Abstract
Background
Substance use, psychiatric problems and pain frequently co-occur; yet clinical profiles of treatment-seeking patients are poorly understood. To inform service and treatment planning, substance use and symptom patterns were examined in an outpatient psychiatry clinic, along with the relationship of these patterns to demographic characteristics and physical health.
Methods
Patients (N=405; age M=38; 69% White; 60% female) presenting for intake in a psychiatry outpatient clinic completed a computerized assessment of psychiatric problems, drinking, and drug use. Substance use and psychiatric symptom patterns among the sample were identified using latent class analysis.
Results
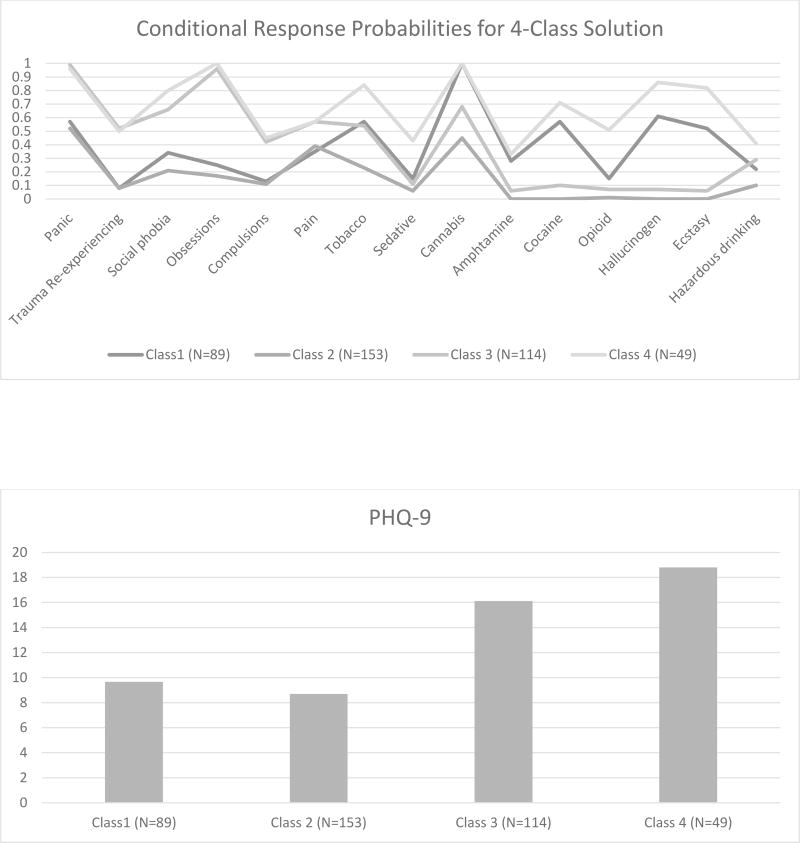
A 4-class model fit the data best: Class 1) Moderate symptoms/Wide range users (22.0%) had moderate depression and panic, tobacco, cocaine, hallucinogen, and ecstasy use; and high cannabis use. Class 2) Moderate depression/panic (37.8%) had moderate depression and panic. Class 3) Depression/Anxiety, tobacco and cannabis users (28.0%) had high depression, obsessions, and panic; and moderate pain severity, social phobia, compulsions, trauma, tobacco, and cannabis use. Class 4) Severe/wide range symptoms/users (12.0%) had high panic, depression, social phobia, obsessions, drug use; and moderate pain. Gender, ethnicity, and health status varied by class.
Conclusions
Findings highlight the preponderance of substance use (particularly cannabis) and its relationship to psychiatric symptom severity, pain and health status among those presenting for mental health treatment.
Keywords: computerized screening, cannabis, tobacco, depression, anxiety, pain, latent class analysis
INTRODUCTION
The comorbidity of substance use and mental health problems is well-established. A review of literature from the National Epidemiologic Survey on Alcohol and Related Conditions identified over 150 papers demonstrating substance use problems among those with diagnosable mental health problems or symptoms (Hasin and Grant 2015). Yet, in contrast to substance use disorders, patterns of alcohol and drug use among psychiatric outpatients have been understudied (Sullivan, Fiellin, and O'Connor 2005). There is, however, also significant potential for subdiagnostic substance use to exacerbate psychiatric problems and contribute to other adverse health effects. Moderate alcohol use may decrease the effectiveness of antidepressant treatment response (Worthington et al. 1996) and increase risk of side effects. Hazardous drinking can impede anxiety and depression symptom recovery (Bahorik et al. 2016), cannabis use can interfere with depression and anxiety treatment (Bricker et al. 2007), and depression and anxiety also complicate the management of prescription opioids for pain, increasing risk of opioid-related overdose (Bohnert et al. 2012). This evidence indicates that substance use is a critical issue for understanding mental health symptoms and problems. Therefore, while not excluding individuals whose substance use problems would meet criteria for a substance use disorder, the current study examined individuals with a range of substance use levels.
Substance use treatment is most successful at early stages, yet many people do not seek treatment until their condition is severe (Babor et al. 2007). Those with potential substance-related problems often first seek mental health treatment (Edlund, Booth, and Han 2012, Weisner and Matzger 2003), and greater substance-related problem severity among patients with depression and other psychiatric problems is associated with motivation to reduce use (Satre et al. 2011). Thus, mental health treatment settings provide an important substance use intervention opportunity.
