Abstract
Objectives:
To determine whether Telemedicine intervention can affect hospital mortality, length of stay, and direct costs for progressive care unit patients.
Design:
Retrospective observational.
Setting:
Large healthcare system in Florida.
Patients:
Adult patients admitted to progressive care unit (PCU) as their primary admission between December 2011 and August 2016 (n = 16,091).
Interventions:
Progressive care unit patients with telemedicine intervention (telemedicine PCU [TPCU]; n = 8091) and without telemedicine control (nontelemedicine PCU [NTPCU]; n = 8000) were compared concurrently during study period.
Measurements and Main Results:
Primary outcome was progressive care unit and hospital mortality. Secondary outcomes were hospital length of stay, progressive care unit length of stay, and mean direct costs. The mean age NTPCU and TPCU patients were 63.4 years (95% CI, 62.9–63.8 yr) and 71.1 years (95% CI, 70.7–71.4 yr), respectively. All Patient Refined-Diagnosis Related Group Disease Severity (p < 0.0001) and All Patient Refined-Diagnosis Related Group patient Risk of Mortality (p < 0.0001) scores were significantly higher among TPCU versus NTPCU. After adjusting for age, sex, race, disease severity, risk of mortality, hospital entity, and organ systems, TPCU survival benefit was 20%. Mean progressive care unit length of stay was lower among TPCU compared with NTPCU (2.6 vs 3.2 d; p < 0.0001). Postprogressive care unit hospital length of stay was longer for TPCU patients, compared with NTPCU (7.3 vs 6.8 d; p < 0.0001). The overall mean direct cost was higher for TPCU ($13,180), compared with NTPCU ($12,301; p < 0.0001).
Conclusions:
Although there are many studies about the effects of telemedicine in ICU, currently there are no studies on the effects of telemedicine in progressive care unit settings. Our study showed that TPCU intervention significantly decreased mortality in progressive care unit and hospital and progressive care unit length of stay despite the fact patients in TPCU were older and had higher disease severity, and risk of mortality. Increased postprogressive care unit hospital length of stay and total mean direct costs inclusive of telemedicine costs coincided with improved survival rates. Telemedicine intervention decreased overall mortality and length of stay within progressive care units without substantial cost incurrences.
Keywords: direct costs, hospital mortality, length of stay, progressive care unit, telemedicine
Patients admitted to hospitals have different disease severity and require different levels of care (1). A large proportion of low risk patients are admitted to ICUs just for monitoring purposes, thus increasing patient load and affecting functionality of ICUs (2). Similarly, a significant proportion of patients who require more intensive care are treated in the wards (3, 4). There is an increasing need for step-down units such as progressive care units (PCUs) due to diverse population characteristics, increased proportion of aging patient population, increasing cost of care, and shortage of intensivists (5). PCUs manage patients who need “intermediate” level of care—patients who require more extensive care than in general wards, but less than in ICUs (6). PCUs were created to provide cost-effective and high-standard care without negatively impacting patient outcomes for less severely ill patients who are admitted to ICUs for monitoring or more serious patients who are treated in the wards (2, 7).
To overcome increasing patient demands and shortage of intensivists, telemedicine, a relatively new method of care delivery, has been applied to critical care (8, 9). Approximately, 11% of critical care units in the United States have integrated telemedicine and many have reported positive health outcomes (10). Telemedicine includes managing patients through monitoring devices controlled by physicians and nurses in remote locations. Telemedicine has improved patient outcomes through advanced monitoring, cognitive affordances, clinical decision-support functions, execution of life saving, and evidence-based critical care protocols. In a retrospective study that looked for the effect of telemedicine on mortality and length of stay (LOS) in community hospital ICUs, it was observed that telemedicine significantly decreased odds of ICU mortality (odds ratio, 0.46; 95% CI, 0.32–0.66) when compared with pretelemedicine implementation stages (11). In addition, telemedicine also decreased LOS. Similarly, another study by Lilly et al (10) reported that hospital mortality rate significantly decreased from 13.6% before telemedicine implementation to 11.8% after intervention. ICU mortality also significantly reduced from 10.7% to 8.6% after the implementation. In a review article on acceptance of telemedicine coverage among ICU staff, it was observed that telemedicine in ICU (Tele-ICU) installations were rapidly accepted by ICU staff despite initial difficulties in autonomy, training, scrutiny, and malfunctions, primarily due to perceived benefits for patients among the ICU staff (12). Telemedicine coverage was associated with decreased ICU mortality and LOS as reported in a meta-analysis (13). Although many studies report improved patient quality and outcomes due to telemedicine (10, 11, 13–15), some studies have noted mixed and inconsistent benefits and stark variations in the application of telemedicine (16–21). Intricacy and variability in the application of telemedicine, along with differences in study designs, creates a challenge to determine the impact on quality and return on investment (22–25).
Although previous studies have reported challenges, advantages, and disadvantages of telemedicine implementation (9, 15, 22, 26–31), there are no studies exploring effect of these innovations on patient outcomes in PCUs. The main objective was to examine effects of telemedicine in PCU (TPCU) on hospital mortality, LOS, and direct costs among PCU patients using a retrospective observational study design at a large healthcare system. Results from our study could provide insights into association between telemedicine and patient outcomes.
