Abstract
Background
Sex, race, and insurance status are associated with treatment and outcomes in several cardiovascular diseases. These disparities, however, have not been well-studied in out-of-hospital cardiac arrest (OHCA).
Objective
Our objective was to evaluate the association of patient sex, race, and insurance status with hospital treatments and outcomes following OHCA.
Methods
We studied adult patients in the 2011–2015 California Office of Statewide Health Planning and Development (OSHPD) Patient Discharge Database with a “present on admission” diagnosis of cardiac arrest (ICD-9-CM 427.5). Insurance status was classified as private, Medicare, and MediCal/government/self-pay. Our primary outcome was good neurologic recovery at hospital discharge, which was determined by discharge disposition. Secondary outcomes were survival to hospital discharge, treatment at a 24/7 percutaneous coronary intervention (PCI) center, “do not resuscitate” orders within 24 hours of admission, and cardiac catheterization during hospitalization. Data were analyzed with hierarchical multiple logistic regression models.
Results
We studied 38,163 patients in the OSHPD database. Female sex, non-white race, and Medicare insurance status were independently associated with worse neurologic recovery [OR 0.94 (0.89–0.98), 0.93 (0.88–0.98), and 0.85 (0.79–0.91), respectively], lower rates of treatment at a 24/7 PCI center [OR 0.89 (0.85–0.93), 0.88 (0.85–0.93), and 0.87 (0.82–0.94), respectively], and lower rates of cardiac catheterization [OR 0.61 (0.57–0.65), 0.90 (0.84–0.97), and 0.44 (0.40–0.48), respectively]. Female sex, white race, and Medicare insurance were associated with DNR orders within 24 hours of admission [OR 1.16 (1.10–1.23), 1.14 (1.07–1.21), and 1.25 (1.15–1.36), respectively].
Conclusions
Sex, race, and insurance status were independently associated with post-arrest care interventions, patient outcomes and treatment at a 24/7 PCI center. More studies are needed to fully understand the causes and implications of these disparities.
Keywords: Cardiac arrest, Disparities, Sex differences
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is the leading cause of death from cardiovascular disease in the United States. Less than 10% of the approximately 350,000 adults who suffer OHCA each year in the United States survive to hospital discharge,1 and survival with good neurologic function is even more rare. Survival with good neurologic function following OHCA depends on immediate bystander recognition of OHCA, rapid prehospital care and effective post-cardiac arrest care. Current guidelines for post-arrest care recommend regionalized care at cardiac resuscitation centers with 24/7 percutaneous coronary intervention (PCI) capability; targeted temperature management for all arrest rhythms; cardiac catheterization for patients with suspected cardiac etiology and deferring prognostication for at least 72 hours post-arrest.2 Early “do not resuscitate” (DNR) orders within 24 hours of admission have been associated with fewer procedures and worse outcomes for post-OHCA patients.3
Outcome and treatment disparities with respect to age,4,5 sex,4,5 race5,6 and insurance status5,7–10 have been suggested for OHCA and acute myocardial infarction. However, these studies do not fully describe disparities in United States patient populations with OHCA. Furthermore, they do not address important prognostic events including in-hospital cardiac catheterization and early DNR orders. In this study, we used the California Office of Statewide Health Planning and Development (OSHPD) Patient Discharge Database to identify demographic and insurance factors associated with in-hospital treatments and outcomes among adults with OHCA. We hypothesized that female sex, non-white race and lack of private insurance would be associated with lower rates of good neurological recovery, survival to hospital discharge, treatment at a 24/7 PCI center, and cardiac catheterization; and higher rates of receiving a DNR order within 24 hours.
METHODS
We analyzed a retrospective cohort of adult patients in the OSHPD Patient Discharge Database. This study was approved by the California Committee for the Protection of Human Subjects and was exempt from review by our Institutional Review Board.
