Abstract
Rationale and objectives
One way to understand medical overuse at the clinician level is in terms of clinical decision‐making processes that are normally adaptive but become maladaptive. In psychology, dual process models of cognition propose 2 decision‐making processes. Reflective cognition is a conscious process of evaluating options based on some combination of utility, risk, capabilities, and/or social influences. Automatic cognition is a largely unconscious process occurring in response to environmental or emotive cues based on previously learned, ingrained heuristics. De‐implementation strategies directed at clinicians may be conceptualized as corresponding to cognition: (1) a process of unlearning based on reflective cognition and (2) a process of substitution based on automatic cognition.
Results
We define unlearning as a process in which clinicians consciously change their knowledge, beliefs, and intentions about an ineffective practice and alter their behaviour accordingly. Unlearning has been described as “the questioning of established knowledge, habits, beliefs and assumptions as a prerequisite to identifying inappropriate or obsolete knowledge underpinning and/or embedded in existing practices and routines.” We hypothesize that as an unintended consequence of unlearning strategies clinicians may experience “reactance,” ie, feel their professional prerogative is being violated and, consequently, increase their commitment to the ineffective practice.
We define substitution as replacing the ineffective practice with one or more alternatives. A substitute is a specific alternative action or decision that either precludes the ineffective practice or makes it less likely to occur.
Both approaches may work independently, eg, a substitute could displace an ineffective practice without changing clinicians' knowledge, and unlearning could occur even if no alternative exists. For some clinical practice, unlearning and substitution strategies may be most effectively used together.
Conclusions
By taking into account the dual process model of cognition, we may be able to design de‐implementation strategies matched to clinicians' decision‐making processes and avoid unintended consequence.
Keywords: de‐implementation, dual process cognition, medical overuse, quality improvement, substitution, unlearning
List of abbreviations
- COPD
chronic obstructive pulmonary disease
- DICE
Describe, Investigate, Create, Evaluate.
1. INTRODUCTION
Medical overuse is the provision of care that causes harms, is either ineffective, or where the harms outweigh the benefits.1 One way to understand medical overuse at the clinician level is in terms of clinical decision‐making processes that are normally adaptive but become maladaptive because of bias,2, 3 or practices that were at one time appropriate become outmoded but are retained out of habit.4, 5 By clinical decision making, we mean the process of choosing from among alternative courses of action in the diagnosis and treatment of a patient.6 For example, a patient with chronic obstructive pulmonary disease (COPD) and mild‐to‐moderate airflow obstruction complains of shortness of breath. The primary care physician prescribes an inhaled corticosteroid, which is effective for treating breathing exacerbations brought on by asthma—another condition that presents with shortness of breath—or for COPD patients with severe airflow obstruction. However, for patients with COPD without reversible airway obstruction, inhaled corticosteroids have limited or no benefits7 and may increase their risk of complications including pneumonia.8, 9, 10 The patient's primary care physician is unfamiliar with current guidelines for managing mild‐to‐moderate COPD, which call for use long‐acting beta or muscarinic agonists and not inhaled steroids. Instead, the physician conflates treatment of one condition with that of another that shares symptoms and the patient receives a medication that does them little good and instead puts them at risk.
Medical overuse is not driven exclusively or necessarily primarily by clinicians. For example, at the patient level, patients often lack awareness of harms; at the organizational level, quality metrics addressing underuse of care outnumber those addressing overuse; at the policy level, reimbursement policies often incentivize liberal use of diagnostics and therapeutics; and at the level of the profession, medical culture generally esteems thoroughness over restraint.11 However, we believe there is an opportunity to develop strategies to address overuse at the clinician level that builds on the great strides made in past decades in cognitive psychology understanding how decision making occurs and why and under what conditions people are susceptible to bias. And we believe that current efforts to address medical overuse—and the few conceptual models that have been applied specifically to overuse—do not adequately consider an important aspect of cognition.
In the present paper, we describe a model of cognition broadly referred to as the dual process model and the distinctive features of 2 types of cognitive processes that appear to guide people's decision‐making, one intuitive and automatic, and one reflective and deliberative. We then propose a conceptual model for promoting de‐implementation at the individual level based on the idea that clinician‐level de‐implementation strategies can be designed to correspond to the type of cognition, as well as designed to anticipate the potential for psychological reactance, a response to perceived threat to freedom that we hypothesize is a particularly highly elevated unintended consequence of de‐implementation efforts. Finally, we conclude with a discussion of where this model fits with prior research on the dual model of cognition and on other models that have been applied to de‐implementation.
