Abstract
OBJECTIVES
To examine the associations of resistance exercise, independent of and combined with aerobic exercise, with the risk of developing hypercholesterolemia in men.
PATIENTS AND METHODS
A total of 7,317 men, aged 18–83 years (mean 46), without hypercholesterolemia at baseline were included. Participants received extensive preventive medical examinations at the Cooper Clinic in Dallas, Texas between January 1, 1987, and December 31, 2006. Frequency (times/week) and total amount (minutes/week) of resistance and aerobic exercise were determined by self-report. Hypercholesterolemia was defined as total cholesterol ≥240 mg/dL or physician-diagnosis.
RESULTS
During median follow-up of 4 years (minimum, 0.1 year; maximum, 19 years), 1,430 men (20%) developed hypercholesterolemia. Individuals meeting the resistance exercise guidelines (≥2 days/week) had a 13% lower risk of developing hypercholesterolemia (HR, 0.87; 95% CI, 0.76– 0.99; P=.04) after adjustment for general characteristics, lifestyle factors and aerobic exercise. In addition, less than 1 hour/week and 2 sessions/week of resistance exercise were associated with 32% and 31% lower risks of hypercholesterolemia (HR, 0.68; 95% CI, 0.54–0.86; P=.001 and HR, 0.69; 95% CI, 0.54–0.88; P=.003), respectively, compared to no resistance exercise. Higher levels of resistance exercise did not show benefits. Meeting both resistance and aerobic exercise (≥500 MET-minutes/week) guidelines lowered the risk of developing hypercholesterolemia by 22% (HR, 0.78; 95% CI, 0.68–0.91; P=.002), compared to meeting none of the guidelines.
CONCLUSIONS
Compared to no resistance exercise, less than 1 hour/week of resistance exercise, independent of aerobic exercise, is associated with a significantly lower risk of developing hypercholesterolemia in men. However, the lowest risk of hypercholesterolemia was found at 58 minutes per week of resistance exercise. This suggests that resistance exercise should be encouraged to prevent hypercholesterolemia in men. However, future studies with a more rigorous analysis including significant potential confounders (e.g., diet, medications) are warranted.
Keywords: Resistance exercise, hypercholesterolemia, physical activity, cardiovascular risk factor, cholesterol
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States and many other countries, especially throughout the Westernized World. 1 Hypercholesterolemia, one of the most important risk factors for CVD 2, 3, occurs in 13.1% of US adult population. 4 Regular physical activity (PA) is recommended for treating and preventing hypercholesterolemia. 5 Aerobic exercise uses large muscle groups continuously and rhythmically, and its benefits on serum cholesterol levels are well-documented. 6–8 On the other hand, resistance exercise is based on repeated bouts of isolated muscle groups and may therefore result in different physiological effects or health benefits. 9 Evidence for the different molecular pathways to reduce total cholesterol by aerobic or resistance exercise is scarce. However, earlier studies showed the different effects of aerobic and resistance exercise on cardiovascular health outcomes. 9–11 Meta-analyses of resistance exercise training on total cholesterol levels found contradictory results. 12–14 However, these trials had relatively short intervention periods and a lack of statistical power. 11 A cross-sectional study showed that engagement in regular resistance exercise was associated with lower total cholesterol levels. 15 However, evidence regarding the effects of resistance exercise on the development of hypercholesterolemia from large prospective cohort studies is very limited. The aim of this study is to examine the association of resistance exercise, independent of and combined with aerobic exercise, with the risk of developing hypercholesterolemia in relatively healthy men. We hypothesize that resistance exercise lowers the risk of developing hypercholesterolemia, and participating in both resistance and aerobic exercise is superior in decreasing the risk of hypercholesterolemia, when compared with each individual type of exercise alone.
Methods
Study Population
Men were included if they had baseline measurements of self-reported resistance exercise and other covariates, performed comprehensive medical examinations at baseline, and participated in at least one follow-up clinical examination. Among 11,601 men meeting the above inclusion criteria, 848 were excluded due to a history of myocardial infarction, stroke, or cancer at baseline. In addition, 3,436 men were excluded as a result of hypercholesterolemia at baseline. The final sample included 7,317 men aged 18–83 years at baseline (mean age 46 years, SD 10). Women were excluded from the study because of a relatively small proportion of women (22%) in the Aerobics Center Longitudinal Study (ACLS) and a very low number of hypercholesterolemia cases in women (n<10) in several main resistance exercise categories, which prevented us from running meaningful analyses due to low statistical power. This study used data from the ACLS, which is a cohort examining the associations of clinical and lifestyle factors including PA with the development of chronic diseases and mortality. Participants received extensive preventive medical examinations at the Cooper Clinic in Dallas, Texas between January 1, 1987, and December 31, 2006.The study population consisted predominantly of non-Hispanic whites (>95%), well educated, and employed in, or retired from, professional or executive positions. 16 The study was annually approved by the Cooper Institute institutional review board. Before data collection at baseline and during follow-up examinations, written informed consents were acquired from each participant.
