Abstract
Background
Clinical observations and results from recent studies support the use of non-invasive vagus nerve stimulation (nVNS) for treating cluster headache (CH) attacks. This study compared nVNS with a sham device for acute treatment in patients with episodic or chronic CH (eCH, cCH).
Methods
After completing a 1-week run-in period, subjects were randomly assigned (1:1) to receive nVNS or sham therapy during a 2-week double-blind period. The primary efficacy endpoint was the proportion of all treated attacks that achieved pain-free status within 15 minutes after treatment initiation, without rescue treatment.
Results
The Full Analysis Set comprised 48 nVNS-treated (14 eCH, 34 cCH) and 44 sham-treated (13 eCH, 31 cCH) subjects. For the primary endpoint, nVNS (14%) and sham (12%) treatments were not significantly different for the total cohort. In the eCH subgroup, nVNS (48%) was superior to sham (6%; p < 0.01). No significant differences between nVNS (5%) and sham (13%) were seen in the cCH subgroup.
Conclusions
Combing both eCH and cCH patients, nVNS was no different to sham. For the treatment of CH attacks, nVNS was superior to sham therapy in eCH but not in cCH. These results confirm and extend previous findings regarding the efficacy, safety, and tolerability of nVNS for the acute treatment of eCH.
Keywords: Episodic cluster headache, chronic cluster headache, non-invasive vagus nerve stimulation, acute treatment, neuromodulation, randomized controlled trial
Introduction
Cluster headache (CH) is a primary headache disorder characterized by recurrent attacks of very severe unilateral headache accompanied by restlessness and cranial autonomic symptoms (1). CH is classified as either episodic (eCH), with attack periods lasting between 1 week and 1 year, and separated by ≥1 month, or chronic (cCH), with attack periods of ≥1 year without remission or with remission lasting <1 month (2). Widely regarded as one of the most painful medical conditions, CH can also profoundly disturb quality of life by limiting patients’ functionality in work-related, domestic, and social activities (3).
Ideal acute therapy for CH attacks should provide rapid symptom relief with minimal adverse events. Evidence-based recommendations for acute CH therapy include the use of subcutaneous (4)/intranasal triptans (5,6) or inhaled oxygen (7). Although effective, these treatments have shortcomings. Triptans are relatively contraindicated in patients with cardiovascular disease (8). While inhaled oxygen is recommended in Europe (9), patient access varies by country across the European Union.
Vagus nerve stimulation (VNS), a well-established neuromodulation treatment for epilepsy (10) and medication-resistant depression (11), has been successfully used open label in CH (12,13). Historically, approved VNS devices were surgically implanted, while more recently, non-invasive VNS methods have been designed to avoid the risks of invasive approaches. gammaCore® was developed as a non-invasive vagus nerve stimulation (nVNS) device for transcutaneous stimulation of the cervical branch of the vagus nerve (14). ACT1 was a randomized, double-blind, sham-controlled study conducted in the United States (15). It demonstrated that nVNS as acute treatment produced a therapeutic response within 15 minutes and pain relief that was sustained through 60 minutes in patients with eCH (15). The new study, ACT2, also compared nVNS and a sham device with respect to efficacy and safety in the acute treatment of eCH and cCH. This trial was undertaken to confirm and extend the results from ACT1 by examining additional clinical and patient-related endpoints in a European setting. The primary outcome has been reported (American Headache Society 59th Annual Scientific Meeting; 10 June 2017, Boston, MA) (16).
Methods
Study design and participants
This pivotal, randomized, double-blind, sham-controlled prospective study (NCT01958125) was conducted in four European countries at nine tertiary care sites, including academic medical centers and headache/pain/neurology clinics, between September 10, 2013, and October 14, 2014. It consisted of a 1-week run-in period; a 2-week, randomized, double-blind period during which subjects were treated with either nVNS or a sham device; and a 2-week, open-label period wherein all subjects received nVNS therapy. The study was conducted in compliance with applicable regulatory requirements and ethical principles in the latest revision of the Declaration of Helsinki. An independent ethics committee approved the study protocol before subjects were enrolled at a site (see supplemental information for a list of independent ethics committees). All subjects provided written informed consent before participating.
Participants were required to be ≥18 years of age, have a diagnosis of eCH or cCH according to the International Classification of Headache Disorders (ICHD; second edition) criteria (17). They were to refrain from starting new treatment, or changing the dose of existing treatments, for CH during the run-in and double-blind periods. Individuals with eCH who were not in a bout at the time of screening and those who were pregnant, nursing or thinking of becoming pregnant during the study, or had an abnormal baseline electrocardiogram, were excluded. Other exclusion criteria are included in the supplemental information.
Interventions and procedures
During the run-in period, subjects maintained their established standard of care regimens. A standard design with a block size of 4 was used to randomly assign subjects to treatment with either nVNS or the sham device (1:1 ratio) in addition to their standard of care regimen during the double-blind period. Each site received sealed randomization envelopes imprinted with subject numbers. Subjects were enrolled in consecutive order at each site. Unblinded trainers provided subjects with the appropriate device, as indicated by their randomization envelope, and training on its use.
Stimulation details
The nVNS device produced a proprietary low-voltage signal to generate an electrical field to stimulate the vagus nerve: pulse width 200 µS, frequency 5 kHz, intensity maximum 24 V. By contrast, the sham device produced a low-frequency biphasic signal that could be felt as a variable tingling sensation but did not stimulate the vagus nerve (18). The nVNS and sham devices were otherwise identical in appearance, weight, visual and audible feedback, and user application. After applying a conductive gel to the device’s stimulation surfaces, subjects were instructed to self-administer three consecutive 120-second stimulations ipsilateral to their CH attack at the time of attack onset (Supplemental Figure 1). If the attack was not aborted within nine minutes after initiation of the first stimulation, three additional consecutive stimulations were allowed during a treatment session, in order to have an endpoint measurement at 15 minutes. Subjects were asked to refrain from using rescue treatments, that is, medications and/or inhaled oxygen, for 15 minutes after beginning stimulation. A minimum of six hours was required between treatment sessions.
