Abstract
Introduction
Obesity and eating disorders are public health problems that have lifelong financial and personal costs and common risk factors, for example, body dissatisfaction, weight teasing and disordered eating. Obesity prevention interventions might lead to the development of an eating disorder since focusing on weight may contribute to excessive concern with diet and weight. Therefore, the proposed research will assess whether integrating obesity and eating disorder prevention procedures (‘integrated approach’) do better than single approach interventions in preventing obesity among adolescents, and if integrated approaches influence weight-related outcomes.
Methods and analysis
Integrated obesity and eating disorder prevention interventions will be identified. Randomised controlled trials and quasi-experimental trials reporting data on adolescents ranging from 10 to 19 years of age from both sexes will be included. Outcomes of interest include body composition, unhealthy weight control behaviours and body satisfaction measurements. MEDLINE/PubMed, PsycINFO, Web of Science and SciELO will be searched. Data will be extracted independently by two reviewers using a standardised data extraction form. Trial quality will be assessed using the Cochrane Collaboration criteria. The effects of integrated versus single approach intervention studies will be compared using systematic review procedures. If an adequate number of studies report data on integrated interventions among similar populations (k>5), a meta-analysis with random effects will be conducted. Sensitivity analyses and meta-regression will be performed only if between-study heterogeneity is high (I2 ≥75%).
Ethics and dissemination
Ethics approval will not be required as this is a systematic review of published studies. The findings will be disseminated through conference presentations and peer-reviewed journals.
Keywords: adolescent, obesity prevention, eating disorders, systematic review, disordered eating
Strengths and limitations of this study.
First review and meta-analysis of stand-alone obesity prevention programmes versus integrated obesity and eating disorder prevention approaches on body composition.
Body composition measures do not precisely measure body fat.
Disordered eating will be measured using self-reported measures.
Age will be limited to 10-year-old to 19-year-old adolescents.
Background
Paediatric overweight and obesity are worldwide public health concerns,1 with the highest rates in the USA where 28.8% of boys and 29.7% of girls are overweight or obese.2 Western low-income and middle-income countries (LMIC) also face unhealthy child weight, for example, 24.3% of individuals between 10 and 19 years of age in Brazil were overweight or obese.2 Some evidence indicates a rapid increase in prevalence levels in LMICs as high or even higher than those found in high-income countries (HICs).3 Obesity has been associated with long-term and short-term physical health conditions, such as cardiometabolic diseases,4 certain types of cancers5 and mental health concerns.6 7 Overweight youth are also at high risk of becoming obese adults,8 indicating prevention should be initiated in youth.
Prior systematic reviews have examined childhood obesity prevention studies.3 9 10 The findings, however, have been mixed. In one review of school-based interventions to prevent obesity among children and adolescents, an average difference between the intervention and control groups was −0.33 kg/m2 (−0.55,–0.11, 95% CI), with 84% of this effect explained by the highest quality studies.11 Alternatively, another reported a difference of 0.03 (95% CI: 0.09 to 0.03, P=0.03) with high heterogeneity (I2=87%).12 Thus, evidence regarding the effectiveness of school-based obesity prevention interventions to reduce body mass index (BMI) in youth is mixed with high heterogeneity among studies. Narrower age groups who experience common problems and receive interventions appropriate to these common problems may be more effective.
