This study evaluates the association of the Patient Protection and Affordable Care Act’s Medicaid expansion with access to timely and recommended care for common and serious surgical conditions.
Key Points
Question
How was Medicaid expansion under the Patient Protection and Affordable Care Act associated with patient presentation with and management of common surgical conditions?
Findings
In this study of patients with 1 of 5 common surgical conditions, Medicaid expansion was associated with a 7.5–percentage point increase in insurance coverage at the time of hospital admission. The policy was also associated with patients obtaining care earlier in their disease course and with an increased probability of receiving optimal care for those conditions.
Meaning
The Patient Protection and Affordable Care Act’s Medicaid expansion was associated with increased coverage of patients, earlier presentation with common diagnoses, and improved surgical care.
Abstract
Importance
Lack of insurance coverage has been associated with delays in seeking care, more complicated diseases at the time of diagnosis, and decreased likelihood of receiving optimal surgical care. The Patient Protection and Affordable Care Act’s (ACA) Medicaid expansion has increased coverage among millions of low-income Americans, but its effect on care for common surgical conditions remains unknown.
Objective
To evaluate the association of the ACA’s Medicaid expansion with access to timely and recommended care for common and serious surgical conditions.
Design, Setting, and Participants
This quasi-experimental, difference-in-differences study used hospital administrative data to compare patient-level outcomes in expansion vs nonexpansion states before (2010-2013) vs after (2014-2015) expansion. A total of 293 529 patients aged 18 to 64 years with appendicitis, cholecystitis, diverticulitis, peripheral artery disease (PAD), or aortic aneurysm admitted to an academic medical center or affiliated hospital in 27 Medicaid expansion states and 15 nonexpansion states from January 1, 2010, through September 31, 2015, were included in the study. Data analysis was performed from November 1, 2016, to March 3, 2017.
Exposures
State adoption of Medicaid expansion.
Main Outcomes and Measures
Presentation with early uncomplicated disease (diverticulitis without abscess, fistula, or sepsis; nonruptured aortic aneurysm at time of repair; and PAD without ulcerations or gangrene) and receipt of optimal management (cholecystectomy for acute cholecystitis, laparoscopic approach for cholecystectomy or appendectomy, and limb salvage for PAD).
Results
Of the 293 529 study patients (128 392 [43.7%] female and 165 137 [56.3%] male), 225 572 had admissions in Medicaid expansion states and 67 957 had admissions in nonexpansion states. Medicaid expansion was associated with a 7.5–percentage point decreased probability of patients being uninsured (95% CI, −12.2 to −2.9; P = .002) and an 8.6–percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P < .001). Medicaid expansion was associated with a 1.8–percentage point increase in the probability of early uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6–percentage point increase in the probability of receiving optimal management (95% CI, 0.8-4.4; P = .006).
Conclusions and Relevance
The ACA’s Medicaid expansion was associated with increased insurance coverage and improved receipt of timely care for 5 common surgical conditions. Health care systems and policymakers should be aware of the influence of insurance coverage expansion (or its repeal) on presentation with and management of surgical disease.
Introduction
The Patient Protection and Affordable Care Act (ACA) aimed to increase access to health care through expanded insurance coverage. Since enactment, more than 20 million individuals have gained health insurance through the ACA, with disproportionate coverage in states that adopted Medicaid expansion. Survey-based studies have found the ACA to be associated with self-reported access to primary care and medications, affordability, and overall health. However, the clinical effect of coverage expansion on patients with common and serious surgical conditions remains unclear.
Uninsured and underinsured patients are significantly more likely to delay care and present with more complicated disease for conditions including appendicitis, cholecystitis, diverticulitis, aortic aneurysms, and lower extremity peripheral artery disease (PAD). Insurance status is also associated with decreased probability of receiving optimal care for such diagnoses, including a lower likelihood of minimally invasive surgery, a lower likelihood of receiving immediate cholecystectomy for acute cholecystitis, and a higher likelihood of amputation for vascular disease. The acute onset or deterioration of these diagnoses provides an ideal setting for studying short-term changes in presentation and management after population-wide insurance coverage expansion. As more individuals gain insurance coverage, one might also expect a greater probability of patients presenting earlier and with less severe disease at the time of diagnosis and in turn receiving more timely and less morbid management.