Measures of pain and health status are also valuable in understanding clinical profiles. It is well established that pain and psychiatric disorders such as depression and anxiety are highly comorbid (Bair et al. 2003, Braden et al. 2009, Edlund et al. 2010), but the additional presence of substance use has been less well studied. This is particularly true for substances other than opioids, although patients often use alcohol or cannabis to address their pain. Relatedly, physical illness is significantly higher among patients with substance use and psychiatric disorders, which presents considerable challenges to successful treatment (Bahorik et al. 2017, Smith et al. 2014). Thus, patients with multiple comorbid conditions, pain and substance use frequently present for services in mental health settings, and it is important to understand potentially common clinical profiles.
Computerized screening tools can be advantageous for identifying patterns of substance use and related problems in health care settings (McNeely et al. 2016). One investigation of computerized self-assessment for substance use screening in a psychiatric outpatient clinic reported high prevalence of cannabis use and heavy episodic drinking among both men and women (Satre et al. 2008), highlighting treatment targets. A follow-up study evaluated the utility of using a computerized health inventory for identifying subdiagnostic substance use for adults with depression (Satre et al. 2011). The current study builds on these studies by examining clinical profiles of patients presenting for psychiatric treatment and identifying symptom and substance use patterns based on computerized screening.
Person-centered approaches such as latent class analysis are advantageous in the study of substance-psychiatric comorbidity in that they account for complex relationships and distinct patterns of heterogeneity (Muthèn and Muthèn 2000). These approaches are best suited for analyzing phenomena in which most individuals in the sample under study do not experience a common underlying process (Nagin 2005). Because some individuals with co-occurring mental health and substance use comorbidity will never present for treatment while others will, potentially with variation in their health and substance use problems, it may be unreasonable to develop classifications based on common dimensions derived using variable-centered models.
A large body of work has employed person-centered approaches to model a range of health-related problems in which the sample under study was expected to vary. This includes: depression symptoms by sex (Rodgers et al. 2014), intimate partner violence victimization in pregnant women (Flanagan et al. 2015), transdiagnostic symptoms in youth (Bonadio et al. 2016), mental health and alcohol use risk in Operation Enduring Freedom/Operation Iraqi Freedom veterans (Cadigan, Klanecky, and Martens 2017), and psychopathology in women with postpartum psychosis (Kamperman et al. 2017). This work has identified several critical risk profiles that have informed targeted patient screening and intervention efforts as well as potential improvements in health management. Thus, person-centered analysis can be useful for profiling variability in complex patient phenomena to inform care. Given the potential for psychiatry patients to present for outpatient treatment with considerable heterogeneity in multiple comorbid conditions and substance use, person-centered approaches could also help explain common patient profiles in this population.
We employed latent class analysis to identify common patterns of substance use, pain and mental health problems among adults presenting for outpatient mental health treatment, and then examined the relationship of the resulting classes to health indicators. We focused on internalizing problems, e.g., symptoms of depression and anxiety, because these are the most common in outpatient treatment-seeking populations (Stahl et al. 2017). It was expected that multiple dominant patterns of substance use and psychiatric symptoms would characterize the sample, and that alcohol and cannabis use would be prevalent. In addition, we expected that tobacco use would be prominent in the classes characterized by polysubstance use and/or severe mental health symptoms, given its relative prevalence among those who use other substances (Guydish et al. 2011) and those with mental health problems (Glasheen et al. 2014, McClave et al. 2010). We expected that pain would be associated with profiles indicative of severe depression, as depression is linked with more pain complaints, greater pain intensity, and longer pain duration (Bair et al. 2003). We also explored the potential for variability among classes by gender and ethnicity and treatment intensity-related correlates of latent classes.
MATERIALS AND METHODS
Participants
Participants included all men and women aged 18 and over seeking outpatient services in the Adult Psychiatry Clinic of the Langley Porter Psychiatric Institute at the University of California, San Francisco (UCSF) Health System who completed computerized intake between July 1, 2014 and June 30, 2015.
Participants were sampled from either the Adult Psychiatry Clinic (APC) or the Partial Hospitalization Program (PHP); two programs of the larger clinic. The APC provides evaluation, psychotherapy and medication management for patients with a range of psychiatric problems. The PHP provides intensive outpatient services where patients typically attend individual and group treatment for 5 hours daily for 10 consecutive weekdays, followed by tapering of services. These clinics lack programming and licensure to treat substance use disorders. Individuals were screened by telephone prior to intake; those seeking substance use disorder treatment were referred to programs elsewhere.
Participant clinical and demographic data was obtained from UCSF medical records, including results of an Electronic Health Inventory (EHI) (Satre et al. 2008, Satre et al. 2011). The EHI (questions are described in the measures section) was completed on computers in the clinic intake area where front desk staff assisted patients if needed. All patients were informed that de-identified medical records may be used for research; however, since the questionnaires were administered as part of intake, patients were not asked for informed consent prior to responding. A total of 405 patients completed the EHI during the study window, accounting for about 48% of patients seeking adult outpatient psychiatric services. We employed χ2 or independent sample t-tests to compare the characteristics of the sample of patients who completed the EHI (N = 405) to those who did not (N = 450) complete the EHI. There were more employed (55.0% vs. 44.9%, p < .001) and younger (M = 26.04; SD = 13.33 vs. M = 45.60; SD = 17.04, p < .001) patients who completed the EHI. There were no other significant differences.