Eating disorders are illnesses in which the people experience severe disturbances in their eating behaviours and related thoughts and emotions. People with eating disorders typically become preoccupied with food and their body weight.13 In the Diagnostic and Statistical Manual of Mental Disorders 5, the eating disorders section was renamed ‘Feeding and Eating Disorders’ and specified three eating disorders: anorexia nervosa, bulimia nervosa and binge eating disorder; and three feeding disorders: pica, rumination disorder and avoidant/restrictive food disorder.13 These categories and associated criteria served to decrease the frequency of the diagnostic category ‘eating disorder not otherwise specified’, a heterogeneous not well-defined group of eating disorders. Eating disorder not otherwise specified was the most common diagnosis in clinical and community samples of adolescents, accounting for around 80% of all eating disorder diagnoses, with psychopathology and adverse consequences comparable with anorexia nervosa and bulimia nervosa.13 14
Disordered eating behaviours and attitudes are part of the eating disorders continuum and include obsessively thinking about food and calories, becoming angry when hungry, being unable to select what to eat, seeking food to compensate for psychological problems, eating until feeling sick and presenting unreal myths and beliefs about eating and weight.15 Disordered eating is not limited to those diagnosed with eating disorders. Indeed, many individuals experience disordered eating behaviours, beliefs and feelings towards food but are unaware that they are manifesting ‘abnormal’ behaviours.15
Most interventions in the field of eating disorders can be classified as primary prevention programmes, aiming to reduce risk factors. In general, these interventions focus on girls as a target group based on the observation, that girls have an increased chance of developing an eating disorder, especially anorexia and bulimia nervosa.16 Schools are the most common setting for the existing evaluated programmes.16 Earlier eating disorder programmes tended to employ fear appeals, threat appeals or fear arousing communications.16 17 These methods have been increasingly abandoned, since they did not show an effect or might have even been ‘more harmful than beneficial’.16 More recent eating disorder prevention programmes focused on protective factors such as life skills and emotion regulation competence.18 19 The PriMa (Primary Prevention of Anorexia Nervosa) programme16 was a new type of prevention programme for girls up to the age of 12. This scientifically based intervention attempted to prevent eating disorders and reduce disordered eating behaviours by primarily focusing on problems associated with anorexia nervosa. The nine lesson programme used standardised posters and guidelines to encourage group discussions. The intervention group reported significant improvements in body self-esteem, figure dissatisfaction, knowledge and eating attitudes. Also, instead of interventionists, the programme used school teachers to deliver the intervention.
A recent systematic review and meta-analyses19 quantified the effectiveness of eating disorder preventive randomised controlled trials for children, adolescents and youth. A total of 112 studies were included; 58% of the trials had high risk of bias. The findings indicated small to moderate effect sizes in reducing eating disorder risk factors. It also revealed that promising preventive interventions for eating disorders risk factors may include cognitive dissonance therapy, cognitive behavioural therapy and media literacy. Whether these interventions lower eating disorder incidence is, however, uncertain, and there is a need for studies that combine eating disorder and obesity prevention.19
Although eating disorder prevention programmes included content of relevance to obesity prevention (eg, promotion of healthy weight management), a few assessed the impact on weight status or other obesity-related outcomes.17 19 20
Being overweight during childhood increases the chances of having an eating disorder during adulthood (compared with normal weight controls).16 Common obesity and eating disorders risk factors can be categorised into three levels according to the Social Ecological Model21: individual (eg, sex, age and weight status), social (eg, media, weight teasing and ideal beauty pattern) and psychological (eg, self-esteem and body satisfaction). Several studies have described the co-presence of these factors, which could be considered risks for the development of eating disorders and obesity.22–24 Thus, an integrated approach could address the differences in these prevention philosophies, for example, eating behaviours (dieting vs no dieting) and body weight (lose vs accept weight).18
Some interventions addressed both obesity and eating disorders in prevention interventions because of the efficiency in addressing two conditions with a single intervention and a possible reduced risk of inadvertently causing eating disorders while trying to prevent obesity,25–27 for example, strategies to prevent obesity (monitoring intake and portion control) might unintentionally promote shape concerns and disordered eating. Integrating obesity and eating disorder prevention programmes may prove easier and more cost-effective than treating them separately, and healthy nutrition and physical activity are the focus of both eating disorders and obesity prevention programmes.28 Body dissatisfaction concerns were also addressed in both approaches, but have mismatched messages. For example, some obesity prevention programmes considered it acceptable to be unhappy about being overweight in order to motivate restricting the amount and content of food consumed to reduce body weight,28 while eating disorder prevention programmes promoted self-acceptance at any weight, discouraging self-consciousness about dietary intake. However, data supporting these alternative viewpoints are scarce.28
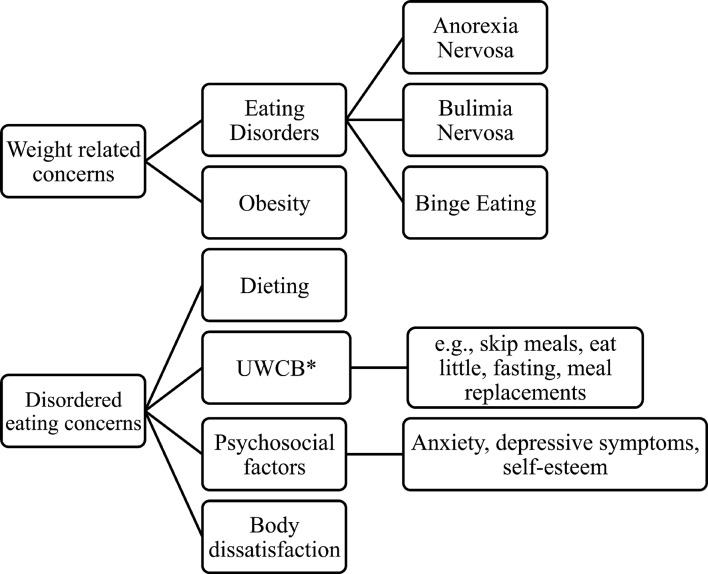
Due to the increasing prevalence of obesity and eating disorders20 25 and shared common risk factors, that is, body dissatisfaction, unhealthy weight control behaviours/dieting and weight teasing (figure 1), there have been calls for integration to address these common concerns.25 For instance, obesity and eating disorders can co-occur in the same individual.25 A cross-cultural comparison between US and Spanish adolescents found dieting and use of unhealthy weight control behaviours were higher among overweight and obese youth and concluded that prevention interventions should address the broad spectrum of eating and weight-related problems.29
Figure 1.
