Abstract
Bisphosphonates are stable structural analogs of pyrophosphate, which suppress the activity of osteoclasts, leading to decreased bone resorption. They are essential medications in the treatment of osteoporosis. Osteonecrosis of the jaw is a serious adverse effect of bisphosphonate therapy. The prevalence of bisphosphonate-related osteonecrosis of the jaw varies from 0% to 28%, and it can be triggered by dental extraction and trauma. Root canal therapy can delay, or even eliminate, the need for tooth extraction, and therefore, may reduce the risk of bisphosphonate-related osteonecrosis of the jaw. We suggest that this might be the best treatment for teeth with pulpal and/or periapical disease.
Bisphosphonates (BPs) are an essential medication in the treatment of osteoporosis, and are also used in the treatment of certain cancers.1 In 1995, the United States approved the first BP, fosamax or alendronate sodium, produced by Merck & Co for use in the treatment of osteoporosis.2 Further developments led to the introduction of new generations of BPs, which are characterized by their long-acting effects that improve patient compliance.2 Currently, BPs are an essential component in the treatment of osteoporosis.1 Bisphosphonate is broadly described worldwide.2 In the European Union countries, approximately 5% of the population aged 50 years or older has osteoporosis, and receives treatment with BPs frequently.3 As with any other medication, BPs have side effects; osteonecrosis of the jaw (BRONJ) related to BP use has important medical and dental implications.4
The purpose of this review is to provide an overview of BPs, highlight their implications in endodontic treatment, and provide guidelines to promote oral care in all patients receiving BP therapy during root canal treatment, to prevent BRONJ.
Bisphosphonate properties and effects
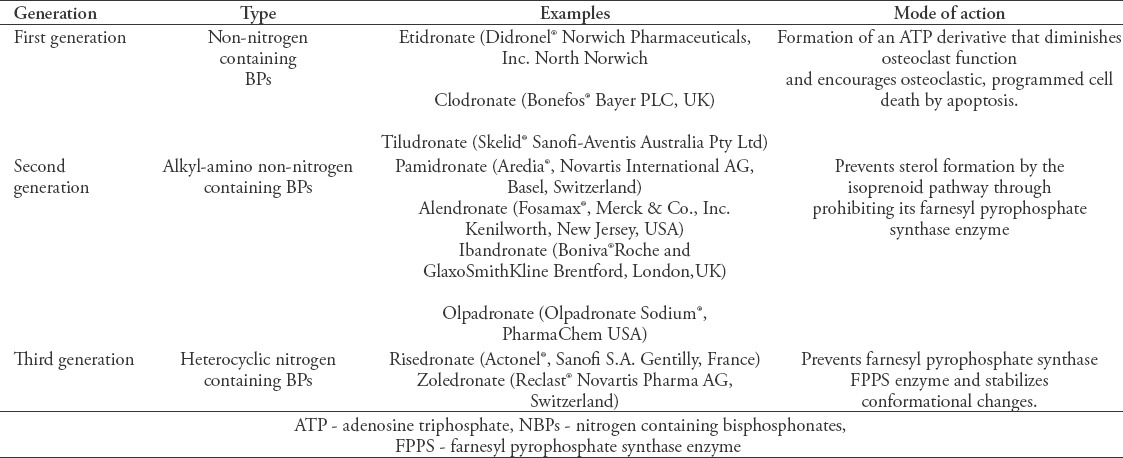
Bisphosphonates are stable structural analogs of pyrophosphate, which are deposited on the bone surface in the first few minutes or hours after uptake, with unbound BP swiftly removed renally.1,4 Bisphosphonates suppress the activity of osteoclasts, which leads to decreased bone resorption.5 The effects of BPs vary according to the generation they belong to (first, second, or third generation). The first generation (non-nitrogen containing) BPs induce apoptosis by the formation of a toxic analog of adenosine triphosphate, whereas the second and third generations (nitrogen-containing BPs) inhibit osteoclast function by targeting the enzyme farnesyl diphosphate synthase, which is necessary for post-translational modification of small Guanosine Triphosphate(GTP)-binding proteins.1 Both the potency and strength of binding to hydroxyapatite differ greatly between individual compounds.6 Table 1 shows the types of BPs, their modes of action, and examples of commercially available BPs.
Table 1.
Types and mode of action of bisphosphonates (BPs).
