Abstract
There is increasing recognition that adults with autism spectrum disorder (ASD) would benefit from treatment to improve social functioning, a key factor in adults’ overall quality of life. However, the various behavioral components of social functioning (i.e. categories of behaviors underlying social functioning), including social motivation, social anxiety, social cognition, and social skills, have not all been assessed together in any sample of adults with ASD, making it difficult to know the relative levels of impairment in these various categories, the relationships among these categories, or promising targets for treatments. We hypothesized there would be significant correlations among measures within the same category, but fewer correlations of measures between categories, indicating the heterogeneity of impairments in adults with ASD. Twenty-nine adults with ASD without co-occurring intellectual disability completed multiple assessments measuring social motivation, social anxiety, social cognition, and social skills, as well as measures of overall ASD symptom levels and community functioning. Results revealed significant positive correlations among measures within most categories; positive correlations between measures of social motivation and all other categories, except for social cognition; as well as positive cross-domain correlations between measures of anxiety and ASD phenotype; measures of social skills and community functioning; and measures of social skills and ASD phenotype. Further studies are warranted to determine causal relationships among these behavioral categories, across developmental stages. However, the lack of correlations between many categories suggests the potential importance of multidimensional treatments that target the particular components of social functioning most in need of improvement in individuals.
Lay Summary
The goal of this study was to measure behaviors that contribute to social functioning difficulties in adults with ASD, with the ultimate goal of guiding treatment development. We found that motivation to interact with others was significantly related to social anxiety and social skill. Our results suggest that motivation may be important to target in treatment, and that treatments should be tailored to the areas most in need of improvement in each individual.
Keywords: adult ASD, social functioning, motivation, anxiety, cognition, skills, treatment
INTRODUCTION
Impairments in social functioning—the ability to navigate the social world and form and maintain relationships in community settings, including home, school, and work—are among the most critical challenges faced by individuals with autism spectrum disorder (ASD). Social functioning difficulties become particularly problematic in adulthood, when expectations for skillful social functioning increase. Such difficulties contribute to a host of negative and costly outcomes in adults with ASD (Buescher, Cidav, Knapp, & Mandell, 2014; Ganz, 2007; Howlin & Moss, 2012; Howlin, Moss, Savage, & Rutter, 2013; Hurlbutt & Chalmers, 2002; Muller, Schuler, Burton, & Yates, 2003; Shattuck, Narendorf, et al., 2012; Shattuck, Roux, et al., 2012). Although approximately 60,000 adolescents with ASD reach adulthood in the United States every year (https://www.cdc.gov/ncbddd/autism/data.html), very little research has been published on interventions to improve social functioning in adults (Bishop-Fitzpatrick, Minshew, & Eack, 2013; Spain & Blainey, 2015).
A substantial challenge for developing effective interventions is the complexity of social functioning. At least four categories of behavior underlie social functioning, that is, are components of social functioning, any one or more of which may be disrupted in adults with ASD. Specifically, social functioning may be disrupted when an individual:
Lacks sufficient motivation to interact with others (Chevallier, Kohls, Troiani, Brodkin, & Schultz, 2012);
Experiences debilitating social anxiety or social avoidance (Gotham, Brunwasser, & Lord, 2015; Maddox & White, 2015);
Lacks adequate social cognition (e.g., understanding of nonverbal social cues such as facial expression, body language, and tone of voice, and the ability to recognize and take other people’s perspectives) (Kennedy & Adolphs, 2012; Volkmar, 2011); or
Lacks adequate social skills (e.g., ability to initiate and carry on a conversation and make use of nonverbal social communication) (Chevallier, Kohls, et al., 2012; Reichow, Steiner, & Volkmar, 2013).
Moreover, social functioning requires an ability to generalize and apply social cognition and social skills flexibly and appropriately in a variety of community settings in order to develop networks of friends and relationships. Efforts to effectively target treatments to improve social functioning and monitor treatment response in adults with ASD may benefit from an understanding of the behavioral components of social functioning and how these components are interrelated.
Relationships between and among these particular components of social functioning – including relationships among subsets of social motivation, anxiety, social cognition, and social skills – have been reported in studies of children with ASD (Chevallier, Kohls, et al., 2012; Factor, Ryan, Farley, Ollendick, & Scarpa, 2017; Hollocks et al., 2014) as well as adults with various neuropsychiatric disorders, such as negative symptoms of schizophrenia (Ruocco et al., 2014; Sachs, Steger-Wuchse, Kryspin-Exner, Gur, & Katschnig, 2004). However, we do not know of studies that have examined relationships among all four components, particularly in adults with ASD. The relationships among these components are important to assess in adults with ASD because these results may not be the same as those in children with ASD, in part because of changes in social functioning and social skills that occur as part of the natural history of ASD across the lifespan (Billstedt, Gillberg, & Gillberg, 2007; Seltzer, Shattuck, Abbeduto, & Greenberg, 2004). Relationships among these components may also differ in ASD versus other neuropsychiatric disorders.
Over the past 20 years, most studies of adults with ASD have focused on only one or two components of social functioning (Bishop-Fitzpatrick, Mazefsky, Minshew, & Eack, 2015; Chen, Bundy, Cordier, Chien, & Einfeld, 2015; Hillier, Fish, Cloppert, & Beversdorf, 2007; Swain, Scarpa, White, & Laugeson, 2015). We do not know of a study that has measured all four components in the same sample of adults with ASD, making it difficult to gauge relationships among these components. The current study is the first, to our knowledge, to measure all four categories of behavior underlying social functioning in the same cohort of adults with ASD. Below, we provide a brief summary of previously published reports on how each of these categories is affected in adolescents and adults with ASD.
Social Motivation
Social motivation has at least five parts: prioritizing and attending to social stimuli (social orienting), endorsing an interest in interaction (social interest), seeking out social interaction (social approach), taking pleasure in interactions (social liking), and engaging in relationships with others over a sustained period of time (social maintaining) (Chevallier, Kohls, et al., 2012). These behavioral manifestations of social motivation can be distinct from one another. For example, one can have a stated interest or take pleasure in a social situation, but not tend to initiate engagement in social behavior (no social approach). Alternatively, one may engage in social behaviors, but derive little pleasure from interactions (Chevallier, Kohls, et al., 2012). Eye tracking experiments have demonstrated that individuals with ASD, in contrast to typically developing controls, spend less time looking at or orienting to social stimuli (i.e., people, faces, eyes) than non-social stimuli (i.e., background objects) (Chevallier et al., 2015; Klin, Jones, Schultz, Volkmar, & Cohen, 2002; Nakano et al., 2010). Social approach also is reduced in many adults with ASD (Association, 2013; Chevallier et al., 2015).
Social “liking” (i.e., pleasure in interacting) is reduced in both adolescents (Pleasure Scale; (Chevallier, Grezes, Molesworth, Berthoz, & Happe, 2012)) and adults with ASD, on average (Social Anhedonia Scale (SAS); (Carre et al., 2015)). This anhedonia appears to be specific to social rather than non-social situations, and the degree of social anhedonia is positively correlated with ASD severity (Carre et al., 2015). In one data set, more than 50% of adults with ASD report having no particular friends (Howlin et al., 2013), and adults with ASD tend to experience less pleasure in close friendships when compared to typically developing controls (Baron-Cohen & Wheelwright, 2003; Chevallier, Kohls, et al., 2012). Despite the evidence for reduced social motivation in ASD, few validated instruments capture the many behavioral manifestations of social motivation.