Clinical examination
Comprehensive medical examinations were performed at baseline. Body mass index (BMI) was calculated using measured weight and height squared (kg/m2). After at least 12-hour fasting, blood was sampled by a trained phlebotomist for determination of total cholesterol (mg/dl) using a basic lipid panel and via automated bioassays in the Cooper Clinic laboratory in accordance with the Centers for Disease Control and Prevention Lipid Standardization Program. Resting systolic and diastolic blood pressure (mm Hg) were calculated as the average of at least two readings after 5 minutes of seated rest using the standard auscultatory methods. A medical history questionnaire was used to assess age, gender, smoking status, alcohol consumption, personal history of physician-diagnosed hypercholesterolemia, cancer and CVD, and parental history of hypercholesterolemia. More than 14 alcoholic drinks per week were defined as heavy alcohol drinking in men. 11
Assessment of resistance and aerobic exercise
Self-reported muscle-strengthening activities, using either free weights or weight training, were collected at baseline by a PA questionnaire. Participants were queried about the weekly frequency and average exercise duration (minutes) in each session over the past 3 months. We multiplied the frequency with the average minutes per session to calculate the total amount of resistance exercise per week (minutes/week). Frequency (0, 1, 2, 3, 4 or ≥5 times/week) and total amount (0, 1–59, 60–119, 120–179 and ≥180 minutes/week) of resistance exercise, as well as meeting the 2008 Physical Activity Guidelines for resistance exercise (≥2 times per week 17) were used as our main exposures. To examine whether frequency (1–2 vs. ≥3 times/week) at the same total amount of resistance exercise affects the risk of hypercholesterolemia, we combined the categories of minutes per week of resistance exercise with frequencies per week of resistance exercise. For instance, some individuals performed resistance exercise for 1 hour in 1 or 2 sessions per week (e.g., weekend warriors), while others performed the same hour of resistance exercise in 3 or more sessions per week. Aerobic exercise was determined by a PA questionnaire containing self-reported leisure-time or recreational activities over the past 3 months. Subsequently, aerobic exercise was divided into four different categories: “inactive (0 MET-minutes/week)”, “insufficient (1–499 MET-minutes/week)”, “medium (500–999 MET-minutes/week)” and “high (≥1,000 MET-minutes/week)” based on the 2008 US Physical Activity Guidelines. Meeting the 2008 Physical Activity Guidelines for aerobic exercise were defined as ≥500 MET-minutes/week (equivalent to ≥150 minutes of moderate-intensity activities/week) based on the guidelines. 17
Definition of hypercholesterolemia
The criteria of the National Cholesterol Education Program Adult Treatment Panel III were used to classify hypercholesterolemia. 18 Hypercholesterolemia was defined as total cholesterol concentration of ≥240 mg/dL or physician-diagnosed hypercholesterolemia. Participants were followed from the baseline examination to the first event or diagnosis of hypercholesterolemia for men who developed hypercholesterolemia, or the last follow-up examination through 2006 for men who did not develop hypercholesterolemia.
Statistical Analysis
We described baseline characteristics by the total weekly amount of resistance exercise (minutes/week). Differences in baseline characteristics for participants across different amounts of resistance exercise were evaluated using the analysis of variance (ANOVA) for continuous variables and chi-squared test for categorical variables. We used Cox proportional hazard regression to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of incident hypercholesterolemia across different strata of weekly amounts of resistance exercise. Participants who were not engaged in resistance exercise were used as the reference category. The first regression model was adjusted for age (years) and examination year (years). The second model was adjusted for variables in model 1 plus BMI (kg/m2), current smoking (yes/no), heavy alcohol drinking (yes/no), abnormal electrocardiography (yes/no), systolic and diastolic blood pressure and parental history of hypercholesterolemia at baseline (yes/no). The third model was adjusted for variables in model 2 plus aerobic exercise (inactive, insufficient, medium, and high) at baseline. In order to assess the independent and combined effects of resistance and aerobic exercise, we compared individuals meeting both aerobic and resistance exercise guidelines, and those meeting only aerobic or resistance exercise guidelines with those who met neither guideline. Further, to illustrate the nature of the possible dose-response relationship between resistance exercise (minutes/week) and hypercholesterolemia, we used restricted cubic spline regression. We tested 3, 4 and 5 knots and calculated the Akaike Information Criterion (AIC) to identify the best fit model. 19 All models had a similar AIC, and we chose the model with 5 knots, which is in line with the categorical analyses. The knots were placed at 5th, 25th, 50th, 75th, and 95th percentile based on men who were participating in resistance exercise. 19, 20 This analysis was adjusted for the covariates of model 3. We performed a test for non-linearity, which compared models with the cubic spline terms and models with only the linear terms using the likelihood ratio test. Significance was set at 2-tailed alpha <.05. All analyses were conducted using SAS software, version 9.4.