Data collection
Subject baseline information was collected at screening (visit 1). Throughout the study, subjects used paper diaries to record all CH attacks, including pain intensity at onset and at 15 and 30 minutes after initiation of stimulation; rescue treatment use, number of stimulations used, and adverse events. Pain intensity was rated on a 5-point scale: 0, no pain to 4, very severe pain (19). During visit 2 (end of run-in period), randomized treatment was assigned. During visit 3 (end of double-blind period), initial devices were collected, new devices were distributed, and blinding assessments were completed.
Study endpoints
All efficacy endpoints were assessed for the total cohort and the eCH and cCH subgroups. The primary efficacy endpoint was the proportion of all treated attacks that achieved pain-free status (i.e. pain score of 0) within 15 minutes after treatment initiation. Secondary efficacy endpoints included the mean proportion of treated attacks per subject that achieved responder status (i.e. pain score of 0 or 1) within 30 minutes, mean proportion of treated attacks per subject that achieved pain-free status within 30 minutes, and mean change in pain intensity from attack onset to 15 and 30 minutes after treatment initiation. The proportions of subjects who achieved pain-free status and who achieved responder status in ≥50% of treated attacks at 15 minutes were evaluated as exploratory efficacy end points to allow parallel comparison with results from other studies. For all efficacy endpoints that involved pain-free/responder status, if rescue treatment was used at any point after initiation of stimulation for an attack, that attack was counted as a treatment failure (i.e. non-pain-free/non-responder). Only attacks for which no rescue treatment was used were included in the analysis of mean change in pain intensity.
The primary safety endpoint was the occurrence of adverse effects (AEs), including type, number, and relationship to the study device. Blinding was assessed by tallying responses when the subjects were asked to guess their treatment group assignment.
Statistical methods
The Full Analysis Set, defined as all subjects who had ≥1 post–run-in period efficacy assessment, was used for the primary, secondary, and exploratory efficacy analyses described here unless otherwise noted. Assuming a response probability of 0.3 for the sham group and 0.6 for the nVNS group, a sample size of 54 per group, including a 10% margin for dropout, was determined to provide 80% power with respect to the primary endpoint. All statistical analyses were performed using SAS® Software version 9.4. For demographic and baseline characteristics, quantitative variables were summarized via descriptive statistics. Qualitative variables were summarized via counts and percentages.
For the double-blind period, the primary efficacy endpoint was evaluated using generalized estimating equations with treatment group and study site as independent factors, except in the eCH subgroup analysis, which was not adjusted for study site. A type 3 test of fixed effects was conducted to evaluate the interaction between treatment group and CH subtype.
Mean proportions of treated attacks per subject that achieved responder status and that achieved pain-free status within 30 minutes were compared between treatment groups using the Wilcoxon rank sum test with stratification by study site. Mean changes in pain intensity between attack onset and subsequent time points were evaluated via 2-sided t tests. Proportions of subjects who achieved pain-free status for ≥50% of treated attacks and who achieved responder status for ≥ 50% of treated attacks at 15 minutes were assessed using the chi-square or Fisher exact test, as appropriate.
The safety population included all subjects who were randomly assigned and received ≥1 device stimulation. The following safety end points were tabulated by treatment group and summarized descriptively for each study period: subjects who had ≥1 AE, ≥1 adverse device effect (ADE), ≥1 AE leading to study discontinuation, and ≥1 serious adverse event (SAE). Blinding question responses were tabulated and summarized descriptively.
No outliers were identified. Data from prematurely withdrawn subjects were included in the analyses to the extent possible.
Results
Subjects
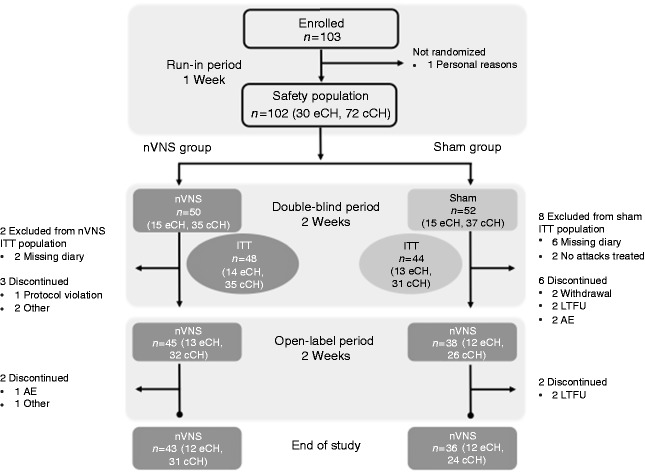
Demographic and baseline characteristics were generally similar between treatment groups (Table 1). Detailed subject disposition during the study is depicted in Figure 1. In total, 495 attacks were treated with active nVNS and 400 with sham.
Table 1.
