Abstract
Background
Children who are picky eaters typically demonstrate persistent food refusal and poor diet quality, and may be resistant to intervention.
Objective
This study tested whether pickiness moderated the effect of a nutrition intervention on diet quality in youth with type 1 diabetes, hypothesizing that the intervention effect would be smaller among picky relative to non-picky eaters.
Design
The study was an 18-month randomized clinical trial.
Participants
Youth age 8.0–16.9 years (n=136) with type 1 diabetes duration ≥1 year, receiving care at an outpatient diabetes center in Boston, Massachusetts, and a parent, participated from 2010–2013.
Intervention
The intervention integrated motivational interviewing, active learning, and applied problem-solving to increase whole plant food intake.
Main outcome measures
Whole Plant Food Density (WPFD, cup/oz equivalents per 1000 kcal of target food groups), Healthy Eating Index-2005 (HEI2005, measures conformance to US dietary guidelines), and dietary variety were calculated from three-day food records completed at six times. Parents completed the pickiness subscale of the Child Feeding Questionnaire.
Statistical analyses performed
Mean WPFD and HEI2005 were estimated using population ratio method; standard errors were computed using jackknife variance-covariance estimation. Overall p-value comparing groups across visits was derived using chi-square test.
Results
Baseline diet quality was lower in picky than non-picky eaters. There was no intervention effect on pickiness or dietary variety. In stratified analyses, the intervention effect on diet quality was significant for picky eaters only (WPFD p=.0003; HEI2005 p=.04). Among picky eaters, diet quality in the treatment group improved, while diet quality in the control group remained low. Diet quality of non-picky eaters in the intervention group changed to a lesser degree.
Conclusions
The intervention resulted in increased diet quality in picky eaters, whereas there was no intervention effect in non-picky eaters. Findings suggest that diet quality of picky eaters can be improved without changing their underlying pickiness.
Keywords: pickiness, diet quality, type 1 diabetes, intervention, families
INTRODUCTION
Diet quality among youth with type 1 diabetes is inconsistent with dietary guidelines, with inadequate intake of fruits, vegetables, and whole grains,1, 2 and excessive intake of total and saturated fat and discretionary foods.2–4 These diet patterns increase risk for numerous chronic diseases.5 As part of standard care, youth with type 1 diabetes typically receive nutrition education addressing carbohydrate counting and guidelines for healthful eating.6, 7 Despite this, diet quality in type 1 diabetes patients appears to be no better than that of the general population of US youth,8 suggesting the importance of understanding potential barriers to dietary change in this population.
Families of youth with type 1 diabetes report child pickiness, generally defined as eating a limited variety of foods while rejecting many foods (whether familiar or unfamiliar),9, 10 as a barrier to improving child diet quality.11 Picky eaters may reject foods due to dislike of their taste or their texture.9 They also tend to demonstrate less food enjoyment, more slowness in eating, and higher satiety responsiveness.9, 12 Pickiness is more common in pre-school than school-age children;9, 13 hence, most research has been conducted in young children.9, 10 Children who are picky eaters typically demonstrate lower vegetable intake12, 14–16 and lower dietary diversity.17 Research examining pickiness in older children and adolescents is scarce; one study reported an inverse association of pickiness with diet variety in youth with type 1 diabetes ages 8–18 years,18 with mean pickiness scores similar to those reported in younger samples. One longitudinal study reported that food variety-seeking in preschoolers was predictive of such behaviors into adulthood.19 Further research investigating the influence of pickiness on diet quality in older children and adolescents, and examining whether pickiness is an important barrier to dietary behavior change in this age group, is warranted.
The characteristics of picky eating – limited variety and food rejection – may represent an important barrier to efforts to improve diet quality. As such, picky eaters may be less likely to benefit from behavioral nutrition interventions designed for the general population. While family-based educational programs designed specifically for parents of children with non-clinical feeding problems have been shown to reduce these feeding problems,20 the impact of pickiness on the efficacy of general behavioral nutrition interventions has not been examined. The authors previously reported an improvement in diet quality among youth with type 1 diabetes participating in a behavioral nutrition intervention relative to controls.21 The family-based intervention incorporated a motivational interviewing interaction style and an applied problem-solving process in which youth selected which healthful foods they wanted to consume. Such an approach may be useful for picky eaters by allowing choice and adapting to their preferences. The purpose of this secondary analysis was to test whether the intervention impacted pickiness, and whether pickiness modified the intervention effect on diet quality.
MATERIALS AND METHODS
Design
An 18-month randomized clinical trial of a behavioral nutrition intervention was conducted from August 2010 through May 2013 at an outpatient, free-standing, multidisciplinary tertiary diabetes center in Boston, Massachusetts.