Results
After a median (interquartile range) follow-up of 4 years (2 to 7), 1,432 men (20%) developed hypercholesterolemia. Among men who participated in resistance exercise, most men (62%) performed resistance exercise for less than 2 hours per week (Table 1). Compared to men with no resistance exercise, men with higher levels of resistance exercise were more likely to be younger, had a lower BMI, and were more aerobically active. In addition, participants performing resistance exercise had a slightly higher prevalence of paternal history of hypercholesterolemia and lower baseline values for total cholesterol.
Table 1.
| Characteristics | Weekly minutes of resistance exercise (min/week) | P-value | ||||
|---|---|---|---|---|---|---|
| 0(n=5,165) | 1–59(n=526) | 60–119(n=802) | 120–179(n=378) | ≥180(n=446) | ||
| Age (years) | 47 (10) | 45 (9) | 46 (9) | 45 (10) | 42 (10) | <.001 |
| BMI (kg/m2) | 26.5 (3.8) | 25.7 (3.1) | 25.6 (3.0) | 26.1 (3.2) | 25.9 (3.5) | <.001 |
| Current smokers | 674 (13%) | 52 (10%) | 81 (10%) | 49 (13%) | 53 (12%) | .06 |
| Heavy alcohol drinking | 490 (9%) | 53 (10%) | 77 (10%) | 36 (10%) | 32 (7%) | .56 |
| Aerobic exercise | ||||||
| (MET-min/week) | <.001 | |||||
| 0 | 1,659 (32%) | 30 (6%) | 32 (4%) | 24 (6%) | 35 (8%) | |
| 1–499 | 771 (15%) | 66 (13%) | 87 (11%) | 52 (14%) | 56 (13%) | |
| 500–999 | 881 (17%) | 121 (23%) | 191 (24%) | 72 (19%) | 73 (16%) | |
| ≥ 1000 | 1,854 (36%) | 309 (59%) | 492 (61%) | 230 (61%) | 282 (63%) | |
| Abnormal ECG | 407 (8%) | 42 (8%) | 61 (8%) | 22 (6%) | 25 (6%) | .30 |
| Parental history of hypercholesterolemia | 99 (2%) | 13 (2%) | 32 (4%) | 16 (4%) | 15 (3%) | <.001 |
| Systolic blood pressure (mmHg) | 121 (13) | 121 (13) | 121 (13) | 121 (12) | 122 (13) | .37 |
| Diastolic blood pressure (mmHg) | 81 (10) | 80 (9) | 80 (9) | 81 (9) | 81 (9) | .06 |
| Total cholesterol (mg/dl) | 194.6 (26.6) | 190.1(26.8) | 188.5(27.6) | 188.4(29.1) | 185.1(29.0) | <.001 |
BMI=body mass index; ECG=electrocardiographic findings; MET=metabolic equivalent task.
Data is presented in mean (SD) unless indicated as n (%).
Men performing any resistance exercise had a 14% lower risk of developing hypercholesterolemia (HR, 0.86; 95% CI, 0.76–0.98; P=.02) after adjustment for potential confounders including aerobic exercise levels (Table 2). Similar hypercholesterolemia risk reduction by 13% (HR, 0.87; 95% CI, 0.76– 0.99; P=.04) was also found in men meeting the resistance exercise guidelines after full adjustment. We found that only less than one hour per week of resistance exercise was significantly associated with a 32% reduced risk of hypercholesterolemia (HR, 0.68; 95% CI, 0.54– 0.86; P=.001) after full adjustment (model 3). Also, 2 times per week of resistance exercise was beneficial in reducing 31% risk of developing hypercholesterolemia (HR, 0.69; 95% CI, 0.54–0.88; P=.003), compared to no resistance exercise (model 3). After further adjustment for baseline levels of total cholesterol in additional analysis, results were similar and less than one hour of weekly resistance exercise remained significant for reducing the risk of hypercholesterolemia (HR, 0.73; 95% CI, 0.58–0.93; P=0.01). When we also adjusted for a borderline hypercholesterolemia (yes or no) at baseline defined as a total cholesterol level of 200–239 mg/dl, 21 we also observed a similar result (HR, 0.69; 95% CI, 0.54–0.87; P=.003). Additional subgroup analyses for different age (<50 vs. ≥50 years old) and BMI (<25 vs. ≥25 kg/m2) groups, and men who participated in resistance exercise less than one year vs. more than one year demonstrated similar negative associations.
Table 2.
