Abstract
Background
Emotion (dys)regulation as well as the interventions for improving these difficulties are receiving a growing attention in the literature. The aim of the present paper was to conduct a systematic review about the efficacy of mindfulness-based interventions (MBIs) in both substance and behavioral addictions (BAs).
Method
A literature search was conducted using Cochrane, PubMed, and Web of Science. Fifty-four randomized controlled trials published in English since 2009 to April 2017 were included into a narrative synthesis.
Results
Mindfulness-based interventions were applied in a wide range of addictions, including substance use disorders (from smoking to alcohol, among others) and BAs (namely, gambling disorder). These treatments were successful for reducing dependence, craving, and other addiction-related symptoms by also improving mood state and emotion dysregulation. The most commonly used MBI approaches were as follows: Mindfulness-Based Relapse Prevention, Mindfulness Training for Smokers, or Mindfulness-Oriented Recovery Enhancement, and the most frequent control group in the included studies was Treatment as Usual (TAU). The most effective approach was the combination of MBIs with TAU or other active treatments. However, there is a lack of studies showing the maintenance of the effect over time. Therefore, studies with longer follow-ups are needed.
Conclusion
The revised literature shows support for the effectiveness of the MBIs. Future research should focus on longer follow-up assessments as well as on adolescence and young population, as they are a vulnerable population for developing problems associated with alcohol, drugs, or other addictions.
Keywords: mindfulness, addiction, behavioral addiction, substance use, gambling
Introduction
Nowadays, the incidence of behavioral addictions (BAs), such as gambling disorder, internet addiction, or compulsive buying, is increasingly important, even though substance use disorders (SUDs) are still the most prevalent addictions (1–6). BAs do not involve substance use but they share many core clinical features with substance addictions. In fact, in the latest version of the Diagnostic and Statistical Manual of Mental Disorders (7), gambling disorder appears in the “substance-related and addictive disorders” chapter, together with SUDs.
Lifetime prevalence rates of SUDs are estimated to be around 35.3% in the general population (8–10). When considering BAs these rates increase considerably (11). Moreover, addiction and other mental problems (especially mood and anxiety disorders) tend to often co-occur, maybe because the use of substances can actually induce mental disorders (12, 13) or because it can be a strategy of self-medication or simply an independent comorbid disorder. This situation generates an impairment in occupational and social functioning, as well as medical and legal problems. SUDs and BAs are characterized by the presence of a set of symptoms including tolerance, withdrawal, continued use despite wishes to stop, and despite knowing the negative consequences, a loss of regulatory control over drug cravings and further drug use [DSM-5 (7)]. Furthermore, craving, defined as “intense desire for drugs or addictive behaviors,” was added as diagnostic criteria and considered a key feature of emotion regulation that can affect drug use (10). Thus, SUDs are frequently associated with emotion regulation deficits and there seems to be a relationship between the severity of these deficits and higher drug use. However, the emotion dysregulation observed in addictions is not only described as an ongoing maintenance factor for drug use but also an early risk factor.
Following to Gross (14), “emotion regulation refers to the process of shaping the emotions that one has, when one has them, and how one experiences or expresses these emotions.” There are three core features of emotion regulation. First, there is an activation of a goal to modify the emotion-generative process (15, 16); second, it produces an engagement of the processes that are responsible for altering the emotion trajectory; and third, there is an impact on emotion dynamics (16, 17). Given the importance of this construct in addictions and in view of the current treatment limitations when approaching emotion (dys)regulation, other therapies have emerged for this aim including Mindfulness-based Relapse Prevention (18), Mindfulness Training (MT) for Smokers (MTS) (19), or Mindfulness-Oriented Recovery Enhancement [MORE (20)], and other therapies have been adapted to this population [e.g., Acceptance and Commitment Therapy, ACT (21)], Dialectical Behavior Therapy (22), or Mindfulness based Cognitive Therapy (23). MT represents the secular adaptation of Buddhist contemplative practices aimed to reduce suffering and foster well-being (24). Mindfulness has been described as “the awareness that arises from paying attention on purpose, in the present moment and non-judgementally to things as they are” [(25), p. 47] and unlike distraction, it is characterized by acceptance rather than withdrawal from aversive emotional experience (26).
The aim of this study is to conduct a systematic review of the efficacy of the mindfulness-based interventions (MBIs) in SUDs and BAs by focusing on randomized controlled trials. This review is necessary due to the inclusion of both behavioral and chemical addictions.
Methods
This systematic review was conducted and reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (27–29).
Search Resources
Two independent reviewers conducted the literature search, including different sources such as electronic databases (Cochrane, PubMed, and Web of Science), citations, and reference lists, as well as gray literature. In addition, the reference lists of all included studies were hand searched, limiting the search to articles published in English. To ensure that articles were recent, the search was focused in trials published from 2009 to April 30, 2017.
The search terms used were a combination of MESH terms and keywords and included “mindfulness addiction,” “mindfulness based relapse prevention,” “mindfulness impulsivity,” “mindfulness substance abuse,” “mindfulness substance use,” “MBRP,” “mindfulness gambling disorder,” “mindfulness pathological gambling” in the title, abstract, or keywords.
Eligibility Criteria
Eligibility criteria for the included studies were as follows: (1) to investigate the efficacy of MBIs in the samples of participants suffering from addictions, (2) inclusion of all ages, (3) to provide quantitative data supported by statistical methodology, (4) inclusion of a control group not receiving MBIs, (5) published in English, and (6) randomized controlled trials. Exclusion criteria were as follows: (1) quasi-experimental reports, (2) qualitative reports, (3) case reports, and (4) reviews (literature, systematic) and meta-analyses.
Mindfulness-based interventions were defined as a treatment addressed to promote the moment-by-moment awareness of thoughts, feelings, bodily sensations, and surrounding environment. It also involves acceptance, paying attention to thoughts and feelings without judging them.
Study Selection
First, all included studies were screened based on their titles and abstracts by two reviewers. Second, the identified studies in this search were distributed between five reviewers. The extracted information was checked by one reviewer. The relevant studies were discussed in the case of a disagreement between reviewers.