The 2006 Massachusetts health reform, a model for the ACA insurance expansions, was associated with an increased probability of patients presenting with less complicated surgical disease and a greater likelihood of patients receiving optimal surgical management after admission. However, it is unclear whether the Massachusetts experience is generalizable to the ACA’s Medicaid expansion. Given current debate on the ACA and reforms to the Medicaid program, evidence on the effects of these policies is critical. The primary objective of this study was to analyze changes associated with the ACA’s Medicaid expansion in access to and receipt of optimal care for common and serious surgical conditions.
Methods
Study Design
Our study used a quasi-experimental, difference-in-differences design to compare patient-level outcomes in Medicaid expansion vs nonexpansion states before (2010-2013) vs after (2014-2015) expansion. We also adjusted for potential time-varying confounders that could bias our estimates and tested the underlying assumption of the study design, namely, that in the absence of the Medicaid expansion, our study outcomes would have had similar trends over time between expansion and nonexpansion states. This study was deemed to be exempt from institutional review board approval by Harvard University because we only examined deidentified data.
Data Source and Outcomes
Our primary data source was the Vizient (formerly University HealthSystem Consortium) Clinical Database/Resource Manager (CD/RM). The CD/RM is an administrative database that captures all discharges from participating hospitals, which include more than 95% of academic medical centers and affiliated hospitals across the country. The database has been used in multiple previous analyses to study surgical care. Our analysis included admissions to 203 hospitals in 27 Medicaid expansion states (including Washington, DC) and 69 hospitals in 15 nonexpansion states (eTable 1 in Supplement). Some hospitals entered and exited the sample during the study period; in sensitivity analyses, we tested the effect of this compositional change. For confidentiality reasons, the public-use file does not include the specific state in which a hospital is located. For our analysis, we were provided with an indicator for whether a hospital was in a state that expanded Medicaid before September 2015.
Our sample contained patients admitted to any hospital in the data set from January 1, 2010, through September 31, 2015, with appendicitis, cholecystitis, diverticulitis, aortic aneurysm, or PAD. Conditions were identified based on International Classification of Diseases, Ninth Revision (ICD-9) diagnosis and procedure codes (eTable 2 in the Supplement). We selected these particular surgical conditions because of extensive documentation of disparities in patient presentation with and subsequent care received based on insurance coverage, in addition to data that suggest an association between insurance expansion and care delivery for these conditions. Surgery for appendicitis, cholecystitis, and diverticulitis represent the 3 most frequent and highest-morbidity procedures in general surgery. Vascular diseases, including aortic aneurysm and PAD, are increasingly prevalent in the United States, and timely, appropriate management directly affects mortality and major morbidity.
We limited our sample to patients aged 18 to 64 years. Adults older than 64 years and those with Medicare coverage were excluded because they were not eligible for the ACA’s Medicaid expansion. Although most patients newly insured under the ACA had enrolled in Medicaid, our primary analysis also included those with private insurance because Medicaid expansion may have affected transitions in coverage between private and public insurance and possible enrollment in ACA Marketplace plans. Because we were unable to specifically determine which individuals gained Medicaid after expansion, we conducted a subgroup analysis, stratifying our sample into those with private coverage and those with Medicaid or no health insurance. If the ACA’s Medicaid expansion was causing the changes that we observed, they should have been concentrated among the latter group (Medicaid recipients and uninsured).
Our study outcomes were composite measures in 2 broad domains: early uncomplicated presentation and receipt of optimal care. These composite outcomes were created to include a variety of common, serious surgical diseases that share a common causal pathway associated with similar outcomes and to increase power to detect significant effects across multiple conditions. For early, uncomplicated presentation, we defined the condition-specific outcomes as follows: uncomplicated diverticulitis as the absence of peritoneal or retroperitoneal abscess, enterocutaneous fistula, sepsis, or septic shock; nonruptured aortic aneurysm at the time of repair; and PAD without ulcerations or gangrene of limb (see eTable 3 in the Supplement for details of the ICD-9 codes used in this definition).
We defined optimal care for select diagnoses based on prior studies that found improved morbidity, mortality, effect on quality of life, and costs. Condition-specific outcomes were as follows: receipt of cholecystectomy when admitted with acute cholecystitis, receipt of minimally invasive appendectomy or cholecystectomy when undergoing surgery for acute appendicitis or cholecystitis, and avoidance of amputation when admitted with lower extremity PAD. Although alternative treatment may be appropriate for individual patients, depending on specific presentation, we contend that receipt of optimal care as defined here represents the ideal treatment if patients present early and are healthy enough to receive it.
