Abstract
Inflammation is one of the main causes of pathologic pain. Knowledge of the molecular links between inflammatory signals and pain-mediating neuronal signals is essential for understanding the mechanisms behind pain exacerbation. Some inflammatory mediators directly modulate the excitability of pain-mediating neurons by contacting the receptor molecules expressed in those neurons. For decades, many discoveries have accumulated regarding intraneuronal signals from receptor activation through electrical depolarization for bradykinin, a major inflammatory mediator that is able to both excite and sensitize pain-mediating nociceptor neurons. Here, we focus on the final effectors of depolarization, the neuronal ion channels, whose functionalities are specifically affected by bradykinin stimulation. Particular G-protein coupled signaling cascades specialized for each specific depolarizer ion channels are summarized. Some of these ion channels not only serve as downstream effectors but also play critical roles in relaying specific pain modalities such as thermal or mechanical pain. Accordingly, specific pain phenotypes altered by bradykinin stimulation are also discussed. Some members of the effector ion channels are both activated and sensitized by bradykinin-induced neuronal signaling, while others only sensitized or inhibited, which are also introduced. The present overview of the effect of bradykinin on nociceptor neuronal excitability at the molecular level may contribute to better understanding of an important aspect of inflammatory pain and help future design of further research on the components involved and pain modulating strategies.
Keywords: Bradykinin, Pain, Nociceptor neuron, Ion channel, Depolarization
INTRODUCTION
Inflammation is frequently accompanied by pain, where several inflammatory pain mediators generated from inflamed tissues have been known to contribute to this pain induction, e.g., bradykinin, nerve growth factors, prostaglandins, and a group of cytokines (Patapoutian et al., 2009). These mediators stimulate the primary nociceptor neurons innervating inflamed locations. The resultant firing of electrical signals is then transmitted to the brain, leading to the perception of pain. Acquiring information on the nature of the stimulatory mechanisms may help to improve therapeutic pain control strategies, and the relevant approaches at cellular and molecular levels have been conducted for many years. Rarely found regarding the properties for other mediators, bradykinin is able to induce action potential firing of the nociceptors as well as to sensitize those to other stimulations. The mechanisms seem to involve various ion channels that function as the final effectors of excitatory outcomes. Although important frames for the molecular signaling that support the mechanisms were built in late 20th century, the molecular identities and detailed properties of most of the ionotropic players were reported during the 21st century.
As early as the 1950s, the hypothesis that bradykinin mediates pain via nociceptor excitation started to be confirmed in various experimental settings with in vitro and in vivo animal models, as well as human subjects. Administration of bradykinin to human skin and muscle clearly elicited pain perception (Armstrong et al., 1957; Whalley et al., 1987; Manning et al., 1991; Kindgen-Milles et al., 1994; Babenko et al., 1999). Injections to the skin, vascular areas, and the peritoneal cavity caused nocifensive reflexes in model animals including mice, rats, cats, rabbits, dogs, and monkeys (Kumazawa and Mizumura, 1976; Steranka et al., 1988; Walter et al., 1989; Khan et al., 1992; Hong and Abbott, 1994; Griesbacher et al., 1998; Katanosaka et al., 2008). Fiber recordings revealed that the nociceptor depolarization initiated those painful outcomes (Juan and Lembeck, 1974; Chahl and Iggo, 1977; Dray et al., 1992; Soukhova-O’Hare et al., 2006), in which models utilizing testis-spermatic nerve and skin-saphenous nerve preparations have greatly contributed to the provision of fundamental information on bradykinin-controlling sensory modalities and phases, nociceptor categorizing, and signaling participants (Beck and Handwerker, 1974; Kumazawa and Mizumura, 1976). As a result, it is now firmly known that the polymodal nociceptors comprising the unmyelinated C and thinly myelinated Aδ neurons are responsible for bradykinin-induced pain, that the B2 receptor is more constitutively responsible for bradykinin detection than the B1 receptor, and that both discharging of action potentials and lowering of its threshold can be caused by bradykinin action (Mizumura et al., 2009).
Following this, the molecular evidence has kept being corroborated regarding bradykinin receptor-mediated signals, using extended technologies such as culture platforms, molecular biology, genetics, and the patch clamp. Bradykinin acts on the B1 and B2 receptors that are among the metabotropic G protein-coupled receptors (GPCRs) expressed at the surface membrane (Burgess et al., 1989; McGuirk et al., 1989; Mcgehee and Oxford, 1991; Dray et al., 1992; McGuirk and Dolphin, 1992). The majority of the downstream information was obtained from B2 studies, but as for many molecular processes, both receptors have been shown to share similar mechanisms of action (Petho and Reeh, 2012). Commonly, Gq/11-mediated phospholipase C (PLC) and Gi/o-mediated phospholipase A2 (PLA2) activation lead to diverse cellular effects. In nociceptor neurons, several depolarizing effectors are activated or positively regulated (sensitized) through such signaling, which are critical steps necessary for action potential firing or threshold lowering. Here we summarize the identities of the depolarizing molecules and bradykinin-related mechanisms for activation and sensitization.
TRANSIENT RECEPTOR POTENTIAL VANILLOID SUBTYPE 1 ION CHANNEL
Transient Receptor Potential Vanilloid subtype 1 ion channel (TRPV1) functions as a receptor and a cation channel in nociceptor sensory neurons. Sensitive to noxious temperature ranges (>43°C), protons (pH <5.5), and pungent chemicals (e.g., capsaicin), TRPV1 responds by opening its pore. Cation influx through TRPV1 depolarizes the nociceptor membrane, discharging action potentials when the membrane voltage reaches its firing threshold. Other mechanisms for activation and activity modulation have been revealed, and bradykinin has been shown to be tightly linked.