Scheme of the weight-related behaviours. *UWCB, Unhealthy Weight Control Behaviours.
In summary, obesity and eating disorders have common risk factors with adverse health outcomes, mainly among overweight and female adolescents. Systematic reviews and meta-analyses have only analysed results for single approaches (ie, obesity or eating disorders prevention) and the results have been mixed. Interventions that integrate obesity and eating disorders prevention components might be more effective. A review of such interventions might provide insight into the mechanisms of effect and inform interventions that address both problems simultaneously. To the authors’ knowledge, no previous review has identified the impact of integrated obesity and eating disorders prevention programmes for adolescents. The present systematic review will answer the following questions:
Do integrated obesity and eating disorders interventions do better than obesity-only prevention interventions in improving adolescents’ health behaviour outcomes and maintaining healthy weight status?
Do integrated interventions promote being more satisfied with one’s body and reduce unhealthy weight control behaviours in adolescents?
Methods and analysis
The study protocol was accepted by PROSPERO (www.crd.york.ac.uk/PROSPERO) in October 2017 (CRD42017076547). This protocol follows the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocol (PRISMA-P) checklist.30 Modifications to the protocol will be tracked and dated in PROSPERO.
Patient and public involvement
Patients and/or public were not involved in this current study.
Criteria for considering studies for this review
Inclusion criteria
Population
Adolescents 10– 19 years of age from both sexes. Adolescents in this age range are at increased risk for unhealthy weight control behaviours and body satisfaction, shared risk factors for obesity and eating disorders.18 31 Most published integrated prevention studies are in this age group.
Types of outcomes
(1) Body composition measurements (ie, body mass index (BMI), waist circumference or per cent body fat); (2) weight control behaviours and/or scales that assess the risk for an eating disorder (such as the Eating Attitudes Test (EAT-26), Sociocultural Attitudes Towards Appearance Questionnaire 3 (SATAQ-3) and Eating Disorder Examination Questionnaire (EDE-Q)); (3) self-reported scales on body satisfaction and (4) other psychological markers (eg, anxiety, depression and/or self-esteem inventories). Inclusion of at least one of the weight control behaviours and/or scales must have been used to assess the risk for eating disorders.15 18 32 33
We define ‘obesity and eating disorder prevention studies’ to be those in which the authors explicitly state they are targeting both sets of outcomes. ‘Obesity prevention alone’ studies are defined to be those in which the authors state only an obesity prevention objective even if mentioning eating disorder prevention. Some obesity prevention studies collect measures of eating disorders to assess possible unanticipated eating disorder side effects. These will be considered obesity prevention alone studies.
Study design
Quasi-randomised controlled trials and randomised controlled trials assessing the impact of integrated or obesity-only prevention interventions.
Types of studies
Quantitative outcome analyses will be included in the systematic review and meta-analysis.