1.1. Dual process model of cognition
Clinical decision making,12, 13 like all human decision making, appears to result from 2 distinct modes of cognitive processing14, 15, 16: reflective cognition, called Type 2 by cognitive psychologists, a conscious process of evaluating options based on some combination of utility, risk, capabilities, and/or social influences, then forming and acting on an intention; and automatic cognition, or Type 1, a set of largely unconscious processes that occur in response to environmental or emotive cues and rely on previously learned, ingrained heuristics.
Automatic cognition is rapid, nimble, and capable of coping with vast amounts of information through ingrained heuristics and learned associations, but takes time to develop through practice and experience. Automatic cognition is exemplified by an experienced automobile driver driving to their local grocery store. It entails rapidly processing vast amounts information (speed, direction, traffic signals, other drivers, pedestrians etc, all while retaining a mental model of the route to their destination) and producing split‐second decisions, yet human drivers can do this so effortlessly that they may arrive at the store with no conscious awareness of driving. At the same time, automatic cognition has important limitations. It is skill specific and context dependent. The heuristics developed in one setting may translate poorly to a different setting (eg, see Kahneman's account of London cab drivers' highly developed spatial and navigation abilities when tested outside London).17 In addition, when a skill or decision‐making process becomes automatic, our performance stops improving and may even decline over time unless we engage in a process of active learning.18, 19
Reflective cognition is the intentional process that is effortful, slow, and limited in terms of the volume or scope of information it can process at one time. An example of reflective cognition in action is multiplying two 3‐digit numbers in one's head. This requires several calculations while retaining incremental results in your working memory. For most people, it is not possible to do while multitasking and is easily disrupted by interruptions, stress, or fatigue. But reflective cognition is capable of self‐correction, and it is reflective cognition that leads to the development of the heuristics underpinning automatic cognition.19 Reflective cognition can continue to improve these heuristics when individuals get detailed feedback on specific aspects of performance and have an opportunity to repeatedly practice the same or similar tasks.20
1.2. Viewing medical overuse through the lens of clinician cognition
The way these different forms of cognition determine clinicians' decisions and behaviours has important implications for how we address medical overuse, that is, the provision of care that either has no benefit (eg, noninvasive preoperative screening for coronary disease in patients undergoing noncardiac surgery) or where the harms of care outweigh its benefits (eg, routine prostate cancer screening for men over 70).11
Many efforts to systematically curtail, or de‐implement, medical overuse can be characterized as either directed at (1) engaging clinicians' reflective cognition to consciously evaluate and correct overuse; or (2) circumventing clinicians' decision‐making altogether. Examples of engaging clinicians' reflective cognition include shared decision making, where clinicians engage with patients to evaluate care options based on patient's priorities; physician education, where clinicians are presented the current evidence‐based guidelines to adjust their clinical practice; and audit and feedback, where they receive information on their current clinical practice relative to some benchmark, such as peer practices or guideline‐recommended practice. In each of these examples, clinician decision making is expected to change as a function of conscious intention to change. Examples of circumventing clinicians' decision making include prior authorization, where clinicians must receive permission before a clinical decision can be acted upon; reimbursement policies unfavourable to certain clinical decisions; and precluding some ordering options (ie, hard‐stops) in electronic medical records. In each of these examples, clinicians' decision making ability is abridged in some way.
The problem with focusing on strategies that target clinicians' reflective cognition is twofold. First, it largely ignores the dominant role and corresponding opportunity represented by automatic cognition in clinical decision making. Many clinical settings where overuse occurs are inimical to reflective cognition. While it may be feasible to engage clinicians in reflective cognition outside the clinical setting, eg, via audit and feedback sessions on cancer screening, behaviour‐change intentions are only effective when they are retained in active memory. Intentions are rapidly forgotten, particularly when individuals multitask, are fatigued and stressed, or are interrupted,21 which often characterizes settings where clinicians have to make decisions about care. Moreover, reflective cognition is also susceptible to bias. One study induced expert physicians to engage in reflective cognition in making a diagnosis. They found that after reflecting on an initial decision during an opportunity to revisit and amend their diagnosis, physicians are likely to make the diagnosis less accurate.22 This may be because expert clinicians develop higher‐order concepts to represent clinical information and related diagnostic choices—a type of automatic cognition. These higher‐order concepts come to replace the laborious biomedical reasoning used by novices.23 Moreover, the reflective system is ineffective if underlying knowledge is absent. If physicians are enjoined to spend extra time on reaching a diagnosis in complex cases, diagnostic accuracy improves for experienced physicians but declines for inexperienced physicians.22 Finally, reflective cognition cannot be used endlessly; an individual's ability to exert self‐control and engage in reflective cognition (eg, problem solving, self‐regulating behaviour, or processing new information) is a finite resource; the more they engage in reflective cognition to make a decision or guide behaviour, the greater the difficulty in exercising reflective cognition for a new task, a condition referred to as ego depletion.24 This is congruent with research that has highlighted the importance of providing alternatives to clinicians when taking away ineffective practices.25, 26
The second problem with current de‐implementation efforts is they may fail to take into account the way all people react when their prerogative is abridged, particularly in a way that seems to impugn their judgement or character. This loss of freedom can manifest in a state of elevated arousal termed psychological reactance.27, 28, 29 Reactance comprises 2 responses: anger and negative cognition.28 While anger is an affective state, negative cognition, or counter arguing, is a cognitive state in which individuals question the authority or the rationale of the entity they perceive as infringing on their freedom.
