Abstract
The purpose of this pilot randomized controlled trial was to investigate the acceptability and efficacy of the ACCESS (Acquiring Career, Coping, Executive Control, Social Skills) Program, a group intervention tailored for young adults with autism spectrum disorder (ASD) to enhance critical skills and beliefs that promote adult functioning, including social and adaptive skills, self-determination skills, and coping self-efficacy. Forty-four adults with ASD (ages 18–38; 13 females) and their caregivers were randomly assigned to treatment or waitlist control. Compared to controls, adults in treatment significantly improved in adaptive and self-determination skills, per caregiver report, and self-reported greater belief in their ability to access social support to cope with stressors. Results provide evidence for the acceptability and efficacy of the ACCESS Program.
Keywords: Young Adults, Autism Spectrum Disorder, Randomized Controlled Trial, Social Skills, Adaptive Skills, Self-Determination, Stress, Anxiety Coping, Self-efficacy, CBT Intervention, Psychosocial Intervention
There is a tsunami of nearly half a million youth with autism spectrum disorder (ASD) entering adulthood in the US over the next decade (Roux et al. 2015). This transition to adult independence may be particularly challenging for individuals with ASD due to their core social communication impairments, extreme difficulty coping with change, overreliance on family, and high rate of co-occurring mental health conditions (Ghaziuddin et al. 1998; Simonoff et al. 2008). Compounding this problem further, upon exiting high school emerging adults with ASD face a “services cliff”, a precipitous drop in mental health and medical services, speech therapy, and case management (Levy and Perry 2011; Shattuck et al. 2011). Given this lack of services and characteristic impairments of young adults with ASD, it is not surprising that outcomes are poor for this population (Roux et al. 2017). Compared to other disability groups, adults with ASD exhibit worse social, vocational, and educational outcomes (Anderson et al. 2014; Baldwin et al. 2014; J. L. Taylor and Mailick 2014), including higher rates of unemployment and underemployment, and lower rates of independent living and college attendance or completion (Howlin et al. 2000; Newman et al. 2010; Wei et al. 2015). Thus, there is an urgent need to develop effective services and interventions to help young adults with ASD achieve optimal life outcomes. A first step is to identify barriers in the transition to adulthood for young adults with ASD, and then target for intervention those skills and beliefs needed to overcome these barriers. An interdisciplinary literature review revealed that enhancing adaptive and social skills, self-determination skills, and coping self-efficacy (i.e., self-perceived beliefs around one’s ability to cope with stressors), may support young adults with ASD in successfully transitioning to adulthood.
Skills and Beliefs that Promote Adult Functioning in ASD
Adaptive and social skills
Persistent deficits in social interactions and social communication have been identified as core deficits of ASD (Perry et al. 2009; Kenworthy et al. 2014; Liss et al. 2001; A.P.A. 2013). Social impairments extend into adulthood for those with ASD, and include difficulty initiating or responding to social interactions, engaging in normal back-and-forth conversation, and developing, maintaining, and understanding relationships. Adaptive behavior encompasses social skills, as well as daily living skills (e.g., skills related to hygiene, performing household chores, handling money, grocery shopping, preparing meals, riding a bus, and understanding personal safety) and conceptual skills (e.g., functional academics, vocational skills), and enables people to engage in daily activities with age-appropriate levels of independence (Tassé et al. 2012). A number of studies indicate that impairments in ASD impact both social skills as well as adaptive skills, including vocational, educational and daily living skills, which may be contributing to the lack of age-appropriate levels of independence and poor quality of life observed in young adults with ASD (Palmen et al. 2012). In addition, research indicates that adaptive behavior impairments become even more profound during the transition to adulthood. For instance, a cross-sectional study, which compared 1,200 children and adolescents with ASD to over 20,000 age-matched peers with intellectual disability, found that those with ASD had better adaptive behavior scores than those with intellectual disability during childhood, but in adolescence this pattern had reversed, indicating that adaptive skills are significantly below expectations for youth with ASD (Jacobson and Ackerman 1990). Despite having no cognitive disability (i.e., IQ scores above 70), youth with ASD in two large-scale studies demonstrated significant impairment in adaptive skills (Kanne et al. 2011; Pugliese et al. 2015). Notably, for those who were older and had higher IQs, adaptive skills deficits fell even further below levels expected for someone of their age and IQ. These findings suggest a greater failure to achieve age-appropriate adaptive skills during adolescence for youth with ASD with higher IQ. These deficits in adaptive skills are maintained in adulthood even for those with ASD who do not have cognitive disability (Kraper et al. 2017). Adaptive behavior is more closely correlated with social and overall functioning outcomes (i.e., socialization, independent living) than IQ or diagnosis (Farley et al. 2009). Taken together, these studies underscore the importance of targeting adaptive skills, including social skills, in interventions to improve adult functioning in ASD.
Individuals with ASD, even those without cognitive disability, demonstrate life-long impairments in adaptive skills, which impacts their independent functioning and quality of life. Yet systematic reviews of the literature indicate there are limited evidence-based interventions tailored to increase adaptive skills in adults with ASD (Palmen et al. 2012). Only a few evidence-based interventions have targeted academic or vocational skills or recreational activities in young adults with ASD (Spain and Blainey 2015; Bishop-Fitzpatrick et al. 2013; Palmen et al. 2012; Julie Lounds Taylor et al. 2012; García-Villamisar and Dattilo 2010), whereas most adaptive skills interventions have focused on social skills development, including the Aspirations Program (Hillier et al. 2007), the Social Cognition and Interaction Training – adapted for ASD (SCIT-A) (Turner-Brown et al. 2008), the UCLA PEERS for Young Adults Program (Gantman et al. 2012), and a non-manualized social skills group based in London (Howlin and Yates 1999). These adult social skills interventions incorporated many of the same topics as in the child interventions (e.g., skills for initiating, maintaining, and exiting conversations, non-verbal communication, interpersonal problem-solving, developing friendships, and managing rejection and bullying), but also extended the content to adult-specific topics related to social and adaptive skills, including employment and job interview skills, dating skills, and interpersonal problem-solving at work. Duration of these adult interventions ranged from 8-weeks to 18-weeks, with weekly sessions, except one program met monthly (Howlin and Yates 1999). They contained a variety of therapeutic techniques, including psychoeducation (i.e., education about mental health issues provided to patients and their families in order to help them better understand and cope with these issues), facilitated group discussion, video examples of social skills, rehearsal, behavior modeling by therapists, role play, feedback on performance, structured games and activities, and shared problem-solving. A group format was used by all of these adult social skills interventions, providing young adults with ASD opportunities to practice social skills among peers, normalize personal difficulties in life, share and validate feelings, reduce stigma, and engage in shared problem-solving. Only one of these evidence-based interventions, the UCLA PEERS for Young Adults Program, engaged caregivers in an adjunctive group in which they learned how to provide social coaching to reinforce concepts and support skills acquisition while also promoting social independence in their young adults with ASD (Laugeson et al. 2015; Gantman et al. 2012). Overall, the existing social skills interventions for adults with ASD utilized similar methodologies, and were found to be efficacious in improving social skills and social engagement, but interventions targeting other adaptive skills remain understudied.
Self-determination skills
Since the implementation of the Individuals with Disabilities Education Act (IDEA) in 1990, promoting self-determination has been recognized as a best practice in special education for adolescents with disabilities and has become a critical target of intervention to help young adults with ASD transition to adult independence. Self-determination is defined as a set of beliefs, knowledge and skills (e.g, goal-setting, planning, decision-making, self-monitoring, and self-advocacy) that enable individuals to engage in self-directed, autonomous behavior (Field et al. 1998; M. L. Wehmeyer 1998). Chou et al. (2016) found that youth with ASD, compared to youth with intellectual disability or learning disabilities, had significantly lower self-determination scores in the area of autonomy. Another study found that parents reported their children with ASD often did not perform well on the seven component self-determination skills (i.e., choice-making, decision-making, goal-setting, problem-solving, self-advocacy & leadership skills, self-awareness & self-knowledge, and self-management & self-regulation skills) (Carter et al. 2013a). Based on the National Longitudinal Transition Study-2 (NLTS2), self-determination was related to employment outcomes specifically in young adults with ASD (Zalewska et al. 2016). Research has found that across disability categories, higher levels of self-determination predict more positive adult outcomes, including increased employment and independent living (M. Wehmeyer and Palmer 2003; M. Wehmeyer and Schwartz 1997), better educational outcomes (Fowler et al. 2007; Lee et al. 2011), and greater quality of life (Lachapelle et al. 2005; Nota et al. 2007; M. Wehmeyer and Schwartz 1998). Taken together, these findings suggest that self-determination is pivotal in supporting optimal adult outcomes and represents a powerful intervention target for adults with ASD.
Psychoeducation is the primary treatment approach for self-determination, and is usually delivered through school-based interventions. There is empirical support for the efficacy of several school-based curricula on self-determination (Test et al. 2000). At the core of these interventions is training on self-talk strategies in which individuals ask themselves questions to set goals, taking into consideration personal interests and strengths, make plans to achieve those goals, take steps toward the goals, and then evaluate progress in order to adapt the plan as necessary. Findings from intervention studies on individuals with disabilities are promising, as they indicate that training in self-determination relates to enhanced self-determination, as well as better employment and academic outcomes (Goldberg et al. 2003; Konrad et al. 2007; Shogren et al. 2015). To our knowledge, however, there are no evidence-based interventions designed specifically for adults with ASD to target self-determination, although the few group social skills interventions designed for adults with ASD incorporate a lesson on general problem problem-solving (Spain and Blainey 2015).