Statistical Analysis
Data analysis was performed November 1, 2016, to March 3, 2017. We used linear regression difference-in-differences models to evaluate changes in presentation and management of surgical conditions for patients in expansion states vs nonexpansion states that were associated with implementation of the ACA’s Medicaid expansion. Linear models provide straightforward estimates of absolute changes, as is typical in difference-in-differences models. An expansion state binary variable was created for discharges from hospitals in states that expanded Medicaid eligibility before September 2015. A separate postreform indicator variable was created if the discharge occurred on or after January 1, 2014, the date of expanded Medicaid eligibility in most adopting states. An interaction term was created between expansion state and the postreform variable that provides the difference-in-differences estimate for the Medicaid expansion.
All models adjusted for patient age, sex, race/ethnicity, and comorbidity, in addition to a linear quarterly time trend. The CD/RM defines categorical age variables as 18 through 30 years, 31 through 50 years, or 51 through 64 years. Patient race/ethnicity was defined in the data set as white, black, Asian, or other. Patient comorbidity was determined using the Charlson Comorbidity Index. The SEs were clustered at the hospital level using cluster-correlated robust estimate of variance because the public-use file does not allow the direct identification of states.
In sensitivity analyses, we assessed parallel trends in outcomes between expansion and nonexpansion states before 2014, which is the key to the validity of the difference-in-differences study design. These models included only admissions that occurred before January 1, 2014. An interaction term between the expansion state variable and the continuous quarter variable was used to identify differential trends in outcomes between expansion states and nonexpansion states before 2014. In addition, we broke down our composite outcomes to assess trends in presentation with and management of individual diagnoses, although with reduced power attributable to smaller sample sizes. Finally, additional sensitivity models limited analysis to 139 hospitals in expansion states and 44 hospitals in nonexpansion states that were consistently represented in the data set from 2010 through 2015.
Data were analyzed using Stata software, version 14 (StataCorp). Statistical significance was tested using a 2-sided threshold of P = .05.
Results
Of the 293 529 study patients (128 392 [43.7%] female and 165 137 [56.3%] male), 225 572 had admissions in Medicaid expansion states and 67 957 had admissions in nonexpansion states. Patient demographic and clinical characteristics are given in Table 1. Patients in expansion states were younger, more likely to be white, and more likely to have private insurance. Patient sex and comorbidity were comparable between expansion and nonexpansion states.
Table 1. Demographic and Clinical Characteristics of Admitted Patients in Medicaid Expansion and Nonexpansion Statesa.
| Characteristic | Expansion States (n = 225 572) | Nonexpansion States (n = 67 957) | P Value |
|---|---|---|---|
| Age group, y | |||
| 18-30 | 32 889 (14.6) | 7636 (11.2) | <.001 |
| 31-50 | 72 000 (31.9) | 21 434 (31.5) | |
| 51-65 | 120 683 (53.5) | 38 887 (57.2) | |
| Female | 98 710 (43.8) | 29 682 (43.7) | .70 |
| Race/ethnicity | |||
| White | 151 654 (67.2) | 42 919 (63.2) | <.001 |
| Black | 32 148 (14.3) | 14 685 (21.6) | |
| Asian | 5631 (2.5) | 937 (1.4) | |
| Other | 36 139 (16.0) | 9416 (13.9) | |
| Charlson Comorbidity Index, mean (SD) | 0.97 (1.66) | 1.16 (1.79) | <.001 |
| Distribution of diagnoses | |||
| Appendicitis | 70 979 (31.5) | 16 616 (24.5) | <.001 |
| Cholecystitis | 13 175 (5.8) | 4077 (6.0) | |
| Diverticulitis | 93 150 (41.3) | 29 257 (43.1) | |
| Aortic aneurysm | 14 089 (6.3) | 5327 (7.8) | |
| Peripheral arterial disease | 34 136 (15.1) | 12 670 (18.7) |
Data are presented as number (percentage) of patients unless otherwise indicated.