We hypothesize that there are 2 potential unintended consequences of reactance for de‐implementation. Individuals may increase their commitment to the threatened behaviour (eg, engage in it more, express greater commitment to it), denigrate the source of the threat, and/or exercise their prerogative in an alternative, undesirable behaviour to restore their freedom.30 The implication is that by engendering reactance we may achieve the opposite of our intended result. There is some evidence of reactance from research on audit and feedback. A meta‐analysis of the literature found a significant decline in quality performance in over a third of feedback interventions. The more feedback could be characterized as about the clinician and less about a specific clinical task, the more likely the feedback intervention was to have a negative effect.31 The second unintended consequence of reactance is that the greater the level of counter arguing, the less receptive a clinician may be to reflect on evidence of overuse of their clinical practice on this or similar issues in the future. They may be more likely to reject data out of hand or rebuff efforts to engage with them on overuse of the ineffective practice. A poorly designed or executed de‐implementation strategy could thus make it less likely that subsequent de‐implementation efforts will be effective.
2. A MODEL FOR DE‐IMPLEMENTATION STRATEGIES BASED ON THE DUAL PROCESS MODEL OF COGNITION
We propose that de‐implementation strategies directed at clinicians can be conceptualized as corresponding to the 2 types of cognition: (1) a process of unlearning based on reflective cognition and (2) a process of substitution based on automatic cognition. In the discussion, we will contrast our approach with several other recent efforts to understand the psychological underpinnings of de‐implementation and their implications for more effective de‐implementation.
2.1. Unlearning
We define unlearning as an active process in which clinicians consciously change their knowledge, beliefs, and intentions about an ineffective practice and alter their behaviour accordingly.32 Cegarra‐Navarro and colleagues33 describe unlearning as “the questioning of established knowledge, habits, beliefs and assumptions as a prerequisite to identifying inappropriate or obsolete knowledge underpinning and/or embedded in existing practices and routines.” We term this critical assessment of the evidence.
For example, antipsychotic medications are often used to address agitation and aggression in patients with dementia,34 even though antipsychotics are associated with side effects (eg, cognitive worsening, abnormal gait), increased stroke risk, and increased mortality,35 and there is limited evidence for their use.36 An unlearning approach to reduce antipsychotic use could be operationalized in terms of an audit and feedback program37 in which the prescribing clinicians were presented with data on both the harms from antipsychotics in this patient population and their prescribing among patients with dementia, compared to peers, over some specified timeframe, with goal setting for prescribing in the future (Figure 1). Whether the clinicians engaged in a critical assessment of the evidence as a result could be measured through surveys or interviews about the clinicians' knowledge and opinions about the evidence and their intention to subsequently change. The overall effectiveness of the strategy could then be assessed in terms of a change in the average use of antipsychotics by the clinician or from chart review of the clinician's patients with dementia who were on antipsychotics to assess the appropriateness of the medication.
Figure 1.