Stress coping and self-efficacy
A serious barrier to the successful transition to adulthood in ASD may be related to low coping self-efficacy (Bandura 1994), or self-perceptions regarding one’s own ability to cope effectively with life stressors and challenges. Compared to the general population and other clinical populations, adults with ASD without ID self-report a poor ability to cope with stressors in everyday life and experience high levels of subjective stress and high rates of anxiety disorders (White et al. 2009; Lugnegård et al. 2011; Joshi et al. 2013; Hofvander et al. 2009; Hirvikoski and Blomqvist 2015). Further, in adults with ASD, higher stress levels are associated with worse social functioning (Bishop-Fitzpatrick et al. 2015). Based on these findings, researchers have begun to argue strongly for the need to develop evidence-based treatments for adults with ASD that focus on enhancing coping self-efficacy and skills to manage stress and anxiety in order to improve adult outcomes (Hirvikoski and Blomqvist 2015; Pahnke et al. 2014; Bishop-Fitzpatrick et al. 2015). Research on the general population has shown that coping self-efficacy influences people’s choices and persistence toward goals when faced with obstacles (Bandura, 1986; Locke & Latham, 1990). Considering this in terms of development in ASD, if young adults with ASD develop greater coping self-efficacy, they may be more likely to persist toward goals even when faced with anxiety-provoking challenges in employment, higher education, independent living, and relationships. Therefore, targeting coping self-efficacy and coping skills in interventions for young adults with ASD may help promote adult functioning.
Cognitive behavioral therapies (CBT) are extensively researched evidence-based treatments that are commonly used to increase coping self-efficacy and teach people skills to manage stress associated with daily hassles, major life events and transitions (Chesney et al. 2003; Hofmann et al. 2012), and are considered the gold standard psychosocial treatment for anxiety (Silverman et al. 2008). CBT provides training in identifying negative or distorted thoughts (e.g., “I always fail”) and physiological reactions to stressors (e.g., heart racing, headache, jittery, stomachache, sweating) and skills to cope when encountering these negative and uncomfortable thoughts or feelings (e.g., skills to challenge distorted thoughts and reappraise the situation to generate more realistic and positive thoughts), which in turn promote coping self-efficacy. In comparison to the general population, adults with ASD report less use of positive reappraisal skills and more distorted thoughts around blaming others for their own problems (Bruggink et al. 2016). Over the last decade, there have been a growing number of studies supporting the efficacy of CBT for treating anxiety in children with ASD (Chalfant et al. 2007; Freitag et al. 2016; Keehn et al. 2013; Lerner et al. 2012; Reaven et al. 2012; Sofronoff et al. 2005; Storch et al. 2013; Weston et al. 2016; Wood et al. 2009; White et al. 2013). However, CBT anxiety treatment studies on adults with ASD are limited to one case study (Cardaciotto and Herbert 2004; Weiss and Lunsky 2010) and three trials utilizing a group therapy modality (Russell et al. 2013; Hesselmark et al. 2014; Weiss and Lunsky 2010). Emerging research suggests that parent involvement may serve as an active ingredient in CBT treatment of anxiety for children with ASD, as it provides parents support and training in how to facilitate skill-building in their children outside of therapy sessions (Puleo and Kendall 2011; Sofronoff et al. 2005; Lang et al. 2010).
Development of the ACCESS Program
To begin to close the wide gap in transition services and treatments for young adults with ASD, we developed an intervention called the Adult Social Knowledge (ASK) Workshop, which was implemented as a clinical program at the MIND Institute, University of California, Davis from February – June 2015. The ASK workshop was delivered for 1.5 hours per week for 20 weeks and was designed to promote social and adaptive functioning, as well as elements of self-determination (goal setting, planning and organization) in young adults with ASD. ASK Workshop sessions were adapted from the empirically-supported Functional Adaptive Skills Training (FAST) (Bowie et al. 2012; McGurk et al. 2005; Patterson et al. 2006), which was first developed for adults with chronic mental illness and provides psychoeducation on social skills and adaptive life skills necessary for adults to engage in activities of daily living, and our evidence-based social skills training program for adolescents as described in Solomon et al. (2004).
ASK Workshop focused on three pivotal areas of adult functioning: (1) Goal Setting & Organization using App technology, (2) Social Skills & Interpersonal Communication, and (3) Communication in the Work Place & Community Engagement. Caregivers attended a concurrent group, led by University Center for Excellence in Developmental Disability (UCEDD) staff, that provided support and information about community resources. To inform the development of future evidence-based programs, we utilized a participatory design model for community health, which involves the collaboration of community members as partners in research design and intervention development (Bracht and Tsouros 1990). Specifically, we invited stakeholders, the young adults with ASD and their caregivers who participated in the ASK Program, to take part in a 1.5-hour post-treatment focus group. The focus group moderator facilitated a group discussion around a list of prepared questions relating to acceptability of the program. In the focus group, stakeholders affirmed a high level of satisfaction with the program, and underlined that the program’s training focus on adaptive, social and self-determination skills was relevant to the young adult participants with ASD and should be expanded upon in future iterations of the program. The adult participants emphasized wanting further lessons on these topics, with less emphasis on learning new app technology as they found technical training at a group level to be difficult due to participant’s varying degrees of familiarity with technology. Participants stated that they wanted more dynamic and interactive sessions to maintain their focus and engagement in the material. The caregivers reported wanting lessons that paralleled the ASD group, in order for them to better support their sons’ and daughters’ acquisition of skills outside of group. We also sought out the stakeholder perspective of the staff who delivered the ASK intervention. The primary facilitators of the young adults with ASD group and caregivers group identified that the ASK Program did not adequately address a prominent issue that thematically arose in both groups regarding stress management. Specifically, the young adults’ low confidence in their ability to manage the stressors associated with adult responsibilities (i.e., low coping self-efficacy) combined with their reliance on avoidance strategies, hindered them from taking steps toward goals and persisting in the face of obstacles. The staff also recommended more teambuilding activities during the beginning of the intervention in order to strengthen group bonding.
Building upon the ASK curriculum by taking into consideration this stakeholder feedback and the research literature, we developed a novel integrative therapy tailored for adults with ASD named the ACCESS Program (Acquiring Career, Coping, Executive Control, and Social Skills Program). Given the strong support by the stakeholders to keep and expand upon the main elements of the ASK program, in the design of the ACCESS Program we enhanced the adaptive and social skills training curriculum by focusing more extensively on social functioning in the workplace and the development of a social support network of friends to reduce reliance on caregivers, as well as provided more extensive training on self-determination skills (i.e., choice making, goal-setting, decision-making, and self-advocacy). Further, to address the criticism about the app technology, we provided a general overview of features found in goal setting and organizational apps instead of providing technical training on specific apps. To address the participants’ concerns around maintaining focus and engagement in the material and staff’s suggestions around improving group bonding, in the ACCESS curriculum we increased the number of interactive and small group activities, which served to deepen understanding of material, as well as increase the number of opportunities to practice social skills, build friendships and strengthen group bonding. In alignment with prior research that has found parent involvement serves as an active ingredient in CBT treatment in ASD (Puleo and Kendall 2011; Sofronoff et al. 2005; Lang et al. 2010), the caregiver’s focus group feedback underscored the need of caregiver training to better support skills acquisition in their young adult family member with ASD. Therefore, in the ACCESS Program we adapted the ASK caregivers support group, which had only provided social support and information on community resources, to additionally focus on providing psychoeducation to caregivers on how to facilitate the participant’s everyday use and generalization of skills and concepts learned in group in order to support their transition to optimal levels of adult independence. A major revision that came out of the staff feedback was the incorporation of stress coping lessons. In particular, ACCESS improved upon ASK by incorporating a CBT-based stress and anxiety coping module to increase coping self-efficacy and reduce stress and anxiety in participants with ASD. In order to address the stakeholders’ feedback and take advantage of the insights gained from efficacious treatments, we designed the ACCESS Program to provide a integrative therapy involving social skills training, group therapy, CBT, psychoeducation and collateral work with caregivers, utilizing a variety of techniques, including modeling of behavior by co-facilitators, role plays by participants, feedback on performance, structured games and activities, and shared problem-solving. The ACCESS curriculum targeted specific skills (adaptive, social, and self-determination skills) and coping self-efficacy (self-perceptions around the ability to cope with stressful challenges in life) because they are known to enhance adult independence.
The current study details the results of a randomized controlled trial (RCT) of the ACCESS Program. This RCT consisted of an experimental group that received the treatment first, followed by a waitlist control group. We hypothesized that the ACCESS Program would be acceptable to consumers. We also hypothesized that it would demonstrate efficacy, as illustrated by improvements from baseline to post-treatment in the treatment group compared to the waitlist control group on informant-report measurements completed by caregivers regarding the adaptive, social and self-determination skills observed in the young adults with ASD, and self-report assessments completed by the young adults with ASD on their coping self-efficacy and anxiety levels.
Methods
Participants
Participants consisted of 44 adults with ASD (13 females; 31 males), aged 18 to 38 years (see Table 1). Eligibility requirements included: a community diagnosis of ASD, meeting DSM-5 criteria for ASD based on a DSM-5 ASD symptom checklist (APA 2013), a score in the ASD range on the Autism Diagnostic Observation Schedule 2 (ADOS-2) (Lord et al. 2012), and verbal IQ ≥ 70 using the Wechsler Abbreviated Scale of Intelligence - Second Edition (WASI-II) (Wechsler and Zhou 2011). An IQ ≥ 70 was used as the cutoff due to the verbal demands of the ACCESS Program curriculum. Participants were excluded if they had not completed high school, had no spoken language, or exhibited evidence of psychosis or behavioral/conduct problems that would be disruptive or dangerous to the group or themselves. Participants were recruited via a local press release, UC Davis MIND Institute’s Subject Tracking System and social media, and recruitment fliers and referrals from psychiatrists, neurologists, general practitioners, psychologists, speech and language pathologists, occupational therapists, advocacy and support groups, California Regional Centers, and local colleges. Recruited participants were assessed for ASD diagnostic eligibility by UC Davis MIND Institute clinical psychologists who have extensive experience assessing individuals with ASD.
