Abstract
The translation of evidence-based health innovations into real-world practice is both incomplete and exceedingly slow. This represents a poor return on research investment dollars for the general public. U.S. funders of health sciences research (e.g., NIH, CDC, NIOSH) are increasingly calling for dissemination plans, and to a lesser extent for dissemination and implementation (D&I) research, which are studies that examine the effectiveness of D&I efforts and strategies and the predictors of D&I success. For example, rather than merely broadcasting information about a preventable hazard, D&I research in occupational safety and health (OSH) might examine how employers or practitioners are most likely to receive and act upon that information. We propose here that D&I research should be seen as a dedicated and necessary area of study within OSH, as a way to generate new knowledge that can bridge the research-to-practice gap. We present D&I concepts, frameworks, and examples that can increase the capacity of OSH professionals to conduct D&I research and accelerate the translation of research findings into meaningful everyday practice to improve worker safety and health.
Keywords: Dissemination, Implementation, Research to practice, Occupational safety and health, TotalWorker Health, Health innovations
In the health sciences, it might seem natural to assume that once an intervention is established as efficacious and effective in promoting health or preventing disease or injury, that intervention should enjoy an effortless spread and widespread uptake. But this is not necessarily the case. Many interventions with no evidence basis (e.g., fad diets for weight loss) are successfully communicated and widely adopted into practice, while some efficacious, inexpensive and simple interventions (e.g., water boiling to prevent pathogenic infection) fail to do so (Bravata et al. 2003; Rogers 2003). In fact, in clinical medicine, many evidence-based health innovations (EBHIs) – programs, practices, and policies with demonstrated efficacy and effectiveness – are never translated into real-world practice, and for those that are, the process is exceedingly slow (Balas and Boren 2000).
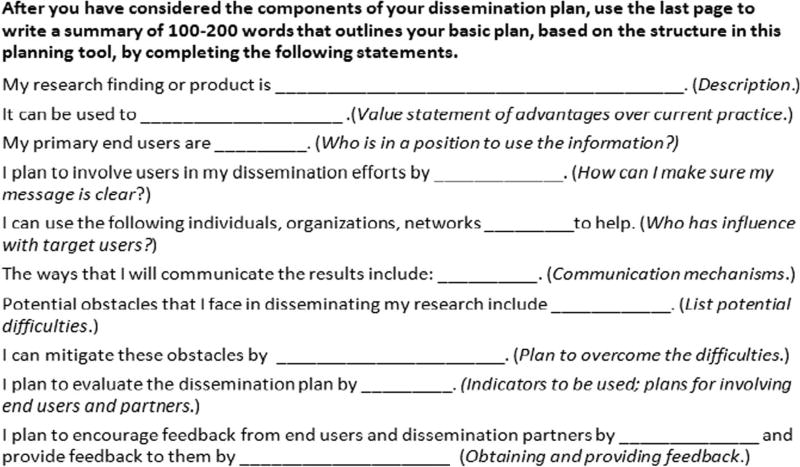
The regrettably low impact of EBHIs for the betterment of public health is a primary concern for the largest funders of health sciences research (e.g., NIH and CDC in the United States), which have acknowledged the poor return on their investment dollars over decades (Rabin et al. 2008). These funders are now increasingly making it a priority to bridge the gap between research and practice by requiring dissemination strategies to be included in research grant applications. Guidelines for good dissemination practice are available, for example, in the Dissemination Planning Tool (Agency for Healthcare Research Quality 2014). This tool was developed via a broad review of dissemination theory and the synthesis of dissemination tools from various fields with expert review, refinement, and testing. It guides investigators through a comprehensive, easy to use six-part process of packaging research findings and products, identifying target end-users, identifying and engaging dissemination partners, communicating the intended message, developing and administering measures to evaluate dissemination success, and implementing the dissemination plan (Figure 1).
Fig. 1.
Summary of Dissemination Plan (AHRQ 2014)
Similarly, the National Institute for Occupational Safety and Health (NIOSH) strongly supports dissemination through its Research-to-Practice (r2p) initiative. The r2p mission is to put NIOSH-generated findings into practice to prevent fatalities, injuries, and illnesses that occur at work (National Institute for Occupational Safety and Health 2015a). The six components of NIOSH’s r2p approach include: developing partnerships with those who can help put research into practice, conducting intramural research, funding extramural research, transferring findings to the public or private sector, communicating findings to target audiences, and evaluating the efficacy of efforts aimed at improving worker health and safety. The NIOSH-funded Center for Construction Research and Training (CPWR) has developed a Dissemination Roadmap, under the auspices of CPWR’s r2p initiative (CPWR Center for Construction Research and Training 2014). This tool prompts researchers to identify their research products and output, stakeholder partners, communication channels, resources and barriers, and indicators of success.
Conducting a well-designed dissemination effort, with consideration of these variables, and then evaluating the net uptake (e.g., number of website hits or document downloads, or changes in clinical practice), are both valuable. However, creating and following a dissemination plan – the practice of dissemination – is not the same as formal study of the variables that determine dissemination effectiveness. Dissemination of information about effective health innovations may have more or less success depending on how the findings are packaged and communicated, as well as characteristics of the intended user and the context (Chaudoir et al. 2013). Often these factors are investigated (if at all) in an ad-hoc manner, by trial and error.
As developed in more detail below, the intent of D&I research is to build a knowledge base of the factors that facilitate or hinder the effective delivery of EBHIs, and the extent to which these predictors might vary among the desired end-user groups or settings where they can have an impact on human well-being (whether in health clinics, workplaces, schools, communities, or other). Increasingly, NIH is urging researchers to conduct formal dissemination and implementation (D&I) research by offering project grants specifically for D&I research (National Institutes of Health 2016) and sponsoring conferences to build researcher capacity to conduct D&I research (e.g., NIH’s Annual Conference on the Science of Dissemination and Implementation in Health).