Hazard ratio of hypercholesterolemia by weekly frequency and minutes of resistance exercise.
| N (%) | No. of cases | Adjusted Hazard Ratio | |||
|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |||
| Weekly minutes of resistance exercise (min/week) | |||||
| 0 | 5,165 (71%) | 1,077 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| 1–59 | 526 (7%) | 76 | 0.65 (0.51–0.82) | 0.66 (0.52–0.83) | 0.68 (0.54–0.86) |
| 60–119 | 802 (11%) | 136 | 0.88 (0.73–1.05) | 0.91 (0.76–1.08) | 0.93 (0.78–1.12) |
| 120–179 | 378 (5%) | 64 | 0.81 (0.63–1.05) | 0.83 (0.65–1.07) | 0.86 (0.67–1.11) |
| ≥180 | 446 (6%) | 77 | 0.94 (0.74–1.18) | 0.95 (0.75–1.20) | 0.98 (0.77–1.24) |
| P for linear trend | .04 | .10 | .28 | ||
| P for quadratic trends | .02 | .04 | .08 | ||
| Any resistance exercise | |||||
| No (0 min/week) | 5,165 (71%) | 1,077 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Yes (≥1 min/week) | 2,152 (29%) | 353 | 0.81 (0.72–0.92) | 0.83 (0.74–0.94) | 0.86 (0.76–0.98) |
| Weekly frequency of resistance exercise (times/week) | |||||
| 0 | 5,165 (71%) | 1,077 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| 1 | 165 (2%) | 20 | 0.74 (0.47–1.15) | 0.75 (0.48–1.18) | 0.77 (0.49–1.20) |
| 2 | 529 (7%) | 71 | 0.66 (0.51–0.83) | 0.67 (0.53–0.85) | 0.69 (0.54–0.88) |
| 3 | 951 (13%) | 171 | 0.89 (0.75–1.04) | 0.91 (0.77–1.07) | 0.93 (0.79–1.10) |
| 4 | 304 (4%) | 50 | 0.78 (0.59–1.04) | 0.81 (0.61–1.08) | 0.84 (0.63–1.12) |
| ≥ 5 | 203 (3%) | 41 | 0.96 (0.70–1.32) | 0.99 (0.72–1.35) | 1.02 (0.74–1.39) |
| P for linear trend | .01 | .04 | .13 | ||
| P for quadratic trends | .02 | 0.02 | .04 | ||
| Recommended resistance exercise | |||||
| No (<2 days/week) | 5,330 (73%) | 1,097 | 1.00 [reference] | 1.00 [reference] | 1.00 [reference] |
| Yes (≥2 days/week) | 1,987 (27%) | 333 | 0.82 (0.73–0.93) | 0.84 (0.74–0.96) | 0.87 (0.76–0.99) |
Adjusted for age and examination year.
Adjusted for model 1 plus body mass index, current smoking, heavy alcohol drinking, abnormal electrocardiography, systolic and diastolic blood pressure, and parental history of hypercholesterolemia.
Adjusted for model 2 plus aerobic exercise (inactive, insufficient, medium, and high)
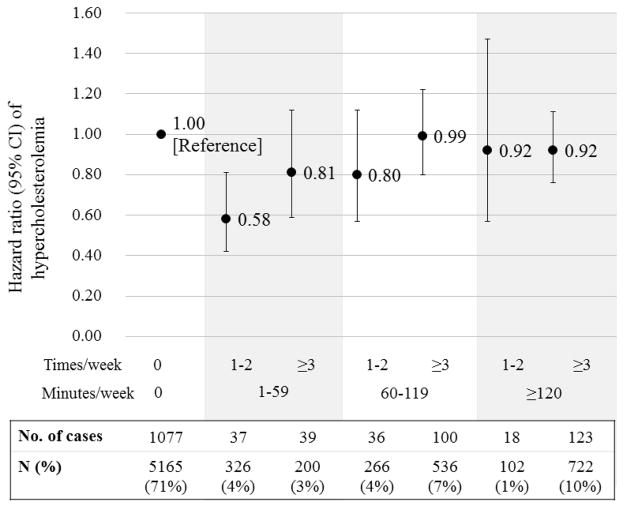
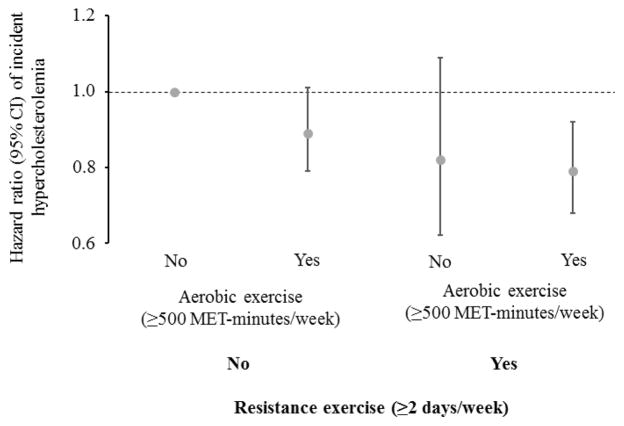
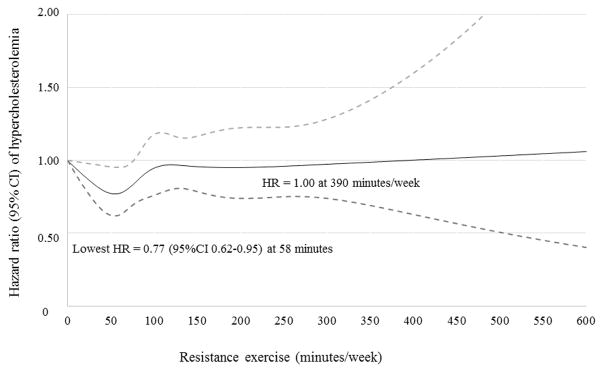
Figure 1 showed that the risk of hypercholesterolemia in those performing less than one hour of weekly resistance exercise in 1–2 times per week was 42% significantly lower, compared to no resistance exercise (HR, 0.58; 95% CI, 0.42–0.81; P=.001). However, we observed no significant results in other categories of resistance exercise. The combined effects of resistance and aerobic exercise are presented in Figure 2. The result demonstrates that meeting both guidelines for resistance and aerobic exercise was associated with the lowest risk (22%) of developing hypercholesterolemia (HR, 0.78; 95% CI, 0.68–0.91; P=.002), compared to meeting none of the guidelines. We tested effect modification by aerobic exercise on the association between resistance exercise and incident hypercholesterolemia using both interaction terms in the regression and by comparing risk estimates in the stratified analysis by meeting the aerobic