Population and Setting
California has a population of nearly 40 million people.11 The OSHPD Patient Discharge Database is a comprehensive data collection system for inpatient encounters in California. Per California Health and Safety Code Section 128736, all acute care hospitals in California (excluding Veterans Affairs and military facilities) must submit data for every inpatient encounter to OSHPD. These data do not represent a sample, but rather surveillance with 100% coverage. Each patient in the OSHPD Patient Discharge Database is assigned a record linkage number, which is a unique alphanumeric value based on the Social Security Number that allows multiple encounters from the same patient to be identified. In this study, we included all adult patients (≥18 years) in the OSHPD Patient Discharge Database with a “present on admission” diagnosis of cardiac arrest (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] 427.5) admitted from the emergency department to an acute care hospital from 1/1/2010 to 9/30/2015. We excluded patients with a length of stay over 60 days. We also excluded patients who were missing predictor variable(s) or outcome(s).
Experimental protocol
Patient-level data obtained from OSHPD included record linkage numbers, age, sex, race, ethnicity, insurance status, diagnosis codes (up to 25), present on admission codes, procedure codes (up to 21), survival to hospital discharge, discharge disposition, and receipt of a DNR order within 24 hours of admission. Insurance status categories were collapsed into private, Medicare, and Medi-Cal/other government/self-pay. Race was collapsed into white and non-white because each non-white race group contained a small number of patients. Ventricular fibrillation or ventricular tachycardia (VF/VT) rhythms and cardiac catheterization procedures were identified using ICD-9-CM codes in any position. Multiple records for the same patient were identified using record linkage numbers. When multiple records resulted from the patient being transferred from one hospital to another, the records were consolidated into a single record. The initial hospital providing care was considered the treating hospital if the length of stay was greater than one day. If the length of stay at the initial hospital was one day or less, the hospital accepting the patient transfer was considered the treating hospital. When multiple records for the same patients were from unique encounters, only the record from the first encounter was included in the analysis.
Data obtained from the OSHPD Hospital Annual Utilization Data for each year included intensive care unit census days, general acute care bed days, teaching hospital status, and level 1 or 2 trauma center status. Presence of 24/7 PCI capability was obtained from the American Heart Association via the Cardiovascular Research Foundation website.12
Key outcome measures
Our primary outcome was good neurologic recovery at hospital discharge. In the OSHPD data, good neurologic recovery was defined as discharge to home, residential care facility, prison, jail, or another hospital for non-acute/non-skilled care. Patients who left against medical advice were also considered to have good neurologic recovery. Patients with all other dispositions, including death, were considered not to have good neurologic recovery.13–15 Secondary outcomes were survival to hospital discharge, receipt of a DNR order within 24 hours of admission, treatment at a 24/7 PCI center, and cardiac catheterization.
Data Analysis
Summary statistics were calculated for each variable. Continuous data reported as the median with interquartile ranges. Univariable analyses were performed to evaluate the relationship between sex, non-white race, and insurance status; and the primary and secondary outcomes.
In the analyses for good neurologic recovery, survival to discharge, cardiac catheterization and DNR order within 24 hours, hierarchical models with hospitals modeled with random intercepts were used to account for correlation among patients treated at the same hospital.16,17 Multiple logistic regression models were specified with the following independent variables: age, sex, race, ethnicity, insurance type, ventricular arrest rhythm, hospital size, intensive care unit bed days, 24/7 PCI capability, level 1–2 trauma center designation, and teaching status.18–20 In the analysis for treatment at a 24/7 PCI center as the dependent variable, a multiple logistic regression model was specified with the following independent variables: age, sex, race, ethnicity, insurance type, and ventricular arrest rhythm. Independent variables were selected a priori based on existing literature18–20 and clinical judgment for all models. All analyses were performed using Stata 14.2 (StataCorp, College Station, TX).
RESULTS
Of 43,909 OSHPD records with a “present on admission” diagnosis of cardiac arrest, 38,163 met our inclusion criteria and had complete data (Figure). Patients missing outcome data (good neurologic recovery, n=221; survival, n=12) were excluded from the respective models. The median age of study subjects was 67 years (55–70), and the majority of patients were male (22,178/38,163, 58%; Table 1). Overall, approximately one-quarter of patients had good neurologic recovery at hospital discharge (9,241/37,942, 24%).
