Abstract
Introduction
Coagulopathic bleeding is a serious complication of cardiac surgery to which an important contributor is acquired hypofibrinogenaemia (plasma fibrinogen <1.5–2.0 g/L). The standard intervention for acquired hypofibrinogenaemia is cryoprecipitate, but purified fibrinogen concentrates are also available. There is little comparative data between the two therapies and randomised trials are needed.
Methods and analysis
FIBrinogen REplenishment in Surgery (FIBRES) is a multicentre, randomised (1:1), active-control, single-blinded, phase III trial in adult cardiac surgical patients experiencing clinically significant bleeding related to acquired hypofibrinogenaemia. The primary objective is to demonstrate that fibrinogen concentrate (Octafibrin/Fibryga; Octapharma) is non-inferior to cryoprecipitate. All patients for whom fibrinogen supplementation is ordered by the clinical team within 24 hours of cardiopulmonary bypass will receive 4 g of fibrinogen concentrate or 10 units of cryoprecipitate (dose-equivalent to 4 g), based on random allocation and deferred consent. The primary outcome is total red cell, platelet and plasma transfusions administered within 24 hours of bypass. Secondary outcomes include major bleeding, fibrinogen levels and adverse events within 28 days. Enrolment of 1200 patients will provide >90% power to demonstrate non-inferiority. One preplanned interim analysis will include 600 patients. The pragmatic design and treatment algorithm align with standard practice, aiding adherence and generalisability.
Ethics and dissemination
The study is approved by the local research ethics board and will be conducted in accordance with the Declaration of Helsinki, Good Clinical Practice guidelines and regulatory requirements. Patient consent prior to treatment is waived, as per criteria in the Tri-Council Policy Statement. Results will be published in the scientific/medical literature, and at international congresses. Non-inferiority of purified fibrinogen concentrate would support its use in acquired hypofibrinogenaemia. The results are likely to improve care for cardiac surgical patients experiencing significant bleeding, an understudied yet high-risk population.
Trial registration number
NCT03037424; Pre-results.
Keywords: bleeding disorders and coagulopathies, cardiac surgery, clinical trials, adult surgery, blood bank & transfusion medicine, haematology
Strengths and limitations of this study.
This is the largest randomised comparison of fibrinogen concentrate versus cryoprecipitate in adult patients with acquired hypofibrinogenaemia due to cardiac surgery involving cardiopulmonary bypass.
A simple, pragmatic study design that aligns with standard clinical practice will enhance adherence and ensure clinical relevance and generalisability, while stratified randomisation by study site is employed to address between-site practice variability.
Use of an active control, cryoprecipitate, as the comparator guarantees that all patients in the study will receive fibrinogen supplementation as clinically indicated.
The large sample size of approximately 1200 patients in this high-risk population will provide >90% power to detect non-inferiority of fibrinogen concentrate to cryoprecipitate.
It will not be possible to fully blind clinicians to treatment allocation, so all outcome assessors will be blinded to minimise the risk of bias.
Introduction
Coagulopathy leading to excessive bleeding is a serious complication of cardiac surgery requiring cardiopulmonary bypass (CPB). Occurring in approximately 10% or more of cases, it often requires massive blood transfusion with allogeneic blood products (ABPs) and is associated with an increased risk of serious postoperative adverse outcomes, including sepsis, renal failure and death.1–4 While the causes of coagulopathy in this setting are likely to be multifactorial, acquired hypofibrinogenaemia, considered as a deficiency in plasma fibrinogen levels below 1.5–2.0 g/L,5 is believed to be one of the primary factors.6
Fibrinogen is the most abundant clotting factor in the human circulation and plays a pivotal role in haemostasis and the coagulation cascade by promoting clot formation and platelet aggregation.7 Physiological levels of fibrinogen are typically in the range of 1.5–4.5 g/L,8 with a half-life following synthesis of approximately 4 days.9 A number of factors may contribute to the development of acquired hypofibrinogenaemia in cardiac surgery. Fibrinogen loss may result from acute bleeding, dilution of the circulatory volume due to administration of fluids and priming of the CPB circuit, and consumption due to activation of the coagulation cascade during CPB.10 Since fibrinogen has only a limited reserve in the body, a modest decrease in levels to <1.5–2.0 g/L impairs coagulation and increases the likelihood of bleeding complications.10–15 Fibrinogen levels have been shown to fall 40%–50% during cardiac surgery,10 with a critical drop observed in approximately 5% of patients.16 In these patients, fibrinogen supplementation is believed to be essential and is the current standard of care in most jurisdictions.6 17
While supplementation of fibrinogen has historically included the use of fresh frozen plasma, the two principal options currently recommended for supplementation in acquired hypofibrinogenaemia are cryoprecipitate and purified fibrinogen concentrate.5 Cryoprecipitate is currently used in North America and is an ABP prepared from fresh frozen plasma through a process of thawing and centrifugation. The clotting factor-enriched precipitate is resuspended in a small volume of plasma and refrozen. Typical fibrinogen content is around 15 g/L,18 although this may vary considerably (3–30 g/L) due to interdonor variability.19 Cryoprecipitate has largely been withdrawn from most European countries due to safety concerns because it does not undergo pathogen reduction,20 where treatment with purified human fibrinogen concentrate is the preferred therapeutic choice for hypofibrinogenaemia. Fibrinogen concentrate has a number of important advantages over cryoprecipitate, including significantly higher purity; standardised fibrinogen content, enabling more accurate dosing; faster preparation and administration time; no requirement for blood type matching; and improved safety, particularly through pathogen reduction technology.6 20–22 Cryoprecipitate, which remains the most common fibrinogen replacement product in North America, may be a more effective haemostatic agent because it also contains haemostatic factors VIII and XIII, von Willebrand factor and platelet microparticles.