exercise guidelines. We found no significant interaction (P>.05), and the associations were similar in both individuals meeting and not meeting the aerobic exercise guidelines. Figure 3 displays the dose-response relationship between resistance exercise (minutes/week) and the risk of hypercholesterolemia. The P-value for nonlinearity was not statistically significant (P=.13), which suggest a linear dose-response relationship. However, the lowest risk of hypercholesterolemia was found at 58 minutes per week of resistance exercise (HR, 0.77; 95% CI, 0.62–0.95; P<.05). This finding is consistent with the results in the categorical analyses (Table 2), suggesting the lowest risk of hypercholesterolemia in 1–59 minutes/week and 2 times/week of resistance exercise.
Figure 1.
Hazard ratios of hypercholesterolemia by the combination of weekly frequency (1–2 vs. ≥3 times/week) and minutes of resistance exercise (0, 1–59, 60–119, and ≥120 min/week). The dots indicate hazard ratios and the bars indicate 95% confidence intervals. The model was adjusted for age, examination year, body mass index, current smoking, heavy alcohol drinking, abnormal electrocardiography, systolic and diastolic blood pressure, parental history of hypercholesterolemia, and aerobic exercise.
Figure 2.
Hazard ratios of hypercholesterolemia by meeting the 2008 US Physical Activity Guidelines for resistance (≥2 days/week) and aerobic activities (≥500 MET-minutes/week). The dots present hazard ratios and the bars 95% confidence intervals. The hazard ratio (95% CI) was 0.89 (95% CI, 0.79–1.01) for only meeting the aerobic exercise guidelines, 0.82 (95% CI, 0.62–1.09) for only meeting the resistance exercise guidelines, and 0.79 (95% CI, 0.68–0.91) for meeting both guidelines. The model was adjusted for age, examination year, body mass index, current smoking, heavy alcohol drinking, abnormal electrocardiography, systolic and diastolic blood pressure, and parental history of hypercholesterolemia.
Figure 3.
The dose-response relationship between resistance exercise (minutes/week) and the risk of hypercholesterolemia. Dotted lines represent 95% confidence intervals for the trend obtained from restricted cubic spline regression (5 knots at 25, 60, 90, 135 and 270 minutes/week). The model included the following covariates: age, examination year, body mass index, current smoking, heavy alcohol drinking, abnormal electrocardiography, systolic and diastolic blood pressure, parental history of hypercholesterolemia, and aerobic exercise. P=.13 for a nonlinear relationship.
Discussion
This study showed that less than one hour of weekly resistance exercise, even 1–2 times per week, was associated with significantly lower risk of developing hypercholesterolemia, compared to no resistance exercise, whereas no benefits were found at higher levels of resistance exercise. In addition, meeting both resistance and aerobic exercise guidelines yielded the largest benefits with a 21% lower risk in developing hypercholesterolemia, compared to meeting none of the guidelines. This result suggests that adding relatively small doses of resistance exercise (<1 hour/week) to aerobic exercise could provide additional benefits in preventing hypercholesterolemia.
