Abstract
Background/Aims
We evaluated the distribution of lower and upper gastrointestinal (GI) symptoms among individuals with irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC) in a nationwide survey.
Methods
Individuals (≥ 18 years of age) were identified from a nationwide sample of > 70 000 United States adults. Participants completed the National Institutes of Health GI Patient Reported Outcomes Measurement Information System (NIH GI-PROMIS) questionnaire. Symptom frequency and intensity in the prior 7 days were assessed using validated PROMIS scores. Odds ratios (OR) with 95% confidence intervals (CI) were calculated to compare symptom prevalence in IBS-C vs CIC, and one-way ANOVA was used to assess differences in PROMIS scores. Regression analysis was performed to adjust for demographic variables.
Results
Nine hundred and seventy adults met eligibility criteria (275 with IBS-C, 734 with CIC). Demographics were similar among groups except for education, marital and employment status, and income. Adjusting for demographic differences, GI-PROMIS scores of global GI symptoms were higher in IBS-C (251.1; 95% CI, 230.0–273.1) compared to CIC (177.8; 95% CI 167.2–188.4) (P < 0.001). Abdominal pain was more prevalent (OR, 4.3; 95% CI, 2.9–6.6) and more severe (P = 0.007) in IBS-C. Constipation was more severe in IBS-C (P = 0.011). Incontinence was more common (OR, 2.9; 95% CI, 1.3–6.3) but just as severe (P = 0.389) in IBS-C versus CIC. Regarding upper GI symptoms, the prevalence of dysphagia, heartburn, and nausea were similar. However, IBS-C individuals had more severe heartburn (P = 0.001).
Conclusion
GI symptoms are generally more severe in IBS-C compared to CIC, however abdominal pain, bloating, and upper GI symptoms still commonly occur in CIC.
Keywords: Cross-sectional studies, Irritable bowel syndrome, Surveys and questionnaires, Symptom assessment
Introduction
Constipation is amongst the most common gastrointestinal (GI) complaints reported by individuals seeking advice from a health care provider.1 Up to 20% of the United States (US) adult population suffers with some form of constipation. Constipation reduces quality of life to a similar degree as other medical conditions such as diabetes, gastroesophageal reflux, or stable inflammatory bowel disease,2,3 and adversely affects work productivity.4
Patients associate a number of bowel related complaints with the word “constipation,” including reduced stool frequency, hard or lumpy stool consistency, straining, and a sensation of incomplete evacuation.5 Some patients with constipation also report abdominal symptoms such as pain, bloating, and distension.6 According to the symptom-based Rome criteria, patients with a combination of bowel and abdominal symptoms have been labelled as suffering with irritable bowel syndrome with constipation (IBS-C), whereas those with bowel related complaints but little in the way of abdominal symptoms have been diagnosed with chronic idiopathic or functional constipation (CIC).7
There is controversy in the literature regarding the classification of IBS-C and CIC as separate and distinct conditions given that overlap between these conditions is common in clinical practice. By definition, CIC patients must not meet criteria for IBS.8 The removal of this restriction was studied in previous large scale cross-sectional surveys, finding 39–90% of IBS-C patients meeting CIC criteria9,10 and 8–44% of CIC patients meeting IBS-C criteria.9–11 The Rome IV publication acknowledged that IBS-C and CIC could represent the extremes of a disease spectrum rather than separate and distinct disorders.8 Insufficiencies in our understanding of the overall symptom complex of these disorders might contribute to the high rates of patient dissatisfaction with treatment for IBS-C and CIC patients.4
Characteristic bowel symptoms and some abdominal symptoms have been evaluated in the literature in a comparative manner between these disorders. However, previous studies focused on (1) lower GI symptoms6,10–13 or (2) overlapping disease states.10,12–14 To our knowledge, a comprehensive, comparative evaluation of lower and upper GI symptoms has not been conducted between IBS-C and CIC.
To advance our understanding of the global phenotype of individuals with IBS-C vs. CIC, the aim of the present study was to evaluate the complex of lower and upper GI symptoms among actively symptomatic individuals with IBS-C compared to individuals with CIC using results from a US population-based survey.