Data Items
The extracted information from each included trial was as follows: (1) characteristics of the participants (including gender, age, and diagnosis) and the inclusion and exclusion criteria; (2) type of intervention (including type, frequency, and duration; versus non-mindfulness intervention; or versus no treatment); (3) type of outcome measure (including validated scales for measuring and main related results); (4) length of follow-up; (5) dropout rates; and (6) limitations of these studies (see Appendix S1 and S2 in Supplementary Material).
Because of the variability between studies (e.g., heterogeneity of participants, interventions, and reported outcome measures), this systematic review focuses on describing these trials, their results, their applicability, and their limitations and on narrative synthesis rather than on conducting a meta-analysis.
Outcome Measures
The primary outcome measure was the difference between MBIs and no MBIs on measures of reduction of addiction-related symptoms. Secondary outcome measures included changes in (1) self-reported mindfulness levels, (2) emotional self-regulation, (3) miscellaneous outcome measures, and (4) drop-out rates.
Findings are classified according to the specific addiction being explored in each study.
Risk of Bias in Individual Studies
For substantiating the validity of the eligible randomized trials, two reviewers worked independently and reliably to determine the adequacy of randomization and concealment of allocation, blinding of patients, data collectors, loss to follow-up, and other sources of bias.
Results
Study Selection and Design
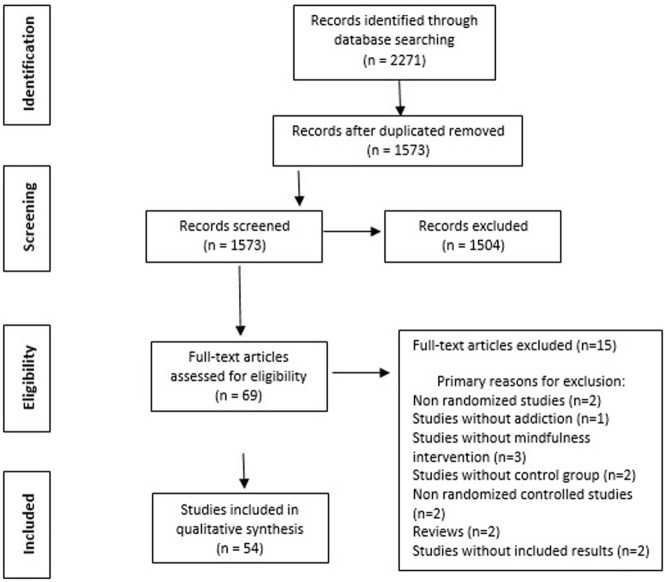
The initial search identified 2,271 independent articles (see Figure 1 for the study selection flow chart). After removing duplicated and screened records, 69 full-text articles were assessed for eligibility and 15 of them were excluded for several reasons (e.g., no-randomized and/or controlled trials, reviews, no-mindfulness interventions, no addiction, or without included results). Finally, 54 articles met the criteria for inclusion and narrative synthesis (see Appendix S1 and S2 in Supplementary Material). All 54 studies finally selected for the review were randomized controlled trials published in English. The quality of these trials was evaluated.
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses flow chart of literature search.
Mindfulness interventions were applied in a wide range of addictions both in SUDs and BAs (e.g., gambling disorder). The majority of these studies focused on heterogeneous substance use, followed by studies on cigarette smoking, alcohol, opioids, gambling disorder, stimulants, marijuana, combination of cocaine and alcohol, and combination of tobacco and alcohol.
Study Characteristics
Participants
The included studies involved 4,916 participants. The mean age of the participants was 34.95, and it was obtained from 51 out of the 54 studies because three trials did not provide age data (30–32). In 50 studies (out of 54), 57.89% were men and 42.11% were women. Four studies did not provide gender data (31, 33–35), five studies included only females (36–40) and six studies only males (41–46). Moreover, the target population of two studies was adolescence (47, 48) and of seven studies were young adults or college students (32, 34, 42, 44, 49–51). One trial (52) was focused on individuals with mild intellectual disabilities.
On the one hand, the most common inclusion criteria were (1) 18 years old or older; (2) English fluency; (3) meeting diagnostic criteria for SUD and other BAs (e.g., gambling disorder); (4) medical clearance; and (5) willingness to be randomized. However, several trials showed other or different inclusion criteria: (1) residency at the treatment center or therapeutic community (20, 30, 37); (2) to be able to speak and read Persian (53); (3) to be 18–29 (40, 50), 18–20 (42), 14 or older (48), 18–40 (33), 20–45 (41), and 21–29 years old (54); (4) living in low socioeconomic areas (55); (5) recurrent pain (56, 57); (6) adult with mild intellectual disability (52), and (7) having participated in a school-based intervention program (58). Furthermore, there were studies which did not provide these data (35, 44, 47, 59–63). On the other hand, the main exclusion criteria were (1) psychosis or other severe psychiatric disorders (e.g., bipolar disorder), (2) dementia, and (3) suicide risk. Nineteen trials did not provide the exclusion criteria (20, 30, 35–37, 42, 44, 46, 47, 49, 52, 54, 55, 60, 62, 64–67).
Intervention
The most frequent mindfulness interventions (Table 1) were MBRP (19, 36, 37, 45, 53, 60, 61, 68–72), MTS (50, 55, 73–75), MORE (20, 30, 43, 56, 57), ACT and variations (42, 62, 64, 66), and different types of Yoga (31, 47, 48).
Table 1.