To date, there has been very limited conduct of D&I research specifically in the field of occupational safety and health (OSH). Our two main objectives in writing this paper are, therefore: (1) to propose D&I research as a dedicated area of study within OSH; and (2) to provide OSH researchers with useful concepts, frameworks, and examples that can increase their capacity to conduct D&I research and accelerate the translation of research findings that improve worker safety and health into meaningful everyday practice.
Important Concepts and Terminology
D&I science is an emerging field with a somewhat disorderly body of literature. The research has roots in many disciplines, with most of the seminal contributions coming from non-health fields (e.g., agriculture, education, marketing, communications, management) (Rabin et al. 2008). These disparate origins have produced a lack of standardization in the use of terminology and the key concepts within D&I science. In addition to confusing terminology, there is no unanimity in D&I science regarding the best ways to model and measure D&I-related phenomena. D&I activities are often complex and situation-specific. There are countless differences across the body of EBHIs in terms of their foci, intended outcomes, designs, approaches, and targeted audiences and settings, and it is nearly impossible to create universal models that capture all these differences (Chaudoir et al. 2013).
Also, the same EBHI at each new instance of real-world implementation is a singular and unique entity, with many moving parts (e.g., people, environments, systems) operating in a constantly shifting state of dynamic interplay. Thus the results of any given trial are difficult to compare to all other instances of implementation of the same EBHI. For all these reasons, D&I science does not yet offer theories or even patterns of consistent causal predictor-outcome relationships among D&I related constructs, or provide well-established measures with strong psychometric properties for assessing constructs in all settings. Nonetheless, the development of taxonomies of relevant characteristics of the dissemination product, strategy, and/or context has begun to facilitate more systematic compilation of the lessons learned to date (e.g., Chaudoir et al. 2013).
In this paper, health innovation means “an idea, practice, or object that is perceived as new by an individual or other unit of adoption” (Rogers 2003, p. 12). We use this term rather than health intervention to indicate that the objects of D&I include the broad range of programs, practices, policies, and guidelines that might improve health or prevent illness (Rabin et al. 2008). Evidence-based health innovations are those that have demonstrated the ability to improve desired health outcomes. This typically occurs via the “Discovery-Delivery Continuum” (Schillinger 2010), a step-wise developmental research approach in which an innovation undergoes first an efficacy study to determine if it improves health under controlled conditions, followed by an effectiveness study to evaluate whether it improves health under real-world conditions.
Implementation is “the use of strategies to adopt and integrate evidence-based health interventions into clinical and community settings in order to improve patient outcomes and benefit population health” (National Institutes of Health 2016). Implementation research examines when, why, and how innovations are integrated (or fail to integrate) into the settings and systems that deliver them, and to test implementation strategies to determine which are associated with the greatest success, as determined by attaining implementation outcomes such as adoption, fidelity, and sustainability.
Dissemination is the active and deliberate process of packaging and distributing information about EBHIs to a specific audience of potential adopters via predetermined media channels (Carpenter et al. 2005; Rabin et al. 2008). It is based on the creation and supply of information about the EBHI by its developers or sponsors and is therefore conceptualized as a “push” strategy from the source of the EBHI (Dearing and Kreuter 2010). Dissemination research examines when, why, and how innovations are most successfully spread to desired end-users, and addresses topics such as innovation messaging and packaging, user-perceptions of information received, and social networks used to transmit EBHIs. Dissemination success may be determined by assessing final outcomes such as adoption and sustainability, as well as intermediary outcomes such as the number of end-users reached with a social marketing campaign, or the number of responses to advertisements in trade journals.
Diffusion is a related but distinct concept from dissemination, defined as the relatively passive and unplanned process by which information about an EBHI spreads in an uncontrolled way through communication channels to members of a social system (Rabin et al. 2008; Carpenter et al. 2005). It is sensitive to social influence and occurs when, through their communication with actual adopters, potential adopters decide to adopt an EBHI. It is conceptualized as a “pull” strategy that is achieved when the EBHI is designed in such a way that potential adopters are drawn to it, experiment with it, adopt it, and talk about it to others (Dearing and Kreuter 2010). Although diffusion is not as effective in spreading EBHIs as dissemination, the two activities are complementary and both should be pursued. For both processes, steps should be taken in the formative stages of developing an innovation to ensure that it meets the needs of and is perceived as desirable by potential adopters (Carpenter et al. 2005, Dearing and Kreuter 2010; Rogers 2003).
In the discovery-delivery sequence summarized above, D&I studies typically occur after effectiveness has been demonstrated. While efficacy and effectiveness research is concerned with studying specific health or safety outcomes, D&I research is specifically concerned with D&I-specific outcomes such as the initial uptake, adoption and sustainability of the innovation. This distinction in study foci and outcomes is important, because an innovation that has not successfully demonstrated health improvements nevertheless has the potential to be successfully disseminated and implemented (and vice versa).
A potential downside to the traditional sequence is that the impact or relative merit of varying dissemination approaches is not examined until effectiveness is established. Yet successful dissemination is precisely one of the factors required to study effectiveness of the EBHI, in contrast to its efficacy. If an effectiveness trial fails because there was insufficient dissemination and uptake in the real world, valuable resources are wasted. Intentionally conducting D&I studies as the second step could produce evidence that guides refinements of the EBHI, its presentation and/or its dissemination so as to produce a more meaningful effectiveness trial.