Participants
Participants were 136 youth-parent dyads meeting the following eligibility criteria: youth age 8.0 to 16.9 years, diagnosis of type 1 diabetes ≥1 year, daily insulin dose ≥0.5 units per kilogram, most recent HbA1c ≥6.5% and ≤10.0%, intensive insulin therapy with either an insulin regimen of ≥3 injections daily or insulin pump, at least one clinic visit in the past year, and ability to communicate in English. Exclusion criteria included daily use of premixed insulin, transition to insulin pump therapy in the last three months, real-time continuous glucose monitoring use in the last three months, participation in another intervention study in the last six months, and presence of gastrointestinal disease such as celiac disease, multiple food allergies, use of medications that interfere significantly with glucose metabolism, or significant mental illness or neurodevelopmental condition. Sample size was based on detecting meaningful differences in dietary intake and glycemic control between intervention and control conditions, and has been reported in detail previously.21
Procedures
Research staff recruited participants during regular clinic visits. Parents and youth turning 18 years of age during the trial provided written informed consent; all youth provided assent. Study procedures were approved by the institutional review board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Randomization was conducted by the data coordinating center using a permuted block randomization scheme, stratified by age (<13 years and ≥13 years), hemoglobin A1c (<8.5% and ≥8.5%), and insulin regimen (injection and insulin pump). Study visits and survey measures were completed in the clinic; diet records were completed following study visits.
Intervention
Youth and parents in the intervention condition (described in greater detail elsewhere21 and available upon request from the lead author) participated in six core and three booster individual sessions targeting increased intake of whole plant foods, defined as whole fruits, vegetables, whole grains, legumes, nuts, and seeds. Sessions integrated a motivational interviewing style of interaction with youth and parents to increase internal motivation for healthful eating, active learning to facilitate skill-building and engagement with the educational information, and applied problem-solving (selecting goals, considering barriers, choosing strategies, and developing a specific action plan) to facilitate goal-directed behavior and self-regulation skills. An initial overview session addressed key principles of healthy eating, focusing on whole plant foods (whole fruit, vegetables, whole grains, legumes, nuts and seeds). The next five sessions applied these principles to specific eating contexts – breakfast, lunch, dinner, snacks, and eating away-from-home. Three booster sessions addressed overcoming challenges associated with social eating, meal planning, and the food environment. Families in the control condition received equal frequency of research contacts, but no additional dietary advice beyond that provided as part of standard care.
Measures
Pickiness
Parents reported youth pickiness at baseline and 6, 12, and 18 months using the Pickiness subscale of the Child Feeding Questionnaire.14 The three items examine parents’ perceptions of their children’s pickiness about food using a five-point Likert scale. Items include “my child’s diet consists of only a few foods,” “my child is unwilling to eat many of the foods that our family eats at mealtimes,” and “my child is fussy or picky about what he or she eats.” Response options range from 1=“strongly disagree” to 5=“strongly agree.” Higher scores on this subscale represent higher levels of pickiness. This brief measure was associated with lower vegetable intake in children.14 Cronbach’s alpha in the current study was 0.92.
Dietary Intake
Participants (youth and a parent) completed three-day youth food records at baseline and 3, 6, 9, 12, and 18 months. Research assistants instructed participants on accurately measuring and reporting food and beverage intake and provided a sample diet record. Families were asked to use measuring utensils when at home, and if away from home, provide their best estimate of portion size. They were instructed to provide all specific details for each food item, including names of brands or restaurants and specific item labeling (e.g., low fat, 1% milk). Recording began on the day of the study visit and continued for the next three full days. Upon receipt of the completed records, research staff reviewed the records to ensure completeness, and solicited missing information (e.g., brand names) as needed. For visits in which a family did not complete a diet record, two non-consecutive 24-hour dietary recalls were obtained by a registered dietitian (1.7% of dietary assessments). Diet records were entered by two registered dietitians and verified for consistency and accuracy. Nutrition Data System for Research software (NDSR 2012; Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN)22 was used to analyze the records and assess nutrient intake and food group servings.