There is scant data comparing cryoprecipitate and fibrinogen concentrate for the treatment of acquired hypofibrinogenaemia; thus, we do not know which of these is the most appropriate therapy in bleeding cardiac surgical patients. Moreover, mounting evidence indicates that haemostatic management of patients with coagulopathic bleeding is evolving from the conventional use of non-purified ABPs to targeted therapeutic algorithms using purified coagulation factor concentrates such as fibrinogen concentrate.23 There is therefore a need for prospective, randomised clinical trials designed to specifically evaluate cryoprecipitate and fibrinogen concentrate in parallel as part of haemostatic treatment algorithms in bleeding cardiac surgical patients.
Our study design addresses these issues by assessing non-inferiority of a purified fibrinogen concentrate against cryoprecipitate for the treatment of acquired hypofibrinogenaemia in cardiac surgery. Given the theoretical and logistical advantages of fibrinogen concentrate relative to cryoprecipitate outlined above, illustrating that fibrinogen concentrate is non-inferior to cryoprecipitate would support the use of this purified fibrinogen concentrate for haemostatic management in this high-risk, clinically important setting. Importantly, the conduct of randomised trials in bleeding surgical patients poses specific challenges, and this trial incorporates several design features to address these challenges.
Methods and analysis
Objective
The primary objective of this study is to demonstrate that the administration of the fibrinogen concentrate Octafibrin/Fibryga (Octapharma AG, Lachen, Switzerland; currently approved in Canada for the treatment of congenital afibrinogenaemia and hypofibrinogenaemia) is non-inferior to cryoprecipitate for treating bleeding in cardiac surgical patients in whom fibrinogen supplementation is ordered in accordance with accepted clinical standards.
Study design and setting
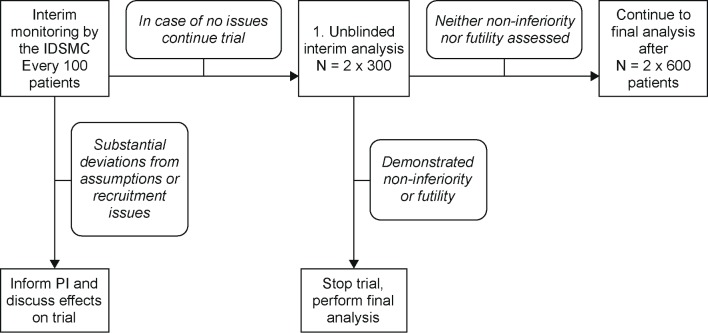
The FIBrinogen REplenishment in Surgery (FIBRES) trial is a pragmatic, multicentre, randomised, active-control, non-inferiority phase III trial in adult cardiac surgical patients experiencing clinically significant bleeding in whom fibrinogen supplementation is deemed to be necessary. A pragmatic study design was chosen because it allows participating sites and surgical teams to maintain standard clinical practice when treating patients, making the study clinically relevant and generalisable to the large population of patients undergoing cardiac surgery, and increases the likelihood of protocol adherence and successful study completion. Approximately 1200 patients will be recruited from up to 12 Canadian hospitals. Patients will be randomised when fibrinogen supplementation is ordered to either of two treatment groups: fibrinogen concentrate 4 g (intervention) or cryoprecipitate 10 units (active control). No placebo arm has been included in the trial because withholding effective treatment is neither consistent with standard practice nor acceptable on ethical grounds. Treatment arm allocation will be maintained for up to 24 hours after termination of CPB; only the randomly allocated fibrinogen replacement product can be provided during this time. No other aspects of care will be modified. Informed consent will be obtained from patient or surrogate decision-maker as soon as possible after surgery. An overview of the study design is presented in figure 1. The study commenced in February 2017 and is expected to complete in late 2018, with results available in early 2019.