Social Anxiety
Some evidence suggests that adults with ASD are more sensitive to stress than adults without ASD, and experience greater perceived stress and interviewer-observed stress than typically developing controls (Bishop-Fitzpatrick et al., 2015). Social anxiety is more commonly observed in individuals with ASD than among the general population (Hillier, Fish, Siegel, & Beversdorf, 2011; Maddox & White, 2015; Roberson-Nay, Strong, Nay, Beidel, & Turner, 2007; S. W. White, Bray, & Ollendick, 2012). Adults with ASD without co-occurring intellectual disability may experience higher levels of social anxiety due to awareness of their social disability or social exclusion, consequently leading to the development of excessive apprehension about social situations and fear of potential negative evaluation by others (Susan W. White, Oswald, Ollendick, & Scahill, 2009). Heightened social anxiety can lead to avoidance of social situations and awkward social exchanges, consequently promoting further social isolation (Myles, Barnhill, Hagiwara, Griswold, & Simpson, 2001).
Social Cognition
Social cognition includes the ability to identify, interpret, and respond to various social cues and to understand other people’s perspectives, which facilitates successful navigation of the social world (Frith, 2008). There is extensive literature on social cognition deficits in ASD, including in theory of mind (ToM) (i.e., the ability to take someone else’s perspective and understand someone else’s thoughts, beliefs, and intentions and nonverbal social cues) (Baron-Cohen, Leslie, & Frith, 1985; Baron-Cohen et al., 1999; Kennedy & Adolphs, 2012; Volkmar, 2011). Older children and adults with ASD, in particular, demonstrate intact simple ToM abilities, but show impairments in advanced ToM tasks like picking up on subtle nonverbal social cues (Baron-Cohen, Wheelwright, Hill, Raste, & Plumb, 2001), interpreting social stories (Happe, 1994), making social inferences (Mathersul, McDonald, & Rushby, 2013), and understanding implied or non-literal meanings in language (Corcoran, Mercer, & Frith, 1995; Craig, Hatton, Craig, & Bentall, 2004).
Several studies find that adults with ASD have reduced ability to identify emotions (Golan, Baron-Cohen, Hill, & Golan, 2006). However, other studies suggest that adults with ASD without co-occurring intellectual disability have more subtle difficulties, with intact basic emotion labeling abilities (Harms, Martin, & Wallace, 2010; Tanaka et al., 2012), but reduced ability to generalize facial emotions across different identities (Tanaka et al., 2012) and/or a tendency to have a potential negative bias in the interpretation of facial expressions (Eack, Mazefsky, & Minshew, 2015).
Social Skills
Deficits in social skills are well documented in individuals with ASD across the lifespan and may relate to deficits in other social domains, such as social motivation, social anxiety, or social cognition (Barnhill, 2007; Chevallier, Kohls, et al., 2012; Howlin, 2000). These skill deficits in adults with ASD are often associated with difficulty in creating and maintaining friendships and romantic relationships, reduced employment rates (D. Hendricks, 2010; Shattuck, Narendorf, et al., 2012; Taylor & Seltzer, 2011), and difficulty with functioning in the community (Barnhill, 2007; D. R. Hendricks & Wehman, 2009; Howlin, 2000).
There is considerable evidence to suggest that adults with ASD demonstrate deficits in all four main categories of behavior underlying social functioning, but these categories have not all been measured in the same sample. In the current study, we measured each category in a cohort of adults with ASD without co-occurring intellectual disability. We assessed correlations among measures within the same category and measures across categories, as well as measures of overall ASD symptom levels and social network size. We hypothesized that there would be high correlations among measures within the same category, supporting their convergent validity. We also hypothesized there would be small to modest correlations between categories, reflecting related but distinct abilities.
METHOD
Participants were recruited for a pilot study of a novel treatment program to improve social functioning in adults with ASD. At baseline, participants were administered a comprehensive battery assessing the four categories of behavior (social motivation, social anxiety, social cognition, social skills), ASD symptoms, community functioning, and overall quality of life. Here we report the results of baseline data.
Procedures
Participants were recruited from various sources, including the Center for Autism Research at the Children’s Hospital of Philadelphia (CHOP); ASD service providers and media advertisements; and the Adult Autism Spectrum Program at Penn Medicine. All interested participants were screened using a brief telephone interview that gathered clinical and developmental history from each participant and an informant (i.e., parent or guardian). Participants who screened into the study were invited for an in-person assessment to finalize eligibility. Twenty-nine participants were identified as eligible. Eligibility and baseline assessments were conducted in two separate sessions at the Perelman School of Medicine at the University of Pennsylvania, in conjunction with CHOP. Following an explanation of study procedures, all participants provided written informed consent. The University of Pennsylvania Institutional Review Board reviewed and approved the study protocol.
Participants
Inclusion and Exclusion Criteria
Participants were required to meet DSM-5 criteria for ASD, which was confirmed using the Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2; (Lord et al., 2012)) and Social Communication Questionnaire (SCQ; (Berument, Rutter, Lord, Pickles, & Bailey, 1999; Rutter, Bailey, & Lord, 2003)). They also had to be at least 18 years old, have a verbal IQ of 70 or above—as measured by the Wechsler Abbreviated Scale of Intelligence (WASI; (Wechsler, 2011))—and have no previous diagnosis of intellectual disability. Individuals who reported having comorbid psychiatric disorders were eligible for this study, with the exception of severe current depressive or manic symptoms or current psychotic symptoms, which would interfere with participation in the intervention. Concomitant neuropsychiatric medication was also permitted. Individuals who were severely self-injurious or aggressive in the four weeks prior to enrollment were not eligible, as this would interfere with participation in the intervention.
Assessment measures
Clinical and cognitive characteristics of participants were assessed using a battery of measures (see Table 1), administered by clinical psychology post-doctoral fellows and trained research staff. For certain behavioral components of social functioning, few standardized assessments have been validated in adults with ASD. Therefore, we included a combination of measures previously used for either adults or younger populations with ASD, those used in adolescent and adult schizophrenia research to assess social deficits, and those designed for the neurotypical adult population.
Table 1.
