Abstract
Background:
Masked depression is often misdiagnosed due to the predominance of somatic symptoms and is further complicated by lack of awareness among doctors.
Aim:
The present survey was conducted to gather the views of psychiatrists and nonpsychiatrists regarding presentation and management aspects of masked depression. This may help in unmasking this condition and facilitate early identification and appropriate management of patients presenting with this condition.
Materials and Methods:
This questionnaire-based survey was conducted as an interview through computer-aided telephonic interview among 300 doctors (150 psychiatrists and 150 nonpsychiatrists) across India.
Results:
Both psychiatrists and nonpsychiatrists reported a high prevalence of somatic symptoms among patients with masked depression. Nonpsychiatrists (44%) more often than psychiatrists (20%) noted chronic pain in the majority of patients with masked depression. Psychiatrists (31%) more often than nonpsychiatrists (9%) noted lack of concentration in the majority of patients with masked depression. Sexual dysfunction among young patients and noncompliance to therapy for chronic illness were considered as potential predictors of masked depression. There was a general agreement among psychiatrists and nonpsychiatrists that medical liaising is beneficial for the management of patients with masked depression.
Conclusion:
Both psychiatrists and nonpsychiatrists agree that somatic symptoms are commonly encountered in patients with masked depression. However, these somatic symptoms are often interpreted as physical illness rather than as an entity of depression which creates an unmet need in terms of managing masked depression, especially by nonpsychiatrists.
Keywords: Masked depression, medical liaising, misdiagnosis, nonpsychiatrists, psychiatrists, somatic symptoms
INTRODUCTION
Several terms have been used to describe atypical depression, such as depression equivalent, a vegetative equivalent, a depression without a depression, and a hidden depression.[1] The term “masked depression” was largely used in the 1970s and 1980s to describe patients who complained of somatic symptoms, without any identifiable organic disorder.[2] This atypical depression was believed to be the underlying cause of illnesses in patients with unexplained somatic symptoms, even if the symptoms of depression were either absent or present at lesser intensity and were not of primary concern.[1] However, masked depression is no more recognized in the Diagnostic and Statistical Manual of Mental Disorders 5th edition.[3] Further, the International Classification of Diseases 10th Revision only briefly mentions “single episodes of masked depression not otherwise specified” under the category of “other depressive episodes.”[4] Masked depression accounts for up to 6%–7% of the depressive disorders,[1] and 30%–40% of outpatients seek medical advice from specialists (not psychiatrists).[5]
It is believed that the clinical picture, in two-thirds of patients with depression, is dominated by somatic symptoms, such as lack of energy and general aches and pains. However, the language and terms used in the literature to describe somatic symptoms in depression are confusing and contradictory. Some of the somatic symptoms in patients with masked depression include painful symptoms such as general aches, pains including headache, backache, musculoskeletal aches, and nonpainful symptoms including changes in appetite and libido, lack of energy, sleep disturbance, dizziness, palpitations, dyspnea, and gastrointestinal tract disturbances.[6]
Underrecognition and undertreatment of depression are common in primary care settings, especially at the initial visit. Although time constraints during consultations are certainly a contributing factor, the inability of primary care physicians (PCPs) to pick and process patient cues for depression may also significantly contribute toward the underdiagnosis of depression. It has been noted that the recognition of depression is less likely in patients with predominant somatic symptoms compared with those with predominant psychological symptoms.[6] A study reported that PCPs missed the diagnosis of depression in >50% of psychiatric patients who presented with somatic symptoms.[7] Even when depression is recognized, appropriate diagnosis and treatment are achieved in only 30%–40% of patients.[8]
While the description and linguistic terms used for somatic disorders are familiar to the psychiatrists, PCPs are not well familiar with these signs and often label them as “medically unexplained physical complaints.” Unlike secondary/specialized care, a PCP is generally aware of the background and history of the patient, but the narratives of patients in primary care may be complex and influenced by multiple social and economic factors. Therefore, making a diagnosis of depression in primary care differs considerably from that of secondary care.[6]
The confusing and redundant terminology for masked depression and associated somatic symptoms reflects the complexity of clinical diagnosis as well as influences decision-making in masked depression.[6] Inaccurate diagnosis and treatment of masked depression result in serious somatic and psychological consequences for the patients and significantly limit patients’ social functioning, increase suicide rate, and further increase the costs of diagnosis and treatment.[1]
Objectives
Considering the high prevalence of somatic symptoms that may mask the depressive disorder and the multiple factors that contribute to the complications of the clinical picture, we sought to identify the symptoms of masked depression that might not be recognized by nonpsychiatrists. The objective of this survey was to analyze the views of nonpsychiatrists and psychiatrists regarding their patient experience with respect to masked depression. This would help in improving the treatment of these patients by increasing awareness of the disorder among the doctors.