Figure 1.
Study design. CPB, cardiopulmonary bypass.
Eligibility criteria
The study will enrol all adult patients undergoing cardiac surgery with CPB for whom fibrinogen supplementation is ordered by the clinicians in response to post-CPB haemorrhage in the presence of confirmed or suspected acquired hypofibrinogenaemia (fibrinogen level <1.5–2.0 g/L). The exclusion criteria are receipt of either fibrinogen concentrate or cryoprecipitate within 24 hours before surgery, a history of severe allergic reaction to fibrinogen concentrate or cryoprecipitate, known refusal of ABPs or either study treatment (ie, for religious reasons), a known fibrinogen level >3.0 g/L within 30 min of the order for treatment (to eliminate the risk of raising a patient’s fibrinogen level above the upper limit of the normal range (4.0 g/L)), and known pregnancy.
Interventions
Intervention
Patients randomised to the intervention group will receive fibrinogen concentrate administered by slow (within 10 min) intravenous injection after reconstitution with 50 mL of sterile water for injection, as per the manufacturer’s instructions. Patients randomised to this group will receive 4 g of fibrinogen concentrate each time fibrinogen supplementation is ordered during the first 24 hours after termination of CPB surgery.
Active control
Those patients randomised to the active control group will each receive cryoprecipitate, given as 10 units (dose-equivalent to approximately 4 g (median 388 mg, range 120–796 mg, per bag), as per internal Canadian Blood Services quality control data; personal communication, Canadian Blood Services24) each time fibrinogen supplementation is ordered during the first 24 hours after termination of CPB. Cryoprecipitate will be prepared according to current Health Canada standards and administered by intravenous infusion following hospital transfusion policies at each of the participating study sites.
In both study arms, study treatment (fibrinogen concentrate or cryoprecipitate) may be administered prior to the determination of fibrinogen levels in a patient who is bleeding if deemed appropriate as per current clinical standards (ie, rapid bleeding precluding waiting for laboratory results). If fibrinogen supplementation is needed after the 24-hour study period is over, patients will receive cryoprecipitate, which is the current standard of care in most of Canada. Concomitant medications to treat bleeding that are part of standard patient care will be permitted throughout the study, but must be recorded in the case report form (CRF).
Outcomes and study duration
The primary outcome of the study is one of efficacy; specifically, comparison between study groups of the total number of red cells, platelets and plasma administered during the first 24 hours after termination of CPB surgery.
Secondary outcomes of the study will include both efficacy and safety outcomes. For the former, the secondary outcomes are (1) comparison of the total number of ABPs (not including cryoprecipitate) administered from the start of surgery up to 7 days after surgery (or discharge if earlier), (2) comparison of major bleeding (using the modified universal definition of perioperative bleeding in cardiac surgery)25 during the first 24 hours after termination of CPB and (3) comparison of the effect of treatment on plasma fibrinogen levels, determined by the change from within 75 min before to 75 min after completion of the first dose of fibrinogen supplementation. The secondary safety outcomes are (1) adverse events (AEs) and serious AEs (SAEs) up to 28 days postoperatively, (2) a composite AE grouping (death, myocardial infarction, stroke, acute liver injury, acute kidney injury and thromboembolic events) up to 28 days postoperatively and (3) the duration of mechanical ventilation, the length of intensive care unit (ICU) admission and total duration of hospitalisation, all censored at 28 days postoperatively.
The duration of the treatment period is 24 hours (from termination of CPB), and the duration of the study for each individual patient is 28 days.
Sample size
The sample size for this study was calculated based on the primary objective of demonstrating efficacy non-inferiority of the intervention (fibrinogen concentrate) relative to an active control (cryoprecipitate), with respect to the primary outcome. Determination of non-inferiority is based on a type I error probability of α=0.025 and a clinical non-inferiority margin of δ=0.20 around the mean units transfused. The choice of non-inferiority margin was largely motivated by the large degree of variation in use of blood products that is to be expected from previous studies reflecting current clinical practice, and clinical relevance in this setting.26
An empirical distribution function with a mean of 16 units and SD of 14 units was calculated based on data from a previous study by Karkouti et al 26 (each dose of apheresis or pooled platelets was counted as four units to correspond with the number of units in pooled platelets). This was used to estimate study power by performing 10 000 simulations for each of the different possible sample sizes. Using this approach, we calculated an empirical power >90% with a sample size ≥550 patients in each treatment group. Therefore, and assuming a 10% drop-out rate (patients randomised but not treated, or lost to follow-up) for the study based on the use of two treatments that are within the standard of care for CPB surgery, the planned total sample size is 1200 patients (600 per treatment group).