Search strategy
A structured electronic search will employ all publication years (up to 2018) using four databases and terms will be searched for all text: Medical Literature Library of Medicine (MEDLINE) via PubMed (≥1979), PsycINFO of the American Psychological Association (≥1954), Web of Science via Clarivate Analytics (≥1983) and Scientific Electronic Library (SciELO) via BIREME Latin American and Caribbean Center on Health Science Information (≥1997). Systematic searchers will be developed from this model, applied in MEDLINE: (Obesity) OR Overweight) OR Weight related problems) AND eating disorder) OR weight control behaviors) AND adolescents) OR youth) OR teenagers) OR girls) OR boys) AND prevent*) OR strategies) OR randomized controlled trial. Congress abstracts, dissertations, theses and articles published in journals without peer review will not be included in the review. Only studies written in English, German, Spanish or Portuguese will be included. The results of this search strategy will be reported in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart.30 The bibliographies of papers that match inclusion criteria will be searched by hand to identify further relevant references, which will be subjected to the same screening and selection process. The full search strategy is referred in the online supplementary figure 1.
bmjopen-2017-020381supp001.pdf (51.2KB, pdf)
Screening and data extraction
All articles identified from the initial electronic search process will be imported into an EndNote library and duplicates are removed. The eligibility criteria will be applied to the results and all identified references are screened independently by two reviewers (ACBL and TL) in a standard blinded way in four stages: (i) reviewing the titles and abstracts; (ii) retrieving and examining the full texts for inclusion; (iii) searching reference lists from the full articles and (iv) examining relevant references for additional studies. TB will be consulted when questions or ambiguity arises. The data extraction form will be pretested with five randomly selected trials.
Quality assessment
The quality of the randomised controlled trials will be assessed using the Cochrane Collaboration’s tool for assessing risk of bias in randomised trials.34 All data will be extracted and quality assessed by two reviewers. Disagreements at each step will be resolved by discussion. When no consensus is reached, a third reviewer will resolve the discrepancy.
Data synthesis and analysis
The results of the studies included in the systematic review will be described in a summary table, consisting of author (year), purpose of the study, population targeted, study quality,34 characteristics of the sample, outcome measures, statistical analyses performed (eg, repeated measures analysis of variance, analysis of covariance or regression analysis) and the results on body composition and disordered eating behaviours. The results of the impact of the intervention will be reported in effect sizes, such as ORs for dichotomous outcomes (eg, satisfied and dissatisfied) or standardised mean differences (SMDs) for continuous outcomes (eg, BMI—kg/m2). All effect sizes will be zero order. To facilitate interpretation and permit comparison with other SMDs and standard effect sizes, the ORs will be converted to Cohen’s d.35 Cohen’s d of 0.2 is a small effect size, 0.5 is medium and ≥0.80 is large.35
An adequate number of studies (k>5)36 will trigger a meta-analysis of the findings with a random-effects model. The magnitude of the effect sizes might vary across the studies due to the differences in sample and outcomes of the studies. The pooled effect sizes will be computed, and each study will be weighted according to its sample size. Cochran’s Q37 and I2 statistics38 will assess the between-study heterogeneity as measures of the percentage of total variation in estimated effects that is a consequence of heterogeneity rather than chance.39 Significant heterogeneity is considered when the Q statistic has P<0.05. An I2 statistic of 25% or less is considered low; 50% moderate and 75% high heterogeneity.40 If study heterogeneity exceeds I2 ≥75% (high), it will be explored through sensitivity analyses and meta-regression. The funnel plot will be inspected for publication bias, with a minimum of 10 studies in the analysis,41 through Duval and Tweedie’s trim and fill method42 and Egger’s regression test.43 All the analyses will be conducted using Comprehensive Meta-Analysis software.
Subgroup analyses might be conducted to assess the possible effects of time differences between integrated prevention versus single obesity approach, and between certain disordered eating behaviours and anthropometric measurements according to the following variables: population (eg, normal weight adolescents vs overweight/obese adolescents) and quality rating (high-rated vs low-rated studies according to the Cochrane Collaboration’s tool34). Age and sex differences in the impact of integrated prevention programmes will be examined since disorder eating behaviours are more common among older adolescents, girls and overweight/obese individuals.24 25 44 Moreover, because previous studies45–48 have found socioeconomic disparities in obesity and disorder eating socioeconomic status, differences will be examined in eating disorder and obesity risk factors in the prevention conditions.