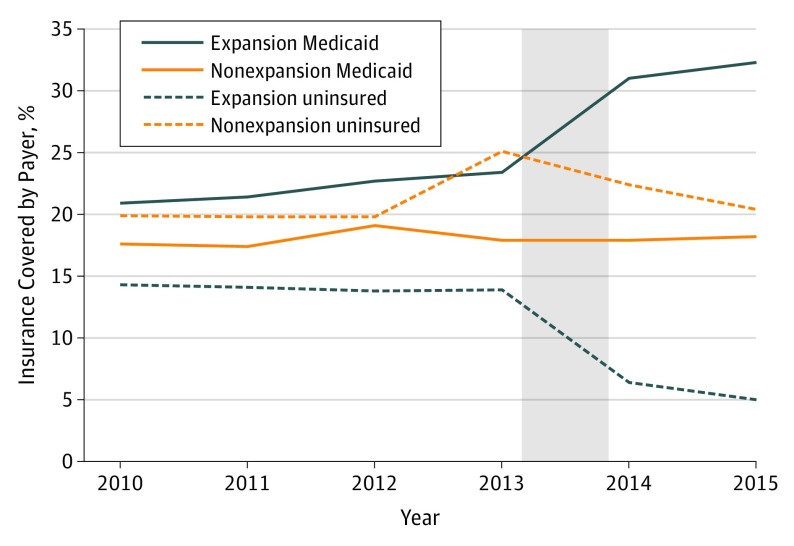
Beginning in 2014, the share of uninsured patients decreased in expansion states compared with nonexpansion states (Figure 1). In adjusted models, the Medicaid expansion was associated with a 7.5–percentage point decrease in the probability of being uninsured (95% CI, −12.2 to −2.9; P = .002) and an 8.6–percentage point increase in the probability of Medicaid coverage (95% CI, 6.1-11.1; P < .001) in our sample of admissions for surgical conditions (Table 2). No significant change was found in the probability of admissions for patients with private insurance.
Figure 1. Unadjusted Trends in Health Insurance Status Among Admissions (2010-2015), by Medicaid Expansion Status.
Shaded area indicates the time of Medicaid expansion.
Table 2. Changes in Probability of Insurance Coverage Among Admissions for Surgical Conditions After the Medicaid Expansion.
| Insurance Coverage | Expansion States | Nonexpansion States | Difference-in-Differences [P Value] | |||||
|---|---|---|---|---|---|---|---|---|
| Before, % | After, % | Difference, Percentage Points | Before, % | After, % | Difference, Percentage Points | Unadjusted, Percentage Points | Adjusted (95% CI), Percentage Pointsa | |
| Uninsured | 14.1 | 6.8 | −7.3 | 21.2 | 21.9 | 0.6 | −7.9 [.001] | −7.5 (−12.2 to −2.9) [.002] |
| Medicaid | 22.1 | 30.5 | 8.4 | 18.0 | 18.0 | 0.0 | 8.4 [.001] | 8.6 (6.1 to 11.1) [<.001] |
| Private | 63.9 | 62.7 | −1.2 | 60.8 | 60.1 | −0.7 | −0.5 [.26] | −1.0 (−5.1 to 3.0) [.62] |
Adjusted for patient age, sex, race/ethnicity, comorbidity, secular trends, and clustering at hospital level.
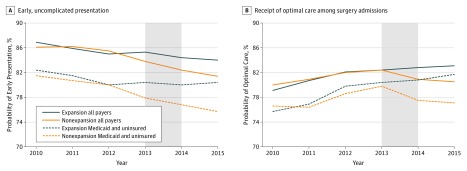
Figure 2 shows unadjusted trends in presentation and treatment throughout the study period, and Table 3 presents adjusted difference-in-differences estimates of changes in patient presentation and management associated with Medicaid expansion. Medicaid expansion was associated with a 1.8–percentage point increased probability (95% CI, 0.7-2.9; P = .001) of early uncomplicated presentation for all patients. Improvements in presentation were concentrated among the Medicaid recipient and uninsured subgroup (2.9 percentage points; 95% CI, 1.2-4.8; P = .001). Medicaid expansion was associated with a 2.6–percentage point increased probability of optimal care (95% CI, 0.8-4.4; P = .006) among all patients, and this estimate increased to 3.7 percentage points (95% CI, 0.7-6.7; P = .02) in the Medicaid recipient and uninsured subgroup. Unadjusted trends in Figure 2 show an apparent divergence in timely presentation beginning in 2013. However, adjusted models comparing preexpansion trends in expansion and nonexpansion states did not reveal any significant differences for either of the composite surgical measures (eTable 4 in the Supplement), offering support for the difference-in-differences design.
Figure 2. Unadjusted Trends in Presentation and Treatment, by State Medicaid Expansion Status and Insurance Type.