Measures
Latent class indicators
Substance use
Substance use questions in the EHI were selected from the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) version 3.0 (WHO ASSIST Working Group 2002) validated for computerized self-administration (McNeely et al. 2016). Patients were asked if they had ever used: tobacco, alcohol, marijuana, prescription sedative/hypnotic pills in a way that was not prescribed, cocaine, amphetamines, opioids (including heroin or prescription opioids in a way that was not prescribed), hallucinogens (including PCP and Mushrooms), or ecstasy/MDMA. Those responding “yes” were asked to indicate past 3-month use (never, once or twice, monthly, weekly, daily or almost daily; which was converted to use/no-use due to low frequency), problems associated with use (never, once or twice, monthly, weekly, daily or almost daily). Further questions on alcohol use included past hazardous drinking defined as ≥4/≥5 drinks in a day for women/men (National Institute on Alcohol Abuse and Alcoholism 2004, Winter).
Psychiatric symptoms
Current depression severity was measured with the PHQ-9 (Lowe, Unutzer, et al. 2004, Lowe, Kroenke, et al. 2004). Current generalized anxiety disorder symptoms were measured with the GAD-7; (Spitzer et al. 2006). Single-item questions were used to screen for the current presence of symptoms of the following mental health problems: panic, trauma re-experiencing, social phobia, obsessions, and compulsions (all y/n) using items based on the MINI International Neuropsychiatric Interview (Sheehan et al. 2006).
Pain
Participants completed a pain screen, including presence of current physical pain (y/n), level of pain (mild, moderate, or severe), and worst amount of pain in past month (1 to 10). (U.S. Department of Veterans Affairs 2000)
All indicators were coded as dichotomous: present or not.
Correlates of interest
Demographics
Demographic information in the EHI included age, gender (sex assigned at birth; current gender identity), sexuality, ethnicity, education level, relationship status (single, partnered, other) and employment.
Overall health
Participants rated their overall health status using the question, “In general, would you say your health is excellent, very good, good, fair or poor.” This question is predictive of future health care utilization and morbidity (Bierman et al. 1999). The measure was dichotomized (excellent, very good, or good vs. fair or poor) for analyses.
Treatment characteristics
Participant treatment upon admission was categorized as regular (Adult Psychiatry Clinic) or intensive (Partial Hospitalization Program) outpatient.
Analyses
The study team obtained permission from the UCSF Institutional Review Board to examine de-identified data. Descriptive statistics examined prevalence and extent of substance use and psychiatric symptoms. Correlations among substance use, pain and mental health variables evaluated whether variables could be considered independent indicators in a finite mixture model, or should be combined with other variables. Relative infrequency of past 3-month use of any drug, coupled with the episodic nature of substance use over the lifespan, led to a decision to include only lifetime presence of substance use as indicators in the mixture model. Infrequency of ratings of pain severity and worst pain led to only including presence of any current pain (y/n) in the final model. Given high correlations between GAD-7 with PHQ-9 (r=.73) and obsessions (r=.55), GAD-7 was not included in the final mixture model.
A series of finite mixture models, with 1 to 5 classes were estimated using MPlus version 7.4 (Muthén and Muthén 2015) using robust maximum likelihood estimation. We used 100 random starts and optimized 20. We made certain all 20 achieved the same maximum likelihood value. The following criteria were used to judge model fit for each model tested: 1) Lo–Mendel–Rubin likelihood ratio (LMR) test (Lo, Mendell, and Rubin 2001) Bayesian information criterion (BIC),(Raferty 1995); and 3) Akaike’s information criterion (AIC),(Akaike 1973). A statistically significant LMR p-value indicates improvement in fit with the inclusion of one more class. Low BIC and AIC values indicate a better model fit, and as such, the model with the lowest AIC and BIC is generally preferred (Muthèn and Muthèn 2000). The entropy value (0–1) was considered to assess the clarity of the classification of individuals into classes; values closer to 1 are desirable (Muthèn and Muthèn 2000, Ramaswamy et al. 1993) but was not used for model selection as an over-fit model will have an entropy value close to 1.0. Missing data were very minimal and no records were dropped from the analysis due to missing data.
Model results were also used to determine the best-fitting model. For a given model, parameter estimates include (1) class membership or posterior probabilities and (2) class-specific conditional response probabilities (CRPs). Observations can be classified into their most likely latent classes based on the estimated posterior probabilities for the observations. CRPs reflect the probability that an individual within a particular class has the presence of a particular variable (e.g., substance or mental health symptom). For continuous variables, responses are given a mean value for a particular class. Based on the patterns of the estimated conditional probabilities, meaningful labels or definitions of the latent classes can be made.
Finally, we examined correlates of the most likely latent-class membership. One-way ANOVA and Pearson chi-square were used to examine differences in these variables by most likely class membership. As these class comparisons were largely exploratory, we evaluated differences in various characteristics using a standard p<.05 criterion.
RESULTS
Sample characteristics
A total of 405 patients completed the EHI, and their demographic, treatment, and health characteristics are reported on Table 1. Sixty percent of the sample were women and the average age was 37.7 (SD = 13.6). Most patients were White 69.2%, the majority graduated from college (77.8%), and were employed full or part-time (59.3%). Most (70.1%) patients reported lifetime cannabis use, almost half (46%) report tobacco use, and about a quarter of the same used cocaine (23%), hallucinogens (26%) and ecstasy (23%) in their lifetime. Most patients also had moderate depression (PHQ-9: M = 12.2; SD = 7.3) and anxiety (GAD-7: M = 10.0; SD = 6.4) symptoms (Table 1).
Table 1.