The strength of the evidence will be evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines.49 The following assessments will be made: (1) quality rating for each study according to Cochrane Collaboration’s tool34; (2) Cohen’s d classification to evaluate the magnitude of individual or pooled effect size (SMD),35 if a meta-analysis is possible; (3) Cochran’s Q37 and I2 statistic38 for heterogeneity and (4) risk of bias by visualising the distribution of the funnel plot if there are at least 10 trials per analysis41 through Duval and Tweedie’s trim and fill method and Eggers’s regression test.
Gaps and limitations
Several gaps and limitations should be noted in anticipation of the findings of the systematic review and meta-analysis. First, the body composition measurements reported in these studies will always be objective measurements (ie, BMI, waist circumference and %body composition) which do not precisely measure percentage body fat.50–52 Second, eating disorder will be assessed through self-reported measurements which might provide biased responses, since under-reporting is highly prevalent, especially among girls and overweight/obese individuals.24 47 48 53 54 Any studies that assess disease preventive intervention impacts on self-reported or anthropometric data may potentially underestimate the effect of the intervention.18 Finally, we are going to cover only adolescents ageing from 10 to 19 years old. However, the majority of the integrated interventions focus on these adolescent years.18
Implications
This systematic review and meta-analysis aims to evaluate the impact of obesity and eating disorder prevention programmes for adolescents. The results of this study should provide new insights into the approaches tested thus far. The systematic review and meta-analysis may also identify specific gaps in the evidence, which would inform the agenda for future research and policy.
Amendments
If there is a need to amend this protocol, the date, rationale and a description of each protocol change will be reported.
Supplementary Material
Footnotes
Contributors: ACBL, the guarantor of the protocol, drafted the protocol and registered it in PROSPERO. TB reviewed and commented on the protocol in PROSPERO. ACBL, DT, KLLD, TN, STP, TL, L-AV-I and TB all reviewed and commented on this protocol.
Funding: This work is a publication of the USDA (USDA/ARS - UNITED STATES DEPARTMENT OF AGRICULTURE/AGRICULTURE RESEARCH SERVICE)) Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine (Houston, Texas) and has had been funded, in part, with federal funds from the USDA/ARS under Cooperative Agreement Number 58-6250-6001. ACBL received a postdoctoral fellowship from the State of São Paulo, Brazil (FAPESP - FUNDANÇÃO DE AMPARO À PESQUISA DO ESTADO DE SÃO PAULO - process nº 2016/ 21144-9).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethics approval will not be required as this is a protocol for systematic review and meta-analysis. This systematic review and meta-analysis will be published in a peer-reviewed journal which will be disseminated electronically and in print.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Hoelscher DM, Kirk S, Ritchie L, et al. . Position of the academy of nutrition and dietetics: interventions for the prevention and treatment of pediatric overweight and obesity. J Acad Nutr Diet 2013;113:1375–94. 10.1016/j.jand.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 2. Ng M, Fleming T, Robinson M, et al. . Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Verstraeten R, Roberfroid D, Lachat C, et al. . Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: a systematic review. Am J Clin Nutr 2012;96:415–38. 10.3945/ajcn.112.035378 [DOI] [PubMed] [Google Scholar]
- 4. Moreno LA. Obesity in children and adolescents. A critical review. Endocrinol Nutr 2013;60(Suppl 1):7–9. 10.1016/S1575-0922(13)70016-0 [DOI] [PubMed] [Google Scholar]
- 5. Kann L, McManus T, Harris WA, et al. . Youth risk behavior Surveillance - United States, 2015. MMWR Surveill Summ 2016;65:1–174. 10.15585/mmwr.ss6506a1 [DOI] [PubMed] [Google Scholar]
- 6. Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes 2011;35:891–8. 10.1038/ijo.2010.222 [DOI] [PubMed] [Google Scholar]
- 7. Wake M, Canterford L, Patton GC, et al. . Comorbidities of overweight/obesity experienced in adolescence: longitudinal study. Arch Dis Child 2010;95:162–8. 10.1136/adc.2008.147439 [DOI] [PubMed] [Google Scholar]
- 8. Tsiros MD, Coates AM, Howe PR, et al. . Obesity: the new childhood disability? Obes Rev 2011;12:26–36. 10.1111/j.1467-789X.2009.00706.x [DOI] [PubMed] [Google Scholar]