Table 1.
Participant Characteristics by Group at Baseline
| Variable | Control Group | Treatment Group | All | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| N | Mean/% | SD | N | Mean/% | SD | N | Mean/% | SD | |
| Age | 16 | 25.5 | 7.1 | 25 | 24.9 | 6.1 | 41 | 25.1 | 6.4 |
| Full-Scale IQ | 16 | 102.8 | 14.4 | 25 | 101.4 | 19.4 | 41 | 102.0 | 17.4 |
| Female | 4 | 25.0 | N/A | 9 | 36.0 | N/A | 13 | 31.7 | N/A |
| Caucasian | 10 | 62.5 | N/A | 20 | 80.0 | N/A | 30 | 73.2 | N/A |
| Living Independently | 5 | 31.3 | N/A | 6 | 24.0 | N/A | 11 | 26.8 | N/A |
| ADOS SA Total | 16 | 10.9 | 3.1 | 25 | 9.2 | 3.1 | 41 | 9.9 | 3.2 |
| ADOS RRB Total | 16 | 3.1 | 2.2 | 25 | 3.0 | 1.3 | 41 | 3.0 | 1.7 |
| ADOS Total | 16 | 14.0 | 3.9 | 25 | 12.2 | 3.2 | 41 | 12.9 | 3.6 |
| ADOS CSS | 16 | 7.4 | 1.6 | 25 | 6.7 | 1.9 | 41 | 7.0 | 1.8 |
| Medication | 8 | 50.0 | N/A | 14 | 56.0 | N/A | 22 | 53.7 | N/A |
| Therapy | 12 | 75.0 | N/A | 17 | 68.0 | N/A | 29 | 70.7 | N/A |
| Anxiety Disorder | 3 | 18.8 | N/A | 3 | 12.0 | N/A | 6 | 14.6 | N/A |
| Borderline Anxiety Levels | 2 | 12.5 | N/A | 3 | 12.0 | N/A | 5 | 12.2 | N/A |
| Clinical Anxiety Levels | 1 | 6.3 | N/A | 1 | 4.0 | N/A | 2 | 4.9 | N/A |
Note. ADOS = Autism Diagnostic Observation Schedule 2. SA = Social Affect. RRB = Restricted and Repetitive Behaviors. CSS = Calibrated Severity Score based on revised ADOS algorithm. Medication = Participants on psychiatric or sleep medications. Therapy = Participants receiving individual therapy services. Anxiety Disorder = Medical diagnosis of Generalized Anxiety Disorder or Social Anxiety Disorder per Social Coach report. Borderline Anxiety Levels = Participant self-reported borderline levels of anxiety based on ASR Anxiety Problems Scale. Clinical Anxiety Levels = Participant self-reported clinical levels of anxiety based on ASR Anxiety Problems Scale.
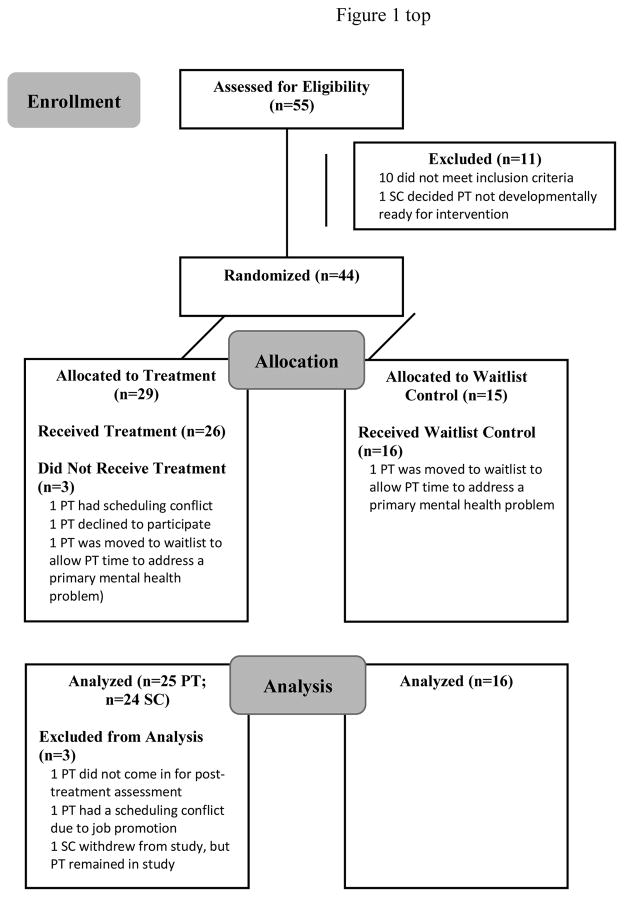
Participants with ASD were randomly assigned to condition, with 40% assigned to the waitlist control condition (n = 16) and 60% to the treatment condition (n = 28). Two separate treatment groups were run on different days of the week but provided the same ACCESS Program curriculum (n = 14/group). The randomization was stratified by age (<25 vs. >=25), sex (male vs. female), and IQ (>=85 vs. <85) after baseline measurements were completed. The waitlist control group received the ACCESS Program intervention 3 months after the two treatment groups had completed the program. See Fig. 1 for flow of participants through the trial. Each “Participant” (i.e., young adult with ASD) selected a parent or close relative, referred to as “Social Coach”, to participate in the concurrent caregiver coaching group. The Social Coach was required to be an adult and not have an ASD diagnosis. Participants assigned to the Treatment and Waitlist Control groups were permitted to continue any current medications or therapy services and to pursue new medications or therapy services as they wished during the study. Because there was not yet data on the efficacy of the intervention, we deemed it unethical to ask Participants to discontinue or change medications or therapy services. See Table 1 for information about medication and therapy utilization. Regarding comorbidity of anxiety, Table 1 presents data on Participants’ self-reported levels of anxiety and Social Coaches’ report of Participants’ current psychiatric diagnoses of anxiety disorders. Although Participants were also asked about their own psychiatric diagnoses, several stated that they were uninformed about their medical history and referred us to their Social Coach for this information. The study was approved by the UC Davis Institutional Review Board and informed consent was obtained from Participants and Social Coaches.
Fig. 1.
Participant flow chart following Consolidated Standards of Reporting Trials (CONSORT) guidelines. PT = participant. SC = Social Coach
Participation and attrition
Fifty-five Participants with ASD were assessed for eligibility, 10 were not eligible due to not meeting verbal or school completion criteria, and 1 withdrew consent before being allocated to treatment. The 44 remaining Participants were randomized to the Treatment Group or Waitlist Control Group. Due to withdrawal of consent from the study, two Participants did not receive treatment and one dropped out during treatment. One Participant was allocated to Treatment and then reported complicating mental health issues and, based on ethical considerations, was transferred to the Waitlist Control group to allow the Participant time to address these issues while still providing him the opportunity to receive the group intervention at the same time as the other members of the waitlist control group. One Participant completed treatment, but the father replaced the mother as the Social Coach early on in treatment and, therefore, the Participant remained in the analysis but the Social Coach data were removed due to the Social Coach being different at baseline and post-treatment assessments. Therefore, analysis comprised 41 Participants with ASD and their Social Coach (see Fig. 1). Regarding baseline equivalence of groups, the Treatment Group (n = 25) and Waitlist Control Group (n = 16) did not differ with respect to age, gender, IQ, and ADOS-2 scores (see Table 1). Missing data for Social Coach reports were minimal, however, there was more substantial data missing for Participant self-reports. Sample sizes per analyses are included in Table 5.
Table 5.
Primary and Selected Secondary Outcomes
| Outcome | Control Group | Treatment Group | Estimated Mean Change Due to Intervention | 95% CI | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| N |
|
N |
|
||||||
| Pre | Post | Pre | Post | ||||||
|
|
|
|
|
||||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| SC ABAS GAC | 16 | 68.1 (8.9) | 68.8 (8.6) | 20 | 68.3 (9.0) | 73.9 (11.7) | 4.1 | 0.2–8.0 | 0.04 |
| SC ABAS Conceptual Composite | 16 | 71.8 (8.8) | 72.1 (9.4) | 20 | 71.6 (10.0) | 76.7 (11.8) | 4.2 | 0.1–8.3 | 0.04 |
| SC ABAS Social Composite | 16 | 69.0 (7.3) | 69.5 (8.9) | 22 | 71.5 (8.1) | 75.9 (9.0) | 3.3 | −0.5–7.2 | 0.09 |
| SC ABAS Practical Composite | 16 | 68.4(11.1) | 69.2 (10.4) | 21 | 68.5 (9.8) | 73.5 (13.7) | 3.0 | −1.6–7.5 | 0.19 |
| SC ABAS Home Living Scale | 16 | 4.6 (2.6) | 4.8 (2.3) | 21 | 4.7 (2.4) | 6.3 (2.8) | 1.3 | 0.3–2.3 | 0.02 |
| SC Self-Determination Performance | 15 | 23.1 (7.6) | 23.7 (8.3) | 24 | 24.4 (5.9) | 28.5 (7.8) | 3.7 | 0.2–7.3 | 0.04 |
| SC Self-Determination Importance | 15 | 44.3 (6.9) | 43.3 (8.6) | 24 | 40.9 (8.3) | 41.6 (8.1) | 1.6 | −2.7–6.0 | 0.44 |
| PT Coping Self-Efficacy Composite | 14 | 128.4 (48.1) | 131.2 (49.9) | 22 | 144.0 (42.1) | 158.3 (38.8) | 16.3 | −5.4–38.0 | 0.14 |
| PT CSES Problem-Focused Coping | 15 | 29.9 (12.3) | 31.8 (12.3) | 22 | 32.8 (11.9) | 35.8 (8.8) | 1.7 | −5.5–8.9 | 0.63 |
| PT CSES Stop Unpleasant Emotions &. Thoughts | 14 | 18.1 (8.2) | 18.3 (9.1) | 21 | 23.3 (8.4) | 22.4 (7.6) | 0.5 | −4.0–5.0 | 0.83 |
| PT CSES Get Support from Friends & Family | 14 | 14.9 (7) | 13.7 (7.1) | 21 | 16.9 (5.5) | 19.1 (5.5) | 3.6 | 0.7–6.5 | 0.02 |
| PT ASEBA Anxiety Problems | 12 | 59.1 (7.7) | 57.6 (6.8) | 22 | 56.7 (7.3) | 57.3 (8.6) | 0.7 | −4.4–5.8 | 0.79 |
Note. SC = Social Coach. PT = Participant with ASD. ABAS = Adaptive Behavior Assessment System. GAC = General Adaptive Composite. CSES= Coping Self-Efficacy Scale. SD= Standard Deviation. CI = Confidence Interval. p = p-value.