Side effects of bisphosphonates
As with any other drug, BPs have their own side effects. Oral BPs can cause nausea, epigastric pain, esophagitis, and gastric ulcer.7,8 Myalgia, arthralgia, low-grade fever, headache, and bone pain due to a temporary acute-phase response could occur during the first 24 to 72 hours following intravenous (IV) administration of BPs.9 Some reports mention an association between atrial fibrillation and the use of BPs.7,10,11 There is no definitive evidence of the increased risk of esophageal cancer or gastric cancer in male and female patients taking BPs.12 A case series study that extracted data from 2 main primary care centers in the United Kingdom showed that there was no relationship between BPs and esophageal cancer, but that using alendronate for a short duration might increase the possibility of gastric cancer.13 Bisphosphonates may rarely cause uveitis, scleritis, and orbital inflammatory disease.14-16 Atypical proximal femoral fractures could occur with long-term use of BP.17,18
Bisphosphonate-related osteonecrosis of the jaw (BRONJ)
Bisphosphonate-related osteonecrosis of the jaw is one of the serious adverse effects of BP therapy.19,20 The first cases of BRONJ related to BPs were reported over a decade ago.21 The American Society for Bone and Mineral Research (ASBMR) defines BRONJ as an exposed area of the bone in the upper or lower jaw, in the maxillofacial region, which does not recover within 8 weeks after diagnosis in a patient taking a BP, who has not received radiation therapy in the maxillofacial region.22
The occurrence of BRONJ has been correlated with 2 hypotheses: firstly, BPs tend to be highly concentrated in the jaw because of high vascularity, causing an anti-angiogenic effect, and secondly, its cytotoxic effect on osteoclasts and periodontal ligament cells suppresses bone turnover.23,24
The prevalence of BRONJ varies from 0% to 28%, with a higher incidence associated with the use of IV nitrogen-containing BP.25 The type of BP, frequency of use, and therapy duration are all factors that have effects on BRONJ. Moreover, oral BP use is associated with not more than a 4% incidence of BRONJ.26 Dental extractions and trauma trigger 64% of BRONJ cases;27 periodontitis accompanies 84% of BRONJ cases.28 The differential diagnoses of BRONJ include sinusitis, alveolar osteitis, periapical pathosis, gingivitis/periodontitis, and some types of cemento-osseous dysplasias with secondary resorption.29 The exposed necrotic bone may continue to be asymptomatic for a long duration.27 Inflammation of tissues surrounding these lesions will cause signs and symptoms such as tooth mobility, soft tissue swelling, erythema, ulcers in the mucosa and soft tissues,25,30 paresthesia, or even numbness of the associated branch of the trigeminal nerve.31 Signs and symptoms may appear before osteonecrosis becomes clinically noticeable.25,32
Table 2 shows the clinical signs and symptoms of Bisphosphonate-related osteonecrosis of the jaw (BRONJ). Most cases of BRONJ undergo conservative treatment; the treatment regimen includes improving and maintaining oral hygiene, removing dental and periodontal disease, mouthwashes with local antibiotics, and systemic antibiotics.29 In unresponsive cases, surgical management should be considered; ostectomy of the affected bone should be continued until normal bone is observed.29
Table 2.
Clinical signs and symptoms of Bisphosphonate-related osteonecrosis of the jaw (BRONJ).
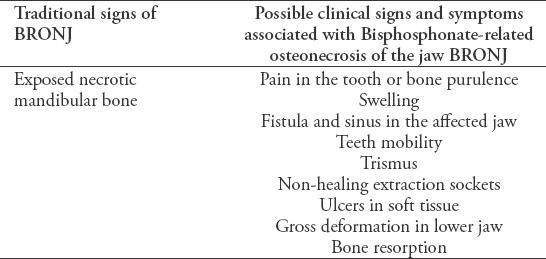
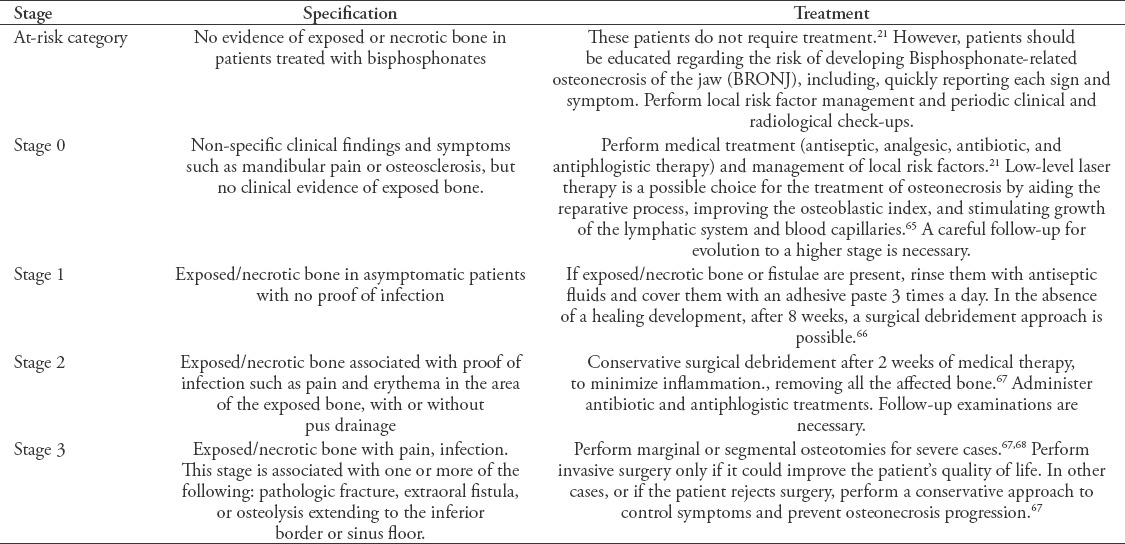
Table 3 shows BRONJ staging systems and suggested treatments, according to the American Association of Oral and Maxillofacial Surgeons.33
Table 3.