Materials and Methods
Data Source
The present study was a post hoc evaluation of a nationwide survey completed in October 2015 which was conducted to assess the burden of GI symptoms amongst adults in the US.15,16 The survey was based on MyGiHealth, a mobile app that systematically collects GI symptom information using a computer algorithm called Automated Evaluation of GI Symptoms (AEGIS). We described the AEGIS algorithm in detail elsewhere.17 Briefly, AEGIS first asked individuals which among 8 GI symptoms they have recently experienced, including: (1) constipation, (2) abdominal pain, (3) bloat/gas, (4) diarrhea, (5) fecal incontinence, (6) heartburn/reflux, (7) dysphagia, and (8) nausea/vomiting. These symptoms are based on the National Institutes of Health (NIH) Gastrointestinal Patient Reported Outcomes Measurement Information System (GI-PROMIS) framework.18–20 For each reported symptom, AEGIS guided patients through the corresponding GI-PROMIS questionnaires to measure symptom severity as compared to population norms. Afterwards, AEGIS guided respondents through questions drawn from a library of over 300 symptoms attributes measuring the timing, severity, frequency, location, quality, bother, and character of their GI symptoms, along with relevant comorbidities and demographics.
Study Population
This nationwide survey was comprised of 71 812 adults (at least 18 years of age) identified from an opt-in list developed by a contract research company (Cint) to represent the general US population, with recruitment quotas for age, sex, and geographic location. The Cint platform utilizes a reward system based on marketplace points. The number of points awarded is driven by the length of interview. On reaching a certain redemption level, panelists can redeem their rewards through different online payment partners linked to Cint. The size of the redemption is based on the number of points earned. Panelists can choose to receive their rewards in cash sent to their bank accounts or they can shop online with participating merchants or make payments to a charity. Incentive levels have been set to encourage long-term participation and to discourage professional respondents who seek to take surveys only to obtain payment.
Subjects were identified with IBS-C and CIC who reported experiencing constipation within the past week to limit recall bias (see Supplementary Table for definitions) in comparison to Rome criteria. Demographic data were extracted from the original survey regarding age, sex, race/ethnicity, education, marital status, employment status, household income, and number of comorbid medical conditions. Participants contributed demographic and GI symptom-specific information within the prior 7 days to this survey which were standardized using the adaptive computer-based GI-PROMIS instrument.18 Seven broad categories of GI symptoms were assessed (constipation, fecal incontinence, abdominal pain, bloating, dysphagia, heartburn, and nausea). Based on survey responses, GI PROMIS scores were assigned to symptomatic subjects on a percentile range from 1 to 100. Asymptomatic patients were not assigned a score. Scores were reported for the composite of reported GI symptoms as well as for each symptom category.
Endpoints
Our primary endpoint was the overall GI-PROMIS score representing a composite assessment of combined GI symptom frequency and severity, for the IBS-C and CIC populations in an analysis adjusted for demographic variables. Secondary endpoints included GI-PROMIS scores for specific GI symptoms in IBS-C and CIC as well as the prevalence of specific GI symptoms in the IBS-C population relative to the CIC population. We also assessed the odds of reporting specific GI symptoms in the IBS-C population relative to the CIC population.
Statistical Methods
We used post-stratification to adjust for over- and under-sampling of subgroups in the National GI Survey. Specifically, population weights based on latest US Census data for age, sex, and race/ethnicity were applied to the sample data in order to produce population estimates.21,22 Differences in demographics between IBS-C and CIC populations were assessed by Student’s t test for continuous variables. A corrected, weighted Pearson chi-square test was utilized for nominal variables.
Descriptive statistics were used to report GI-PROMIS scores with 95% confidence interval (CI) estimates, as well as prevalence of symptoms. Differences in GI-PROMIS scores for the composite symptom analysis as well as specific GI symptoms were determined with Student’s t test. A corrected, weighted Pearson chi-square test was calculated for comparison of GI symptom prevalence in IBS-C and CIC. The odds of specific GI symptoms in the IBS-C relative to CIC population were reported as odds ratios with 95% CI. Logistic regression was used to adjust for demographic variables in the analysis of symptom prevalence, and linear regression used to assess for demographic variables in the analysis of GI-PROMIS scores. Ordered logistic regression adjusted for demographic variables was used to analyze differences between groups regarding responses to individual constipation questions. Analysis was performed using Stata 13.1 software (StataCorp LP, College Station, TX, USA).