Description of assessment measures administered to participants
| ASSESSMENT NAME | DESCRIPTION | SCORE USED | CRONBACH’S α | FORMAT | REFERENCE |
|---|---|---|---|---|---|
| INTELLECTUAL FUNCTIONING | |||||
| Wechsler Abbreviated Scale of Intelligence, 2nd Ed. (WASI-II) | Assessment of cognitive functioning (intelligence) for clinical populations and typically developing control populations 6 to 90 years of age. It generates an estimate of general intellectual ability by using four subtests, two verbal and two performance scores. | FSIQ-4; VCI; PRI | -- | Clinical Interview | (Wechsler, 2011) |
| ASD PHENOTYPE | |||||
| Autism Diagnostic Observation Schedule, 2nd Ed. (ADOS-2) – Module 4 | Gold-standard diagnostic assessment for ASD; involves a semi-structured interview assessment of communication, social interaction, imagination/creativity, and stereotyped behaviors and restricted interests designed specifically for individuals suspected of having ASD. The current study utilized Module 4, targeting older adolescents and adults with fluent speech. Internal consistency, measured by Cronbach’s alpha (Cronbach, 1951), was 0.84 and 0.61 for the social affect and restricted repetitive behavior domains respectively (Hus & Lord, 2014). | Module 4 Calibrated Severity Score (CSS) | 0.62a | Clinical Interview | (Lord et al., 2012) |
| Social Communication Questionnaire (SCQ) | 40 ‘yes or no’ questions used to assess behavioral impairments in the areas of reciprocal social interaction, language and communication, and repetitive and stereotyped patterns of behavior over the course of the individual’s lifetime. The SCQ has shown strong discrimination between ASD and non-ASD cases with a sensitivity score of 0.88 and a specificity score of 0.72 (Chandler et al. 2007). | Total Score | 0.83 | Informant Report | (Berument, Rutter, Lord, Pickles, & Bailey, 1999); (Chandler et al., 2007) |
| Social Responsiveness Scale, 2nd Ed., Adult (SRS-II) | 65-item assessment designed to measure reciprocal behavior, social use of language, and other behaviors characteristic of ASD. The SRS-II Adult form has shown a high internal consistency (coefficient alpha) of approximately 0.90 – 0.95 in several studies (Bolte et al 2011; Chan, Smith, Hong, Greenberg, & Mailick, 2017; Constantino & Gruber, 2012; Seltzer et al., 2011). | Total Score | 0.95 | Informant Report | (Constantino & Gruber, 2012) |
| Social Responsiveness Scale, 2nd Ed., Self-Report (SRS-SR) | Self-report version of the SRS-II (see description above). | Total Score | 0.93 | Self-Report | (Constantino & Gruber, 2012) |
| The Broad Autism Phenotype Questionnaire (BAPQ) | 36-item scale designed to measure the Broad Autism Phenotype (BAP), a set of personality and language characteristics that reflect the phenotypic expression of the genetic liability to autism in adults with and without ASD. Items are broken down into three subscales measuring aloofness, pragmatic language problems, and rigid personality. Inter-item reliability (as measured by Cronbach’s a coefficient) is reported as 0.95 across all 36 items and 0.94, 0.91, and 0.85 for the aloof, rigid, and pragmatic language subscales respectively (Hurley et al. 2007). | Total Score | 0.94 | Self-Report | (Hurley, Losh, Parlier, Reznick, & Piven, 2007) |
| SOCIAL MOTIVATION | |||||
| The Broad Autism Phenotype Questionnaire (BAPQ) | (Refer to description above) | Aloof Subscale | -- | Self-Report | (Hurley et al., 2007) |
| Motivation and Pleasure Scale - Self-Report (MAP-SR) | 15-item scale of social motivation and the self-report version of the Clinical Assessment Interview for Negative Symptoms (CAINS) Motivation and Pleasure subscale. Items measure consummatory and anticipatory pleasure related to social and recreational or work domains and motivation and effort to engage in relationships and activities. Validated in individuals with adults schizophrenia and demonstrated excellent internal consistency (Cronbach’s α = 0.90) (Llerena et al., 2013). | Total Score | 0.85 | Self-Report | (Llerena et al., 2013) |
| Conte Social Interest Questionnaire (CSIQ) | 9-item scale of social interest created by Daniel Wolf, Asst Professor of Psychiatry at the University of Pennsylvania. 9 items were modified, adapted, and summarized from similar items in the Autism Spectrum Quotient (AQ; Bishop and Seltzer, 2012), Affilitative Tendency Scale (MAFF; Mehrabian, 1994), and MBTI (Myers and McCaulley, 1985). | Total Score | 0.81 | Self-Report | |
| The Schizotypal Personality Questionnaire (SPQ) | 74-item scale based on DSM-III-R criteria for schizotypal personality disorder. The measure contains subscales based around nine schizotypal traits, some of which have overlap with symptoms of ASD, including social motivation and social anxiety. We also used the 7-item Jackson Infrequency subscale in order to gauge validity of responses in the dataset. The measure was found to have high sampling validity, high internal consistency (Cronbach’s α = 0.91) and good test-retest reliability (0.82) (Raine 1991). | No Close Friends Subscale (SPQ-NCF) | 0.91b | Self-Report | (Raine, 1991) |
| SOCIAL ANXIETY | |||||
| Liebowitz Social Anxiety Scale (LSAS) | 24-item scale of social anxiety that allows for discrimination between how fearful participants with and without ASD find a particular situation versus how often they avoid the same situation. The LSAS-SR has shown good psychometric properties as demonstrated by the results of test-retest reliability, internal consistency of 0.95 (Fresco et al. 2001), and convergent and discriminant validity and has been shown to be comparable to the clinician-administered version (Liebowitz 1987; Fresco et al. 2001; Baker et al. 2002). | Total Score | 0.96 | Self-Report | (Fresco et al., 2001); (Bejerot, Eriksson, & Mortberg, 2014) |
| The Schizotypal Personality Questionnaire (SPQ) | (Refer to description above) | Social Anxiety Subscale (SPQ-SA) | -- | Self-Report | (Raine, 1991) |
| SOCIAL COGNITION | |||||
| Penn Emotion Recognition Task-40 (ER40) | Standardized test of facial emotion recognition ability consisting of 40 color photographs of evoked expressions from adult actors displaying four basic emotions (happy, sad, angry, and fearful) and neutral facial expressions. The participant is asked to identify the emotions displayed by the face. The timing of the responses is recorded. Assessment has been used to evaluate individuals with ASD, schizophrenia, and typically developing individuals. Internal consistency of response accuracy is moderate (Cronbach’s α = 0.59) (Gur et al., 2010). | Total Score | -- | Performance Based | (Kohler et al., 2003; A.E. Pinkham et al., 2008) |
| The Hinting Task | Measure of Theory of Mind (ToM, i.e. ability to understand others mental states) consisting of ten short written vignettes involving social interactions between two characters, one of whom drops a hint at the end of the vignette about their desire or intention. The participant is read the vignettes and is asked to infer what the character means by their hint. Internal consistency (Cronbach’s α) and test-retest reliability (Pearson’s r) for typically-developing controls was reported as 0.56 and 0.42 respectively and for adults with schizophrenia was reported as 0.73 and 0.64 respectively (A. E. Pinkham, Penn, Green, & Harvey, 2016). | Total Score | 0.84 | Performance Based | (Corcoran, Mercer, & Frith, 1995) |
| SOCIAL SKILLS | |||||
| The Contextual Assessment of Social Skills (CASS-INT and CASS-BORED) | Observational measure of social skills designed for adolescents and young adults with ASD. Participants engage in two 3-minute role-play conversations with two confederates who are unfamiliar to the participant; measures response of participant to nonverbal social cues of the ‘interested’ confederate and the ‘bored’ confederate with higher scores representing greater social skill level. Two trained raters coded each set of role-plays from recorded footage. Both raters achieved at least 90% inter-rater agreement (IRA) with the lead author (AAP) on practice videos before rating study videos. IRA was calculated by dividing agreements by disagreements for each item. Following training, both raters achieved 85% IRA between one another. The CASS demonstrated sound internal consistency (Cronbach’s α = 0.75) and good external validity (correlations with theory of mind and autism severity) (Ratto et al. 2011). | Total Interested Condition Score; Total Bored Condition Score | 0.80 | Performance Based | (Ratto, Turner-Brown, Rupp, Mesibov, & Penn, 2011) |
| COMMUNITY SOCIAL FUNCTIONING | |||||
| Social Network Index (SNI) | 15-item scale used to assess 12 types of social relationships and the amount of contact they may have with each type of relationship roughly every two weeks. Helps to determine the type and size of the social network held by each participant. | Total Score | --c | Self-Report | (Bickart, Wright, Dautoff, Dickerson, & Barrett, 2011; Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997) |
| The Scales of Psychological Well-Being (SPWB) | 42-item scale designed to measure six dimensions of psychological well-being, including autonomy, environmental mastery, personal growth*, positive relations with other, purpose in life*, and self-acceptance*. *Indicates subscales used in this study. Scale intercorrelations (Pearson’s r) ranged from 0.16 to 0.31 and internal consistency (Cronbach’s α) ranged from 0.33 to 0.52 (Ryff & Keyes, 1995). | Total Score | 0.69 | Self-Report | (Ryff, 1989; Ryff & Keyes, 1995) |
Note:
‘Description’ column provides general information on each assessment and data from previously published studies. ‘Cronbach’s alpha’ column provides data from our study.