Demographic and baseline characteristics (safety population).
| By treatment
group (n = 102) |
By
cohort (n = 102) |
|||
|---|---|---|---|---|
| Characteristic | nVNS (n = 50) | Sham (n = 52) | eCH (n = 30) | cCH (n = 72) |
| Age, mean (SD), y | 43.9 (10.6) | 46.9 (10.6) | 42.9 (12.7) | 46.5 (9.6) |
| Male, No. (%) | 35 (70.0) | 38 (73.1) | 22 (73.3) | 51 (70.8) |
| Ethnic origin, No. (%) | ||||
| White | 49 (98.0) | 52 (100.0) | 30 (100.0) | 71 (98.6) |
| Black | 0 | 0 | 0 | 0 |
| Asian | 1 (2.0) | 0 | 0 | 1 (1.4) |
| Duration of CH attacks during run-in period, mean (SD), min | 69.9 (68.7) | 77.4 (76.9) | 69.6 (83.3) | 76.1 (69.0) |
| CH type, No. (%) | ||||
| eCH | 15 (30.0) | 15 (28.8) | 30 (100.0) | 0 |
| cCH | 35 (70.0) | 37 (71.2) | 0 | 72 (100.0) |
| Number of attacks per week (median, min/max) | 10, 1–53 | 11, 2–39 | 10, 1–53 | 11, 2–39 |
| Medications used to manage CH, No. (%) | ||||
| Triptans | 37 (74.0) | 34 (65.3) | 19 (63.3) | 52 (72.2) |
| Oxygen | 27 (54.0) | 31 (59.6) | 20 (66.7) | 38 (52.8) |
| Mild analgesics | 7 (14.0) | 6 (11.5) | 2 (6.7) | 11 (15.3) |
| Narcotics | 3 (6.0) | 0 | 1 (3.3) | 2 (2.8) |
| Verapamil | 18 (36.0) | 23 (44.2) | 11 (36.7) | 30 (41.7) |
| Lithium | 4 (8.0) | 4 (7.7) | 1 (3.3) | 7 (9.7) |
| Propranolol | 1 (2.0) | 0 | 0 | 1 (1.4) |
| Tricyclic antidepressants | 2 (4.0) | 1 (1.9) | 1 (3.3) | 2 (2.8) |
| Serotonin receptor antagonists | 2 (4.0) | 2 (3.8) | 1 (3.3) | 3 (4.2) |
| Antiepileptics | 10 (20.0) | 6 (11.5) | 3 (10.0) | 13 (18.1) |
| Corticosteroids | 1 (2.0) | 2 (3.8) | 1 (3.3) | 2 (2.8) |
| Other | 5 (10.0) | 8 (15.4) | 4 (13.3) | 9 (12.5) |
| None | 0 | 5 (9.6) | 1 (3.3) | 4 (5.6) |
| One or more preventives | 32 (64.0) | 33 (63.4) | 15 (50.0) | 50 (69.5) |
Abbreviations: cCH: chronic cluster headache; CH: cluster headache; eCH: episodic cluster headache; nVNS; non-invasive vagus nerve stimulation; SD: standard deviation.
Figure 1.
Subject disposition.
Abbreviations: AE: adverse event; cCH: chronic cluster headache; eCH: episodic cluster headache; ITT: intent-to-treat; LTFU: lost to follow-up; nVNS: non-invasive vagus nerve stimulation.
Efficacy, double-blind period
Primary end point
The proportions of all treated attacks that achieved pain-free status within 15 minutes did not differ between the nVNS (14%) and sham (12%) groups in the total cohort (p = 0.71, Figure 2). There was a differential treatment effect between the eCH and cCH subgroups, as indicated by a type 3 test of fixed effects that revealed a significant interaction between treatment group and CH subtype (p = 0.04). In the eCH subgroup, a higher proportion of treated attacks achieved pain-free status with nVNS (48%) than with sham (6%; p < 0.01). No treatment difference for this end point was seen in the cCH subgroup (nVNS, 5%; sham, 13%; p = 0.13).
Figure 2.
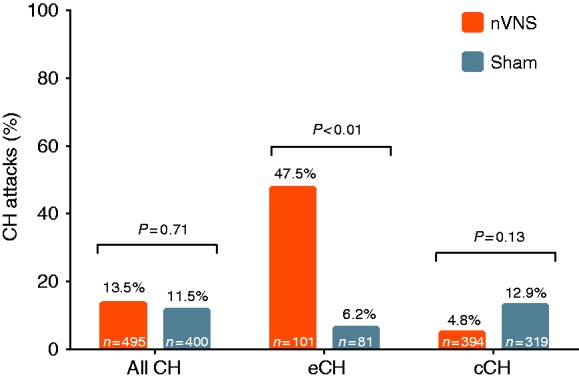
Proportions of all treated attacks that achieved pain-free status within 15 minutes (ITT population).
n Values denote the numbers of treated CH attacks; ORs (95% CIs) are 1.22 (0.42, 3.51) for all CH, 9.19 (1.77, 47.80) for eCH, and 0.41 (0.13, 1.30) for cCH. ORs and p values are from the generalized estimating equations model, which was adjusted for site in the total cohort and cCH subgroups but was not adjusted for site in the eCH subgroup. OR > 1 favors nVNS.
Abbreviations: cCH: chronic cluster headache; CH: cluster headache; CI: confidence interval; eCH: episodic cluster headache; ITT: intent-to-treat; nVNS: non-invasive vagus nerve stimulation; OR: odds ratio.
Secondary end points
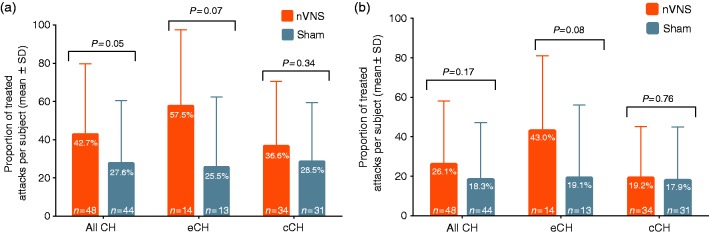
The mean proportion of treated attacks per subject that achieved responder status within 30 minutes was greater with nVNS (43%) than with sham (28%) for the total cohort (p = 0.05), but not for the eCH subgroup (nVNS, 58%; sham, 28%; p = 0.07) or the cCH subgroup (nVNS, 37%; sham, 29%; p = 0.34, Figure 3(a)). No significant differences between treatments were found for the mean proportion of treated attacks per subject that achieved pain-free status within 30 minutes (Figure 3(b)).