MATERIALS AND METHODS
Survey participants
The survey was conducted among both psychiatrists and nonpsychiatrists. A total of 300 participants, comprising 150 psychiatrists and 150 nonpsychiatrists (124 general and family practitioners and 26 consultants), across India were part of the survey. About 50% of the participants had >15 years of clinical experience. The participants were from various cities in India and represented a wide geographic spread.
Survey method
The survey was conducted between February 2016 and April 2016.
This questionnaire-based survey was conducted among doctors from across India through computer-aided telephonic interview. The participants were first contacted over telephone and requested for a favorable time to conduct the survey over telecon. The participants were given a background about the study objectives. A set of questions [Box 1] regarding masked depression was prepared based on the review of literature. This set of survey questions was asked to all the participating doctors. Their responses were entered into the unique survey link in real time.
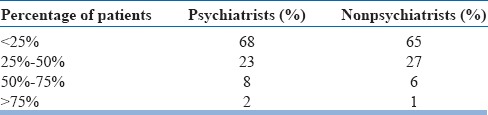
Box 1.
Survey questions
Statistical analysis
The collected data were analyzed using the Statistical Package for the Social Sciences version 11.5 (SPSS Inc, Chicago, US) for Windows. Findings were described in terms of percentage of participants (overall psychiatrists and nonpsychiatrists). Chi-square test was applied to identify the difference in perspectives among psychiatrists and nonpsychiatrists.
RESULTS
Responses of the participants were analyzed and outcomes have been described here. The results are presented as a comparative view of perspectives of psychiatrists and nonpsychiatrists.
Presenting complaints
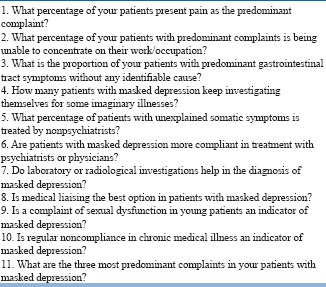
The views of the psychiatrists and nonpsychiatrists, with respect to the predominant complaints, are summarized in Table 1.
As shown in Table 1, nonpsychiatrists more often encountered chronic pain as the predominant complaint compared with psychiatrists. Forty-four percentage of the nonpsychiatrists agreed that chronic pain was present in a majority (>50%) of the patients with masked depression. Only 20% of the psychiatrists agreed that chronic pain was present in a majority (>50%) of patients with masked depression. Gastrointestinal tract problems as the predominant complaints in patients with masked depression were noted by psychiatrists and nonpsychiatrists to a similar extent. Seventeen percentage of the psychiatrists and 23% of the nonpsychiatrists agreed that gastrointestinal symptoms were present in a majority of their patients with masked depression. Only 9% of nonpsychiatrists, compared with 31% of psychiatrists, agreed that lack of concentration was present in a majority of patients with masked depression
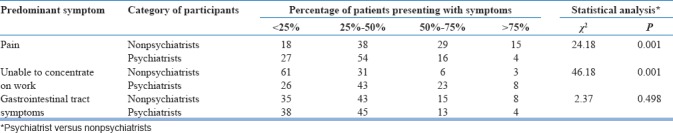
The participants were asked about the most predominant complaints in patients with masked depression in their clinical practice. For nonpsychiatrists, insomnia was the major concern and for psychiatrists, both insomnia and lack of interest were of major concern [Table 2].
Table 1.
Psychiatrists versus nonpsychiatrists' perspectives: Predominant complaints in patients with masked depression
Other potential indicators of masked depression
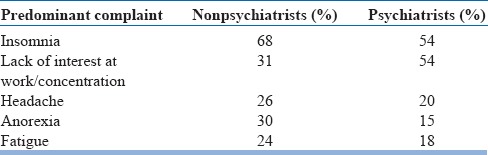
Both psychiatrists and nonpsychiatrists agreed that few patients seek investigation for imaginary illness [Chi-square value = 1.08; P = 0.782; Table 3].
Table 2.
Top five predominant complaints in patients with masked depression: Experience of nonpsychiatrists versus psychiatrists
Furthermore, majority of psychiatrists as well as nonpsychiatrists agreed that sexual dysfunction in young patients and regular noncompliance to chronic illness therapy were predictors of masked depression [Table 4].