METHODS
Study Design and Population
This study was reviewed and approved by the institutional review board. We performed a retrospective observational study, with primary data collected from patients admitted to PCUs between December 2011 and August 2016 across five hospitals in South Florida region. Not all PCU beds were equipped to receive telemedicine care; hence, patients who did not receive telemedicine (nontelemedicine PCU [NTPCU]) became suitable concurrent controls to those patients who received telemedicine (TPCU) in same unit or hospital. Hospital policies for those patients admitted or discharged to PCUs were based on American College of Critical Care Medicine guidelines (3). Inclusion criteria were all adult patients admitted in PCUs as their primary admission without a prior ICU admission. All patients required a minimum of 24 hours of PCU LOS to be included. If the encounter did not reach these thresholds, patients were excluded. When patients were downgraded to telemetry or med/surgical unit, they were consequently discharged from TPCU, regardless of bed availability. Patients were also excluded if demographics information was missing (Fig. 1).
Figure 1.
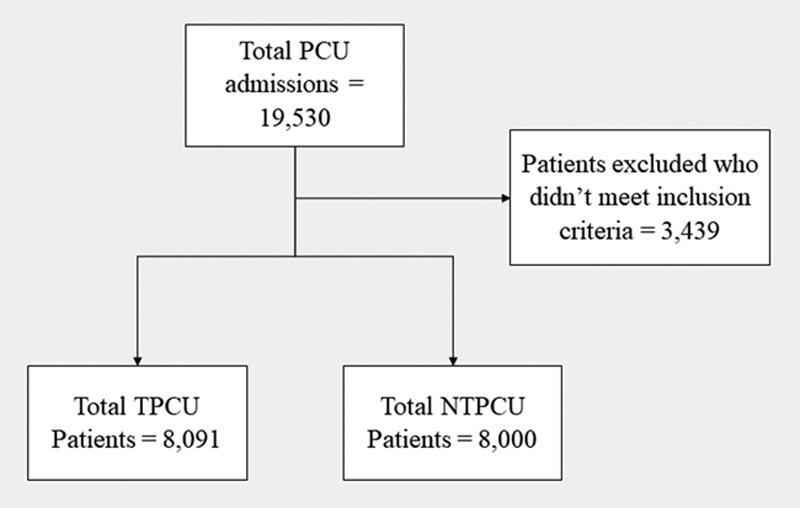
Inclusion of patients into telemedicine progressive care unit (PCU) (TPCU) and nontelemedicine PCU (NTPCU) groups.
Measures
Demographic variables included age, gender, and race/ethnicity. Measures included admission diagnosis, PCU and hospital LOS, PCU and hospital mortality, and the “total direct cost” of hospitalization. Total direct cost is comprised of “direct fixed” and “direct variable.” Direct fixed costs are for unit level operations, and the cost of telemedicine is reflected in direct fixed costs per licensed bed per patient stay; “direct variable” includes variable clinician staffing and patient care utilization costs.
We used the All Patient Refined-Diagnosis Related Group (APR-DRG) disease severity and APR-DRG risk of mortality (ROM) to stratify patients based on severity scores. Both APR-DRG disease severity and APR-DRG ROM were categorized into Minor (= 1), Moderate (= 2), Major (= 3), and Extreme (= 4) (32). Hospital mortality was defined as death in hospital due to any cause. Hospital LOS was calculated as difference between admission date and time and discharge date and time. PCU LOS was calculated from the time acuity status order was placed for each primary PCU stay until their status change was placed. Age was categorized into 18–40, 41–65, 66–85, and greater than and equal to 86 years. Race and ethnicity were categorized into White, Black, White Hispanic, Black Hispanic, and Other. Mortality (PCU and hospital), LOS (PCU and hospital), and mean total direct costs were outcome measures.
Statistical Analyses
We used univariate, bivariate, chi-square, and independent samples t test to describe the demographic characteristics, APR-DRG disease severity, and APR-DRG ROM. Bivariate statistics were also calculated for LOS and hospital mortality stratified by TPCU and NTPCU status. Survival analyses using a multivariate Cox proportional hazards model were conducted to calculate hazard ratios (HRs) for hospital mortality. HR were adjusted for hospital entity, demographics, organ systems, APR-DRG disease severity, and APR-DRG ROM. Sensitivity analysis was performed after randomly selecting 50% TPCU patients (n = 4,000) and matching (1:1) these with NTPCU patients based on propensity score. Propensity score was calculated from a logistic regression model which included age, sex, race, APR-DRG disease severity, and APR-DRG ROM. Up to 95% (or n = 3,800) TPCU patients were matched 1:1 with the pool of control patients based on their closest propensity score. In addition to propensity score matching, HRs were calculated from this subsample after adjusting for hospital entities and Agency for Healthcare Research and Quality clinical classification system (CCS) organ system categories in the model. Generalized linear mixed models were used for estimating differences in direct costs between two groups. For power and sample size calculation, it was hypothesized that after 15 days of admission into PCU, at least 5% difference in HR would be observed between two groups. A sample size of 7,993 in each group would be required to detect the difference at 90% power and 5% level of significance. SAS software version 9.4 (SAS Institute Inc., Cary, NC) was used for statistical analyses. Statistical significance was set at p value of less than 0.05.
RESULTS
Patient Characteristics
During the study period, 19,530 patients were admitted in the PCUs (2011–2016). After excluding patients who did not meet the study criteria, 16,091 patients were included in the study, 8,091 (50.3%) patients admitted to TPCU, and 8,000 (49.7%) into NTPCU. The mean age of the participants admitted to NTPCU and TPCU was 63.4 years (95% CI, 62.9–63.8 yr) and 71.1 years (95% CI, 70.7–71.4 yr), respectively (Table 1). Among patients admitted to TPCU, 50.6% were females, 63.5% were Hispanics, 25.7% Whites, and 7.1% Blacks. Among those admitted to NTPCUs, 53.5% were females and 57.9% were Hispanics, 27.6% Whites, and 10.5% Blacks. APR Disease Severity (p < 0.0001) and APR patient ROM (p < 0.0001) scores were significantly different between patients admitted to TPCU and NTPCU.