Relation of the main included mindfulness-based interventions (MBIs) in the search literature and the type of related addiction.
| Main included MBIs | Studies | Type of related addiction |
|---|---|---|
| Mindfulness-Based Relapse Prevention | Bowen et al. (70) | Substance use disorder (SUD) |
| Brewer et al. (19) | Cocaine and alcohol | |
| Carroll (71) | SUD | |
| Chawla et al. (60) | SUD | |
| Hsin Hsu et al. (61) | SUD | |
| Lee et al. (45) | SUD | |
| Glasner-Edwards et al. (72) | Stimulants | |
| Glasner et al. (76) | Stimulants | |
| Witkiewitz and Bowen (68) | SUD | |
| Witkiewitz et al. (36, 69) | SUD | |
| Witkiewitz et al. (37) | SUD | |
| Witkiewitz et al. (36, 69) | SUD | |
| Zemestani and Ottavia (53) | SUD | |
| Mindfulness Training for Smokers | Brewer et al. (73) | Tobacco |
| Davis et al. (50) | Tobacco and alcohol | |
| Davis et al. (55) | Tobacco | |
| Davis et al. (74) | Tobacco | |
| Kober et al. (75) | Tobacco | |
| Mindfulness-Oriented Recovery Enhancement | Garland et al. (20) | Alcohol |
| Garland et al. (30) | Alcohol | |
| Garland et al. (56) | Opioid | |
| Garland et al. (57) | Opioid | |
| Garland et al. (43) | SUD | |
| Acceptance and Commitment Therapy | Bricker et al. (64) | Tobacco |
| Dixon et al. (42) | Gambling disorder | |
| Luoma et al. (62) | SUD | |
| Smallwood et al. (66) | Opioid | |
| Yoga | Butzer et al. (47) | SUD |
| Butzer et al. (47) | SUD | |
| Fishbein et al. (48) | SUD | |
| Hallgren et al. (31) | Alcohol | |
| Mindfulness-Based Stress Reduction | Reza and Hosseinalipour (46) | Opioid |
| Vidrine et al. (77) | Tobacco | |
| Mindfulness-Based Addiction Treatment | Vidrine et al. (78) | Tobacco |
| Mind-Body Bridging | Nakamura et al. (38) | SUD |
| Mindfulness-Based Group Therapy | Imani et al. (33) | Opioid |
| Integrative Body-Mind Training | Tang et al. (34) | Tobacco |
| Mindfulness Based Substance Abuse Treatment | Himelstein et al. (44) | SUD |
| Mindfulness-enhanced Cognitive Behavior Therapy | Toneatto et al. (79) | Gambling disorder |
| Dialectical Behavioral Therapy | Azizi et al. (41) | SUD |
| Affect Regulation Training | Stasiewicz et al. (80) | Alcohol |
| Mindful Awareness in Body-oriented Therapy | Price et al. (39) | SUD |
| Mindfulness Based Cognitive Therapy | Negrei et al. (35) | SUD |
| Non-specified mindfulness-based intervention | Alterman et al. (59) | SUD |
| Vinci et al. (51) | Alcohol | |
| Bowen and Marlatt (49) | Tobacco | |
| Rogojanski et al. (65) | Tobacco | |
| Singh et al. (52) | Tobacco | |
| Murphy and MacKillop (54) | Alcohol | |
| Vernig and Orsillo (32) | Alcohol | |
| McIntosh et al. (63) | Gambling disorder | |
| Vinci et al. (67) | Alcohol | |
| Harris et al. (58) | Alcohol | |
| Valls-Serrano et al. (81) | SUD | |
| de Dios et al. (40) | Marijuana | |
Almost all interventions were composed of 7–12 weekly sessions with a duration of 1–3 h per session, were guided by two therapists, and were performed in a group format. Eight studies showed different characteristics. First, Bricker et al. (64) used a smartphone app-delivered ACT intervention for smoking cessation. Second, Fishbein et al. (48), Nakamura et al. (38), Butzer et al. (47), and Vinci et al. (51) implemented more intensive interventions (e.g., between 20 and 32 sessions). In third and last place, three trials conducted a single session intervention (32, 49, 54). In addition, two studies (52, 65) did not explain the characteristics of their interventions.
Comparator
The most frequently used control group in the included studies was Treatment as Usual (TAU) (31, 33, 38, 39, 44, 45, 48, 52, 53, 58–63, 68, 69, 77). Two studies (70, 71) compared MBRP with Relapse Prevention (RP) and TAU; and two studies more (36, 37) compared MBRP with RP. Cognitive Behavioral Treatment (19), Health Education [HE (66, 72, 76, 80)], Freedom from Smoking [FFS (73, 75)], Quit Line (74), Interactive Learning for Smokers [ILS (50)], Support Group [SG (20, 30, 56, 57)], a QuitGuide app (64), Physical Education (47), relaxation (34), medication treatment (naltrexone or others) (35, 41), and suppression (65) were other comparators. Several trials used two control groups: FFS and Quit Line Intervention (55), CBT and TAU (43, 78), relaxation and puzzle group (51, 67), distraction strategy and passive control (54), and TAU and healthy controls (32). Finally, six trials (40, 42, 46, 49, 79, 81) did not administer any treatment in the control groups (waiting list).
Outcomes
Primary
In the majority of studies, the primary outcome assessed was substance use (severity, abstinence, and craving). Chawla et al. (60) evaluated the adherence and competence of the intervention. Brain activation patterns and subjective ratings of slot machine outcomes during the fMRI tasks were the primary outcomes in the study by Dixon et al. (42), as well as in the studies by Toneatto et al. (79) and McIntosh et al. (63) gambling severity and urges were the primary outcomes. Smallwood et al. (66) assessed ACT in pain and addiction comorbidity using fMRI to evaluate neurophysiologic alterations across the treatment. In another study (46), the health-related quality of life (HRQOL) was the primary outcome. Finally, Negrei et al. (35) investigated if the combination of mindfulness techniques and a CBT group protocol diminished the level of depression and anxiety among a population with addictions.
Secondary and Additional Outcomes
These included levels of emotion regulation, dispositional mindfulness, distress tolerance, psychiatric severity, event-related brain potentials, general health, and mood. The timing of the outcome measures was variable and could include weekly assessment, post-treatment evaluation and 1, 2, 3, 4, 6, and 12-month follow-up evaluation. Sixteen studies did not report follow-up periods (20, 32, 33, 35, 38, 41–44, 46, 48, 57, 66, 67, 77, 81).