Table 3.
Psychiatrists versus nonpsychiatrists’ perspectives: Percentage of patients seeking investigation for imaginary illnesses
Clinical issues
The participants were of divided opinions regarding the use of radiological or other investigations for the diagnosis of masked depression. More nonpsychiatrists (62%), compared to psychiatrists (36%), believed that laboratory/radiological investigations are required in patients of masked depression [Figure 1]. Both psychiatrists and nonpsychiatrists were in unison that medical liaising helps in the management of patients with masked depression [Figure 1].
Figure 1.
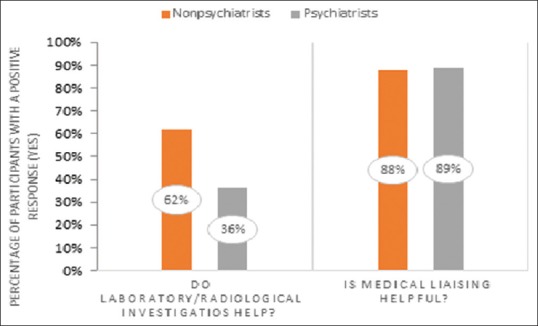
Psychiatrists versus nonpsychiatrists’ perspectives: Need for laboratory/radiological investigations and medical liaising in masked depression
According to 64% of psychiatrists, majority of patients (>50%) with unexplained somatic symptoms are treated by nonpsychiatrists [Chi-square value = 48.58; P = 0.000; Figure 2].
Figure 2.
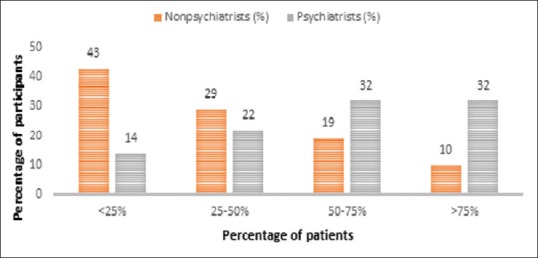
Psychiatrists versus nonpsychiatrists’ perspectives: Proportion of patients with unexplained somatic symptoms being treated by nonpsychiatrists
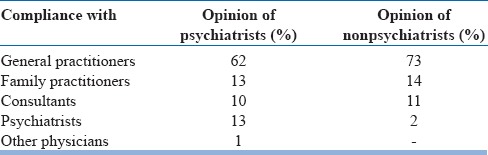
Majority of psychiatrists (62%) and nonpsychiatrists (73%) agreed that patients were more compliant to treatment with general practitioners [Chi-square value = 17.00; P = 0.002; Table 5]. Both psychiatrists and nonpsychiatrists felt that only a small percentage of the patients were compliant to therapy when treated by a psychiatrist [Table 5].
Table 4.
Psychiatrists versus nonpsychiatrists' perspectives: Clinical predictors of masked depression
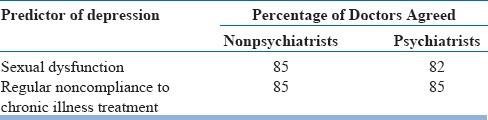
Table 5.
Psychiatrists versus nonpsychiatrists’ perspectives: Proportion of patients compliant with therapy prescribed by their treating physician
DISCUSSION
The current survey indicates that somatic pain was the predominant complaint in patients with depression, especially in the primary care settings. In this survey, more nonpsychiatrists (44%) agreed that chronic pain was present in a majority of patients with masked depression when compared to psychiatrists (20%). On the contrary, more psychiatrists (31%) reported lack of concentration in a majority of patients with masked depression than nonpsychiatrists. Nonpsychiatrists (62%) were more favorable toward the need for laboratory/radiological investigations compared with psychiatrists (36%). Both psychiatrists and nonpsychiatrists agreed that sexual dysfunction among young patients and noncompliance to therapy for chronic illness were potential predictors of masked depression. It was also a shared opinion that patients are more compliant to treatment with general practitioners. Thus, it was agreed that medical liaising is beneficial for the management of patients with masked depression.