Intervention
The ACCESS Program curriculum (see Table 2) consisted of 19 1.5-hour weekly lessons, and consisted of two introductory lessons followed by three modules: (1) Stress & Anxiety Coping Skills module that provided lessons on identifying distorted thoughts (i.e., thinking traps) and physical feelings associated with stress, anxiety and other emotions, the CBT cognitive model, and cognitive restructuring tools, (2) Self-Determination Skills module that contained lessons on how to initiate, set goals, plan, organize, and self-advocate, and (3) Adaptive & Social Skills module that comprised psychoeducation on the development and importance of friendships and social rules of the workplace. We utilized several adaptations recommended by Kerns et al. (2016) to enhance the delivery of CBT to young adults with ASD, including general adaptations (e.g., work as a team with caregivers, instill structure, use interactive, multimodal teaching methods and concrete activities to ground abstract concepts), psychoeducation (e.g., on ASD and anxiety, normalize symptoms and instill hope), cognitive restructuring, and behavioral activation (integrate social skills training and teach problem-solving strategies). The lessons followed the same structure each week: review of the previous week’s topic and homework, presentation and group discussion on the current session-specific topic, co-facilitator role-plays to demonstrate skills, and small group activities to enhance practical understanding and generalization of skills.
Table 2.
ACCESS Curriculum
| Module | Lesson Topic | Lesson Content |
|---|---|---|
| Introduction and Core Skills for Group Work |
|
|
|
|
|
| Stress and Anxiety Coping Skills |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Self-Determination Skills |
|
|
|
|
|
|
|
|
| Adaptive and Social Skills |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The Social Coach group covered the same session-specific topics as the Participant group but were also given psychoeducation on how to facilitate the Participant’s use and generalization of skills and concepts learned in group. The Social Coaches completed weekly homework assignments (i.e., “life practice”) alongside the Participants with ASD to reinforce skill-building and promote a more positive and equitable relationship. In conjunction with this curriculum, Participants in the treatment group were required to participate in a structured vocational activity (paid or volunteer) of their choice, outside of the group, that was a commitment of at least 3 hours a week. The Social Coach leader, with expertise in job coaching, consulted with Participants who did not yet have a job to help them identify vocational activity placements.
The supervisor for the ACCESS Program was a licensed psychologist who had developed and directed the UC Davis MIND Institute’s Social Skills Training Program. The Participant Group leader had a PhD in psychology, 10 years of experience working with children, youth and adults with ASD, previously co-facilitated a teen social skills group at the MIND Institute, and was completing postdoctoral clinical training hours in her role as the Participant Group leader. The Social Coach Group leader had a bachelor of social work and over 25 years of experience working with people with developmental disabilities in the areas of supported living and employment, and was serving as the Transition Specialist for the UC Davis UCEDD. The co-facilitators had prior experience working with youth and adults with ASD and advanced degrees (i.e., BS, MS, PhD, and/or MD). The supervisor met weekly with the Participant Group leader and the Social Coach Group leader to provide supervision. Further, the Participant Group leader and the Social Coach Group leader together provided group supervision to the co-facilitators.
Fidelity and Acceptability
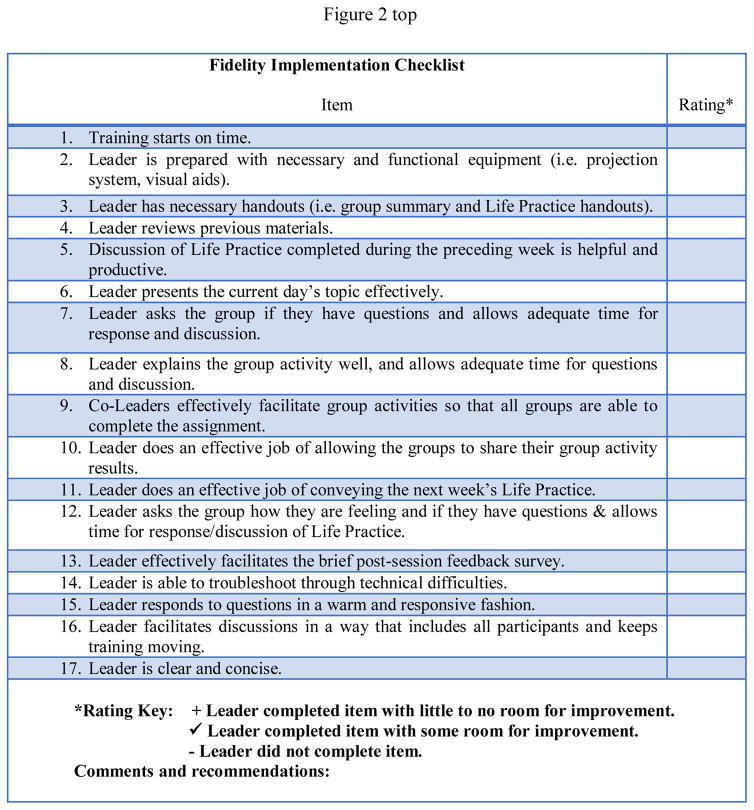
To ensure rigor of the intervention study, fidelity of delivery of the ACCESS Program was monitored by the supervisor of the study through weekly supervision meetings with the two leaders of the groups, and through fidelity ratings (see Fig. 2) based on observations of the Tuesday or Wednesday night Participant and Social Coach treatment groups. The Fidelity Checklist assessed implementation of the instructional sequence and program content. The checklist consisted of 17 items rated from 0–3; 0 – leader did not complete item, 1 – leader completed item with some room for improvement, 2 – leader completed item with little to no room for improvement. The fidelity checklist was also completed at the end of each session by the Participant Group leader, Social Coach Group leader, and co-facilitators. High fidelity of delivery was demonstrated in both the Tuesday and Wednesday groups of Participants and Social Coaches per curriculum module (see Table 3).
Fig. 2.
Fidelity Implementation Checklist
Table 3.
Treatment Fidelity Ratings by Module for Participants and Social Coaches
| Module | Treatment Group | |||
|---|---|---|---|---|
|
| ||||
| Participants | Social Coaches | |||
|
|
|
|||
| Tuesday | Wednesday | Tuesday | Wednesday | |
| Stress & Anxiety Coping Skills | 93.08% | 97.09% | 97.24% | 96.54% |
| Self-Determination Skills | 95.61% | 99.47% | 93.21% | 95.63% |
| Adaptive & Social Skills | 87.25% | 91.08% | 93.08% | 93.85% |
| Modules Combined | 91.98% | 95.88% | 94.51% | 95.34% |
Note. Tuesday = Group that met on Tuesdays. Wednesday = Group that met on Wednesdays
Attendance and acceptability measures were collected only from Participants and Social Coaches in the Treatment Group. Attendance was high for both Participants (average 93.7%) and their Social Coaches (average 92.8%), and no one was absent for more than three sessions. To measure acceptability, the research team developed the Satisfaction Survey, which was completed by Participants and Social Coaches at the end of each session. The survey consisted of a 7-point Likert scale with three anchor points, 0 (not at all true), 3 (somewhat true), and 6 (very true). They were asked to rate the following statements: “Today I enjoyed group very much”, “Today the activities we did were interesting”, and “Today what I learned in group will help me”. It also allowed them to provide comments. Based on the Satisfaction Survey of the Treatment Group, Participants and Social Coaches indicated that they perceived the program to be between “somewhat” and “very” helpful, interesting, and enjoyable per curriculum module (see Table 4). To ensure highest quality of data entry for the outcome measures, double data entry with monitoring by supervisors was established.
Table 4.