Attrition Rates
There was wide variability in the number of participants dropping out from MBIs with attrition rates ranging from 0 to 61% (median attrition = 23.765%). Some studies did not show attrition rates (31, 32, 35, 41, 42, 49, 54, 57, 60, 61, 63, 66, 67, 69, 72, 75).
Discussion
Overall, the revised literature shows the value of MBIs for reducing dependence, craving, and other addiction-related symptoms as well as improving depression, anxiety, and perceived stress and emotion regulation difficulties. Nevertheless, in the majority of the included trials, the MBI effects do not persist at follow-up assessment. In addition, studies seem to indicate that a combination of a mindfulness intervention together with TAU (including active treatments) would be the best treatment option. With regard to the effects of MBIs, it has been observed that the combination of different processes such as acceptance, awareness, and non-judgment is necessary to predict changes in craving (69).
Efficacy of MBIs Compared With TAU
In this review, several of the included studies compare MBIs with TAU. With regard to MBRP versus TAU, individuals who received MBRP and showed lower distress tolerance reported greater reductions in alcohol and other drugs use frequency over time (61) and craving scores (53, 69), although the changes were not maintained at the 4-month follow-up (61). Moreover, MBRP participants showed significantly higher negative expectancies of drug use and decreased depressive mood (45, 53) and anxiety (53) as well as no association between craving and depressive symptoms when compared to TAU individuals, who evidenced a strong association between these two lastly mentioned variables (68). Another result of these trials was a tendency toward a greater acceptance and less judgment when measured with Acceptance and Action Questionnaire (82) and Five-Facet Mindfulness Questionnaire (83) in MBRP participants (69).
For its part, Luoma et al. (62) examined the effects of ACT on shame when compared with TAU. They confirmed that the more gradual reductions in shame in the ACT group protected against high levels of substance use, and this intervention led to higher levels of outpatient treatment attendance during follow-up and continuous treatment gains, especially on psychosocial measures. The combination of other types of MBIs and TAU showed a significant reduction of urges to drink (31), and a greater degree of mindfulness was associated with less nicotine dependence and less withdrawal severity (52, 58, 77). Furthermore, the combination of MBIs and TAU provided a high self-efficacy regarding one’s ability to abstain from smoking in high-risk situations (77) and less craving and drug use in response to social pressure (39). MBIs reduced dissociation, perceived stress, and emotion regulation difficulties in a women population (39) and decreased medical problems over time in a meditation group although without long-term effects (59). Furthermore, the combination of MBIs and TAU decreased the primary outcome measure of drug and alcohol craving and the impact of past trauma and disturbed sleep as well as increased mindfulness, self-compassion and well-being (38), and self-esteem (44).
Finally, McIntosh et al. (63) explored the contribution of a MBIs + CBT for pathological gambling and whether the sequencing of these interventions impacted the effectiveness of the treatment (Mindfulness + CBT or CBT + Mindfulness). They found the combination of psychoeducation, mindfulness intervention, and CBT may be a useful complement of traditional CBT treatments, and it may be offered as an alternative treatment for gambling disorder to improve secondary dysfunction.
Efficacy of MBIs Compared With CBT
While in treatment, participants in MBIs (e.g., MT) did not significantly differ from participants in CBT regarding treatment satisfaction, retention, or frequency of substance use, but MBI participants showed diminished physiological and psychological responses to stress provocation compared with the CBT group (19). In the study by Garland et al. (43), MORE intervention was associated with modest statistically significant improvements in post-traumatic stress symptoms, craving, and positive and negative affect from pre-to-post treatment versus the CBT group. Additionally, this intervention showed a significant indirect effect on craving and post-traumatic stress through increased dispositional mindfulness. In another study (78) that evaluated the efficacy of MBAT versus CBT and TAU, there were no significant overall differences in abstinence rates across the three treatments. However, MBAT showed benefits over CBT and TAU in promoting recovery from a lapse among participants who were not abstinent at the end of treatment. Still, Azizi et al. (41) observed that the cognitive therapy and naltrexone treatment were fewer effective than the emotion regulation treatment. Nevertheless, both mindfulness and cognitive therapy showed an increment in other symptoms such as distress tolerance or emotion regulation, and a decrement in the amount of drug abuse, anxiety, somatic symptoms, social dysfunction, and depression in comparison with pharmacotherapy. Furthermore, the combination of mindfulness and CBT (35) produced lower scores in depression and anxiety compared to the medication group.
Efficacy of MBIs Compared With RP
One of the trials that compared MBIs with RP (70) assessed the relative efficacy of MBRP, RP, and TAU on 12-month SUD outcomes. MBRP and RP showed a decreased risk of relapse of drug and alcohol use. Compared with RP, the MBRP group showed an increased relapse risk of the first drug they used but RP and MBRP did not differ significantly on the time of the first heavy drinking. At the 3-month follow-up, no differences were found between groups; at the 6-month follow-up, RP and MBRP had a significantly reduced risk of drug use relapse and heavy drinking versus TAU, with an advantage in RP group over MBRP on the first drug use; and at the 12-month follow-up, MBRP reported significantly higher probability of not engaging in heavy drinking and fewer drug use days compared with RP. These results partially coincide with those of Witkiewitz et al. (36, 37), who found lower addiction severity and less drug use at follow-up in MBRP group versus RP. In the study by Carroll (71), MBRP was significant and positively related to mindfulness, whereas RP was significant and inversely related to mindfulness and associated with higher levels of thought suppression. Moreover, MBRP produced psychophysiological responses against stress that suggest self-regulation and self-soothing behaviors instead of abusing substances.
Efficacy of MBIs Compared With HE
Mindfulness-Based Relapse Prevention and ART showed greater declines in negative affect (72, 76, 80), and MBRP is effective in reducing psychiatric severity (e.g., major depression and generalized anxiety disorder) as well as stimulant use among those with these health mental problems (72, 76). Stasiewicz et al. (80) found that the combination of CBT and ART demonstrated significantly greater increases of the percentage of abstinent days from the baseline to the tendency of treatment versus the combination CBT and HE even though this effect began to slightly decline during follow-up. Besides, MBIs (e.g., ACT) had neurophysiologic effects as the brain’s responsiveness to painful stimuli decreased in patients with chronic low back pain and opioid addiction comorbidity (66).