Bisphosphonate-related osteonecrosis of the jaw staging systems according to the American Association of Oral and Maxillofacial Surgeons and suggested treatments.21
Endodontic clinical implications of bisphosphonates
Pulpal necrosis is the result of microorganism invasion into the root canal system, leading to infiltration and inflammation through the apical foramen, into the periapical tissues, causing an increase in osteoclastic activity and bone resorption.34,35
The activated inflammatory cells secrete multiple proteins, including cytokines (namely, interleukin 6 or TNF-a) and degrading proteins (namely, collagenase or proteinases) that interfere with healing.36 Bacterial endotoxins will activate the complement system, all these factors provoke the differentiation of macrophages into osteoclasts.37
The BPs target osteoclast-mediated bone resorption, and ultimately inhibit bone remodeling. This process can interfere with healing of periapical lesions following root canal treatment.38 The periapical lesions can be considered as predisposing factors that may aggravate the development of BRONJ, following tooth extraction.39
A recent animal study evaluated the role of periapical lesions in exacerbation of BP-related osteonecrosis of the jaw (BRONJ) following tooth extraction. This revealed the increasing occurrence of BP-related osteonecrosis following the extraction of teeth with periapical lesions, and pointed out that periapical lesions should be controlled before tooth extraction, to minimize the risk of BRONJ.39
Patients undergoing BP therapy are at a higher risk of developing BRONJ.40 Extraction of the affected teeth may trigger BRONJ. Dental extraction could be delayed or even avoided by performing root canal therapy in the affected teeth.41 Non-surgical root canal treatment, as an alternative to extraction, will decrease the risk of BRONJ incidence.38 The purpose of root canal therapy is to eliminate infection and prevent it from infiltrating into the periapical tissues.38 In a study, it was found that the healing rate of periapical lesions following root canal treatment in patients taking oral BPs for long time was 73.5%; and was not significantly difference than the healing rate of periapical lesions after root canal treatment in patients who did not use oral BPs (81.6%).38
The major limitation of the study was the small size of the sample. The evidence-quality of that study was moderate. Therefore, this subject requires further research to explain the relationship between endodontic treatment and the effects on patients undergoing BP therapy.42 A recent study evaluated the effect of IV zolendronate on the clinical and radiographic success of non-surgical root canal treatment. The results of this study revealed a strong relationship between the duration of BP treatment and the success of root canal treatment, where the success rate increased in patients with shorter BP treatment durations (less than 1 year).43 Also, the major limitation of the study was a small sample size, and observation period was only 12 months. Further studies are needed on this subject. Most patients reported to have BRONJ have had a history of chemotherapy or dexamethasone use.44 The other risk factors of BRONJ are intraoral trauma, alcohol/tobacco use, and preexisting periodontal disease.44
Root canal therapy can trigger the process of BRONJ through soft tissue damage, especially during application of a rubber dam and apical extrusion of debris during cleaning and shaping of the root canal system.45 Patel and Saberi46 described case series of external cervical resorption in patients taking BPs, where there was no other possible cause of resorption. Amino-containing BPs could cause an acute-phase response and release of proinflammatory cytokines, which appears to be associated with the release of tumor necrosis factor-alpha (TNF-α), Interleukin-1 (IL-1), and IL6;46 this may initiate external cervical resorption in teeth.46 In rats, the local application of BPs causes an increasing of IL-1 and TNF- α activity which lead to increasing of odontoclast numbers.47 Animal studies revealed that the superficial application of zoledronate and alendronate decreased replacement root resorption in intentional replanted teeth.48,49 The low concentrations of alendronate could inhibit the receptor activator of nuclear factor kappa-β ligand (RANKL) of generated osteoclasts without cytotoxic influences.49 The clinical importance of these in vitro findings are not known; further studies must be conducted to prove its clinical capability as a therapeutic procedure for avulsion teeth.