A D&I Framework and Taxonomy
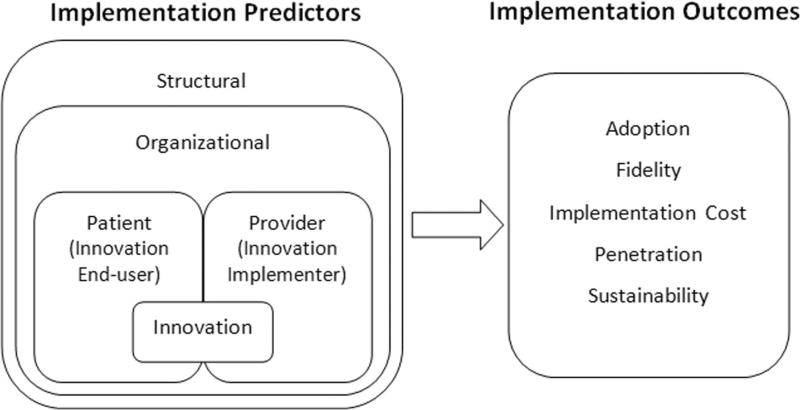
For researchers who want to conduct a D&I study, a relatively simple framework proposed by Chaudoir et al. (2013) is a useful starting point for identifying predictors (barriers and facilitators) and outcomes of D&I success, and examining associations between them. The authors showed a convergence among published D&I models by organizing the factors hypothesized to predict implementation outcomes into broad classes of variables operating at different levels of influence, from micro to macro (Figure 2). This multi-level framework contains five nested factors that are implementation predictors – variables that act as barriers or facilitators of implementation success – and five categories of implementation outcomes.
Fig. 2.
Five-level Framework by Chaudoir et al. (2013)
Among the predictors, structural factors pertain to aspects of the external physical environment, political and economic context, and sociocultural context of the outer community where the organization implementing the EBHI is located. Organizational factors are related to the organization that is implementing the EBHI. Provider factors pertain to the person who is implementing the EBHI in the field. Innovation factors are characteristics of the EBHI being implemented. Although intervention recipients are rarely taken into consideration in implementation research, the people whose health is intended to benefit from the EBHI can also influence implementation success. Thus, in contrast to prior D&I models, this framework includes patient factors, which pertain to the person receiving the EBHI (e.g., their level of health literacy or socioeconomic status). See Table 1 for more detailed information and examples of the five levels of implementation predictors.
Table 1.
Taxonomy of implementation predictors
| Predictor Level | Definition | Examples |
|---|---|---|
| Structural | Variables related to the outer physical environment (natural and built), political and economic systems and circumstances, or sociocultural context within which the organization implementing the EBHI is nested | A mountainous community with limited access to employment and health services, a town with car-free infrastructure for bicycle and pedestrian transit, a conservative state with laws that restrain labor unions, a country with universal health care, a city with an ordinance banning public smoking, a community with a strong commitment to diversity and inclusion |
| Organizational | Variables related to the organization implementing the EBHI | An organization (e.g., a business, labor union, school, church) with a strong health and safety culture, senior leaders that are supportive of their members, or organizational members with high morale and engagement |
| Provider | Variables related to the individual person implementing the EBHI | An EBHI implementer (e.g., an allied health professional, industrial hygienist, psychologist, human resources professional) who has an extroverted personality, is highly educated, is philosophically aligned with evidence-based practice, is satisfied with their job and pay, or has high self-efficacy with implementing the EBHI |
| Alternative term: EBHI implementer | ||
| Patient | Variables related to the individual person receiving the EBHI | An EBHI end-user (e.g., a patient, worker, student, consumer) with high levels of health literacy, motivation, conscientiousness, socioeconomic status, or trust in EBHI developers and implementers |
| Alternative term: EBHI end-user | ||
| Innovation | Variables related to the EBHI being implemented | An EBHI (e.g., program, practice, policy, product) that is acceptable, appropriate, simple, trialable, observable, feasible, adaptable, cost-effective, compatible, scientifically credible, effective in achieving health goals, or has relative advantage |
EBHI = Evidence-based health innovations
This social-ecological type framework is broad enough to capture the many moving parts of an implementation process and can also be adapted for use with many types of EBHIs in many different settings, including workplaces. The terminology of provider and patient derives from the D&I literature, which mainly addresses EBHIs evaluated in clinical care settings. However, the constructs of provider and patient can generally be understood as EBHI implementer and EBHI end-user, and this language can be adapted to any non-clinical implementation setting. In the workplace, for example, if the EBHI is a hearing conservation program, the implementer might be the occupational hygienist and the end-user would be the worker. Given the hierarchies of decision authority in most workplaces, the implementer might also be the manager who has the authority to allocate the necessary resources for the program.
The framework also shows the five implementation outcomes – adoption, fidelity, cost, penetration, and sustainability – which are indicators of implementation success, as originally compiled and defined by Proctor et al. (2011). Most of the outcomes can be assessed at the individual, organizational, and structural levels of analysis, whichever is most appropriate for the type of EBHI (See Table 2 for more detailed information and examples of the five implementation outcomes.)
Table 2.