Randomisation and blinding
The randomisation schedule will be prepared by an independent biostatistician not involved in the conduct of the study using a permuted-block, random allocation schedule. As transfusion practice is not standardised, randomisation will be stratified by study site. The random allocation schedule will be provided to participating centres in opaque, consecutively numbered envelopes and neither healthcare providers nor individuals responsible for randomising patients will be aware of the treatment allocation at the time fibrinogen supplementation is ordered.
Patients will be randomised in a ratio of 1:1 to either the intervention (fibrinogen concentrate) or the active control (cryoprecipitate) by the blood bank technologist once the order for fibrinogen supplementation is received and inclusion/exclusion criteria are confirmed. The requirement for informed consent prior to randomisation will be waived (see the Ethics section). Patients will be blinded to treatment allocation throughout the study; treating clinicians will remain blinded only up to the point of use since the study products have distinct physical appearances and maintaining blinding is not logistically possible. All attempts will be made to blind clinicians outside of the operating room and ICU, as well as outcome assessors, to the treatment allocation.
Data analysis plan
Data collection and management
Data collection will occur following randomisation and procurement of consent (see the Ethics section). Full details of the data to be collected during the study, together with the timing and frequency of data collection, are provided in table 1.
Table 1.
Flow chart of study procedures and information collected at each study visit
| Procedures | Prior to enrolment |
Visit 1 post- randomisation (0–24 hours)* |
Visit 2 POD7/DC |
Visit 3 POD28 |
| Blood bank receives fibrinogen order† | X | (X)‡ | ||
| Inclusion and exclusion criteria | X | |||
| Randomisation | X | |||
| IMP administration§ | X | |||
| Patient (surrogate) debriefing and consent | X | (X) | ||
| Baseline data | ||||
| Demographics | X | |||
| Medical history | X | |||
| Preoperative medications | X | |||
| Surgical data | ||||
| Intraoperative medications | X | |||
| CPB time | X | |||
| Cross-clamp time | X | |||
| Circulatory arrest | X | |||
| Vital signs | X | |||
| Fluid input and output monitoring | X | |||
| Inotropes and vasopressors | X | |||
| Laboratory assessments | ||||
| Chemistry¶ | X | X | ||
| Haematology¶ | X** | X | ||
| Coagulation profile¶ | X** | X | ||
| Safety laboratories¶ | X | X | ||
| Transfusion requirements†† | ||||
| RBCs | X | X | ||
| Pooled and apheresis platelets | X | X | ||
| Plasma | X | X | ||
| Other haemostatic products | X | X | ||
| Blood loss determination using UDPB | X | X | ||
| Extubation time | X | (X) | (X) | |
| ICU length of stay | X | (X) | (X) | |
| Hospital length of stay | X | (X) | ||
| AEs and SAEs | X | X | X | |
| Concomitant medications | X | X | X | |
| Physical examination | X |
*For any activities not completed during this visit, additional visits will be undertaken to complete activities.
†After the start of surgery and during or after CPB.
‡Patients will be treated according to their group allocation for any subsequent doses needed during the treatment period (up to 24 hours after termination of CPB).
§IMP will first be administered after CPB termination.
¶As per standard practice.
**Prior to and up to 75 min after IMP administration.
††From beginning of surgery to postoperative day 7.
() if needed.
AE, adverse event; CPB, cardiopulmonary bypass; DC, discharge; ICU, intensive care unit; IMP, investigational medicinal product; POD, postoperative day; RBC, red blood cell; SAE, serious adverse event; UDPB, universal definition of perioperative bleeding.
All source records and source data will be maintained by the site investigator and preserved as stipulated by the regulatory authorities. An Electronic Data Capture system will be used to collect study data. All patient information and data will be maintained as confidential, and patients will only be identified using a sequential numbering system. The site investigator will maintain a confidential patient identification code list.
Statistical methods
In this randomised, active-control, non-inferiority trial, statistical analysis of the primary efficacy outcome will be conducted according to modified intention-to-treat (mITT) principles. The mITT population will comprise all randomised eligible patients who undergo cardiac surgery, receive at least one (partial or complete) dose of the allocated treatment and for whom consent was obtained (see the Ethics section). A secondary analysis will also be performed for the per-protocol population, which excludes patients with major protocol deviations (for example, receiving the incorrect treatment, receiving <80% of the planned dose or missing the primary efficacy assessment).
