Key Points
Question
What are the spatial and temporal trends in mortality due to alcohol use disorders, drug use disorders, self-harm, and interpersonal violence among US counties from 1980 to 2014?
Findings
In this study of 2 848 768 deaths in the United States from 1980 to 2014, mortality rates varied widely among counties and increased by 618.3% for drug use disorders but decreased by 8.1% for alcohol use disorders, 6.0% for self-harm, and 44.9% for interpersonal violence. Mortality rates due to drug use disorders increased in every county, while mortality rates due to alcohol use disorders, self-harm, and interpersonal violence increased in some counties and decreased in others.
Meaning
Between 1980 and 2014, there were important differences among US counties in the level and trend in mortality rates due to alcohol use disorders, drug use disorders, self-harm, and interpersonal violence.
Abstract
Importance
Substance use disorders, including alcohol use disorders and drug use disorders, and intentional injuries, including self-harm and interpersonal violence, are important causes of early death and disability in the United States.
Objective
To estimate age-standardized mortality rates by county from alcohol use disorders, drug use disorders, self-harm, and interpersonal violence in the United States.
Design and Setting
Validated small-area estimation models were applied to deidentified death records from the National Center for Health Statistics (NCHS) and population counts from the US Census Bureau, NCHS, and the Human Mortality Database to estimate county-level mortality rates from 1980 to 2014 for alcohol use disorders, drug use disorders, self-harm, and interpersonal violence.
Exposures
County of residence.
Main Outcomes and Measures
Age-standardized mortality rates by US county (N = 3110), year, sex, and cause.
Results
Between 1980 and 2014, there were 2 848 768 deaths due to substance use disorders and intentional injuries recorded in the United States. Mortality rates from alcohol use disorders (n = 256 432), drug use disorders (n = 542 501), self-harm (n = 1 289 086), and interpersonal violence (n = 760 749) varied widely among counties. Mortality rates decreased for alcohol use disorders, self-harm, and interpersonal violence at the national level between 1980 and 2014; however, over the same period, the percentage of counties in which mortality rates increased for these causes was 65.4% for alcohol use disorders, 74.6% for self-harm, and 6.6% for interpersonal violence. Mortality rates from drug use disorders increased nationally and in every county between 1980 and 2014, but the relative increase varied from 8.2% to 8369.7%. Relative and absolute geographic inequalities in mortality, as measured by comparing the 90th and 10th percentile among counties, decreased for alcohol use disorders and interpersonal violence but increased substantially for drug use disorders and self-harm between 1980 and 2014.
Conclusions and Relevance
Mortality due to alcohol use disorders, drug use disorders, self-harm, and interpersonal violence varied widely among US counties, both in terms of levels of mortality and trends. These estimates may be useful to inform efforts to target prevention, diagnosis, and treatment to improve health and reduce inequalities.
This population epidemiology study estimates county-level mortality rates for alcohol use disorders, drug use disorders, self-harm, and interpersonal violence in the United States between 1980 and 2014.
Introduction
Substance use disorders (ie, drug use disorders and alcohol use disorders) and intentional injuries (ie, self-harm and interpersonal violence) impose a significant health and financial burden in the United States. In 2015, substance use disorders and intentional injuries comprised 3.9% of all deaths. Because substance use disorders and intentional injuries disproportionately impact young and middle-aged adults, nearly 10% of all years of life lost were due to these causes. Moreover, recent research has implicated so-called deaths of despair, including substance use disorders and self-harm, in contributing to the increasing rates of midlife mortality among certain demographic groups.
A number of studies have previously documented significant geographic variation in mortality rates from self-harm, interpersonal violence, and drug poisoning. Information on how mortality rates vary spatially at a local level is an important input for developing an effective public health and policy response. However, existing studies of spatial patterns in mortality from self-harm and interpersonal violence are primarily from the 1980s and 1990s, and more timely data on local-level trends are unavailable. Additionally, studies of drug poisoning have failed to distinguish between accidental and intentional overdoses (ie, overdoses intended to self-inflict harm or to harm others), despite important differences in the underlying etiology of unintentional and intentional overdoses.
More recently, a new small-area methodology was used to estimate county-level trends in mortality from 21 major causes of death. Among these 21 categories were mental and substance use disorders (which combines both drug use disorders and alcohol use disorders as well as deaths due to several mental health disorders) and intentional injuries (which combines self-harm and interpersonal violence).
This study utilizes the same small-area estimation method to describe county-level trends in mortality rates separately for 4 causes: alcohol use disorders, drug use disorders, self-harm, and interpersonal violence from 1980 to 2014.
Methods
This study used previously reported methods that are described briefly in this section. This research received institutional review board approval from the University of Washington. Informed consent was not required because the study used deidentified data and was retrospective.
Data
This analysis used deidentified death records from the National Center for Health Statistics (NCHS) and population counts from the US Census Bureau, NCHS, and the Human Mortality Database. Deaths and population were tabulated by county of residence, age group (0, 1-4, 5-9, …, 70-74, 75-79, and ≥80 years), sex, year, and (for deaths only) underlying cause. County-level covariates, including levels of education, income, race/ethnicity, Native American reservations, and population density were derived from data provided by the US Census Bureau and NCHS (eTable 1 in the Supplement). Counties were combined as needed to ensure historically stable units of analysis (eTable 2 in the Supplement).
Cause List and Garbage Redistribution
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) cause list was used for this analysis. This cause list is arranged hierarchically in 4 levels, and within each level, the list is exhaustive and mutually exclusive. eTable 3 (in the Supplement) lists all causes in the GBD cause list and the International Classification of Diseases, Ninth Revision (ICD-9) and ICD-10 codes that correspond to each cause. The focus of this study was on substance use disorders and intentional injuries, specifically: alcohol use disorders (ICD-9 codes 291-291.9, 303-303.93, 305.0-305.03, 357.5, 790.3, E860-E860.19; ICD-10 codes F10-F10.99, G31.2, G72.1, P04.3, Q86.0, R78.0, X45-X45.9), drug use disorders (ICD-9 codes 292-292.9, 304.0-304.83, 305, 305.1-305.93, 760.7-760.79, E850-E850.29; ICD-10 codes F11-F16.99, F18-F19.99, P04.4-P04.49, P96.1, R78.1-R78.5), self-harm (ICD-9 codes E950-E959; ICD-10 codes X60-X84.9, Y87.0), and interpersonal violence (ICD-9 codes E960-E969; ICD-10 codes X85-Y08.9, Y87.1). However, all causes of death in the GBD cause list were analyzed concurrently.
Previous studies have documented the existence of “garbage codes”—insufficiently specific or implausible cause of death codes used in death registration data that may lead to misleading geographic and temporal patterns. Algorithms developed for the GBD (and described in detail elsewhere) were used to reallocate deaths assigned one of these garbage codes to plausible alternatives. First, plausible target causes were assigned to each garbage code or group of garbage codes. Second, deaths were reassigned to specified target codes according to proportions derived in 1 of 4 ways: (1) published literature or expert opinion; (2) regression models; (3) according to the proportions initially observed among targets; and (4) for HIV/AIDs specifically, by comparison to years before HIV/AIDS became widespread.