In the current survey, somatic pain was more commonly noted in the nonpsychiatric clinical practice, compared with psychiatric practice. The presence of somatic symptoms in patients with depression is well recognized. A study from Canada reported that 76% of patients diagnosed with depression reported somatic symptoms as a primary complaint for health-care consultation.[9] Yet another study from the US reported that 69% of patients with depression had complained of general aches and pains of mild severity or above.[10] In the current survey, gastrointestinal symptoms were also reported in patients with masked depression, both in psychiatric and nonpsychiatric practice. A cross-sectional survey from a primary care setting in the US has also reported a significant association between gastrointestinal symptoms and depression and anxiety.[11] With such a high prevalence of somatic symptoms in depression, one may consider the possibility of the underlying depression in patients presenting with unexplained somatic symptoms.[6]
In the current survey, insomnia was the most commonly reported problem in patients presenting to nonpsychiatrists and this may often go unrecognized in the assessment of depression and subsequently, in the treatment goals. These findings are supported by another study which reported about 10-fold higher likelihood of depression in people with insomnia than those without insomnia.[12] Furthermore, cognitive symptoms, such as poor concentration, have also been commonly reported in association with depression.[13] These trends were also reflected in the current survey, as the lack of concentration was reported as one of the most common presenting complaints for psychiatrists.
Depressive symptoms, such as loss of interest, lack of energy, lowered self-esteem, irritability, and social withdrawal, may impair the sexual relationships.[14] In the current survey, both psychiatrists and nonpsychiatrists recognize sexual dysfunction as an indicator of masked depression. These findings were similar to another study, which reported that 72% of patients with unipolar depression had complaint of loss of sexual interest.[15] Considering the prevalence of sexual dysfunction in depressive disorders, it is important to elicit the history of sexual dysfunction in patients suspected to have masked depression.
Patients with psychological disorders often have other comorbid chronic illnesses.[16] It has been noted that depression plays a significant role in nonadherence to therapy for chronic illnesses. In the current survey, psychiatrists and nonpsychiatrists agreed that noncompliance to medical therapy is a potential predictor of masked depression. According to the meta-analysis data, depression is one of the strongest predictors of patient nonadherence to medical treatment; risk of nonadherence is 27% higher in medically depressed patients compared with nondepressed patients.[17] Thus, a history of noncompliance to treatment for chronic illnesses should be elicited in patients suspected of masked depression.
In the current survey, psychiatrists and nonpsychiatrists agreed that only a few patients were expecting diagnosis for imaginary illness. This indicates a high prevalence of masked depression in the community. In the current survey, 62% of nonpsychiatrists believed that laboratory/radiological investigations help in the diagnosis of masked depression. It has been noted that PCPs, being anxious not to miss any life-threatening organic condition, tend to investigate the somatic symptoms before they investigate the psychological symptoms.[6] Very often, physicians prescribe a battery of tests to rule out any organic condition for patient satisfaction. This approach of several tests follows the concept of ruling out all other possibilities, except depression, leading to an expensive but ineffective diagnostic search.[18] Most of the investigations in these patients are not required and may only add to the cost burden.
Considering the stigma associated with mental illnesses,[6] we analyzed the general view among therapy compliance with psychiatrists versus nonpsychiatrists. In the current survey, there has been an agreement that patients were more compliant to treatment with general practitioners and a majority of patients with unexplained somatic symptoms were treated by nonpsychiatrists. A similar survey, which was conducted among nonpsychiatrists in India, indicated that a substantial proportion of them underestimate psychiatric morbidity, especially about unexplained physical symptoms and specific depressive symptoms, and that there is an urgent need to improve training to provide best and optimal care to such patients.[19] In this regard, medical liaising becomes an important aspect of management of masked depression in clinical practice. Studies indicate that liaising in psychiatry helps in providing comprehensive health care to patients, and many tertiary hospitals in India carry out liaison work with various departments including neurology, organ transplant, Intensive Care Units, and cosmetic surgery.[20]
In the current survey, majority of psychiatrists, as well as nonpsychiatrists, agreed that medical liaising helped in the management of patients with masked depression. Medical liaising may help improve treatment outcomes, without burdening the patient. The justification and benefits of offering mental care in primary health care have been formally reported by the World Health Organization in association with the World Organization of Family Doctors which support integration of mental health into primary care.[21]
CONCLUSION
Somatic symptoms often complicate the clinical presentation of depression. Predominance of somatic symptoms over psychological symptoms, coupled with time constraints during consultations and lack of awareness among patients as well as doctors, often lead to the misdiagnosis of masked depression, resulting in delayed treatments and poorer outcomes. This survey is one of a kind from India which aimed to gather views of psychiatrists and nonpsychiatrists regarding the presentation and management aspects of masked depression. This survey indicates that both psychiatrists and nonpsychiatrists encounter somatic symptoms, such as chronic pain and gastrointestinal tract symptoms, as predominant presenting symptoms among patients with masked depression. Apart from somatic symptoms, insomnia and lack of concentration were reported to be the major presenting complaints. Sexual dysfunction among the young people and nonadherence to therapy for chronic illnesses were reported to be potential predictors of masked depression. Considering the findings that majority of patients with unexplained somatic symptoms are treated by nonpsychiatrists and that patients are more compliant to treatment with general practitioners, medical liaising was considered to be beneficial in patients with masked depression. A focus on the holistic approach by PCPs, especially in patients with medically unexplained somatic symptoms, may help identify masked depression at the initial visit. Adequate awareness and training regarding the recognition and treatment of masked depression may help reduce misdiagnosis by PCPs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank BioQuest Solutions Pvt., Ltd., for their editorial services.