Taxonomy of implementation outcomes
| Outcome Variable | Definition | Levels of Analysis with Examples |
|---|---|---|
| Adoption | Intending to use, deciding to use, or actually using an EHBI | Structural: A state health district’s decision to adopt a county-wide cardiovascular health awareness and action campaign |
| Organizational: A company’s decision to utilize a new health promotion program | ||
| Individual EBHI implementer: An occupational hygienist’s intent to try out a new hearing conservation program | ||
| Individual EBHI end-user: A worker’s use of noise-cancelling headphones | ||
| Fidelity | The degree to which the EBHI was implemented as specified or intended by its developers | Structural: The number of topics covered in a community-wide eight-session bullying prevention program of the eight topics prescribed (one per session) |
| Organizational: The percentage of CDC vending-machine guidelines for healthy food and nutrition that a worksite’s vending machine meets | ||
| Individual EBHI implementer: The level of a counselor’s skill in delivering a brief cognitive-behavioral intervention to police officers with post-traumatic stress | ||
| Individual EBHI end-user The extent of a worker’s adherence to an exercise prescription with weekly goals for exercise type, frequency, duration, and intensity | ||
| Cost | The financial impact of the implementation effort; can be assessed as cost-effectiveness, cost-benefit, or actual cost | Structural: The expense of maintaining a social media platform to promote and coordinate a county-wide partnership of businesses, schools, and faith groups focused on preventing chronic disease |
| Organizational: The cost of training maintenance workers at a worksite in new ventilation cleaning procedures to improve indoor air quality | ||
| Individual EBHI implementer: The fee that a substance abuse professional pays for a professional development training on group counseling for addicted workers | ||
| Individual EBHI end-user: The amount a worker pays for an employer-subsidized annual gym membership | ||
| Penetration | The extent to which the EBHI reaches all eligible people, including all possible people who could implement the EBHI, and/or all possible people who could receive the EBHI | Structural: The percentage of a city’s population that participates in at least one component of a community health promotion and disease prevention initiative |
| Organizational: The ratio of workers who participate in a sleep improvement intervention to the total number of workers in the company. | ||
| Sustainability | The extent to which the EBHI becomes institutionalized within an implementing organization’s permanent operations or becomes a routine practice within an individual end-user’s behavioral repertoire | Organizational: A company has a permanent line item on its annual budget to fund the development and delivery of a health improvement workshop for its workforce |
| Individual EBHI implementer: After being trained to use a structured participatory ergonomics process for generating health interventions, HR professionals were significantly more likely to use the process to address workforce health concerns | ||
| Individual EBHI end-user: A group of transportation workers significantly increased daily sunscreen application following a skin cancer prevention program |
EBHI = Evidence-based health innovations
Adoption (sometimes referred to as uptake) is defined as intending to use, deciding to use, or actually using an EHBI. It can be measured with surveys, interviews, administrative data, and observation. Fidelity (sometimes referred to as adherence) is the degree to which the EBHI was implemented as specified or intended by its developers, and measures typically assess three aspects of fidelity: adherence to the program protocol, dose (or amount) of program delivered, and quality of program delivery. Fidelity assesses the EBHI implementer’s activities, whether at the individual, organizational, or structural/community level (depending on who the implementer is), and can be evaluated through observation or self-report using activity checklists, rating sheets, or coding schemes. Cost is the financial impact of the implementation effort, and can be assessed as cost-effectiveness, cost-benefit, or actual cost. The level of analysis depends on who is providing or utilizing the EBHI and can come through administrative data or self-report. Penetration (sometimes referred to as reach or spread) is the extent to which the EBHI reaches all eligible people, including all possible providers who could deliver the EBHI, and/or all possible patients who could receive the EBHI. Penetration is often assessed with checklists or by case audit, and may be measured by calculating a ratio of the number of actual EBHI recipients divided by the total number of eligible EBHI recipients, or the number of providers who actually deliver the EBHI divided by the total number of providers expected to deliver the EBHI. Sustainability (sometimes referred to as maintenance or institutionalization) is the extent to which an EBHI becomes institutionalized within an implementing organization’s permanent operations (e.g., through stable funding, annual training programs, or performance evaluation criteria), or becomes a routine practice within an individual user’s behavioral repertoire. Sustainability can be assessed using surveys, interviews, administrative data, checklists, or case audits.
As indicated above, implementation predictors and outcomes can be assessed quantitatively (e.g., survey scales), qualitatively (e.g., focus groups, interviews), or both. Chaudoir et al. (2013) listed 62 scales available to measure the five levels of implementation predictors, along with information about criterion validity (i.e., whether the construct is associated with key implementation outcomes). Proctor et al. (2011) provided details regarding how the implementation outcomes have been measured in previous studies, using qualitative and quantitative methods, and in many cases, where to find them.
Examples of Worker Health D&I Research
Here we provide examples of how CPH-NEW researchers could use or have used the Chaudoir et al. (2013) five-level framework to inform D&I research on topics related to worker health. These include four (hypothetical) studies in which adoption or related outcomes are assessed with the end-user being the implementer or her/his organization, and two (actual) studies with assessment of the individual worker as the end-user. Some illustrate use of an experimental design and quantitative comparison; others involve primarily qualitative assessment, using methods similar to those typical of process evaluation. Although not specific to occupational health, the clinical and community health literature offers additional examples of published D&I-related articles, including both experimental D&I studies (Dunn et al. 2012; Nahm et al. 2015; Tapp et al. 2014) as well as studies that examine D&I constructs as part of their process evaluation (Hernandez et al. 2017; Kennedy et al. 2017; Northridge et al. 2017).
Most of the following examples refer to the Healthy Workplace Participatory Program (HWPP) developed by researchers at the Center for the Promotion of Health in the New England Workplace (CPH-NEW), a NIOSH Center of Excellence for Total Worker Health® (TWH). The HWPP is a suite of program tools (Center for the Promotion of Health in the New England Workplace 2011) for conducting participatory action research that was created specifically to fill a gap in the translational OSH and TWH research literature (National Institute for Occupational Safety and Health, 2015b; Nobrega et al. 2017). The core tool is the Intervention Design and Analysis Scorecard (IDEAS), a 7-step process for planning TWH interventions, which are “integrated” interventions that both promote and protect worker health by addressing factors that affect health at work and outside of work. IDEAS is used by a committee or design team of frontline workers to identify priority health and safety concerns along with their root causes, brainstorm and design possible interventions, and recommend interventions to a steering committee of middle- and/or senior-level managers (Robertson et al. 2013).
Example One
The HWPP is publicly available on-line with training materials, but some users seek practical training from CPH-NEW. We could design a study in which we offer training either in person or by webinar. We might identify 24 organizations that have requested training and randomize them between the two delivery systems. Two months later, we could contact each trainee and ask if s/he intends to use the program in that organization, and whether or not s/he has already done so. Comparison of the responses would evaluate the implementation delivery format (i.e., the effect of a feature of the innovation) on program adoption.