Several recent meta-analyses of controlled exercise trials found inconsistent results regarding the effect of resistance exercise training on total cholesterol levels. 12–14 The lack of improvement in total cholesterol in several intervention studies might be due to short exercise intervention periods, lack of statistical power because of small sample sizes and low total cholesterol values at baseline in relatively healthy populations, which may reduce the potential effects of resistance exercise. 11 However, our large prospective study with a long-term follow-up clearly demonstrates that engagement in resistance exercise is significantly associated with a lower risk of incident hypercholesterolemia. This result is consistent with the findings from the earlier cross-sectional analysis by Drenowatz et al. 15 However, the current study further investigated the prospective effect of meeting the resistance exercise guidelines, independent of and combined with aerobic exercise, and the dose-response relationship between resistance exercise and the incidence of hypercholesterolemia.
Although the current PA guidelines suggest that more exercise and physical activity generally provide greater health benefits, the dose-response relationships of different types and intensities of exercise with different health outcomes are still unclear and controversial. 22, 23 Therefore, we investigated the dose-response relationship between resistance exercise and the risk of hypercholesterolemia in this study. First, in the association between exercise frequency and hypercholesterolemia, we found that 2 times per week of resistance exercise was associated with a lower risk of developing hypercholesterolemia. However, higher frequencies of resistance exercise were not necessary to produce additional benefits to prevent hypercholesterolemia (Table 2). The limitation of using frequency of exercise is that it does not fully reflect the total amount of exercise, since exercise duration in each session is not considered in frequency of exercise. Therefore, we also used the total volume (minutes) of resistance exercise, and found a significantly lower risk of developing hypercholesterolemia in less than one hour per week. However, the benefits to prevent hypercholesterolemia with higher amounts of resistance exercise were not significant (P >.05), compared to no resistance exercise, which again suggests no further benefits by performing more resistance exercise. In fact, the associations between frequency and total amount of weekly resistance exercise and hypercholesterolemia were more likely reverse J- or U-shaped with a quadratic trend rather than linear trend (Table 2). When using the restricted cubic spline regression (Figure 3), the P-value for non-linearity suggested a linear dose-response relationship. However, we found the largest benefit at 58 minutes/week of resistance exercise (HR, 0.77; 95% CI, 0.62–0.95), similar to the result from the categorical data analyses in Table 2. Further, HRs for higher levels of resistance exercise were directed towards 1.00. Nevertheless, these results should be interpret carefully, since the CIs are wide and sample size are smaller at higher dose of resistance exercise. A recent study investigating the association between resistance exercise and CVD in women also found no additional benefits in higher levels of resistance exercise. However, they found a significant effect of resistance exercise in 60–119 minutes per week, which is a higher amount of resistance exercise (minutes/week) than what we found. 24 An earlier study investigating the associations between muscular strength and CVD and all-cause mortality also found no additional benefits in the highest third, compared to the middle third of muscular strength in a similar population. 25 Nevertheless, other studies examining CVD risk factors such as diabetes did show a linear dose-response relationship with larger benefits by participating in more resistance exercise. 26, 27 The difference might be explained by different dose-response curves of resistance exercise with hypercholesterolemia and diabetes, possibly related with the improvements in insulin sensitivity noted with resistance exercise in patients with marked insulin resistance, such as those with diabetes mellitus. These contradicting findings suggest that further studies focussing on the dose-response relationship between resistance exercise and different health outcomes are needed to identify the optimal amount of resistance exercise and whether there exists an upper limit for various health outcomes.
Whether a lower frequency of resistance exercise provides health benefits is important from a public health perspective, since lack of time is a common barrier to perform exercise. 28 For example, some people may prefer 1 hour of resistance exercise in 1–2 sessions per week, whereas others prefer to divide the same hour of weekly resistance exercise in more than 2 sessions. A recent observational study demonstrated that individuals who met the aerobic activity guidelines by performing their activities in only 1–2 days per week (weekend warriors) had a similar lower risk of CVD and mortality as regularly active individuals, compared to inactive individuals. 29 These findings align with our data, where we did not find a difference in risk estimates for different frequencies (1–2 vs. ≥3 sessions/week) at the same amount of resistance exercise (Figure 1). This result suggests that even a small amount of resistance exercise at a low frequency may provide maximal benefits to prevent hypercholesterolemia. This finding could motivate more people to start participating in relatively low doses of resistance exercise for health benefits and makes performing resistance exercise more feasible at population levels.