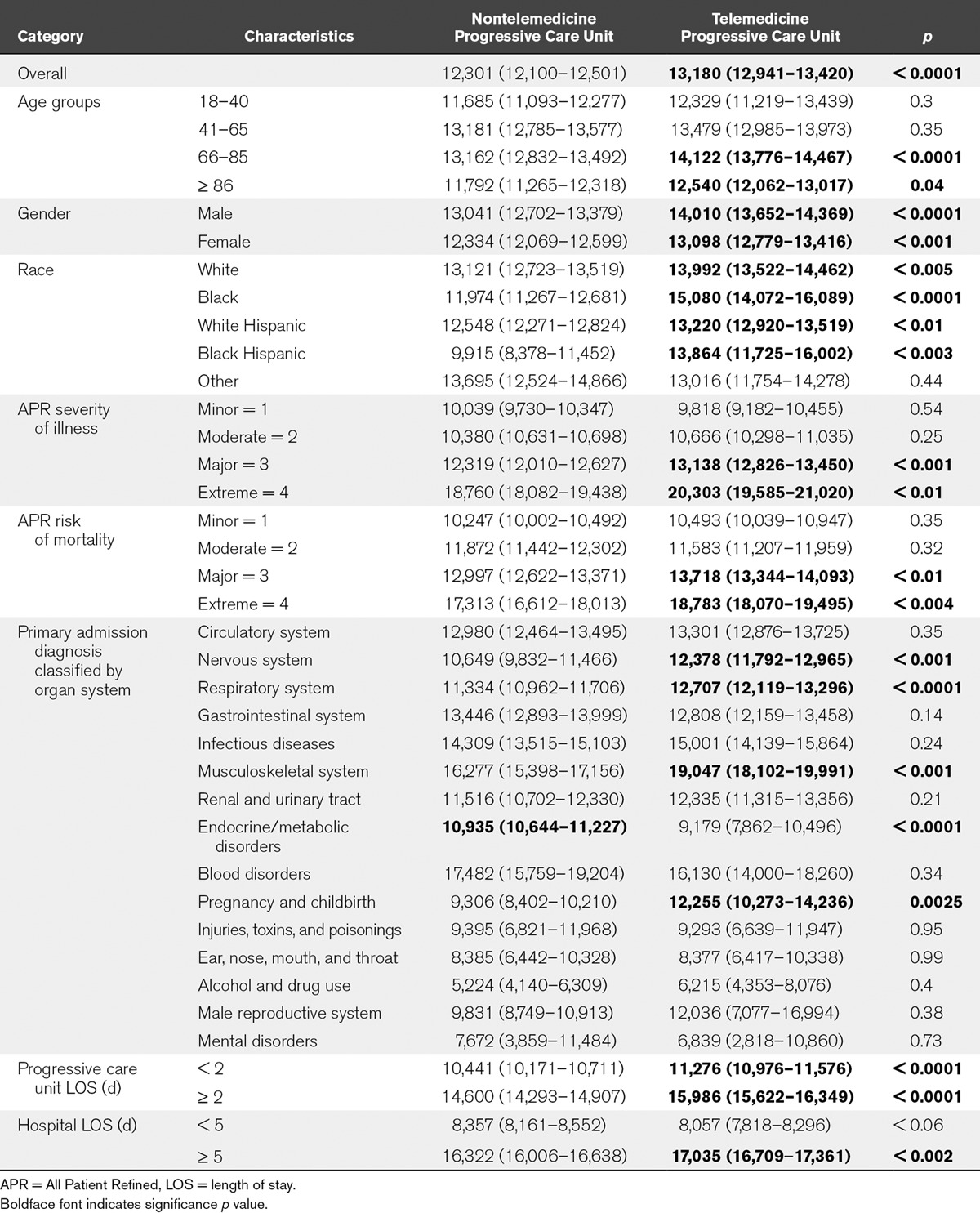
TABLE 1.