Example Two
Having determined that the webinar is equally successful, and because it requires less person-time per recipient, our next study might use the webinar format only. We could select a new group of 24 volunteer employer organizations, eight each with small, medium, and large workforces (size implying more Human Resources (HR) and OSH resources available within the organization to support the HWPP). We would contact them two months after the webinar and ask if they intend to use the program, and whether or not they actually have. In this case, comparison of the results would provide evaluation of the effect of a feature of the intended end-user (i.e., the size of the organization) on adoption. If we also re-contacted them one year later, to ask whether they were still using it and how many workers they had engaged in design teams, this would give us a comparison of sustainability and penetration as a function of organization size.
Example Three
In this study we might recruit new potential HWPP users through four different regional professional organizations, for occupational health nurses, employee assistance professionals, occupational hygienists, and HR professionals. We would offer continuing education credits to each group, and each group would receive a different URL to register for the webinar so that we could count them separately. The professional organizations would provide us with information on the size of their mailing lists, so we would be able to compute an outcome variable and compare responses as proportion of e-mail recipients. Thus we could evaluate the influence of an end-user characteristic (i.e., the professional training and background of the implementer) on penetration of the profession in one geographical region.
Example Four
In order to evaluate options for effective dissemination, we could compare two strategies for communicating information about the webinar through different media channels: broadcasting through an e-mail listserv and a social media campaign through Facebook. Each announcement would contain the same content (i.e., information about the program, what needs it is designed to serve, how it is innovative, and how to find and register for the webinar). A different webinar registration URL would be circulated within each medium, enabling us to identify which information source each person is responding to; we could then compare the number of “hits” for more information and the number of registrations at each web site as the dissemination outcomes.
Example Five
In an actual study of health and safety in nursing homes, we formed and trained teams of workers in three facilities to engage in an early version of the participatory process later codified as the HWPP (Zhang et al. 2015). We conducted focus groups for needs assessment, discussed the range of possible influences on workers’ health and safety from both work and non-work sources (the integration concept central to the TWH program), and then invited them to envision and jointly brainstorm an ideal nursing home which was a health-promoting environment for the workers themselves as well as the residents for whom they provided care (Holmberg et al. 2013). Qualitative evaluations showed that the team members were highly receptive to the idea of integration, the brainstorming and prioritizing of risk factors, and the participatory process for developing solutions. Thus we were able to assess end-user perceptions of the innovation (i.e., acceptability and relevance of the participatory process and its core constructs) and demonstrate its adoption in all three facilities.
Example Six
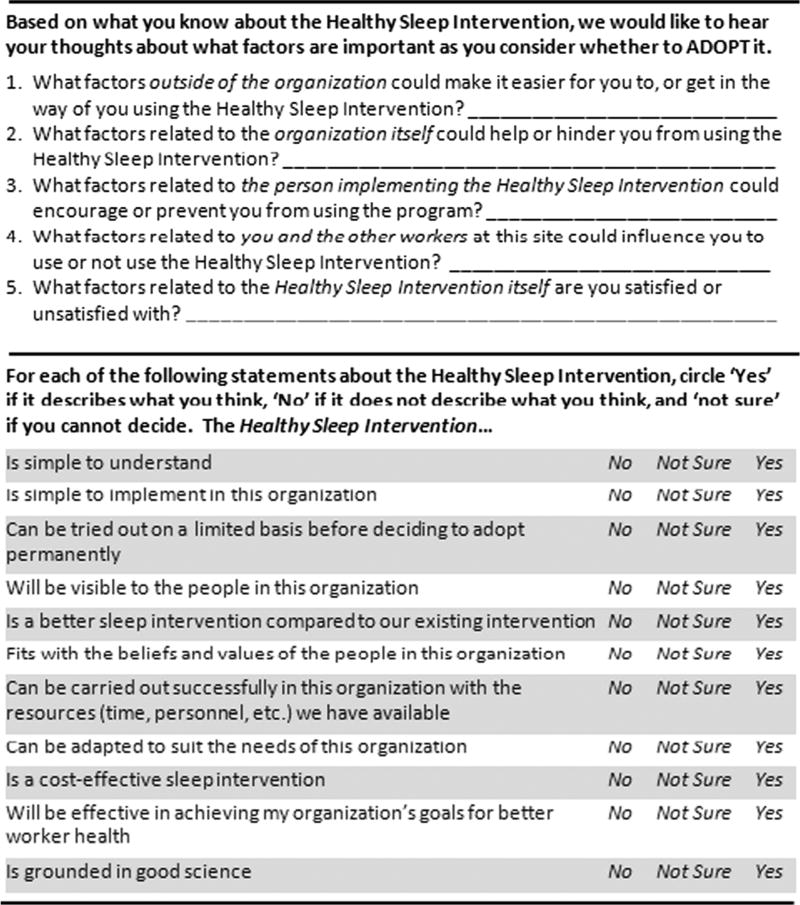
In a forthcoming study of correctional worker health and safety, correctional supervisors used the HWPP to brainstorm a list of health and safety issues and elected to prioritize sleep quality and quantity as their first priority. A Healthy Sleep Intervention was developed and is currently being implemented and evaluated.
The Five and Ten D&I Evaluation Tool (Figure 3) was developed for post-intervention assessment of selected implementation outcomes and their predictors. The first section consists of five open-ended questions on the structural, organizational, intervener, end-user, and innovation factors that may affect a given implementation outcome. The wording shown here represents factors that may be important to users as they consider whether to adopt the innovation. This section can readily be adapted to assess predictors of other implementation outcomes. For example, to assess predictors of sustainability at a later stage, the instructions could ask what factors are important as users consider whether to continue using the innovation.
Fig. 3.