Characteristics of adults seeking outpatient mental health services (N=405).
| Characteristic | M(SD)/% | n |
|---|---|---|
| Age - M(SD) | 37.7 (13.6) | |
| Female - % | 60.2 | |
| Sexuality - % | ||
| Heterosexual | 78.8 | |
| Homosexual | 13.4 | |
| Bisexual | 6.1 | |
| Something else or don’t know | 1.8 | |
| Ethnicity -% | ||
| White | 69.2 | |
| African-American | 3.6 | |
| Hispanic/Latino | 10.5 | |
| Asian/Pacific Islander | 10.5 | |
| Other | 6.2 | |
| Education - % | ||
| Did not complete high school | 3.2 | |
| High school diploma or GED | 19.2 | |
| AA or BA degree | 39.3 | |
| Postgraduate degree | 38.5 | |
| Employed - % | 59.3 | |
| Treatment type - % | ||
| Outpatient | 90.9 | |
| Partial hospitalization | 9.1 | |
| Health quality - % | ||
| Poor | 5.2 | |
| Fair | 23.2 | |
| Good | 34.3 | |
| Very good | 28.6 | |
| Excellent | 8.6 | |
| Current Pain - % yes | 45.4 | |
| Substance Use | ||
| Alcohol use | ||
| Lifetime (%) | 91.9 | 372 |
| Past 30 days (%) | 80.2 | 325 |
| Drinking days, past 30 – M(SD) | 7.0 (8.8) | |
| Average drinks per drinking day – M(SD) | 1.7 (1.4) | |
| Hazardous drinking episode, past year (%) | 20.5 | 83 |
| Tobacco use | ||
| Lifetime (%) | 46.4 | 188 |
| Past 30 days (%) | 16.0 | 63 |
| Cigarettes per day among past 30 day smokers – M(SD) | 7.4 (9.7) | |
| Sedative misuse (%) | ||
| Lifetime | 13.6 | 55 |
| Past 90 days | 4.7 | 19 |
| Problems among past 30 day users | 36.8 | 7 |
| Cannabis use (%) | ||
| Lifetime | 70.1 | 284 |
| Past 90 days | 30.1 | 122 |
| Problems among past 30 day users | 8.2 | 10 |
| Amphetamine use | ||
| Lifetime | 11.9 | 48 |
| Past 90 days | 1.5 | 6 |
| Problems among past 30 day users | 0.0 | 0 |
| Cocaine use | ||
| Lifetime | 24.0 | 97 |
| Past 90 days | 4.0 | 16 |
| Problems among past 30 day users | 25.0 | 4 |
| Opiate misuse | ||
| Lifetime | 11.6 | 47 |
| Past 90 days | 1.5 | 6 |
| Problems among past 30 day users | 66.7 | 4 |
| Hallucinogen use | ||
| Lifetime | 25.7 | 104 |
| Past 90 days | 4.2 | 17 |
| Problems among past 90 day users | 5.8 | 1 |
| Ecstasy use | ||
| Lifetime | 23.0 | 93 |
| Past 90 days | 2.0 | 8 |
| Problems among past 90 day users | 25.0 | 2 |
| Mental Health Symptoms | ||
| PHQ-9a – M(SD) | 12.2 (7.3) | |
| GAD-7b – M(SD) | 10.0 (6.4) | |
| Panic – (% yes) | 71.1 | 288 |
| Experienced traumatic event – (% yes) | 46.7 | 189 |
| Re-experienced traumatic event – (% yes) | 25.5 | 101 |
| Social anxiety – (% yes) | 43.2 | 175 |
| Obsessive thoughts – (% yes) | 50.9 | 206 |
| Compulsive behaviors – (% yes) | 23.5 | 95 |
Note. Current pain = endorsed pain within the past 30-days; PHQ-9 = patient health questionnaire; GAD-7 = generalized anxiety disorder scale.
PHQ-9 total score; higher scores indicate greater depression severity.
GAD-7 total score; higher scores indicate greater anxiety severity.
Model Selection
Model fit statistics with one to five classes are presented in Table 2. The BIC, LMR chi-square, and entropy all favored a 4-class solution, while the AIC favored a 5-class solution but only very slightly (8447 vs. 8463). The AIC has been criticized as a test of model fit for its favoring of more complex solutions (Nylund, Asparouhov, and Muthèn 2007). In addition to the favoring by three of the four model fit indicators, conditional response probabilities for the 4-class solution showed overall meaningful interpretation, and thus it was chosen as the most parsimonious, best fitting model.
Table 2.
Fit statistics, p-values and entropy values for models of 1 through 5 classes.
| AIC | BIC | LMR CS | p-value | Entropy | |
|---|---|---|---|---|---|
| 1-Class | 9246.03 | 9314.09 | -- | -- | -- |
| 2-Class | 8764.01 | 8900.14 | 511.02 | 0.0079 | 0.79 |
| 3-Class | 8577.94 | 8782.14 | 217.93 | 0.0002 | 0.81 |
| 4-Class | 8463.12 | 8735.39 | 147.37 | 0.0010 | 0.81 |
| 5-class | 8447.97 | 8788.30 | 48.68 | 0.0869 | 0.80 |
Notes: AIC = Akaike’s information criterion, BIC = Bayesian information criterion, LMR CS = Lo–Mendel–Rubin likelihood ratio chi-square test.
Quality of classification
The cross-classification of the average latent class probabilities for the most likely class by the latent class membership was examined for quality of classification. High diagonal (lowest = 0.87) and low off diagonal probabilities (highest = 0.08) showed strong classification. The entropy value of 0.81 indicates a fairly clear classification.