Bradykinin-induced activation of TRPV1 via arachidonic acid metabolism
TRPV1-mediated action potential spike generation upon bradykinin exposure has successfully been repeated in the primary sensory afferents from various sources, including cutaneous nociceptors, cardiac afferents, jejunal afferents, and tracheobronchial afferents (Fig. 1) (Carr et al., 2003; Pan and Chen, 2004; Rong et al., 2004; Lee et al., 2005a). Research efforts have been put into seeking the link between bradykinin-initiated G protein signaling and depolarizing effector functions. Increased production of arachidonic acid by bradykinin and its further metabolism has been considered an important candidate for the signaling (Thayer et al., 1988; Burgess et al., 1989; Gammon et al., 1989). Not only in neurons but also in other tissues, Gi/o mediated arachidonic acid liberation through bilayer digestion of PLA2 activated by bradykinin has been proposed to be involved (Burch and Axelrod, 1987; Gammon et al., 1989; Yanaga et al., 1991). The resultant excitation and sensitization of the nociceptor has also been demonstrated (Taiwo et al., 1990; Ferreira et al., 2004). The role of members of the lipoxygenase (LOX) in furthering arachidonic acid metabolism has been raised for the immediate depolarization caused by bradykinin (McGuirk and Dolphin, 1992; Shin et al., 2002; Carr et al., 2003; Wu and Pan, 2007). Formation of 12-LOX products like 12(S)-hydroxyeicosatetraenoic acid (12(S)-HETE) was also confirmed in nociceptor neurons and skin (Wang et al., 1999; Shin et al., 2002; Tang et al., 2005).
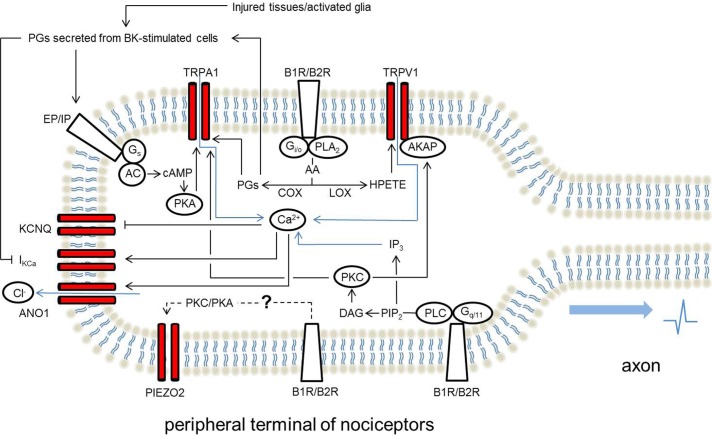
Fig. 1.
Summary of the roles of important effector ion channels which account for bradykinin-induced excitation of pain-mediating nociceptors. AA, arachidonic acid; AC, adenylate cyclase; AKAP, A kinase anchoring protein; ANO1, anoctamin 1; B1R, bradykinin receptor B1; B2R, bradykinin receptor B2; BK, bradykinin; cAMP, 3′,5′-cyclic adenosine monophosphate; COX, cyclooxygenase; DAG, diacylglycerol; EP/IP, prostaglandin E2 receptor and prostaglandin I2 receptor; HPETE, hydroperoxyeicosatetraenoic acid; IKCa, Ca2+-activated K+ channels; IP3, inositol 1,4,5-trisphosphate; KCNQ, voltage-gated K+ channel subfamily KCNQ; LOX, lipoxygenase; PG, prostaglandin; PIP2, phosphatidylinositol 4,5-bisphosphate; PKA, protein kinase A; PKC, protein kinase C; PLA2, phospholipase A2; TRPA1, transient receptor potential ankyrin subtype 1; TRPV1, transient receptor potential vanilloid subtype 1.
Production of arachidonic acid can result from PLC metabolism, as well as from PLA2-mediated one. Diacylglycerol (DAG) produced via PLC action may further be converted into arachidonic acid by DAG lipase and monoacylglycerol lipase (Gammon et al., 1989; Allen et al., 1992; Dray et al., 1992). Attenuation of locally injected bradykinin-elicited acute nocifensive behaviors that reflect immediate sensory action potential discharge is achieved via PLC inhibitors, as well as PLA2 and 5-LOX inhibitors (Ferreira et al., 2004).
LOX metabolites have been shown to activate TRPV1 (Hwang et al., 2000). A number of HETEs, hydroperoxyeicosatetraenoic acids (HPETEs), and leukotrienes displayed this activity, where 12(S)-HPETE has the greatest potency. A later study from the same group reported the B2 receptor-PLA2LOX axis for the signaling cascade for TRPV1 activation (Shin et al., 2002). The same signaling paradigm was successfully repeated by a pharmacological approach for visceral afferents by using multiple TRPV1 blockers and LOX inhibitors (Carr et al., 2003). LOX product pools that have TRPV1 activating potential and the neuronal outcomes other than nociception for example memory, are both being currently extended (Gibson et al., 2008; Gregus et al., 2012). Although the binding pocket for LOX-produced ligands or TRPV1 is less conclusively determined, their structural similarity with capsaicin as predicted by 3-dimensional simulation suggests that the capsaicin binding site, the S4–S5 intracellular linker region of TRPV1 protein is a strong candidate (Ikeda et al., 2001b; Gao et al., 2016).