Figure 3.
Proportions of treated attacks per subject that achieved responder (a) or pain-free (b) status within 30 minutes (ITT population). (a) Responder status. Differences (±SE) between treatment groups are 15.1 (7.3) for all CH, 32.0 (15.0) for eCH, and 8.1 (8.1) for cCH. (b) Pain-free status. Differences (± SE) between treatment groups are 7.8 (6.4) for all CH, 23.9 (14.4) for eCH, and 1.3 (6.5) for cCH.
nValues denote numbers of patients; p values are from the Wilcoxon rank sum test stratified by study site.
Abbreviations: cCH: chronic cluster headache; CH: cluster headache; eCH: episodic cluster headache; ITT: intent-to-treat; nVNS: non-invasive vagus nerve stimulation; SD: standard deviation; SE: standard error.
Mean decreases in pain intensity from attack onset to the 15- and 30-minute time points were not significant with nVNS therapy in the total cohort. The differences between treatment groups reached significance in the eCH subgroup at both time points. There was no meaningful difference between treatment groups in the mean change in pain intensity for the cCH subgroup at either time point (Table 2).
Table 2.
| Time point | Treatment group | n | Attack-onset mean | Post–attack- onset mean | Change from attack onsetc |
|
|---|---|---|---|---|---|---|
| Mean (SE) | p valued | |||||
| All CH | ||||||
| 15 minutes | nVNS | 36 | 2.4 | 1.1 | −1.3 (0.2) | 0.06 |
| Sham | 31 | 2.1 | 1.2 | −0.9 (0.1) | ||
| 30 minutes | nVNS | 36 | 2.4 | 0.8 | −1.6 (0.2) | 0.07 |
| Sham | 31 | 2.1 | 0.9 | −1.2 (0.2) | ||
| eCH | ||||||
| 15 minutes | nVNS | 11 | 2.2 | 0.5 | −1.7 (0.4) | 0.01 |
| Sham | 8 | 1.6 | 1.0 | −0.6 (0.2) | ||
| 30 minutes | nVNS | 11 | 2.2 | 0.3 | −1.9 (0.4) | 0.03 |
| Sham | 8 | 1.6 | 0.9 | −0.8 (0.4) | ||
| cCH | ||||||
| 15 minutes | nVNS | 25 | 2.5 | 1.4 | −1.2 (0.2) | 0.52 |
| Sham | 23 | 2.3 | 1.3 | −1.0 (0.2) | ||
| 30 minutes | nVNS | 25 | 2.5 | 1.0 | −1.5 (0.2) | 0.50 |
| Sham | 23 | 2.3 | 0.9 | −1.3 (0.2) | ||
Rated on a 5-point pain scale (0 = none, 1 = mild, 2 = moderate, 3 = severe, 4 = very severe).
All patients in the safety population who had at least one treated attack for which rescue treatments were not used and had a pain score at attack onset and at the specified post–attack onset time periods were included in the analysis.
Calculated using the mean change (from attack onset to the time point of interest) in pain intensity for each subject. Only treated attacks without the use of rescue treatment were evaluated.
From 2-sided t tests.
Abbreviations: cCH: chronic cluster headache; CH: cluster headache; eCH: episodic cluster headache; nVNS: non-invasive vagus nerve stimulation; SE: standard error.
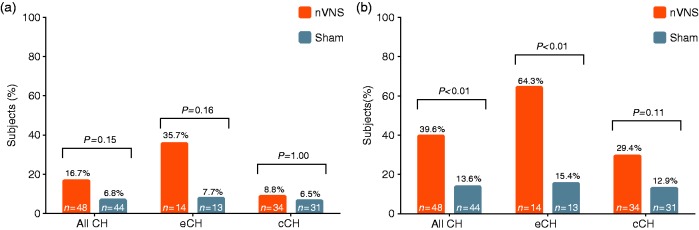
Exploratory end points
The proportions of subjects who achieved pain-free status in ≥50% of treated attacks at 15 minutes did not differ between treatment groups for the total cohort (nVNS, 17%; sham, 7%; p = 0.15), the eCH subgroup (nVNS, 36%; sham, 8%; p = 0.16), or the cCH subgroup (nVNS, 9%; sham, 7%; p = 1.00, Figure 4(a)). The proportion of subjects who achieved responder status for ≥50% of treated attacks at 15 minutes was higher with nVNS than with sham in the total cohort (nVNS, 40%; sham, 14%; p < 0.01) and the eCH subgroup (nVNS, 64%; sham, 15%; p < 0.01), but not in the cCH subgroup (nVNS, 29%; sham, 13%; p = 0.11; Figure 4(b)).
Figure 4.
Proportions of subjects who achieved pain-free (A) or responder (B) status in ≥50% of treated attacks at 15 minutes (ITT population). (a) Pain-free status. (b) Responder status.
p values were determined from the chi-square or Fisher’s exact test, as appropriate.
Abbreviations: cCH: chronic cluster headache; CH: cluster headache; eCH: episodic cluster headache; ITT: intent-to-treat; nVNS: non-invasive vagus nerve stimulation.
Efficacy, open-label period
The proportion of all treated attacks that achieved pain-free status within 15 minutes was 14% in the total cohort, 26% in the eCH subgroup, and 11% in the cCH subgroup during the open-label period. Interpretation of nVNS efficacy data from the open-label period was limited by changes in subjects’ prophylactic treatment regimens, which were allowed after completion of the double-blind period.