Latent class probability and class definitions
Figure 1 reports the conditional response probabilities and mean PHQ-9 scores for the 4-class solution. Class 1 was comprised of patients with moderate depression symptoms (PHQ-9: M = 9.8), moderate likelihood of panic symptoms, and moderate likelihood of lifetime tobacco, cocaine, hallucinogen, and ecstasy use, and high likelihood of cannabis use; labeled Moderate symptoms/Wide range users (22.0%). Class 2 was comprised by those with moderate depression (PHQ-9: M = 8.7) and moderate likelihood of panic symptoms and was thus labeled Moderate depression/panic (37.8%). Class 3 consisted of patients with high depression symptoms (PHQ-9: M =16.0), moderate likelihood of social phobia, compulsive, and trauma re-experiencing, pain, tobacco use, and cannabis use, and high likelihood of obsessive and panic symptoms and was labeled Depression/Anxiety, tobacco and cannabis users (28.0%). Class 4 consisted of patients with high depression symptoms (PHQ-9: M = 18.8), high likelihood of panic, social phobia, and obsessive symptoms, and moderate likelihood of pain. Class 4 patients also demonstrated high likelihood of tobacco use, cannabis use, cocaine use, hallucinogen use, ecstasy use, and moderate likelihood of opiate misuse and was thus labeled Severe/wide range symptoms/users (12.0%)
Figure 1.
Conditional Response Probabilities for 4-Class solution and mean PHQ-9 score in each class (N=405).
Characteristics of latent classes
As shown in Table 3, those most likely to be Moderate symptoms/Wide range users (Class 1) had a high likelihood to be non-Hispanic White (X2=26.24; p=.010). Those most likely to be Moderate depression/panic (Class 2) had high likelihood of being female at birth (X2=7.95; p=.047) and by gender identity (X2=22.97; p=.028), as well as being heterosexual (X2=37.66; p<.001), non-Hispanic White, employed (X2=11.87; p=.008), and to have a good health status (X2=23.38; p=.001). Those most likely to be Depression/Anxiety, tobacco and cannabis users (Class 3) had a high likelihood of being female at birth and by gender identity, as well as to be unemployed (X2=11.87; p=.008), and to have a fair/poor health (X2=23.4, p<.001). Finally, Severe/wide range symptoms/users (Class 4) had a high likelihood to be non-Hispanic White, to identify as homosexual, to be unemployed and to have poor/fair overall health.
Table 3.
Observed individual characteristics by latent class (N = 405).
| Class 1a | Class 2b | Class 3c | Class 4d | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Variable | n = 89 | n = 153 | n = 114 | n = 49 | F/X2 | P |
| Age (M) | 37.7 | 36.1 | 38.6 | 41.1 | 1.64 | .180 |
| Sex at birth (% female) | 53.9 | 62.5 | 67.5 | 46.9 | 7.95 | .047 |
| Gender identity (%) | 22.97 | .028 | ||||
| Female | 53.9 | 62.1 | 64.0 | 44.9 | ||
| Male | 44.9 | 37.3 | 31.6 | 53.1 | ||
| Transgender/queer | 1.1 | 0.7 | 2.6 | 2.0 | ||
| Sexual orientation | 37.66 | <.001 | ||||
| Heterosexual | 72.7 | 92.0 | 76.1 | 54.4 | ||
| Homosexual | 17.1 | 5.4 | 15.0 | 28.3 | ||
| Bisexual | 9.1 | 2.0 | 7.1 | 10.9 | ||
| Other/don’t know | 1.1 | 0.7 | 1.8 | 6.5 | ||
| Ethnicity (%) | 26.24 | .010 | ||||
| White | 83.7 | 67.4 | 58.0 | 74.5 | ||
| Asian | 4.7 | 10.4 | 16.1 | 8.5 | ||
| African-American | 3.5 | 2.8 | 4.5 | 4.3 | ||
| Hispanic/Latino | 4.7 | 9.0 | 17.0 | 10.6 | ||
| Other | 3.5 | 10.4 | 4.5 | 2.1 | ||
| Education (%) | 9.82 | .132 | ||||
| <= High school or GED | 16.9 | 22.2 | 23.7 | 28.6 | ||
| AA or BA degree | 47.2 | 32.0 | 43.9 | 36.7 | ||
| Postgraduate degree | 36.0 | 45.8 | 32.5 | 34.7 | ||
| Employed (%) | 65.2 | 66.7 | 48.3 | 51.0 | 11.87 | .008 |
| In a relationship (%) | 38.2 | 36.0 | 37.7 | 34.7 | 4.37 | .627 |
| Health status | 23.38 | .001 | ||||
| Poor/fair | 15.7 | 22.9 | 40.4 | 40.8 | ||
| Excellent/Very good/Good | 84.2 | 77.2 | 59.7 | 59.2 | ||
| Treatment type | 5.98 | .113 | ||||
| Outpatient | 95.1 | 92.2 | 86.0 | 89.8 | ||
| Intensive outpatient | 4.5 | 7.8 | 14.0 | 10.2 | ||
Note. Bold text indicates significant F or chi-square at p < .05 level.
Class 1 = Moderate symptoms/ Wide range users
Class 2 = Moderate depression /panic
Class 3 = Depression/Anxiety, tobacco/ cannabis users
Class 4 = Severe/ wide range symptoms/ users
DISCUSSION
The present study highlights the preponderance of substance use (particularly cannabis) among those presenting for mental health treatment, and the potential utility of using person-centered approaches to understand patterns of substance use and psychiatric symptoms and associated health and pain indicators. Results showed considerable heterogeneity in patterns of substance use and mental health symptoms. Four classes were identified, and three were characterized by at least some substance use. Depression and anxiety symptoms were present in all four classes. Classes differed notably in patterns of comorbidity of mental health symptoms and substance use. While similar patterns that existed between two classes in terms of mental health symptoms, these classes were clearly differentiated by substance use. (e.g., classes 3 and 4 had similarly high prevalence of anxiety disorders and pain; class 3 had very low prevalence of all substance use while class 4 had high prevalence of use). This differentiation validates the importance of considering comorbidity as a fundamental part of the clinical profile of new patients in a clinic treatment setting, and of incorporating health status and pain, which are so clearly tied to mental health and substance use symptom severity. As anticipated, profiles with greater depression severity also reported worse overall health.