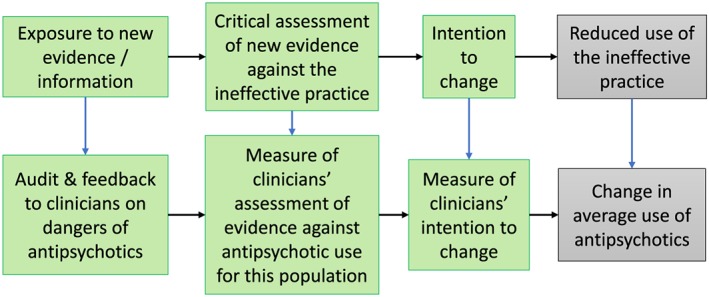
The unlearning process
The unlearning process can occur across a spectrum, from simple to deep unlearning.38 Simple unlearning occurs when new evidence that a practice is undesirable can be evaluated and understood within a clinician's existing mental models (ie, the way they understand the world to work). The idea that antipsychotics could increase risks of falls may fit within existing mental models for prescribing clinicians and only simple unlearning would need to take place to unlearn the practice in the context of reducing the risk of falls. Deep unlearning entails overcoming a significant challenge to a mental model, particularly when the assumptions inherent to the model may be so fundamental that they are not even recognized as assumptions. For example, clinicians may not understand why some events will seem to trigger patients with dementia to act out violently. It may require deep unlearning to accept the idea that a patient with dementia exhibits aggression or agitation as a rational reaction to external stimuli, such as changes made to the organization of their room, or someone reminding them that a loved one is dead. The clinician may not perceive the stimulus or fail to see how it could account for the ensuing behaviour.
2.2. Substitution
We define substitution as the promotion of one or more alternatives to the ineffective practice, in which the substitutes replace or displace the ineffective practice. We define a substitute practice as a specific alternative action or decision that either precludes the ineffective practice or makes it less likely to occur.
For example, a substitution approach to reduce antipsychotic use could be operationalized in terms of training frontline nursing aides at a long‐term care facility in the Describe, Investigate, Create, Evaluate (DICE) program (Figure 2). The DICE is a collaborative training program to empower nursing aides and other frontline staff to address patient agitation and aggression by targeting the behavioural symptom and the context in which it is occurring, examining and addressing likely precipitants, such as unexpressed pain, and iteratively evaluating the effectiveness of solutions to the underlying causes.39 The DICE represents substitution because frontline nursing staff are the ones who first and most frequently encounter patients' agitation and aggression and are the ones who most often bring it to the attention of prescribing staff.
Figure 2.
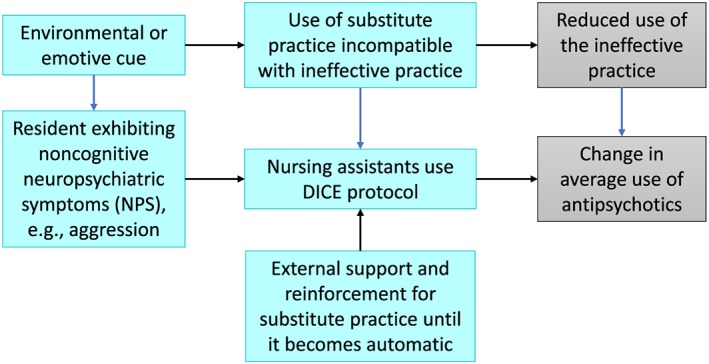
The substitution process
To be effective, the substitution strategy would likely require a period where external support from a trainer or other expert reinforced use of DICE until it became an ingrained part of nursing care, ie, until nursing aids and frontline staff developed new heuristics and routines related to DICE. Whether nursing aides use DICE could be measured through direct observation, surveys, or interviews. As with unlearning, the overall effectiveness of the strategy could then be assessed in terms of changes in antipsychotic use.
While we focus on introducing a substitute in the model, we hypothesize that in some situations it may be possible to engage automatic cognition in other ways, such as removing cues that trigger the initial decision to use an ineffective practice, changing choice architectures to discourage an ineffective practice, or introducing behavioural nudges. For example, an electronic order set for upper respiratory tract infection can be designed to discourage the use of antibiotics by presenting over‐the‐counter treatments first, and grouping all prescription options after.40
2.3. The relationship between the two
We expect that both approaches may work independently. The DICE could displace antipsychotic use without causing prescribing clinicians to question their former knowledge or assumptions about the risks and benefits of antipsychotic use. Conversely, the audit and feedback intervention could cause prescribing clinicians to eschew prescribing antipsychotics more frequently, even if no true alternative for addressing aggression and agitation exists. Unlearning and substitution strategies may work best, however, when used together rather than separately, such as using both audit and feedback and training in the DICE program.