Bradykinin-induced activation of TRPV1 via protein kinase C
Gq/11-activated PLC metabolizes the membrane bilayer phosphatidylinositol 4,5-bisphosphate (PIP2) into DAG and inositol 1,4,5-trisphosphate (IP3). The increased level of these two products upon bradykinin stimulation has been reported in nociceptor dorsal root ganglionic (DRG) neurons, indicating the activation of Gq/11-PLC axis by bradykinin (Thayer et al., 1988; Burgess et al., 1989; Gammon et al., 1989; Kano et al., 1994; Tang et al., 2004). Both of the two messengers contribute to protein kinase C (PKC) activation.
Evidence has been accumulating that PKC activation upon bradykinin exposure leads to an immediate excitation in studies with various platforms using ectopically receptor expressing cells (Crandall et al., 2002), cultured sensory neurons (Rang and Ritchie, 1988; Burgess et al., 1989; Mcgehee and Oxford, 1991; McGuirk and Dolphin, 1992), afferent nerve fibers (Mizumura et al., 1997; Guo et al., 1998, 1999), spinal cord-tail preparations (Dray et al., 1988, 1992), or animals with nocifensive behaviors (Ferreira et al., 2004). Suppression of excitatory responses by pharmacological inhibition of PKC and mimicking of depolarization when exposed to PKC-activating phorbol esters support the finding. The excitatory effect appears to be caused by the increased permeability of the neuronal membrane to both Na+ and K+ ions, indicating that nonselective cation channels are probably a final effector for this bradykinin-induced PKC action (Rang and Ritchie, 1988; Burgess et al., 1989; Mcgehee and Oxford, 1991). Further research revealed that TRPV1 participates as the ion-permeating effector and suggested that bradykinin leads to TRPV1 activation by PKC phosphorylation and that PKCε plays a crucial role (Premkumar and Ahern, 2000; Vellani et al., 2004). When strongly depolarized, sensory afferents secrete peptidergic transmitters, specifically Substance P and calcitonin gene-related peptide, which is augmented by PKC activation and reduced by PKC downregulation (Barber and Vasko, 1996). Two serine residues located in the intracellular S2–S3 linker and N-terminal end of TRPV1 protein were identified as PKCε phosphorylation targets (Numazaki et al., 2002; Bhave et al., 2003; Choi et al., 2014). Although neuronal excitation by PKC has readily been repeated, ectopic expression systems have often shown less effective induction of the inward current but relatively prominent sensitization of the TRPV1 response to other stimulation, which remains to be quantitatively dissected.
Bradykinin-induced sensitization of TRPV1 activity
In comparison with an acute excitatory action, constantly sensitized nociception caused by a mediator may more broadly explain pathologic pain mechanisms. Since TRPV1 is the major heat sensing molecule, heat hyperalgesia induced by bradykinin, which has long been studied in pain research, may putatively involve changes in TRPV1 activity. Therefore, here we provide an overview of the role of bradykinin in pathology-induced heat hyperalgesia and then discuss the evidence supporting the possible participation of TRPV1 in this type of bradykinin-exacerbated thermal pain. Different from acute nociception where data were produced mostly in B2 receptor setting, the focus may include both B1 and B2-mediated mechanisms underlying pathology-induced chronic nociception, since roles for inducible B1 may emerge in certain disease states. A number of specific pathologies may even show pronounced dependence on B1 function. Nonetheless, both receptors likely share the intracellular signaling mechanisms for effector sensitization.
B1 receptor-dependent pathologic pain: Since the 1980s, B2 receptor involvement has been extensively demonstrated in relatively short-term inflammation models primed with an adjuvant carrageenan or other mediator treatments (Costello and Hargreaves, 1989; Ferreira et al., 1993b; Ikeda et al., 2001a). On the other hand, B1 receptor seems to be more tightly involved in heat hyperalgesia in relatively chronic inflammatory pain models such as the complete Freund’s adjuvant (CFA)-induced inflammation model. While B2 knockout mice failed to show any difference in comparison with wild types, either B1 knockouts or B1 antagonism leads to reduced heat hyperalgesia (Rupniak et al., 1997; Ferreira et al., 2001; Porreca et al., 2006). Because of the ignorable difference in CFA-induced edema between wild types and B1 knockouts, B1 is thought to be involved in heightened neuronal excitability rather than inflammation itself (Ferreira et al., 2001). In diabetic neuropathy models, B1 knockouts are resistant to development of the heat hyperalgesia, and treatment with a B1 antagonist was effective in preventing heat hyperalgesia in naïve animals (Gabra and Sirois, 2002, 2003a, 2003b; Gabra et al., 2005a, 2005b). In a brachial plexus avulsion model, B1 knockouts but not B2 knockouts have shown prolonged resistance to heat hyperalgesia (Quintão et al., 2008). Pharmacological studies on ultraviolet (UV) irradiation models have also shown B1 dominance (Perkins and Kelly, 1993; Perkins et al., 1993; Gougat et al., 2004). Both the peptidergic antagonist des-Arg9,Leu8-bradykinin and a synthetic B1 antagonist SSR240612 commonly prevented UV-induced heat hyperalgesia, whereas the effect of HOE 140, a B2 antagonist, was largely limited. The hyperalgesia was further aggravated by a relatively selective B1 agonist des-Arg9-bradykinin and reversed only by the B1 antagonist.