Safety and tolerability
AEs and Adverse Device Effects (ADEs) during the study are summarized in Supplemental Table 1. Twenty nVNS-treated subjects (40%) and 14 sham-treated subjects (27%) had ≥1 AE during the double-blind period, and 23 subjects (23%) had ≥1 AE during the open-label period. The proportion of subjects with ≥1 ADE was similar between the nVNS (18%) and sham (19%) groups during the double-blind period and was 12% during the open-label period. Two subjects reported four SAEs during the study, none of which were considered treatment related. One nVNS-treated subject had severe lower abdominal and back pain during the double-blind period, which resolved without intervention. One sham-treated subject reported severe depression and anxiety during the double-blind period. The subject discontinued from the study, and both SAEs resolved.
Blinding
Similar proportions of subjects in the nVNS (30%; Bang Blinding Index [95% CI], −0.08 [−0.242, 0.082]) and sham (39%; −0.18 [0.029, 0.338]) groups correctly guessed their treatment assignment.
Discussion
The data show that combining acute treatment outcomes in patients with eCH and cCH did not show an effect of nVNS. However, nVNS was superior to sham in patients with eCH for pain-free rates, responder rates, and decreases in pain intensity, while it was ineffective on all endpoints in cCH patients. These findings are consistent with those from open-label data (12,13) and ACT1 (15), which also demonstrated significant responses to nVNS in acute attacks in patients with eCH but not cCH. Taken together, the new data support the use of nVNS in the treatment of acute attacks in patients with eCH.
The mechanisms underlying the effects of VNS in treating headache have not been fully elucidated. In recent rat model studies of trigeminovascular nociception, VNS inhibited both spontaneous ongoing neuronal firing and firing in response to noxious dural or superior salivatory nucleus stimulation (20). These results suggest that the efficacy of VNS may involve modulation of nociceptive trigeminocervical neurons via direct projections and incitement of bilateral structures implicated in descending modulation of nociceptive inputs (20). These data are consistent with an important sensory afferent role for the vagus nerve (21,22), and of its central projections (23). Moreover, a role for vagal modulation in non-cranial pain has also been suggested by preclinical (24,25) and clinical studies (26). These data are certainly consistent with the results of the new study.
By definition, cCH involves attack periods of ≥1 year without remission or with remission lasting <1 month (2). A subset of patients with cCH may be refractory to prophylactic therapy after trials with several preventive options (27), which has led to invasive neuromodulatory approaches being considered (28,29). A consensus statement from the European Headache Federation has recommended appending the ICHD criteria to include a subclassification for refractory cCH (30). Considering the refractory nature of cCH, it is perhaps not surprising that patients with this subtype may be less likely than those with eCH to respond to acute therapies (13,15,31). Brain anatomy differs between patients with cCH, and both healthy individuals and patients with eCH (32), while pain and sensory thresholds studied with quantitative sensory testing are no different between eCH and cCH (33). Establishing causal links to chronicity is difficult, such differences may contribute to the disparity in treatment response for cCH and eCH. Further research comparing the CH subtypes, as well as patients with primary (i.e. de novo) cCH and cCH that evolves from eCH, is required to understand better the mechanisms involved in chronicity and whether these exist at disease onset or develop later in the disease process.
Individually, adjusted dosing could also influence treatment response in patients with cCH. During initial open-label exploratory investigations in CH, nVNS was used as both acute and preventive therapy, and dosing regimens were adjusted according to patient needs and responses to explore optimal treatment approaches (12). No differences in the efficacy of nVNS as acute or preventive therapy were apparent between eCH and cCH subtypes, although not all treatment outcomes were formally compared between the CH subtypes. Benefits of individually adjusted dosing in patients with cCH are also supported by findings from a retrospective review of nVNS in patients with treatment-refractory CH (34). Such results are from open-label studies, but are nevertheless pertinent given that sustained improvements were noted in several patients with CH that had been refractory to treatment.
Triptans, subcutaneous and intranasal, and inhaled oxygen are mainstays of acute therapy in CH owing to their efficacy (9). Such therapies are limited by dosing, tolerability, and practicality issues, and efforts to develop options to fill treatment gaps continue (35). Other neuromodulatory therapies, such as sphenopalatine ganglion stimulation (36,37), are becoming more established while the less recent approach of occipital nerve stimulation (28,38), has many practical challenges (39,40). In the current study, nVNS was safe and well tolerated. Rates of AEs were generally similar between the nVNS and sham groups, and no severe device-related AEs were reported. This profile, along with the clinical benefits demonstrated here and through previous research (15), suggests that nVNS is a safe, effective, well-tolerated treatment for patients with eCH. As a non-pharmacologic option, nVNS can be used alongside other treatments and can easily be incorporated into therapeutic regimens. This modality could be especially useful when acute treatment options are limited owing to AEs, risk of medication overuse and/or drug interactions, or delayed/inconsistent accessibility.