Five and Ten D&I Evaluation Tool
The second half of the instrument contains ten items to assess key innovation characteristics associated with implementation success: simplicity, trialability, observability, relative advantage, compatibility, feasibility, adaptability, cost-effectiveness, effectiveness in making desired changes, and credibility (Chaudoir et al. 2013; Rogers 2003). In our study, this Five and Ten instrument is accompanied by three quantitative items that assess the D&I outcomes of adoption, sustainability, and diffusion. In this specific case, respondents are asked to rate their level of agreement with three items: “I am using the sleep improvement strategies I learned in the sleep intervention;” “In the future, I will continue using the sleep improvement strategies I learned during the sleep intervention;” and “I have spoken with other people about the sleep intervention that I participated in.” Future analysis will include assessing associations between the ten innovation-level predictors and these D&I outcomes of interest. We plan to test the hypothesis that participants who rate the sleep intervention most highly on key innovation characteristics will also have higher levels of adoption, intentions for sustained use, and behaviors supporting diffusion of the program. (Note that assessing effectiveness of the intervention for improving supervisors’ sleep [i.e., a health outcome] is a separate activity from assessing dissemination success [i.e., D&I outcomes] which is what we are using the Five and Ten instrument for.)
The Value of End-User Participation
One common feature of clinical translational research has been the predominant use of source-based models of research, where the EBHI study originates from the world of research and its developer (“the source”), usually an academic investigator, whose end goal is to transfer an EBHI to users, whether s/he is directly involved in that transfer or hands the results off to others for dissemination (Wandersman et al. 2008). Source-based models describe a linear research-to-practice process in which the innovation’s lifespan can be followed from gestation to marketing (i.e., research, development, evaluation, packaging, and dissemination).
In contrast, D&I science has increasingly recognized the value of user-based models, where the EBHI study originates from the practical experience of an individual or an organization (“the user”). The innovation may be created initially by the user, or by a researcher who has learned of the user’s need, perhaps with later refinements based on feedback from users; examples of both types can be found in the occupational ergonomics and safety literature (e.g., Dasgupta et al. 2016; Moir and Buchholz 1996; Moir and Azaroff 2007). User-based models of research depict a linear process in which the evaluation can be traced from the user’s initial awareness of a health problem to the incorporation of the EBHI into the user’s behavioral repertoire (i.e., empirical assessment of the problem and resource capacity, innovation development and selection, adoption, implementation, evaluation, and scale-up) (Wandersman et al. 2008).
User-based models such as participatory action research (PAR) and community-based participatory research (CBPR) are grounded in a participatory approach in which end-user participants are both the objects of study and agents of change (McNiff and Whitehead 2011). Members of the end-user community become active partners in the research process and are equitably involved in the design and conduct of the study, rather than being passive research participants (Israel et al. 1998). Community is defined as a unit of identity that may or may not have a defined geography, but whose members share a connection to one another, have shared norms and values, common language and customs, similar goals and needs, and an interest in the shared well-being of the community (Schulz et al. 1998).
In CBPR, community members contribute as subject matter experts (Agency for Healthcare Research Quality 2003) whose knowledge of the community and its context permits a highly customized study. The researchers in turn are able to develop context-sensitive measures to assess community needs and resources; identify health concerns and their root causes; create acceptable study approaches; select appropriate measures of efficacy; develop strategies to recruit/retain participants and collect data; design socially- and culturally-relevant interventions; and interpret, disseminate and translate findings back to the user community with sensitivity to its norms and climate (Israel et al. 2013).
User-based models have been instrumental in exposing invisible but rigorous systems of control, often leading to the change of systems previously considered unchangeable, and are increasingly viewed as effective method for reducing health disparities (Kidd and Kral 2005; Wallerstein and Duran 2006, 2010). These models are also valuable in preempting problems of generalizability (external validity) that occur when innovations with established efficacy fail to translate into practical use; this is because the innovations are created and tested with the involvement of actual end-users within specific real-world settings. User-based models accelerate translational research because they allow research products to be put immediately and directly into action (Israel et al. 1998). They also ideally result in innovation designs with relevance and appeal to desired end-users; the innovations should therefore have a greater likelihood of diffusion through social systems, reaching larger and wider populations of potential adopters (Rogers 2003). It is for these reasons that CPH-NEW uses a participatory method (HWPP) in its OSH research and has successfully developed and delivered TWH innovations in both the healthcare and public safety sectors.
Conclusion
The sequential discovery-delivery continuum, dominant in clinical translational research, has been criticized for slowing down the r2p pipeline. D&I studies are a key component for bridging the gap between research and practice because they are designed to identify which innovation features will promote successful dissemination to different groups of implementers and end-users in different settings. This is the type of knowledge needed to develop best practices in dissemination.
However, there are barriers to both D&I practice and research that need to be overcome to advance the state of D&I science. A primary obstacle is the need to build capacity through dedicated D&I training programs for academic researchers and graduate students. D&I science training for reviewers, editors, decision-makers, and practitioners would address additional barriers that posed by a lack understanding among these stakeholder groups (Proctor et al. 2015). In addition to new training initiatives, regular national and international meetings (e.g., annual conferences) for D&I researchers and practitioners is essential for the sharing of new knowledge. Other D&I barriers that need to be addressed include a lack of: well-established designs for D&I research (that emphasize external validity), D&I theory regarding consistent causal relationships among specific predictors and outcomes, psychometrically sound measures of D&I constructs, and D&I-specific reporting guidelines (Proctor et al. 2015).
There are many facilitators of D&I research that should be noted, and where possible, taken advantage of. Grants that require dissemination strategies encourage dissemination practice, and competitive D&I grants promote more numerous D&I studies, but also more rigorous D&I research. The wider availability of D&I tools for dissemination practice and evaluation (Agency for Healthcare Research Quality 2014), as well as resources that spotlight existing models and measures (Chaudoir et al. 2013; Proctor et al. 2011) is also very helpful. Additionally, new models of research can speed the translational process, such as those the invite end-user participation to refine and immediately use innovations, or research designs that blend the efficacy and effectiveness phases of research (Glasgow et al. 2003; Wells 1999), as well as the effectiveness and implementation phases (Curran et al. 2012; Nielsen and Abildgaard 2013).