Efficacy of MBIs Compared With Usual Smoking Interventions
There was variability with respect to the control groups of the included smoking studies. MBIs (e.g., MTS) showed significant improvements on self-reported measures of attentional control, emotion regulation, and mindfulness. Post-treatment, these measures were significantly correlated with meditation time and smoking abstinence versus Quit Line intervention or FFS (55, 73, 74). In addition, this type of mindfulness intervention (MTS) produced lower neural reactivity stress in regions including amygdala and insula (75).
When MTS was compared with ILS (50), there were no significant differences between groups in smoking abstinence although MTS participants showed significantly greater number of abstinence days in the first 2 weeks. With reference to alcohol use, controls significantly increased alcohol consumption over the course of the intervention, whereas MBI participants decreased consumption. For its part, in the study by Bricker et al. (64), a smartphone app-delivered ACT intervention for smoking cessation (SmartQuit) showed striking higher dropout rate versus a QuitGuide group control.
Efficacy of MBIs Compared With SG
In a set of studies conducted by Garland et al. (20, 30, 56, 57), in which they compared MORE with a SG, they found stress and alcohol bias reduction and alcohol thought suppression as well as HRV recovery increase from alcohol cues following stress induction in MORE groups. Contrary to their hypotheses, MORE did not significantly increase self-reported mindfulness, nor did it result in significant decrements in craving, but significantly reduced symptoms associated with chronic pain and prescription opioid misuse.
Efficacy of MBIs Compared With Non-Treatment
Dixon et al. (42) observed a neurological change in an ACT intervention toward similar brain activation patterns as non-pathological gamblers, including activation in the middle frontal gyrus and inferior parietal lobule. Following treatment, ACT participants were more likely to report higher engagement in psychological flexibility and mindfulness-related behaviors. In another study targeting problem gamblers (79), MBIs reported significantly fewer gambling symptoms, gambling urges, and psychiatric symptoms at post-treatment, and they demonstrated that the mindfulness practice (measured by number of minutes) was significantly correlated with a reduction in psychiatric symptoms. MBIs versus no treatment have been associated with negative affect and urges (49), improvements in working memory, reflection-impulsivity/decision-making and performance, reduced stress levels and increased planning (81), decreased marijuana use at post-treatment and 3-month follow-up in a women population (40), and better HRQOL due to increased awareness of thoughts and emotions, acceptance, and compassion (46).
Efficacy of MBIs Compared With Other Interventions
Mindfulness-based interventions have been compared with numerous control interventions. With reference to yoga versus physical education, Butzer et al. (47) concluded that yoga has beneficial effects on emotional self-control (females) and willingness to smoke cigarettes (females and males). No differences between groups pre- to post-interventions were found although they observed improvements over an extended period of time.
In college students, MBIs compared with relaxation (34, 51, 67) showed a significant smoking and craving reduction, an increased activity at inferior frontal gyrus/ventrolateral PFC and ACC/medial PFC and a decreased activity at cerebellum, posterior cingulated cortex/precuneus, and other regions after the intervention. Furthermore, MBIs were effective at increasing mindfulness state, and MBIs such as relaxation showed decreased negative affect and urge after interventions. However, higher levels of some of the facets of impulsivity, such as Sensation seeking, Negative and Positive urgency were associated with increased negative affect and urge and decreased positive affect in the post-mindfulness intervention.
When MBIs were compared to a distraction strategy or passive control or suppression condition (54, 65), there were no overall differences between groups. It seems that dispositional anxiety sensitivity did not have an impact on the outcomes but, state symptom-focused anxiety immediately after the cue induction procedure was a significant predictor of self-efficacy at follow-up. Specifically, and contrary to previous research, individuals who are anxiety sensitive do equally well, or better, when coping with cravings using a suppression-based approach as they do when using a mindfulness strategy, at least in the short term.
Limitations
The systematic review reported here intent to show MBIs’ results and effects. The main limitation of this review is that the patient population, MBIs, comparators, and outcome measures are not the same across studies. Moreover, the quality was adequate in all studies. Another limitation of our study is the number of trials included in the review, 54, and the consequent difficulty to integrate all information. However, for solving this problem we used five reviewers.
Conclusion and Future Perspectives
The revised literature gives support to the effectiveness of the MBIs. These treatments are adequate to reduce dependence, craving, and other addiction-related symptoms as well as to improve mood state and emotion dysregulation. There are certain interventions that presented better results in the treatment of addiction such as MBRP, MTS, or MORE. Nevertheless, the best effectiveness may be the combination of the MBIs with TAU or another active treatment. Besides, few studies have found maintenance of the effects over time, and it would be important to conduct more follow-up studies. As for the target population, it would be interesting to investigate addiction problems in adolescents and young adults because they are a fragile and sensitive population to develop special interests in drugs and other addictions.
Author Contributions
Research project elaboration: MS, SJ-M, IS, and JM; organization: MS; execution: MS, MG, CR, NM-B, and JS-G; design: MS and CR; writing of the first draft: MS; review and critique: MS, MG, CR, NM-B, JS-G, SJ-M, IS, and JT.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This manuscript and research were supported by grants from Instituto de Salud Carlos III (ISCIII) and cofounded by FEDER funds/European Regional Development Fund (ERDF), a way to build Europe. CIBERobn and CIBERsam are initiatives of ISCIII. This work was also supported by the Ministerio de Economía y Competitividad (PSI2015-68701-R).
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00095/full#supplementary-material.