Characteristics of Telemedicine Progressive Care Unit and Nontelemedicine Progressive Care Unit Patients (n = 16,091)
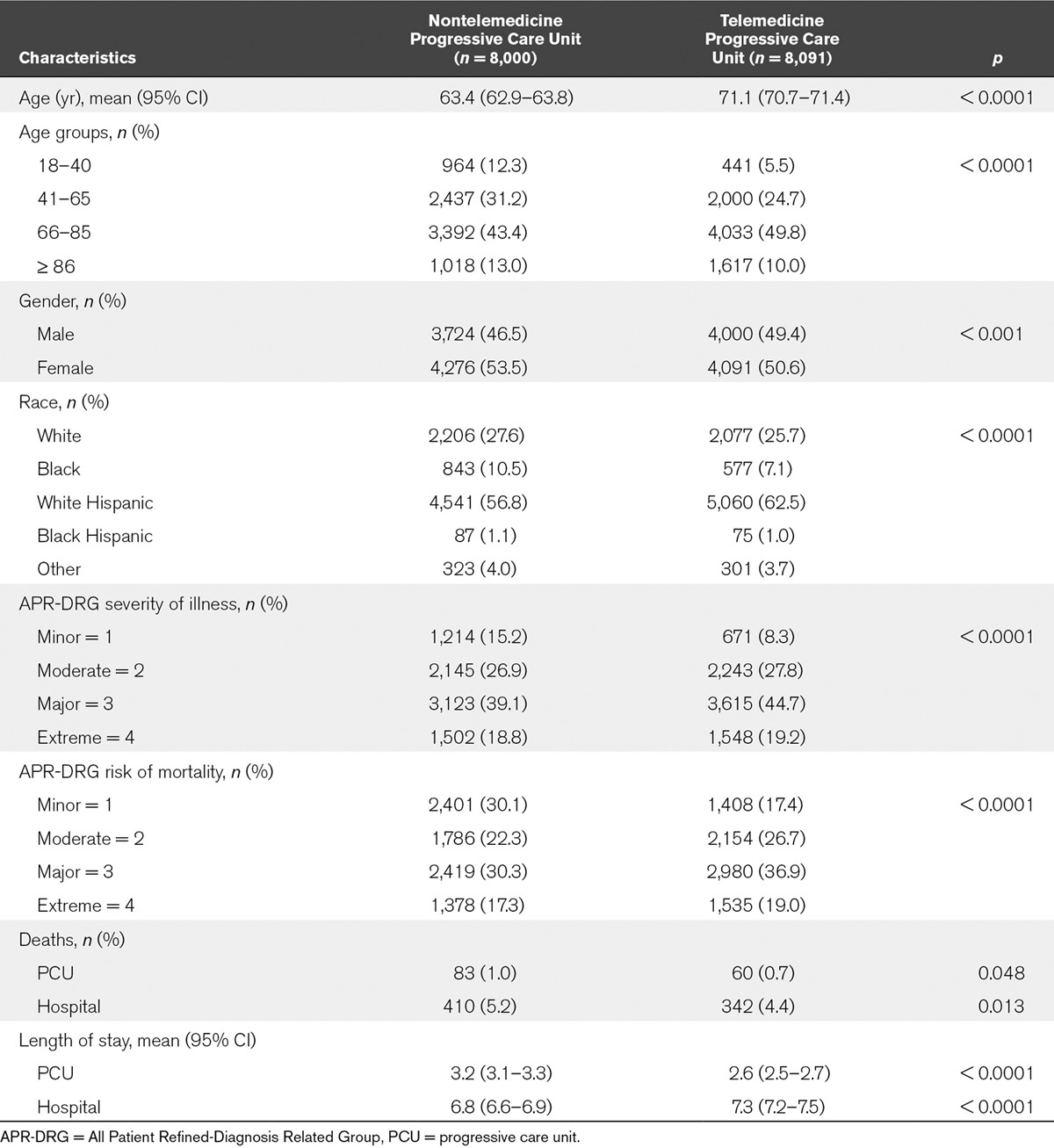
Mortality and LOS
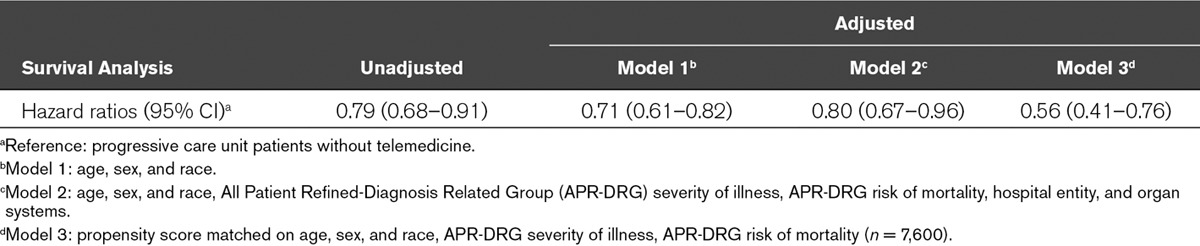
During the study period, 60 patients (0.7%) died in TPCU, compared with 83 patients (1%) in NTPCU (Table 1). The difference in proportion of patients who died in the TPCUs, compared with NTPCUs, was statistically significant (p = 0.048). Hospital mortality rates were 4.4% for TPCUs and 5.2% for NTPCUs, and the differences were statistically significant (p = 0.013). Mean PCU LOS was higher among NTPCU patients compared with TPCU (3.2 vs 2.6 d; p < 0.0001). Post-PCU hospital LOS was longer for TPCU patients, compared with NTPCU patients (7.3 vs 6.8 d; p < 0.0001). Unadjusted Cox proportion survival analysis showed that patients admitted to TPCUs were 21% more likely to survive compared with those admitted to NTPCUs (Fig. 2). After adjusting for age, sex, race, APR-DRG disease severity, APR-DRG ROM, hospital entities, and organ systems, the survival benefit decreased slightly to 20% (Table 2). Within each Clinical Classifications Software (CCS) for International Classification of Diseases, 9th Edition and International Classification of Diseases, 10th Edition categories, patients with diseases and disorders of the kidney and urinary tract (n = 679; HR, 0.40; 95% CI, 0.17–0.90; p = 0.028), nervous system (n = 1435; HR, 0.50; 95% CI, 0.27–0.91; p = 0.023), and circulatory system (n = 4,601; HR, 0.69; 95% CI, 0.50–0.95; p = 0.021) showed the highest survival benefit. Among five entities, highest survival benefit of 30% was seen at the facility which was an urban community full services hospital that were predominantly patients with cardiovascular and neurovascular illnesses in PCU. Sensitivity analysis was performed on a pool of 7,600 propensity score matched patients (3,800 in each group). Results from the sensitivity analysis showed that after accounting for age, sex, race, APR-DRG disease severity, APR-DRG ROM, hospital entities, and organ systems, patients in TPCU group were 44% (24–59%) more likely to survive compared with NTPCU patients.