A single de‐implementation strategy might incorporate both unlearning and substitution approaches simultaneously. Taking the prior example of inhaled corticosteroids prescribed to patients with COPD, in an integrated delivery system with an electronic health record, a team of pulmonologists could proactively conduct a chart review of all patients with COPD who have an inhaled corticosteroids prescription to determine if there is an indication for inhaled corticosteroids. If not, the pulmonologist could write an unsigned order to cancel the inhaled steroid order and change the patient's therapy to a more suitable agent (usually a long‐acting beta agonist or a long‐acting anticholinergic bronchodilator), providing an explanation for the change and a link the guidelines. The primary care provider would see the unsigned order with the explanation for the change from the pulmonologist, with plans for communicating the change to the patient. The unsigned order could operate through substitution approach because it gives the primary care provider an immediate alternative, ie, sign the order leading to the patient transitioning to a standalone long‐acting agent. Furthermore, through repeated exposure to the unsigned order, the provider might internalize the association (ie, to take patients with mild‐to‐moderate COPD off inhaled corticosteroids and put them exclusively on long‐acting beta or muscarinic agonist) on the level of automatic cognition. The unsigned order also embodies unlearning as it includes an explanation for the change and link to the guidelines; persuasion through presentation of evidence and formation of intention to change could be a key mechanism by which the provider de‐implements inhaled corticosteroids. As with the example of antipsychotics, the effect of the unsigned orders in terms of unlearning could be assessed through interviews or surveys with primary care providers about their knowledge of options about inhaled corticosteroids use in this patient population. This could occur before and after the de‐implementation strategy was used. The effect of the unsigned order in terms of substitution could be assessed by discontinuing the unsigned orders after a period and measuring whether inhaled corticosteroids use declined while the unsigned orders were in place and returned to baseline levels when they were discontinued.
3. DISCUSSION
The model for de‐implementation strategies described above is focused on how provider cognition might be considered in the design of provider‐level de‐implementation strategies. We believe it makes an important contribution to the literature on medical overuse and clinician decision making by proposing how de‐implementation strategies can be designed to correspond to a specific type of cognition and designed to anticipate the potential for unintended consequences. Specifically, this model introduces the idea of substitution as a strategy for addressing overuse at the clinician level; it specifies substitution as a strategy distinct from but complementary to unlearning strategies; and it hypothesizes psychological reactance as an unintended consequence of de‐implementation efforts, particularly from unlearning approaches, that could have long‐term consequences.
Others have applied dual process models to learning, unlearning, and implementation of evidence‐based practices.41, 42, 43, 44, 45 For example, Nilsen et al,45 drawing from learning and habit theory, propose 2 types of learning—adaptive and developmental. The former involves a gradual shift from slower, deliberate behaviours to faster, smoother, and more efficient behaviours while the latter is conceptualized as a process in the opposite direction, whereby more or less automatically enacted behaviours become deliberate and conscious. They see adaptive and developmental learning as continuous, iterative processes that allow new evidence‐based knowledge to be incorporated into clinical care. The process they term developmental learning is unlearning in our model. In contrast, we differentiate between unlearning and substitution. Substitution is more analogous to human‐factor approaches to change behaviour by redesigning the work environment,46, 47, 48 or behavioural economic approaches that introduce nudges and change the way options are presented to clinicians (choice architecture).40, 49, 50, 51, 52 These approaches, in contrast to unlearning, do not seek to engage clinicians in consciously correcting the underlying bias driving medical overuse.3 We believe this is a novel addition to the application of dual process models to evidence‐based care.
In terms of conceptual models of de‐implementation, we are aware of three. Niven and colleagues,53 as part of their literature synthesis on de‐implementation, propose adapting the Knowledge‐to‐Action model, which is a continuous cycle of knowledge inquiry, synthesis, and adaptation in the clinical setting, in which implementation strategies are selected and tailored on the basis of the barriers to knowledge use and informed by monitoring and evaluation. Parchman and colleagues54 have proposed a planned‐action model that articulates steps in engaging clinical practices in practice transformation to address overuse. The steps include creating conditions for change, engaging in sense‐making conversations with care teams and allowing them to take a sense of ownership of the issue to make their own decision about where the balance of benefit and harm lies. Finally, several studies have adapted the Theoretical Domains Framework to guide or interpret de‐implementation findings.55, 56, 57, 58 The Theoretical Domains Framework synthesizes psychological theories of behaviour change to help develop theoretically grounded behaviour‐change interventions. It encompasses 84 constructs organized in 14 domains, such as knowledge, intention, and beliefs about consequences.59 All 3 models are valuable contributions to the de‐implementation literature that articulate a process for systematic unlearning at multiple levels (in the first two) and keys domains that can be targeted (in the last). All 3 of these implicitly focus on engaging frontline clinicians in unlearning. Our model adds to this literature by juxtaposing the idea of substitution as a distinct, potentially complementary strategy for de‐implementation at the provider level. Furthermore, our model identifies psychological reactance as a particular risk from de‐implementation efforts.