Two indicators of diet quality and a measure of diet variety were calculated. The Healthy Eating Index-2005 (HEI2005) measures conformance to the 2005 Dietary Guidelines for Americans, and is comprised of 12 component scores corresponding to dietary guidelines for intake of total fruit, whole fruit, total vegetables, dark green/orange vegetables and legumes, total grains, whole grains, milk, meat and beans, oils, saturated fat, sodium and energy from solid fat, alcohol and added sugars.23 The maximum component score is achieved if intake meets recommended intake levels, with truncation for intakes exceeding recommendations. Recommendations and scores are expressed on a per-1000 kilocalorie basis to enable comparability across individuals with different energy requirements. Component scores are summed to obtain the total score, with possible values ranging from 0–100; a score of 100 indicates meeting intake recommendations for all dietary components. Because the HEI2005 reflects the dietary guidance available to participants at the time of recruitment, it was deemed more appropriate for these analyses than the HEI2010. Whole Plant Food Density (WPFD) is a continuous measure representing the proportion of the diet allocated to whole grains, whole fruit, vegetables, legumes, nuts, and seeds; calculated as the total number of cup or ounce equivalents of these foods consumed per 1000 kilocalorie total intake.24 WPFD was developed by two of the investigators to provide a measure that directly corresponds to the target food groups of the intervention; it has shown associations with cardiovascular biomarkers in the general US population.24 Diet variety was measured using a modified version of the index developed by Murphy and colleagues.25 Diet variety is calculated as the number of food groups consumed from among pre-specified healthful food groups. The original measure, which included 22 food groups, was modified in accordance with the 2010 Dietary Guidelines for Americans,26 which recommends reducing intake of processed meat and non-whole grains, and emphasizes low-fat versus high-fat dairy products. Thus, the food groups “franks, lunchmeat” and “non-whole grains” were eliminated, and foods from dairy food groups were counted only if low or reduced fat. Scores for the modified measure thus have a possible range of 0 to 20; higher counts reflect greater diet variety.
Analysis
Baseline demographic and disease-related characteristics of the study participants were summarized with means and standard deviations for continuous variables and frequencies for categorical and ordinal variables. Independent t-tests for continuous variables and Pearson chi-square for categorical variables were used to compare these characteristics between intervention and control groups.
Youth were classified as picky versus non-picky eaters using a median split on the baseline pickiness score. The resulting groups were those in which the mean indicated non-endorsement of pickiness (score ≤2.0) versus those in which the mean indicated any degree of endorsement of pickiness (score >2.3).
Effect of the intervention on pickiness and dietary variety was tested using two-sample t-tests to compare intervention groups at each visit, and linear mixed-effect models to asses for difference in change over time. Mean values for each diet quality variable at each visit by treatment condition and pickiness group were estimated using the population ratios method – the ratio of total nutrient or food group intake to total energy intake at the group level; this method reduces bias in estimates of usual intakes from limited dietary assessment data.27 The jackknife method was used to estimate the standard errors and correlations of the mean values across clinic visits. Between-group comparisons within each pickiness subgroup, and testing for pickiness by intervention interaction for each outcome were conducted using chi-square test based on the estimated means and their variance-covariance matrix, assuming that the quadratic form of the means weighted by the inverse of their variance-covariance matrix follows asymptotically a chi-square distribution. A p-value of < 0.05 was considered statistically significant. All analyses were done using R software, version 3.1.2.28
RESULTS
Participant flow from recruitment through follow-up has been reported previously.21 Of 622 invited, 148 provided informed consent and 139 completed baseline. Data were excluded from 1 sibling each of 3 sibling pairs. Subject retention through study completion was 92%. All withdrawn subjects had been randomized to the intervention group: one withdrew after baseline but before being informed of treatment assignment; two withdrew within the first three study months; three between months three and six, one between months six and nine, three between months nine and twelve, and one after month twelve. Reasons for withdrawal were primarily lack of time to participate. No study-related adverse events were reported.
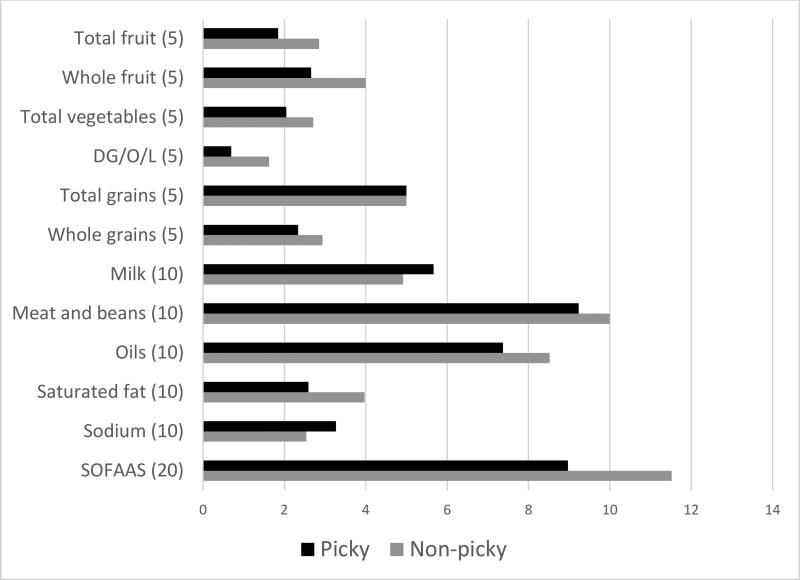
Baseline characteristics were well-balanced between the intervention and control groups (Table 1). Baseline diet variety (5.55 vs. 7.59, p=.001) and quality (HEI2005 51.67 vs. 60.58, p=.001; WPFD 1.56 vs. 2.12, p=.002) were lower in picky eaters than in non-picky eaters. This difference in diet quality was reflected across most subscales of the HEI2005 (Figure 1).