REFERENCES
- 1.Miodek A, Szemraj P, Kocur J, Ryś A. Masked depression – History and present days. Pol Merkur Lekarski. 2007;23:78–80. [PubMed] [Google Scholar]
- 2.Swaine Z. Encyclopedia of Clinical Neuropsychology. Springer; 2011. Masked depression; pp. 1524–5. [Google Scholar]
- 3.Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: Classification and criteria changes. World Psychiatry. 2013;12:92–8. doi: 10.1002/wps.20050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Classification of Diseases. Mental and Behavioural Disorders. [Last accessed on 2017 Feb 21]. Available from: http://www.apps.who.int/classifications/apps/icd/icd10online2003/fr-icdhtm?gf30.htm .
- 5.Wrodycka B, Chmielewski H, Gruszczyński W, Zytkowski A, Chudzik W. Masked (atypical) depression in patients with back pain syndrome in outpatient neurological care. Pol Merkur Lekarski. 2006;21:38–40. [PubMed] [Google Scholar]
- 6.Tylee A, Gandhi P. The importance of somatic symptoms in depression in primary care. Prim Care Companion J Clin Psychiatry. 2005;7:167–76. doi: 10.4088/pcc.v07n0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–9. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- 8.Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99. [PMC free article] [PubMed] [Google Scholar]
- 9.Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–41. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- 10.Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K, et al. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66:17–22. doi: 10.1097/01.psy.0000106883.94059.c5. [DOI] [PubMed] [Google Scholar]
- 11.Mussell M, Kroenke K, Spitzer RL, Williams JB, Herzog W, Löwe B, et al. Gastrointestinal symptoms in primary care: Prevalence and association with depression and anxiety. J Psychosom Res. 2008;64:605–12. doi: 10.1016/j.jpsychores.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 12.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 13.Papazacharias A, Nardini M. The relationship between depression and cognitive deficits. Psychiatr Danub. 2012;24(Suppl 1):S179–82. [PubMed] [Google Scholar]
- 14.Baldwin DS. Depression and sexual dysfunction. Br Med Bull. 2001;57:81–99. doi: 10.1093/bmb/57.1.81. [DOI] [PubMed] [Google Scholar]
- 15.Casper RC, Redmond DE, Jr, Katz MM, Schaffer CB, Davis JM, Koslow SH, et al. Somatic symptoms in primary affective disorder. Presence and relationship to the classification of depression. Arch Gen Psychiatry. 1985;42:1098–104. doi: 10.1001/archpsyc.1985.01790340082012. [DOI] [PubMed] [Google Scholar]
- 16.Rijavec N, Grubic VN. Depression and pain: Often together but still a clinical challenge: A review. Psychiatr Danub. 2012;24:346–52. [PubMed] [Google Scholar]
- 17.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 18.Wise TN, Fishbain DA, Holder-Perkins V. Painful physical symptoms in depression: A clinical challenge. Pain Med. 2007;8(Suppl 2):S75–82. doi: 10.1111/j.1526-4637.2007.00352.x. [DOI] [PubMed] [Google Scholar]
- 19.Khan F, Malik A, Azeem S, Abeyagunaratne J, Azeem H, Ali MS, et al. Contemporary issues in liaison psychiatry and growing older adult population in India: Experiences from UK initiatives. AP J Psychol Med. 2013;14:25–32. [Google Scholar]
- 20.Parkar SR, Sawant NS. Liaison psychiatry and Indian research. Indian J Psychiatry. 2010;52:S386–8. doi: 10.4103/0019-5545.69274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. [Last accessed on 2016 Nov 27];Integration Mental Health into Primary Care. 2008 Available from: http://www.who.int/mental_health/resources/mentalhealth_PHC_2008.pdf . [Google Scholar]