Results
Out of the 71 812 US adults who completed the surveys, we identified 275 subjects with IBS-C and 734 subjects with CIC who reported experiencing constipation within the past week (Table 1). Demographic variables of age, sex, and race/ethnicity distribution were similar in both groups, however CIC subjects had higher prevalence of university graduation, marriage/long term relationship status, full-time employment, and income.
Table 1.
Population Characteristics and Demographics
| Characteristic | IBS-C | CIC |
|---|---|---|
| Population (n) | 275 | 734 |
| Age | 42.7 ± 12.6 | 43.3 ± 13.2 |
| Female | 77.5% | 78.1% |
| Race | ||
| Non-Hispanic white | 77.8% | 80.3% |
| Non-Hispanic black | 6.2% | 6.5% |
| Hispanic | 9.5% | 8.2% |
| Asian | 1.5% | 1.9% |
| Other | 5.1% | 3.1% |
| At least college graduatea | 32.0% | 42.1% |
| Married/long term relationshipa | 62.6% | 69.4% |
| Employed or full-time | 50.9% | 51.1% |
| Income 50 k or greatera | 38.2% | 48.1% |
Denotes statistically significant difference between irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC) (P < 0.05).
Composite Gastrointestinal Symptom Frequency and Severity
The mean composite GI-PROMIS score for the IBS-C group was higher (251.1, 95% CI 230.0 to 273.1) than for the CIC group (177.8, 95% CI 167.2 to 188.4). This was statistically significant (P < 0.001) adjusting for demographic variables.
Individual Gastrointestinal Symptom Frequency and Severity
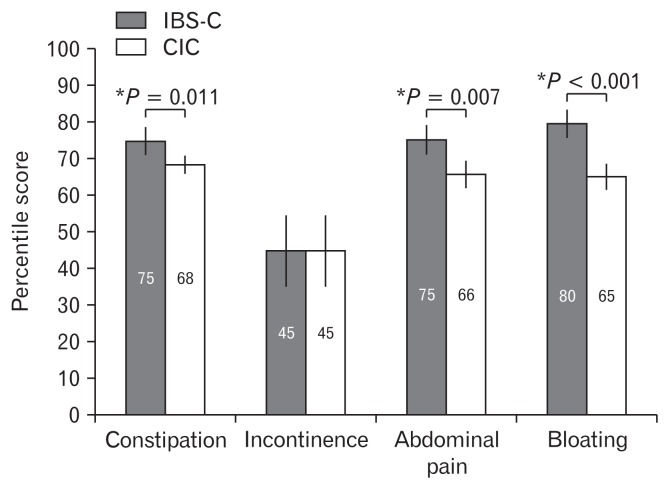
Four lower GI complaints were assessed using the GI-PROMIS score in this survey (Fig. 1). Regarding bowel symptoms, composite frequency and severity of constipation (P = 0.011) but not incontinence (P = 0.389) was greater in IBS-C compared to CIC. For abdominal symptoms, GI-PROMIS scores for abdominal pain (P = 0.007) and bloating (P < 0.001) were higher in IBS-C than in CIC adjusting for demographic variables.
Figure 1.
Gastrointestinal patient reported outcomes measurement information system scores for lower gastrointestinal symptoms as a composite measure of frequency and severity. Abdominal pain, bloating, and constipation, but not fecal incontinence, were more frequent/severe in irritable bowel syndrome with constipation (IBS) than in chronic idiopathic constipation (CIC).
We identified differences between IBS-C and CIC subjects regarding responses to constipation-pertinent questions within the GI-PROMIS questionnaire (Table 2). Answers to questions involving straining and incomplete bowel movements were generally similar between IBS-C and CIC subjects. However, IBS-C subjects were more likely to report use of digitation as well as more severe/frequent symptoms of passing hard or lumpy stools. IBS-C subjects were also more likely to report more frequent rectal or anal pain, however there was no statistically significant difference in rectal/anal pain severity. Interestingly, while questions pertinent to abdominal “pain” suggested more severe and frequent symptoms in IBS-C subjects, there was no statistically significant difference in abdominal “discomfort” symptoms between IBS-C and CIC subjects.