There are some limitations in our study. We examined a large population for a relatively long follow-up period, but this cohort included primarily well-educated non-Hispanic white men from middle-to-upper socio-economic strata. This may limit the generalizability of the results to other populations. Also, the findings from this study apply only to men. However, physiological characteristics including total cholesterol value of this cohort were comparable to other representative population samples although ACLS participants were slightly more active and leaner. 16 Second, this study used self-reported data on aerobic and resistance exercise, which may cause measurement errors due to over-reporting of leisure-time physical activity in general. 30 Nevertheless, over-reporting generally induces an underestimation of the true effect of resistance exercise on the incidence of hypercholesterolemia. 31 Also, we only took baseline levels of PA into account for the analyses, therefore changes in PA patterns over time were not included in the study. However, subgroup analyses for men who participated in resistance exercise less than one year vs. more than one year at baseline demonstrated similar negative associations with incident hypercholesterolemia. Third, we had no information about lipid-lowering medication or health-promoting drugs that affect the cholesterol level. However, we excluded participants with a history of CVD and hypercholesterolemia at baseline. Finally, cholesterol levels could be affected by diet and sedentary lifestyle, but information on diet and sedentary lifestyle was lacking in this cohort. Since diet and sedentary lifestyle might be possible confounders in the association between resistance exercise and hypercholesterolemia, future studies should take diet and sedentary lifestyle into account to see whether the association is affected. Also, future investigations should explore the type/nature (e.g., intensity, isolated, circuit, etc.) of resistance exercise on hypercholesterolemia outcomes. Further, randomized controlled trials of resistance exercise are necessary to examine the causality and dose-response effects of resistance exercise on hypercholesterolemia in the future. Despite these limitations, this is the first study, to our knowledge, that has investigated the dose-response relationship between resistance exercise and incident hypercholesterolemia in a large population. In addition, we conducted more comprehensive analyses using both weekly frequency and total amount of resistance exercise, and the effects of meeting the current resistance exercise guidelines, independent of and combined with meeting the aerobic exercise guidelines.
Conclusion
Compared to no resistance exercise, men performing resistance exercise less than 1 hour per week, which could be easily accomplished by most adults, is significantly associated with the lowest risk of hypercholesterolemia, independent of aerobic exercise. However, the lowest risk of hypercholesterolemia was found at 58 minutes per week of resistance exercise based on restricted cubic spline regression (Figure 3). Meeting both recommended resistance and aerobic exercise guidelines provides the highest additional health benefit in the prevention of hypercholesterolemia. Therefore, our results suggest that resistance exercise, combined with aerobic exercise, could be encouraged in order to reduce the risk for developing hypercholesterolemia and further CVD in men. This supports the current PA guidelines and could have profound impact from a population and public health perspectives. However, future studies with a more rigorous analysis including significant potential confounders (e.g., diet, medications) are needed to produce more reliable and unbiased results.
Acknowledgments
Funding/Support: This study was supported by the National Institutes of Health grants (AG06945, HL62508, DK088195, and HL133069). FBO research activity is supported by grants from the Spanish Ministry of Economy and Competitiveness (RYC-2011-09011) and by additional funding from the University of Granada, Plan Propio de Investigación 2016, Excellence actionns: Units of Excellence; Unit of Excellence on Exercise and Health (UCEES). Steven N. Blair has received unrestricted research grants from The Coca-Cola Company, but these grants were not used to support this manuscript.
Role of the Funder/Sponsor: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors thank the Cooper Clinic physicians and technicians for collecting the baseline data and staff at the Cooper Institute for data entry and data management.
Abbreviations
- AIC
akaike Information Criterion
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
- HR
hazard ratio
- PA
physical activity
Footnotes
Conflict of interest disclosures: No
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: Final Data for 2013. Natl Vital Stat Rep. 2016;64(2):1–119. [PubMed] [Google Scholar]
- 2.Ezzati M, Hoorn SV, Rodgers A, et al. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003;362(9380):271–80. doi: 10.1016/s0140-6736(03)13968-2. [DOI] [PubMed] [Google Scholar]
- 3.Tzoulaki I, Elliott P, Kontis V, Ezzati M. Worldwide Exposures to Cardiovascular Risk Factors and Associated Health Effects: Current Knowledge and Data Gaps. Circulation. 2016;133(23):2314–33. doi: 10.1161/CIRCULATIONAHA.115.008718. [DOI] [PubMed] [Google Scholar]