B1 & B2 receptor-dependent pathologic pain: In neuropathic pain models, both B1 and B2 receptor-mediated mechanisms are generally important (Levy and Zochodne, 2000; Yamaguchi-Sase et al., 2003; Ferreira et al., 2005; Petcu et al., 2008; Luiz et al., 2010). In the models of chronic constriction injury, infraorbital nerve constriction injury, and partial sciatic nerve ligation, selective pharmacological antagonism of either of the receptor types was effective against the putatively TRPV1-mediated heat hyperalgesia, as well as cold hyperalgesia and mechanical allodynia. Heat hyperalgesia occurring in a rat plantar incision model was once shown to be unrelated to bradykinin-mediated mechanisms (Leonard et al., 2004). Later, a contradictory result that the heat hyperalgesia was partially reversed by treatment with either B1 or B2 receptor antagonist was obtained in a different laboratory (Füredi et al., 2010). In the same model, treatment with an LOX inhibitor or a TRPV1 antagonist was also effective. Interestingly, in the same study, heat injury-evoked heat hyperalgesia was attenuated only by B2 antagonist treatment.
Bradykinin-induced heat hypersensitivity: Injection of bradykinin itself has also been shown to augment heat pain sensitivity in humans, monkeys, and rats (Manning et al., 1991; Khan et al., 1992; Schuligoi et al., 1994; Griesbacher et al., 1998). It is commonly likely that the heat sensitivity was left-shifted with lowered heat threshold by bradykinin injection. There are several different points when speculating possible mechanisms that could explain direct excitation and sensitization. Direct nociception in response to bradykinin generally undergoes strong tachyphylaxis, but such sensitization appears to be relatively persistent in time scale. In-depth analyses at the cellular or molecular levels that are mentioned below have shown that the sensitizing effect sometimes occurs in the absence of direct excitation (Beck and Handwerker, 1974; Kumazawa et al., 1991; Khan et al., 1992). Nonetheless, nociceptors that more readily fire upon bradykinin exposure appeared to tend to be more sensitized in heat responsiveness (Kumazawa et al., 1991; Liang et al., 2001). Common PKC-centered machinery is hypothesized to be responsible for both excitation and sensitization, which still requires further careful dissection to understand how those differentiated outcomes are realized.
The sensitizing action of bradykinin on nociceptors: After feline nociceptors were once demonstrated to be sensitized by acute bradykinin exposure of their termini in terms of heat-evoked spike discharges in an in vivo model, many similar in vitro or ex vivo results were produced, again for example, in rodent skin-saphenous nerve and canine testis-spermatic nerve models (Beck and Handwerker, 1974; Lang et al., 1990; Kumazawa et al., 1991). As shown in the in vivo experiments mentioned above, the potency and efficacy of heat-induced electrical responses were increased by bradykinin stimulation of the relevant receptive fields, which was mainly observed in unmyelinated C- or thinly myelinated Aδ nociceptors with polymodality (Kumazawa et al., 1991; Koltzenburg et al., 1992; Haake et al., 1996; Liang et al., 2001). Such facilitation occurred at lower doses than needed for bradykinin-evoked excitation, and moreover, subpopulations of nociceptors that were without bradykinin- or heat-evoked excitation in a naïve stage became sensitive to heat by bradykinin exposure (Kumazawa et al., 1991; Liang et al., 2001). The observed population enlargement is unlikely to be due to an elevated expression of TRPV1 at the surface membrane as this failed to be demonstrated in a more recent study (Camprubi-Robles et al., 2009). Although the experiment did not manipulate heat, research revealed that the capsaicin responses in trachea-innervating vagal C-fibers was sensitized by bradykinin, underlying cough exacerbation upon bradykinin accumulation as an adverse effect of treatment with angiotensin converting enzyme inhibitors for hypertension (Fox et al., 1996). B2 receptor participation was confirmed in the models above.
TRPV1 as a principal actuator for bradykinin-induced heat sensitization: As mentioned above, PKC activation is involved in TRPV1 activation and sensitization. Electrophysiological recordings of canine testis-spermatic nerve preparations raised a role for PKC in the bradykinin-induced sensitization of the heat responses (Mizumura et al., 1997). PKCε phosphorylation initiated by bradykinin was proposed to sensitize the native heat-activated cation channels of cultured nociceptor neurons (Cesare and McNaughton, 1996; Cesare et al., 1999). This was successfully repeated in TRPV1 experiments after its genetic identification and the temperature threshold for TRPV1 activation was lowered by PKC phosphorylation (Vellani et al., 2001; Sugiura et al., 2002). Not only to heat but also to other activators such as protons and capsaicin, TRPV1 responses were sensitized by PKC phosphorylation in several different experimental models (Stucky et al., 1998; Crandall et al., 2002; Lee et al., 2005b; Camprubi-Robles et al., 2009). However, it remains to be elucidated if inducible B1 receptor may utilize the same pathway.
Molecular mechanisms for TRPV1 sensitization by PKC phosphorylation: TRPV1 protein contains a number of target amino acid residues for phosphorylation by various protein kinases. The phosphorylation of these residues largely contributes to the facilitation of TRPV1 activity but it is likely that bradykinin mainly utilizes PKC for its TRPV1 sensitization according to an in vitro analysis of phosphorylated proteins (Lee et al., 2005b). PKC has been shown to directly phosphorylate two TRPV1 serine residues that are located in the first intracellular linker region between the S2 and S3 transmembrane domains, and in the C-terminal (Numazaki et al., 2002; Bhave et al., 2003; Wang et al., 2015). Mutant TRPV1 that was missing these target sequences were tolerant in terms of sensitization upon bradykinin treatment. Interestingly, an adaptor protein seems to be critical to access to the target residues by PKC. Members of A kinase anchoring proteins (AKAPs) are able to modulate intracellular signaling by recruiting diverse kinase and phosphatase enzymes (Fischer and McNaughton, 2014). The activity of some of ion channels is known to be controlled by this modulation when these proteins form a complex, the best known example being the interaction of TRPV1 with AKAP79/150 (AKAP79 indicates the human homolog of the rodent AKAP150) (Zhang et al., 2008). Specifically, AKAP79/150 bound to the C-terminal of TRPV1 protein has been shown to greatly facilitate PKC action by physically recruiting it upon bradykinin stimulation.