Small-Area Models
Bayesian, spatially explicit mixed-effects regression models were estimated separately for each cause and for males and females. The model was specified as
| Dj,t,a ∼ Poisson(mj,t,a · Pj,t,a) log(mj,t,a) = β0 + β1Xj,t + γ1,a,t + γ2,j + (γ3,j · t + γ4,j,t) + (γ5,j · α + γ6,j,a) |
in which Dj,t,a indicates the number of deaths, Pj,t,a indicates the population, and mj,t,a indicates the underlying mortality rate for a given county (j), year (t), and age group (a). The model for mj,t,a contained 6 components: an intercept (β0); fixed covariate effects (β1); random age-time effects (γ1,a,t); random spatial effects (γ2,j); random space-time effects (γ3,j and γ4,j,t); and random space-age effects (γ5,j and γ6,j,a). The model incorporated 7 covariates: the proportion of the adult population who graduated from high school, the proportion of the population that is Hispanic (regardless of race), the proportion of the population that is black (regardless of Hispanic ethnicity), the proportion of the population that is a race other than black or white (regardless of Hispanic ethnicity), the proportion of a county that is contained within a state or federal Native American reservation, the median household income, and the population density. The random effects γ1, γ2, γ3, and γ5 were assumed to follow conditional autoregressive distributions, which allow for smoothing over adjacent age groups and years (γ1) or counties (γ2, γ3, and γ5). The random effects γ4 and γ6 were assumed to follow independent mean-zero normal distributions.
Models were fit using the Template Model Builder Package in the R statistical software (version 3.2.4). One thousand draws of mj,t,a were taken from the posterior distribution and then raked (ie, scaled along multiple dimensions) by cause and by county to ensure consistency between levels of the cause hierarchy as well as with national estimates from the GBD. Mortality rates for both sexes combined were calculated from the population-weighted average of the male and female mortality rates. Age-standardized mortality rates were calculated using the US 2010 census population as the standard. Years of life lost were calculated by multiplying the mortality rate by population by age-specific life expectancy from the reference life table used in the GBD and then summing across all ages. Point estimates were calculated from the mean of all draws, and 95% uncertainty intervals (UIs) were calculated from the 2.5th and 97.5th percentiles. Changes over time were considered statistically significant if the posterior probability of an increase (or decrease) was at least 95% (ie, if there was an increase (or decrease) in more than 95% of the 1000 posterior draws). Changes over the full time range (1980-2014) were the primary focus; however, changes between 1980 and 2000, as well as changes between 2000 and 2014, were also considered because preliminary results indicated a reversal in trends from 2000 to 2014 compared with 1980 to 2000 for self-harm.
No explicit correction for multiple testing (ie, across multiple counties) was applied; however, the risk of spuriously detecting changes due to multiple testing was mitigated by modeling all counties simultaneously. County-level inequality in mortality rates was quantified by comparing the 10th and 90th percentile rates among counties: the difference between the 10th and 90th percentile was used as a measure of absolute geographic inequality and the ratio between the 10th and 90th percentile was used as a measure of relative geographic inequality.
Results
A total of 2 848 768 deaths due to substance use disorders and intentional injuries were recorded in the United States between 1980 and 2014. Of these deaths, 73.9% were originally assigned ICD codes that map exclusively to 1 of these 4 causes, including 91.1% of deaths due to alcohol use disorders, 15.0% of deaths due to drug use disorders, 87.6% of deaths due to self-harm, and 88.6% of deaths due to interpersonal violence. ICD codes related to accidental poisonings (ICD-9: E850.3-E854.3, E854.8, E855-E855.6, E855.8-E855.9, E858-E858.9, E866-E866.9; ICD-10: X40-X44.9, X49-X49.9), which were redistributed primarily to substance use disorders among individuals aged 15 years and older and to unintentional poisonings among individuals younger than age 15 years, contributed 5.2% of deaths due to alcohol use disorders and 80.0% of deaths due to drug use disorders. ICD codes related to injury deaths for which intent was undetermined (ICD-9: E980-E989; ICD-10: Y10-Y34.9, Y86-87, Y87.2, Y89, Y89.9, Y90-Y99.9) contributed a further 1.2% of deaths due to alcohol use disorders, 1.4% of deaths due to drug use disorders, 6.7% of deaths due to self-harm, and 5.3% of deaths due to interpersonal violence. In addition, other garbage codes contributed 2.4% of deaths due to alcohol use disorders, 3.6% of deaths due to drug use disorders, 5.6% of deaths due to self-harm, and 6.1% of deaths due to interpersonal violence.
Alcohol Use Disorders
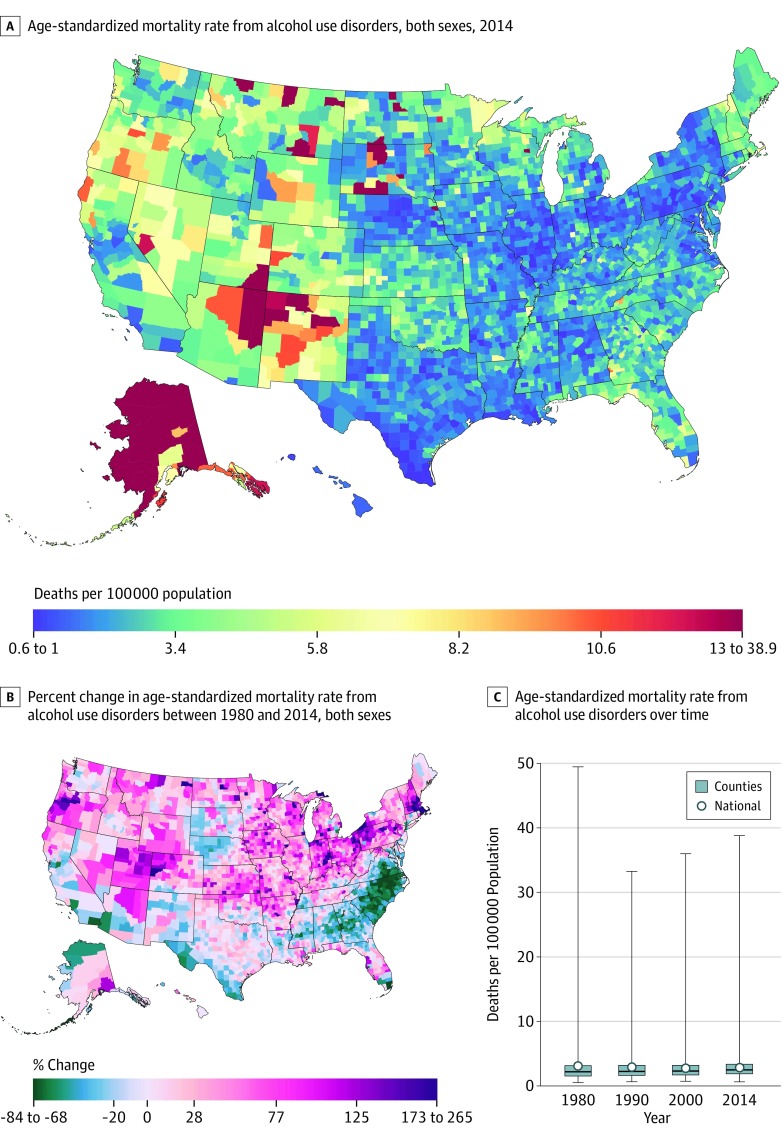
Between 1980 and 2014, there were 256 432 deaths due to alcohol use disorders recorded in the United States. In 2014, the age-standardized national mortality rate due to alcohol use disorders was 2.8 (95% UI, 2.7-3.0) deaths per 100 000 persons but varied among counties from 0.6 deaths per 100 000 to 38.8 deaths per 100 000 persons (Table 1). The distribution of counties, according to the mortality rate from alcohol use disorders, was highly skewed: in 2014, the 90th percentile among counties was 4.7 deaths per 100 000, compared with the maximum rate of 38.8 deaths per 100 000 persons (Table 1). Western counties generally experienced higher levels of mortality than counties in the East, and counties with especially high mortality rates, compared with the rest of United States (>12.9 deaths per 100 000 persons [top 1%]), were found in parts of Wisconsin, North Dakota, South Dakota, Nebraska, Montana, New Mexico, Arizona, Utah, and Alaska (Figure 1).
