our sample may be biased because all surveys were completed online, and because we used a 12-step sample recruited online (since AA and its counterparts do not participate directly in research). This means that those with good access to the internet are likely to be over-represented in our data.
Nonetheless, we took several measures to obtain the most representative samples possible given these constraints, such as implementing a wide range of recruitment strategies that included recruitment from in-person meetings. Further, as our baseline data indicate, our samples were essentially comparable to samples obtained via internal surveys conducted AA, WFS, LifeRing, and SMART, with one exception—that is, the PAL Study’s 12-step sample included a disproportionate number of women (Zemore et al., 2017). We also obtained good representation of those early in recovery: Within each group, 39–54% of participants reported less than 1 year of abstinence from alcohol (Zemore et al., 2017). An additional strength is that the data show no evidence of differential loss to follow-up across primary group affiliation or involvement (see Section 2.1). Finally, we see no reason to believe that the relationships between primary group involvement and substance use outcomes would be substantially altered even in the presence of selection biases, since selection biases are likely to apply equally to each group and not to one alternative differentially.
Other concerns are the relatively small sample size, which limits power, and (relatedly) the fact that we were forced to combine participants across 12-step groups, despite the fact that members of these groups may well differ on demographic, clinical, and other variables. Further, we could not control for involvement in groups other than one’s primary group without creating an overly complex model. Partially addressing this concern, we did replicate analyses without those who reported changing primary group affiliation, obtaining similar results. Finally, we did not address the entire range of factors that may be associated with primary group affiliation and may affect recovery outcomes, either directly or via moderating effects of involvement. Such factors could include use of medications and other recovery support services as well as length of primary group involvement, which deserve research attention. These limitations again point to the need for larger and better-powered studies, ideally incorporating a focus on factors affecting selection into groups and unique and shared mechanisms of action.
5. Conclusions
Despite some limitations, we believe that this study makes a valuable contribution to the extremely limited evidence base on 12-step alternatives. Results from our comparative efficacy analyses tentatively suggest that clinicians, the courts, and others who assist and advise those with AUD consider referral to a broad array of mutual help options including WFS, LifeRing, and SMART. Referral to a broad array of effective options promises to be maximally effective, as some of those who are deterred by 12-step groups are likely to be attracted to an alternative, and others who are basically satisfied with 12-step groups may opt to become involved in a second group. Results from the recovery goal analysis also suggest that, regardless of group choice, those with a history of AUD are best off choosing a recovery goal of lifetime total abstinence, as those who did so fared the best by far in relation to all substance use outcomes. An optimal care plan may thus involve facilitating involvement in a broad array of mutual help support groups and encouraging abstinence motivation and social networks that are supportive of abstinence.
Supplementary Material
Highlights.
Presents outcome data from the only longitudinal study comparing 12-step groups and their alternatives
Results suggest comparable benefits for involvement in 12-step groups, WFS, LifeRing, and SMART
Results also point to differential selection of participants into groups, affecting outcomes
Findings support referral to a broad array of mutual help groups and encouragement of abstinence motivation
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health (R21AA022747). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We are very grateful for the important contributions of our collaborators in implementing this research, including Becky Fenner (Executive Director for Women for Sobriety); Byron Kerr and Robert Stump (Board Chair and Executive Director of LifeRing, respectively); Tom Horvath and Shari Allwood (President and Executive Director of SMART, respectively); Ronald Tannebaum and Kenny Pomerance (Co-Founders of IntheRooms.com); Shelley Osborn and Deborah Krug (the project management team at ICF International), and Deidre Patterson (Research Associate of the Alcohol Research Group).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: None.
We have framed our investigation as a study of comparative efficacy (and not effectiveness) because our question and analysis address the comparative effects of varying levels of involvement on recovery outcomes across different mutual help groups, which is more analogous to investigating dosage effects (i.e., “efficacy”) than it is to investigating condition assignment (i.e., “effectiveness”) (Gartlehner, Hansen, Nissman, Lohr, & Carey; Singal, Higgins, & Waljee, 2014). We do not wish to imply that our analysis is definitive, and acknowledge that a clinical trial would be ideal for establishing both the efficacy and effectiveness of mutual help group involvement.