Shaded area indicates the time of Medicaid expansion.
Table 3. Changes in Rates of Early, Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion.
| Variable | Expansion States | Nonexpansion States | Difference-in-Differences [P Value] | |||||
|---|---|---|---|---|---|---|---|---|
| Before, % | After, % | Difference, Percentage Points | Before, % | After, % | Difference, Percentage Points | Unadjusted, Percentage Points | Adjusted (95% CI), Percentage Pointsa | |
| Early or Uncomplicated Presentation | ||||||||
| Full sample (n = 188 629) | 85.8 | 84.4 | −1.4 | 85.4 | 82.2 | −3.2 | 1.9 [<.001] | 1.8 (0.7 to 2.9) [.001] |
| Private insurance (n = 121 725) |
88.3 | 86.7 | −1.6 | 88.8 | 85.7 | −3.1 | 1.5 [.001] | 1.4 (0.3 to 2.5) [.02] |
| Medicaid and uninsured (n = 66 904) | 80.9 | 80.3 | −0.6 | 80.1 | 76.4 | −3.7 | 3.1 [<.001] | 2.9 (1.2 to 4.8) [.001] |
| Optimal Management | ||||||||
| Full sample (n = 147 439) | 81.0 | 82.9 | 1.9 | 81.3 | 80.9 | −0.4 | 2.4 [<.001] | 2.6 (0.8 to 4.4) [.006] |
| Private insurance (n = 84 689) | 82.9 | 84.4 | 1.5 | 84.0 | 84.0 | +0.0 | 1.4 [.03] | 1.7 (−0.2 to 3.5) [.07] |
| Medicaid and uninsured (n = 62 750) | 78.1 | 81.0 | 2.9 | 78.1 | 77.4 | −0.7 | 3.7 [<.001] | 3.7 (0.7 to 6.7) [.02] |
Adjusted for patient age, sex, race/ethnicity, comorbidity, secular trends, and clustering at hospital level.
Evaluating individual components of our composite measures produced similar directional estimates for the association of the Medicaid expansion with outcomes but with variable statistical significance (eTable 5 and eTable 6 in the Supplement). The association between Medicaid expansion and early presentation for diverticulitis remained significant (percentage point increase, 1.6; 95% CI, 0.5-2.7; P = .004), as did that between expansion and optimal management of acute cholecystitis (percentage point increase, 2.8; 95% CI, −0.0 to 5.7; P = .05), whereas the remaining outcomes had positive but nonsignificant coefficients (aortic aneurysm: percentage point increase, 1.3 [95% CI, −1.1 to 3.8], P = .29; PAD: percentage point increase, 2.3 [95% CI, −0.2 to 4.9], P = .07; minimally invasive appendectomy: percentage point increase, 1.9 [95% CI, −0.7 to 4.5], P = .15; and limb-sparing PAD: percentage point increase, 1.5 [95% CI, 0.9 to 4.0], P = .22). Results were also consistent when limiting analyses to patients admitted to hospitals present in the sample throughout the study period (eTable 7 in the Supplement).
Finally, because our outcomes were calculated as a proportion of total admissions, we assessed whether admission rates for these conditions changed in association with Medicaid expansion (eTable 8 in the Supplement). In our full sample, no differential changes in admission rates were found for these conditions in expansion states compared with nonexpansion states (incident rate ratio [IRR], 0.99; 95% CI, 0.97-1.00; P = .14). Among the insurance subgroups, we detected significant but small changes: a slight increase in volume of admissions for Medicaid recipients and uninsured (IRR, 1.02; 95% CI, 1.02-1.02; P < .001) in expansion vs nonexpansion states and a slight decrease for privately insured patients (IRR, 0.99; P < .001). This finding indicates that the changes in our composite outcomes (Figure 2 and Table 3) are primarily attributable to changes in the numerator (ie, early presentation and optimal care received) rather than the denominator (ie, number of admissions).
Discussion
In a study of more than 290 000 hospital admissions in 42 states (including Washington, DC), we found that the ACA’s Medicaid expansion was associated with significant increases in insurance coverage among patients who presented with serious surgical conditions. The Medicaid expansion was also associated with a significantly greater likelihood of patients presenting with earlier, less complicated disease at the time of admission and an increased likelihood of receiving optimal care after admission. As expected, these changes were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance. To our knowledge, these are among the first non–survey-based data that indicate improvements in quality of care associated with the ACA’s Medicaid expansion. Our findings supplement a large body of research that found improved access, satisfaction with care, and self-reported health since enactment of the ACA.