To demonstrate that treatment with fibrinogen concentrate (intervention) is clinically non-inferior to cryoprecipitate (active control) with respect to the primary outcome, a two-sample, one-sided test of the hypotheses, H0: μF/μc≥(1+δ) (inferiority) and H1: μF/μc<(1+δ) (non-inferiority), will be conducted (where μF and μc denote the mean number of transfused units in the fibrinogen concentrate and cryoprecipitate treatment groups, respectively). This will be based on a Poisson regression model (generalised linear model for count data with log-link function and a Poisson error term27) and clinical non-inferiority margin of δ=0.20 around the mean units transfused. Non-inferiority of fibrinogen concentrate will be concluded if the upper limit of the one-sided CI for the ratio μF/μc is less than (1 + δ). Where non-inferiority is demonstrated, a test for clinical superiority of fibrinogen concentrate with respect to the number of ABPs transfused will be performed by testing the hypotheses: H′0: μF/μc≥1 (inferiority) and H′1: μF/μc<1 (superiority).
We also plan to examine a number of exploratory secondary outcomes in the analysis of efficacy: the number of ABPs administered from beginning of surgery up to 7 days postoperatively and within 24 hours after CPB termination, stratified by ABP type, will be examined using point estimates with two-sided 95% CIs, and descriptive statistics; major bleeding type will be evaluated by frequency distributions; and change in fibrinogen levels within 75 min before and after intervention will be tested using the Wilcoxon rank-sum test and the Hodges-Lehmann estimator of median differences with 95% CIs. Analyses for efficacy will also be performed in patient subgroups, classified based on urgency and complexity of surgery.
Evaluation of safety outcomes, AEs and SAEs will be conducted in the safety analysis population (SAF), comprising all patients who receive at least one dose of study drug and provide informed consent (see the Ethics section). Analysis of AEs will focus on treatment emergent AEs, defined as AEs that start or worsen after the start of treatment (intervention or active control group). This analysis will be based on calculating point estimates and two-sided 95% CIs, in addition to descriptive statistics.
The number of patients who died will be summarised. A possible difference between treatment groups will be estimated by the risk ratio with 95% CI. Kaplan-Meier estimates for the time to death distribution will be calculated and graphically presented.
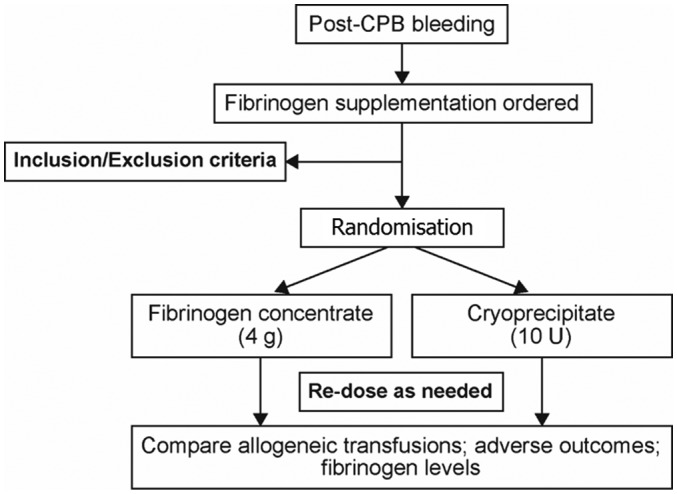
One preplanned interim analysis will be conducted after 600 patients have been randomised. This will take the form of an unblinded interim analysis using an adjusted type I error rate according to the O’Brien-Fleming method.28 At this point, enrolment may be stopped if a positive outcome, that is, rejection of H0, is demonstrated based on the adjusted one-sided significance level of α=0.00258 (efficacy stop) or if the predictive power for the test of non-inferiority is less than 0.25 (futility stop) (figure 2). The study will continue as planned if neither scenario is fulfilled at the interim analysis. A final analysis will then be performed after an additional 600 patients have been randomised at the adjusted significance level of α=0.02242 to maintain the overall one-sided significance level of 0.025.
Figure 2.
Study decision process at the point of the interim analysis. IDSMC, Independent Data and Safety Monitoring Committee; N, number; PI, Principal Investigator.