References
- Alterman AI, Cacciola JS, Ivey MA, Habing B, Lynch KG. Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. Journal of Studies on Alcohol and Drugs. 2009;70(2):304–307. doi: 10.15288/jsad.2009.70.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM- 5) Arlington, VA: 2013. [Google Scholar]
- Atkins RG, Hawdon JE. Religiosity and participation in mutual-aid support groups for addiction. Journal of Substance Abuse Treatment. 2007;33(3):321–331. doi: 10.1016/j.jsat.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AK, Forbes E, Baker AL, Kelly PJ, Deane FP, Shakeshaft A, Kelly JF. Systematic review of SMART Recovery: outcomes, process variables, and implications for research. Psychology of Addictive Behaviors. 2017;31(1):1–20. doi: 10.1037/adb0000237. [DOI] [PubMed] [Google Scholar]
- Borges G, Zemore SE, Orozco R, Cherpitel CJ, Ye Y, Bond J, Wallisch L. Co-occurrence of alcohol, drug use, DSM-5 alcohol use disorder, and symptoms of drug use disorder on both sides of the U.S.-Mexico border. Alcoholism: Clinical and Experimental Research. 2015;39(4):679–687. doi: 10.1111/acer.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloud RN, Kingree JB. Concerns about dose and underutilization of twelve-step programs: models, scales, and theory that inform treatment planning. In: Galanter M, Kaskutas LA, Borkman T, Zemore SE, Tonigan JS, editors. Recent Developments in Alcoholism, Volume 18: Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. New York: Springer; 2008. pp. 283–301. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Dermen KH. Characteristics of participants in secular organizations for sobriety (SOS) The American Journal of Drug and Alcohol Abuse. 1996;22(2):281–295. doi: 10.3109/00952999609001659. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. First. Hoboken, NJ: James Wiley & Sons; 2004. [Google Scholar]
- Galanter M, Egelko S, Edwards H. Rational recovery: alternative to AA for addiction? The American Journal of Drug and Alcohol Abuse. 1993;19(4):499–510. doi: 10.3109/00952999309001638. [DOI] [PubMed] [Google Scholar]
- Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS. Technical Review 12 (Prepared by the RTI-International-University of North Carolina Evidence-based Practice Center under Contract No 290-02-0016) Rockville, MD: Agency for Healthcare Research and Quality; Apr, 2006. Criteria for distinguishing effectiveness from efficacy trials in systematic reviews. (AHRQ Publication No. 06-0046). [PubMed] [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. Journal of Consulting and Clinical Psychology. 1991;59(4):526–532. doi: 10.1037//0022-006x.59.4.526. [DOI] [PubMed] [Google Scholar]
- Hester RK, Lenberg KL, Campbell W, Delaney HD. Overcoming addictions, a web-based application, and SMART Recovery, an online and in-person mutual help group for problem drinkers, part 1: three-month outcomes of a randomized controlled trial. Journal of Medical Internet Research. 2013;15(7):e134. doi: 10.2196/jmir.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K. Circles of Recovery: Self-help organizations for addictions. Cambridge, UK: Cambridge University Press; 2004. [Google Scholar]
- Humphreys K, Kaskutas LA, Weisner C. The Alcoholics Anonymous Affiliation Scale: development, reliability, and norms for diverse treated and untreated populations. Alcoholism: Clinical and Experimental Research. 1998;22(5):974–978. doi: 10.1111/j.1530-0277.1998.tb03691.x. [DOI] [PubMed] [Google Scholar]
- In the Rooms: A Global Recovery Community. Fort Lauderdale, FL: 2016. Accessed: 2016-05-26. Archived by WebCite® at http://www.webcitation.org/6hniG9RCs. [Google Scholar]
- Kaskutas LA. Women For Sobriety: a qualitative analysis. Contemporary Drug Problems. 1989;16(2):177–200. [Google Scholar]
- Kaskutas LA. Beliefs on the source of sobriety: interactions of membership in Women For Sobriety and AA. Contemporary Drug Problems. 1992;19(4):631–648. [Google Scholar]