Open apex teeth with pulpal necrosis provides a great challenge to dental practitioners; however, recent years have witnessed a new concept for management of these cases which is called “revascularization.”50 This concept, based on disinfecting the root canal system and inducing intracanal bleeding through the apical foramen creates a suitable atmosphere for endogenous mesenchymal stem cells (MSCs) to differentiate to several type of odontogenic cells and complete root maturity.50 The root canal revascularization procedures include induction of intracanal bleeding through the apical foramen by over instrumentation, and this may trigger BRONJ. Therefore, the treatments of choice in these cases are apexification or apexogenesis.
Clinical recommendations
The following recommendations could reduce the risk of BRONJ during endodontic treatment.51
Informed consent and communication with the patient’s treating physician are the first and most essential steps before any procedure.
A chlorhexidine mouthwash rinse for one minute, before starting treatment, reduces the number of microorganisms in the oral cavity,52 and minimizes the possibility of bacteremia that may be present due to soft tissue trauma.
Avoid using anesthetic agents with vasoconstrictors53 to reduce the risk of inadequate vascularization, as BPs already have anti-angiogenic effects.54
Minimize trauma, particularly to the soft tissues, during rubber dam clamp application.45
Perform the work in a strictly aseptic environment. Disinfect the tooth and the rubber dam by rubbing them with a suitable disinfecting solution for 2 minutes.51 Tincture of iodine (5%) has proved to be one of the few reliable agents for disinfecting rubber dam and tooth surfaces during the preparation of an aseptic endodontic workfield.55
Avoid patency of the apical foramen, which can increase the possibility of bacteremia from extruded debris.51 Electronic apex locators are used to determine the apical constriction. Therefore, it may be recommended to use the electronic apex locators during cleaning and shaping to maintained the files at apical constriction and prevent it from apical extrusion.56
During root canal shaping, use Nickle Titanium (NiTi) rotary systems and avoid reciprocating systems, which may cause more extrusion of debris.57
Apply obturation techniques with minimum risks of overfilling and overextension, to increase the efficiency of root canal treatment58 and reduce the possibility of periapical tissue irritation.59 The cold lateral compaction technique minimizes the risk of apical overfilling of the root canal compared to warm root filling techniques.60
High-risk patients include those under IV or oral BP therapy for more than 3 years and patients presenting systemic issues (such as chronic kidney disease, diabetes, and corticosteroid therapy), who require care.21,61
Prophylactic antibiotic use in patients treated with BPs before a nonsurgical root canal has not achieved consensus.62 We recommend prophylactic antibiotics in the following cases:51,63,64 necrotic pulps in patients undergoing IV BPs treatment, patients treated with oral BPs more than 3 years, and patients with several teeth requiring root canal treatment. It is preferred to schedule all the treatments during a single visit, to limit the dosage of antibiotic prophylaxis to a single regime.
In conclusion, BPs are essential medications for osteoporosis treatment. As with any other drug, BPs have their own side effects. Patients on BP therapy are at a high risk of developing BRONJ. Extraction of the affected teeth may trigger BRONJ. Non-surgical root canal therapy, as an alternative to extraction, will decrease the risk of BRONJ incidence, eliminate the infection, and prevent it from infiltrating into periapical tissues. There are special preventive measures, which should be followed strictly to reduce the risk of BRONJ during endodontic treatment: the work should be performed in a strictly aseptic environment with minimum trauma, prophylactic antibiotics are recommended for necrotic pulp in patients undergoing IV BPs treatment, patients treated with oral BPs more than 3 years, and patients with several teeth requiring root canal treatment. It is preferred to schedule all the treatments during a single visit, to limit the dosage of antibiotic prophylaxis to a single regime.