Monitoring and quality control and assurance
An Independent Data and Safety Monitoring Committee (IDSMC) will be established by the Principal Investigator/Sponsor to review study data after each (approximately) 100 patients have been randomised. A meeting will also be convened to specifically evaluate the outcome of the preplanned interim analysis. Meetings of the committee may also be called at other times, as deemed necessary based on occurrence of serious adverse events or any logistical concerns. The results of each IDSMC meeting will be communicated to the Principal Investigator/Sponsor within 15 days, or earlier in matters relating to ensuring patient safety and/or study integrity. The IDSMC will comprise a minimum of three voting members with collective expertise in the fields of statistics, perioperative medicine and haematology, who will review accumulating data pertaining to efficacy, safety, outcomes and other study aspects such as recruitment, compliance, data quality and risk versus benefit. The IDSMC will provide recommendations regarding the continuation, modification or termination of the study, as appropriate. The duties and responsibilities of the IDSMC will be defined in a written, study-specific charter. Ultimately, the role of the IDSMC will be to protect and serve study participants, and to assist and advise the Principal Investigator/Sponsor in the overall conduct, interpretation, validity, integrity and ongoing relevance of the study. The Principal Investigator/Sponsor will have ultimate authority in all aspects of the trial and will have access to the final trial dataset.
For quality control and assurance purposes, periodic monitoring of all study-related source data/records, adherence to the approved study protocol, and the completeness and accuracy of CRFs will be undertaken by an appointed independent study monitor. Full and direct access to all source documents will be provided. All study-related material will also be made available to independent quality assurance auditors and regulatory inspectors, as required.
Ethics and dissemination
The study will be conducted in accordance with the ethical principles defined by the Declaration of Helsinki, and in compliance with the approved study protocol, Good Clinical Practice guidelines, and all appropriate regulatory requirements (including collecting and reporting of SAEs) governing the study centres participating in the trial. The study, the study protocol and all other study documents have been approved by the University Health Network’s (the coordinating centre) research ethics board (REB no. 16-5636; approval date: 12 January 2017), the local REB of all participating sites and regulatory authority (Health Canada). The trial is registered at ClinicalTrials.gov (identifier: NCT03037424). Changes to protocol will be communicated by the Sponsor to all REBs, Health Canada, and will be documented on ClinicalTrials.gov.
Due to the emergency nature of the clinical setting, that is, bleeding during or after surgery, all patients included in the study will be incapable of providing informed consent at the time treatment is required. Furthermore, delays brought about by obtaining surrogate consent can be severely detrimental to patient well-being. Moreover, this bleeding complication occurs infrequently (approximately 5% of cases) and cannot be reliably predicted before surgery, and a requirement to obtain prior consent from patients would make it impracticable to conduct the study. The study compares two fibrinogen replacement sources that are currently within the standard of care for this surgical procedure in patients who have consented to receiving blood transfusions, requires no additional interventions outside of standard clinical care and therefore poses only minimal risk to patients. For the reasons outlined, the study therefore meets the criteria stated in Article 3.7A of the 2014 Tri-Council Policy Statement on the Ethical Conduct for Research Involving Humans that define situations where exceptions to obtaining prior consent are warranted. As per these criteria, written informed consent for follow-up and use of the patients’ data will be obtained as soon as possible after randomisation. If the patient is not capable of providing informed consent, consent will be sought from the surrogate decision-maker. Patients will then be revisited every few days up to postoperative day 28 to obtain their direct consent where possible. Waiver of patient consent at time of randomisation allows efficient inclusion of a large number of bleeding patients and minimises postrandomisation drop-outs; this is a novelty of the study design and an approach not commonly used in bleeding surgical patients.
At completion of the study, and in accordance with the relevant guidelines, the Sponsor/Investigator will prepare a clinical study report to report the outcomes of the study and may publish the data in their entirety as a multicentre dataset. We intend to disseminate the findings of the study in a timely fashion at international scientific meetings and will publish our findings in the scientific/medical literature.
Patient and public involvement
Patients and the public were not involved in the design of the study.
Conclusion
This protocol for the phase III FIBRES trial describes a multicentre, randomised, non-inferiority study comparing the use of fibrinogen concentrate versus cryoprecipitate as active control in the treatment of acquired hypofibrinogenaemia in patients undergoing CPB cardiac surgery. The study has a number of strengths. First, it uses a pragmatic approach and treatment algorithm that align with standard clinical practice. This increases the likelihood of protocol adherence and also increases generalisability by ensuring that the study has direct clinical relevance to current treatment practice. Second, the waiver of patient consent prior to treatment improves study feasibility (cost and time) and minimises postrandomisation drop-outs. Third, use of an active control group ensures that all randomised patients receive fibrinogen supplementation according to clinical need. Fourth, the enrolment of approximately 1200 patients represents the largest randomised controlled trial in this setting to date.