- Kaskutas LA. What do women get out of self help? Their reasons for attending Women For Sobriety and Alcoholics Anonymous. Journal of Substance Abuse Treatment. 1994;11(3):185–195. doi: 10.1016/0740-5472(94)90075-2. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. Pathways to self-help among Women For Sobriety. The American Journal of Drug and Alcohol Abuse. 1996a;22(2):259–280. doi: 10.3109/00952999609001658. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. Predictors of self esteem among members of Women For Sobriety. Addiction Research. 1996b;4(3):273–281. doi: 10.3109/16066359609005572. [DOI] [Google Scholar]
- Kaskutas LA. A road less traveled: choosing the “Women For Sobriety” program. Journal of Drug Issues. 1996c;26(1):77–94. doi: 10.1177/002204269602600106. [DOI] [Google Scholar]
- Kaskutas LA. Alcoholics Anonymous effectiveness: faith meets science. Journal of Addictive Diseases. 2009;28(2):145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Borkman TJ, Laudet A, Ritter LA, Witbrodt J, Subbaraman MS, Bond J. Elements that define recovery: the experiential perspective. Journal of Studies on Alcohol and Drugs. 2014;75(6):999–1010. doi: 10.15288/jsad.2014.75.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Turk N, Bond J, Weisner C. The role of religion, spirituality and Alcoholics Anonymous in sustained sobriety. Alcoholism Treatment Quarterly. 2003;21(1):1–16. doi: 10.1300/J020v21n01_01. [DOI] [Google Scholar]
- Kelly JF. Is Alcoholics Anonymous religious, spiritual, neither? Findings from 25 years of mechanisms of behavior change research. Addiction. 2017;112(6):929–936. doi: 10.1111/add.13590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC. Beyond motivation: initial validation of the commitment to sobriety scale. Journal of Substance Abuse Treatment. 2014;46(2):257–263. doi: 10.1016/j.jsat.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addiction Research and Theory. 2009;17(3):236–259. doi: 10.1080/16066350902770458. [DOI] [Google Scholar]
- Kelly JF, Moos R. Dropout from 12-step self-help groups: prevalence, predictors, and counteracting treatment influences. Journal of Substance Abuse Treatment. 2003;24(3):241–250. doi: 10.1016/S0740-5472(03)00021-7. [DOI] [PubMed] [Google Scholar]
- Kelly JF, White WL. Broadening the base of addiction mutual-help organizations. Journal of Groups in Addiction and Recovery. 2012;7(2-4):82–101. doi: 10.1080/1556035X.2012.705646. [DOI] [Google Scholar]
- Kelly PJ, Deane FP, Baker AL. Group cohesion and between session homework activities predict self-reported cognitive-behavioral skill use amongst participants of SMART Recovery groups. Journal of Substance Abuse Treatment. 2015;51:53–58. doi: 10.1016/j.jsat.2014.10.008. [DOI] [PubMed] [Google Scholar]
- LifeRing: Secular Recovery. Oakland, CA: 2016. Accessed: 2016-05-24. http://webcache.googleusercontent.com/search?q=cache:uy6eF6fGek8J:lifering.org/+&cd=1&hl=en&ct=clnk&gl=us. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series. Vol. 4. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health; 1995. The Drinker Inventory of Consequences (DrInC): an instrument for assessing adverse consequences of alcohol abuse; p. 84. (NIH Pub. No. 95-3911). Accessed: 2015-03-03. Archived by WebCite® at http://www.webcitation.org/6Wl5CLTWX. [Google Scholar]
- Morgenstern J, Frey RM, McCrady BS, Labouvie E, Neighbors CJ. Examining mediators of change in traditional chemical dependency treatment. Journal of Studies on Alcohol. 1996;57(1):53–64. doi: 10.15288/jsa.1996.57.53. [DOI] [PubMed] [Google Scholar]
- O’Sullivan D, Blum JB, Watts J, Bates JK. SMART recovery: continuing care considerings for rehabilitation counselors. Rehabilitation Counseling Bulletin. 2015;58(4):203–216. doi: 10.1177/0034355214544971. [DOI] [Google Scholar]