Figure 2.
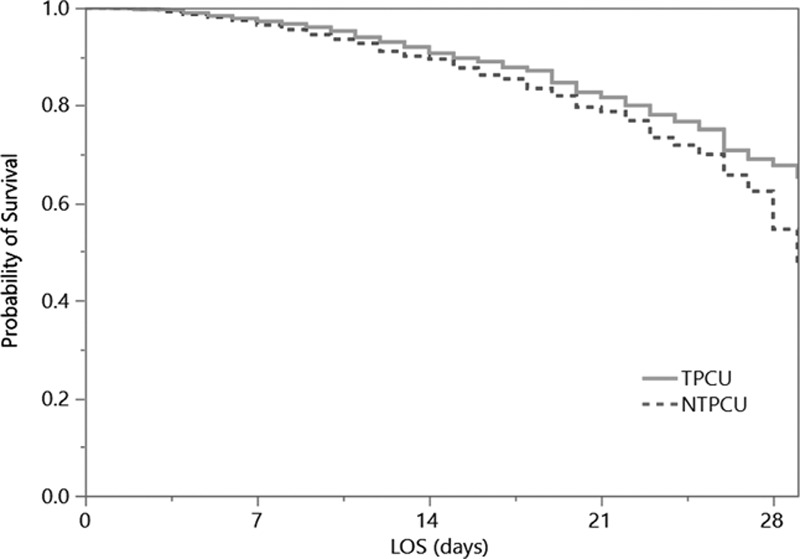
Survival curves for Cox proportional hazards model with telemedicine at progressive care unit (PCU) (TPCU) admission (solid line) and without telemedicine at PCU (NTPCU) admission (dotted line). LOS = length of stay.
TABLE 2.
Cox Proportional Survival Analysis With Unadjusted and Adjusted Hazard Ratios for Hospital Mortality in Telemedicine Progressive Care Unit (n = 16,091)
Cost of Telemedicine in PCUs
The overall mean direct costs were higher for patients admitted to TPCUs, compared with NTPCUs ($13,180 vs $12,301; p < 0.0001) (Table 3). Mean direct costs were higher for TPCUs in the age groups, 18–40, 41–65, and 66–85 years (p < 0.0001), but among greater than and equal to 86 years age group, it was higher for NTPCU group. TPCU patients with APR-DRG disease severity scores of major (p < 0.001) and extreme (p < 0.01) had significantly higher mean direct costs than patients did in NTPCU. Similarly, mean direct costs for patients with APR-DRG ROM scores of major (p < 0.01) and extreme (p < 0.01) were significantly higher in patents admitted to TPCU when compared with NTPCUs. Patients with nervous, respiratory, and musculoskeletal system disorders, and diagnosis of pregnancy and childbirth in TPCU had higher mean direct costs; and in NTPCU group, it was higher among patients with endocrine and metabolic disorders.
TABLE 3.
Mean (95% CI) Direct Costs Associated With Patient Admissions Stratified by Telemedicine Progressive Care Unit and Nontelemedicine Progressive Care Unit (in U.S. Dollars; n = 16,091)
DISCUSSION
Although there are many studies about the effects of Tele-ICU, currently, to the best of our knowledge, this is the first study to examine the impact of telemedicine on mortality, LOS, and direct costs in patients with PCU (TPCU) admissions. The ICU admission, discharge, and triage guidelines set forth by Nates et al (3) and endorsed by the Society of Critical Care Medicine recommend patients with high severity of illness, multiple comorbidities, and need for organ support be cared for in a “step-down unit.” These types of units are variably referred to as “high dependency, intermediate, or transitional care units.” The label PCU has been applied to encompass all the variations. Just as varied as the labels are the configurations and capabilities across healthcare settings. Little formal investigation exists to describe and evaluate the effectiveness of PCUs (3). It is hypothesized that ICU services, bed utilization, and patient care outcomes may be positively impacted through use of PCUs (4, 33–35); similarly Tele-ICU has shown to impact these factors positively (10, 11, 13–15, 36) and therefore, Tele-PCU may also provide a distinct advantage. We found that PCU and hospital mortality rates were significantly lower for patients in TPCU group, compared with patients in NTPCUs. PCU LOS was also significantly lower for TPCU patients, compared with NTPCU patients. We found that mean post-PCU hospital LOS and total mean direct cost were higher for patients admitted to TPCUs that coincided with improved survival.
Several reasons PCUs were established or became part of the hospital system are because studies indicated that a significant proportion of adult ICU occupancies were lower severity patients admitted for monitoring rather than active treatment (37). Often these patients were admitted postoperatively for observation and had very small mortality rates of 0.03 with short ICU and hospital LOS (2). Solberg et al (38) concluded that the introduction of PCU has increased the operational efficiency of the ICU with fewer low risk patients being admitted. A recent prospective multinational European study demonstrated that adults admitted to ICUs of hospitals with an intermediate care unit (IMCU) have significantly lower adjusted hospital mortality 0.63 (95% CI, 0.45–0.88; p = 0.007) than those admitted to ICUs of hospitals without an IMCU after severity and characteristics adjustments (39). Closures of PCUs also seemed to have a negative impact on the ICUs (39). However, further evidence is required to cement the view that PCUs lead to improved patient outcomes and optimal healthcare delivery (6, 40).