Table 1. National-Level Deaths, Years of Life Lost, and Age-Standardized Mortality Rates; and County-Level Distribution of Age-Standardized Mortality Rates in 1980, 2000, and 2014 Due to Alcohol Use Disorders, Drug Use Disorders, Self-harm, and Interpersonal Violence.
| Cause of Death | National Level | US County-Level Mortality Rates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deaths, No. in Thousands (95% Uncertainty Interval) | Years of Life Lost, No. in Thousands (95% Uncertainty Interval) | Age-Standardized Mortality Rate, No. of Deaths/100 000 Population (95% Uncertainty Interval) | No. of Deaths/100 000 Population | 90th/10th Percentile Ratiob | ||||||
| Minimum | 10th Percentile | Median | 90th Percentile | Maximum | 90th Minus 10th Percentilea | |||||
| Alcohol Use Disorders | ||||||||||
| 1980 | 5.8 (5.4-6.3) | 202.8 (189.1-217.7) | 3.1 (2.9-3.3) | 0.5 | 1.1 | 2.2 | 5.0 | 49.4 | 3.8 | 4.3 |
| 2000 | 7.2 (6.9-7.5) | 247.7 (238.0-256.8) | 2.8 (2.7-2.9) | 0.7 | 1.3 | 2.3 | 4.4 | 36.0 | 3.0 | 3.2 |
| 2014 | 9.4 (8.8-9.9) | 307.4 (289.7-324.5) | 2.8 (2.7-3.0) | 0.6 | 1.5 | 2.5 | 4.7 | 38.8 | 3.2 | 3.2 |
| Drug Use Disorders | ||||||||||
| 1980 | 3.3 (3.1-3.5) | 162.9 (154.0-174.8) | 1.4 (1.4-1.5) | 0.2 | 0.4 | 0.6 | 1.1 | 9.3 | 0.7 | 3.0 |
| 2000 | 14.3 (13.7-14.9) | 647.9 (621.2-676.8) | 4.9 (4.7-5.1) | 0.8 | 1.7 | 3.2 | 6.1 | 27.0 | 4.5 | 3.6 |
| 2014 | 33.1 (30.9-34.6) | 1455.5 (1359.6-1524.0) | 10.4 (9.7-10.9) | 1.6 | 4.1 | 8.6 | 17.0 | 57.1 | 12.9 | 4.2 |
| Self-harm | ||||||||||
| 1980 | 31.9 (30.6-33.1) | 1416.2 (1359.0-1473.9) | 14.7 (14.2-15.3) | 6.6 | 11.2 | 14.3 | 18.9 | 46.0 | 7.6 | 1.7 |
| 2000 | 34.7 (33.8-35.6) | 1458.0 (1418.9-1496.1) | 12.5 (12.2-12.8) | 5.6 | 10.4 | 13.7 | 18.7 | 66.2 | 8.3 | 1.8 |
| 2014 | 44.8 (43.2-46.4) | 1785.4 (1721.7-1847.8) | 13.9 (13.3-14.4) | 5.9 | 11.6 | 16.1 | 23.0 | 98.7 | 11.5 | 2.0 |
| Interpersonal Violence | ||||||||||
| 1980 | 24.7 (23.5-25.5) | 1322.1 (1257.9-1370.8) | 10.4 (9.9-10.8) | 1.5 | 2.5 | 6.0 | 15.5 | 50.4 | 13.0 | 6.1 |
| 2000 | 19.5 (19.0-20.1) | 1047.6 (1018.8-1076.9) | 6.8 (6.6-7.0) | 1.1 | 2.0 | 4.2 | 9.9 | 40.9 | 8.0 | 5.0 |
| 2014 | 18.3 (17.6-19.1) | 942.0 (905.8-982.3) | 5.7 (5.5-6.0) | 1.0 | 1.9 | 3.9 | 9.0 | 35.7 | 7.1 | 4.7 |
Measure of absolute geographic inequality.
Measure of relative geographic inequality.
Figure 1. County-Level Mortality From Alcohol Use Disorders.
A, Age-standardized mortality rate for both sexes combined in 2014.
B, Relative change in the age-standardized mortality rate for both sexes combined between 1980 and 2014. A and B, the color scale is truncated at approximately the first and 99th percentile as indicated by the range given in the color scale.
C, Age-standardized mortality rate for both sexes combined in 1980, 1990, 2000, and 2014. The bottom border of the boxes indicates the 25th percentile; middle line, the 50th percentile; and top border indicates the 75th percentile across all counties; whiskers indicate the full range across counties; and the circles indicate the national-level rate.