Table 2.
Differences Between Chronic Idiopathic Constipation and Irritable Bowel Syndrome With Constipation Subjects in Responses to Constipation Questions From Gastrointestinal Patient Reported Outcomes Measurement Information System Questionnaire
| Question | OR (95% CI) of more severe/frequent symptom in IBS-C relative to CIC | P-value |
|---|---|---|
| In the past 7 days, how often did you pass very hard or lumpy stools? | 1.47 (1.00 to 2.16) | 0.049a |
| In the past 7 days, how much did hard or lumpy stools bother you? | 1.41 (1.01 to 1.98) | 0.044a |
| In the past 7 days, how often did you strain while trying to have bowel movements? | 1.18 (0.83 to 1.67) | 0.359 |
| In the past 7 days, how much did you usually strain while trying to have a bowel movement? | 1.04 (0.75 to 1.44) | 0.819 |
| In the past 7 days, how much did straining during bowel movements bother you? | 1.17 (0.84 to 1.65) | 0.353 |
| In the past 7 days, how often did you feel pain in your rectum or anus while trying to have a bowel movement? | 1.60 (1.14 to 2.25) | 0.007a |
| In the past 7 days, at its worst how would you rate the pain in your rectum or anus during bowel movements? | 1.31 (0.95 to 1.81) | 0.100 |
| In the past 7 days, how often after a bowel movement did you feel unfinished - that is that you had not passed all your stool? | 1.45 (0.98 to 2.15) | 0.064 |
| In the past 7 days, how often did you use your finger or toilet paper to get out a stool? | 1.48 (1.03 to 2.14) | 0.036 |
| In the past 7 days, how often did you have belly pain? | 1.96 (1.33 to 2.90) | 0.001 |
| In the past 7 days, at its worst how would you rate your belly pain? | 1.68 (1.04 to 2.70) | 0.034 |
| In the past 7 days, how much did belly pain interfere with your day-to-day activities? | 1.99 (1.32 to 3.00) | 0.001 |
| In the past 7 days, how much did belly pain bother you? | 1.66 (1.10 to 2.50) | 0.015 |
| In the past 7 days, how often did you have discomfort in your belly? | 1.15 (0.77 to 1.72) | 0.490 |
Denotes statistically significant difference between irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC) (P < 0.05).
Differences are reported as odds ratios of a more severe or frequent symptom in IBS-C relative to CIC. A higher odds ratio suggests a more severe or frequent symptom in a subject with IBS-C than a subject with CIC.
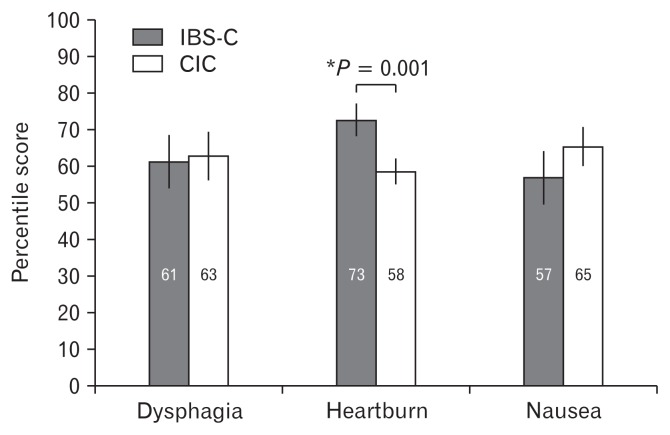
Three upper GI symptoms (dysphagia, heartburn, nausea) were assessed. Composite frequency and severity of heartburn (P = 0.001) was more severe in IBS-C than CIC, though nausea (P = 0.167) and dysphagia (P = 0.327) were not. GI-PROMIS scores for upper GI symptoms are reported in Figure 2.
Figure 2.
Gastrointestinal patient reported outcomes measurement information system scores for upper gastrointestinal symptoms as a composite measure of frequency and severity. Heartburn, but not dysphagia or nausea, was more frequent/severe in irritable bowel syndrome with constipation (IBS) than in chronic idiopathic constipation (CIC).