References
- 1.O’Brien C. Addiction and dependence in DSM-V. Addiction (2011) 106:866–7. 10.1111/j.1360-0443.2010.03144.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gearhardt AN, White MA, Potenza MN. Binge eating disorder and food addiction. Curr Drug Abuse Rev (2011) 4:201–7. 10.2174/1874473711104030201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Potenza MN. Non-substance addictive behaviors in the context of DSM-5. Addict Behav (2014) 39:1–2. 10.1016/j.addbeh.2013.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiménez-Murcia S, Granero R, Fernández-Aranda F, Arcelus J, Aymamí MN, Gómez-Peña M, et al. Predictors of outcome among pathological gamblers receiving cognitive behavioral group therapy. Eur Addict Res (2015) 21(4):169–78. 10.1159/000369528 [DOI] [PubMed] [Google Scholar]
- 5.Farré JM, Fernández-Aranda F, Granero R, Aragay N, Mallorquí-Bague N, Ferrer V, et al. Sex addiction and gambling disorder: similarities and differences. Compr Psychiatry (2015) 56:59–68. 10.1016/j.comppsych.2014.10.002 [DOI] [PubMed] [Google Scholar]
- 6.Del Pino-Gutiérrez A, Jiménez-Murcia S, Fernández-Aranda F, Agüera Z, Granero R, Hakansson A, et al. The relevance of personality traits in impulsivity-related disorders: from substance use disorders and gambling disorder to bulimia nervosa. J Behav Addict (2017) 6(3):396–405. 10.1556/2006.6.2017.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington, DC: Association AP; (2013). 947 p. [Google Scholar]
- 8.National Institute of Mental Health (NIMH). National Comorbidity Survey: Lifetime Prevalence Estimates. (2007). Available from: www.hcp.med.harvard.edu/ncs (Accessed: December 10, 2017).
- 9.Substance Abuse and Mental Health Services Administration (SAMSHA). Results from the 2010 National Survey on Drug Use and Health (NSDUH): Summary of National Findings (NSDUH Series H-41). Rockville, MD: Substance Abuse and Mental Health Services Administration (SAMSHA) (2011). [Google Scholar]
- 10.Kober H. Emotion regulation in substance use disorders. 2nd ed In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Press; (2014). p. 428–46. [Google Scholar]
- 11.Sauvaget A, Trojak B, Bulteau S, Jiménez-Murcia S, Fernández-Aranda F, Wolz I, et al. Transcranial direct current stimulation (tDCS) in behavioral and food addiction: a systematic review of efficacy, technical, and methodological issues. Front Neurosci (2015) 9:349. 10.3389/fnins.2015.00349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Nelson CB, McGonagle KA. The epidemiology of co-ocurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry (1996) 66:17–31. 10.1037/h0080151 [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62:617–27. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol (1998) 2:271–99. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- 15.Gross JJ, Sheppes G, Urry HL. Emotion generation and emotion regulation: a distinction we should make (carefully). Cogn Emot (2011) 25:765–81. 10.1080/02699931.2011.555753 [DOI] [PubMed] [Google Scholar]
- 16.Gross JJ. Emotion regulation: conceptual and empirical foundations. 2nd ed In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Press; (2014). p. 3–20. [Google Scholar]
- 17.Thompson RA. Emotion and self-regulation. Socioemotional Development: Nebraska Symposium on Motivation. (Vol. 36), Lincoln: University of Nebraska Press; (1990). p. 367–467. [PubMed] [Google Scholar]
- 18.Bowen S, Chawla N, Marlatt GA. Mindfulness-Based Relapse Prevention for Addictive Behaviors: A Clinician’s Guide. New York: Guilford Press; (2010). [Google Scholar]
- 19.Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, et al. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Subst Abus (2009) 30:306–17. 10.1080/08897070903250241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: results of a randomized controlled pilot trial. J Psychoactive Drugs (2010) 42(2):177–92. 10.1080/02791072.2010.10400690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York: Guilford Press; (1999). [Google Scholar]
- 22.Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press; (1993). [Google Scholar]
- 23.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford Press; (2002). [Google Scholar]
- 24.Farb NAS, Anderson AK, Irving JA, Segal ZV. Mindfulness interventions and emotion regulation. 2nd ed In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Press; (2014). p. 548–67. [Google Scholar]
- 25.Williams JMG. The Mindful Way through Depression: Freeing Yourself from Chronic Unhappiness. New York: Guilford Press; (2007). [Google Scholar]
- 26.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry (1982) 4(1):33–47. 10.1016/0163-8343(82)90026-3 [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (2009) 339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (2009) 339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris JD, Quatmen CE, Marning MM, Siston RA, Flanigan DC. How to write a systematic review. Am J Sports Med (2014) 42(11):2761–8. 10.1177/0363546513497567 [DOI] [PubMed] [Google Scholar]
- 30.Garland E, Franken I, Howard M. Cue-elicited heart rate variability and attentional bias predict alcohol relapse following treatment. Psychopharmacology (2011) 222:17–26. 10.1007/s00213-011-2618-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hallgren M, Romberg K, Bakshi A, Andréasson S. Yoga as an adjunct treatment for alcohol dependence: a pilot study. Complement Ther Med (2014) 22:441–5. 10.1016/j.ctim.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 32.Vernig PM, Orsillo SM. Psychophysiological and self-reported emotional responding in alcohol-dependent college students: the impact of brief acceptance/mindfulness instruction. Cogn Behav Ther (2009) 38(3):174–83. 10.1080/16506070902767563 [DOI] [PubMed] [Google Scholar]
- 33.Imani S, Kazem Atef Vahid A, Gharraee B, Noroozi A, Habibi M, Bowen S. Effectiveness of mindfulness-based group therapy compared to the usual opioid dependence treatment. Iran J Psychiatry (2015) 10(3):175–84. [PMC free article] [PubMed] [Google Scholar]