Nationally, the age-standardized mortality rate from alcohol use disorders decreased by 8.1% (95% UI, −0.5% to 21.1%) between 1980 and 2014 due to a decrease of 11.0% (95% UI, 3.9% to 18.8%) between 1980 and 2000 and an increase of 3.2% (95% UI, −3.9% to 10.0%) between 2000 and 2014 (Table 2). Despite the national decrease in alcohol use mortality between 1980 and 2014, more counties experienced increases in the mortality rate (65.4%; statistically significant in 26.8% of counties) than decreases (34.6%; statistically significant in 12.5% of counties). Counties with above average increases were located predominantly in the northern and western United States. In contrast, counties with particularly large decreases (>67.8% [top 1%]) were found in South Carolina, North Carolina, Virginia, Georgia, Florida, and Alaska (Figure 1). The degree of absolute and relative inequality among counties in mortality from alcohol use disorders decreased from 1980 to 2014 (Table 1; 99.7% posterior probability of decrease in absolute inequality; >99.9% posterior probability of decrease in relative inequality); in 1980, the mortality rate in counties in the 10th percentile was 1.1 deaths per 100 000 persons and the mortality rate in counties in the 90th percentile was 5.0 deaths per 100 000 persons (absolute difference, 3.8 deaths per 100 000 persons; relative difference, 4.3-fold), compared to a 2014 mortality rate of 1.5 deaths per 100 000 persons in counties in the 10th percentile and a mortality rate of 4.7 deaths per 100 000 persons in counties in the 90th percentile (absolute difference, 3.2 deaths per 100 000 persons; relative difference, 3.2-fold).
Table 2. Change in the Age-Standardized Mortality Rate Due to Alcohol Use Disorders, Drug Use Disorders, Self-harm, and Interpersonal Violence, 1980-2000, 2000-2014, and 1980-2014.
| Cause of Death by Year | National Change in Mortality Rate, % (95% Uncertainty Interval) | No. (%) of US Counties | |||
|---|---|---|---|---|---|
| Increases in Mortality Rate | Decreases in Mortality Rate | ||||
| Total | Statistically Significant Increasea | Total | Statistically Significant Decreaseb | ||
| Alcohol Use Disorders | |||||
| 1980-2000 | −11.0 (–18.8 to –3.9) | 1854 (59.61) | 527 (16.95) | 1256 (40.39) | 328 (10.55) |
| 2000-2014 | 3.2 (–3.9 to 10.0) | 2135 (68.65) | 520 (16.72) | 975 (31.35) | 223 (7.17) |
| 1980-2014 | –8.1 (–21.1 to 0.5) | 2033 (65.37) | 832 (26.75) | 1077 (34.63) | 388 (12.48) |
| Drug Use Disorders | |||||
| 1980-2000 | 238.2 (211.8 to 261.5) | 3109 (99.97) | 3099 (99.65) | 1 (0.03) | 0 |
| 2000-2014 | 112.4 (98.4 to 125.7) | 3107 (99.90) | 3087 (99.26) | 3 (0.10) | 0 |
| 1980-2014 | 618.3 (526.8 to 648.3) | 3110 (100.00) | 3105 (99.84) | 0 | 0 |
| Self-harm | |||||
| 1980-2000 | –15.3 (–19.1 to –11.3) | 1096 (35.24) | 387 (12.44) | 2014 (64.76) | 960 (30.87) |
| 2000-2014 | 11.0 (6.4 to 15.7) | 3016 (96.98) | 2611 (83.95) | 94 (3.02) | 21 (0.68) |
| 1980-2014 | –6.0 (–11.2 to –1.0) | 2320 (74.60) | 1558 (50.10) | 790 (25.40) | 342 (11.00) |
| Interpersonal Violence | |||||
| 1980-2000 | –34.6 (–37.4 to –31.0) | 71 (2.28) | 5 (0.16) | 3039 (97.72) | 1529 (49.16) |
| 2000-2014 | –15.6 (–19.0 to –11.7) | 1044 (33.57) | 29 (0.93) | 2066 (66.43) | 274 (8.81) |
| 1980-2014 | –44.9 (–47.7 to –41.0) | 204 (6.56) | 14 (0.45) | 2906 (93.44) | 1375 (44.21) |
Posterior probability of an increase equal to or greater than 95%.
Posterior probability of a decrease equal to or greater than 95%.
Drug Use Disorders
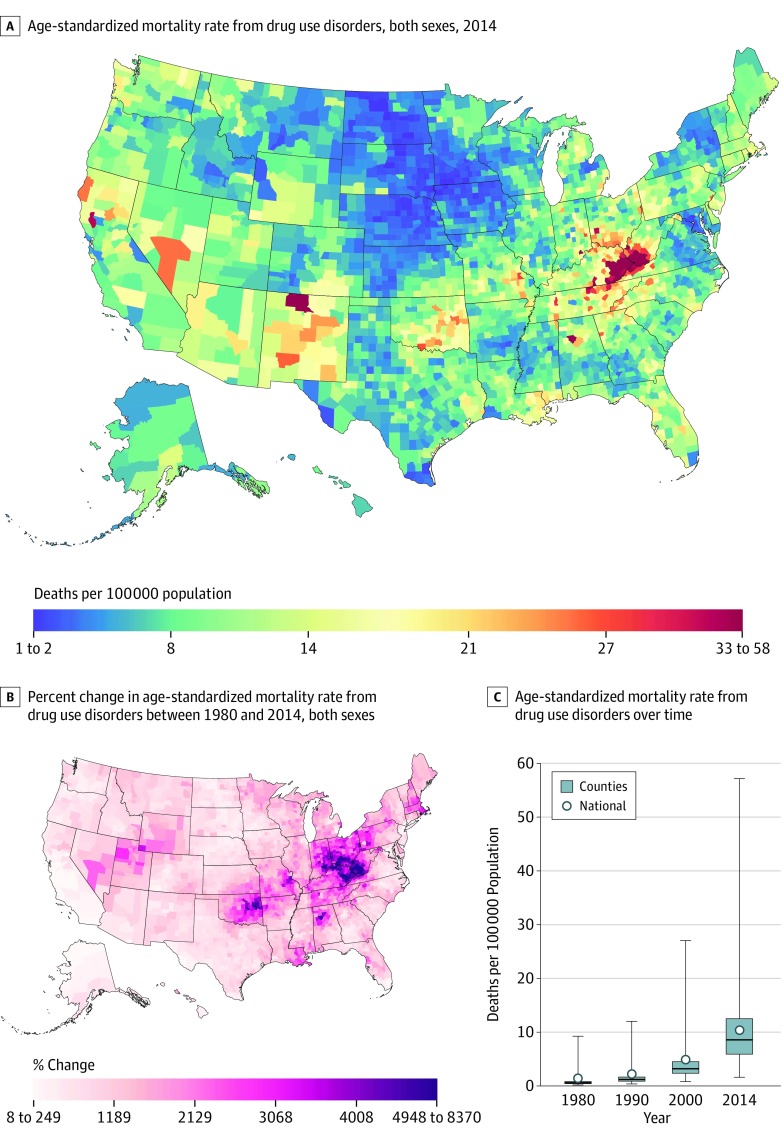
Between 1980 and 2014, there were 542 501 deaths due to drug use disorders recorded in the United States. Nationally, the age-standardized mortality rate from drug use disorders was 10.4 (95% UI, 9.7 to 10.9) deaths per 100 000 persons in 2014, while at the county level, mortality rates varied from 1.6 deaths per 100 000 to 57.1 deaths per 100 000 persons (Table 1). The distribution of counties by mortality rate was highly skewed: the 90th percentile among counties was 17.0 deaths per 100 000 persons, compared to the maximum rate of 57.1 deaths per 100 000 persons (Table 1). Counties near the border of Kentucky and West Virginia, as well as individual counties in New Mexico, Alabama, Indiana, Tennessee, and Virginia had very high mortality rates relative to the rest of the United States (>32.3 deaths per 100 000 persons [top 1%]) (Figure 2).