The potential for unblinding is an inherent concern in the study of any medical device (41). The issue was addressed here with a sham device that delivered a perceptible tingling sensation without stimulating the vagus nerve. Similar proportions of subjects in each group correctly guessed their treatment assignment, which suggests adequate blinding. Nevertheless, this study had limitations, including its short duration, which did not allow for evaluation of continued/change in response with long-term nVNS therapy. Some evidence suggests that patients who initially respond to nVNS as acute therapy for CH have a stable response with continued treatment (12). In epilepsy, long-term nVNS therapy has been associated with improved efficacy, which suggests possible disease-modifying effects (10). Such effects have yet to be substantiated in CH. Another study limitation was the imbalance between CH subtypes, with the eCH subgroup comprising <30% of subjects. This imbalance was probably due, in part, to the nature of the study sites (i.e. tertiary care centers) and the recruitment of subjects throughout the year rather than specifically when attack bouts are most common among patients with eCH, such as during seasonal transition periods (42). The stipulation that subjects’ preventive treatment regimens continue unchanged during the run-in and double-blind periods may have impeded enrollment of individuals with eCH, who may have opted to begin bridging therapies immediately rather than participate in the study. During the open-label period, subjects could alter their CH treatment regimens by adding prophylactic therapies, or changing doses of existing treatments, or both. This stipulation confounded the results, making it impossible to discern whether changes in efficacy outcomes were attributable to nVNS therapy or to other changes in treatment during this period. In addition, there is the possible bias of multiple attack treatment that we mitigate using the analytic technique, and with the secondary endpoints of treated attacks on a per subject basis. Moreover, a substantial number of attacks were treated in both arms, making multiple successful attack treatment by individuals an unlikely source of the positive outcome.
Results from this trial and prior studies underscore several potential advantages of nVNS. When used as an adjunct to a broad range of established standard of care regimens, nVNS was effective in patients with CH (13,15). In previous trials, nVNS therapy was associated with adherence rates ≥90% and treatment satisfaction rates ≥38% and was generally regarded as easy to use (12,13,15). These findings, along with the portability and flexibility of nVNS and the fact that it can be used multiple times per day, here up to four, in conjunction with virtually any other therapy, highlight its utility. The results of the current study align with prior observations suggesting the accrual of clinical benefits with long-term nVNS therapy (12,13,15).
Conclusions
In the ACT2 study, nVNS was superior to sham therapy for acute treatment of attacks in patients with eCH but not those with cCH or in the total population. nVNS was safe and well tolerated in all patients. These results confirm and extend findings from the previous ACT1 study (15) and demonstrate that nVNS is an effective acute attack treatment option for patients with eCH, with a favorable risk/benefit profile.
Clinical implications
In patients with episodic cluster headache (eCH) but not chronic cluster headache (cCH), acute use of non-invasive vagus nerve stimulation (nVNS) led to significantly higher pain-free rates, higher responder rates, and greater decreases in pain intensity than sham therapy did.
Non-invasive vagus nerve stimulation therapy was safe and well tolerated in all patients.
These results confirm those of previous studies, indicating that nVNS is a safe and effective treatment that can be used alongside other therapies in patients with eCH without increasing the risk for drug interactions or adverse events. The data do not support the acute use of nVNS in patients with cCH.
With its favorable risk/benefit profile, nVNS could fill a gap in the treatment of cluster headache (CH).
Supplementary Material
Acknowledgments
The authors would like to acknowledge Annelie Andersson of electroCore, LLC, who acted as sponsor representative/project leader; Candace K McClure of NAMSA, who provided statistical analysis support; and Elizabeth Barton of MedLogix Communications, LLC, who provided professional writing and editorial support under the direction of the authors.
ACT2 Study Group
Investigators are listed by study site at the time of the trial. Royal Free Hospital, London NHS Foundation Trust, London, UK: Peter J Goadsby (coordinating clinical investigator), Juana CA Marin (principal investigator); Migraine and Headache Clinic, Königstein, Germany: Charly Gaul (principal investigator); Leiden University Medical Centre, Leiden, the Netherlands: Michel D Ferrari (principal investigator); The Walton Centre for Neurology and Neurosurgery, Liverpool, UK: Nicolas Silver (principal investigator); Southern General Hospital (renamed Queen Elizabeth University Hospital Glasgow), Glasgow, UK: Alok Tyagi (principal investigator); Hull Royal Infirmary, Hull, UK: Fayyaz Ahmed (principal investigator); Glostrup Hospital, Glostrup, Denmark: Rigmor H Jensen (principal investigator); West German Headache Center, Essen, Germany: Kasja Solbach (principal investigator); University of Munich, Munich, Germany: Andreas Straube (principal investigator).
Author contributions
PJG, EL, JCAM, and MDF contributed to the design, execution, and analysis of the study and to the initial and final drafts of the manuscript. IFdC, NS, AT, FA, CG, RHJ, HCD, KR, and AS contributed to the execution and analysis of the study and to the initial and final drafts of the manuscript.