Figure.
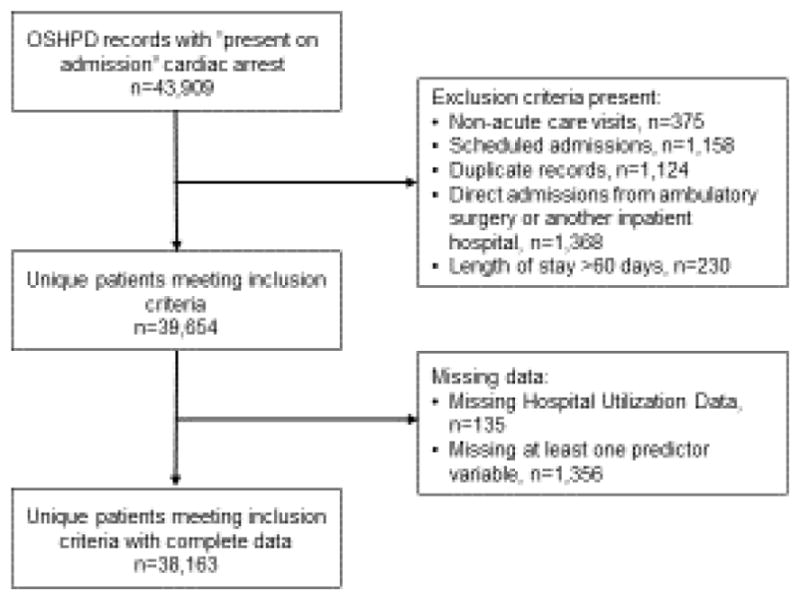
Flow diagram of OSHPD study population.
Table 1.
Demographic and clinical characteristics
| Variable | N (%) |
|---|---|
| Demographics | |
| Age* | 67 (55–79) |
| Male sex | 22,178 (58%) |
| White race | 25,347 (66%) |
| Unknown/missing race | -- |
| Hispanic ethnicity | 8,471 (22%) |
| Private insurance | 7,396 (19%) |
| Medicare insurance | 21,216 (56%) |
| Government insurance/self-pay | 9,551 (25%) |
| Arrest characteristics | |
| VF/VT rhythm | 11,036 (29%) |
| Outcomes | |
| Treatment at STEMI center | 27,826 (73%) |
| Good neurologic recovery | 9,241 (24%) |
| Survival to hospital discharge | 15,238 (40%) |
| DNR within 24 hours | 7,633 (20%) |
| Cardiac catheterization | 6,844 (18%) |
Age presented as median (interquartile range)
VF/VT = Ventricular fibrillation/ventricular tachycardia; CPR = Cardiopulmonary resuscitation; STEMI = ST segment elevation myocardial infarction; DNR = Do not resuscitate
Sex and outcomes
In multivariable analysis of the OSHPD data, female sex was associated with worse neurologic recovery (OR 0.94, 95% CI 0.89–0.98), worse survival (OR 0.94, 95% CI 0.90–0.99), decreased odds of cardiac catheterization (OR 0.61, 95% CI 0.57–0.65), decreased odds of treatment at a 24/7 PCI center (OR 0.89, 95% CI 0.85–0.93), and increased odds of receiving a DNR order within one day of admission (OR 1.16, 95% CI 1.10–1.23) (Table 2).
Table 2.