D&I science is still a relatively new field. We propose that it would be useful to develop a D&I research agenda in OSH generally, so as to better define D&I as a meaningful component of workplace intervention research. Specific elements of that research agenda might include developing a taxonomy of facilitators of and obstacles to uptake and adoption, at multiple levels (i.e., organizational, workforce, researcher, etc.); discussion of whether it would be feasible to develop a generic set of metrics for these and for assessment of D&I outcomes at different levels; and criteria for systematic review of D&I studies (similar to those applied now to cohort and intervention studies) in order to facilitate comparison of methodologies and pooling of high-quality findings. With further contributions from other scientists, this agenda could provide a structure for determining what types of D&I research might be most worthwhile in guiding the translation of EBHIs into effective occupational safety and health practice.
The contribution of OSH scientists to a literature of rigorous D&I research will advance the field more generally by enhancing our understanding of implementation predictors and informing the development of better quantitative research measures. This paper aims to offer useful information for those OSH scientists who want to communicate their research findings to the world of workplace practice, in order to reach broader audiences and have greater impact on OSH outcomes. Knowledge about D&I methods and findings can assist us all in being more successful with those communication efforts.
Acknowledgments
This research was supported by the U.S. National Institute for Occupational Safety and Health (NIOSH), Grant Number 1 U19 OH008857. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. The authors express warm appreciation of Dr. Robert Henning for suggesting this article and for his enthusiasm and commitment to D&I in OSH. We also thank Kiley Dugan for her assistance in compiling and formatting our references and proofreading the final version of this manuscript. Finally, we are grateful for the entire CPH-NEW research team of graduate research assistants, research staff and faculty members from the University of Massachusetts Lowell and the University of Connecticut. Their collective efforts have been instrumental in the development, application, and evaluation of the HWPP and more generally in deepening our multi-disciplinary understanding of how to conduct user-centered research of organizational change in the service of worker health and well-being.
References
- Agency for Healthcare Research and Quality. The Role of Community-Based Participatory Research: Creating Partnerships, Improving Health. Agency for Healthcare Research and Quality; Rockville, MD: 2003. [Accessed July 1, 2017]. AHRQ Publication No. 03–0037. Available at https://archive.ahrq.gov/research/cbprrole.htm. [Google Scholar]
- Agency for Healthcare Research and Quality. [Accessed June 30, 2017];Dissemination Planning Tool. 2014 Available at: https://www.ahrq.gov/professionals/quality-patient-safety/patient-safety-resources/resources/advances-in-patient-safety/vol4/planningtool.html.
- Balas EA, Boren SA. Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, editors. Yearbook of medical informatics 2000: Patient-centered systems. Stuttgart, Germany: Schattauer; 2000. pp. 65–70. [PubMed] [Google Scholar]
- Bravata DM, Sanders L, Huang J, Krumholz HM, Olkin I, Gardner CD, Bravata DM. Efficacy and safety of low-carbohydrate diets: A systematic review. Journal of the American Medical Association. 2003;289(14):1837–1850. doi: 10.1001/jama.289.14.1837. [DOI] [PubMed] [Google Scholar]
- Carpenter D, Nieva V, Albaghal T, Sorra J. Advances in patient safety: From research to implementation. Vol. 4. Rockville, MD: Agency for Healthcare Research and Quality; 2005. [Accessed July 1, 2017]. Development of a planning tool to guide dissemination of research results. Programs, tools, and products. AHRQ pub. 05–0021-4. Available at: https://www.ncbi.nlm.nih.gov/books/NBK20603/ [Google Scholar]
- Center for Promotion of Health in the New England Workplace. The Healthy Worksite Participatory Program Online Toolkit. University of Massachusetts Lowell: Center for Promotion of Health in the New England Workplace; 2011. [Accessed July 1, 2017]. Available at: www.uml.edu/cphnewtoolkit. [Google Scholar]
- Chaudoir SR, Dugan AG, Barr CH. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implementation Science. 2013;8:22–42. doi: 10.1186/1748-5908-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CPWR Center for Construction Research and Training. [Accessed July 1, 2017];Dissemination Roadmap. 2014 Available at: http://www.cpwr.com/sites/default/files/Roadmap%20and%20Worksheet%20FINAL.pdf.