Finally, effective de‐implementation efforts—as with effective implementation efforts—need to consider multiple levels synergistically: individuals, teams, organizations, and environments.60 We will need to consider how de‐implementation strategies at different levels can be designed synergistically with unlearning and/or substitution strategies. Patient education and reimbursement policies, for example, might be incorporated with audit and feedback to create a synergistic intervention to reduce the use of active follow‐up of incidental lung nodules found during nonlung cancer chest CT scans. This may require developing collaborations outside the existing research model in which researchers engage with advocacy groups, patients and caregivers, policy makers, payers, and others.
4. CONCLUSION
Under certain circumstances, normally adaptive clinician decision making is susceptible to bias and becomes maladaptive. This may be one important contributor to medical overuse. By taking into account the dual process model of cognition, we may be able to design de‐implementation strategies that take into account clinicians' decision‐making processes and avoid the unintended consequence of psychological reactance.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
FUNDING
This work was supported by grant no. QUE 15‐271 from the United States Department of Veterans Affairs Quality Enhancement Research Initiative (QUERI) Program. Dr. Graham is a recipient of the Canadian Institutes of Health Research (CIHR) Foundation Grant #143237. The CIHR funded Integrated Knowledge Translation Research Network (FDN# 143237) provided partial funding for the article's open access costs.
ETHICAL APPROVAL
No ethical approval required for this study.
CONSENT FOR PUBLICATION
No data are reported.
AVAILABILITY OF DATA AND MATERIALS
No data are reported.
AUTHORS' CONTRIBUTIONS
C.D.H. drafted the original model and wrote the manuscript. A.J.R., C.W.H., L.B.V., I.D.G., S.J.W., B.R.M., C.B.G., L.M.P., S.B., D.H.A., and D.C.A. provided feedback and revisions on the conceptual model and reviewed and revised the manuscript. All authors reviewed and approved the final manuscript.
ACKNOWLEDGEMENTS
Dr Steven B. Zeliadt, Dr George S. Sayre and Ms Kathryn Todd of VA Puget Sound have provided feedback on early drafts of the conceptual model.
This project was conducted as part of VHA Health Care Operations in accordance with VHA Handbooks 1605.1 and 1605.2. The project team had full responsibility for the design and conduct of this project; and preparation of the manuscript. The project was reviewed through normal administrative channels. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Helfrich CD, Rose AJ, Hartmann CW, et al. How the dual process model of human cognition can inform efforts to de‐implement ineffective and harmful clinical practices: A preliminary model of unlearning and substitution. J Eval Clin Pract. 2018;24:198–205. https://doi.org/10.1111/jep.12855
REFERENCES
- 1. Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171‐178. [DOI] [PubMed] [Google Scholar]
- 2. Graber M. Diagnostic errors in medicine: a case of neglect. Jt Comm J Qual Patient Saf. 2005;31(2):106‐113. [DOI] [PubMed] [Google Scholar]
- 3. Scott IA, Soon J, Elshaug AG, Lindner R. Countering cognitive biases in minimising low value care. Med J Aust. 2017;206(9):407‐411. [DOI] [PubMed] [Google Scholar]
- 4. Nilsen P, Roback K, Broström A, Ellström P‐E. Creatures of habit: accounting for the role of habit in implementation research on clinical behaviour change. Implement Sci. 2012;7(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hanrahan K, Wagner M, Matthews G, et al. Sacred cow gone to pasture: a systematic evaluation and integration of evidence‐based practice. Worldviews Evid Based Nurs. 2015;12(1):3‐11. [DOI] [PubMed] [Google Scholar]
- 6. Banning M. A review of clinical decision making: models and current research. J Clin Nurs. 2008;17(2):187‐195. [DOI] [PubMed] [Google Scholar]
- 7. Collins BF, Ramenofsky D, Au DH, Ma J, Uman JE, Feemster LC. The association of weight with the detection of airflow obstruction and inhaled treatment among patients with a clinical diagnosis of COPD. Chest. 2014;146(6):1513‐1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775‐789. [DOI] [PubMed] [Google Scholar]
- 9. Kew KM, Seniukovich A. Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD010115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wedzicha JA, Calverley PM, Seemungal TA, et al. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19‐26. [DOI] [PubMed] [Google Scholar]