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: PJ Goadsby reports grants and personal fees from Allergan, Amgen, and Eli Lilly and Company; and personal fees from Akita Biomedical, Alder Biopharmaceuticals, Avanir Pharma, Cipla Ltd, Dr Reddy’s Laboratories, eNeura, Novartis, Pfizer Inc, Quest Diagnostics, Scion, Teva Pharmaceuticals, Trigemina Inc., Scion; and personal fees from MedicoLegal work, Journal Watch, Up-to-Date, Massachusetts Medical Society, Oxford University Press; and in addition, Dr. Goadsby has a patent Magnetic stimulation for headache assigned to eNeura. IF de Coo has received travel grants from electroCore, LLC. N Silver has received honoraria from Allergan and electroCore, LLC, and investigator fees paid to The Walton Centre. A Tyagi has received honoraria from Allergan, Inc., and electroCore, LLC. F Ahmed has nothing to disclose. C Gaul has received honoraria from Allergan; electroCore, LLC; Grünenthal; Desitin; Bayer; Boehringer Ingelheim; Autonomic Technologies; Reckitt Benckiser; Ratiopharm GmbH; Novartis; Lilly Deutschland; Teva and Hormosan. Dr. Gaul has no ownership interests and does not own any pharmaceutical company stocks. RH Jensen has given lectures and conducted clinical trials for Autonomic Technologies; electroCore, LLC; and Eli Lilly and Company. H-C Diener has received honoraria for participation in clinical trials and for contributions to advisory boards and oral presentations sponsored by Addex Pharma; Adler; Allergan; Almirall; Amgen; Autonomic Technologies; AstraZeneca; Bayer; Vital; Berlin-Chemie; Boehringer Ingelheim; Bristol-Myers Squibb; Chordate Medical; Coherex Medical; CoLucid Pharmaceuticals; electroCore, LLC; GlaxoSmithKline; Grünenthal; Janssen-Cilag; Labrys Biologics; Eli Lilly and Company; La Roche; 3M Medica; Medtronic; Menarini; Minster Pharmaceuticals; MSD; NeuroScore; Novartis; Johnson & Johnson; Pierre Fabre; Pfizer; Schaper and Brümmer; Sanofi; St. Jude Medical; and Weber & Weber. Dr. Diener has also received research funding from Allergan; Almirall; AstraZeneca; Bayer; electroCore, LLC; GlaxoSmithKline; Janssen-Cilag; MSD; and Pfizer. He has received additional research support from the German Research Council; the German Ministry of Education and Research; and the European Union. Dr. Diener has no ownership interests and does not own any pharmaceutical company stocks.K Solbach has received honoraria for oral presentations from Pharm-Allergan and Desitin GmbH. A Straube has received honoraria from Allergan; Berlin-Chemie; Desitin; MSD; Pfizer; electroCore, LLC; Boehringer Ingelheim; and St. Jude Medical. He has also received grants from the German Science Council; the German Secretary of Education; the Else Kröner-Fresenius Foundation; and the University of Munich. E Liebler is an employee of electroCore, LLC, and receives stock ownership. J Marin has received honoraria and travel grants from electroCore, LLC. MD Ferrari has received consultancy fees from Medtronic and research support from the Netherlands Organization for Scientific Research (NWO); the European Community; ZonMw; and the Dutch Heart Foundation. Dr. Ferrari is a member of the Editorial Board for Cephalalgia.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was sponsored by electroCore, LLC. Professional writing and editorial support from MedLogix Communications, funded by electroCore, LLC, was under the direction of the authors throughout draft development and revisions in accordance with the International Committee of Medical Journal Editors (ICMJE) criteria for authorship. Independent data analysis from North American Science Associates (NAMSA) and DZS Clinical Services was funded by electroCore, LLC.
References
- 1.Nesbitt AD, Goadsby PJ. Cluster Headache. Brit Med J 2012; 344: e2407–e2407. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013; 33: 629–808. [DOI] [PubMed] [Google Scholar]
- 3.D’Amico D, Rigamonti A, Solari A, et al. Health-related quality of life in patients with cluster headache during active periods. Cephalalgia 2002; 22: 818–821. [DOI] [PubMed] [Google Scholar]
- 4.The Sumatriptan Cluster Headache Study Group Treatment of acute cluster headache with sumatriptan. New Eng J Med 1991; 325: 322–326. [DOI] [PubMed] [Google Scholar]
- 5.Cittadini E, May A, Straube A, et al. Effectiveness of intranasal zolmitriptan in acute cluster headache. A randomized, placebo-controlled, double-blind crossover study. Arch Neurol 2006; 63: 1537–1542. [DOI] [PubMed] [Google Scholar]
- 6.Rapoport AM, Mathew NT, Silberstein SD, et al. Zolmitriptan nasal spray in the acute treatment of cluster headache: A double-blind study. Neurology 2007; 69: 821–826. [DOI] [PubMed] [Google Scholar]
- 7.Cohen AS, Burns B, Goadsby PJ. High flow oxygen for treatment of cluster headache. A randomized trial. JAMA 2009; 302: 2451–2457. [DOI] [PubMed] [Google Scholar]
- 8.Dodick D, Lipton RB, Martin V, et al. Consensus statement: Cardiovascular safety profile of triptans (5-HT1B/1D agonists) in the acute treatment of migraine. Headache 2004; 44: 414–425. [DOI] [PubMed] [Google Scholar]
- 9.May A, Leone M, Afra J, et al. EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias. Eur J Neurol 2006; 13: 1066–1077. [DOI] [PubMed] [Google Scholar]
- 10.Schachter SC. Vagus nerve stimulation therapy summary: Five years after FDA approval. Neurology 2002; 59: S15–S20. [DOI] [PubMed] [Google Scholar]
- 11.Yuan TF, Li A, Sun X, et al. Vagus nerve stimulation in treating depression: A tale of two stories. Curr Mol Med 2016; 16: 33–39. [DOI] [PubMed] [Google Scholar]
- 12.Nesbitt AD, Marin JCA, Tompkins E, et al. Initial experience with a novel non-invasive vagus nerve stimulation device for the treatment of cluster headache. Neurology (Minneap) 2015; 84: 1–5. [Google Scholar]
- 13.Gaul C, Diener HC, Silver N, et al. Non-invasive vagus nerve stimulation for PREVention and Acute treatment of chronic cluster headache (PREVA): A randomised controlled study. Cephalalgia 2016; 36: 534–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuan H, Silberstein SD. Vagus nerve and vagus nerve stimulation, a comprehensive review: Part II. Headache 2016; 56: 259–266. [DOI] [PubMed] [Google Scholar]