-- indicate values were not computed
Social affect and restricted repetitive behavior total score.
SPQ total score.
Response format of the Social Network Index not amenable to internal consistency coefficient calculation.
Data analysis
Validation items from a modified Jackson Infrequency subscale embedded in the Schizotypal Personality Questionnaire were used to screen data for random or careless self-report responding (>3 infrequency items endorsed). Data from one participant were removed from analyses due to incomplete questionnaires and random responding.
In order to standardize interpretation of data from all assessment measures, raw scores of some measures were inverted so that higher scores indicated greater impairment across all measures. Raw scores for each measure were then converted into standard scores (z-scores), and pair-wise bivariate correlations (i.e., Pearson correlation coefficients) between scores were analyzed using IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, N.Y., USA). To correct for multiple comparisons, significance thresholds were set at a false discovery rate of 10% (Benjamini & Hochberg, 1995). To assess internal consistency reliability, we computed Cronbach’s alpha (Cronbach, 1951) for each total scale, and for relevant subscales as indicated in Table 1.
RESULTS
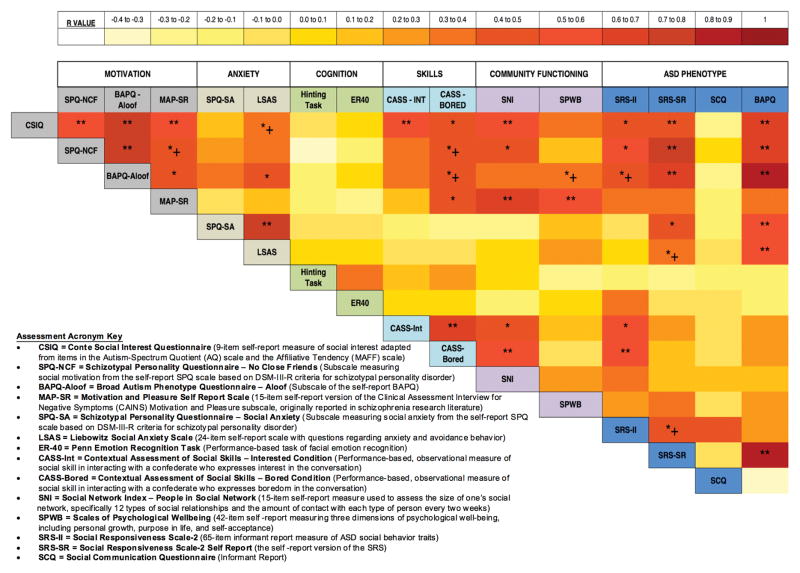
As shown in Table 1, all measures exhibited adequate to excellent internal consistency, commensurate with prior reports. Demographic and diagnostic information of participants are presented in Table 2. Bivariate correlation analyses demonstrated significant, positive correlations among measures within each of the social motivation, social anxiety, and social skills categories, but not within measures of social cognition and community functioning (Figure 1, see Supporting Information for Pearson correlation coefficient values). All measures of social motivation were significantly correlated with each other (0.47≤r≤ 0.78; p<0.01). The two measures of social anxiety were significantly correlated (r=0.74; p<0.001), as were the two measures of social skills (r=0.62; p<0.001). Significant correlations among measures of ASD phenotype ranged from r=0.44 to r=0.82 (p<0.05). Measures of social cognition were not significantly correlated with each other (r=0.30).
Table 2.
Participant demographic and diagnostic data (n = 28)
| Participant Information | ||||
|---|---|---|---|---|
| N | % | |||
| Sex | ||||
| Male | 24 | 85.7 | ||
| Female | 4 | 14.3 | ||
| Race | ||||
| White | 22 | 78.6 | ||
| African-American | 3 | 10.7 | ||
| Asian-American | 3 | 10.7 | ||
| Neuropsychiatric Medication Usage | 25 | 89 | ||
| Frequency of Co-Occurring Psychiatric Disorders | ||||
| Depression | 4 | 14.3 | ||
| Anxiety Disorder | 9 | 32.1 | ||
| Bipolar Disorder | 2 | 7.1 | ||
| Attention Deficit Hyperactivity Disorder | 14 | 50 | ||
| Obsessive-Compulsive Disorder | 7 | 25 | ||
| Employment Status | ||||
| Full Time | 5 | 17.6 | ||
| Part Time, Paid (Part-Time, Unpaid) | 6 (2) | 21.4 (7.1) | ||
| Unemployed | 15 | 53.6 | ||
| Current Living Situation | ||||
| Living Independently | 3 | 10.7 | ||
| Living with Family/Guardian | 25 | 89.3 | ||
| Mean | SD | Min | Max | |
| Age (in years) | 26 | 7.3 | 20 | 48 |
| ASD Phenotype | ||||
| Autism Diagnostic Observation Schedule Overall Calibrated Severity Score (CSS) | 7.3 | 1.9 | 2.0 | 10.0 |
| Social Communication Questionnaire (SCQ; N=26) | 16.4 | 7.1 | 3.0 | 28.0 |
| Social Responsiveness Scale-2 Raw/T-Score (SRS-II; N=24) | 86.5/66.2 | 28.2/9.9 | 42/51 | 149/88 |
| Social Responsiveness Scale-2 Self-Report Raw/T-Score (SRS-SR) | 79.8/63.9 | 24.5/8.7 | 33/47 | 126/80 |
| Broad Autism Phenotype Questionnaire (BAPQ) | 3.7 | 0.7 | 2.2 | 5.0 |
| Intellectual Functioning | ||||
| Wechsler Abbreviated Scale of Intelligence | ||||
| VCI | 107.7 | 21.0 | 71.0 | 160.0 |
| PRI | 100.8 | 22.8 | 65.0 | 160.0 |
| FSIQ-4 | 104.6 | 19.7 | 72.0 | 140.0 |
| Social Motivation | ||||
| BAPQ - Aloof Subscale (BAPQ-Aloof) | 3.7 | 1.0 | 2.1 | 5.3 |
| Motivation and Pleasure Self Report (MAP-SR) | 28.8 | 8.3 | 11.0 | 45.0 |
| Conte Social Interest Questionnaire (CSIQ) | 24.2 | 5.5 | 13.0 | 35.0 |
| Schizotypal Personality Questionnaire - No Close Friends Subscale (SPQ-NCF) | 5.0 | 2.1 | 0.0 | 9.0 |
| Social Anxiety | ||||
| Liebowitz Social Anxiety Scale (LSAS) | 45.0 | 26.8 | 7.0 | 113.0 |
| SPQ – Social Anxiety Subscale (SPQ-SA) | 5.4 | 2.5 | 0.0 | 8.0 |
| Social Cognition | ||||
| Penn Emotion Recognition Task (ER-40) | 77.9 | 9.2 | 57.5 | 95.0 |
| The Hinting Task | 14.3 | 4.2 | 2.0 | 19.0 |
| Social Skills | ||||
| Contextual Assessment of Social Skills | ||||
| Interested Condition Score (CASS-INT) | 15.9 | 4.5 | 8.0 | 24.0 |
| Bored Condition Score (CASS-BORED) | 19.8 | 6.3 | 8.0 | 31.5 |
| Community Social Functioning | ||||
| Social Network Index – People in Social Network Subscale (SNI) | 11.4 | 7.4 | 1.0 | 33.0 |
| Scales of Psychological Wellbeing (SPWB) | 162.3 | 15.9 | 132.0 | 201.0 |
Figure 1.