Table 1.
Baseline sample characteristics of 136 youth with type 1 diabetes participating in a behavioral nutrition efficacy trial, stratified by baseline pickiness.
| Picky (N=57) | Non-picky (N=79) | |||||
|---|---|---|---|---|---|---|
| Treatment (N=31) |
Control (N=26) |
Pa | Treatment (N=35) |
Control (N=44) |
Pa | |
| Mean±SD or N (%) |
Mean±SD or N (%) |
Mean±SD or N (%) |
Mean±SD or N (%) |
|||
| Demographics | ||||||
| Youth age (years) | 12.17±2.69 | 12.99±2.39 | 0.2 | 12.76±2.65 | 12.96±2.55 | 0.7 |
| Youth sex | 0.9 | 0.2 | ||||
| Male | 16(51.61) | 14(53.85) | 19(54.29) | 17(38.64) | ||
| Female | 15(48.39) | 12(46.15) | 16(45.71) | 27(61.36) | ||
| Youth race/ethnicity | 0.9 | 0.1 | ||||
| White, non-Hispanic | 28(90.32) | 24(90.32) | 30(85.71) | 41(93.18) | ||
| Hispanic | 1(3.23) | 1(1.75) | 1(2.86) | 2(4.55) | ||
| Black, non-Hispanic | 2(6.45) | 1(1.75) | 4(11.43) | 0(0) | ||
| Multi-racial | 0(0) | 0(0) | 0(0) | 1(2.27) | ||
| Highest parent education levelb | 0.4 | 0.8 | ||||
| High school or equivalent | 1(1.75) | 2(7.69) | 3(8.57) | 2(4.55) | ||
| Junior college, technical or some college | 5(16.13) | 7(26.92) | 6(17.14) | 9(20.45) | ||
| College degree | 9(29.03) | 9(34.62) | 11(31.43) | 17(38.64) | ||
| Graduate education | 16(51.61) | 8(30.77) | 15(42.86) | 16(36.36) | ||
| Family income to poverty ratioc | 5.39±3.10 | 4.21±2.92 | 0.2 | 5.64±3.34 | 5.28±3.03 | 0.6 |
| Diabetes characteristics | ||||||
| Duration of diabetes (years) | 5.88±2.71 | 6.50 ±3.58 | 0.5 | 5.27±2.38 | 6.23±3.61 | 0.2 |
| Insulin regimen | 0.7 | 0.8 | ||||
| Injection only | 7(22.58) | 7(26.92) | 13(37.14) | 15(34.09) | ||
| Pump | 24(77.42) | 19(73.08) | 22(62.86) | 29(65.91) | ||
| Frequency of blood glucose monitoring (times/day) | 5.71±2.32 | 5±2.5 | 0.3 | 5.83±2.43 | 5.89±2.39 | 0.9 |
| Hemoglobin A1c (%) | 8.13±0.86 | 8.22±086 | 0.7 | 8.09±1.31 | 8.03±1.07 | 0.8 |
| Diet characteristics | ||||||
| Dietary pickiness | 3.27±0.75 | 3.49±0.89 | 0.4 | 1.38±0.44 | 1.39±0.43 | 0.9 |
| Dietary varietyc | 5.8±2.16 | 5.26±2.56 | 0.4 | 7.41±1.83 | 7.73±1.66 | 0.4 |
| Healthy eating index 2005d | 52.86±13.3 | 50.1±16 | 0.5 | 60.46±15.05 | 60.66±15.67 | 0.9 |
| Whole plant food densitye | 1.62±0.94 | 1.48±0.86 | 0.6 | 2.1±1.15 | 2.13±1.12 | 0.9 |
Comparisons between intervention and control groups using independent t-tests for continuous variables or chi-square for categorical variables.
Missing data from 1 participant on highest parent education and from 2 participants on family income.
Represents the number of food groups consumed from 20 pre-specified healthful food groups.
Represents Healthy Eating Index-2005 total score; measures conformance to 2005 Dietary Guidelines for Americans (min=0, max=100, higher scores indicate closer conformance).
Continuous measure representing the total number of cup or ounce equivalents per 1000 kcal consumed of whole grains, fruit, vegetables, legumes, nuts and seeds.
Adapted with permission from: Nansel TR, Laffel L, Haynie D, Mehta S, Lipsky L, Volkening L, Butler D, Higgins L, Liu A. Improving dietary quality in youth with type 1 diabetes: randomized clinical trial of a family-based behavioral intervention. International Journal of Behavioral Nutrition and Physical Activity 2015; 12:58.
Figure 1.