Odds of Reporting Gastrointestinal Symptoms for Irritable Bowel Syndrome With Constipation Versus Chronic Idiopathic Constipation
Regarding lower GI abdominal symptoms, the odds of reporting abdominal pain (OR, 4.3; 95% CI, 2.9 to 6.6), bloating (OR, 1.9; 95% CI, 1.3 to 2.8), and incontinence (OR, 2.9; 95% CI, 1.3 to 6.3) were greater in IBS-C than CIC. There was no statistically significant difference in odds for reporting of upper GI symptoms of dysphagia (OR, 1.2; 95% CI, 0.7 to 2.2), heartburn (OR, 1.1; 95% CI, 0.7 to 1.5), or nausea (OR, 1.4; 95% CI, 0.9 to 2.2) between IBS-C and CIC. Prevalence of individual GI symptoms is reported in Figure 3.
Figure 3.
Prevalence of gastrointestinal symptoms in irritable bowel syndrome with constipation (IBS) and chronic idiopathic constipation (CIC). Abdominal pain, bloating, and incontinence (but not dysphagia, heartburn, or nausea) were more prevalent in constipation-predominant IBS than in CIC.
Discussion
In this study, we evaluated and compared the severity and prevalence of GI symptoms among IBS-C or CIC patients who were symptomatic during the prior week, identified from a large, representative sample of the US population. Given the construct of symptom-based diagnostic criteria which distinguish between IBS-C and CIC on the presence of abdominal pain, it is not surprising that abdominal symptoms (abdominal pain and bloating) were more severe and more frequent in patients with IBS-C when compared to those with CIC. Interestingly, we also found that bowel-related symptoms, such as stool frequency and consistency, were more severe in IBS-C than CIC patients. It then follows that IBS-C patients had a significantly higher composite assessment of global GI symptoms than patients with CIC. The results of this study raise important questions about the current symptom-based construct which dichotomizes IBS-C and CIC into separate and distinct disorders.
Our findings are consistent with prior cross-sectional surveys which evaluated the symptom experience in IBS-C and CIC patients. A recent nationwide US-based survey which compared symptoms in IBS-C and CIC found more bothersome abdominal symptoms (abdominal pain, bloating, discomfort, and cramping) and constipation symptoms in those with IBS-C.6 Another survey enrolled consecutive unselected outpatients in GI secondary care from 2 Canadian hospitals reported similar results.10 Two recent large surveys from Spain11 and China12 reported less of a difference in the symptom experience reported by patients with IBS-C and CIC. Though IBS-C patients had a significant increase in the frequency of straining when compared to CIC patients, other symptoms yielded inconsistent findings or were not significantly different between groups.
IBS-C and functional constipation, also known as CIC, are classified as separate and distinct disorders according to the Rome diagnostic criteria. CIC is defined by bowel symptoms and IBS-C by abdominal pain in addition to bowel symptoms.8 While more severe in IBS-C, abdominal symptoms (pain and bloating) were still common in CIC subjects completing the survey. Acknowledging that symptom frequency and severity can vary over time, the fact that almost half of the CIC group reported abdominal symptoms confirms that these symptoms are common in CIC and thus, the distinction between these 2 groups of patients in clinical practice may be difficult.
It is possible that IBS-C and CIC could represent a spectrum of constipation related disease rather than 2 separate and distinct disorders. Using Rome III diagnostic criteria, a prior survey of primary care patients with either IBS-C or CIC found that approximately one-third of patients migrated to the alternate diagnosis (IBS-C to CIC, or CIC to IBS-C by Rome III criteria) after one year of follow-up.9 It is likely that individuals experience varying levels of abdominal symptoms over time based upon contributions from intrinsic factors including motility, degree of fecal loading, visceral hypersensitivity, gut permeability, and immune activation and further influenced by extrinsic factors such as microbiome, food, and stress. In a study evaluating platelet-depleted plasma serotonin levels in subjects with IBS-C or CIC, prior authors reported platelet-depleted plasma serotonin levels varying with pain and stool thresholds, but that both IBS-C and CIC appeared to have similar characteristic symptom and physiologic overlap.23
The prevalence of abdominal discomfort appeared similar in IBS-C and CIC cohorts. Previous iterations of the Rome criteria (including Rome III) defined IBS by the presence of either abdominal pain or discomfort, however the updated Rome IV criteria removed abdominal discomfort from the definition. This was done mostly because of the lack of cohesive patient understanding and even agreement on the definition for abdominal discomfort across languages and cultures in translated versions of the Rome diagnostic questionnaire.24 However, this is not to suggest that abdominal discomfort might not be an important symptom in IBS. Moreover, only 79% of IBS-C patients experienced abdominal pain within the last week in this study, with the remaining patients instead reporting abdominal discomfort. Abdominal discomfort questions included in GI-PROMIS were critically evaluated both qualitatively to confirm consistent patient understanding and quantitatively in a validation cohort to derive the score distribution. While our findings suggest similarities in abdominal discomfort across IBS-C and CIC, further cross-cultural studies are warranted to confirm whether IBS-C and CIC patients experience abdominal discomfort similarly and to understand differences in the symptom experience.