This study in bleeding cardiac surgical patients aims to show efficacy non-inferiority of fibrinogen concentrate, a highly purified fibrinogen product that has improved safety, ease of administration, and a predictable and robust effect on fibrinogen levels, when compared with cryoprecipitate. A finding of non-inferiority would support the use of this purified fibrinogen concentrate as an appropriate option for fibrinogen supplementation in acquired hypofibrinogenaemia. Ultimately, the results of this trial are likely to improve the care of cardiac surgical patients experiencing significant bleeding, an understudied yet high-risk population.
Supplementary Material
Acknowledgments
Editorial assistance was provided by Portland Medical Communications Ltd.
Footnotes
Contributors: Conception and design: KK, JC. Preparation of the first draft of the manuscript: KK. Critical revision of the manuscript for important intellectual content: KK, JC, VR, NH, MEF, MAC, DCS. Read and approved the final version of the manuscript to be published: KK, JC, VR, NH, MAF, MAC, DCS.
Funding: This work was supported by Octapharma AG through an unrestricted grant for study conduct and the provision of fibrinogen concentrate. Cryoprecipitate was provided by Canadian Blood Services.
Competing interests: KK has received support for research and/or honoraria from Octapharma. JC has received support for research through peer-reviewed grants from Canadian Blood Services. NH is the Research Director for the McMaster Centre for Transfusion Research, which receives funding support from Canadian Blood Services and Health Canada. The remaining authors have no competing interests or conflicts to declare.
Patient consent: Not required.
Ethics approval: UHN.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Karkouti K, O’Farrell R, Yau TM, et al. Prediction of massive blood transfusion in cardiac surgery. Can J Anaesth 2006;53:781–94. 10.1007/BF03022795 [DOI] [PubMed] [Google Scholar]
- 2. Karkouti K, Wijeysundera DN, Beattie WS, et al. Variability and predictability of large-volume red blood cell transfusion in cardiac surgery: a multicenter study. Transfusion 2007;47:2081–8. 10.1111/j.1537-2995.2007.01432.x [DOI] [PubMed] [Google Scholar]
- 3. Karkouti K, Wijeysundera DN, Yau TM, et al. The independent association of massive blood loss with mortality in cardiac surgery. Transfusion 2004;44:1453–62. 10.1111/j.1537-2995.2004.04144.x [DOI] [PubMed] [Google Scholar]
- 4. Moulton MJ, Creswell LL, Mackey ME, et al. Reexploration for bleeding is a risk factor for adverse outcomes after cardiac operations. J Thorac Cardiovasc Surg 1996;111:1037–46. 10.1016/S0022-5223(96)70380-X [DOI] [PubMed] [Google Scholar]
- 5. Kozek-Langenecker SA, Ahmed AB, Afshari A, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: first update 2016. Eur J Anaesthesiol 2017;34:332–95. 10.1097/EJA.0000000000000630 [DOI] [PubMed] [Google Scholar]
- 6. Levy JH, Welsby I, Goodnough LT. Fibrinogen as a therapeutic target for bleeding: a review of critical levels and replacement therapy. Transfusion 2014;54:1389–405. 10.1111/trf.12431 [DOI] [PubMed] [Google Scholar]
- 7. Mosesson MW, Siebenlist KR, Meh DA. The structure and biological features of fibrinogen and fibrin. Ann N Y Acad Sci 2001;936:11–30. 10.1111/j.1749-6632.2001.tb03491.x [DOI] [PubMed] [Google Scholar]
- 8. Miesbach W, Schenk J, Alesci S, et al. Comparison of the fibrinogen Clauss assay and the fibrinogen PT derived method in patients with dysfibrinogenemia. Thromb Res 2010;126:e428–33. 10.1016/j.thromres.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 9. Acharya SS, Dimichele DM. Rare inherited disorders of fibrinogen. Haemophilia 2008;14:1151–8. 10.1111/j.1365-2516.2008.01831.x [DOI] [PubMed] [Google Scholar]
- 10. Karkouti K, McCluskey SA, Syed S, et al. The influence of perioperative coagulation status on postoperative blood loss in complex cardiac surgery: a prospective observational study. Anesth Analg 2010;110:1533–40. 10.1213/ANE.0b013e3181db7991 [DOI] [PubMed] [Google Scholar]