Footnotes
References
- 1.Reyes C, Hitz M, Prieto-Alhambra D, Abrahamsen B. Risks and benefits of bisphosphonate therapies. J Cell Biochem. 2016;117:20–28. doi: 10.1002/jcb.25266. [DOI] [PubMed] [Google Scholar]
- 2.Khajuria DK, Razdan R, Mahapatra DR. Drugs for the management of osteoporosis: a review. Rev Bras Reumatol. 2011;51:379–382. [PubMed] [Google Scholar]
- 3.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017;12:43. doi: 10.1007/s11657-017-0324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jobke B, Milovanovic P, Amling M, Busse B. Bisphosphonate-osteoclasts: changes in osteoclast morphology and function induced by antiresorptive nitrogen-containing bisphosphonate treatment in osteoporosis patients. Bone. 2014;59:37–43. doi: 10.1016/j.bone.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 6.Sun Y, Chen L, Wu X, Ding Q. Bifunctional bisphosphonate derivatives and platinum complexes with high affinity for bone hydroxyapatite. Bioorg Med Chem Lett. 2017;27:1070–1075. doi: 10.1016/j.bmcl.2016.12.050. [DOI] [PubMed] [Google Scholar]
- 7.McClung M, Harris ST, Miller PD, Bauer DC, Davison KS, Dian L, et al. Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med. 2013;126:13–20. doi: 10.1016/j.amjmed.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 8.Khan M, Cheung AM, Khan AA. Drug-related adverse events of osteoporosis therapy. Endocrinol Metab Clin North Am. 2017;46:181–192. doi: 10.1016/j.ecl.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Popp A, Senn R, Curkovic I, Senn C, Buffat H, Popp P, et al. Factors associated with acute-phase response of bisphosphonate-naïve or pretreated women with osteoporosis receiving an intravenous first dose of zoledronate or ibandronate. Osteoporos Int. 2017;6:1995–2002. doi: 10.1007/s00198-017-3992-5. [DOI] [PubMed] [Google Scholar]
- 10.Sharma A, Chatterjee S, Arbab-Zadeh A, Goyal S, Lichstein E, Ghosh J, et al. Risk of serious atrial fibrillation and stroke with use of bisphosphonates: evidence from a meta-analysis. Chest Journal. 2013;144:1311–1122. doi: 10.1378/chest.13-0675. [DOI] [PubMed] [Google Scholar]
- 11.Herrera L, Leal I, Lapi F, Schuemie M, Arcoraci V, Cipriani F, et al. Risk of atrial fibrillation among bisphosphonate users: a multicenter, population-based, Italian study. Osteoporos Int. 2015;26:1499. doi: 10.1007/s00198-014-3020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright E, Schofield PT, Molokhia M. Bisphosphonates and evidence for association with esophageal and gastric cancer: a systematic review and meta-analysis. BMJ Open. 2015;5:e007133. doi: 10.1136/bmjopen-2014-007133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vinogradova Y, Coupland C, Hippisley-Cox J. Exposure to bisphosphonates and risk of gastrointestinal cancers: series of nested case-control studies with QResearch and CPRD data. BMJ. 2013;346:f114. doi: 10.1136/bmj.f114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel DV, Bolland M, Nisa Z, Al-Abuwsi F, Singh M, Horne A, et al. Incidence of ocular side effects with intravenous zoledronate: secondary analysis of a randomized controlled trial. Osteoporos Int. 2015;26:499–503. doi: 10.1007/s00198-014-2872-5. [DOI] [PubMed] [Google Scholar]
- 15.Pirbhai A, Rajak SN, Goold LA, Cunneen TS, Wilcsek G, Martin P, et al. Bisphosphonate-induced orbital inflammation: a case series and review. Orbit. 2015;34:331–335. doi: 10.3109/01676830.2015.1078380. [DOI] [PubMed] [Google Scholar]
- 16.Rappoport D, Leiba H. Bisphosphonates and ocular inflammation. Harefuah. 2017;156:71–73. [PubMed] [Google Scholar]
- 17.Nogués X, Prieto-Alhambra D, Güerri-Fernández R, Garcia-Giralt N, Rodriguez-Morera J, Cos L, et al. Fracture during oral bisphosphonate therapy is associated with deteriorated bone material strength index. Bone. 2017;103:64–69. doi: 10.1016/j.bone.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Phillips HK, Harrison SJ, Akrawi H, Sidhom SA. Retrospective review of patients with atypical bisphosphonate related proximal femoral fractures. Injury. 2017;48:1159–1164. doi: 10.1016/j.injury.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 19.Sivolella S, Lumachi F, Stellini E, Favero L. Denosumab and anti-angiogenetic drug-related osteonecrosis of the jaw: an uncommon but potentially severe disease. Anticancer Res. 2013;33:1793–1797. [PubMed] [Google Scholar]