Heat map (heat scores were assigned on the basis of the Pearson correlation coefficient values) showing analysis of correlation (**correlation is significant at P<.01 level (2-tailed) and remained significant after false discovery rate analysis; *correlation is significant at P<.05 level (2-tailed) and remained significant after false discovery rate analysis; *1 correlation is .03<P<.05 but did not remain significant after false discovery rate analysis) among standard scores of measures within and between behavioral components involved in social functioning in adults with ASD. See Supporting Information for Pearson correlation coefficient values.
Regarding correlations across categories, measures of social motivation were significantly correlated with measures of all other categories (social anxiety, social skills) as well as with community functioning and ASD phenotype (0.43≤r≤0.80; p<0.05), but not with social cognition. Additional correlations were found between measures of social anxiety and ASD phenotype (0.45≤r≤0.52; p<0.05); measures of social skills & community functioning (0.44≤r≤0.52; p<0.02); and measures of social skills & ASD phenotype (0.50≤r≤0.56; p<0.02).
After false discovery rate analysis was performed, the majority of significant correlations remained significant, with the exceptions noted in Figure 1.
DISCUSSION
To our knowledge, this is the first study to assess the associations of multiple measures of social motivation, social anxiety, social cognition, and social skills within the same sample of adults with ASD without co-occurring intellectual disability, an important step towards developing and targeting treatments to improve social functioning in this group. We found significant correlations within the categories of social motivation, social anxiety, and social skills, and some significant correlations between assessments across different categories. Measures of social motivation, in particular, demonstrated significant correlations with all categories except for social cognition.
Within Category Correlations
Significant correlations among measures within the categories of social motivation, social anxiety, and social skills
Social motivation, social anxiety, social cognition, social skills, and community functioning are each quite complex, and comprise many subdomains. In some cases, multiple measures within a category were quite overlapping in what they assessed, and in other cases less so. Our finding of significant correlations among measures within some categories may be attributable to the fact that these measures assess similar aspects of the category, and may also be attributable to the convergent validity of these tools for measuring the category. For example, the measures of social anxiety used in this study – LSAS and SPQ-SA – both contain items that measure social anxiety (i.e., the subjective, emotional aspect of social anxiety) as well as social avoidance (i.e., the behavioral consequence of social anxiety), and these two measures were significantly correlated in our sample.
As a second example, social motivation comprises social orienting, social interest, social approach (seeking), social pleasure (liking), and social maintaining (Chevallier, Kohls, et al., 2012). The measures used in the current study, the MAP-SR and SPQ-NCF, both utilize items that tap into a participant’s social interest, as well as the pleasure that they derive from social interaction, and those measures were significantly correlated. Finally, the CASS includes two testing conditions measuring social skills of participants during conversation with two different confederates. In one condition, the confederate was engaged and interested in the conversation and in the other condition the confederate was bored and disinterested in the conversation. While the nature of each social situation was very different, overall the social interaction skills (e.g. question asking, topic changes, gestures, positive affect) overlapped as seen by their significantly correlated scores. The significant correlations between multiple measures within the social anxiety and social motivation categories support the hypothesis that there is convergent validity among measures within these categories, and that such measures potentially could be used to track treatment response.
Measures of social cognition and community functioning demonstrated non-significant correlations within each category, perhaps because individual measures assessed distinct, largely non-overlapping aspects of each of those categories. Within social cognition, the ER40 and Hinting Task were used to measure various aspects of this category, but were not significantly correlated, perhaps because they measure two distinct sub-categories of social cognition. This latter interpretation is suggested by recent work (Pinkham et al., 2014) describing four core aspects of social cognition – 1) emotion processing, 2) social perception, 3) theory of mind/mental state attribution, and 4) attributional style/bias – involving different types of social information (Pinkham et al., 2014). The ER40 primarily assesses emotion-processing, whereas the Hinting Task primarily assesses mental state attribution (Pinkham et al., 2014). Another potential reason for lack of correlation between ER40 and the Hinting Task could be insufficient test-retest reliability in the Hinting Task (but not in the ER40), as pointed out by Pinkham et al. (2016).
Similarly, the two measures of community functioning used in this study, the SNI – a measure of the number of people in one’s social network – and SPWB – a measure of overall psychological wellbeing – were not significantly correlated, perhaps because they tap into distinctively different subdomains of community functioning. Social network size may not be related to a sense of overall psychological wellbeing in all individuals with ASD. In other words, the relationship between social network size and psychological well-being may be moderated by level of social motivation. The lack of correlation among the measures that we used suggests that it may be advisable to use multiple measures of both social cognition and community functioning, covering various aspects of each category.
Between Category Correlations
Social Motivation correlated with social anxiety, social skills, community functioning, and ASD phenotype
Our finding that social motivation correlated significantly with social anxiety, social skills, community functioning, and ASD phenotype is consistent with previous reports. For example, Carre and colleagues (Carre et al., 2015) found significant positive correlations between autistic traits and social anhedonia scores in both individuals with ASD and neurotypical individuals. Previous work has also demonstrated that impaired social motivation is significantly related to increased social anxiety in young adults with ASD (Swain et al., 2015). Overall, the correlations between measures of social motivation and measures of most other components of social functioning suggest a potentially important role for social motivation in overall social functioning and highlight the importance of targeting social motivation in treatment.
Anxiety correlated with ASD phenotype
The SPQ-SA was positively correlated with the SRS-SR and with the BAPQ. However, we did not find significant correlations between measures of anxiety and measures of social cognition, social skills, and community functioning. It may be that social cognition measures did not correlate with other categories of behavior, in part, because the social cognition measures were performance based, whereas other measures were not; however, the social cognition measures also did not correlate with each other. More work is needed with larger sample sizes to clarify the relationship between anxiety and these other categories in adults with ASD (Hillier et al., 2011).
Social skills correlated with ASD phenotype and community functioning
Measures of social skills impairment in this study were significantly correlated with measures of ASD phenotype and with measures of community functioning difficulties. These findings are consistent with prior reports that greater participation in social activities was predicted by less impairment in social interaction skills (Orsmond, Krauss, & Seltzer, 2004). However, concerns have been raised about the generalizability of social skills training in a clinical setting to daily functioning in the community. Increased focus on practicing social skills in various contexts and community settings (“programming for generalization”) may maximize the impact of social skills training on real-world functioning (Gates, Kang, & Lerner, 2017).
Limitations
The data presented in this study should be interpreted in light of several methodological limitations. As mentioned above, the current study is unique in measuring all of these behavioral categories and correlations among them in the same sample of adults with ASD; however, the modest sample size in this study limits statistical power and the ability to use statistical reduction approaches like factor analysis that more formally illuminate the structure of social function in adults with ASD. Given the limited sample size, future studies are needed to replicate these findings and test whether the categories of behavior, community functioning, and/or ASD phenotype can be considered predictors of social functioning in adults with ASD. Larger, more diverse sample sizes in future studies would also allow for latent class analyses to examine variability within individuals and identify subgroups based on patterns of strengths and weaknesses within each component of social functioning. The predominance of young, white, male adults in this study limits the generalizability of these findings to more diverse groups. A matched sample of neurotypical individuals would enhance conclusions regarding the magnitude of impairments. Additionally, this sample is not representative of the general population of adults with ASD due to the fact that we excluded individuals with ongoing major issues with aggression or emotion dysregulation (Mazefsky et al., 2013).