The ACA expanded insurance coverage to more than 20 million Americans, largely through Medicaid, and one main goal of the law was to decrease barriers to timely receipt of high-quality care for serious medical conditions. Our study focused on common surgical conditions for several reasons: they are typically urgent conditions that require prompt evaluation, delays in care may respond quickly to changes in health insurance status, and they are highly costly and morbid conditions. Thus, our study captured outcomes with important implications for public health and health care costs. Beyond financial protection for individual patients, Medicaid expansion mitigates uncompensated care and improves finances for hospitals that care for vulnerable populations. These data also build on previous work from Massachusetts and the ACA’s dependent coverage provision that showed an association between insurance expansion and improved clinical care of acute-onset diseases, including appendicitis, cholecystitis, and lower extremity vascular disease.
Our findings are likely explained by several main factors. Newly insured individuals may be less likely to delay seeking care and thus present sooner when early symptoms develop. Such behavior is consistent with the Oregon health insurance experiment and numerous ACA-related studies that found Medicaid coverage to be associated with decreased delays in seeking care and increased use of emergency department, primary care, and outpatient clinics. Having presented earlier in the clinical progression or deterioration of their conditions, patients may be more likely to receive optimal management with decreased morbidity and improved outcomes. In addition, hospitals may be more willing to provide care for newly insured individuals who previously lacked coverage. As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.
Limitations
The study has a number of limitations that should be considered. First, the CD/RM is an administrative data set and as such is vulnerable to coding errors and limited clinical granularity captured through ICD-9 coding. However, these data have been used extensively for hospital quality benchmarking, including studies of the diagnoses used in our analyses, and such benchmarking is valid compared with clinical data and large administrative data sets. The CD/RM also only includes participating academic medical centers and affiliated hospitals, which may differ in important ways from nonacademic hospitals. However, academic centers play a key role in the health care safety net and thus are highly relevant to evaluating the effects of the Medicaid expansion. Furthermore, our analysis included more than 203 hospitals in 42 states (including Washington, DC), capturing a fairly broad segment of inpatient care in the United States. Recognizing these limitations, we believe the advantages of the CD/RM data set outweigh many of these concerns and enable a robust, timely analysis of clinical outcomes with a validated data source.
Although our analysis presents evidence that the expansion led to increases in insurance coverage, we recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations. Evaluation of individual components (eTable 6 and eTable 7 in the Supplement) revealed varying patterns of change after expansion, with some components with marked improvement in expansion states after expansion and others with less of a decline in improvement after expansion. Despite this heterogeneity, the overall changes and pattern are consistent with improved care for each component in expansion states compared with changes in nonexpansion states. Furthermore, Medicaid recipients and uninsured patients experienced more improved outcomes in expansion states compared with privately insured patients (Table 3). Privately insured patients in expansion states may serve as an additional within-state control group to assess for regional differences independent of insurance expansion, although they are not truly a control group given the ACA’s numerous policies that affect this population.
In addition, we defined the postreform period as any discharge after January 1, 2014. Although 5 states partially expanded Medicaid before 2014 and another 7 states expanded after 2014, the insurance coverage trends seen in our data set had the most marked shift starting in 2014. Limitations on state identifiers in our data set prevented additional sensitivity testing through inclusion or exclusion of these states from analysis. However, the early expansion states may have contributed to a trend toward a decreasing uninsured rate in expansion states before 2014. Analysis of our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014 (Table 2), which could partly explain the worsening of outcomes after 2014, whereas expansion states had stabilization or improvement.
Our findings also may not be generalizable for other medical conditions. We selected these diagnoses and procedures based on well-established disparities in presentation and management based on insurance coverage. Underlying pathophysiologic mechanisms or comorbidities, rather than delays in care, may contribute to severity of disease at presentation and subsequent management. Compared with states that expanded Medicaid, nonexpansion states are known to have higher rates of comorbid conditions, including obesity and cardiovascular disease, which may limit generalizability. However, these differences between expansion and nonexpansion states should not bias our difference-in-differences analysis unless they were changing significantly during the study period; stable differences between expansion and nonexpansion states were filtered out with our study design.