OSHPD hierarchical multiple logistic regression models.
| Variable | Good neurologic recovery | Survival | DNR within 24 hours | Cardiac catheterization | 24/7 PCI center care |
|---|---|---|---|---|---|
| Age (per 10 years) | 0.86 (0.85–0.88) | 0.88 (0.87–0.90) | 1.36 (1.33–1.39) | 0.99 (0.97–1.02) | 1.00 (0.99–1.02) |
| Female sex | 0.94 (0.89–0.98) | 0.94 (0.90–0.99) | 1.16 (1.10–1.23) | 0.61 (0.57–0.65) | 0.89 (0.85–0.93) |
| White race | 1.08 (1.02–1.14) | 1.02 (0.97–1.07) | 1.14 (1.07–1.21) | 1.11 (1.03–1.19) | 1.13 (1.07–1.18) |
| Hispanic ethnicity | 1.01 (0.95–1.08) | 0.94 (0.89–0.99) | 1.04 (0.97–1.11) | 0.98 (0.90–1.06) | 0.91 (0.86–0.96) |
| VF/VT rhythm | 2.04 (1.94–2.15) | 2.42 (2.30–2.53) | 0.56 (0.52–0.59) | 7.22 (6.78–7.69) | 1.84 (1.74–1.94) |
| Insurance status | |||||
| Medicare insurance | 0.85 (0.79–0.91) | 0.78 (0.73–0.83) | 1.25 (1.15–1.36) | 0.44 (0.40–0.48) | 0.87 (0.82–0.94) |
| Government insurance | 0.94 (0.88–1.01) | 0.65 (0.61–0.69) | 1.24 (1.13–1.36) | 0.56 (0.51–0.61) | 0.91 (0.85–0.98) |
| Private insurance | (ref) | (ref) | (ref) | (ref) | (ref) |
| 24/7 PCI center | 1.45 (1.29–1.63) | 1.23 (1.12–1.35) | 0.79 (0.65–0.95) | 13.1 (10.4–16.6) | -- |
| ICU census days (per 1,000) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | 1.00 (0.98–1.01) | 1.00 (0.99–1.02) | -- |
| General acute care bed days (per 100,000) | 1.07 (0.95–1.20) | 0.93 (0.85–1.02) | 1.03 (0.87–1.21) | 0.92 (0.78–1.08) | -- |
| Teaching hospital | 1.06 (0.87–1.28) | 1.08 (0.92–1.26) | 1.08 (0.77–1.51) | 1.14 (0.82–1.59) | -- |
| Level 1–2 trauma center | 0.91 (0.80–1.05) | 0.90 (0.81–1.01) | 1.04 (0.82–1.33) | 1.15 (0.91–1.46) | -- |
|
| |||||
| N=37,942 | N=38,151 | N=38,163 | N=38,163 | N=38,163 | |
Data are presented as odds ratios with 95% confidence intervals.
DNR = Do not resuscitate; VF/VT = Ventricular fibrillation/ventricular tachycardia; PCI = Percutaneous coronary intervention; ICU = Intensive care unit
Race and outcomes
White race was associated with better neurologic recovery (OR 1.08, 95% CI 1.02–1.14), increased odds of receiving a DNR order within one day of admission (OR 1.14, 95% CI 1.07–1.21), increased odds of treatment at a 24/7 PCI center (OR 1.13, 95% CI 1.07–1.18), and increased odds of cardiac catheterization (OR 1.11, 95% CI 1.03–1.19) (Table 2).
Insurance and outcomes
Medicare insurance was associated with worse neurologic recovery (OR 0.85, 95% CI 0.79–0.91). Non-private insurance was associated with worse survival (OR 0.65, 95% CI 0.61–0.69 for government insurance and OR 0.78, 95% CI 0.73–0.83 for Medicare), increased odds of a DNR order within one day of admission (OR 1.24, 95% CI 1.13–1.36 for government insurance and OR 1.25, 95% CI 1.15–1.36 for Medicare), decreased odds of treatment at a 24/7 PCI center (OR 0.91, 95% CI 0.85–0.98 for government insurance and OR 0.87, 95% CI 0.82–0.94 for Medicare), and decreased odds of cardiac catheterization (OR 0.56, 95% CI 0.51–0.61 for government insurance, OR 0.44, 95% CI 0.40–0.48 for Medicare) (Table 2).