Baseline mean values on HEI2005 a component scores by baseline pickiness in 136 youth with type 1 diabetes
a Healthy Eating Index-2005 measures conformance to 2005 Dietary Guidelines for Americans and is comprised of 12 subscales: Total fruit, whole fruit, total vegetables, dark green and orange vegetables and legumes (DG/O/L), total grains, whole grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fat, alcohol, and added sugar. Higher scores represent better conformance to dietary guidelines. Values in parentheses represent highest possible score for each component.
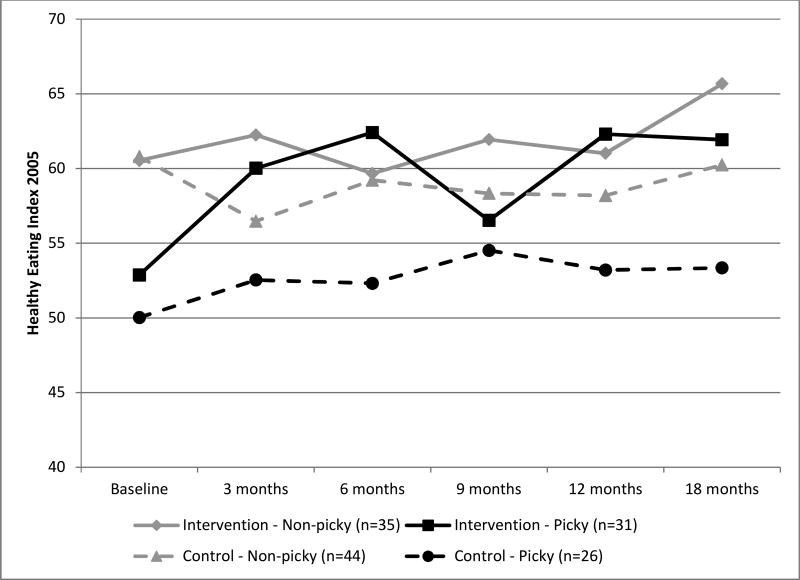
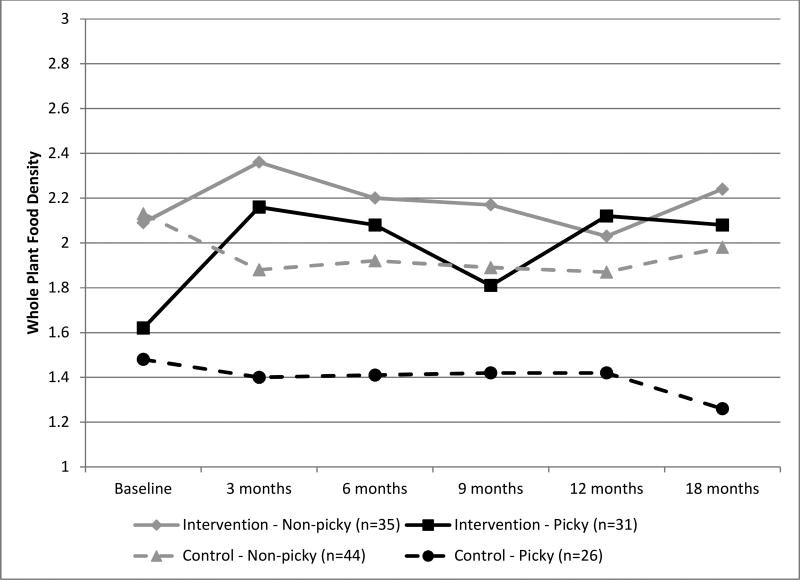
There was no intervention effect on either pickiness or diet variety; scores were relatively stable across time in both groups (data not shown). In analyses stratified by baseline pickiness, the intervention effect on diet quality across the study duration was significant for picky eaters only (WPFD p=.0003; HEI2005 p=.04) (Figures 2&3). Among these youth, positive changes were spread across the HEI component scores representing fruit and vegetable intake, whole grains, meat/beans, oils, sodium, and empty calories (Table 2). Tests for interaction of intervention group by pickiness on WPFD and HEI2005 were not statistically significant.
Figure 2.
Effect of a behavioral nutrition intervention on mean Healthy Eating Index 2005 a stratified by baseline pickiness in 136 youth with type 1 diabetes
a Healthy Eating Index-2005 total score measures conformance to 2005 Dietary Guidelines for Americans (min=0, max=100, higher scores indicate closer conformance).
Figure 3.
Effect of a behavioral nutrition intervention on mean Whole Plant Food Density a stratified by baseline pickiness in 136 youth with type 1 diabetes
aContinuous measure representing the total number of cup or ounce equivalents per 1000 kcal consumed of whole grains, fruit, vegetables, legumes, nuts and seeds.
Table 2.