Figure 2. County-Level Mortality From Drug Use Disorders.
A, Age-standardized mortality rate for both sexes combined in 2014.
B, Relative change in the age-standardized mortality rate for both sexes combined between 1980 and 2014. A and B, the color scale is truncated at approximately the first and 99th percentile as indicated by the range given in the color scale.
C, Age-standardized mortality rate for both sexes combined in 1980, 1990, 2000, and 2014. The bottom border of the boxes indicates the 25th percentile; middle line, the 50th percentile; and top border indicates the 75th percentile across all counties; whiskers indicate the full range across counties; and the circles indicate the national-level rate.
Nationally, the age-standardized mortality rate due to drug use disorders increased by 238.2% (95% UI, 211.8% to 261.5%) from 1980 to 2000 and by 112.4% (95% UI, 98.4% to 125.7%) from 2000 to 2014, for an overall increase of 618.3% (95% UI, 526.8% to 648.3%) between 1980 and 2014 (Table 2). Mortality rates increased in every county between 1980 and 2014 (statistically significant in 99.8% of counties), although the magnitude of this increase varied regionally. Counties located in Kentucky, West Virginia, Ohio, Indiana, and eastern Oklahoma experienced the largest increases (>5000%) over this period (Figure 2). As a result of this variability, there was a marked increase in both absolute and relative inequality (Table 1; >99.9% posterior probability of increase); in 1980, the mortality rate in counties in the 10th percentile was 0.4 deaths per 100 000 persons and in counties in the 90th percentile was 1.1 deaths per 100 000 persons (absolute difference, 0.7 deaths per 100 000 persons; relative difference, 3.0-fold), compared to a 2014 mortality rate of 4.1 deaths per 100 000 persons in counties in the 10th percentile and a rate of 17.0 deaths per 100 000 persons in counties in the 90th percentile (absolute difference, 12.9 deaths per 100 000 persons; relative difference, 4.2-fold).
Self-harm
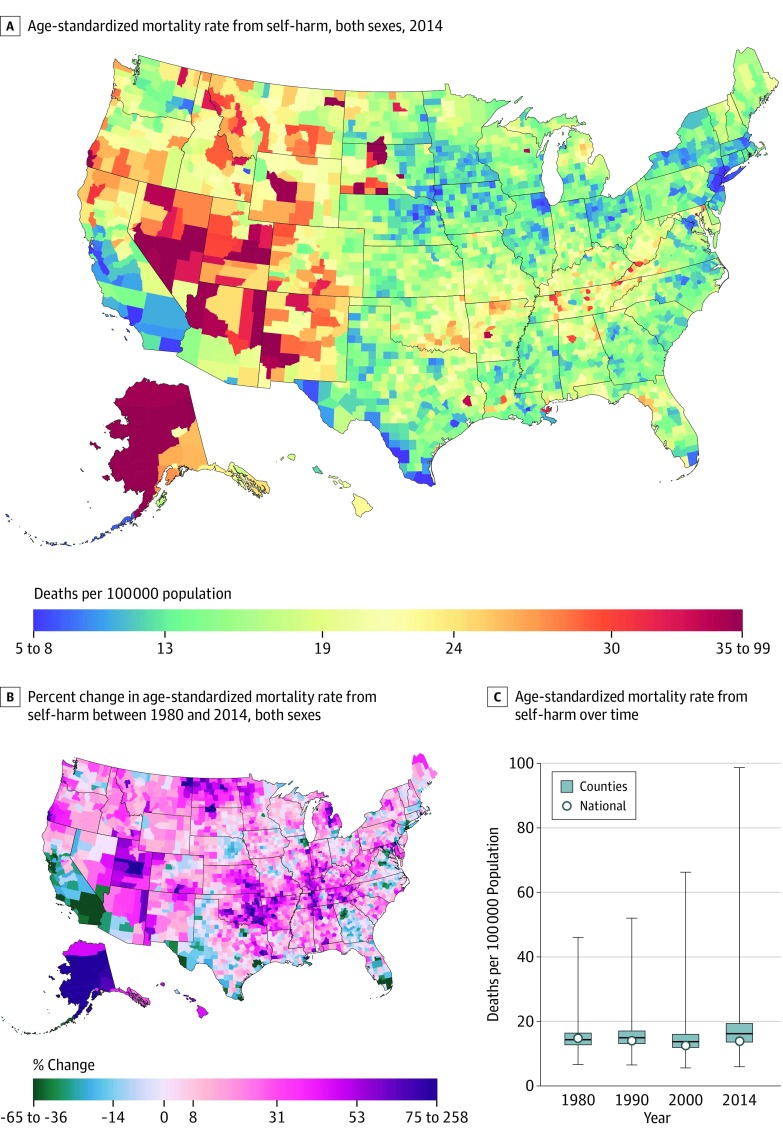
Between 1980 and 2014, there were 1 289 086 deaths due to self-harm recorded in the United States. In 2014, the national age-standardized mortality rate due to self-harm was 13.9 (95% UI, 13.3 to 14.4) deaths per 100 000 persons, while among counties, the mortality rate due to self-harm varied from 5.9 deaths per 100 000 to 98.7 deaths per 100 000 persons with an 11.5 deaths per 100 000-persons gap between counties in the 10th and 90th percentiles (Table 1). Counties with very high mortality rates (>34.2 deaths per 100 000 persons [top 1%]) were found primarily in states in the Western United States, including Alaska, Nevada, South Dakota, Utah, New Mexico, Arizona, Montana, North Dakota, Oregon, and Wyoming, as well as 1 county in Maryland (Figure 3).
Figure 3. County-Level Mortality From Self-harm.
A, Age-standardized mortality rate for both sexes combined in 2014.
B, Relative change in the age-standardized mortality rate for both sexes combined between 1980 and 2014. A and B, the color scale is truncated at approximately the first and 99th percentile as indicated by the range given in the color scale.
C, Age-standardized mortality rate for both sexes combined in 1980, 1990, 2000, and 2014. The bottom border of the boxes indicates the 25th percentile; middle line, the 50th percentile; and top border indicates the 75th percentile across all counties; whiskers indicate the full range across counties; and the circles indicate the national-level rate.