Correlations between various measures depend upon the manner in which they are administered (e.g. self-report, performance-based) and psychometric properties of those measures. Many of the measures selected for this study have been reported to have test-retest reliability and/or internal consistency (Cronbach’s α) in the range of 0.8 – 1.0, and our internal consistency findings in this sample align with these reports. However, some measures used in this study, including the Hinting Task, ER-40, and the Scales of Psychological Well-Being, have lower reliabilities (Table 1) (Pinkham, Penn, Green, & Harvey, 2016). Given inherent variability in measure reliability, the correlations observed here are likely lower bound estimates of the true correlations. Consequently, it is possible that some of our observed correlations underestimate true correlations. In addition, many of the measures used to assess social functioning in adults with ASD rely upon self-report which may affect their sensitivity. For example, self-reported anxiety can be affected by the respondents’ insight level and self-reflective capacities, which can be limited in adults with ASD (Bird & Cook, 2013). Finally, due to limited availability of measures validated in adults with ASD, there is some overlap in the measures used, such that a particular measure focused on one category may also capture aspects of another category(ies). In fact, some categories may not be fully separable, e.g. social skill may be a category of behavior that goes beyond social cognition, but may necessarily involve some degree of social cognition. More research is needed to establish best practices for measuring these components of social functioning with reliable methods validated specifically in adults with ASD, especially in the context of treatment studies.
Conclusions
Despite these limitations, our results have implications for the development of treatments to improve social functioning in adults with ASD without co-occurring intellectual disability. Specifically, our findings suggest that future treatment research to increase social motivation may be important, as motivation was related to many other components of social functioning in our dataset. Future research may be warranted to test the hypothesis suggested by our data that increasing social motivation and sustaining that motivation over time may facilitate improvements in other domains and aspects of social functioning. Many existing social skills training programs for individuals with ASD lack strategies to substantially enhance motivation (Bishop-Fitzpatrick et al., 2013; Spain & Blainey, 2015).
While the categories that we have focused on are likely to be important, they may not be the only constructs impacting social functioning in adults with ASD. Future studies may want to expand this framework and include additional behaviors, including measures of emotion regulation that capture dysregulated behavior. In addition to the individual behaviors on which this study has focused, future studies are needed to address the role of societal acceptance, accommodation, and inclusivity of neurodiversity, which may go a long way towards improving well-being and overall social functioning in adults with ASD.
Overall, our data support the hypothesis that there may be distinct but related components of social functioning. The lack of robust correlations between categories of behavior underlying social functioning suggests that multidimensional treatments targeting an individual’s particular areas of need may be more effective than general, “one-size-fits-all” treatments. We expect that adults with ASD will show variability in their patterns of strengths and weaknesses in these various categories of behavior, and that a treatment program aimed at improving social functioning in adults with ASD may be most effective if it has elements that can be used in a modular way, tailored to the needs of a given individual. By designing treatment studies targeting specific behavioral components of social functioning, and measuring effects on those as well as other components, we stand to gain insight into cause-and-effect relationships among these components, thus opening the door to maximizing treatment effectiveness and improving long-term outcomes.
Supplementary Material
Acknowledgments
This work was supported by NIMH grant R34MH104407, Services to Enhance Social Functioning in Adults with Autism Spectrum Disorder (Brodkin, PI); The Asperger Syndrome Program of Excellence (ASPE) at the University of Pennsylvania (Brodkin, co-Director); the National Center for Research Resources, Grant UL1RR024134, now the National Center for Advancing Translational Sciences, Grant UL1TR000003; and the Translational Medicine and Therapeutics’ (ITMAT) Transdisciplinary Program in Translational Medicine and Therapeutics at the University of Pennsylvania. We also thank all the families who participated in this study, without whom this research could not have been conducted. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders . 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]; Association, A. P. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: American Psychiatric Association; 2013. (DSM-5) [Google Scholar]
- Baker SL, Heinrichs N, Kim H-J, Hofmann SG. The Liebowitz social anxiety scale as a self-report instrument: A preliminary psychometric analysis. Behavior Research and Therapy. 2002;40(6):701–715. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Barnhill GP. Outcomes in adults with Asperger syndrome. Focus on Autism and other Developmental Disabilities. 2007;22(2):116–126. [Google Scholar]
- Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985;21:37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Ring HA, Wheelwright S, Bullmore ET, Brammer MJ, Simmons A, Williams SC. Social intelligence in the normal and autistic brain: an fMRI study. European Journal of Neuroscience. 1999;11:1891–1898. doi: 10.1046/j.1460-9568.1999.00621.x. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S. The Friendship Questionnarie: an investigation of adults with Asperger syndrome or high-functioning autism, and normal sex differences. Journal of Autism and Developmental Disorders. 2003;33:509–517. doi: 10.1023/a:1025879411971. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “Reading the Mind in the Eyes” test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. Journal of Child Psychology and Psychiatry. 2001;42:241–251. [PubMed] [Google Scholar]
- Bejerot S, Eriksson JM, Mortberg E. Social anxiety in adult autism spectrum disorder. Psychiatry Res. 2014;220(1–2):705–707. doi: 10.1016/j.psychres.2014.08.030. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. 1995;57(1):289–300. [Google Scholar]
- Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism Screening Questionnaire: Diagnostic validity. British Journal of Psychiatry. 1999;175:444–451. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism Screening Questionnaire: Diagnostic validity. British Journal of Psychiatry. 1999;175:444–451. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- Bickart KC, Wright CI, Dautoff RJ, Dickerson BC, Barrett LF. Amygdala volume and social network size in humans. Nat Neurosci. 2011;14(2):163–164. doi: 10.1038/nn.2724. doi: http://www.nature.com/neuro/journal/v14/n2/abs/nn.2724.html#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billstedt E, Gillberg IC, Gillberg C. Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. Journal of Child Psychology and Psychiatry. 2007;48(11):1102–1110. doi: 10.1111/j.1469-7610.2007.01774.x. [DOI] [PubMed] [Google Scholar]