DISCUSSION
Our results demonstrate that female sex, non-white race and lack of private insurance were predictors of less aggressive treatment and worse clinical outcomes for patients admitted following OHCA. Our results align with several recent studies of OHCA patients which demonstrated similar disparities.5,6 However, our study extends these findings by exploring differences in 24/7 PCI center treatment, early DNR orders and cardiac catheterization in patients resuscitated from OHCA.
The most striking disparities we found were based on insurance status. Several factors may contribute to this relationship between insurance status and clinical outcomes. First, patients lacking private insurance may be less likely to successfully manage chronic health conditions than privately insured patients, possibly resulting in more severe baseline disease.21–23 Patients lacking private insurance may receive less aggressive inpatient treatment following OHCA.8,9 They may also be less likely to be accepted in transfer to centers that can provide cardiac catheterization and a higher level of care.7,24 Providers at centers may also be less willing to perform cardiac catheterization when they know that they will be reimbursed at a lower rate.25 Similarly, patients without insurance may decline costly procedures or move to DNR status due to financial concerns. Future policy should address this disparity in poorer outcomes among the different insurance classes.
Our observation that race and insurance status were strongly associated with a decreased likelihood of undergoing cardiac catheterization is in agreement with other studies on in-hospital care disparities.10 Although women, non-white, and economically disadvantaged groups tend to decline invasive cardiac procedures more often than other groups, patient refusal is less likely to explain differences in OHCA due to its emergent presentation.26,27 Implicit physician bias regarding the effect that a patient’s comorbidities and socioeconomic barriers will have on post-procedural care has also been suggested to account for the performance of fewer invasive cardiac procedures in certain groups.28 Additionally, a role for racial bias in physician recommendations for invasive cardiac procedures cannot be discounted.29 Cardiac catheterization outcome reporting may also discourage centers from performing this procedure in certain post-OHCA patient populations.30
Several factors likely contribute to the sex differences we observed in OHCA survival and likelihood of undergoing cardiac catheterization. Female patients are less likely to receive guideline-recommended treatments for OHCA in the prehospital setting and more likely to experience an unwitnessed OHCA, both of which predict negative outcomes.31,32 Sex differences in the pathophysiology of ischemic heart disease and presence of ST segment elevation myocardial infarction (STEMI) on post-arrest electrocardiogram may contribute to the lower rates of cardiac catheterization in women.33,34 Interestingly, women underwent cardiac catheterization at much lower rates than men but had only a slightly decreased likelihood of survival with good neurologic recovery. Our data do not allow us to determine whether cardiac catheterization is over-used in men, under-used in women, or appropriately used in both populations. It is possible that interventional cardiologists are appropriately selecting women who are most likely to benefit from cardiac catheterization.
Guidelines from the American Heart Association and the International Liaison Committee on Resuscitation in place during the study period suggest that prognostication be done no earlier than 72 hours post-arrest with the exception of conditions such as non-survivable brain injury, underlying terminal disease or metastatic cancer.35 Despite these recommendations, approximately 20% of patients included in our study received a DNR order within 24 hours of admission (Table 1). These patients were more likely to be female, white, or lack private insurance. These findings align with those from a prior study of a nationally representative sample including Medicare patients hospitalized with several acute conditions.36 Lower rates of DNR orders in non-white patients may be explained by less effective communication between physicians and their non-white patients, a lack of confidence in the doctor-patient relationship on the part of patients and their families, or a cultural incompatibility with DNR orders.36,37 Due to the critical nature of OHCA, surrogate decision makers have a greater impact on DNR decision making than the patients themselves. Some DNR orders may have been due to surrogate decision makers enacting patients’ wishes. However, when a patient’s wishes are unknown, surrogate decision makers may follow physicians’ guidance on DNR status. Thus, DNR orders in these groups may represent compromised patient autonomy.36,38 Future studies are warranted to further understand DNR order disparities.