- 34.Tang Y, Tang R, Posner MI. Brief meditation training induces smoking reduction. Proc Natl Acad Sci U S A (2013) 110(34):13971–5. 10.1073/pnas.1311887110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Negrei C, Stan M, Balalau C, Ginghina O, Baconi DL, Craciun B. The effectiveness of combining pharmacologic strategies with MCBT for diminishing the level of depression and anxiety at patients diagnosed with addiction. Toxicol Lett (2015) 238S:S56–383. 10.1016/j.toxlet.2015.08.468 [DOI] [Google Scholar]
- 36.Witkiewitz K, Greenfield BL, Bowen S. Mindfulness-Based Relapse Prevention with racial and ethnic minority women. Addict Behav (2013) 38:2821–4. 10.1016/j.addbeh.2013.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Witkiewitz K, Warner K, Sully B, Barricks A, Stauffer C, Thompson BL, et al. Randomized trial comparing MBRP with RP for women offenders at a Residential Addiction Treatment Center. Subst Use Misuse (2014) 49:536–46. 10.3109/10826084.2013.856922 [DOI] [PubMed] [Google Scholar]
- 38.Nakamura Y, Lipschitz D, Kanarowski E, McCormick T, Sutherland D, Melow-Murchie M. Investigating impacts of incorporating an adjuvant mind–body intervention method into treatment as usual at a community-based substance abuse treatment facility: a pilot randomized controlled study. SAGE Open (2015):1–18. 10.1177/2158244015572489 [DOI] [Google Scholar]
- 39.Price CJ, Wells EA, Donovan DM, Rue T. Mindful awareness in body-oriented therapy as an adjunct to women’s substance use disorder treatment: a pilot feasibility study. J Subst Abuse Treat (2012) 43:94–107. 10.1016/j.jsat.2011.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Dios MA, Herman DS, Britton WB, Hagerty CE, Anderson BJ, Stein MD. Motivational and mindfulness intervention for young adult female marijuana users. J Subst Abuse Treat (2012) 42:56–64. 10.1016/j.jsat.2011.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Azizi A, Borjali A, Golzari M. The effectiveness of emotion regulation training and cognitive therapy on the emotional and addictional problems of substance abusers. Iran J Psychiatry (2010) 5(2):60–5. [PMC free article] [PubMed] [Google Scholar]
- 42.Dixon MR, Wilson AN, Habib R. Neurological evidence of acceptance and commitment therapy effectiveness in college-age gamblers. J Context Behav Sci (2016) 5:80–8. 10.1016/j.jcbs.2016.04.004 [DOI] [Google Scholar]
- 43.Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav Res Ther (2016) 77:7–16. 10.1016/j.brat.2015.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Himelstein S, Saul S, Garcia-Romeu A. Does Mindfulness meditation increase effectiveness of substance abuse treatment with incarcerated youth? A pilot randomized controlled trial. Mindfulness (2015) 6:1472–80. 10.1007/s12671-015-0431-6 [DOI] [Google Scholar]
- 45.Lee K, Bowen S, An-fu B. Psychosocial outcomes of Mindfulness-Based Relapse Prevention in incarcerated substance abusers in Taiwan: a preliminary study. J Subst Use (2011) 16(6):476–83. 10.3109/14659891.2010.505999 [DOI] [Google Scholar]
- 46.Reza HLN, Hosseinalipour F. Effectiveness of mindfulness-based stress reduction intervention for health-related quality of life in drug-dependent males. Iran Red Crescent Med J (2014) 16(9):e12608. 10.5812/ircmj.12608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butzer B, LoRusso A, Skin SH, Khalsa SBS. Evaluation of yoga for preventing adolescent substance use risk factors in a middle school setting: a preliminary group-randomized controlled trial. J Youth Adolesc (2017) 46:603–32. 10.1007/s10964-016-0513-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fishbein D, Miller S, Herman-Stahl M, Williams J, Lavery B, Markovitz L, et al. Behavioral and pychophysiological effects of a yoga intervention on high-risk adolescents: a randomized control trial. J Child Fam Stud (2015) 25:518–29. 10.1007/s10826-015-0231-6 [DOI] [Google Scholar]
- 49.Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychol Addict Behav (2009) 23(4):666–71. 10.1037/a0017127 [DOI] [PubMed] [Google Scholar]
- 50.Davis JM, Mills DM, Stankevitz KA, Manley AR, Majeskie MR, Smith SS. Pilot randomized trial on mindfulness training for smokers in young adult binge drinkers. BMC Complement Altern Med (2013) 13:215. 10.1186/1472-6882-13-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vinci C, Peltier MR, Shah S, Kinsaul J, Waldo K, McVay MA, et al. Effects of a brief mindfulness intervention on negative affect and urge to drink among college student drinkers. Behav Res Ther (2014) 59:82–93. 10.1016/j.brat.2014.05.012 [DOI] [PubMed] [Google Scholar]
- 52.Singh NN, Lancioni GE, Myers RE, Karazsia BT, Winton ASW, Singh J. A randomized controlled trial of a mindfulness-based smoking cessation program for individuals with mild intellectual disability. Int J Ment Health Addic (2014) 12:153–68. 10.1007/s11469-013-9471-0 [DOI] [Google Scholar]
- 53.Zemestani M, Ottavia C. Effectiveness of MBRP for co-ocurring substance use and depression disorders. Mindfulness (2016) 7:1347–55. 10.1007/s12671-016-0576-y [DOI] [Google Scholar]
- 54.Murphy CM, MacKillop J. Mindfulness as a strategy for coping with cue-elicited cravings for alcohol: an experimental examination. Alcohol Clin Exp Res (2014) 38(4):1134–42. 10.1111/acer.12322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davis JM, Manley AR, Goldberg SB, Smith SS, Jorenby DE. Randomized trial comparing mindfulness training for smokers to a matched control. J Subst Abuse Treat (2014) 47(3):213–21. 10.1016/j.jsat.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garland EL, Froeliger B, Williams JM, Manusov EG, Kelly A, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. J Consult Clin Psychol (2014) 82(3):448–439. 10.1037/a0035798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garland EL, Froeliger B, Howard MO. Neurophysiological evidence for remediation of reward processing deficits in chronic pain and opioid misuse following treatment with Mindfulness-Oriented Recovery Enhancement: exploratory ERP findings from a pilot RCT. J Behav Med (2015) 38:327–36. 10.1007/s10865-014-9607-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harris JS, Stewart DG, Stanton BC. Urge surfing as a aftercare in adolescent alcohol use: a randomized control trial. Mindfulness (2017) 8:144–9. 10.1007/s12671-016-0588-7 [DOI] [Google Scholar]