- Bird G, Cook R. Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism. Translational Psychiatry. 2013;3:1–8. doi: 10.1038/tp.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SL, Seltzer MM. Self-reported autism symptoms in adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42(11):2354–2363. doi: 10.1007/s10803-012-1483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, Minshew NJ, Eack SM. The relationship between stress and social functioning in adults with autism spectrum disorder and without intellectual disability. Autism Res. 2015;8(2):164–173. doi: 10.1002/aur.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43:687–694. doi: 10.1007/s10803-012-1615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolte S, Westerwald E, Holtmann M, Freitag C, Poustka F. Autistic traits and autism spectrum disorders: the clinical validity of two measures presuming a continuum of social communication skills. Journal of Autism and Developmental Disorders. 2011;41:66–72. doi: 10.1007/s10803-010-1024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics. 2014;168(8):721–728. doi: 10.1001/jamapediatrics.2014.210. [DOI] [PubMed] [Google Scholar]
- Carre A, Chevallier C, Robel L, Barry C, Maria AS, Pouga L, … Berthoz S. Tracking social motivation systems deficits: the affective neuroscience view of autism. J Autism Dev Disord. 2015;45(10):3351–3363. doi: 10.1007/s10803-015-2498-2. [DOI] [PubMed] [Google Scholar]
- Chan W, Smith LE, Hong J, Greenberg JS, Mailick MR. Validating the Social Responsiveness Scale for adults with autism. Autism Research. 2017;10:1663–1671. doi: 10.1002/aur.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler S, Charman T, Baird G, Simonoff E, Loucas T, Meldrum D, Scott M, Pickles A. Validation of the social communication questionnaire in a population cohort of children with autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(10):1324–1332. doi: 10.1097/chi.0b013e31812f7d8d. [DOI] [PubMed] [Google Scholar]
- Chen YW, Bundy AC, Cordier R, Chien YL, Einfeld SL. Motivation for everyday social participation in cognitively able individuals with autism spectrum disorder. Neuropsychiatr Dis Treat. 2015;11:2699–2709. doi: 10.2147/NDT.S87844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevallier C, Grezes J, Molesworth C, Berthoz S, Happe F. Brief report: Selective social anhedonia in high functioning autism. J Autism Dev Disord. 2012;42(7):1504–1509. doi: 10.1007/s10803-011-1364-0. [DOI] [PubMed] [Google Scholar]
- Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT. The social motivation theory of autism. Trends in Cognitive Sciences. 2012;16:231–239. doi: 10.1016/j.tics.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevallier C, Parish-Morris J, McVey A, Rump K, Sasson NJ, Herrington JD, Schultz RT. Measuring social attention and motivation in autism spectrum disorder using eye-tracking: stimulus type matters. 2015 doi: 10.1002/aur.1479. manuscript in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997;277:1940–1944. [PubMed] [Google Scholar]
- Constantino J, Gruber CP. Social Responsiveness Scale. Second Edition. Los Angeles, CA: Western Psychological Services; 2012. [Google Scholar]
- Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomataology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophrenia Research. 1995;17(1):5–13. doi: 10.1016/0920-9964(95)00024-g. [DOI] [PubMed] [Google Scholar]
- Craig JS, Hatton C, Craig FB, Bentall RP. Persecutory beliefs, attributions and theory of mind: comparison of patients with paranoid delusions, Asperger’s syndrome and healthy controls. Schizophrenia Research. 2004;69:29–33. doi: 10.1016/S0920-9964(03)00154-3. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- Eack SM, Mazefsky CA, Minshew NJ. Misinterpretation of facial expressions of emotion in verbal adults with autism spectrum disorder. Autism. 2015;19(3):308–315. doi: 10.1177/1362361314520755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factor RS, Ryan SM, Farley JP, Ollendick TH, Scarpa A. Does the Presence of Anxiety and ADHD Symptoms Add to Social Impairment in Children with Autism Spectrum Disorder? Journal of Autism and Developmental Disorders. 2017;47(4):1122–1134. doi: 10.1007/s10803-016-3025-9. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31(06) doi: 10.1017/s0033291701004056. [DOI] [PubMed] [Google Scholar]
- Frith CD. Social cognition. Philos Trans R Soc Lond B Biol Sci. 2008;363(1499):2033–2039. doi: 10.1098/rstb.2008.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161:343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- Gates JA, Kang E, Lerner MD. Efficacy of group social skills interventions for youth with autism spectrum disorder: A systematic review and meta-analysis. Clin Psychol Rev. 2017;52:164–181. doi: 10.1016/j.cpr.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golan O, Baron-Cohen S, Hill JJ, Golan Y. The “Reading the Mind in Films” task: complex emotion recognition in adults with and without autism spectrum conditions. Soc Neurosci. 2006;1(2):111–123. doi: 10.1080/17470910600980986. [DOI] [PubMed] [Google Scholar]
- Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(5):369–376. doi: 10.1016/j.jaac.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur RC, Richard J, Hughett P, Calkins ME, Macy L, Bilker WB, Brensinger C, Gur RE. A cognitive neuroscience-based computerized battery for efficient measurement of individual differences: standardization and initial construct validation. Journal of Neuroscience Methods. 2010;187(2):254–262. doi: 10.1016/j.jneumeth.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Happe FGE. An advanced test of theory of mind: understanding of story characters’ thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. Journal of Autism and Developmental Disorders. 1994;24:129–154. doi: 10.1007/BF02172093. [DOI] [PubMed] [Google Scholar]
- Harms MB, Martin A, Wallace GL. Facial emotion recognition in autism spectrum disorders: a review of behavioral and neuroimaging studies. Neuropsychol Rev. 2010;20(3):290–322. doi: 10.1007/s11065-010-9138-6. [DOI] [PubMed] [Google Scholar]
- Hendricks D. Employment and adults with autism spectrum disorders: challenges and strategies for success. Journal of Vocational Rehabilitation. 2010;32(2):125–134. [Google Scholar]
- Hendricks DR, Wehman P. Transition from school to adulthood for youth with autism spectrum disorders: review and recommendations. Focus on Autism and Other Developmental Disabilties. 2009;24(2):77–88. [Google Scholar]
- Hillier A, Fish T, Cloppert P, Beversdorf DQ. Outcomes of a social and vocational skills support group for adolescents and young adults on the autism spectrum. Focus on Autism and other Developmental Disabilities. 2007;22(2):107–115. [Google Scholar]
- Hillier A, Fish T, Siegel JH, Beversdorf DQ. Social and vocational skills training reduces self-reported anxiety and depression among young adults on the autism spectrum. Journal of Developmental and Physical Disabilities. 2011;23:267–276. doi: 10.1007/s10882-011-9226-4. [DOI] [Google Scholar]
- Hollocks MJ, Jones CRG, Pickles A, Baird G, Happé F, Charman T, Simonoff E. The Association Between Social Cognition and Executive Functioning and Symptoms of Anxiety and Depression in Adolescents With Autism Spectrum Disorders. Autism Research. 2014;7(2):216–228. doi: 10.1002/aur.1361. [DOI] [PubMed] [Google Scholar]
- Howlin P. Outcome in adult life for more able individuals with autism or Asperger syndrome. Autism. 2000;4(1):63–83. [Google Scholar]
- Howlin P, Moss P. Adults with autism spectrum disorders. The Canadian Journal of Psychiatry. 2012;57(5):275–283. doi: 10.1177/070674371205700502. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(6):572–581. doi: 10.1016/j.jaac.2013.02.017. [DOI] [PubMed] [Google Scholar]
- Hurlbutt K, Chalmers L. Adults with autism speak out: perceptions of their life experiences. Autism. 2002;17(2):103–111. [Google Scholar]
- Hurley RS, Losh M, Parlier M, Reznick JS, Piven J. The broad autism phenotype questionnaire. J Autism Dev Disord. 2007;37(9):1679–1690. doi: 10.1007/s10803-006-0299-3. [DOI] [PubMed] [Google Scholar]
- Hus V, Lord C. The Autism Diagnostic Observation Schedule, Module 4: Revised Algorithm and Standardized Severity Scores. Journal of Autism and Developmental Disorders. 2014;44(8):1996–2012. doi: 10.1007/s10803-014-2080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy DP, Adolphs R. Perception of emotions from facial expressions in high-functioning adults with autism. Neuropsychologia. 2012;50(14):3313–3319. doi: 10.1016/j.neuropsychologia.2012.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klin A, Jones W, Schultz R, Volkmar F, Cohen D. Visual fixation patterns during viewing of naturalistic social situations as predictors of social competence in individuals with autism. Archives of General Psychiatry. 2002;59:809–816. doi: 10.1001/archpsyc.59.9.809. [DOI] [PubMed] [Google Scholar]