Similar to our findings, previous studies conducted in ICU settings have shown that Tele-ICU was associated with improved patient outcomes. For example, in a prospective stepped-wedge clinical practice study, installation of Tele-ICU was associated with decreased mortality and hospital LOS (10). This was attributed to improved adherence to best practices in critical care such as prevention of venous thrombosis, cardiovascular complications, ventilator associated pneumonia, stress ulcers, timely administration of antimicrobial medications, and resuscitation procedures (10). Improvements in clinical outcomes due to Tele-ICU implementation in ICUs were also observed in a large scale study involving more than 24,000 patients (41). This study demonstrated a decrease in severity-adjusted ICU LOS, along with a decrease of 0.77 in relative risk of hospital mortality (41). Probable mechanisms for this improvement include greater levels of participation of the Tele-ICU team in implementing patient care and improved coordination with bedside caregivers (41). In another study, it was observed that severity-adjusted ICU LOS significantly improved from 0.84 to –0.03 (or 4,772 saved ICU days; p < 0.001) and severity-adjusted hospital LOS improved from 0.97 to –0.64 (or 6,091 saved floor days; p = 0.001) (42). In a study evaluating 15 rural multistate ICUs, Tele-ICU implementation was associated with lower mortality and LOS in ICUs (21). A meta-analysis of 13 studies involving 35 ICUs showed similar findings where Tele-ICU implementation was associated with lower ICU mortality rates and LOS; there was no effect of Tele-ICU outside of ICU on hospital mortality rates or hospital LOS (13).
While implementing TPCUs, both costs and patient outcome characteristics should be considered. Previous studies in this field revealed considerable variability concerning the benefits to mortality or LOS after Tele-ICU implementation in relationship to cost (43, 44). For example, an observational study of 4,142 ICU patients reported 24% increase in daily hospital costs, 43% increase in cost per case, and 28% increase in cost per patient (44). A retrospective study using administrative database from 106 adult ICU beds showed that capital costs for telemedicine units were $1,186,220 and annual operational costs were $1,250,112, thus accounting to $23,150 per telemedicine unit (43). Benefits to mortality or LOS after Tele-ICU implementation may be associated with increased cost; however, it has also been noted the initial costs in establishing and operating TPCUs may be reclaimed over the years through cost savings due to favorable patient outcomes (23, 24, 45, 46). The conduct of Tele-ICU cost analyses has been recognized as an “imperfect science,” (47) requires “alternative research designs,” (48) and is an “analyses of a complex intervention.” (24)
For our study, the total enterprise-wide annual operation cost for telemedicine was equally distributed across the organization as a cost per licensed bed per patient unit stay. This cost was reflected in the “direct fixed” within the “total direct costs.” Because we wished to ascertain the exact added cost of telemedicine, inclusion of the “direct fixed” within the “total direct costs” was necessary. This turned out to be an advantage as we have accounted for both “direct variable” (direct patient care utilization) and “direct fixed” (cost of TPCU and cost of PCU level care). We believe inclusion of PCU level operational costs may be considered relevant for examination of the overall cost of care delivery. PCU cost of care delivery is fundamentally lower than that of ICU and higher than telemetry or med/surg. The cost of TPCU added to PCU is another layer of additional costs. However, our study demonstrated, despite the additional cost of TPCU, the total mean direct costs in the TPCU group only increased by a nominal amount of 300 dollars per patient per day when the estimated TPCU cost was $650 per patient per unit stay more than NTPCU in this healthcare system.
Yoo et al (25) compared Tele-ICU to non-Tele-ICU cost effectiveness through probabilistic analyses conducted on available literature to calculate incremental cost effectiveness ratios and quality-adjusted life years over a 5-year span. Yoo et al (25) calculated weighted averages from studies reporting both favorable and unfavorable costs/benefit ratios. Their resultant comparison for with and without tele models was comprised of the product of cost(s) multiplied by reported benefits available in literature to create impact ratios (0.94; 0.71–1.14) for ICU and (1.02; 0.80–1.30) for floor post-ICU for alive patients (25). Combining the mean estimated costs for ICU and post-ICU plus tele-operational costs, the difference between total hospital cost with Tele-ICU and without was only 304 dollars per patient per hospital stay. To the extent that Yoo et al (25) data provide valid results as they are constructed upon the extant literature beleaguered with inherent variability and theoretical assumptions, our results based on primary data are in agreement with the direction of their hypothetical results.
Our study has some limitations. The current study was conducted on retrospective data and had limitations of an observational study design. The lack of ability to control for clinician selection of telemedicine intervention in PCU or the lack of technologically equipped bed availability in some locations is inherent in this study. The PCU bed configuration is complex in this health system and likely complex in other organizations based on available literature (3). Our system is mixture of beds and/or units with TPCU and NTPCU; therefore, selection bias may be of concern. Although each entity had both TPCU monitored and NTPCU beds under various configurations, all other services provided and staffing were considered relatively equal within entity and units. Additionally, majority of our patients were of Hispanic ethnicity, which is not representative of the general population.