Substance use was more common in this population than among other populations, including the general population (Center for Behavioral Health Statistics and Quality 2015) and those in primary care (Mertens et al. 2005). However, the levels of substance use in our results are comparable to those with mental health problems found in primary care (Roeloffs et al. 2002) and emergency room settings (Barry et al. 2006). While these other studies examined patients with depression, our sample may not be directly comparable because patients seeking specialty psychiatric services have sociodemographic and clinical differences compared with patients treated in primary care, including higher income, education, and history of suicidality, and better physical health (Gaynes et al. 2008, Simon et al. 2001, Xakellis 2005). Therefore, this sample is likely to be somewhat different in substance use prevalence and psychiatric severity and demographics from patients with mental health problems treated in primary care.
With regard to the general population, we found that our estimates of lifetime cannabis, cocaine, sedative, hallucinogen, amphetamine, and ecstasy use were all higher than that reported by adults in the National Survey on Drug Use and Health in 2014 (Substance Abuse and Mental Health Services Administration 2015a; SAMHSA). At 46%, lifetime tobacco use was notably lower than that reported by adult aged 26 or older in 2014 throughout the United States (72%) (Substance Abuse and Mental Health Services Administration 2015c). This is likely due to a location effect as tobacco use is lower in California than in other states (Substance Abuse and Mental Health Services Administration 2015b). Given that individuals with psychiatric or substance use disorders are twice as likely to smoke than the general population (Lasser et al. 2000) and are estimated to consume more than half of the cigarettes in the United States (Grant et al. 2004), treating nicotine dependence in psychiatric outpatients should remain a top priority (Prochaska 2011).
Marijuana use was prevalent in this psychiatric sample. This could reflect increasingly liberal views of marijuana compared to other substances within California (Hasin et al. 2017) or also self-medication for psychiatric or health symptoms (Volkow et al. 2014). Those in classes with the highest likelihood of marijuana use were also most likely to endorse current pain and anxiety symptoms, which are some of the most common reasons why people use medical marijuana (Grella, Rodriguez, and Kim 2014). Given the changing landscape about marijuana legalization, psychiatry patients may be more likely to ask their providers about its potential adverse and beneficial effects on health (Volkow et al. 2014). Our results not only indicate that marijuana use should be routinely assessed in outpatient psychiatry settings, but that heavy use should be addressed with evidence-based strategies (Budney et al. 2007), and that any use should be addressed in light of other medical and psychosocial treatment, including pain management.
Substance use, while a common and prevalent problem among many psychiatry patients, is not the same for everyone presenting for mental health treatment. There appears to be remarkable and complex heterogeneity in patients’ substance use and psychiatric symptom presentation, signaling subgroups that may show differences in etiology, maintaining factors, and treatment needs. Substance use should be routinely assessed and addressed in the context of outpatient mental health treatment, because understanding common substance use and psychiatric symptom patterns may be critical to facilitate effective treatment planning. Given the high comorbidity of substance use and mental health symptoms, coupled with worse health and lower likelihood of employment than other groups may make the Severe/wide range symptoms/users (Class 4) in the greatest need of formal comorbidity treatment. Integrated substance use interventions such as motivational interviewing (Satre et al. 2016) and cognitive behavioral therapy (Baker et al. 2014) based in psychiatry could be especially valuable for such patients. Co-occurrence of depression and anxiety symptoms among all four classes suggests treatment for a combination of these disorders may be an ideal strategy.
Limitations should be noted. Not all mental health problems were assessed, although we included those most common among psychiatry outpatients. Externalizing symptoms apart from substance use, e.g., related to conduct disorder, aggression or criminal behavior, were not assessed. Data were based on self-report measures and subject to recall bias and potential under-reporting of substance use. For latent class analysis, substance use was measured as lifetime and dichotomous, which limits our understanding use patterns. We compared classes on individual characteristics of interest rather than incorporating covariates in the latent class models due to sample size, but this strategy did not account for relative probability of membership in all classes. Further, we did not validate the classes against subsequent treatment outcomes. Future research is needed in order to replicate our findings and examine the relationship of these patterns to clinical outcomes. We do not know if cannabis was used recreationally or medically. Patients using recreationally may have different use patterns and use cannabis more frequently with other substances (Lin et al. 2016). Those using cannabis in Moderate depression/panic (Class 2) and Depression/Anxiety, tobacco/cannabis users (Class 3) may be more likely than others to use medically given that they primarily use cannabis rather than other substances.
CONCLUSIONS
Four patterns of mental health symptoms, pain and substance use among patients in outpatient psychiatry were identified. Results largely indicate that patients presenting for outpatient mental health treatment display complex heterogeneity in their substance use and psychiatric symptom patterns, and have an overall high prevalence of marijuana use. Findings suggest that examination of symptom patterns can aid in understanding and addressing substance use in the context of outpatient mental health treatment, a critical step to informing service and treatment planning for this complex population.
Acknowledgments
The authors acknowledge the contributions of the staff and research participants in this study.
FUNDING: National Institute on Drug Abuse (K23DA032578 and T32DA007250) and National Institute on Alcohol Abuse and Alcoholism (R01AA020463).