- 20.Fung P, Bedogni G, Bedogni A, Petrie A, Porter S, Campisi G, et al. Time to onset of bisphosphonate-related osteonecrosis of the jaws: a multicentre retrospective cohort study. Oral Dis. 2017;23:477–483. doi: 10.1111/odi.12632. [DOI] [PubMed] [Google Scholar]
- 21.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw-2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 22.López-Cedrún J, Sanromán J, García A, Peñarrocha M, Feijoo J, Limeres J, et al. Oral bisphosphonate-related osteonecrosis of the jaws in dental implant patients: a case series. Br J Oral Maxillofac Surg. 2013;51:874–879. doi: 10.1016/j.bjoms.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 23.Soydan SS, Uckan S. Management of bisphosphonate-related osteonecrosis of the jaw with a platelet-rich fibrin membrane: technical report. J Oral Maxillofac Surg. 2014;72:322–326. doi: 10.1016/j.joms.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 24.Williams DW, Lee C, Kim T, Yagita H, Wu H, Park S, et al. Impaired bone resorption and woven bone formation are associated with development of osteonecrosis of the jaw-like lesions by bisphosphonate and anti–receptor activator of NF-kB ligand antibody in mice. Am J Pathol. 2014;184:3084–3093. doi: 10.1016/j.ajpath.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharma D, Ivanovski S, Slevin M, Hamlet S, Pop TS, Brinzaniuc K, et al. Bisphosphonate-related osteonecrosis of jaw (BRONJ): diagnostic criteria and possible pathogenic mechanisms of an unexpected anti-angiogenic side effect. Vasc Cell. 2013;5:1. doi: 10.1186/2045-824X-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoshiga D, Nakamichi I, Yamashita Y, Yamamoto N, Yamauchi K, Nogami S, et al. Prognosis factors in the treatment of bisphosphonate-related osteonecrosis of the jaw - prognostic factors in the treatment of BRONJ. J Clin Exp Dent. 2014;6:e22–e28. doi: 10.4317/jced.51213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grisar K, Schol M, Schoenaers J, Dormaar T, Coropciuc R, Vander Poorten V, et al. Osteoradionecrosis and medication-related osteonecrosis of the jaw: similarities and differences. Int J Oral Maxillofac Surg. 2016;45:1592–1599. doi: 10.1016/j.ijom.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 28.Thumbigere-Math V, Michalowicz BS, Hodges JS, Tsai ML, SInson KK, RockIll L, et al. Periodontal disease as a risk factor for bisphosphonate-related osteonecrosis of the jaw. J Periodontol. 2014;85:226–233. doi: 10.1902/jop.2013.130017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, et al. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015;30:3–23. doi: 10.1002/jbmr.2405. [DOI] [PubMed] [Google Scholar]
- 30.Lu SY, Liang CC, Lin LH. Retrospective analysis of 27 cases of bisphosphonate-related osteonecrosis of the jaw treated surgically or nonsurgically. J Dent Sci. 2014;9:185–194. [Google Scholar]
- 31.Zadik Y, Benoliel R, Fleissig Y, Casap N. Painful trigeminal neuropathy induced by oral bisphosphonate-related osteonecrosis of the jaw: a new etiology for the numb-chin syndrome. Quintessence Int. 2012;43:97–104. [PubMed] [Google Scholar]
- 32.Thayer M. Radiographic evidence of treatment with bisphosphonates. British Dental Journal. 2017;222:507. doi: 10.1038/sj.bdj.2017.307. [DOI] [PubMed] [Google Scholar]
- 33.Rosella D, Papi P, Giardino R, Cicalini E, Piccoli L, Pompa G. edication-related osteonecrosis of the jaw: Clinical and practical guidelines. Journal of International Society of Preventive & Community Dentistry. 2016;6:97. doi: 10.4103/2231-0762.178742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belibasakis G, Rechenberg D, Zehnder M. The receptor activator of NF-kB ligand-osteoprotegerin system in pulpal and periapical disease. Int Endod J. 2013;46:99–111. doi: 10.1111/j.1365-2591.2012.02105.x. [DOI] [PubMed] [Google Scholar]