- 9. Wang Y, Cai L, Wu Y, et al. . What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev 2015;16:547–65. 10.1111/obr.12277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boff RM, Liboni RPA, Batista IPA, et al. . Weight loss interventions for overweight and obese adolescents: a systematic review. Eat Weight Disord 2017;22:211–29. 10.1007/s40519-016-0309-1 [DOI] [PubMed] [Google Scholar]
- 11. Silveira JA, Taddei JA, Guerra PH, et al. . The effect of participation in school-based nutrition education interventions on body mass index: a meta-analysis of randomized controlled community trials. Prev Med 2013;56(3-4):237–43. 10.1016/j.ypmed.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 12. Guerra PH, Nobre MR, da Silveira JA, et al. . School-based physical activity and nutritional education interventions on body mass index: a meta-analysis of randomised community trials - project PANE. Prev Med 2014;61:81–9. 10.1016/j.ypmed.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 13. APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
- 14. Smink FR, van Hoeken D, Oldehinkel AJ, et al. . Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. Int J Eat Disord 2014;47:610–9. 10.1002/eat.22316 [DOI] [PubMed] [Google Scholar]
- 15. Alvarenga MS, Scagliusi FB, Philippi ST. Development and validity of the Disordered Eating Attitude Scale (DEAS). Percept Mot Skills 2010;110:379–95. 10.2466/PMS.110.2.379-395 [DOI] [PubMed] [Google Scholar]
- 16. Berger U, Sowa M, Bormann B, et al. . Primary prevention of eating disorders: characteristics of effective programmes and how to bring them to broader dissemination. Eur Eat Disord Rev 2008;16:173–83. 10.1002/erv.861 [DOI] [PubMed] [Google Scholar]
- 17. Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: encouraging findings. Annu Rev Clin Psychol 2007;3:207–31. 10.1146/annurev.clinpsy.3.022806.091447 [DOI] [PubMed] [Google Scholar]
- 18. Sánchez-Carracedo D, Neumark-Sztainer D, López-Guimerà G. Integrated prevention of obesity and eating disorders: barriers, developments and opportunities. Public Health Nutr 2012;15:2295–309. 10.1017/S1368980012000705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Le LK, Barendregt JJ, Hay P, et al. . Prevention of eating disorders: a systematic review and meta-analysis. Clin Psychol Rev 2017;53:46–58. 10.1016/j.cpr.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 20. Leal GVdaS, Philippi ST, Polacow VO, et al. . O que é comportamento de risco para transtornos alimentares em adolescentes? J Bras Psiquiatr 2013;62:62–75. 10.1590/S0047-20852013000100009 [DOI] [Google Scholar]
- 21. Sallis JF, Owen N, Fisher EB. Ecological models of health behavior, in Health behavior and health education. Theory, research, and practice. San Francisco, CA: Jossey-Bass, 2008:465–85. [Google Scholar]
- 22. Balantekin KN, Birch LL, Savage JS. Family, friend, and media factors are associated with patterns of weight-control behavior among adolescent girls. Eat Weight Disord 2018;23:215–23. 10.1007/s40519-016-0359-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Frederick DA, Sandhu G, Scott T, et al. . Reducing the negative effects of media exposure on body image: Testing the effectiveness of subvertising and disclaimer labels. Body Image 2016;17:171–4. 10.1016/j.bodyim.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 24. Loth K, Wall M, Larson N, et al. . Disordered eating and psychological well-being in overweight and nonoverweight adolescents: secular trends from 1999 to 2010. Int J Eat Disord 2015;48:323–7. 10.1002/eat.22382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 2006;21:770–82. 10.1093/her/cyl094 [DOI] [PubMed] [Google Scholar]
- 26. Tanofsky-Kraff M, Shomaker LB, Wilfley DE, et al. . Targeted prevention of excess weight gain and eating disorders in high-risk adolescent girls: a randomized controlled trial. Am J Clin Nutr 2014;100:1010–8. 10.3945/ajcn.114.092536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sánchez-Carracedo D, Fauquet J, López-Guimerà G, et al. . The MABIC project: an effectiveness trial for reducing risk factors for eating disorders. Behav Res Ther 2016;77:23–33. 10.1016/j.brat.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 28. Irving LM, Neumark-Sztainer D. Integrating the prevention of eating disorders and obesity: feasible or futile? Prev Med 2002;34:299–309. 10.1006/pmed.2001.0997 [DOI] [PubMed] [Google Scholar]
- 29. López-Guimerà G, Neumark-Sztainer D, Hannan P, et al. . Unhealthy weight-control behaviours, dieting and weight status: a cross-cultural comparison between North American and Spanish adolescents. Eur Eat Disord Rev 2013;21:276–83. 10.1002/erv.2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Watson HJ, Joyce T, French E, et al. . Prevention of eating disorders: a systematic review of randomized, controlled trials. Int J Eat Disord 2016;49:833–62. 10.1002/eat.22577 [DOI] [PubMed] [Google Scholar]