Our results confirm previous findings that patients treated at a 24/7 PCI center following OHCA are more likely to survive with good neurologic recovery.14,39 Treatment at a 24/7 PCI center was also associated with fewer early DNR orders, suggesting that care at 24/7 PCI centers may be more compliant with current prognostication guidelines.35 It is unclear why OHCA patients who were female, non-white, Hispanic or who lacked private insurance were less likely to be treated at a 24/7 PCI center. Insurance status may affect whether a patient is accepted for transfer by a 24/7 PCI center.7,24 Attempted inter-facility transfer may be declined more often by these groups. Female patients may manifest more atypical symptoms than men preceding OHCA leading to delayed recognition of a cardiac etiology and delayed transfer to a 24/7 PCI center.31 Finally, limited geographical access to 24/7 PCI centers may contribute to these differences.40
LIMITATIONS
Our study is not without limitations. We were unable to adjust for prehospital arrest characteristics that are associated with outcomes.18–20 Our data did not capture attempted but ultimately unsuccessful transfers to 24/7 PCI centers or cardiac catheterization procedures that were offered but ultimately declined by patients.
CONCLUSION
We found sex, race and insurance status differences in the likelihood of good neurological recovery, survival to hospital discharge, treatment at a 24/7 PCI center, receiving a DNR order within 24 hours of admission and undergoing cardiac catheterization in patients experiencing OHCA. Future investigation is warranted to better understand the reasons underlying these disparities and develop strategies to mitigate them. Understanding and overcoming these disparities is critical to developing evidence-based systems of care for all OHCA patients.
Acknowledgments
Source of support: The project described was supported by the National Heart, Lung, and Blood Institute (NHLBI) through grant #5K08HL130546.
The authors would like to thank Daniel Tancredi, PhD, for contributing his statistical expertise to the project.
Footnotes
Conflict of Interest declaration: The authors have no conflicts of interest to disclose. All authors have reviewed and approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report from the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S465–82. doi: 10.1161/CIR.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson DK, Zive D, Daya M, et al. The Impact of Early Do Not Resuscitate (DNR) Orders on Patient Care and Outcomes Following Resuscitation from out of Hospital Cardiac Arrest. Resuscitation. 2013;84:483–7. doi: 10.1016/j.resuscitation.2012.08.327. [DOI] [PubMed] [Google Scholar]
- 4.Hagihara A, Onozuka D, Ono J, et al. Age X Gender Interaction Effect on Resuscitation Outcomes in Patients with out-of-Hospital Cardiac Arrest. Am J Cardiol. 2017 doi: 10.1016/j.amjcard.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Eid SM, Abougergi MS, Albaeni A, et al. Survival, Expenditure and Disposition in Patients Following out-of-Hospital Cardiac Arrest: 1995–2013. Resuscitation. 2017;113:13–20. doi: 10.1016/j.resuscitation.2016.12.027. [DOI] [PubMed] [Google Scholar]
- 6.Shah KS, Shah AS, Bhopal R. Systematic Review and Meta-Analysis of out-of-Hospital Cardiac Arrest and Race or Ethnicity: Black US Populations Fare Worse. Eur J Prev Cardiol. 2014;21:619–38. doi: 10.1177/2047487312451815. [DOI] [PubMed] [Google Scholar]
- 7.Ward MJ, Kripalani S, Zhu Y, et al. Role of Health Insurance Status in Inter-Facility Transfers of Patients with St-Elevation Myocardial Infarction. Am J Cardiol. 2016;118:332–7. doi: 10.1016/j.amjcard.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiestand BC, Prall DM, Lindsell CJ, et al. Insurance Status and the Treatment of Myocardial Infarction at Academic Centers. Acad Emerg Med. 2004;11:343–8. doi: 10.1197/j.aem.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Hasan O, Orav EJ, Hicks LS. Insurance Status and Hospital Care for Myocardial Infarction, Stroke, and Pneumonia. J Hosp Med. 2010;5:452–9. doi: 10.1002/jhm.687. [DOI] [PubMed] [Google Scholar]
- 10.Calvin JE, Roe MT, Chen AY, et al. Insurance Coverage and Care of Patients with Non–St Segment Elevation Acute Coronary Syndromes. Ann Int Med. 2006;145:739–48. doi: 10.7326/0003-4819-145-10-200611210-00006. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Census Bureau. [Accessed September 17th 2017];Quickfacts Selected: California. 2016 2017, at https://www.census.gov/quickfacts/fact/table/CA - viewtop.