- 11. Morgan DJ, Brownlee S, Leppin AL, et al. Setting a research agenda for medical overuse. BMJ. 2015;351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184‐1204. [DOI] [PubMed] [Google Scholar]
- 13. Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022‐1028. [DOI] [PubMed] [Google Scholar]
- 14. Kahneman D. Maps of bounded rationality: psychology for behavioral economics. Am Econ Rev. 2003;93(5):1449‐1475. [Google Scholar]
- 15. Evans JSB. Dual‐processing accounts of reasoning, judgment, and social cognition. Annu Rev Psychol. 2008;59(1):255‐278. [DOI] [PubMed] [Google Scholar]
- 16. Evans JSB, Stanovich KE. Dual‐process theories of higher cognition: advancing the debate. Perspect Psychol Sci. 2013;8(3):223‐241. [DOI] [PubMed] [Google Scholar]
- 17. Kahneman D. Thinking, fast and slow. New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 18. Ericsson KA, Krampe RT, Tesch‐Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100(3):363‐406. [Google Scholar]
- 19. Ericsson, K.A. , The influence of experience and deliberate practice on the development of superior expert performance The Cambridge handbook of expertise and expert performance (Cambridge Handbooks in Psychology). Cambridge: Cambridge University Press; 2006;38:685‐705. [Google Scholar]
- 20. Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10):S70‐S81. [DOI] [PubMed] [Google Scholar]
- 21. Einstein GO, McDaniel MA, Williford CL, Pagan JL, Dismukes R. Forgetting of intentions in demanding situations is rapid. J Exp Psychol‐Appl. 2003;9(3):147‐162. [DOI] [PubMed] [Google Scholar]
- 22. Norman GR, Monteiro SD, Sherbino J, Ilgen JS, Schmidt HG, Mamede S. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Acad Med. 2016. [DOI] [PubMed] [Google Scholar]
- 23. Ericsson KA, Lehmann AC. Expert and exceptional performance: evidence of maximal adaptation to task constraints. Annu Rev Psychol. 1996;47(1):273‐305. [DOI] [PubMed] [Google Scholar]
- 24. Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self‐control: a meta‐analysis. Psychol Bull. 2010;136(4):495‐525. [DOI] [PubMed] [Google Scholar]
- 25. Robert G, Harlock J, Williams I. Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services. Implement Sci. 2014;9(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Voorn V, Marang‐van de Mheen PJ, Wentink MM, et al. Perceived barriers among physicians for stopping non–cost‐effective blood‐saving measures in total hip and total knee arthroplasties. Transfusion. 2014;54(10pt2):2598‐2607. [DOI] [PubMed] [Google Scholar]
- 27. Brehm SS, Brehm JW. Psychological reactance: a theory of freedom and control. New York, NY: Academic Press; 2013. [Google Scholar]
- 28. Quick BL, Stephenson MT. Further evidence that psychological reactance can be modeled as a combination of anger and negative cognitions. Commun Res. 2007;34(3):255‐276. [Google Scholar]
- 29. Miron AM, Brehm JW. Reactance theory‐40 years later. Z Sozialpsychol. 2006;37(1):9‐18. [Google Scholar]
- 30. Dillard JP, Shen L. On the nature of reactance and its role in persuasive health communication. Commun Monogr. 2005;72(2):144‐168. [Google Scholar]
- 31. Kluger AN, DeNisi A. The effects of feedback interventions on performance: a historical review, a meta‐analysis, and a preliminary feedback intervention theory. Psychol Bull. 1996;119(2):254‐284. [Google Scholar]
- 32. Rushmer R, Davies HTO. Unlearning in health care. Qual Saf Health Care. 2004;13(suppl 2):ii10‐ii15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cegarra‐Navarro JG, Wensley AKP, Polo MTS. A conceptual framework for unlearning in a homecare setting. Knowl Manage Res Pract. 2014;12(4):375‐386. [Google Scholar]
- 34. Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350(mar02 7):h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maust DT, Kim HM, Seyfried LS, et al. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiat. 2015;72(5):438‐445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liperoti R, Pedone C, Corsonello A. Antipsychotics for the treatment of behavioral and psychological symptoms of dementia (BPSD). Curr Neuropharmacol. 2008;6(2):117‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ivers NM, Sales A, Colquhoun H, et al. No more ‘business as usual’ with audit and feedback interventions: towards an agenda for a reinvigorated intervention. Implement Sci. 2014;9(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Aron D, Lowery J, Tseng C‐l, Conlin P, Kahwati L. De‐implementation of inappropriately tight control (of hypoglycemia) for health: protocol with an example of a research grant application. Implement Sci. 2014;9(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kales HC, Gitlin LN, Lyketsos CG. Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62(4):762‐769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tannenbaum D, Doctor JN, Persell SD, et al. Nudging physician prescription decisions by partitioning the order set: results of a vignette‐based study. J Gen Intern Med. 2015;30(3):298‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ. 2009;14(1):27‐35. [DOI] [PubMed] [Google Scholar]