Other proposed mechanisms for bradykinin-induced TRPV1 sensitization: As mentioned above, pharmacological inhibition or genetic downregulation studies have demonstrated that PKC may be a predominant factor required for bradykinin-induced TRPV1 sensitization. In addition, different molecular mechanisms also appear to contribute to this sensitization under bradykinin-mediated pathway. PLC is an upstream enzyme of PKC, which consumes bilayer PIP2 to produce IP3 and DAG. PIP2 seems to bind to TRPV1 protein in its resting state, tonically inhibiting TRPV1 activity. In response to bradykinin stimulation however, PIP2 is consumed by Gq-mediated PLC, thereby disinhibiting TRPV1. Responses to capsaicin and protons have been shown to be augmented by this mechanism, although sensitization to heat by bradykinin remains to be explored (Chuang et al., 2001; Prescott and Julius, 2003). As arachidonic acid metabolizing enzymes, LOXs generate a number of endogenous TRPV1 activators. Interestingly, 12-LOX inhibition was also effective at erasing bradykinin-induced heat sensitization of TRPV1 (Shin et al., 2002). 12(S)-HPETE or 12(S)-HETE, its metabolites may therefore not only activate TRPV1, but also facilitate the heat response, which remains to be experimentally confirmed.
Complicated results were obtained from research exploring the role of a different group of arachidonic acid metabolizing enzymes, cyclooxygenases (COXs), as mentioned in the Unsolved problems section. COX activation undoubtedly contributes as a downstream from bradykinin signaling to nociceptor sensitization and excitation but it remains under debate where among nociceptors and surrounding cells COXs plays the predominant role. Whatever the major source of prostaglandins is, the activation of neuronal G-protein-coupled receptors, including EP1, EP4, and IP, by secreted prostaglandins causes activation of not only PKC, but also protein kinase A (PKA) that also phosphorylates and sensitizes TRPV1 (Moriyama et al., 2005).
Unsolved problems
While the major heat sensor TRPV1 has been massively studied regarding bradykinin-induced nociception, the contribution of thermosensitive cousins of TRPV1 in the same superfamily, including TRPV2 and TRPV3, have largely been unexplored. Interestingly, another polymodal TRPV member, TRPV4, which is sensitive to warm temperatures and mechanical stretches, has very recently been shown to mediate at least mechanical hyperalgesia of a mouse under paclitaxel-induced peripheral neuropathy via bradykinin-B1/B2-PKCε axis (Costa et al., 2018). In addition, for bradykinin-induced sensitization, effector components other than such direct temperature sensors are possibly involved. For example, knockouts of a tetrodotoxin-insensitive voltage-gated Na+ channel, Nav1.9, have displayed a blunted phenotype in bradykinin-induced heat hyperalgesia (Amaya et al., 2006).
Still, it remains as theoretical predictions how exactly PKC underlies both activation and sensitization of TRPV1. It is reasonable to hypothesize that these differential outcomes might result from phosphorylation of different serine residues, which possibly contributes to channel gating in different manners. Alternatively, at the point of AKAP79/150 action, the differential roles of PKC could be diverged. Although it seems be limited to a particular tissue like cutaneous areas, the transcellular mechanism involving prostaglandins may exclusively be engaged in sensitization.
The central molecular mechanisms for TRPV1 activation and sensitization have firmly been shown to engage voltage-dependence (Voets et al., 2004). The relevant stimuli, including heat, capsaicin, protons, endogenous ligands, phosphorylations, etc., appear to converge into the leftward shift of TRPV1 voltage-dependence. In this regard, given multiple stimuli may be additive or synergistic for enhancing TRPV1 voltage sensitivity, which can be seen as one stimulus facilitates the response to others (Vyklický et al., 1999). Accordingly, bradykinin-induced phosphorylation may left-shift the effect of heat on TRPV1 voltage-dependence, leading to augmented firing of the nociceptors upon heat stimulation. An extreme shift may enable TRPV1 activation by ambient temperatures, which can be seen as bradykinin directly excites the neurons. Since TRPV1 is known to essentially undergo Ca2+-induced desensitization to itself, Reeh and colleagues have suggested that, prior to desensitization, bradykinin may induce short-term direct firing, and that the relatively blunted shift of TRPV1 sensitivity may look as if its lowered heat threshold during desensitized state (Reeh and Pethö, 2000; Liang et al., 2001). A newly found mechanism unrelated to voltage dependence or even to other signal transductions mentioned above has recently been proposed. Exocytic trafficking of TRPV1-containing vesicle may selectively contribute to the sensitization of peptdifergic nociceptors, which awaits replication (Mathivanan et al., 2016).