- 12. [Accessed 3 October 2016];Cath Lab Global Directory. 2016 at https://www.tctmd.com/cathlabmap.)
- 13.Bernard SA, Gray TW, Buist MD, et al. Treatment of Comatose Survivors of out-of-Hospital Cardiac Arrest with Induced Hypothermia. N Engl J Med. 2002;346:557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 14.Stub D, Smith K, Bray JE, et al. Hospital Characteristics Are Associated with Patient Outcomes Following out-of-Hospital Cardiac Arrest. Heart. 2011;97:1489–94. doi: 10.1136/hrt.2011.226431. [DOI] [PubMed] [Google Scholar]
- 15.Raina KD, Callaway C, Rittenberger JC, et al. Neurological and Functional Status Following Cardiac Arrest: Method and Tool Utility. Resuscitation. 2008;79:249–56. doi: 10.1016/j.resuscitation.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Littell RC, Milliken GA, Stroup WW, et al. Sas for Mixed Model. Cary, NC: SAS Publishing; 2006. [Google Scholar]
- 17.Normand ST, Glickman ME, Gatsonis CA. Statistical Methods for Profiling Providers of Medical Care: Issues and Applications. Journal Am Stat Assoc. 1997;92:803–14. [Google Scholar]
- 18.Sasson C, Rogers MA, Dahl J, et al. Predictors of Survival from out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 19.Liu JM, Yang Q, Pirrallo RG, et al. Hospital Variability of out-of-Hospital Cardiac Arrest Survival. Prehosp Emerg Care. 2008;12:339–46. doi: 10.1080/10903120802101330. [DOI] [PubMed] [Google Scholar]
- 20.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 21.Bittoni MA, Wexler R, Spees CK, et al. Lack of Private Health Insurance Is Associated with Higher Mortality from Cancer and Other Chronic Diseases, Poor Diet Quality, and Inflammatory Biomarkers in the United States. Prev Med. 2015;81:420–6. doi: 10.1016/j.ypmed.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 22.Dumas F, Blackwood J, White L, et al. The Relationship Between Chronic Health Conditions and Outcome Following Out-of-Hospital Ventricular Fibrillation Cardiac Arrest. Resuscitation. 2017;120:71–6. doi: 10.1016/j.resuscitation.2017.08.239. [DOI] [PubMed] [Google Scholar]
- 23.Zhang J, Huang E, Drum M, et al. Insurance Status and Quality of Diabetes Care in Community Health Centers. Am J Public Health. 2009;99:742–7. doi: 10.2105/AJPH.2007.125534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mumma BE, Diercks DB, Holmes JF. Availability and Utilization of Cardiac Resuscitation Centers. West J Emerg Med. 2014;15:758–63. doi: 10.5811/westjem.2014.8.21877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sada MJ, French WJ, Carlisle DM, et al. Influence of Payor on Use of Invasive Cardiac Procedures and Patient Outcome After Myocardial Infarction in the United States. J Amer Coll Cardiol. 1998;31:1474–80. doi: 10.1016/s0735-1097(98)00137-5. [DOI] [PubMed] [Google Scholar]
- 26.Schecter AD, Goldschmidt-Clermont PJ, McKee G, et al. Influence of Gender, Race, and Education on Patient Preferences and Receipt of Cardiac Catheterizations among Coronary Care Unit Patients. Am J Cardiol. 1996;78:996–1001. doi: 10.1016/s0002-9149(96)00523-1. [DOI] [PubMed] [Google Scholar]