- 15.Silberstein SD, Mechtler LL, Kudrow DB, et al. Non-invasive vagus nerve stimulation for the ACute Treatment of cluster headache: Findings from the randomized, double-blind, sham-controlled ACT1 Study. Headache 2016; 56: 1317–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goadsby PJ, de Coo I, Silver N, et al. Non-invasive vagus nerve stimulation for the ACute Treatment of episodic and chronic cluster headache: Findings from the randomized, double-blind, sham-controlled ACT2 Study. Headache 2017; 57(Suppl 3): 128–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Headache Classification Committee of The International Headache Society. The International Classification of Headache Disorders (second edition). Cephalalgia 2004; 24: 1–160. [DOI] [PubMed] [Google Scholar]
- 18.Nonis R, D’Ostilio K, Schoenen J, et al. Evidence of activation of vagal afferents by non-invasive vagus nerve stimulation: An electrophysiological study in healthy volunteers. Cepahalalgia 2017; 37: 1285–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilgrim AJ. Methodology of clinical trials of sumatriptan in migraine and cluster headache. Eur Neurol 1991; 31: 295–299. [DOI] [PubMed] [Google Scholar]
- 20.Akerman S, Simon B, Romero-Reyes M. Vagus nerve stimulation suppresses acute noxious activation of trigeminocervical neurons in animal models of primary headache. Neurobiol Dis 2017; 102: 96–104. [DOI] [PubMed] [Google Scholar]
- 21.Foley JO, DuBois FS. Quantitative studies of the vagus nerve in the cat. J Comp Neurol 1937; 67: 49–67. [Google Scholar]
- 22.Agostoni E, Chinnock JE, De Daly MB, et al. Functional and histological studies of the vagus nerve and its branches to the heart, lungs and abdominal viscera in the cat. J Physiol 1957; 135: 182–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalia M, Mesulam MM. Brain stem projections of sensory and motor components of the vagus complex in the cat. II. Laryngeal, tracheobronchial, pulmonary, cardiac and gastrointestinal branches. J Comp Neurol 1980; 193: 467–508. [DOI] [PubMed] [Google Scholar]
- 24.Ren K, Randich A, Gebhart GF. Vagal afferent modulation of spinal nociceptive transmission in the rat. J Neurophysiol 1989; 62: 401–415. [DOI] [PubMed] [Google Scholar]
- 25.Ren K, Randich A, Gebhart GF. Electrical stimulation of cervical vagal afferents. I. Central relays for modulation of spinal nociceptive transmission. J Neurophysiol 1990; 64: 1098–1114. [DOI] [PubMed] [Google Scholar]
- 26.Kirchner A, Birklein F, Stefan H, et al. Left vagus nerve stimulation suppresses experimentally induced pain. Neurology 2000; 55: 1167–1171. [DOI] [PubMed] [Google Scholar]
- 27.Goadsby PJ, Schoenen J, Ferrari MD, et al. Towards a definition of intractable headache for use in clinical practice and trials. Cephalalgia 2006; 26: 1168–1170. [DOI] [PubMed] [Google Scholar]
- 28.Burns B, Watkins L, Goadsby PJ. Successful treatment of medically intractable cluster headache using occipital nerve stimulation (ONS). The Lancet 2007; 369: 1099–1106. [DOI] [PubMed] [Google Scholar]
- 29.Leone M, Franzini A, Cecchini AP, et al. Hypothalamic deep brain stimulation in the treatment of chronic cluster headache. Ther Adv Neurol Dis 2010; 3: 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitsikostas DD, Edvinsson L, Jensen RH, et al. Refractory chronic cluster headache: A consensus statement on clinical definition from the European Headache Federation. J Headache Pain 2014; 15: 79–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bahra A, Gawel MJ, Hardebo J-E, et al. Oral zolmitriptan is effective in the acute treatment of cluster headache. Neurology 2000; 54: 1832–1839. [DOI] [PubMed] [Google Scholar]
- 32.Naegel S, Holle D, Desmarattes N, et al. Cortical plasticity in episodic and chronic cluster headache. Neuro Clin 2014; 6: 415–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ladda J, Straube A, Forderreuther S, et al. Quantitative sensory testing in cluster headache: Increased sensory thresholds. Cephalalgia 2006; 26: 1043–1050. [DOI] [PubMed] [Google Scholar]
- 34.Marin J, Consiglio E, McClure C, et al. Non-invasive vagus nerve stimulation (nVNS) for treatment of cluster headache: Early UK clinical experience. Cephalalgia 2016; 26: 99–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pierson NS, Gelfand JM, Gelfabd A, et al. Influence of lumbar puncture volume on the incidence of post-dural puncture headaches. Headache 2016; 56(Suppl 1): 57–57. [Google Scholar]
- 36.Schoenen J, Jensen RH, Lanteri-Minet M, et al. Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment – Pathway CH-1: A randomized, sham-controlled study. Cephalalgia 2013; 33: 816–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jurgens TP, Barloese M, May A, et al. Long-term effectiveness of sphenopalatine ganglion stimulation for cluster headache. Cephalalgia 2017; 37: 423–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burns B, Watkins L, Goadsby PJ. Treatment of intractable chronic cluster headache by occipital nerve stimulation in 14 patients. Neurology 2009; 72: 341–345. [DOI] [PubMed] [Google Scholar]
- 39.Martelletti P, Jensen RH, Antal A, et al. Neuromodulation of chronic headaches: Position statement from the European Headache Federation. J Headache Pain 2013; 14: 86–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robbins MS, Starling AJ, Pringsheim TM, et al. Treatment of cluster headache: The American Headache Society evidence-based guidelines. Headache 2016; 56: 1093–1106. [DOI] [PubMed] [Google Scholar]
- 41.Asano E, Goadsby PJ. How do we fashion better trials for neurostimulator studies in migraine? Neurology 2013; 80: 694–694. [DOI] [PubMed] [Google Scholar]
- 42.Barloese M, Lund N, Petersen A, et al. Sleep and chronobiology in cluster headache. Cephalalgia 2015; 35: 969–978. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.