Footnotes
CONTRIBUTIONS: All authors contributed to the study design. Drs. Ramo and Delucchi conducted the analyses in consultation with Drs Bahorik and Satre. Dr. Ramo and Bahorik completed the first draft of the manuscript, and all authors reviewed and revised subsequent drafts of the manuscript. All authors contributed to and have approved the final manuscript.
References
- Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov BN, Csaki F, editors. Second International Symposium in Information Theory. Akademiai: Kiado, Budapest; 1973. pp. 267–281. [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD. The role of hazardous drinking reductions in predicting depression and anxiety symptom improvement among psychiatry patients: A longitudinal study. J Affect Disord. 2016;206:169–173. doi: 10.1016/j.jad.2016.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, Cannabis, and Opioid Use Disorders, and Disease Burden in an Integrated Health Care System. J Addict Med. 2017;11(1):3–9. doi: 10.1097/ADM.0000000000000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, McElduff P. Randomized controlled trial of MICBT for co-existing alcohol misuse and depression: outcomes to 36-months. J Subst Abuse Treat. 2014;46(3):281–90. doi: 10.1016/j.jsat.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Barry KL, Milner K, Blow FC, Impens A, Welsh D, Amash J. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatr Serv. 2006;57(7):1039–42. doi: 10.1176/ps.2006.57.7.1039. [DOI] [PubMed] [Google Scholar]
- Bierman AS, Bubolz TA, Fisher ES, Wasson JH. How well does a single question about health predict the financial health of Medicare managed care plans? Eff Clin Pract. 1999;2(2):56–62. [PubMed] [Google Scholar]
- Bohnert AS, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169(1):64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- Bonadio FT, Dynes M, Lackey J, Tompsett C, Amrhein K. Grouping Youth With Similar Symptoms: A Person-Centered Approach to Transdiagnostic Subgroups. J Clin Psychol. 2016;72(7):676–88. doi: 10.1002/jclp.22274. [DOI] [PubMed] [Google Scholar]
- Braden JB, Sullivan MD, Ray GT, Saunders K, Merrill J, Silverberg MJ, Rutter CM, Weisner C, Banta-Green C, Campbell C, Von Korff M. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31(6):564–70. doi: 10.1016/j.genhosppsych.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker JB, Russo J, Stein MB, Sherbourne C, Craske M, Schraufnagel TJ, Roy-Byrne P. Does occasional cannabis use impact anxiety and depression treatment outcomes?: Results from a randomized effectiveness trial. Depress Anxiety. 2007;24(6):392–8. doi: 10.1002/da.20248. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Roffman R, Stephens RS, Walker D. Marijuana dependence and its treatment. Addict Sci Clin Pract. 2007;4(1):4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan JM, Klanecky AK, Martens MP. An examination of alcohol risk profiles and co-occurring mental health symptoms among OEF/OIF veterans. Addict Behav. 2017;70:54–60. doi: 10.1016/j.addbeh.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, editor. Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. (HHS Publication No. SMA 15-4927, NSDUH Series H-50). Retrieved from http://www.samhsa.gov/data/ [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs. 2012;73(4):635–46. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Martin BC, Fan MY, Braden JB, Devries A, Sullivan MD. An analysis of heavy utilizers of opioids for chronic noncancer pain in the TROUP study. J Pain Symptom Manage. 2010;40(2):279–89. doi: 10.1016/j.jpainsymman.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan JC, Gordon KC, Moore TM, Stuart GL. Women's Stress, Depression, and Relationship Adjustment Profiles as They Relate to Intimate Partner Violence and Mental Health During Pregnancy and Postpartum. Psychol Violence. 2015;5(1):66–73. doi: 10.1037/a0036895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynes BN, Rush AJ, Trivedi MH, Wisniewski SR, Balasubramani GK, McGrath PJ, Thase ME, Klinkman M, Nierenberg AA, Yates WR, Fava M. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23(5):551–60. doi: 10.1007/s11606-008-0522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasheen C, Hedden SL, Forman-Hoffman VL, Colpe LJ. Cigarette smoking behaviors among adults with serious mental illness in a nationally representative sample. Ann Epidemiol. 2014;24(10):776–80. doi: 10.1016/j.annepidem.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(11):1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grella CE, Rodriguez L, Kim T. Patterns of medical marijuana use among individuals sampled from medical marijuana dispensaries in los angeles. J Psychoactive Drugs. 2014;46(4):267–75. doi: 10.1080/02791072.2014.944960. [DOI] [PubMed] [Google Scholar]
- Guydish J, Passalacqua E, Tajima B, Chan M, Chun J, Bostrom A. Smoking prevalence in addiction treatment: a review. Nicotine Tob Res. 2011;13(6):401–11. doi: 10.1093/ntr/ntr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1609–40. doi: 10.1007/s00127-015-1088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerda M, Keyes KM, Stohl M, Galea S, Wall MM. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry. 2017 doi: 10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamperman AM, Veldman-Hoek MJ, Wesseloo R, Robertson Blackmore E, Bergink V. Phenotypical characteristics of postpartum psychosis: A clinical cohort study. Bipolar Disord. 2017 doi: 10.1111/bdi.12523. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284(20):2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Lin LA, Ilgen MA, Jannausch M, Bohnert KM. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict Behav. 2016;61:99–103. doi: 10.1016/j.addbeh.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) J Affect Disord. 2004;81(1):61–6. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42(12):1194–201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- McClave AK, McKnight-Eily LR, Davis SP, Dube SR. Smoking characteristics of adults with selected lifetime mental illnesses: results from the 2007 National Health Interview Survey. Am J Public Health. 2010;100(12):2464–72. doi: 10.2105/AJPH.2009.188136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Rotrosen J, Ramautar A, Gourevitch MN. Validation of an audio computer-assisted self-interview (ACASI) version of the alcohol, smoking and substance involvement screening test (ASSIST) in primary care patients. Addiction. 2016;111(2):233–44. doi: 10.1111/add.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens JR, Weisner C, Ray GT, Fireman B, Walsh K. Hazardous drinkers and drug users in HMO primary care: prevalence, medical conditions, and costs. Alcohol Clin Exp Res. 2005;29(6):989–98. doi: 10.1097/01.alc.0000167958.68586.3d. [DOI] [PubMed] [Google Scholar]
- MPlus Version 7.4. Muthén & Muthén; Los Angeles, CA: [Google Scholar]
- Muthèn BO, Muthèn LK. Integrating person-centered and variable-centered analysis: Growth mixture modeling with latent trajectory classes. Alcoholism, Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Nagin DS. Group-based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. [accessed May 20];NIAAA council approves definition of binge drinking. 2004 Winter; http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.htm.