- 11. Blome M, Isgro F, Kiessling AH, et al. Relationship between factor XIII activity, fibrinogen, haemostasis screening tests and postoperative bleeding in cardiopulmonary bypass surgery. Thromb Haemost 2005;93:1101–7. 10.1160/TH04-12-0799 [DOI] [PubMed] [Google Scholar]
- 12. Karkouti K, Callum J, Crowther MA, et al. The relationship between fibrinogen levels after cardiopulmonary bypass and large volume red cell transfusion in cardiac surgery: an observational study. Anesth Analg 2013;117:14–22. 10.1213/ANE.0b013e318292efa4 [DOI] [PubMed] [Google Scholar]
- 13. Karlsson M, Ternström L, Hyllner M, et al. Plasma fibrinogen level, bleeding, and transfusion after on-pump coronary artery bypass grafting surgery: a prospective observational study. Transfusion 2008;48:2152–8. 10.1111/j.1537-2995.2008.01827.x [DOI] [PubMed] [Google Scholar]
- 14. Ternström L, Radulovic V, Karlsson M, et al. Plasma activity of individual coagulation factors, hemodilution and blood loss after cardiac surgery: a prospective observational study. Thromb Res 2010;126:e128–e133. 10.1016/j.thromres.2010.05.028 [DOI] [PubMed] [Google Scholar]
- 15. Yang L, Vuylsteke A, Gerrard C, et al. Postoperative fibrinogen level is associated with postoperative bleeding following cardiothoracic surgery and the effect of fibrinogen replacement therapy remains uncertain. J Thromb Haemost 2013;11:1519–26. 10.1111/jth.12304 [DOI] [PubMed] [Google Scholar]
- 16. Mace H, Lightfoot N, McCluskey S, et al. Validity of thromboelastometry for rapid assessment of fibrinogen levels in heparinized samples during cardiac surgery: a retrospective, single-center, observational study. J Cardiothorac Vasc Anesth 2016;30:90–5. 10.1053/j.jvca.2015.04.030 [DOI] [PubMed] [Google Scholar]
- 17. Fenger-Eriksen C, Ingerslev J, Sørensen B. Fibrinogen concentrate—a potential universal hemostatic agent. Expert Opin Biol Ther 2009;9:1325–33. 10.1517/14712590903193051 [DOI] [PubMed] [Google Scholar]
- 18. Stinger HK, Spinella PC, Perkins JG, et al. The ratio of fibrinogen to red cells transfused affects survival in casualties receiving massive transfusions at an army combat support hospital. J Trauma 2008;64:S79–S85. 10.1097/TA.0b013e318160a57b [DOI] [PubMed] [Google Scholar]
- 19. Nascimento B, Goodnough LT, Levy JH. Cryoprecipitate therapy. Br J Anaesth 2014;113:922–34. 10.1093/bja/aeu158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sørensen B, Bevan D. A critical evaluation of cryoprecipitate for replacement of fibrinogen. Br J Haematol 2010;149:834–43. 10.1111/j.1365-2141.2010.08208.x [DOI] [PubMed] [Google Scholar]
- 21. Franchini M, Lippi G. Fibrinogen replacement therapy: a critical review of the literature. Blood Transfus 2012;10:23–7. 10.2450/2011.0015-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kozek-Langenecker S, Fries D, Spahn DR, et al. III. Fibrinogen concentrate: clinical reality and cautious Cochrane recommendation. Br J Anaesth 2014;112:784–7. 10.1093/bja/aeu004 [DOI] [PubMed] [Google Scholar]
- 23. Fries D. The early use of fibrinogen, prothrombin complex concentrate, and recombinant-activated factor VIIa in massive bleeding. Transfusion 2013;53(Suppl 1):91S–5. 10.1111/trf.12041 [DOI] [PubMed] [Google Scholar]
- 24. Callum JL, Karkouti K, Lin Y. Cryoprecipitate: the current state of knowledge. Transfus Med Rev 2009;23:177–88. 10.1016/j.tmrv.2009.03.001 [DOI] [PubMed] [Google Scholar]
- 25. Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg 2014;147:1458–63. 10.1016/j.jtcvs.2013.10.070 [DOI] [PubMed] [Google Scholar]
- 26. Karkouti K, Callum J, Wijeysundera DN, et al. Point-of-care hemostatic testing in cardiac surgery: a stepped-wedge clustered randomized controlled trial. Circulation 2016;134:1152–62. 10.1161/CIRCULATIONAHA.116.023956 [DOI] [PubMed] [Google Scholar]
- 27. Cameron AC, Trivedi PK. Regression analysis of count data. 1st edn Cambridge, UK: Cambridge University Press, 1998. [Google Scholar]
- 28. Fleming TR, Harrington DP, O’Brien PC. Designs for group sequential tests. Control Clin Trials 1984;5:348–61. 10.1016/S0197-2456(84)80014-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.