- Kohler CG, Turner TH, Bilker WB, Brensinger CM, Siegel SJ, Kanes SJ, Gur RE, Gur RC. Facial emotion recognition in schizophrenia: intensity effects and error pattern. American Journal of Psychiatry. 2003;160:1768–1774. doi: 10.1176/appi.ajp.160.10.1768. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Mod Probl Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Llerena K, Park SG, McCarthy JM, Couture SM, Bennett ME, Blanchard JJ. The Motivation and Pleasure Scale-Self-Report (MAP-SR): reliability and validity of a self-report measure of negative symptoms. Compr Psychiatry. 2013;54(5):568–574. doi: 10.1016/j.comppsych.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule. 2. Torrance, CA: Western Psychological Services; 2012. [Google Scholar]
- Maddox BB, White SW. Comorbid social anxiety disorder in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(12):3949–3960. doi: 10.1007/s10803-015-2531-5. [DOI] [PubMed] [Google Scholar]
- Mathersul D, McDonald S, Rushby JA. Understanding advanced theory of mind and empathy in high-functioning adults with autism spectrum disorder. J Clin Exp Neuropsychol. 2013;35(6):655–668. doi: 10.1080/13803395.2013.809700. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, White SW. The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(7) doi: 10.1016/j.jaac.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrabian A. Evidence bearing on the Affiliative Tendency (MAFF) and Sensitivity to Rejection (MSR) scales. Current Psychology: Developmental, Learning, Personality, Social. 1994;13:97–116. [Google Scholar]
- Muller E, Schuler A, Burton BA, Yates GB. Meeting the vocational support needs of individuals with Asperger syndrome and other autism spectrum disorders. Journal of Vocational Rehabilitation. 2003;18(3):163–175. [Google Scholar]
- Myers IB, McCaulley MH. Manual: a guide to the development and use of the Myers-Briggs Type Indicator. Palo Alto, CA: Consulting Psychologists Press; 1985. [Google Scholar]
- Myles BS, Barnhill GP, Hagiwara T, Griswold DE, Simpson RL. A synthesis of studies on the intellectual, academic, social/emotional and sensory characteristics of children and youth with asperger syndrome. Education and Training in Mental Retardation and Developmental Disabilities. 2001;36(3):304–311. [Google Scholar]
- Nakano T, Tanaka K, Endo Y, Yamane Y, Yamamoto T, Nakano Y, … Kitazawa S. Atypical gaze patterns in children and adults with autism spectrum disorders dissociated from developmental changes in gaze behaviour. Proc Biol Sci. 2010;277(1696):2935–2943. doi: 10.1098/rspb.2010.0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmond GI, Krauss MW, Seltzer MM. Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders. 2004;34:245–256. doi: 10.1023/b:jadd.0000029547.96610.df. [DOI] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Green MF, Harvey PD. Social Cognition Psychometric Evaluation: Results of the Initial Psychometric Study. Schizophr Bull. 2016;42(2):494–504. doi: 10.1093/schbul/sbv056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Green MF, Buck B, Healey K, Harvey PD. The social cognition psychometric evaluation study: results of the expert survey and RAND panel. Schizophr Bull. 2014;40(4):813–823. doi: 10.1093/schbul/sbt081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Green MF, Harvey PD. Social Cognition Psychometric Evaluation: Results of the Initial Psychometric Study. Schizophr Bull. 2016;42(2):494–504. doi: 10.1093/schbul/sbv056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham AE, Sasson NJ, Calkins ME, Richard J, Hughett P, Gur RE, et al. The other-race effect in face processing among African American and Caucasian individuals with schizophrenia. American Journal of Psychiatry. 2008;165(5):639–645. doi: 10.1176/appi.ajp.2007.07101604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raine A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophrenia Bulletin. 1991;17(4):555–564. doi: 10.1093/schbul/17.4.555. [DOI] [PubMed] [Google Scholar]
- Ratto AB, Turner-Brown L, Rupp BM, Mesibov GB, Penn DL. Development of the Contextual Assessment of Social Skills (CASS): a role play measure of social skill for individuals with high-functioning autism. J Autism Dev Disord. 2011;41(9):1277–1286. doi: 10.1007/s10803-010-1147-z. [DOI] [PubMed] [Google Scholar]
- Reichow B, Steiner AM, Volkmar F. Cochrane Review: Social skills groups for people aged 6 to 21 with autism spectrum disorders (ASD) Evidence-Based Child Health. 2013;8(2):266–315. doi: 10.1002/ebch.1903. [DOI] [PubMed] [Google Scholar]
- Roberson-Nay R, Strong DR, Nay WT, Beidel DC, Turner SM. Development of an abbreviated Social Phobia and Anxiety Inventory (SPAI) using item response theory: the SPAI-23. Psychol Assess. 2007;19(1):133–145. doi: 10.1037/1040-3590.19.1.133. [DOI] [PubMed] [Google Scholar]
- Ruocco AC, Reilly JL, Rubin LH, Daros AR, Gershon ES, Tamminga CA, … Sweeney JA. Emotion recognition deficits in schizophrenia-spectrum disorders and psychotic bipolar disorder: Findings from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) study. Schizophr Res. 2014;158:105–112. doi: 10.1016/j.schres.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire. Western Psychological Services; Los Angeles: 2003. [Google Scholar]
- Ryff CD. Happiness is everything, or is it? explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57(6):1069–1081. [Google Scholar]
- Ryff CD, Keyes CLM. The Structure of Psychological Well-Being Revisited. Journal of Personality and Social Psychology. 1995;69(4):719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Sachs G, Steger-Wuchse D, Kryspin-Exner I, Gur RC, Katschnig H. Facial recognition deficits and cognition in schizophrenia. Schizophrenia Research. 2004;68(1):27–35. doi: 10.1016/s0920-9964(03)00131-2. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, Taylor JL, Smith L, Orsmond GI, Esbensen AJ, Hong J. Adolescents and adults with autism spectrum disorders. New York, NY: Oxford University; 2011. [Google Scholar]
- Seltzer MM, Shattuck P, Abbeduto L, Greenberg JS. Trajectory of development in adolescents and adults with autism. Mental Retardation and Developmental Disabilities Research Reviews. 2004;10(4):234–237. doi: 10.1002/mrdd.20038. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. 2012;129(6):1042–1049. doi: 10.1542/peds.2011-2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Roux AM, Hudson LE, Taylor JL, Maenner MJ, Trani JF. Services for adults with an autism spectrum disorder. Canadian Journal of Psychiatry. 2012;57(5):284–291. doi: 10.1177/070674371205700503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spain D, Blainey SH. Group social skills interventions for adults with high-functioning autism spectrum disorders: A systematic review. Autism. 2015;19(7):874–886. doi: 10.1177/1362361315587659. [DOI] [PubMed] [Google Scholar]
- Swain D, Scarpa A, White S, Laugeson E. Emotion Dysregulation and Anxiety in Adults with ASD: Does Social Motivation Play a Role? J Autism Dev Disord. 2015;45(12):3971–3977. doi: 10.1007/s10803-015-2567-6. [DOI] [PubMed] [Google Scholar]
- Tanaka JW, Wolf JM, Klaiman C, Koenig K, Cockburn J, Herlihy L, … Schultz RT. The perception and identification of facial emotions in individuals with autism spectrum disorders using the Let’s Face It! Emotion Skills Battery. J Child Psychol Psychiatry. 2012;53(12):1259–1267. doi: 10.1111/j.1469-7610.2012.02571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders. 2011;41:566–574. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmar F. Understanding the social brain in autism. Developmental Psychobiology. 2011;53:428–434. doi: 10.1002/dev.20556. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. 2. San Antonio, TX: Psychological Corporation; 2011. [Google Scholar]
- White SW, Bray BC, Ollendick TH. Examining shared and unique aspects of Social Anxiety Disorder and Autism Spectrum Disorder using factor analysis. J Autism Dev Disord. 2012;42(5):874–884. doi: 10.1007/s10803-011-1325-7. [DOI] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.