Participant and Social Coach Acceptability Mean Ratings by Module
| Module | Treatment Group | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Participants | Social Coaches | |||||
|
|
|
|||||
| Mean Ratings | SD | N | Mean Ratings | SD | N | |
| Stress & Anxiety Coping Skills | 4.28 | 1.29 | 25 | 4.88 | 0.99 | 24 |
| Self-Determination Skills | 4.12 | 1.38 | 25 | 4.69 | 1.02 | 24 |
| Adaptive & Social Skills | 4.12 | 1.45 | 25 | 4.84 | 0.98 | 24 |
| Modules Combined | 4.17 | 1.35 | 25 | 4.80 | 1.00 | 24 |
Outcome measures
Informant-report measures
Social and adaptive functioning measure
Adaptive Behavior Assessment System – Adult Form, Third Edition (ABAS-3) (Harrison and Oakland 2015) is an informant report providing comprehensive assessment of adaptive functioning in individuals with developmental delays, including ASD. The ABAS-3 includes the norm-referenced General Adaptive Composite (GAC), which we used as the primary outcome, and three Composite scales (Social, Conceptual, Practical), which we used as secondary outcome measures. The Social composite score measures performance across the Social Skill and Leisure areas. The Conceptual composite score assesses performance across the Self-Direction, Communication, and Functional Academics areas. The Practical composite score summarizes performance across the Home Living, Self-Care, Community Use, and Health and Safety skill areas. Informants report how frequently the individual performs each activity on a 4-point scale. Internal Consistency was high for the ABAS GAC (Cronbach’s alpha = .97) and the Conceptual, Social, Practical domains (Cronbach’s alpha = .91 – .98), and good for the 10 individual skill areas (Cronbach’s alpha =.80 – .97) (Harrison and Oakland 2015).
Self-determination measure
Seven Component Self-Determination Skills Survey (Carter et al. 2013b) is an informant report that has been used to measure self-determination skills and capacities of young adults with ASD and measures two domains; Performance and Importance. The Performance scale served as a primary outcome and assesses how well the Participant demonstrates 7 critical self-determination skills: choice-making skills, decision-making skills, goal-setting skills, problem-solving skills, self-advocacy/leadership skills, self-awareness/self-knowledge, and self-management/self-regulation skills. The Importance scale measures how important the informant believes it is for the Participant to have these skills. Both domains use a 3-point Likert scale. In a large-scale study on self-determination in students with ASD and ID, Carter et al. (2013a) reported good internal consistency for the Importance scale (Cronbach’s alpha = .80) and the Performance scale (Cronbach’s alpha = .80).
Self-report measures
Coping self-efficacy measure
Coping Self-Efficacy Scale (CSES) (Chesney et al. 2006) is a 26-item self-report measure of one’s own perceived ability to cope effectively with life challenges. It has been used as an outcome measure in intervention research (Barroso et al. 2014), and was included as a primary outcome. Participants are asked, “When things aren’t going well for you, or when you’re having problems, how confident or certain are you that you can do the following:” They rate on an 11-point scale the extent to which they believe they could perform certain behaviors important to adaptive coping. Anchor points on the scale are 0 (‘cannot do at all’), 5 (‘moderately certain can do’) and 10 (‘certain can do’). The composite CSES score is generated by summing the item ratings (Cronbach’s alpha =.95). The measure includes three subscales, use problem-focused coping (6 items, alpha=.91), stop unpleasant emotions and thoughts (4 items, alpha=.91), and get support from friends and family (3 items, alpha=.80).
Anxiety measure
ASEBA Adult Self-Report (ASR) (Achenbach and Rescorla 2003) is a standardized self-report completed by the Participant that contains the DSM-oriented scale Anxiety Problems. For the DSM-oriented scales, a score between 65–69 is considered in the borderline range and a score of 70 or higher is considered in the clinical range. The Anxiety Problems scale was used as the anxiety outcome measure, and is comprised of age-appropriate items identified by the experts as being very consistent with DSM-5 criteria for Generalized Anxiety Disorder, Separation Anxiety Disorder, Social Anxiety Disorder, and Specific Phobia. Reliability for most scales ranges from moderate to high (coefficient alpha’s > 70;) (Achenbach and Rescorla 2003).
Statistical Analysis
Preliminary analyses revealed that IQ was significantly correlated with outcome measures, therefore, we included IQ as a covariate in primary and secondary analyses. Further, exploratory analyses indicated that changes in medication and changes in individual therapy had minimal impact on outcome measures, but are reported on below. For the primary and secondary analyses, we tested the hypothesis of greater improvement in outcome variable scores between baseline and post-treatment for the Treatment group versus the Waitlist Control group, employing analysis of covariance (ANCOVA) on the change in outcome variables from baseline to post-treatment, controlling for IQ. Given the preliminary nature of the study, “as treated” analysis was used to explore treatment efficacy by analyzing Participants according to the condition they received (one Participant did not adhere to condition assigned) and who completed the trial (three Participants did not complete the trial). Missing data was accounted for by using baseline-observation-carried-forward (BOCF), a conservative method in which the pre-treatment baseline observation is treated as the final response. Due to the specific hypotheses tested and global composite scores used per hypothesis, no adjustment of the significance level was required (Maurer et al. 1995). SAS version 9.4 (SAS Institute Inc 2013) was used for all descriptive analyses and primary analyses.
Results
Primary outcomes
As hypothesized, Social Coaches reported significant improvements in Participants’ global adaptive functioning after receiving the intervention, such that mean changes in ABAS GAC scores was 4.1 (95% CI: 0.2–8.0) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.04; see Table 5). Participants with higher IQ showed greater improvement in ABAS GAC scores at post-treatment (p = .04). Social Coaches also reported significant mean changes in Self-Determination Performance scores which were 3.7 (95% CI: 0.2–7.3) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.04). Participants with higher IQ showed greater increases in Self-Determination Performance post-treatment (p = .02). There was no significant group effect for change in Self-Determination Importance scores, indicating that across groups at baseline and post-treatment Social Coaches consistently rated that it was highly important for their sons and daughters with ASD to have self-determination. Counter to predictions, there was no significant group difference between baseline and post-treatment in Participant self-reported ASR Anxiety Problems or Composite Coping Self-Efficacy Scale.
Secondary outcomes
Social Coaches reported significant improvements in Participants’ conceptual adaptive functioning after receiving the intervention, such that mean changes in ABAS Conceptual Composite scores was 4.1 (95% CI: 0.1–8.3) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.04; see Table 5). Participants with higher IQ showed greater improvement in Conceptual Composite scores at post-treatment (p = .03). Social Coaches reported trend-level increases in Participants’ social adaptive functioning post intervention, such that mean changes in ABAS Social Composite scores was 3.3 (95% CI: -0.6–7.2) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.09). There was no significant group effect for change in ABAS Practical Composite scores, but mean changes in the Home Living Skills subscale scores was 1.3 (95% CI: 0.3–2.3) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.02). Participants with higher IQ showed greater improvement in Home Living Skills post-treatment (p = .02). Participants self-reported a significantly higher belief in their ability to cope with stress by seeking social support from friends and family, such that mean changes in CSES “Get support from friends and family” scale scores was 3.6 (95% CI: 0.7–6.5) higher in the Treatment compared with Waitlist Control group after controlling for Participant IQ (p=0.02).
Changes in Therapy and Medication
Regarding therapeutic interventions, during the course of the study 2 (8.0%) Participants in Treatment Group discontinued receiving individual therapy and 2 (8.0%) switched therapists, while 1 (6.3%) Participant in Control Group discontinued individual therapy. Changes in therapy had no statistically significant effect on outcome variables. With respect to psychiatric and sleep medications, during the study 4 (16%) Participants in Treatment Group started a new medication or increased their dose and 1 (4.0%) discontinued medication, while 4 (25.0%) Participants in Control Group started or increased a medication. The only effect due to changes in psychiatric and sleep medications on outcome variables was found for the subscale ABAS Home Living (p=.03), such that Participants with more changes in psychiatric medication showed greater improvement in ABAS Home Living at post-treatment (p = .03).
Discussion
The current study begins to address the urgent need for effective interventions that facilitate the transition to adulthood in individuals with ASD. We implemented a RCT research design to examine the ACCESS Program, a novel integrative therapy to increase the acquisition of targeted skills (i.e., adaptive skills, social skills, self-determination skills) and coping self-efficacy, which are known to support adult functioning. The results of the RCT provided support for the acceptability and efficacy of the intervention. The group leaders delivered the program with a high degree of fidelity, and consumers had a high rate of attendance and reported that the treatment was helpful and interesting. Consistent with our predictions, based on Social Coach report, Participants in Treatment compared to the Waitlist Control group demonstrated significant improvements in the primary outcome measures of global adaptive functioning and self-determination performance. On secondary outcome measures of adaptive functioning, Social Coaches reported significant improvements in the Conceptual composite, and the Home Living Skills subscale of the Practical composite, as well as trend-level increases in Participants’ social adaptive functioning, for the Treatment compared to Waitlist Control Group post intervention. Counter to our predictions, individuals with ASD did not self-report greater improvements post-treatment in anxiety or composite stress coping self-efficacy in the Treatment group relative to Waitlist Control group. However, Participants in the Treatment compared to Waitlist Control group did report significant increases in stress coping self-efficacy related to accessing support from friends and family. In the current study, close to 75% of the young adults with ASD lived with their caregivers, compared to the historic high of 36% in 2013 of young adults in the general US population (Dettling and Hsu 2014), suggesting there is a considerable lack of autonomy in the ASD population. Thus, it is noteworthy that after receiving the intervention, Participants demonstrated enhanced self-determination (e.g., goal-setting, planning, initiation, self-advocacy), social and conceptual adaptive functioning (e.g., communication, self-direction), and adaptive home living skills (e.g., cleaning, property maintenance, food preparation, chores). The fact that Participants reported a stronger belief in their ability to access social supports in times of stress, not only from family but friends, may represent another shift toward increased autonomy after treatment.