- Peele S, Bufe C, Brodsky A. Resisting 12-Step Coercion: How to fight forced participation in AA, NA, or 12-step treatment. Tucson, AZ: See Sharp Press; 2000. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22(6):1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Saha TD, Compton WM, Chou SP, Smith S, Ruan WJ, Huang B, Grant BF. Analyses related to the development of DSM-5 criteria for substance use related disorders 1. Toward amphetamine, cocaine, and prescription drug use disorder continua using Item Response Theory. Drug and Alcohol Dependence. 2012;122(1-2):38–46. doi: 10.1016/j.drugalcdep.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Mertens J, Arean P, Weisner C. Contrasting outcomes of older versus middle-aged, and younger adult chemical dependency patients in a managed care program. Journal of Studies on Alcohol. 2003;64(4):520–530. doi: 10.15288/jsa.2003.64.520. [DOI] [PubMed] [Google Scholar]
- Singal AG, Higgins PDR, Waljee AK. A primer on effectiveness and efficacy trials. Clinical and Translational Gastroenterology. 2014;5(1):e45. doi: 10.1038/ctg.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SMART Recovery - Self Management for Addiction Recovery. Mentor, OH: 2016. Accessed: 2016-05-24. Archived by WebCite® at http://www.webcitation.org/6hkSrC4mS. [Google Scholar]
- Timko C. Outcomes of AA for special populations. In: Galanter M, Kaskutas LA, Borkman T, Zemore SE, Tonigan JS, editors. Recent Developments in Alcoholism, Volume 18: Research on Alcoholics Anonymous and spirituality in addiction recovery. New York: Springer; 2008. pp. 373–392. [DOI] [PubMed] [Google Scholar]
- Timko C, Debenedetti A. A randomized controlled trial of intensive referral to12-step self-help groups: one-year outcomes. Drug and Alcohol Dependence. 2007;90(2-3):270–279. doi: 10.1016/j.drugalcdep.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Timko C, DeBenedetti A, Billow R. Intensive referral to 12-step self-help groups and 6-month substance use disorder outcomes. Addiction. 2006;101:678–688. doi: 10.1111/j.1360-0443.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor TF, del Boca FK, editors. Treatment Matching in Alcoholism. New York, NY: Cambridge University Press; 2003. pp. 184–204. [Google Scholar]
- Tonigan JS, Miller WR, Schermer C. Atheists, agnostics and Alcoholics Anonymous. Journal of Studies on Alcohol. 2002;63(5):534–541. doi: 10.15288/jsa.2002.63.534. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. Journal of Studies on Alcohol. 1996;57(1):65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- Witbrodt J, Romelsjö A. Treatment seeking and subsequent 1-year drinking outcomes among treatment clients in Sweden and the U.S.A.: a cross-cultural comparison. Addictive Behaviors. 2012;37(10):1122–1131. doi: 10.1016/j.addbeh.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Women for Sobriety. Quakertown, PA: 2016. Accessed: 2016-05-24. Archived by WebCite® at http://www.webcitation.org/6hkUpJTb6. [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview: Authorize Core Version 1.1. Geneva: World Health Organization; 1993. [Google Scholar]
- Zemore SE, Kaskutas LA. 12-step involvement and peer helping in day hospital and residential programs. Substance Use and Misuse. 2008;43(12-13):1882–1903. doi: 10.1080/10826080802297534. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA, Mericle A, Hemberg J. Comparison of 12-Step groups to mutual help alternatives for AUD in a large, national study: differences in membership characteristics and group participation, cohesion, and satisfaction. Journal of Substance Abuse Treatment. 2017;73:16–26. doi: 10.1016/j.jsat.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Subbaraman M, Tonigan JS. Involvement in 12-step activities and treatment outcomes. Journal of Substance Abuse. 2013;34(1):60–69. doi: 10.1080/08897077.2012.691452. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