Mean change in HEI2005a component scores from baseline to 18-month follow-up among 66 youth receiving a dietary intervention, stratified by baseline pickiness.
| HEI2005 component | Non-picky | Picky |
|---|---|---|
| Total fruit | −0.52 | 0.24 |
| Whole fruit | −0.76 | 0.77 |
| Total vegetables | 0.70 | 0.72 |
| DG/O/L | 0.66 | 0.50 |
| Total grains | 0.00 | 0.00 |
| Whole grains | 0.69 | 0.87 |
| Milk | −0.02 | −0.47 |
| Meat and beans | 0.00 | 0.77 |
| Oils | 0.91 | 1.83 |
| Saturated fat | 0.71 | −0.02 |
| Sodium | −0.06 | 0.96 |
| SOFAAS | 2.80 | 2.80 |
Healthy Eating Index-2005 measures conformance to 2005 Dietary Guidelines for Americans and is comprised of 12 subscales: Total fruit, whole fruit, total vegetables, dark green and orange vegetables and legumes (DG/O/L), total grains, whole grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fat, alcohol, and added sugar. Higher scores represent better conformance to dietary guidelines.
DISCUSSION
Diet quality improved to a greater extent in picky eaters compared to non-picky eaters participating in this behavioral nutrition intervention trial. This improvement occurred despite the absence of an effect on pickiness and diet variety, suggesting that youth may have increased intake of foods already acceptable to them, rather than expanding the range of foods consumed. Changes in HEI subscales suggest that their increase and whole plant foods was accompanied by a decrease in empty calories (represented by the SOFAAS subscale; calories from solid fat, alcohol, and added sugar). Consistent with previous literature,12, 14–16 baseline diet quality of picky eaters was poorer than that of non-picky eaters. However, diet quality of picky eaters in the intervention group improved to the level of non-picky eaters in the control group. The effect on HEI2005 is comparable to a 1-quintile difference in the Nurses’ Health and Health Professionals Follow-Up Studies, in which HEI2005 was linearly associated with chronic disease risk29. Findings suggest that despite common perceptions of pickiness as a barrier to healthful eating,11, 30 the diet quality of picky eaters can be substantially improved without changing their underlying pickiness.
Despite the centrality of diet in managing type 1 diabetes, there is a paucity of research on picky eating specifically, or approaches to improve diet quality generally, in this population. The intervention approach tested in this study incorporated behavioral elements with evidence of efficacy across populations and behaviors (e.g, motivational interviewing, problem-solving), in a way that incorporated diabetes-specific needs (i.e., carbohydrate estimation) and was tailored to families’ varying circumstances. The flexible and individualized approach used in the intervention may have facilitated its utility among picky eaters. A motivational interviewing interaction style communicated respect for the youth’s perspective and preferences, and may have facilitated engagement and buy-in. Youth were encouraged to choose which food groups they wanted to increase at each meal type, allowing them to focus on increasing intake of foods they already accepted. This may be particularly important among picky eaters, who have difficulty accepting new tastes and textures.9 The family-based nature of the intervention may have prompted parents to engage in role modeling of healthful eating, which is associated with improved diet quality among children.20 It is also possible that engaging parents and children in collaboratively planning healthy meal changes may have decreased parent-child conflict regarding food, a common problem among families with picky children.13 Additionally, the intervention was designed to be fun and engaging, with activities such as youth competing with their parents in creating a recipe. This may have been particularly helpful for picky eaters, who tend to have lower food enjoyment than those with less pickiness.9, 12
It is unclear why the intervention was less effective for non-picky eaters than for picky eaters. Findings are not explained by a ceiling effect, as diet quality among the non-picky eaters was also well below recommendations. However, it is possible that different intervention strategies may be more effective for persons with poorer versus better diet quality. Parents of picky eaters may have perceived a greater need to improve their child’s diet and more fully engaged in the intervention as a result. Overall, people tend to overestimate their own diet quality31 and that of their children,32 which may inhibit perceived need for change. Additionally, parents of picky eaters report greater food-related conflict and difficulty identifying healthy foods that their children will eat,14, 33 thus potentially motivating greater engagement in the intervention. An important area of future research may include further examining differences in experiences of families of picky and less picky eaters participating in behavioral nutrition interventions.
Findings from this study should be interpreted in light of its strengths and limitations. This is the first study to examine the extent to which the effect of an intervention on diet quality and variety differed by pickiness, and one of the few examining pickiness in youth with type 1 diabetes. Three-day diet records are among the most reliable and valid measures of dietary intake. While measurement error is associated with all methods of dietary assessment, steps were taken to mitigate measurement error, such as providing participants with tools to make records as accurate and complete as possible, reviewing completed records upon receipt from the family to ensure completeness, and soliciting missing information from the family as needed. The study had a 92% retention rate; however, the 24% participation rate and the clinical sample limits the ability to generalize findings. As this was a post hoc analysis, the study had limited power to detect an interaction of the intervention group by pickiness on diet quality and was underpowered to examine the intervention effect by subgroups. Additionally, the sample size is insufficient to assess the effect of the intervention in the most extreme picky eaters.