The lack of change in anxiety levels self-reported by our Participants with ASD post-intervention was counter to our prediction. In our study, only a few participants had a diagnosis of anxiety (diagnosed by an outside provider), suggesting the possibility that participants in fact had subclinical levels of anxiety. Therefore, outcome measures of stress rather than of clinical levels of anxiety may have served as more appropriate measures of treatment effects for our study. However, our non-significant findings of change in anxiety levels are consistent with results from a group CBT anxiety treatment study on children with a dual diagnosis of ASD and anxiety (Reaven et al. 2009). Theories have been developed to account for these null findings. One theory postulates that anxiety questionnaires are not valid for the ASD population, as they were standardized on the general population and lack the sensitivity and specificity needed to detect clinical levels of anxiety in ASD (Kerns et al. 2015). A second theory proposes that people with ASD underreport their symptoms pre-treatment due to lack of self-awareness regarding their anxiety symptoms, resulting in reduced effect sizes. A third theory maintains that due to their poor ability to generalize learned skills, individuals with ASD may need extensive practice before making noticeable gains from an intervention (Wilczynski et al. 2007). Consistent with the latter two theories, a young adult with ASD stated during the post-treatment focus group, “I learned… how to address problems like at the time… and remain calm and function well… It will take some more practice, but at least I was able to be aware of when I was in a thinking trap”. Regarding the first theory, it is not clear whether the chosen measures used in the study for the adults with ASD were inappropriate given that the research findings on the validity of self-report measures of anxiety for the ASD population are equivocal. Some studies find that self-report ratings made by youth with ASD are equally accurate to parent-report ratings of anxiety symptoms (Ozsivadjian et al. 2014), other studies reveal that children with ASD are more accurate at reporting on their anxiety because their ratings correlate better with their levels of the stress hormone cortisol compared to parent-report ratings (Bitsika et al. 2015), and still other investigations find that self-report relative to parent-report ratings less accurately reflect anxiety symptoms (May et al. 2015). Given these inconsistent findings, further study of measurement validity in ASD is crucial, as valid measures of internalizing symptoms would enable researchers to more accurately assess the treatment effects of intervention studies for ASD.
Although the current study implemented a rigorous RCT design, limitations were present. A primary limitation was low statistical power to detect changes in outcomes, as the sample size was relatively small and the response rate for self-report questionnaires was reduced due to Participants not returning them. We had allowed Participants to complete some self-report measures at home because the assessment sessions in the laboratory were already lengthy due to the semi-structured interviews and structured assessments conducted by experimenters (e.g., ADOS, WASI). However, to enhance statistical power, future studies should allocate adequate time for Participants to complete self-report questionnaires in the laboratory and the sample size should be increased. Regarding a second limitation, although Social Coaches provided informant reports on the Participants, they were not blind to the treatment and were likely invested in the change in outcomes, which may have introduced a bias. To address rater bias, future investigations could utilize objective measures, such as performance-based measures (Patterson et al. 2001) or measures rated by clinical observation or blind informants observing Participants in different settings (e.g., their structured vocational activities, in the community, or home). One issue with many performance-based measures is that Participants would have been exposed to the task pre-treatment, so improvements post-treatment might be biased by practice effects. Future investigations should also consider implementing a crossover experimental design, where a placebo control group and active treatment group switch halfway through the study. This design is similar to the waitlist control design we used in that it ethically provides all Participants with the active treatment, but the crossover design has the added benefit of having blinded conditions, which likely reduces rater bias in reporting. A third limitation is that we did not have long-term follow-up data collection, and for this population significant gains may be most evident after an extended period post-treatment. Future research should include a larger-scale RCT of ACCESS with long-term follow-ups, which could enable us to validate the efficacy of the treatment and to examine mediators that may serve as active ingredients or targets to be engaged in the intervention. Further, a study design that allocates Participants to only one treatment module (e.g., Stress & Anxiety Coping Skills, Self-determination Skills, or Adaptive & Social Skills) would allow researchers to examine the efficacy of modules and contribution of individual modules to specific outcomes effects, which may provide insights for a personalized medicine approach (Kasari 2015). Finally, it is essential for future intervention studies to develop modified protocols to enhance adaptive functioning in adults with co-occurring ASD and intellectual disability.
In conclusion, the study had innovative features and provided evidence supporting the acceptability and efficacy of the ACCESS Program. Speaking to innovation, the ACCESS Program to our knowledge is the first comprehensive, yet brief, group intervention tailored for young adults with ASD to enhance social and adult adaptive skills, stress coping self-efficacy, and self-determination. Another innovation of the study was the implementation of a participatory design model for community health, incorporating stakeholder input in the design for ACCESS, which may have contributed to the good satisfaction ratings by Participants and Social Coaches in ACCESS. Post-treatment we also held stakeholder focus groups, and both Participants with ASD and their Social Coaches emphasized that visual models were particularly helpful in clarifying abstract concepts, the group format provided a sense of belonging and validation, interactive small group activities were essential for building social skills and friendships amongst group members, and that Participants and Social Coaches developed a greater sense of equitability in their relationships and engaged in deeper conversations because the lessons and homework gave them a shared language and common issues to discuss. One of the primary themes that emerged during the focus groups with the young adults with ASD was the need for repetition of material in order to practice and consolidate session topics. Based upon feedback from Participants, the topics covered in the ACCESS curriculum appeared to be relevant to individuals across the wide age range of 18–38 years. Further, some Participants recommended that the curriculum be extended to cover more adaptive skills related to independent living, dating, romantic relationships, and employment. A practical and cost-effective way to address the range of needs and interests present in our groups may be to implement a modularized intervention design which allows Participants to select treatment modules most relevant to their needs, consistent with a personalized medicine approach (Kasari 2015).
Acknowledgments
This work was supported by a Behavioral Health Center of Excellence grant and a National Institute Mental Health R01 grant (1R01MH106518) awarded to Marjorie Solomon. We would like to thank the young adults and families who generously participated, and the co-facilitators and research assistants for their invaluable help.
Funding: This study was funded by a Behavioral Health Center of Excellence grant and a National Institute Mental Health R01 grant (1R01MH106518).
Footnotes
Compliance with Ethical Standards
Disclosure of potential conflicts of interest: The authors declare that they have no conflict of interest.
Research involving Human Participants: All procedures performed on human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- A.P.A. Diagnostic and statistical manual of mental disorders - Fifth edition. Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- Achenbach TM, Rescorla L. Manual for the ASEBA Adult Forms & Profiles. Burlington VT: University of Vermont Research Center for Children, Youth and Families; 2003. [Google Scholar]
- Anderson KA, Shattuck PT, Cooper BP, Roux AM, Wagner M. Prevalence and correlates of postsecondary residential status among young adults with an autism spectrum disorder. Autism. 2014;18(5):562–570. doi: 10.1177/1362361313481860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association, A. P. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [DOI] [PubMed] [Google Scholar]
- Baldwin S, Costley D, Warren A. Employment activities and experiences of adults with high-functioning autism and Asperger’s Disorder. J Autism Dev Disord. 2014;44(10):2440–2449. doi: 10.1007/s10803-014-2112-z. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy. In. VS Ramachaudran. Encyclopedia of human behavior. 1994;4:71–81. [Google Scholar]
- Barroso J, Relf MV, Williams MS, Arscott J, Moore ED, Caiola C, et al. A randomized controlled trial of the efficacy of a stigma reduction intervention for HIV-infected women in the Deep South. AIDS patient care and STDs. 2014;28(9):489–498. doi: 10.1089/apc.2014.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, Minshew NJ, Eack SM. The relationship between stress and social functioning in adults with autism spectrum disorder and without intellectual disability. Autism Res. 2015;8(2):164–173. doi: 10.1002/aur.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43(3):687–694. doi: 10.1007/s10803-012-1615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsika V, Sharpley CF, Andronicos NM, Agnew LL. Agreement Between Self- vs Parent-Ratings of General Anxiety Disorder Symptoms and Salivary Cortisol in Boys with an ASD. [journal article] Journal of Developmental and Physical Disabilities. 2015;27(4):467–477. doi: 10.1007/s10882-015-9431-7. [DOI] [Google Scholar]
- Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. American Journal of Psychiatry. 2012;169(7):710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- Bracht N, Tsouros A. Principles and strategies of effective community participation. Health promotion international. 1990;5(3):199–208. [Google Scholar]
- Bruggink A, Huisman S, Vuijk R, Kraaij V, Garnefski N. Cognitive emotion regulation, anxiety and depression in adults with autism spectrum disorder. Research in Autism Spectrum Disorders. 2016;22:34–44. [Google Scholar]
- Cappadocia MC, Weiss JA. Review of social skills training groups for youth with Asperger syndrome and high functioning autism. Research in Autism Spectrum Disorders. 2011;5(1):70–78. [Google Scholar]
- Cardaciotto L, Herbert AD. Cognitive behavior therapy for social anxiety disorder in the context of Asperger’s syndrome: A single-subject report. Cognitive and Behavioral Practice. 2004;11(1):75–81. doi: 10.1016/S1077-7229(04)80009-9. [DOI] [Google Scholar]
- Carter EW, Lane K, Cooney M, Weir K, Moss C, Machalicek W. Parent assessments of self-determination importance and performance for students with autism or intellectual disability. Am J Intellect Dev Disabil. 2013a;118(1):16–31. doi: 10.1352/1944-7558-118.1.16. [DOI] [PubMed] [Google Scholar]
- Carter EW, Lane KL, Cooney M, Weir K, Moss CK, Machalicek W. Self-Determination among Transition-Age Youth with Autism or Intellectual Disability: Parent Perspectives. Research and Practice for Persons with Severe Disabilities. 2013b;38(3):129–138. doi: 10.1177/154079691303800301. [DOI] [Google Scholar]
- Chalfant AM, Rapee R, Carroll L. Treating anxiety disorders in children with high functioning autism spectrum disorders: a controlled trial. J Autism Dev Disord. 2007;37(10):1842–1857. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: Results from a randomized clinical trial testing a group-based intervention. Psychosomatic medicine. 2003;65(6):1038–1046. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. British journal of health psychology. 2006;11(3):421–437. doi: 10.1348/135910705X53155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou Y-C, Wehmeyer ML, Palmer SB, Lee J. Comparisons of Self-Determination Among Students With Autism, Intellectual Disability, and Learning Disabilities A Multivariate Analysis. Focus on Autism and Other Developmental Disabilities. 2016 1088357615625059. [Google Scholar]
- Dettling LJ, Hsu JW. FEDS Working Paper No. 2014–80. 2014. Returning to the nest: Debt and parental co-residence among young adults. [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Res. 2009;2(2):109–118. doi: 10.1002/aur.69. [DOI] [PubMed] [Google Scholar]
- Field S, Martin J, Miller R, Ward M, Wehmeyer M. Self-determination for persons with disabilities: A position statement of me division on career development and transition. Career Development for Exceptional Individuals. 1998;21(2):113–128. [Google Scholar]
- Fowler CH, Konrad M, Walker AR, Test DW, Wood WM. Self-determination interventions’ effects on the academic performance of students with developmental disabilities. Education and training in developmental disabilities. 2007:270–285. [Google Scholar]
- Freitag CM, Jensen K, Elsuni L, Sachse M, Herpertz-Dahlmann B, Schulte-Ruther M, et al. Group-based cognitive behavioural psychotherapy for children and adolescents with ASD: the randomized, multicentre, controlled SOSTA-net trial. J Child Psychol Psychiatry. 2016;57(5):596–605. doi: 10.1111/jcpp.12509. [DOI] [PubMed] [Google Scholar]
- Gantman A, Kapp SK, Orenski K, Laugeson EA. Social skills training for young adults with high-functioning autism spectrum disorders: a randomized controlled pilot study. J Autism Dev Disord. 2012;42(6):1094–1103. doi: 10.1007/s10803-011-1350-6. [DOI] [PubMed] [Google Scholar]
- García-Villamisar D, Dattilo J. Effects of a leisure programme on quality of life and stress of individuals with ASD. Journal of Intellectual Disability Research. 2010;54(7):611–619. doi: 10.1111/j.1365-2788.2010.01289.x. [DOI] [PubMed] [Google Scholar]
- Ghaziuddin M, Weidmer-Mikhail E, Ghaziuddin N. Comorbidity of Asperger syndrome: a preliminary report. J Intellect Disabil Res. 1998;42(Pt 4):279–283. doi: 10.1111/j.1365-2788.1998.tb01647.x. [DOI] [PubMed] [Google Scholar]
- Goldberg RJ, Higgins EL, Raskind MH, Herman KL. Predictors of Success in Individuals with Learning Disabilities: A Qualitative Analysis of a 20-Year Longitudinal Study. Learning Disabilities Research & Practice. 2003;18(4):222–236. [Google Scholar]
- Harrison P, Oakland T. Adaptive Behavior Assessment System. 3. Torrance, CA: Western Psychological Services; 2015. [Google Scholar]
- Hesselmark E, Plenty S, Bejerot S. Group cognitive behavioural therapy and group recreational activity for adults with autism spectrum disorders: a preliminary randomized controlled trial. Autism. 2014;18(6):672–683. doi: 10.1177/1362361313493681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier A, Fish T, Cloppert P, Beversdorf DQ. Outcomes of a social and vocational skills support group for adolescents and young adults on the autism spectrum. Focus on Autism and Other Developmental Disabilities. 2007;22(2):107–115. [Google Scholar]
- Hirvikoski T, Blomqvist M. High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism. 2015;19(6):752–757. doi: 10.1177/1362361314543530. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive therapy and research. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009;9(1):35. doi: 10.1186/1471-244X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive language disorder--a follow-up comparison in early adult life. II: Social, behavioural, and psychiatric outcomes. J Child Psychol Psychiatry. 2000;41(5):561–578. doi: 10.1111/1469-7610.00643. [DOI] [PubMed] [Google Scholar]
- Howlin P, Yates P. The potential effectiveness of social skills groups for adults with autism. Autism. 1999;3(3):299–307. [Google Scholar]
- Jacobson JW, Ackerman LJ. Differences in adaptive functioning among people with autism or mental retardation. J Autism Dev Disord. 1990;20(2):205–219. doi: 10.1007/BF02284719. [DOI] [PubMed] [Google Scholar]
- Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: a comparative study. Journal of autism and developmental disorders. 2013;43(6):1314–1325. doi: 10.1007/s10803-012-1679-5. [DOI] [PubMed] [Google Scholar]
- Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, Saulnier CA. The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. J Autism Dev Disord. 2011;41(8):1007–1018. doi: 10.1007/s10803-010-1126-4. [DOI] [PubMed] [Google Scholar]
- Kasari C. Update on behavioral interventions for autism and developmental disabilities. Curr Opin Neurol. 2015;28(2):124–129. doi: 10.1097/WCO.0000000000000185. [DOI] [PubMed] [Google Scholar]
- Keehn RHM, Lincoln AJ, Brown MZ, Chavira DA. The Coping Cat Program for Children with Anxiety and Autism Spectrum Disorder: A Pilot Randomized Controlled Trial. Journal of autism and developmental disorders. 2013;43(1):57–67. doi: 10.1007/s10803-012-1541-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenworthy L, Anthony LG, Naiman DQ, Cannon L, Wills MC, Luong-Tran C, et al. Randomized controlled effectiveness trial of executive function intervention for children on the autism spectrum. J Child Psychol Psychiatry. 2014;55(4):374–383. doi: 10.1111/jcpp.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns CM, Maddox BB, Kendall PC, Rump K, Berry L, Schultz RT, et al. Brief measures of anxiety in non-treatment-seeking youth with autism spectrum disorder. Autism. 2015;19(8):969–979. doi: 10.1177/1362361314558465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns CM, Roux AM, Connell JE, Shattuck PT. Adapting Cognitive Behavioral Techniques to Address Anxiety and Depression in Cognitively Able Emerging Adults on the Autism Spectrum. Cognitive and Behavioral Practice. 2016;23(3):329–340. [Google Scholar]
- Konrad M, Fowler CH, Walker AR, Test DW, Wood WM. Effects of self-determination interventions on the academic skills of students with learning disabilities. Learning Disability Quarterly. 2007;30(2):89–113. [Google Scholar]
- Kraper CK, Kenworthy L, Popal H, Martin A, Wallace GL. The Gap Between Adaptive Behavior and Intelligence in Autism Persists into Young Adulthood and is Linked to Psychiatric Comorbidities. Journal of autism and developmental disorders. 2017 doi: 10.1007/s10803-017-3213-2. doi: https://doi.org/10.1007/s10803-017-3213-2. [DOI] [PubMed]
- Lachapelle Y, Wehmeyer ML, Haelewyck MC, Courbois Y, Keith KD, Schalock R, et al. The relationship between quality of life and self-determination: an international study. Journal of Intellectual Disability Research. 2005;49(10):740–744. doi: 10.1111/j.1365-2788.2005.00743.x. [DOI] [PubMed] [Google Scholar]
- Lang R, Regester A, Lauderdale S, Ashbaugh K, Haring A. Treatment of anxiety in autism spectrum disorders using cognitive behaviour therapy: A systematic review. Developmental Neurorehabilitation. 2010;13(1):53–63. doi: 10.3109/17518420903236288. [DOI] [PubMed] [Google Scholar]
- Laugeson EA, Gantman A, Kapp SK, Orenski K, Ellingsen R. A Randomized Controlled Trial to Improve Social Skills in Young Adults with Autism Spectrum Disorder: The UCLA PEERS Program. J Autism Dev Disord. 2015;45(12):3978–3989. doi: 10.1007/s10803-015-2504-8. [DOI] [PubMed] [Google Scholar]
- Lee Y, Wehmeyer ML, Palmer SB, Williams-Diehm K, Davies DK, Stock SE. The effect of student-directed transition planning with a computer-based reading support program on the self-determination of students with disabilities. The Journal of Special Education. 2011;45(2):104–117. [Google Scholar]
- Lerner MD, White SW, McPartland JC. Mechanisms of change in psychosocial interventions for autism spectrum disorders. Dialogues Clin Neurosci. 2012;14(3):307–318. doi: 10.31887/DCNS.2012.14.3/mlerner. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy A, Perry A. Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders. 2011;5(4):1271–1282. doi: 10.1016/j.rasd.2011.01.023. [DOI] [Google Scholar]
- Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, et al. Predictors and correlates of adaptive functioning in children with developmental disorders. J Autism Dev Disord. 2001;31(2):219–230. doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule–2nd edition (ADOS-2) Los Angeles, CA: Western Psychological Corporation; 2012. [Google Scholar]
- Lugnegård T, Hallerbäck MU, Gillberg C. Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities. 2011;32(5):1910–1917. doi: 10.1016/j.ridd.2011.03.025. [DOI] [PubMed] [Google Scholar]