- 27.Mumma BE, Baumann BM, Diercks DB, et al. Sex Bias in Cardiovascular Testing: The Contribution of Patient Preference. Ann Emerg Med. 2011;57:551–60e4. doi: 10.1016/j.annemergmed.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 28.Philbin EF, McCullough PA, DiSalvo TG, et al. Socioeconomic Status Is an Important Determinant of the Use of Invasive Procedures after Acute Myocardial Infarction in New York State. Circulation. 2000;102:III107–III15. doi: 10.1161/01.cir.102.suppl_3.iii-107. [DOI] [PubMed] [Google Scholar]
- 29.Groeneveld PW, Heidenreich PA, Garber AM. Racial Disparity in Cardiac Procedures and Mortality among Long-Term Survivors of Cardiac Arrest. Circulation. 2003;108:286–91. doi: 10.1161/01.CIR.0000079164.95019.5A. [DOI] [PubMed] [Google Scholar]
- 30.Peberdy MA, Donnino MW, Callaway CW, et al. Impact of Percutaneous Coronary Intervention Performance Reporting on Cardiac Resuscitation Centers: A Scientific Statement from the American Heart Association. Circulation. 2013;128:762–73. doi: 10.1161/CIR.0b013e3182a15cd2. [DOI] [PubMed] [Google Scholar]
- 31.Mumma BE, Umarov T. Sex Differences in the Prehospital Management of out-of-Hospital Cardiac Arrest. Resuscitation. 2016;105:161–4. doi: 10.1016/j.resuscitation.2016.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim C, Fahrenbruch CE, Cobb LA, et al. Out-of-Hospital Cardiac Arrest in Men and Women. Circulation. 2001;104:2699–703. doi: 10.1161/hc4701.099784. [DOI] [PubMed] [Google Scholar]
- 33.Bairey Merz CN, Shaw LJ, Reis SE, et al. Insights from the Nhlbi-Sponsored Women’s Ischemia Syndrome Evaluation (Wise) Study: Part Ii: Gender Differences in Presentation, Diagnosis, and Outcome with Regard to Gender-Based Pathophysiology of Atherosclerosis and Macrovascular and Microvascular Coronary Disease. J Am Coll Cardiol. 2006;47:S21–9. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 34.Bosson N, Kaji AH, Fang A, et al. Sex Differences in Survival from out-of-Hospital Cardiac Arrest in the Era of Regionalized Systems and Advanced Post-Resuscitation Care. J Am Heart Assoc. 2016:5. doi: 10.1161/JAHA.116.004131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Callaway CW, Soar J, Aibiki M, et al. Part 4: Advanced Life Support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation. 2015;132:S84–145. doi: 10.1161/CIR.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 36.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of Do-Not-Resuscitate Orders: Disparity by Age, Diagnosis, Gender, Race, and Functional Impairment. Arch Intern Med. 1995;155:2056–62. [PubMed] [Google Scholar]
- 37.Shepardson LB, Gordon HS, Ibrahim SA, et al. Racial Variation in the Use of Do-Not-Resuscitate Orders. J Gen Intern Med. 1999;14:15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quill CM, Ratcliffe SJ, Harhay MO, et al. Variation in Decisions to Forgo Life-Sustaining Therapies in Us Icus. Chest. 2014;146:573–82. doi: 10.1378/chest.13-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mumma BE, Diercks DB, Wilson MD, et al. Association between Treatment at an St-Segment Elevation Myocardial Infarction Center and Neurologic Recovery after out-of-Hospital Cardiac Arrest. Am Heart J. 2015;170:516–23. doi: 10.1016/j.ahj.2015.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen YC, Hsia RY. Association between Emergency Department Closure and Treatment, Access, and Health Outcomes among Patients with Acute Myocardial Infarction. Circulation. 2016;134:1595–7. doi: 10.1161/CIRCULATIONAHA.116.025057. [DOI] [PMC free article] [PubMed] [Google Scholar]