- 35.Aw V. Discuss the role of microorganisms in the aetiology and pathogenesis of periapical disease. Aust Endod J. 2016;42:53–59. doi: 10.1111/aej.12159. [DOI] [PubMed] [Google Scholar]
- 36.Martins VL, Caley M, O'Toole EA. Matrix metalloproteinases and epidermal wound repair. Cell Tissue Res. 2013;351:255–268. doi: 10.1007/s00441-012-1410-z. [DOI] [PubMed] [Google Scholar]
- 37.Ricucci D, Siqueira JF, Loghin S, Lin LM. Repair of extensive apical root resorption associated with apical periodontitis: radiographic and histologic observations after 25 years. J Endod. 2014;40:1268–1274. doi: 10.1016/j.joen.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Hsiao A, Glickman G, He J. A retrospective clinical and radiographic study on healing of periradicular lesions in patients taking oral bisphosphonates. J Endod. 2009;35:1525–1528. doi: 10.1016/j.joen.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 39.Song M, Alshaikh A, Kim T, Kim S, Dang M, Mehrazarin S, et al. Preexisting periapical inflammatory condition exacerbates tooth extraction–induced bisphosphonate-related osteonecrosis of the jaw lesions in mice. J Endod. 2016;42:1641–1646. doi: 10.1016/j.joen.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gupta S, Gupta H, Mandhyan D, Srivastava S. Bisphophonates related osteonecrosis of the jaw. Natl J Maxillofac Surg. 2013;4:151. doi: 10.4103/0975-5950.127643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kyrgidis A, Arora A, Lyroudia K, Antoniades K. Root canal therapy for the prevention of osteonecrosis of the jaws: An evidence-based clinical update. Aust Endod J. 2010;36:130–133. doi: 10.1111/j.1747-4477.2010.00280.x. [DOI] [PubMed] [Google Scholar]
- 42.Aminoshariae A, Kulild JC, Mickel A, Fouad AF. Association between Systemic Diseases and Endodontic Outcome: A Systematic Review. J Endod. 2017;43:514–519. doi: 10.1016/j.joen.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 43.Dereci Ö, Orhan EO, Irmak Ö, Ay S. The effect of the duration of intravenous zolendronate medication on the success of non-surgical endodontic therapy: a retrospective study. Bmc Oral Health. 2016;16:6–9. doi: 10.1186/s12903-016-0163-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tardast A, Sjöman R, Løes S, Abtahi J. Bisphosphonate associated osteomyelitis of the jaw in patients with bony exposure: prevention, a new way of thinking. J Appl Oral Sci. 2015;23:310–314. doi: 10.1590/1678-775720140506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gallego L, Junquera L, Pelaz A, Díaz-Bobes C. Rubber dam clamp trauma during endodontic treatment: a risk factor of bisphosphonate-related osteonecrosis of the jaw? J Oral Maxillofac Surg. 2011;69:e93–e95. doi: 10.1016/j.joms.2010.06.197. [DOI] [PubMed] [Google Scholar]
- 46.Patel S, Saberi N. External cervical resorption associated with the use of bisphosphonates: a case series. J Endod. 2015;41:742–748. doi: 10.1016/j.joen.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 47.Putranto R, Oba Y, Kaneko K, Shioyasono A, Moriyama K. Effects of bisphosphonates on root resorption and cytokine expression during experimental tooth movement in rats. Orthodontic Waves. 2008;67:141–149. [Google Scholar]
- 48.Najeeb S, Siddiqui F, Khurshid Z, Zohaib S, Zafar MS, Ansari SA. Effect of bisphosphonates on root resorption after tooth replantation. A systematic review. Dent Traumatol. 2017;33:77–83. doi: 10.1111/edt.12316. [DOI] [PubMed] [Google Scholar]
- 49.Martins CA, Leyhausen G, Volk J, Geurtsen W. Effects of alendronate on osteoclast formation and activity in vitro. J Endod. 2015;41:45–49. doi: 10.1016/j.joen.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Alrahabi MK, Ali MM. Root canal revascularization. Saudi Med J. 2014;35:429–434. [PubMed] [Google Scholar]
- 51.Parm M. Case selection and treatment planning. In: Lhb KMH, editor. Cohen's Pathways of the Pulp. 11th ed. Amsterdam: Elsevier Inc; 2016. pp. 71–89. [Google Scholar]