- Maurer W, Hothorn L, Lehmacher W. Multiple comparisons in drug clinical trials and preclinical assays: a-priori ordered hypotheses. Biometrie in der chemisch-pharmazeutischen Industrie. 1995;6:3–18. [Google Scholar]
- May T, Cornish K, Rinehart N. Parent-child agreement using the spence children’s anxiety scale and a thermometer in children with autism spectrum disorder. Autism research and treatment. 2015;2015 doi: 10.1155/2015/315495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Pascaris A. Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial. Schizophrenia bulletin. 2005;31(4):898–909. doi: 10.1093/schbul/sbi037. [DOI] [PubMed] [Google Scholar]
- Newman L, Wagner M, Cameto R, Knokey A-M, Shaver D. NCSER 2010–3008. National Center for Special Education Research; 2010. Comparisons across Time of the Outcomes of Youth with Disabilities up to 4 Years after High School. A Report of Findings from the National Longitudinal Transition Study (NLTS) and the National Longitudinal Transition Study-2 (NLTS2) [Google Scholar]
- Nota L, Ferrari L, Soresi S, Wehmeyer M. Self-determination, social abilities and the quality of life of people with intellectual disability. Journal of Intellectual Disability Research. 2007;51(11):850–865. doi: 10.1111/j.1365-2788.2006.00939.x. [DOI] [PubMed] [Google Scholar]
- Ozsivadjian A, Hibberd C, Hollocks MJ. Brief report: the use of self-report measures in young people with autism spectrum disorder to access symptoms of anxiety, depression and negative thoughts. Journal of autism and developmental disorders. 2014;44(4):969–974. doi: 10.1007/s10803-013-1937-1. [DOI] [PubMed] [Google Scholar]
- Pahnke J, Lundgren T, Hursti T, Hirvikoski T. Outcomes of an acceptance and commitment therapy-based skills training group for students with high-functioning autism spectrum disorder: A quasi-experimental pilot study. Autism. 2014;18(8):953–964. doi: 10.1177/1362361313501091. [DOI] [PubMed] [Google Scholar]
- Palmen A, Didden R, Lang R. A systematic review of behavioral intervention research on adaptive skill building in high-functioning young adults with autism spectrum disorder. Research in Autism Spectrum Disorders. 2012;6(2):602–617. [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophrenia bulletin. 2001;27(2):235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach BT, McKibbin C, Goldman S, Bucardo J, Jeste DV. Functional adaptation skills training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophrenia research. 2006;86(1):291–299. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Perry A, Flanagan HE, Dunn Geier J, Freeman NL. Brief report: the Vineland Adaptive Behavior Scales in young children with autism spectrum disorders at different cognitive levels. J Autism Dev Disord. 2009;39(7):1066–1078. doi: 10.1007/s10803-009-0704-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugliese CE, Anthony L, Strang JF, Dudley K, Wallace GL, Kenworthy L. Increasing adaptive behavior skill deficits from childhood to adolescence in autism spectrum disorder: role of executive function. J Autism Dev Disord. 2015;45(6):1579–1587. doi: 10.1007/s10803-014-2309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puleo CM, Kendall PC. Anxiety disorders in typically developing youth: autism spectrum symptoms as a predictor of cognitive-behavioral treatment. J Autism Dev Disord. 2011;41(3):275–286. doi: 10.1007/s10803-010-1047-2. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: a randomized trial. J Child Psychol Psychiatry. 2012;53(4):410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Nichols S, Dasari M, Flanigan E, Hepburn S. Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders a pilot study. Focus on Autism and Other Developmental Disabilities. 2009;24(1):27–37. [Google Scholar]
- Reichow B, Volkmar FR. Social skills interventions for individuals with autism: Evaluation for evidence-based practices within a best evidence synthesis framework. Journal of autism and developmental disorders. 2010;40(2):149–166. doi: 10.1007/s10803-009-0842-0. [DOI] [PubMed] [Google Scholar]
- Roux A, Shattuck P, Rast J, Anderson K. National Autism Indicators Report: Developmental Disability Services and Outcomes in Adulthood. Philadelphia, PA: 2017. [Google Scholar]
- Roux A, Shattuck P, Rast J, Rava J, Anderson K. National Autism Indicators Report: transition into young adulthood. Philadelphia, PA: Life Course Outcomes Research Progra, AJ Drexel Autism Institute, Drexel University; 2015. [Google Scholar]
- Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, et al. Cognitive behavior therapy for comorbid obsessive-compulsive disorder in high-functioning autism spectrum disorders: a randomized controlled trial. Depress Anxiety. 2013;30(8):697–708. doi: 10.1002/da.22053. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. Base SAS® 9.4 Procedures Guide: Statistical Procedures. 2. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post-high school service use among young adults with an autism spectrum disorder. Arch Pediatr Adolesc Med. 2011;165(2):141–146. doi: 10.1001/archpediatrics.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shogren KA, Wehmeyer ML, Palmer SB, Rifenbark GG, Little TD. Relationships between self-determination and postschool outcomes for youth with disabilities. The Journal of Special Education. 2015;48(4):256–267. [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. J Child Psychol Psychiatry. 2005;46(11):1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Solomon M, Goodlin-Jones BL, Anders TF. A social adjustment enhancement intervention for high functioning autism, Asperger’s syndrome, and pervasive developmental disorder NOS. Journal of autism and developmental disorders. 2004;34(6):649–668. doi: 10.1007/s10803-004-5286-y. [DOI] [PubMed] [Google Scholar]
- Spain D, Blainey SH. Group social skills interventions for adults with high-functioning autism spectrum disorders: A systematic review. Autism. 2015;19(7):874–886. doi: 10.1177/1362361315587659. [DOI] [PubMed] [Google Scholar]
- Storch EA, Arnold EB, Lewin AB, Nadeau JM, Jones AM, De Nadai AS, et al. The Effect of Cognitive-Behavioral Therapy Versus Treatment as Usual for Anxiety in Children With Autism Spectrum Disorders: A Randomized, Controlled Trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(2):132–142. doi: 10.1016/j.jaac.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Tassé MJ, Schalock RL, Balboni G, Hank Bersani J, Borthwick-Duffy SA, Spreat S, et al. The Construct of Adaptive Behavior: Its Conceptualization, Measurement, and Use in the Field of Intellectual Disability. American Journal on Intellectual and Developmental Disabilities. 2012;117(4):291–303. doi: 10.1352/1944-7558-117.4.291. [DOI] [PubMed] [Google Scholar]
- Taylor JL, Mailick MR. A longitudinal examination of 10-year change in vocational and educational activities for adults with autism spectrum disorders. Dev Psychol. 2014;50(3):699–708. doi: 10.1037/a0034297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, McPheeters ML, Sathe NA, Dove D, Veenstra-VanderWeele J, Warren Z. A systematic review of vocational interventions for young adults with autism spectrum disorders. Pediatrics. 2012 doi: 10.1542/peds.2012-0682. peds. 2012–0682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Test DW, Karvonen M, Wood WM, Browder D, Algozzine B. Choosing a Self-Determination Curriculum. TEACHING Exceptional Children. 2000;33(2):48–54. doi: 10.1177/004005990003300207. [DOI] [Google Scholar]
- Turner-Brown LM, Perry TD, Dichter GS, Bodfish JW, Penn DL. Brief report: Feasibility of social cognition and interaction training for adults with high functioning autism. Journal of autism and developmental disorders. 2008;38(9):1777–1784. doi: 10.1007/s10803-008-0545-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D, Zhou X. Wechsler Abbreviated Scale of Intelligence -Second Edition. San Antonio, Texas: Psychological Corporation; 2011. [Google Scholar]
- Wehmeyer M, Palmer SB. Adult outcomes for students with cognitive disabilities three-years after high school: The impact of self-determination. Education and training in developmental disabilities. 2003:131–144. [Google Scholar]
- Wehmeyer M, Schwartz M. Self-determination and positive adult outcomes: A follow-up study of youth with mental retardation or learning disabilities. Exceptional children. 1997;63(2):245–255. [Google Scholar]
- Wehmeyer M, Schwartz M. The relationship between self-determination and quality of life for adults with mental retardation. Education and training in mental retardation and developmental disabilities. 1998:3–12. [Google Scholar]
- Wehmeyer ML. Self-Determination and Individuals with Significant Disabilities: Examining Meanings and Misinterpretations. Journal of the Association for Persons with Severe Handicaps. 1998;23(1):5–16. doi: 10.2511/rpsd.23.1.5. [DOI] [Google Scholar]
- Wei X, Wagner M, Hudson L, Yu JW, Shattuck P. Transition to adulthood: Employment, education, and disengagement in individuals with autism spectrum disorders. Emerging Adulthood. 2015;3(1):37–45. [Google Scholar]
- Weiss JA, Lunsky Y. Group cognitive behaviour therapy for adults with Asperger syndrome and anxiety or mood disorder: a case series. Clin Psychol Psychother. 2010;17(5):438–446. doi: 10.1002/cpp.694. [DOI] [PubMed] [Google Scholar]
- Weston L, Hodgekins J, Langdon PE. Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: A systematic review and meta-analysis. Clin Psychol Rev. 2016;49:41–54. doi: 10.1016/j.cpr.2016.08.001. [DOI] [PubMed] [Google Scholar]
- White SW, Keonig K, Scahill L. Social skills development in children with autism spectrum disorders: A review of the intervention research. Journal of autism and developmental disorders. 2007;37(10):1858–1868. doi: 10.1007/s10803-006-0320-x. [DOI] [PubMed] [Google Scholar]
- White SW, Ollendick T, Albano AM, Oswald D, Johnson C, Southam-Gerow MA, et al. Randomized controlled trial: Multimodal Anxiety and Social Skill Intervention for adolescents with autism spectrum disorder. J Autism Dev Disord. 2013;43(2):382–394. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilczynski SM, Menousek K, Hunter M, Mudgal D. Individualized education programs for youth with autism spectrum disorders. Psychology in the Schools. 2007;44(7):653–666. [Google Scholar]
- Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. J Child Psychol Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalewska A, Migliore A, Butterworth J. Self-determination, social skills, job search, and transportation: Is there a relationship with employment of young adults with autism? Journal of Vocational Rehabilitation. 2016;45(3):225–239. [Google Scholar]