The age-standardized mortality rate due to self-harm decreased by 6.0% (95% UI, 1.0% to 11.2%) overall between 1980 and 2014 (Table 1) due to a decrease of 15.3% (95% UI, 11.3% to 19.1%) between 1980 and 2000 and an increase of 11.0% (95% UI, 6.4% to 15.7%) from 2000 to 2014 (Table 2). Most counties experienced an increase in self-harm mortality from 1980 to 2014 (74.6%; statistically significant in 50.1% of counties). Counties with particularly large increases (>74.4% [top 1%]) in mortality from self-harm were found in Alaska, Utah, Arkansas, Montana, North Dakota, Oklahoma, Tennessee, Colorado, Indiana, Kentucky, Maryland, Michigan, South Dakota, and Texas (Figure 3). Absolute and relative inequality among counties in mortality from self-harm also increased over this period (Table 1; posterior probability of increase >99.9%): in 1980 the mortality rate in counties in the 10th percentile was 11.2 deaths per 100 000 persons and for counties in the 90th percentile was 18.9 deaths per 100 000 persons (absolute difference, 7.6 deaths per 100 000 persons; relative difference, 1.7-fold), compared to a 2014 mortality rate of 11.6 deaths per 100 000 persons for counties in the 10th percentile and 23.0 deaths per 100 000 persons for counties in the 90th percentile (absolute difference, 11.5 deaths per 100 000 persons; relative difference, 2.0-fold).
Interpersonal Violence
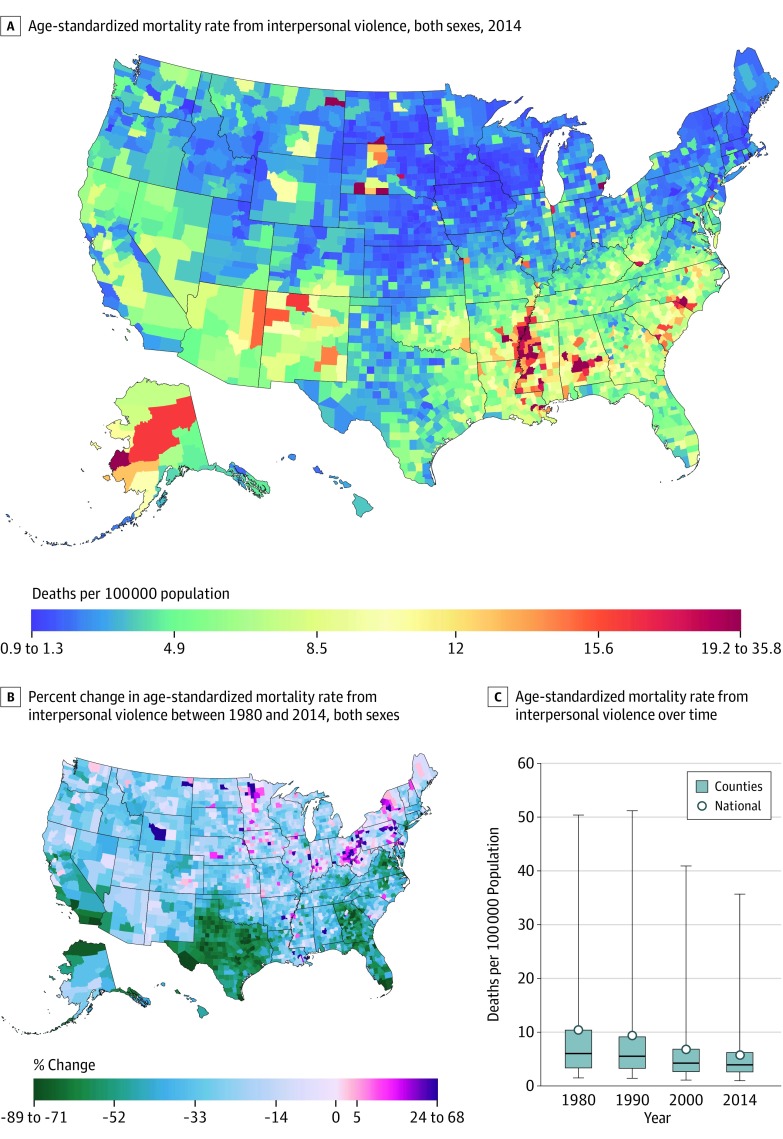
Between 1980 and 2014, there were 760 749 deaths due to interpersonal violence recorded in the United States. The national age-standardized mortality rate due to interpersonal violence was 5.7 (95% UI, 5.5 to 6.0) deaths per 100 000 persons in 2014. Among counties, the mortality rate from interpersonal violence varied from 1.0 deaths per 100 000 to 35.7 deaths per 100 000 persons, with a 7.1 deaths per 100 000-persons gap between the 10th and 90th percentile (Table 1). Counties with very high mortality rates from interpersonal violence (>19.1 deaths per 100 000 persons [top 1%]) were found along the southern half of the Mississippi River and in Alabama, as well as in Alaska, Montana, North Dakota, South Dakota, Kansas, Michigan, Maryland, Virginia, and North Carolina (Figure 4).
Figure 4. County-Level Mortality From Interpersonal Violence.
A, Age-standardized mortality rate for both sexes combined in 2014.
B, Relative change in the age-standardized mortality rate for both sexes combined between 1980 and 2014. A and B, the color scale is truncated at approximately the first and 99th percentile as indicated by the range given in the color scale.
C, Age-standardized mortality rate for both sexes combined in 1980, 1990, 2000, and 2014. The bottom border of the boxes indicates the 25th percentile; middle line, the 50th percentile; and top border indicates the 75th percentile across all counties; whiskers indicate the full range across counties; and the circles indicate the national-level rate.
Nationally, the age-standardized mortality rate due to interpersonal violence decreased by 34.6% (95% UI, 31.0% to 37.4%) from 1980 to 2000 and by 15.6% (95% UI, 11.7% to 19.0%) from 2000 to 2014, for an overall decrease of 44.9% (95% UI, 41.0% to 47.7%) between 1980 and 2014 (Table 2). Most counties also experienced a decrease between 1980 and 2014 (93.4%; statistically significant in 44.2% of counties), although increases in the mortality rate due to interpersonal violence were observed in 6.6% of counties (statistically significant in 0.5%). Counties with increases were concentrated in northern Midwestern and Atlantic states, while counties with the largest decreases (>70.6% [top 1%]) were found in Virginia, Georgia, Florida, Texas, California, and New York (Figure 4). Despite these differences, both absolute and relative inequality among counties in mortality from interpersonal violence decreased substantially over this period (Table 1; posterior probability of decrease >99.9%); in 1980, the mortality rate in counties in the 10th percentile was 2.5 deaths per 100 000 persons and for counties in the 90th percentile, it was 15.5 deaths per 100 000 persons (absolute difference, 13.0 deaths per 100 000 persons; relative difference. 6.1-fold), compared to a 2014 mortality rate of 1.9 deaths per 100 000 persons for counties in the 10th percentile and 9.0 deaths per 100 000 persons for counties in the 90th percentile (absolute difference, 7.1 deaths per 100 000 persons; relative difference, 4.7-fold).
All results by county, year, and sex are available in an online visualization tool. Selected sex-specific results are also presented in eTables 4 and 5 and eFigures 1 through 8 in the Supplement.