- 4.Writing Group M. Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 5.Stone NJ, Robinson JG, Lichtenstein AH, et al. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 American College of Cardiology/American Heart Association cholesterol guideline. Ann Intern Med. 2014;160(5):339–43. doi: 10.7326/M14-0126. [DOI] [PubMed] [Google Scholar]
- 6.Kraus WE, Houmard JA, Duscha BD, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347(19):1483–92. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 7.Kelley GA, Kelley KS, Vu Tran Z. Aerobic exercise, lipids and lipoproteins in overweight and obese adults: a meta-analysis of randomized controlled trials. Int J Obes (Lond) 2005;29(8):881–93. doi: 10.1038/sj.ijo.0802959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kujala UM, Jokelainen J, Oksa H, et al. Increase in physical activity and cardiometabolic risk profile change during lifestyle intervention in primary healthcare: 1-year follow-up study among individuals at high risk for type 2 diabetes. BMJ Open. 2011;1(2):e000292. doi: 10.1136/bmjopen-2011-000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116(5):572–84. doi: 10.1161/CIRCULATIONAHA.107.185214. [DOI] [PubMed] [Google Scholar]
- 10.Artero EG, Lee DC, Lavie CJ, et al. Effects of muscular strength on cardiovascular risk factors and prognosis. J Cardiopulm Rehabil Prev. 2012;32(6):351–8. doi: 10.1097/HCR.0b013e3182642688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braith RW, Stewart KJ. Resistance exercise training: its role in the prevention of cardiovascular disease. Circulation. 2006;113(22):2642–50. doi: 10.1161/CIRCULATIONAHA.105.584060. [DOI] [PubMed] [Google Scholar]
- 12.Pattyn N, Cornelissen VA, Eshghi SR, Vanhees L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome: a meta-analysis of controlled trials. Sports Med. 2013;43(2):121–33. doi: 10.1007/s40279-012-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950–8. doi: 10.1161/HYPERTENSIONAHA.111.177071. [DOI] [PubMed] [Google Scholar]
- 14.Strasser B, Siebert U, Schobersberger W. Resistance training in the treatment of the metabolic syndrome: a systematic review and meta-analysis of the effect of resistance training on metabolic clustering in patients with abnormal glucose metabolism. Sports Med. 2010;40(5):397–415. doi: 10.2165/11531380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Drenowatz C, Sui X, Fritz S, et al. The association between resistance exercise and cardiovascular disease risk in women. J Sci Med Sport. 2015;18(6):632–6. doi: 10.1016/j.jsams.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blair SN, Kannel WB, Kohl HW, Goodyear N, Wilson PW. Surrogate measures of physical activity and physical fitness. Evidence for sedentary traits of resting tachycardia, obesity, and low vital capacity. Am J Epidemiol. 1989;129(6):1145–56. doi: 10.1093/oxfordjournals.aje.a115236. [DOI] [PubMed] [Google Scholar]
- 17.Kemps HM, Schep G, de Vries WR, et al. Predicting effects of exercise training in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. The American journal of cardiology. 2008;102(8):1073–8. doi: 10.1016/j.amjcard.2008.05.054. [DOI] [PubMed] [Google Scholar]
- 18.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 19.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 20.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037–57. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 21.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 22.Lee DC, Lavie CJ, Vedanthan R. Optimal dose of running for longevity: is more better or worse? J Am Coll Cardiol. 2015;65(5):420–2. doi: 10.1016/j.jacc.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 23.Eijsvogels TM, Molossi S, Lee DC, Emery MS, Thompson PD. Exercise at the Extremes: The Amount of Exercise to Reduce Cardiovascular Events. J Am Coll Cardiol. 2016;67(3):316–29. doi: 10.1016/j.jacc.2015.11.034. [DOI] [PubMed] [Google Scholar]
- 24.Shiroma EJ, Cook NR, Manson JE, et al. Strength Training and the Risk of Type 2 Diabetes and Cardiovascular Disease. Med Sci Sports Exerc. 2016 doi: 10.1249/MSS.0000000000001063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruiz JR, Sui X, Lobelo F, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008:337a439. doi: 10.1136/bmj.a439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grontved A, Rimm EB, Willett WC, Andersen LB, Hu FB. A prospective study of weight training and risk of type 2 diabetes mellitus in men. Arch Intern Med. 2012;172(17):1306–12. doi: 10.1001/archinternmed.2012.3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grontved A, Pan A, Mekary RA, et al. Muscle-strengthening and conditioning activities and risk of type 2 diabetes: a prospective study in two cohorts of US women. PLoS Med. 2014;11(1):e1001587. doi: 10.1371/journal.pmed.1001587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly S, Martin S, Kuhn I, et al. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviours by People at Mid-Life: A Rapid Systematic Review. PLoS One. 2016;11(1):e0145074. doi: 10.1371/journal.pone.0145074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Donovan G, Lee IM, Hamer M, Stamatakis E. Association of "Weekend Warrior" and Other Leisure Time Physical Activity Patterns With Risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern Med. 2017;177(3):335–42. doi: 10.1001/jamainternmed.2016.8014. [DOI] [PubMed] [Google Scholar]
- 30.Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol. 2005;161(4):389–98. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Celis-Morales CA, Perez-Bravo F, Ibanez L, et al. Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7(5):e36345. doi: 10.1371/journal.pone.0036345. [DOI] [PMC free article] [PubMed] [Google Scholar]