Overlap of IBS-C and CIC with upper GI disorders has also been previously evaluated. 33–42% of individuals with IBS-C also report gastroesophageal reflux disease symptoms and functional dyspepsia (75–89% of IBS-C individuals).13,25 In contrast, another study reported that co-morbid gastroesophageal reflux disease as well as dyspepsia only occured in 6% of CIC individuals.12 However, our present study found that while heartburn was more severe in IBS-C than CIC, upper GI symptoms and especially heartburn were not uncommon in CIC (a traditionally lower GI disorder) and there was no difference in symptom prevalence compared to IBS.
Some authors have suggested a painful “subtype” of CIC which might be in-between both disease states.26,27 While not meeting Rome criteria for IBS, these patients can still experience greater use of healthcare resources and worse quality of life than nonpainful CIC counterparts. Another study employed latent class analysis to identify a subgroup of chronically constipated patients differentiated by severity of GI symptoms rather than presence of specific abdominal or bowel symptoms.3 Fifty-six point seven percent of the latent class with more severe symptoms had IBS-C by Rome III criteria, compared to 25% of the latent class with less severe symptoms. These findings correlate with our study reporting more severe symptoms in IBS-C.
One potential limitation of this study was the low prevalence of IBS-C and CIC in our survey population, even lower than the prevalence reported in other cross-sectional surveys3,6,11 and systematic reviews.28,29 The primary reason for this is likely our use of the validated GI-PROMIS system, which assesses symptoms over the prior 7 days unlike the Rome questionnaire. The prevalence of IBS-C and CIC are already well reported, and our present study design is not intended to assess prevalence of IBS-C and CIC. In light of the waxing and waning nature of symptoms in these diseases,30 this study was designed to assess IBS-C and CIC patients with symptoms during the past week in an effort to limit recall bias and increase power of detecting interpretable and meaningful differences between IBS-C and CIC populations. As such, the time frame for questions was in line with published criteria for development of NIH PROMIS instruments designed for the intended purpose of this study.31 In addition, one could argue that restricting the analysis to a 1-week time frame provides the most accurate representation of the clinical experience in actively symptomatic patients and might reduce problems with recall bias that could accompany studies which require longer recall periods.
Finally, there are 3 sufficiently independent upper GI symptom domains within the framework of the GI-PROMIS instrument which themselves encompass a variety of individual GI complaints. Supported by a prospective validation trial (10.1038/ajg.2014.237), an individual complaint would primarily affect only a single GI-PROMIS domain and therefore not have an outsized effect on the overall GI-PROMIS score. While the instrument has broad applications in quantitatively assessing clinically meaningful changes in overall GI symptomatology, a weakness of this instrument is that individual complaints are not reported. Additional instruments in future studies would likely prove valuable in detailing upper GI experiences among IBS-C and CIC individuals.
In summary, we found that abdominal symptoms were common in IBS-C and CIC, but that individual symptoms including bowel symptoms were generally more severe in IBS-C patients. Upper GI symptoms were common in both conditions. These findings have important practical implications for patients and providers. The current regulatory and payer environment is predicated upon distinguishing between IBS-C and CIC. By doing so, this may create confusion and potentially deleterious barriers to the use of different doses of pharmaceuticals which are specifically indicated for one or the other disorder. For example, there are different doses of both lubiprostone and linaclotide which are approved by the US Food and Drug Administration for IBS-C and CIC. By separating the 2 conditions, it is also possible that we are underestimating the overall prevalence and personal and economic burden of constipation-related disorders. While it is certainly important to clinically phenotype patients in a way that embraces their overall illness experience, one wonders if the current paradigm of separating between IBS-C and CIC should be reconsidered to reflect the growing body of evidence which supports the notion that they represent a spectrum of disease which tracks by symptom frequency.