The major tissue type where bradykinin induces COX-dependent prostaglandin secretion remains elusive. While nociceptor neurons has been raised as a crucial source of prostaglandins in the pharmacological inhibition of COXs and labeling of COX expression (Mizumura et al., 1987; Kumazawa et al., 1991; Dray et al., 1992; Rueff and Dray, 1993; Vasko et al., 1994; Weinreich et al., 1995; Maubach and Grundy, 1999; Jenkins et al., 2003; Oshita et al., 2005; Inoue et al., 2006; Tang et al., 2006; Jackson et al., 2007), other studies have failed to corroborate this finding and have instead suggested surrounding tissues innervated by neuronal termini (Lembeck and Juan, 1974; Lembeck et al., 1976; Juan, 1977; Franco-Cereceda, 1989; McGuirk and Dolphin, 1992; Fox et al., 1993; Sauer et al., 1998; Kajekar et al., 1999; Sauer et al., 2000; Pethö et al., 2001; Shin et al., 2002; Ferreira et al., 2004). Possibly, COXs in non-neuronal cells may be of more importance during the initial stages of bradykinin action and a relatively long term exposure (∼hours or longer) is needed for the induction of neuronal expression of COXs (Oshita et al., 2005). However, the relative importance of COX-1 and COX-2 needs to be fully assessed (Jackson et al., 2007; Mayer et al., 2007). In addition, many lines of pharmacological evidence for COX participation include the reduction in bradykinin-evoked immediate excitation of nociceptors by COX inhibition. On the other hand, the protein kinase-mediated molecular mechanisms of bradykinin action mentioned above only explain sensitized heat responses.
TRANSIENT RECEPTOR POTENTIAL ANKYRIN SUBTYPE 1 ION CHANNEL
Transient Receptor Potential ankyrin subtype 1 (TRPA1) is a comparably important TRP channel in nociception with regards to polymodality. The opening of TRPA1 depolarizes polymodal nociceptors in response to temperatures <17°C, mechanical stretches, and reactive irritants (e.g., mustard oil, cinnamaldehyde, air pollutants, prostaglandins with α,β-carbonyl carbon, etc.) (Bang and Hwang, 2009). Inflammatory pain mediators such as bradykinin also appear to positively modulate TRPA1 activity, leading to pain exacerbation.
Bradykinin-induced activation of TRPA1 via arachidonic acid metabolism
In an early study where cinnamaldehyde was first found as a specific agonist for TRPA1, bradykinin also displayed an ability to activate TRPA1 via intracellular signaling. In a heterologous expression system co-transfected with DNAs encoding B2 receptor and TRPA1, immediate TRPA1-specific responses occurred upon bradykinin perfusion, as measured by TRPA1-mediated electrical currents and Ca2+ influx (Bandell et al., 2004). Perfusions of a membrane-permeable DAG analog and an arachidonic acid analog also replicated this response, indicating that the bradykinin pathway may utilize PLC (perhaps together with DAG lipase) for TRPA1 activation and possibly PLA2. Although further downstream signaling has not been thoroughly explored, it is also possible that other substances more metabolized from arachidonic acid can activate TRPA1. For example, a number of prostaglandins (PGs) have also been shown to activate TRPA1 (Andersson et al., 2008; Materazzi et al., 2008). The PGs include 15-deoxy-Δ12, 14-PGJ2, Δ12-PGJ2, PGA1, PGA2, and 8-iso PGA2, all of which contain a reactive carbon that can covalently bind to reactive serine or cysteine residues in TRPA1 protein in the same manner that mustard oil and cinnamaldehyde interact (Hinman et al., 2006; Macpherson et al., 2007). Because the PGs are non-enzymatically generated from COX products such as PGH2 and PGE2, the bradykinin-mediated COX activation mentioned above may be linked to depolarization resulting from TRPA1 activation. Whatever the strongest contributor among the metabolites is, bradykinin appears to depolarize nociceptor neurons not only via TRPV1 but also via TRPA1, which was confirmed in TRPA1 knockout studies through action potential firing and nocifensive behaviors (Bautista et al., 2006; Kwan et al., 2006). TRPA1 knockouts have also exhibited reduced hypersensitivity in response to bradykinin (Bautista et al., 2006; Kwan et al., 2006).
Bradykinin-induced sensitization of TRPA1 activity
Molecular mechanisms for TRPA1 sensitization by bradykinin: Not only activation, but also sensitization of TRPA1 when exposed to bradykinin occurs in nociceptor neurons (Fig. 1). The same research group has suggested that there exist two parallel signaling pathways for bradykinin-induced TRPA1 sensitization, which were the PLC and PKC pathways (Dai et al., 2007; Wang et al., 2008). However, this awaits further confirmation because of some discrepancies. The Gq/11-mediated PLC pathway was raised first (Dai et al., 2007). Without further requirement of downstream signaling such as PKC activation, bilayer PIP2 consumption has been demonstrated to disinhibit TRPA1, which seems to adequately explain enhanced TRPA1 activity observed when exposed to a known specific agonist for TRPA1. This study proposed that the membrane PIP2 intrinsically masks the channel’s activity in the resting state, which was confirmed by an independent study showing that the addition of intracellular PIP2 inhibits TRPA1 opening (Kim et al., 2008). Two other studies have shown the opposite effect, where TRPA1 is directly activated by PIP2 (Akopian et al., 2007; Karashima et al., 2008), while another group failed to show this activation (Kim and Cavanaugh, 2007). TRPV1 has once been demonstrated to be either positively or negatively modulated by the presence of PIP2, which may depend on the extent of channel activation, which is not shown yet to be the case for TRPA1 modulation (Lukacs et al., 2007).
Another proposed mechanism for TRPA1 sensitization by bradykinin is via the PKA. As mentioned above, TRPV1 can be sensitized in a similar manner, but PKA action appears to take a relatively long time (∼10 minutes) and requires PG synthesis as an upstream signal. However, fast sensitization of TRPA1 was shown to be dependent on Gs-mediated adenylate cyclase activity and subsequent PKA activation but unlikely with PG production. Such Gs-mediated signaling by bradykinin stimulation has been reported to occur in different cell types (Stevens et al., 1994; Liebmann et al., 1996; Bae et al., 2003). TRPA1, as well as TRPV1, needs further repetition in this regard.