Finally, additional changes in care delivery associated with and independent of the ACA could have potentially influenced our findings. Because these data do not enable the evaluation of hospital- or state-specific programs of redesigned care, ongoing assessment of alternative payment and delivery models is needed to ensure that changes are equitable across populations.
Conclusions
In this study of surgical patients in 42 states (including Washington, DC), the ACA’s Medicaid expansion was associated with higher coverage rates, earlier presentation, and improved probability of optimal care for common and serious surgical conditions. Our data reinforce that insurance coverage is an important contributor to earlier presentation with less severe disease at the time of diagnosis. As policymakers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion.
eTable 1. List of Medicaid Expansion and Nonexpansion States Included in Study
eTable 2. ICD-9 Codes Used for Inclusion in Study
eTable 3. Coding for Early Uncomplicated Care and Optimal Care
eTable 4. Trends in Outcomes Before the Full Medicaid Expansion
eTable 5. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, by Condition and for Full Sample
eTable 6. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, by Condition and for Medicaid and Uninsured Patients
eTable 7. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, for Hospitals Present in Database for All 6 Years
eTable 8. Changes in Admission Rates After Medicaid Expansion
References
- 1.Cohen RA, Martinez ME, Zammitti EP. Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey, 2015. Hyattsville, MD: National Center for Health Statistics; 2016. [Google Scholar]
- 2.Frean M, Gruber J, Sommers BD. Disentangling the ACA’s coverage effects: lessons for policymakers. N Engl J Med. 2016;375(17):1605-1608. [DOI] [PubMed] [Google Scholar]
- 3.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366-374. [DOI] [PubMed] [Google Scholar]
- 4.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501-1509. [DOI] [PubMed] [Google Scholar]
- 5.Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164(12):795-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott JW, Havens JM, Wolf LL, et al. . Insurance status is associated with complex presentation among emergency general surgery patients. Surgery. 2017;161(2):320-328. doi: 10.1016/j.surg.2016.08.038 [DOI] [PubMed] [Google Scholar]
- 7.Greenstein AJ, Moskowitz A, Gelijns AC, Egorova NN. Payer status and treatment paradigm for acute cholecystitis. Arch Surg. 2012;147(5):453-458. [DOI] [PubMed] [Google Scholar]
- 8.Giacovelli JK, Egorova N, Nowygrod R, Gelijns A, Kent KC, Morrissey NJ. Insurance status predicts access to care and outcomes of vascular disease. J Vasc Surg. 2008;48(4):905-911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersen ND, Hanna JM, Ganapathi AM, et al. . Insurance status predicts acuity of thoracic aortic operations. J Thorac Cardiovasc Surg. 2014;148(5):2082-2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varela JE, Nguyen NT. Disparities in access to basic laparoscopic surgery at U.S. academic medical centers. Surg Endosc. 2011;25(4):1209-1214. [DOI] [PubMed] [Google Scholar]
- 11.Guller U, Jain N, Curtis LH, Oertli D, Heberer M, Pietrobon R. Insurance status and race represent independent predictors of undergoing laparoscopic surgery for appendicitis: secondary data analysis of 145,546 patients. J Am Coll Surg. 2004;199(4):567-575. [DOI] [PubMed] [Google Scholar]
- 12.Henry AJ, Hevelone ND, Belkin M, Nguyen LL. Socioeconomic and hospital-related predictors of amputation for critical limb ischemia. J Vasc Surg. 2011;53(2):330-339.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loehrer AP, Hawkins AT, Auchincloss HG, Song Z, Hutter MM, Patel VI. Impact of expanded insurance coverage on racial disparities in vascular disease: insights from Massachusetts. Ann Surg. 2016;263(4):705-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Massachusetts health care reform and reduced racial disparities in minimally invasive surgery. JAMA Surg. 2013;148(12):1116-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Influence of health insurance expansion on disparities in the treatment of acute cholecystitis. Ann Surg. 2015;262(1):139-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen NT, Hinojosa MW, Fayad C, et al. . Laparoscopic surgery is associated with a lower incidence of venous thromboembolism compared with open surgery. Ann Surg. 2007;246(6):1021-1027. [DOI] [PubMed] [Google Scholar]
- 17.Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikov D. Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg. 2012;256(3):462-468. [DOI] [PubMed] [Google Scholar]