Discussion
This study documents spatial and temporal variation in mortality rates from 4 causes of death: alcohol use disorders, drug use disorders, self-harm, and interpersonal violence. For all 4 causes, there were substantial differences in mortality rates among counties. Moreover, for drug use disorders and self-harm, these differences have increased over time. The findings in this study may help clinicians, local health authorities, and policymakers address the burden of substance use disorders and intentional injuries in their communities.
The results of this study are consistent with earlier reports, based on data from the 1980s and early 1990s, of large regional differences in mortality rates from self-harm and interpersonal violence. This study improves on these earlier efforts by using small-area estimation methods that do not require pooling multiple years of data or combining counties into larger areas, and it also updates these analyses to include data from more recent decades. A number of previous studies have also considered regional differences in unintentional poisonings or all drug use overdoses, but in the former case, they do not distinguish between drug- and alcohol-related poisonings and other types of poisoning, and in the latter case do not distinguish between intentional overdoses (ie, as a means of self-harm or interpersonal violence) and unintentional overdoses. To our knowledge, this study is the first to consider alcohol and drug use disorders, apart from other types of unintentional poisonings and distinct from intentional overdoses, at the county level in the United States.
Substance use disorders and intentional injury are responsible for a significant health burden in the United States, particularly among young and middle-aged adults. Indeed, among people aged 15 to 49 years in the United States, self-harm, drug use disorders, and interpersonal violence are the first, second, and fifth leading causes of death; combined, substance use disorders and intentional injuries are responsible for nearly one-third of all deaths in this age group.
Overall, there was a slight decrease in mortality from alcohol use disorders between 1980 and 2014, although there were geographic areas, such as Alaska and the region in which the 4 Southwest states of Utah, Colorado, Arizona, and New Mexico meet, that had very high mortality rates relative to rest of the country, and many counties experienced an increase in the mortality rate due to alcohol use disorders over the same period. However, mortality rates from drug use disorders increased by more than 600% between 1980 and 2014, largely due to increasing numbers of deaths from both prescription and nonprescription opioid overdoses. Every county experienced an increase in deaths from drug use disorders, but that the burden of drug use overdoses was particularly acute in certain communities, with more than a 4-fold variation from counties in the 10th percentile to counties in the 90th percentile. These findings highlight the need for a multipronged public health response focusing on prevention, harm-reduction, treatment, and recovery support. Potentially beneficial strategies for each of these dimensions have been described, including fully implementing safer prescribing practices for opioid analgesics, increasing availability of the opioid antagonist Naloxone, and expanding access to treatment (including behavioral therapies and medication-assisted treatment). Moreover, fuller integration of substance use disorder screening and treatment into primary care and other health care settings is required to promote earlier identification of at-risk or affected individuals and increase access to and utilization of appropriate services.
Mortality rates from self-harm decreased overall between 1980 and 2014, but despite this overall decrease, mortality rates from self-harm increased between 2000 and 2014. In terms of geographic variation, deaths from self-harm were particularly high in regions of the Western United States with high rates of firearm availability and relatively low population density. Further action is required to reverse these recent increases and reduce the substantial health and social burden imposed by self-harm. In particular, improved access to effective mental health services, and structural approaches such as means reduction should be considered. In contrast to self-harm, mortality rates due to interpersonal violence decreased substantially between 1980 and 2014. Nonetheless, there was still significant inequality among counties with certain regions experiencing much higher rates of mortality due to interpersonal violence than the nation as a whole. In general, these counties were not located in regions typically noted for high rates of gun ownership (eg, the Western United States), nor were they primarily in more urban areas as might be expected. Substance use disorders increase the risk of suicide and intentional injuries, and efforts to reduce exposure to drugs and alcohol through prevention and treatment for at-risk individuals may also help to reduce mortality rates from self-harm and interpersonal violence in addition to mortality rates from substance use disorders; in 2015, 23% of deaths due to self-harm and 18% of deaths due to interpersonal violence were attributable to substance use.
Relative geographic inequality in mortality rates from the conditions discussed in this article (a ratio of 4.2 for drug use disorders and 4.7 for interpersonal violence between counties in the 90th and the 10th percentile in 2014) was high compared to most other causes (eg, this ratio ranges from 1.2 to 2.2 among different cancers) This suggests that there are important opportunities to more closely examine counties and communities with notably high or low mortality rates or particularly substantial increases or decreases in the mortality rate over time. Such research could facilitate identifying potential solutions to these problems that might include social, cultural, legal, policy, or health service–related approaches.
Limitations
This study has several limitations. First, the population, deaths, and covariates data used are all subject to error. Second, the garbage code redistribution algorithms used to redistribute deaths assigned implausible or nonspecific causes to likely true causes of death have not been validated because appropriate criterion standard data are unavailable. Third, although these redistribution methods are likely associated with nontrivial uncertainty, this uncertainty is difficult to quantify and consequently has not been included in the uncertainty intervals associated with the estimated mortality rates. Fourth, the small-area models used in this analysis smooth mortality rates over time, space, and age groups, and may in some cases attenuate unusually low or high mortality rates, underestimating true geographic variability.
Conclusions
Mortality due to alcohol use disorders, drug use disorders, self-harm, and interpersonal violence varied widely among US counties, both in terms of levels of mortality and trends. These estimates may be useful to inform efforts to target prevention, diagnosis, and treatment efforts to improve health and reduce inequalities.
eTable 1. Data Sources Used for Covariates
eTable 2. Counties Combined to Ensure Historically Stable Units of Analysis
eTable 3. GBD Cause List and Associated ICD9 and ICD10 Codes
eTable 4. National Deaths, Years of Life Lost, and Age-Standardized Mortality Rate; and Distribution of Age-Standardized Mortality Rates at the County Level in 1980, 2000, and 2014 Due to Alcohol Use Disorders, Drug Use Disorders, Self-Harm, and Interpersonal Violence, by Sex
eTable 5. Change in the Age-Standardized Mortality Rate Due to Alcohol Use Disorders, Drug Use Disorders, Self-Harm, and Interpersonal Violence, 1980–2000, 2000–2014, and 1980–2014, by Sex
eFigure 1. County-Level Mortality Among Men From Alcohol Use Disorders
eFigure 2. County-Level Mortality Among Women From Alcohol Use Disorders
eFigure 3. County-Level Mortality Among Men From Drug Use Disorders
eFigure 4. County-Level Mortality Among Women From Drug Use Disorders
eFigure 5. County-Level Mortality Among Men From Self-Harm
eFigure 6. County-Level Mortality Among Women From Self-Harm
eFigure 7. County-Level Mortality Among Men From Interpersonal Violence
eFigure 8. County-Level Mortality Among Women From Interpersonal Violence
References
- 1.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Case A, Deaton A. Brookings papers on economic activity, spring 2017: Mortality and morbidity in the 21st century. https://www.brookings.edu/wp-content/uploads/2017/08/casetextsp17bpea.pdf. Accessed February 20, 2018. [DOI] [PMC free article] [PubMed]
- 4.Baker SP, Whitfield RA, O’Neill B. County mapping of injury mortality. J Trauma. 1988;28(6):741-745. [DOI] [PubMed] [Google Scholar]
- 5.Devine OJ, Annest JL, Kirk ML, et al. Injury Mortality Atlas of the United States, 1979-1987. Atlanta, GA: US Dept of Health and Human Services; 1991. http://hdl.handle.net/2027/pur1.32754061595363. Originally accessed April 18, 2017. Access confirmed February 20, 2018. [Google Scholar]
- 6.Pickle LW, Mungiole M, Jones GK, White AA. Atlas of United States Mortality. Hyattsville, MD: National Center for Health Statistics; 1996. http://www.cdc.gov/nchs/products/other/atlas/atlas.htm. Originally accessed May 10, 2016. Access confirmed February 20, 2018.