Evidence from nociceptors and animals: Formalin and mustard oil are TRPA1-selective activators that were used as experimental stimulants for nociceptor excitation in the pain research field prior to their relationship with TRPA1 being discovered. Acute nocifensive behaviors are typically evoked by intraplantar administration of either of formalin or mustard oil, and were shown to be significantly facilitated by injections in the same location of bradykinin itself or bradykinin receptor specific agonists (De Campos et al., 1998; Wang et al., 2008). In addition to these chemical-specific modalities, TRPA1 seems to be involved in noxiously mechanical ones to an extent due to its intrinsic mechanosensitivity (Kwan et al., 2006; Petrus et al., 2007; Brierley et al., 2009; Kwan et al., 2009; Yu and Ouyang, 2009). Nociceptor firing in response to mechanical stimuli was significantly diminished in TRPA1-deficient mice or by pharmacological antagonism (Brierley et al., 2005; Brierley et al., 2009; Yu and Ouyang, 2009).
Therefore, it is worth speculating the relationship between TRPA1 and the molecular mechanisms underlying bradykinin-elicited mechanical hypersensitivities that have been proposed from behavioral studies. Protein kinase G (PKG) has been relatively unexplored with regards to TRPA1 modulation, and PKG inhibition has been shown to reduce bradykinin-induced mechanical hyperalgesia (Nakamura et al., 1996). The same study actually suggested that the nitric oxide synthase (NOS)-guanylate cyclase (GC)-PKG cascade mediates the mechanical hypersensitivity. NOS is possibly activated by PLC-IP3-mobilized Ca2+. However, NO itself is known to react with TRPA1 protein and seemed to be inadequate to lead to hyperalgesia despite the heightened level of NO, indicating that further signal amplification via subsequent GC and PKG activation may be required.
Other studies have raised the role of the PLA2-COX pathway in the development of bradykinin-induced mechanical hyperalgesia (Taiwo and Levine, 1988; Taiwo et al., 1990). COX induction by bradykinin may require a transcellular process in the sensitized heat responses mentioned above. In a multitude of studies on this mechanical hypersensitivity, details particularly including complicated upstreams for the COX mechanism have been described (Ferreira et al., 1993a; Ferreira et al., 1993b; Poole et al., 1999; Cunha et al., 2007). Collectively, the causality seems to involve a transcellular mechanism and to be that the sequential secretions of TNF-α, other cytokines including interleukin-1β (IL-1β), IL-6, and IL-8, and then finally prostaglandins and sympathetic amines. It appears that the major sources of TNF-α and sympathetic amines may be vicinal macrophages and sympathetic nerve termini respectively, indicating that the bradykinin-induced mechanical hyperalgesia may also involve transcellular processes. Seeing as surgical sympathectomy alleviated mechanical, but not heat hyperalgesia, the downstream sympathetic amines from the postganglionic neurons may only control the peripheral mechanical function of nociceptors (Koltzenburg et al., 1992; Meyer et al., 1992; Schuligoi et al., 1994).
Interestingly, the occurrence of mechanical hypersensitivity appears to depend on the location of bradykinin accumulation (Manning et al., 1991; Khan et al., 1992; Khasar et al., 1993). This may again indicate that not only the changes in the functionality of nociceptors but also transcellular interactions where specific cellular components that additionally participate are important. In accordance with a study showing that mechanical hyperalgesia was induced by intradermal injections of bradykinin or PGE2, but not readily by subcutaneous treatments, later studies using a diverse range of nociceptor markers demonstrated that nociceptor termini are differentially distributed in terms of the depth of the skin layer, and that a more superficial subpopulation may supposedly be responsible for mechanical hyperalgesia (Khasar et al., 1993; Zylka et al., 2005; Cavanaugh et al., 2009). Interestingly, it has recently been demonstrated that TRPA1 in the central terminal of nociceptors also contribute to the development of mechanical hyperalgesia by participating in B1 receptor-dependent spinal neuroinflammation where intracellular and transcellular mechanisms may operate in a similar manner as mentioned above (Meotti et al., 2017).
TRPA1 contributes to bradykinin-induced heat hyperalgesia: Although TRPA1 is not intrinsically sensitive to hot temperatures, TRPA1 knockouts have exhibited a blunted phenotype in bradykinin-induced heat hyperalgesia when compared to wild type littermates (Bautista et al., 2006). In the same study, however, CFA-induced heat hyperalgesia was not affected by TRPA1 deletion. TRPA1 may only mildly influence TRPV1-based heat sensation. Intracellular Ca2+ elevated first by TRPV1 opening in response to heat was once proposed to link TRPV1 activation to the subsequent TRPA1 activation. However a current theory is that a part of TRPV1 and TRPA1 proteins may be physically coupled to form a sensory complex located on the surface of the nociceptor terminal (Staruschenko et al., 2010; Fischer et al., 2014; Weng et al., 2015).
Difference between TRPA1 and PIEZO2: Piezo-type mechanosensitive ion channel component 2 (PIEZO2) is a recently discovered cation channel that has been shown to be a sensor responsible for innocuous touch and proprioception by displaying rapidly-inactivating feature with a low mechanical threshold and by being expressed in a medium to large diameter non-nociceptive population of sensory neurons, whereas TRPA1 represents a slowly-inactivating component with a high mechanical threshold. Interestingly, one study has shown that a fraction of the nociceptive subpopulation expresses PIEZO2 that can be functionally modified in response to bradykinin signaling (Dubin et al., 2012). Unlike TRPA1, PIEZO2 was only sensitized but not activated by bradykinin exposure. Its mechanosensitivity and response efficacy were both heightened with a moderate threshold shift. PKA and PKC are involved in the enhancement in mechanosensitivity, but surprisingly, nothing upstream of PKC activation related to Gq/11- or Gi/o-coupled PLC activation was associated.