Supplementary Information
Footnotes
Note: To access the supplementary table mentioned in this article, visit the online version of Journal of Neurogastroenterology and Motility at http://www.jnmjournal.org/, and at https://doi.org/10.5056/jnm17112.
Financial support: The National GI Survey was supported by Ironwood Pharmaceuticals.
Conflicts of interest: Drs Spiegel and Chey are consultants for Ironwood Pharmaceuticals. Drs Spiegel and Chey are also patent holders and principals at My Total Health. Dr Chey is a consultant for Allergan. Dr Almario has a stock option grant in My Total Health. Dr Shah does not have any relevant disclosures.
Author contributions: Eric D Shah, Christopher V Almario, Brennan M R Spiegel, and William D Chey were involved in study concept and design and interpretation of data; Christopher V Almario conducted data analysis; Eric D Shah authored the initial draft of the manuscript; and all authors critically revised the manuscript and approved the final copy.
References
- 1.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187. e1–e3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171–1185. doi: 10.1046/j.1365-2036.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 3.Koloski NA, Jones M, Young M, et al. Differentiation of functional constipation and constipation predominant irritable bowel syndrome based on Rome III criteria: a population-based study. Aliment Pharmacol Ther. 2015;41:856–866. doi: 10.1111/apt.13149. [DOI] [PubMed] [Google Scholar]
- 4.Johanson JF, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther. 2007;25:599–608. doi: 10.1111/j.1365-2036.2006.03238.x. [DOI] [PubMed] [Google Scholar]
- 5.Talley NJ, Holtmann G, Agréus L, Jones M. Gastrointestinal symptoms and subjects cluster into distinct upper and lower groupings in the community: a four nations study. Am J Gastroenterol. 2000;95:1439–1447. doi: 10.1111/j.1572-0241.2000.02075.x. [DOI] [PubMed] [Google Scholar]
- 6.Heidelbaugh JJ, Stelwagon M, Miller SA, Shea EP, Shey WD. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. Am J Gastroenterol. 2015;110:580–587. doi: 10.1038/ajg.2015.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palsson OS, Whitehead WE, van Tilburg MAL, et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. doi: 10.1053/j.gastro.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. doi: 10.1053/j.gastro.2016.02.031. Published Online First: 18 Feb 2016. [DOI] [Google Scholar]
- 9.Wong RK, Palsson OS, Turner MJ, et al. Inability of the Rome III criteria to distinguish functional constipation from constipation-subtype irritable bowel syndrome. Am J Gastroenterol. 2010;105:2228–2234. doi: 10.1038/ajg.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford AC, Bercik P, Morgan DG, Bolino C, Pintos-Sanchez MI, Moayyedi P. Characteristics of functional bowel disorder patients: a cross-sectional survey using the Rome III criteria. Aliment Pharmacol Ther. 2014;39:312–321. doi: 10.1111/apt.12573. [DOI] [PubMed] [Google Scholar]
- 11.Rey E, Balboa A, Mearin F. Chronic constipation, irritable bowel syndrome with constipation and constipation with pain/discomfort: similarities and differences. Am J Gastroenterol. 2014;109:876–884. doi: 10.1038/ajg.2014.18. [DOI] [PubMed] [Google Scholar]
- 12.Zhao Y-F, Ma XQ, Wang R, et al. Epidemiology of functional constipation and comparison with constipation-predominant irritable bowel syndrome: the systematic investigation of gastrointestinal diseases in China (SILC) Aliment Pharmacol Ther. 2011;34:1020–1029. doi: 10.1111/j.1365-2036.2011.04809.x. [DOI] [PubMed] [Google Scholar]