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care. 2012;50(3):217. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta PS, Punnett L, Moir S, Kuhn S, Buchholz B. Does drywall installers' innovative idea reduce the ergonomic exposures of ceiling installation: A field case study. Applied Ergonomics. 2016;55:183–193. doi: 10.1016/j.apergo.2016.02.004. [DOI] [PubMed] [Google Scholar]
- Dearing JW, Kreuter MW. Designing for diffusion: How can we increase uptake of cancer communication innovations? Patient Education and Counseling. 2010;81(Supplement):100–110. doi: 10.1016/j.pec.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AL, Buller DB, Dearing JW, Cutter G, Guerra M, Wilcox S, Bettinghaus EP. Adopting an evidence-based lifestyle physical activity program: Dissemination study design and methods. Translational Behavioral Medicine. 2012;2(2):199–208. doi: 10.1007/s13142-011-0063-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health. 2003;93(8):1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez BF, Peskin MF, Shegog R, Gabay EK, Cuccaro PM, Addy RC, et al. iCHAMPSS: Usability and Psychosocial Impact for Increasing Implementation of Sexual Health Education. Health Promotion Practice. 2017;18(3):366–380. doi: 10.1177/1524839916682004. [DOI] [PubMed] [Google Scholar]
- Holmberg MD, Flum M, West C, Zhang Y, Qamili S, Punnett L. Nursing Assistants’ Dilemma: Caregiver versus Caretaker. Hospital Topics. 2013;91(1):1–8. doi: 10.1080/00185868.2013.757953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Eng E, Schulz AJ, Parker EA. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2013. [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19(1):173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Kennedy AB, Schenkelberg M, Moyer C, Pate R, Saunders RP. Process evaluation of a preschool physical activity intervention using web-based delivery. Evaluation and Program Planning. 2017;60:24–36. doi: 10.1016/j.evalprogplan.2016.08.022. [DOI] [PubMed] [Google Scholar]
- Kidd SA, Kral MJ. Practicing participatory action research. Journal of Counseling Psychology. 2005;52(2):187. [Google Scholar]
- McNiff J, Whitehead J. All you need to know about action research. London: Sage Publications; 2011. [Google Scholar]
- Moir S, Azaroff LS. The Boston-area HASWIC Research Circle: An innovative participatory method for coloring in the picture of a special work environment. New Solutions: A Journal of Environmental and Occupational Health Policy. 2007;17(1):123–136. doi: 10.2190/Q364-44T7-P7X8-3652. [DOI] [PubMed] [Google Scholar]
- Moir S, Buchholz B. Emerging participatory approaches to ergonomic interventions in the construction industry. American Journal of Industrial Medicine. 1996;29(4):425–430. doi: 10.1002/(SICI)1097-0274(199604)29:4<425::AID-AJIM31>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Nahm ES, Resnick B, Bellantoni M, Zhu S, Brown C, Brennan PF, et al. Dissemination of a theory-based online bone health program: Two intervention approaches. Health Informatics Journal. 2015;21(2):120–136. doi: 10.1177/1460458213505573. [DOI] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. [Accessed July 1, 2017];Research to Practice. 2015a Retrieved from https://www.cdc.gov/niosh/r2p/about.html.
- National Institute for Occupational Safety and Health. [Accessed June 1, 2017];Total Worker Health.®. 2015b Retrieved from http://www.cdc.gov/niosh/programs/totalworkerhealth/.
- National Institutes of Health. Dissemination and implementation research in health (R01) Program announcement PAR-16-238 (current FOA); 2016. [Accessed July 1, 2017]. Retrieved from https://grants.nih.gov/grants/guide/pafiles/PAR-16-238.html. [Google Scholar]
- Nielsen K, Abildgaard JS. Organizational interventions: A research-based framework for the evaluation of both process and effects. Work and Stress. 2013;27(3):278–297. [Google Scholar]
- Nobrega S, Kernan L, Plaku-Alakbarova B, Robertson M, Warren N, Henning R Research Team, C. P. H.-N. E. W. Field tests of a participatory ergonomics toolkit for Total Worker Health. Applied Ergonomics. 2017;60:366–379. doi: 10.1016/j.apergo.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge ME, Kavathe R, Zanowiak J, Wyatt L, Singh H, Islam N. Implementation and dissemination of the Sikh American Families Oral Health Promotion Program. Translational Behavioral Medicine. 2017:1–9. doi: 10.1007/s13142-017-0466-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E, Carpenter C, Brown CH, Neta G, Glasgow R, Grimshaw J, et al. Advancing the science of dissemination and implementation: three" 6th NIH Meetings" on training, measures, and methods. Implementation Science. 2015;10(1):A13. [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver ND. A glossary for dissemination and implementation research in health. Journal of Public Health Management Practice. 2008;14:117–123. doi: 10.1097/01.PHH.0000311888.06252.bb. [DOI] [PubMed] [Google Scholar]
- Robertson M, Henning R, Warren N, Nobrega S, Dove-Steinkamp M, Tibirica L, Bizarro A Research Team, C. P. H.-N. E. W. The Intervention Design and Analysis Scorecard: A planning tool for participatory design of integrated health and safety interventions in the workplace. Journal of Occupational and Environmental Medicine. 2013;55:S86–S88. doi: 10.1097/JOM.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York: Free Press; 2003. [Google Scholar]
- Schillinger D. An introduction to effectiveness, dissemination and implementation research. From the Series: UCSF Clinical and Translational Science Institute (CTSI) Resource Manuals and Guides to Community-Engaged Research. In: Fleisher P, editor. Clinical Translational Science Institute Community Engagement Program. San Francisco: University of California; 2010. [Google Scholar]
- Schulz AJ, Israel BA, Selig SM, Bayer IS, Griffin CB. Development and implementation of principles for community-based research in public health. In: MacNair RH, editor. Research strategies for community practice. New York: Haworth Press; 1998. pp. 83–110. [Google Scholar]
- Tapp H, McWilliams A, Ludden T, Kuhn L, Taylor Y, Alkhazraji T, et al. Comparing traditional and participatory dissemination of a shared decision making intervention (ADAPT-NC): A cluster randomized trial. Implementation Science. 2014;9(1):158. doi: 10.1186/s13012-014-0158-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N, Duran B. Using community-based participatory research to address health disparities. Health Promotion Practice. 2006;7(3):312–323. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. American Journal of Public Health. 2010;100(S1):S40–S46. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, et al. Bridging the gap between prevention research and practice: The interactive systems framework for dissemination and implementation. American Journal of Community Psychology. 2008;41(3–4):171–181. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- Wells KB. Treatment research at the crossroads: the scientific interface of clinical trials and effectiveness research. American Journal of Psychiatry. 1999;156(1):5–10. doi: 10.1176/ajp.156.1.5. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Flum M, West C, Punnett L. Assessing organizational readiness for a participatory occupational health/health promotion intervention in skilled nursing facilities. Health Promotion Practice. 2015;16(5):724–732. doi: 10.1177/1524839915573945. [DOI] [PMC free article] [PubMed] [Google Scholar]