- 59.Alterman AI, Koppenhaver JM, Mulholland E, Ladden LJ, Baime MJ. Pilot trial of effectiveness of mindfulness meditation for substance abuse patients. J Subst Use (2004) 9(6):259–68. 10.1080/14659890410001711698 [DOI] [Google Scholar]
- 60.Chawla N, Collins S, Bowen S, Hsu S, Grow J, Douglasss A, et al. The Mindfulness-Based Relapse Prevention adherence and competence scale: development, interrater reliability and validity. Psychother Res (2010) 20(4):388–97. 10.1080/10503300903544257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsin Hsu S, Collins SE, Marlatt A. Examining psychometric properties of distress tolerance and its moderation of Mindfulness-Based Relapse Prevention effects on alcohol and other drug use outcomes. Addict Behav (2013) 38:1852–8. 10.1016/j.addbeh.2012.11.002 [DOI] [PubMed] [Google Scholar]
- 62.Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and Steady wins the race: a randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J Consult Clin Psychol (2012) 80(1):43–53. 10.1037/a0026070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McIntosh CC, Crino RD, O’Neill KO. Treating problem gambling samples with cognitive behavioural therapy and mindfulness-based interventions. A clinical trial. J Gamb Stud (2016) 32:1305–25. 10.1007/s10899-016-9602-1 [DOI] [PubMed] [Google Scholar]
- 64.Bricker JB, Mull KE, Kientz JA, Vilardaga R, Mercer LD, Akioka KJ, et al. Randomized controlled trial pilot of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend (2014) 143:87–94. 10.1016/j.drugalcdep.2014.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rogojanski J, Vettese LC, Antony MM. Role of sensitivity to anxiety symptoms in responsiveness to mindfulness versus suppression strategies for coping with smoking cravings. J Clin Psychol (2011) 67(4):439–45. 10.1002/jclp.20774 [DOI] [PubMed] [Google Scholar]
- 66.Smallwood RF, Potter JS, Robin DA. Neurophysiological mechanisms in acceptance and commitment therapy in opioid addicted patients with chronic pain. Psychiatry Res (2016) 250:12–4. 10.1016/j.pscychresns.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vinci C, Peltier M, Waldo K, Kinsaul J, Shah S, Coffey SF, et al. Examination of trait impulsivity on the response to a brief mindfulness intervention among college student drinkers. Psychiatry Res (2016) 242:365–74. 10.1016/j.psychres.2016.04.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Witkiewitz K, Bowen S. Depression, craving and substance use following a randomized trial of Mindfulness-Based Relapse Prevention. J Consult Clin Psychol (2010) 78(3):362–74. 10.1037/a0019172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-Based Relapse Prevention for substance craving. Addict Behav (2013) 38:1563–71. 10.1016/j.addbeh.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, et al. Relative efficacy of Mindfulness-Based Relapse Prevention, standard relapse prevention and treatment as usual for substance use disorders. A randomized controlled trial. JAMA Psychiatry (2014) 71(5):547–56. 10.1001/jamapsychiatry.2013.4546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carroll H. Do mindfulness and/or thought suppression mediate treatment effects on cardiac vagal control in substance abusers treated with mindfulness-based relapse prevention, relapse prevention or treatment as usual? Psychophysiology (2014) 51:S35. [Google Scholar]
- 72.Glasner-Edwards S, Mooney L, Ang A, Garneau HC, Hartwell EE, Brecht M, et al. Mindfulness Based Relapse Prevention improves stimulant use among adults with major depression and generalized anxiety disorder. Drug Alcohol Depend (2015) 156:e80. [Google Scholar]
- 73.Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend (2011) 119(1–2):72–80. 10.1016/j.drugalcdep.2011.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial on mindfulness training for smokers targeted to a disadvantaged population. Subst Use Misuse (2014) 49:571–85. 10.3109/10826084.2013.770025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kober H, Brewer JA, Height KL, Sinha R. Neural stress reactivity relates to smoking outcomes and differentiates between mindfulness and cognitive-behavioral treatments. Neuroimage (2017) 151:4–13. 10.1016/j.neuroimage.2016.09.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Glasner S, Mooney LJ, Ang A, Garneau HC, Hartwell E, Brecht M, et al. Mindfulness-Based Relapse Prevention for stimulant dependent adults: a pilot RCT. Mindfulness (2017) 8:126–35. 10.1007/s12671-016-0586-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, et al. Associations of mindfulness with nicotine dependence withdrawal, and agency. Subst Abus (2009) 30:318–27. 10.1080/08897070903252973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vidrine JI, Spears CA, Heppner WL, Reitzel LR, Marcus MT, Cinciripini PM, et al. Efficacy of mindfulness-based addiction treatment (MBAT) for smoking cessation and lapse recovery: a randomized clinical trial. J Consult Clin Psychol (2016) 84(9):824–38. 10.1037/ccp0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Toneatto T, Pillai S, Courtice EL. Mindfulness-enhanced cognitive behavior therapy for problem gambling: a controlled pilot study. Int J Ment Health Addic (2014) 12:197–205. 10.1007/s11469-014-9481-6 [DOI] [Google Scholar]
- 80.Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, et al. Affect regulation training (ART) for alcohol use disorders: development of a novel intervention for negative affect drinkers. J Subst Abuse Treat (2013) 45:433–43. 10.1016/j.jsat.2013.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Valls-Serrano C, Caracuel A, Verdejo-García A. Goal Management Training and Mindfulness meditation improve executive functions and transfer to ecological tasks of daily life in polysubstance users enrolled in therapeutic community treatment. Drug Alcohol Depend (2016) 165:9–14. 10.1016/j.drugalcdep.2016.04.040 [DOI] [PubMed] [Google Scholar]
- 82.Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, et al. Preliminary psychometric properties of the acceptance and action questionnaire–II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther (2011) 42(4):676–88. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 83.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment (2006) 13:27–45. 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.