- 13.Vakil N, Stelwagon M, Shea EP, Miler S. Symptom burden and consulting behavior in patients with overlapping functional disorders in the US population. United European Gastroenterol J. 2016;4:413–422. doi: 10.1177/2050640615600114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park KS, Jee SR, Lee BE, et al. Nationwide multicenter study for overlaps of common functional gastrointestinal disorders in korean patients with constipation. J Neurogastroenterol Motil. 2017;23:569–577. doi: 10.5056/jnm17033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Almario CV, Chey WD, Spiegel B. Tu1066 burden of gastrointestinal symptoms in the united states: results from a survey of over 71,000 americans. Gastroenterology. 2016;150(suppl 1):S831–S832. doi: 10.1016/S0016-5085(16)32813-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almario CV, Almario AA, Cunningham ME, et al. Old farts – fact or fiction? Results from a population-based survey of 16,000 americans examining the association between age and flatus. Clin Gastroenterol Hepatol. 2017;15:1308–1310. doi: 10.1016/j.cgh.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 17.Almario CV, Chey W, Kaung A, et al. Computer-generated vs. physician-documented history of present illness (HPI): results of a blinded comparison. Am J Gastroenterol. 2015;110:170–179. doi: 10.1038/ajg.2014.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spiegel BM, Hays RD, Bolus R, et al. Development of the NIH patient-reported outcomes measurement information system (PROMIS) gastrointestinal symptom scales. Am J Gastroenterol. 2014;109:1804–1814. doi: 10.1038/ajg.2014.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spiegel BM. Patient-reported outcomes in gastroenterology: clinical and research applications. J Neurogastroenterol Motil. 2013;19:137–148. doi: 10.5056/jnm.2013.19.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagaraja V, Hays RD, Khanna PP, et al. Construct validity of the patient-reported outcomes measurement information system gastrointestinal symptom scales in systemic sclerosis. Arthritis Care Res. 2014;66:1725–1730. doi: 10.1002/acr.22337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Population Distribution by Race/Ethnicity. Henry J Kaiser Family Foundation; [accessed 11 March, 2018]. Avaliable from URL: https://www.kff.org/statedata/ [Google Scholar]
- 22.Howden L, Meyer J. Age and Sex Composition: 2010. United states cescus bureau; [accessed 11 March, 2018]. Avaliable from URL: http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. [Google Scholar]
- 23.Shekhar C, Monaghan PJ, Morris J, et al. Rome III functional constipation and irritable bowel syndrome with constipation are similar disorders within a spectrum of sensitization, regulated by serotonin. Gastroenterology. 2013;145:749–757. doi: 10.1053/j.gastro.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Spiegel BM, Bolus R, Agarwal N, et al. Measuring symptoms in the irritable bowel syndrome: development of a framework for clinical trials. Aliment Pharmacol Ther. 2010;32:1275–1291. doi: 10.1111/j.1365-2036.2010.04464.x. [DOI] [PubMed] [Google Scholar]
- 25.Talley NJ, Dennis EH, Schettler-Duncan VA, Lacy BE, Olden KW, Crowel MD. Overlapping upper and lower gastrointestinal symptoms in irritable bowel syndrome patients with constipation or diarrhea. Am J Gastroenterol. 2003;98:2454–2459. doi: 10.1111/j.1572-0241.2003.07699.x. [DOI] [PubMed] [Google Scholar]
- 26.Drossman DA, Morris C, Hu Y, et al. Further characterization of painful constipation (PC): clinical features over one year and comparison with IBS. J Clin Gastroenterol. 2008;42:1080–1088. doi: 10.1097/MCG.0b013e31815146f9. [DOI] [PubMed] [Google Scholar]
- 27.Cremonini F, Lembo A. IBS with constipation, functional constipation, painful and non-painful constipation: e pluribus…plures? Am J Gastroenterol. 2014;109:885–886. doi: 10.1038/ajg.2014.119. [DOI] [PubMed] [Google Scholar]
- 28.Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750–759. doi: 10.1111/j.1572-0241.2004.04114.x. [DOI] [PubMed] [Google Scholar]
- 29.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halder SL, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Melton LJ, 3rd, Talley NJ. Natural history of functional gastrointestinal disorders: a 12-year longitudinal population-based study. Gastroenterology. 2007;133:799–807. doi: 10.1053/j.gastro.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Cella D, Yount S, Rothrock N, et al. The patient-reported outcomes measurement information system (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care. 2007;45(5 suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.