- 7.Fingerhut LA, Ingram DD, Feldman JJ. Homicide rates among US teenagers and young adults: differences by mechanism, level of urbanization, race, and sex, 1987 through 1995. JAMA. 1998;280(5):423-427. [DOI] [PubMed] [Google Scholar]
- 8.Paulozzi LJ, Jones CM, Mack KA, Rudd RA; Centers for Disease Control and Prevention (CDC) . Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492. [PubMed] [Google Scholar]
- 9.Rossen LM, Khan D, Warner M. Trends and geographic patterns in drug-poisoning death rates in the US, 1999-2009. Am J Prev Med. 2013;45(6):e19-e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. US county-level trends in mortality rates for major causes of death, 1980-2014. JAMA. 2016;316(22):2385-2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Vital Statistics System Multiple cause of death data file: 1980-2014. https://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm. Accessed February 20, 2018.
- 12.United States Census Bureau Intercensal county estimates by age, sex, race: 1980-1989. 2009. https://www.census.gov/data/datasets/time-series/demo/popest/1980s-county.html. Originally accessed January 8, 2015. Access confirmed February 20, 2018.
- 13.National Center for Health Statistics Bridged-race intercensal estimates of the resident population of the United States for July 1, 1990-July 1, 1999, by year, county, single-year of age (0, 1, 2, ..., 85 years and over), bridged race, Hispanic origin, and sex. 2004. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#july1990-1999. Originally accessed November 21, 2011. Access confirmed February 20, 2018.
- 14.National Center for Health Statistics Bridged-race intercensal estimates of the resident population of the United States for July 1, 2000-July 1, 2009, by year, county, single-year of age (0, 1, 2, ..., 85 years and over), bridged race, Hispanic origin, and sex. 2012. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#july2000-2009. Originally accessed October 30, 2012. Access confirmed February 20, 2018.
- 15.National Center for Health Statistics Vintage 2014 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010-July 1, 2014), by year, county, single-year of age (0, 1, 2, ..., 85 years and over), bridged race, Hispanic origin, and sex. 2015. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2014. Originally accessed December 18, 2015. Access confirmed February 20, 2018.
- 16.University of California, Berkeley, Max Planck Institute for Demographic Research Human Mortality Database. http://www.mortality.org/cgi-bin/hmd/country.php?cntr=USA&level=1. Originally accessed July 8, 2013. Access confirmed February 20, 2018.
- 17.Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leroux BG, Lei X, Breslow N. Estimation of disease rates in small areas: a new mixed model for spatial dependence In: Halloran ME, Berry D, eds. Statistical Models in Epidemiology, the Environment, and Clinical Trials. Vol 116 New York, NY: Springer-Verlag; 2000:179-191. [Google Scholar]
- 19.Knorr-Held L. Bayesian modelling of inseparable space-time variation in disease risk. Stat Med. 2000;19(17-18):2555-2567. [DOI] [PubMed] [Google Scholar]
- 20.Kristensen K, Nielsen A, Berg CW, Skaug H, Bell B. TMB: automatic differentiation and Laplace approximation. J Stat Softw. 2016;70(5):1-21. doi: 10.18637/jss.v070.i05 [DOI] [Google Scholar]
- 21.Fienberg SE. An iterative procedure for estimation in contingency tables. Ann Math Stat. 1970;41(1):3. doi: 10.1214/aoms/1177696968 [DOI] [Google Scholar]
- 22.Institute for Health Metrics and Evaluation, University of Washington US health map. https://vizhub.healthdata.org/subnational/usa. Accessed February 20, 2018.
- 23.Nkhoma ET, Ed Hsu C, Hunt VI, Harris AM. Detecting spatiotemporal clusters of accidental poisoning mortality among Texas counties, US, 1980-2001. Int J Health Geogr. 2004;3(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382. [DOI] [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services, Office of the Surgeon General Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/. Originally accessed June 13, 2017. Access confirmed February 20, 2018. [PubMed]
- 26.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim D, Irwin KS, Khoshnood K. Expanded access to naloxone: options for critical response to the epidemic of opioid overdose mortality. Am J Public Health. 2009;99(3):402-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lang M. The impact of mental health insurance laws on state suicide rates. Health Econ. 2013;22(1):73-88. [DOI] [PubMed] [Google Scholar]
- 29.Sarchiapone M, Mandelli L, Iosue M, Andrisano C, Roy A. Controlling access to suicide means. Int J Environ Res Public Health. 2011;8(12):4550-4562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yip PS, Caine E, Yousuf S, Chang S-S, Wu KC-C, Chen Y-Y. Means restriction for suicide prevention. Lancet. 2012;379(9834):2393-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.GBD 2015 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980-2014. JAMA. 2017;317(4):388-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Data Sources Used for Covariates
eTable 2. Counties Combined to Ensure Historically Stable Units of Analysis
eTable 3. GBD Cause List and Associated ICD9 and ICD10 Codes
eTable 4. National Deaths, Years of Life Lost, and Age-Standardized Mortality Rate; and Distribution of Age-Standardized Mortality Rates at the County Level in 1980, 2000, and 2014 Due to Alcohol Use Disorders, Drug Use Disorders, Self-Harm, and Interpersonal Violence, by Sex
eTable 5. Change in the Age-Standardized Mortality Rate Due to Alcohol Use Disorders, Drug Use Disorders, Self-Harm, and Interpersonal Violence, 1980–2000, 2000–2014, and 1980–2014, by Sex
eFigure 1. County-Level Mortality Among Men From Alcohol Use Disorders
eFigure 2. County-Level Mortality Among Women From Alcohol Use Disorders
eFigure 3. County-Level Mortality Among Men From Drug Use Disorders
eFigure 4. County-Level Mortality Among Women From Drug Use Disorders
eFigure 5. County-Level Mortality Among Men From Self-Harm
eFigure 6. County-Level Mortality Among Women From Self-Harm
eFigure 7. County-Level Mortality Among Men From Interpersonal Violence
eFigure 8. County-Level Mortality Among Women From Interpersonal Violence