- 32. Neumark-Sztainer D. Integrating messages from the eating disorders field into obesity prevention. Adolesc Med State Art Rev 2012;23:529–43. [PubMed] [Google Scholar]
- 33. Neumark-Sztainer D. Addressing obesity and other weight-related problems in youth. Arch Pediatr Adolesc Med 2005;159:290–1. 10.1001/archpedi.159.3.290 [DOI] [PubMed] [Google Scholar]
- 34. Higgins JP, Altman DG, Gøtzsche PC, et al. . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cohen J. A power primer. Psychol Bull 1992;112:155–9. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 36. Davey J, Turner RM, Clarke MJ, et al. . Characteristics of meta-analyses and their component studies in the Cochrane Database of Systematic Reviews: a cross-sectional, descriptive analysis. BMC Med Res Methodol 2011;11:160 10.1186/1471-2288-11-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cochran WG. The χ test of goodness of t. Ann Math Stat 1952;23:315–45. [Google Scholar]
- 38. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 39. Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, et al. . Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 2006;11:193–206. 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 40. Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc 2009;172:137–59. 10.1111/j.1467-985X.2008.00552.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sutton AJ, Duval SJ, Tweedie RL, et al. . Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574–7. 10.1136/bmj.320.7249.1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Duval S, Tweedie R. A nonparametric “trim and ll” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 2000;95:89–98. [Google Scholar]
- 43. Egger M, Davey Smith G, Schneider M, et al. . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Suisman JL, Thompson JK, Keel PK, et al. . Genetic and environmental influences on thin-ideal internalization across puberty and preadolescent, adolescent, and young adult development. Int J Eat Disord 2014;47:773–83. 10.1002/eat.22321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Stamatakis E, Wardle J, Cole TJ. Childhood obesity and overweight prevalence trends in England: evidence for growing socioeconomic disparities. Int J Obes 2010;34:41–7. 10.1038/ijo.2009.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jaacks LM, Slining MM, Popkin BM. Recent trends in the prevalence of under- and overweight among adolescent girls in low- and middle-income countries. Pediatr Obes 2015;10:428–35. 10.1111/ijpo.12000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Spencer RA, Rehman L, Kirk SF. Understanding gender norms, nutrition, and physical activity in adolescent girls: a scoping review. Int J Behav Nutr Phys Act 2015;12:6 10.1186/s12966-015-0166-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Goldschmidt AB, Wall MM, Loth KA, et al. . Risk factors for disordered eating in overweight adolescents and young adults. J Pediatr Psychol 2015;40:1048–55. 10.1093/jpepsy/jsv053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Atkins D, Best D, Briss PA, et al. . Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490–4. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bogart LM, Elliott MN, Cowgill BO, et al. . Two-year BMI outcomes from a school-based intervention for nutrition and exercise: a randomized trial. Pediatrics 2016;137:e20152493 10.1542/peds.2015-2493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sharif Ishak SI, Chin YS, Mohd Taib MN, et al. . School-based intervention to prevent overweight and disordered eating in secondary school Malaysian adolescents: a study protocol. BMC Public Health 2016;16:1101 10.1186/s12889-016-3773-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pbert L, Druker S, Barton B, et al. . A school-based program for overweight and obese adolescents: a randomized controlled trial. J Sch Health 2016;86:699–708. 10.1111/josh.12428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dunstan CJ, Paxton SJ, McLean SA. An evaluation of a body image intervention in adolescent girls delivered in single-sex versus co-educational classroom settings. Eat Behav 2017;25:23–31. 10.1016/j.eatbeh.2016.03.016 [DOI] [PubMed] [Google Scholar]
- 54. Datar A, Chung PJ. Accuracy of weight perceptions in a nationally representative cohort of US 8th grade adolescents. Acad Pediatr 2016;16:267–74. 10.1016/j.acap.2015.06.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-020381supp001.pdf (51.2KB, pdf)