The main strengths of our study were large sample size, rigorous analytical procedures, severity adjustments, and homogenous TPCU and NTPCU patient characteristics. Despite older and more severely ill patient population in TPCU group, we found statistically significant benefits. The circumstances of this study that not all PCU beds or units were equipped with TPCU capability, which created a suitable concurrent control group and propensity score matched analysis, may have minimized this selection bias. In addition to this, pooling data from five different hospitals allowed us to minimize selection bias. Furthermore, there were equal distribution of deaths among the PCU sites based on their bed capacity. Although the use of TPCU versus NTPCU was driven by both availability and clinical judgment, PCU designation is based on acuity and was severity adjusted in this study. PCU is not only a relevant strategy to reduce ICU LOS and readmissions and optimize ICU bed utilization, it serves the needs of many patients that do not require ICU level care but are at a high risk of deterioration. Tele-ICU innovation has improved ICU treatment in critical care, have reduced ICU mortality and ICU LOS based on numerous studies. Using these evidences, we can theorize on the efficiency and role in reducing morbidity and mortality in the PCU if a TPCU intervention approach is used.
CONCLUSIONS
Although there are many studies about the effects of telemedicine in ICU, currently there are no studies on the effects of telemedicine in PCU settings. Our study showed that TPCU intervention significantly decreased mortality in PCU and hospital and PCU LOS despite the fact patients in TPCU were older and had higher disease severity, and ROM. Increased post-PCU hospital LOS and total mean direct costs inclusive of telemedicine costs coincided with improved survival rates. Evidence from our study suggests that Telemedicine decreases overall mortality and LOS within PCU without substantial cost incurrences.
Footnotes
*See also p. 816.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Zimmerman JE, Wagner DP, Knaus WA, et al. The use of risk predictions to identify candidates for intermediate care units. Implications for intensive care utilization and cost. Chest 1995; 108:490–499. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal GE, Sirio CA, Shepardson LB, et al. Use of intensive care units for patients with low severity of illness. Arch Intern Med 1998; 158:1144–1151. [DOI] [PubMed] [Google Scholar]
- 3.Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 2016; 44:1553–1602. [DOI] [PubMed] [Google Scholar]
- 4.Prin M, Wunsch H.The role of stepdown beds in hospital care. Am J Respir Crit Care Med 2014; 190:1210–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stacy KM.Progressive care units: Different but the same. Crit Care Nurse 2011; 31:77–83. [DOI] [PubMed] [Google Scholar]
- 6.Vincent JL, Rubenfeld GD.Does intermediate care improve patient outcomes or reduce costs? Crit Care 2015; 19:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teres D, Steingrub J.Can intermediate care substitute for intensive care? Crit Care Med 1987; 15:280. [DOI] [PubMed] [Google Scholar]
- 8.Fuhrman SA, Lilly CM.ICU telemedicine solutions. Clin Chest Med 2015; 36:401–407. [DOI] [PubMed] [Google Scholar]
- 9.Kahn JM.Intensive care unit telemedicine: Promises and pitfalls. Arch Intern Med 2011; 171:495–496. [DOI] [PubMed] [Google Scholar]
- 10.Lilly CM, Cody S, Zhao H, et al. University of Massachusetts Memorial Critical Care Operations Group: Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011; 305:2175–2183. [DOI] [PubMed] [Google Scholar]
- 11.Sadaka F, Palagiri A, Trottier S, et al. Telemedicine intervention improves ICU outcomes. Crit Care Res Pract 2013; 2013:456389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young LB, Chan PS, Cram P.Staff acceptance of tele-ICU coverage: A systematic review. Chest 2011; 139:279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young LB, Chan PS, Lu X, et al. Impact of telemedicine intensive care unit coverage on patient outcomes: A systematic review and meta-analysis. Arch Intern Med 2011; 171:498–506. [DOI] [PubMed] [Google Scholar]
- 14.Wilcox ME, Adhikari NK.The effect of telemedicine in critically ill patients: Systematic review and meta-analysis. Crit Care 2012; 16:R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lilly CM, McLaughlin JM, Zhao H, et al. UMass Memorial Critical Care Operations Group: A multicenter study of ICU telemedicine reengineering of adult critical care. Chest 2014; 145:500–507. [DOI] [PubMed] [Google Scholar]
- 16.Marcin JP, Nesbitt TS, Kallas HJ, et al. Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr 2004; 144:375–380. [DOI] [PubMed] [Google Scholar]
- 17.Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: Results from two community hospitals. Crit Care Med 2010; 38:2–8. [DOI] [PubMed] [Google Scholar]
- 18.Nassar BS, Vaughan-Sarrazin MS, Jiang L, et al. Impact of an intensive care unit telemedicine program on patient outcomes in an integrated health care system. JAMA Intern Med 2014; 174:1160–1167. [DOI] [PubMed] [Google Scholar]
- 19.Shaffer JP, Johnson JW, Kaszuba F, et al. Remote ICU management improves outcomes in patients with cardiopulmonary arrest. Critical Care Medicine 2005; 33:A5 [Google Scholar]
- 20.Thomas EJ, Lucke JF, Wueste L, et al. Association of telemedicine for remote monitoring of intensive care patients with mortality, complications, and length of stay. JAMA 2009; 302:2671–2678. [DOI] [PubMed] [Google Scholar]