- 42. Sun R, Slusarz P, Terry C. The interaction of the explicit and the implicit in skill learning: a dual‐process approach. Psychol Rev. 2005;112(1):159‐192. [DOI] [PubMed] [Google Scholar]
- 43. Presseau J, Johnston M, Heponiemi T, et al. Reflective and automatic processes in health care professional behaviour: a dual process model tested across multiple behaviours. Ann Behav Med. 2014;48(3):347‐358. [DOI] [PubMed] [Google Scholar]
- 44. Potthoff S, Presseau J, Sniehotta FF, Johnston M, Elovainio M, Avery L. Planning to be routine: habit as a mediator of the planning‐behaviour relationship in healthcare professionals. Implement Sci. 2017;12(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nilsen P, Neher M, Ellström PE, Gardner B. Implementation of evidence‐based practice from a learning perspective. Worldviews Evid Based Nurs. 2017;14(3):192‐199. [DOI] [PubMed] [Google Scholar]
- 46. Carayon P. Handbook of human factors and ergonomics in health care and patient safety. New York: CRC Press; 2016. [Google Scholar]
- 47. Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)‐based healthcare system redesign for quality of care and patient safety. Ergonomics. 2015;58(1):33‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ Qual Saf. 2012: p. bmjqs‐2011‐000421;21(4):347‐351. [DOI] [PubMed] [Google Scholar]
- 49. Cornia PB, Amory JK, Fraser S, Saint S, Lipsky BA. Computer‐based order entry decreases duration of indwelling urinary catheterization in hospitalized patients. Am J Med. 2003;114(5):404‐407. [DOI] [PubMed] [Google Scholar]
- 50. Liao JM, Fleisher LA, Navathe AS. Increasing the value of social comparisons of physician performance using norms. JAMA. 2016;316(11):1151‐1152. [DOI] [PubMed] [Google Scholar]
- 51. Meeker D, Knight TK, Friedberg MW, et al. Nudging guideline‐concordant antibiotic prescribing: a randomized clinical trial. JAMA Intern Med. 2014;174(3):425‐431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA. 2016;315(6):562‐570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Niven DJ, Mrklas KJ, Holodinsky JK, et al. Towards understanding the de‐adoption of low‐value clinical practices: a scoping review. BMC Med. 2015;13(1):255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Parchman, M.L. , Henrikson N.B., Blasi P.R., Buist D.S., Penfold R., Austin B., and Ganos E.H.. Taking action on overuse: creating the culture for change Healthcare. 2016. [Epub ahead of print]. https://doi.org/10.1016/j.hjdsi.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 55. Voorn VM, Marang‐van de Mheen PJ, van der Hout A, et al. The effectiveness of a de‐implementation strategy to reduce low‐value blood management techniques in primary hip and knee arthroplasty: a pragmatic cluster‐randomized controlled trial. Implement Sci. 2017;12(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Barnes GD, Misirliyan S, Kaatz S, et al. Barriers and facilitators to reducing frequent laboratory testing for patients who are stable on warfarin: a mixed methods study of de‐implementation in five anticoagulation clinics. Implement Sci. 2017;12(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hahn EE, Munoz‐Plaza CE, Wang J, Garcia Delgadillo J, Mittman BS, Gould MK. Working towards de‐implementation: a mixed‐methods study in breast cancer surveillance care. J Patient Cent Res Rev. 2016;3(3):177‐178. [Google Scholar]
- 58. Voorn VM, Marang‐van de Mheen PJ, So‐Osman C, et al. De‐implementation of expensive blood saving measures in hip and knee arthroplasties: study protocol for the LISBOA‐II cluster randomized trial. Implement Sci. 2014;9(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Phillips CJ, Marshall AP, Chaves NJ, et al. Experiences of using the theoretical domains framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc. 2015;8:139‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Weiner BJ, Lewis MA, Clauser SB, Stitzenberg KB. In search of synergy: strategies for combining interventions at multiple levels. J Natl Cancer Inst Monogr. 2012;2012(44):34‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are reported.