- Nylund KL, Asparouhov T, Muthèn BO. Deciding on the number of latent classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. [Google Scholar]
- Prochaska JJ. Smoking and mental illness--breaking the link. N Engl J Med. 2011;365(3):196–8. doi: 10.1056/NEJMp1105248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raferty A. Bayesian model selection in social research (with discussion) In: Marsden P, editor. Sociological Metholdology. Cambridge, MA: Blackwells; 1995. pp. 111–196. [Google Scholar]
- Ramaswamy V, DeSarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science. 1993;12(1):103–124. [Google Scholar]
- Rodgers S, Grosse Holtforth M, Muller M, Hengartner MP, Rossler W, Ajdacic-Gross V. Symptom-based subtypes of depression and their psychosocial correlates: a person-centered approach focusing on the influence of sex. J Affect Disord. 2014;156:92–103. doi: 10.1016/j.jad.2013.11.021. [DOI] [PubMed] [Google Scholar]
- Roeloffs CA, Wells KB, Ziedonis D, Tang L, Unutzer J. Problem substance use among depressed patients in managed primary care. Psychosomatics. 2002;43(5):405–12. doi: 10.1176/appi.psy.43.5.405. [DOI] [PubMed] [Google Scholar]
- Satre DD, Chi FW, Eisendrath S, Weisner C. Subdiagnostic alcohol use by depressed men and women seeking outpatient psychiatric services: consumption patterns and motivation to reduce drinking. Alcohol Clin Exp Res. 2011;35(4):695–702. doi: 10.1111/j.1530-0277.2010.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Leibowitz A, Sterling SA, Lu Y, Travis A, Weisner C. A randomized clinical trial of Motivational Interviewing to reduce alcohol and drug use among patients with depression. J Consult Clin Psychol. 2016;84(7):571–9. doi: 10.1037/ccp0000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre D, Wolfe W, Eisendrath S, Weisner C. Computerized screening for alcohol and drug use among adults seeking outpatient psychiatric services. Psychiatr Serv. 2008;59(4):441–4. doi: 10.1176/ps.2008.59.4.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Janavs J, Baker R, Harnett-Sheehan K, Knapp E, Sheehan M. MINI International Neuropsychiatric Interview - English Version 5.0.0 DSM-IV 2006 [Google Scholar]
- Simon GE, Von Korff M, Rutter CM, Peterson DA. Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry. 2001;58(4):395–401. doi: 10.1001/archpsyc.58.4.395. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Court H, McLean G, Martin D, Langan Martin J, Guthrie B, Gunn J, Mercer SW. Depression and multimorbidity: a cross-sectional study of 1,751,841 patients in primary care. J Clin Psychiatry. 2014;75(11):1202–8. doi: 10.4088/JCP.14m09147. quiz 1208. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stahl ST, Reynolds CF, 3rd, Whyte EM, Albert SM. Psychiatric Diagnoses Among Older Recipients of Publicly Funded Mental Health Services. J Am Geriatr Soc. 2017;65(7):1569–1572. doi: 10.1111/jgs.14865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services, editor. Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: Detailed Tables. Rockville. MD: Substance Abuse Mental Health Services Administration; 2015a. [Google Scholar]
- Department of Health and Human Services, editor. Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: State Estimates - California. Rockville. MD: Substance Abuse Mental Health Services Administration; 2015b. [Google Scholar]
- Department of Health and Human Services, editor. Substance Abuse and Mental Health Services Administration. Table 2.20B – Tobacco Product Use in Lifetime, Past Year, and Past Month among Persons Aged 26 or Older, by Demographic Characteristics: Percentages, 2013 and 2014. Rockville. MD: Substance Abuse Mental Health Services Administration; 2015c. [Google Scholar]
- Sullivan LE, Fiellin DA, O'Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118(4):330–41. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. Pain as the 5th Vital Sign Toolkit, Revised Edition 2000 [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–27. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Matzger H. Missed opportunities in screening for alcohol problems in medical and mental health services. Alcoholism: Clinical and Experimental Research. 2003;27(7):1132–1141. doi: 10.1097/01.ALC.0000075546.38349.6. [DOI] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, Rosenbaum JF. Consumption of alcohol, nicotine, and caffeine among depressed outpatients - Relationship with response to treatment. Psychosomatics. 1996;37(6):518–522. doi: 10.1016/S0033-3182(96)71515-3. [DOI] [PubMed] [Google Scholar]
- Xakellis GC. Are patients who use a generalist physician healthier than those who seek specialty care directly? Fam Med. 2005;37(10):719–26. [PubMed] [Google Scholar]