- 21.Zawada ET, Jr, Herr P, Larson D, et al. Impact of an intensive care unit telemedicine program on a rural health care system. Postgrad Med 2009; 121:160–170. [DOI] [PubMed] [Google Scholar]
- 22.Kahn JM, Le TQ, Barnato AE, et al. ICU telemedicine and critical care mortality: A national effectiveness study. Med Care 2016; 54:319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lilly CM, Motzkus C, Rincon T, et al. UMass Memorial Critical Care Operations Group: ICU telemedicine program financial outcomes. Chest 2017; 151:286–297. [DOI] [PubMed] [Google Scholar]
- 24.Lilly CM, Motzkus CA.ICU telemedicine: Financial analyses of a complex intervention. Crit Care Med 2017; 45:1558–1561. [DOI] [PubMed] [Google Scholar]
- 25.Yoo BK, Kim M, Sasaki T, et al. Economic evaluation of telemedicine for patients in ICUs. Crit Care Med 2016; 44:265–274. [DOI] [PubMed] [Google Scholar]
- 26.Kahn JM, Cicero BD, Wallace DJ, et al. Adoption of ICU telemedicine in the United States. Crit Care Med 2014; 42:362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mullen-Fortino M, DiMartino J, Entrikin L, et al. Bedside nurses’ perceptions of intensive care unit telemedicine. Am J Crit Care 2012; 21:24–31; quiz 32. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen YL, Kahn JM, Angus DC.Reorganizing adult critical care delivery: The role of regionalization, telemedicine, and community outreach. Am J Respir Crit Care Med 2010; 181:1164–1169. [DOI] [PubMed] [Google Scholar]
- 29.Kahn JM, Hill NS, Lilly CM, et al. The research agenda in ICU telemedicine: A statement from the Critical Care Societies Collaborative. Chest 2011; 140:230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahn JM.The use and misuse of ICU telemedicine. JAMA 2011; 305:2227–2228. [DOI] [PubMed] [Google Scholar]
- 31.Kahn JM.Virtual visits–confronting the challenges of telemedicine. N Engl J Med 2015; 372:1684–1685. [DOI] [PubMed] [Google Scholar]
- 32.Baram D, Daroowalla F, Garcia R, et al. Use of the all patient refined-diagnosis related group (APR-DRG) Risk of Mortality Score as a severity adjustor in the medical ICU. Clin Med Circ Respirat Pulm Med 2008; 2:19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Confalonieri M, Trevisan R, Demsar M, et al. Opening of a respiratory intermediate care unit in a general hospital: Impact on mortality and other outcomes. Respiration 2015; 90:235–242. [DOI] [PubMed] [Google Scholar]
- 34.Hager DN, Chandrashekar P, Bradsher RW, 3rd, et al. Intermediate care to intensive care triage: A quality improvement project to reduce mortality. J Crit Care 2017; 42:282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quimby AE, Shamy MC, Rothwell DM, et al. A novel neuroscience intermediate-level care unit model: Retrospective analysis of impact on patient flow and safety. Neurohospitalist 2017; 7:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kalb T, Raikhelkar J, Meyer S, et al. A multicenter population-based effectiveness study of teleintensive care unit-directed ventilator rounds demonstrating improved adherence to a protective lung strategy, decreased ventilator duration, and decreased intensive care unit mortality. J Crit Care 2014; 29:691.e7–691.14. [DOI] [PubMed] [Google Scholar]
- 37.Halpern NA, Pastores SM.Critical care medicine beds, use, occupancy, and costs in the united states: A methodological review. Crit Care Med 2015; 43:2452–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Solberg BC, Dirksen CD, Nieman FH, et al. Introducing an integrated intermediate care unit improves ICU utilization: A prospective intervention study. BMC Anesthesiol 2014; 14:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Capuzzo M, Volta C, Tassinati T, et al. Working Group on Health Economics of the European Society of Intensive Care Medicine: Hospital mortality of adults admitted to intensive care units in hospitals with and without intermediate care units: A multicentre European cohort study. Crit Care 2014; 18:551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ranzani OT, Zampieri FG, Taniguchi LU, et al. The effects of discharge to an intermediate care unit after a critical illness: A 5-year cohort study. J Crit Care 2014; 29:230–235. [DOI] [PubMed] [Google Scholar]
- 41.Willmitch B, Golembeski S, Kim SS, et al. Clinical outcomes after telemedicine intensive care unit implementation. Crit Care Med 2012; 40:450–454. [DOI] [PubMed] [Google Scholar]
- 42.Howell G, Ardilles T, Bonham AJ.Implementation of a remote intensive care unit monitoring system correlates with improvements in patient outcomes. Chest 2008; 134:s58003–s58003. [Google Scholar]
- 43.Fortis S, Weinert C, Bushinski R, et al. A health system-based critical care program with a novel tele-ICU: Implementation, cost, and structure details. J Am Coll Surg 2014; 219:676–683. [DOI] [PubMed] [Google Scholar]
- 44.Franzini L, Sail KR, Thomas EJ, et al. Costs and cost-effectiveness of a telemedicine intensive care unit program in 6 intensive care units in a large health care system. J Crit Care 2011; 26:329.e1–329.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breslow MJ, Rosenfeld BA, Doerfler M, et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: An alternative paradigm for intensivist staffing. Crit Care Med 2004; 32:31–38. [DOI] [PubMed] [Google Scholar]
- 46.Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: Alternate paradigm for providing continuous intensivist care. Crit Care Med 2000; 28:3925–3931. [DOI] [PubMed] [Google Scholar]
- 47.Ries M.Evaluating tele-ICU cost–an imperfect science. Crit Care Med 2016; 44:441–442. [DOI] [PubMed] [Google Scholar]
- 48.Tuckson RV, Edmunds M, Hodgkins ML.Telehealth. N Engl J Med 2017; 377:1585–1592. [DOI] [PubMed] [Google Scholar]