- 52.Choi SE, Kim HS. Sodium bicarbonate solution versus chlorhexidine mouthwash in oral care of acute leukemia patients undergoing induction chemotherapy: a randomized controlled trial. Asian Nurs Res. 2012;6:60–66. doi: 10.1016/j.anr.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 53.Fedele S, Kumar N, Davies R, Fiske J, Greening S, Porter S. Dental management of patients at risk of osteochemonecrosis of the jaws: a critical review. Oral Diseases. 2009;15:527–537. doi: 10.1111/j.1601-0825.2009.01581.x. [DOI] [PubMed] [Google Scholar]
- 54.Zhang X, Hamadeh IS, Song S, Katz J, Moreb JS, Langaee TY, et al. Osteonecrosis of the Jaw in the United States Food and Drug Administration's Adverse Event Reporting System (FAERS) J Bone Miner Res. 2016;31:336–340. doi: 10.1002/jbmr.2693. [DOI] [PubMed] [Google Scholar]
- 55.Peters O.A, Cip B. Basrani Cleaning and Shaping of the Root Canal System. In: Hargreaves K, editor. Cohen's Pathways of the Pulp. 11th ed. Amsterdam: Elsevier Inc; 2011. pp. 209–79. [Google Scholar]
- 56.Connert T, Judenhofer MS, Hülber JM, Schell S, Mannheim JG, Pichler BJ, et al. Evaluation of the accuracy of nine electronic apex locators by using Micro-CT. International Endodontic Journal. 2018;51:223–232. doi: 10.1111/iej.12814. [DOI] [PubMed] [Google Scholar]
- 57.Bürklein S, Schäfer E. Apically extruded debris with reciprocating single-file and full-sequence rotary instrumentation systems. J Endod. 2012;38:850–852. doi: 10.1016/j.joen.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 58.Vivekanandhan P, Subbiya A, Mitthra S, Karthick A. Comparison of apical debris extrusion of two rotary systems and one reciprocating system. Journal of Conservative Dentistry. 2016;19:245. doi: 10.4103/0972-0707.181941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scelza M, Linhares A, Da Silva L, Granjeiro J, Alves G. A multiparametric assay to compare the cytotoxicity of endodontic sealers with primary human osteoblasts. Int Endod J. 2012;45:12–18. doi: 10.1111/j.1365-2591.2011.01941.x. [DOI] [PubMed] [Google Scholar]
- 60.Moeller L, Wenzel A, Wegge-Larsen A, Ding M, Kirkevang L. Quality of root fillings performed with two root filling techniques. An in vitro study using micro-CT. Acta Odontol Scand. 2013;71:689–696. doi: 10.3109/00016357.2012.715192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, Clarke BL, Clines GA, et al. Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31:16–35. doi: 10.1002/jbmr.2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Katz H. Endodontic implications of bisphosphonate-associated osteonecrosis of the jaws: a report of three cases. J Endod. 2005;31:831–834. doi: 10.1097/01.don.0000186481.96169.cd. [DOI] [PubMed] [Google Scholar]
- 63.Bermúdez-Bejarano EB, Serrera-Figallo MÁ, Gutiérrez-Corrales A, Romero-Ruiz MM, Castillo-de-Oyagüe R, Gutiérrez-Pérez JL, et al. Prophylaxis and antibiotic therapy in management protocols of patients treated with oral and intravenous bisphosphonates. J Clin Exp Dent. 2017;9:e141. doi: 10.4317/jced.53372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.The American Association of Endodontists. AAE Position Statement AAE Guidance on the use of systemic antibiotics in endodontics. J Endod. 2017;43:1409–1413. doi: 10.1016/j.joen.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 65.Latifyan S, Genot M, Klastersky J. Bisphosphonate-related osteonecrosis of the jaw: a review of the potential efficacy of low-level laser therapy. Supportive Care Cancer. 2016;24:3687–3693. doi: 10.1007/s00520-016-3139-9. [DOI] [PubMed] [Google Scholar]
- 66.Ristow O, Otto S, Troeltzsch M, Hohlweg-Majert B, Pautke C. Treatment perspectives for medication-related osteonecrosis of the jaw (MRONJ) J Craniomaxillofac Surg. 2015;43:290–293. doi: 10.1016/j.jcms.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 67.Rugani P, Acham S, Kirnbauer B, Truschnegg A, Obermayer-Pietsch B, Jakse N. Stage-related treatment concept of medication-related osteonecrosis of the jaw--a case series. Clin Oral Investig. 2015;19:1329. doi: 10.1007/s00784-014-1384-1. [DOI] [PubMed] [Google Scholar]
- 68.Pompa G, Bignozzi I, Cristalli M, Quaranta A, Di Carlo S, Annibali S. Bisphosphonate and osteonecrosis of the jaw: The oral surgeon's perspective. London (UK): SAGE Publications Sage; 2012. [Google Scholar]