CONCLUSIONS
Findings provide preliminary evidence that dietary interventions may be effective for improving diet quality in picky eaters, even without improving pickiness or diet variety. Future research examining the intervention approach used in this study with a non-clinical sample and a larger number of picky eaters would further inform this question, and would allow for an examination of the types of dietary changes made by picky eaters. Qualitative data about families’ experiences implementing dietary changes with picky youth would also be useful. The findings presented herein, suggesting that dietary pickiness may not represent a substantial barrier to healthful diet change, are promising for health care providers and families of picky eaters.
RESEARCH SNAPSHOT.
Research Questions
Does the effect of a behavioral nutrition intervention differ between picky and non-picky eaters?
Key Findings
In this randomized clinical trial of 136 youth with type 1 diabetes, the intervention effect on diet quality was significant for picky eaters only in analyses stratified by baseline pickiness. Among picky eaters, diet quality in the treatment group improved, while diet quality in the control group remained low. Diet quality of non-picky eaters in the intervention group changed to a lesser degree.
Acknowledgments
This research was supported by the intramural research program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development, contract #’s HHSN267200703434C and HHSN2752008000031/HHSN275002. The authors acknowledge the contributions of the clinical site research staff and the families who participated in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions
TRN led development, implementation, and oversight of the study. DHL and LML contributed to study development, implementation, and oversight. TRN, MHE, and KD drafted the manuscript. AL developed the analysis plan and performed statistical analysis. All authors contributed to manuscript revisions. All authors read and approved the final manuscript.
Conflict of interest disclosures
The authors have no financial interest or conflicts to disclose.
ClinicalTrials.gov identifier: NCT00999375
Contributor Information
Tonja R. Nansel, Health Behavior Branch; Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6937, fax 301-402-2084.
Leah M. Lipsky, Health Behavior Branch; Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6951, fax 301-402-2084.
Denise L. Haynie, Health Behavior Branch; Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6933, fax 301-402-2084.
Miriam H. Eisenberg, Health Behavior Branch, Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6940, fax 301-402-2084.
Katie Dempster, Health Behavior Branch, Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6875, fax 301-402-2084.
Aiyi Liu, Biostatistics and Bioinformatics Branch, Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, 6710B Rockledge Dr., MSC 7004, Bethesda, MD 20892, phone 301-435-6952, fax 301-402-2084.
References
- 1.Mayer-Davis EJ, Liese NM, Bell RA, et al. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J.Am.Diet.Assoc. 2006;106:689–697. doi: 10.1016/j.jada.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Nansel TR, Haynie DL, Lipsky LM, Laffel LMB, Mehta SM. Multiple indicators of poor diet quality in children and adolescents with type 1 diabetes are associated with higher body mass index percentile but not glycemic control. Journal of the Academy of Nutrition and Dietetics. 2012;112:1728–1735. doi: 10.1016/j.jand.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helgeson VS, Viccaro L, Becker D, Escobar O, Siminerio L. Diet of adolescents with and without diabetes: Trading candy for potato chips? Diabetes Care. 2006;29:982–987. doi: 10.2337/diacare.295982. [DOI] [PubMed] [Google Scholar]
- 4.Katz ML, Mehta S, Nansel T, Quinn H, Lipsky LM, Laffel LM. Associations of nutrient intake with glycemic control in youth with type 1 diabetes: differences by insulin regimen. Diabetes technology & therapeutics. 2014;16:512–518. doi: 10.1089/dia.2013.0389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rovner AJ, Nansel TR. Are children with type 1 diabetes consuming a healthful diet?: a review of the current evidence and strategies for dietary change. Diabetes Educ. 2009;35:97–107. doi: 10.1177/0145721708326699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ADA. Nutrition recommendations and interventions for diabetes: A position statement of the American Diabetes Association. Diabetes Care. 2008;31:S61–S78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- 7.Smart C, Aslander-van Vliet E, Waldron S. Nutritional management in children and adolescents with diabetes. Pediatr Diabetes. 2009;10(Suppl 12):100–117. doi: 10.1111/j.1399-5448.2009.00572.x. [DOI] [PubMed] [Google Scholar]