- 18.Sutton JM, Hayes AJ, Wilson GC, et al. . Validation of the University HealthSystem Consortium administrative dataset: concordance and discordance with patient-level institutional data. J Surg Res. 2014;190(2):484-490. [DOI] [PubMed] [Google Scholar]
- 19.Scott JW, Olufajo OA, Brat GA, et al. . Use of national burden to define operative emergency general surgery. JAMA Surg. 2016;151(6):e160480. [DOI] [PubMed] [Google Scholar]
- 20.Schermerhorn ML, Bensley RP, Giles KA, et al. . Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Ann Surg. 2012;256(4):651-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110(6):738-743. [DOI] [PubMed] [Google Scholar]
- 22.Lo CM, Liu CL, Fan ST, Lai EC, Wong J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227(4):461-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 2010;97(2):141-150. [DOI] [PubMed] [Google Scholar]
- 24.Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 2011;254(6):927-932. [DOI] [PubMed] [Google Scholar]
- 25.Yau KK, Siu WT, Tang CN, Yang GPC, Li MKW. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007;205(1):60-65. [DOI] [PubMed] [Google Scholar]
- 26.Lujan JA, Parrilla P, Robles R, Marin P, Torralba JA, Garcia-Ayllon J. Laparoscopic cholecystectomy vs open cholecystectomy in the treatment of acute cholecystitis: a prospective study. Arch Surg. 1998;133(2):173-175. [DOI] [PubMed] [Google Scholar]
- 27.Egorova NN, Guillerme S, Gelijns A, et al. . An analysis of the outcomes of a decade of experience with lower extremity revascularization including limb salvage, lengths of stay, and safety. J Vasc Surg. 2010;51(4):878-885, 885.e1. [DOI] [PubMed] [Google Scholar]
- 28.Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47(1, pt 1):255-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 30.Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1993;13:19-23. [Google Scholar]
- 31.Collins SR, Gunja M, Doty MM, Beutel S. Americans’ Experiences With ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction. New York, NY: The Commonwealth Fund; 2016. [PubMed] [Google Scholar]
- 32.Shartzer A, Long SK, Anderson N. Access to care and affordability have improved following Affordable Care Act implementation; problems remain. Health Aff (Millwood). 2016;35(1):161-168. [DOI] [PubMed] [Google Scholar]
- 33.Dranove D, Garthwaite C, Ody C. Uncompensated care decreased at hospitals in Medicaid expansion states but not at hospitals in nonexpansion states. Health Aff (Millwood). 2016;35(8):1471-1479. [DOI] [PubMed] [Google Scholar]
- 34.Blavin F. Association between the 2014 Medicaid expansion and US hospital finances. JAMA. 2016;316(14):1475-1483. [DOI] [PubMed] [Google Scholar]
- 35.Scott JW, Rose JA, Tsai TC, et al. . Impact of ACA insurance coverage expansion on perforated appendix rates among young adults. Med Care. 2016;54(9):818-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finkelstein AN, Taubman SL, Allen HL, Wright BJ, Baicker K. Effect of Medicaid coverage on ED use: further evidence from Oregon’s experiment. N Engl J Med. 2016;375(16):1505-1507. [DOI] [PubMed] [Google Scholar]
- 37.Doyle JJ. Health insurance, treatment and outcomes: using auto accidents as health shocks. Rev Econ Stat. 2005;87:256-270. [Google Scholar]
- 38.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886-892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg. 2011;146(3):308-314. [DOI] [PubMed] [Google Scholar]
- 40.Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of US adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring). 2014;22(3):868-874. [DOI] [PubMed] [Google Scholar]
- 41.Cushman M, Cantrell RA, McClure LA, et al. . Estimated 10-year stroke risk by region and race in the United States: geographic and racial differences in stroke risk. Ann Neurol. 2008;64(5):507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ezzati M, Oza S, Danaei G, Murray CJL. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117(7):905-914. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. List of Medicaid Expansion and Nonexpansion States Included in Study
eTable 2. ICD-9 Codes Used for Inclusion in Study
eTable 3. Coding for Early Uncomplicated Care and Optimal Care
eTable 4. Trends in Outcomes Before the Full Medicaid Expansion
eTable 5. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, by Condition and for Full Sample
eTable 6. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, by Condition and for Medicaid and Uninsured Patients
eTable 7. Changes in Rates of Early Uncomplicated Presentation and Optimal Care for Select Surgical Conditions After Medicaid Expansion, for Hospitals Present in Database for All 6 Years
eTable 8. Changes in Admission Rates After Medicaid Expansion