- 8.Patton SR. Adherence to diet in youth with type 1 diabetes. Journal of the American Dietetic Association. 2011;111:550–555. doi: 10.1016/j.jada.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cardona Cano S, Hoek HW, Bryant-Waugh R. Picky eating: the current state of research. Current opinion in psychiatry. 2015;28:448–454. doi: 10.1097/YCO.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 10.Dovey TM, Staples PA, Gibson EL, Halford JCG. Food neophobia and 'picky/fussy' eating in children: A review. Appetite. 2008;50:181–193. doi: 10.1016/j.appet.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Patton SR, Clements MA, George K, Goggin K. "I Don't Want Them to Feel Different": A Mixed Methods Study of Parents' Beliefs and Dietary Management Strategies for Their Young Children with Type 1 Diabetes Mellitus. J Acad Nutr Diet. 2016;116:272–282. doi: 10.1016/j.jand.2015.06.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tharner A, Jansen PW, Kiefte-de Jong JC, et al. Toward an operative diagnosis of fussy/picky eating: a latent profile approach in a population-based cohort. The international journal of behavioral nutrition and physical activity. 2014;11:14. doi: 10.1186/1479-5868-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mascola AJ, Bryson SW, Agras WS. Picky eating during childhood: A longitudinal study to age 11years. Eating Behaviors. 2010;11:253–257. doi: 10.1016/j.eatbeh.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galloway AT, Lee Y, Birch LL. Predictors and consequences of food neophobia and pickiness in young girls. Journal of the American Dietetic Association. 2003;103:692–698. doi: 10.1053/jada.2003.50134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galloway AT, Fiorito L, Lee Y, Birch LL. Parental pressure, dietary patterns, and weight status among girls who are "picky eaters". J Am Diet Assoc. 2005;105:541–548. doi: 10.1016/j.jada.2005.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobi C, Agras WS, Bryson S, Hammer LD. Behavioral validation, precursors, and concomitants of picky eating in childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:76–84. doi: 10.1097/00004583-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Carruth BR, Ziegler PJ, Gordon A, Barr SI. Prevalence of picky eaters among infants and toddlers and their caregivers' decisions about offering a new food. J Am Diet Assoc. 2004;104:s57–64. doi: 10.1016/j.jada.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 18.Quick V, Lipsky LM, Laffel LM, Mehta SN, Quinn H, Nansel TR. Relationships of neophobia and pickiness with dietary variety, dietary quality and diabetes management adherence in youth with type 1 diabetes. Eur J Clin Nutr. 2014;68:131–136. doi: 10.1038/ejcn.2013.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicklaus S, Boggio V, Chabanet C, Issanchou S. A prospective study of food variety seeking in childhood, adolescence and early adult life. Appetite. 2005;44:289–297. doi: 10.1016/j.appet.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell GL, Farrow C, Haycraft E, Meyer C. Parental influences on children's eating behaviour and characteristics of successful parent-focussed interventions. Appetite. 2013;60:85–94. doi: 10.1016/j.appet.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Nansel TR, Laffel LM, Haynie DL, et al. Improving dietary quality in youth with type 1 diabetes: randomized clinical trial of a family-based behavioral intervention. The international journal of behavioral nutrition and physical activity. 2015;12:58. doi: 10.1186/s12966-015-0214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Austin M, Harnack L, Jasthi B, et al. Nutrition Data System for Research. Minneapolis, MN: University of Minnesota; 2012. [Google Scholar]
- 23.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108:1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Lipsky L, Cheon K, Nansel TR, Albert P. Candidate measures of whole plant food intake are related to biomarkers of nutrition and health in the US population (NHANES 1999–2002) Nutrition Research. 2012;32:251–259. doi: 10.1016/j.nutres.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy SP, Foote JA, Wilkens LR, et al. Simple measures of dietary variety are associated with improved dietary quality. J Am Diet Assoc. 2006;106:425–429. doi: 10.1016/j.jada.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office Washington, DC; 2010. U.S.Department of Agriculture USDoHaHS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freedman LS, Guenther PM, Krebs-Smith SM, Kott PS. A population's mean Healthy Eating Index-2005 scores are best estimated by the score of the population ratio when one 24-hour recall is available. J Nutr. 2008;138:1725–1729. doi: 10.1093/jn/138.9.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 29.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. Journal of Nutrition. 2012;142:1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fulkerson J, Story M, Neumark-Sztainer D, Rydell S. Family Meals: Perceptions of Benefits and Challenges among Parents of 8- to 10-Year-Old Children. Journal of the American Dietetic Association. 2008;108:706–709. doi: 10.1016/j.jada.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Powell-Wiley TM, Miller PE, Agyemang P, Agurs-Collins T, Reedy J. Perceived and objective diet quality in US adults: a cross-sectional analysis of the National Health and Nutrition Examination Survey (NHANES) Public Health Nutr. 2014;17:2641–2649. doi: 10.1017/S1368980014000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kourlaba G, Kondaki K, Grammatikaki E, Roma-Giannikou E, Manios Y. Diet quality of preschool children and maternal perceptions/misperceptions: the GENESIS study. Public health. 2009;123:738–742. doi: 10.1016/j.puhe.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 33.Carruth BR, Skinner J, Houck K, Moran J, Coletta F, Ott D. The Phenomenon of “Picky Eater”: A Behavioral Marker in Eating Patterns of Toddlers. Journal of the American College of Nutrition. 1998;17:180–186. doi: 10.1080/07315724.1998.10718744. [DOI] [PubMed] [Google Scholar]