Ca2+-ACTIVATED Cl− CHANNELS
The two aforementioned TRPs are not the only excitatory effector ion channels involved in bradykinin-induced nociceptor firing. Many studies have shown that incapacitating TRPs by using antagonist pharmacology or gene deletion did not completely ablate the action potential discharges of nociceptors upon bradykinin exposure (Dray et al., 1990; Dickenson and Dray, 1991; Zahner et al., 2003; Kollarik and Undem, 2004; Rong et al., 2004; Qin et al., 2006; Katanosaka et al., 2008; Brierley et al., 2009). An explanation as to the unknown excitatory component, i.e., the role for Cl− channels has been emerging. Chemical inhibition of Ca2+-activated Cl− channels (CaCCs) was effective in reducing bradykinin-induced firing in an ex vivo tissue-nerve model from the guinea pig airway sensory system and in in vitro cultured nodose neurons (Oh and Weinreich, 2004; Lee et al., 2005a). In sensory neurons, it is well known that the intracellular Cl− concentration is high and that opening of Cl− channels leads to the efflux of Cl−, resulting in depolarization, which was confirmed by the same studies. In pathologic conditions, like chronic exposure to major inflammatory pain mediators in the periphery including prostaglandins, nerve growth factor (NGF), and ATP, the intracellular Cl− concentration is known to even further be elevated owing to the facilitated activities of surface Na+-K+-2Cl− cotransporters (NKCCs), indicating that Cl− channel opening may contribute more to nociceptor firing than non-inflamed situations (Sung et al., 2000; Labrakakis et al., 2003; Funk et al., 2008; Price et al., 2009).
Delicate molecular approach was conducted by a group for determining the genetic identity of CaCC of rodent nociceptors contributing to bradykinin-induced excitation and the underlying activation mechanisms (Liu et al., 2010; Jin et al., 2013). The central player is anoctamin 1 (ANO1, also known as TMEM16A), a relatively newly discovered ion channel. The studies dissected how the intracellular Ca2+ was affected by bradykinin stimulation and revealed two phases, and the first of which may more depend on intracellular mobilization by IP3. This indicates that bradykinin-evoked G protein signaling leads to PLC activation, resulting in productions of IP3 and DAG as mentioned above (Thayer et al., 1988; Burgess et al., 1989; Kano et al., 1994; Kozaki et al., 2007), followed by the activation of IP3 receptors on the endoplasmic reticulum (ER) membrane. This causes Ca2+ release from the ER, completing the first Ca2+ phase. This firstly elevated cytoplasmic Ca2+ activates ANO1. ANO1 was shown to physically couple to IP3 receptor type 1 and bradykinin B2 receptor to compose a signaling complex, enabling the efficient utilization of the locally increased levels of Ca2+. The second phase of Ca2+ elevation may depend on the influx of extracellular Ca2+, resulting from activation of voltage-gated Ca2+ channels by ANO1-elicited depolarization, and of TRP channels that are highly Ca2+ permeable. Such ANO1-dependent bradykinin-mediated nociception was again confirmed in an in vivo study using tissue-specific ANO1-deficient mice (Advillin/Ano1fl/fl) that lost ANO1 expression mainly in DRG neurons (Lee et al., 2014).
K+ CHANNEL INHIBITION
The decreased activity of resting K+ channels may contribute to depolarization. Indeed, two studies that were mentioned previously, exploring the outcomes of the first phase of Ca2+ elevation in response to bradykinin stimulation have proposed that together with CaCC activation, K+ channel inhibition is also involved in nociceptor firing during this first phase (Oh and Weinreich, 2004; Liu et al., 2010). Two different K+-permeating components were identified as contributors by the two studies respectively, as explained in the following section.
KCNQ voltage-gated K+ channels
The outward K+ current mediated by the opening of the KCNQ channel (also known as Kv7) refers to the M current as it was first found as a downstream effector of M2 muscarinic receptor signaling. A fraction of KCNQ channels open in the resting state and control the resting membrane potential and action potential rheobase (Delmas and Brown, 2005). The M current can be inhibited in the early phase of the intracellular Ca2+ wave caused by bradykinin exposure (Liu et al., 2010). Further inhibition of the KCNQ-mediated current by a synthetic specific antagonist potentiated bradykinin-induced firing while its activation using the channel opener retigabine diminished it. Acutely pretreated retigabine also prevented nocifensive behaviors caused by intraplantar bradykinin injection in in vivo observations. Additionally, chelation of the early Ca2+ rise but not PKC or PLA2 inhibition reversed the closing of the K+ channel in in vitro nociceptor assays, indicating that the Gq/11-coupled-PLC-IP3-Ca2+ cascade is required for the K+ channel contribution and that no other signaling downstream of PLC or other branches of G protein signaling seems to be involved. The genetic identity of the KCNQ subtypes responsible for the underlying molecular mechanisms involved in bradykinin-induced signaling remain to be elucidated. Very recently, KCNQ3 and KCNQ5 have been raised as major Kv7 subtypes that depolarize murine and human visceral nociceptors upon B2 receptor stimulation (Peiris et al., 2017).
Ca2+-activated K+ channels
Another K+ component altered by bradykinin stimulation has been shown to be mediated by Ca2+-activated K+ channels (IKCa). With regards to the action potential phase, these K+ currents typically compose a slow component of the afterhy-perpolarization (AHP). AHP is responsible for spike frequency accommodation in repeated firing. A shortened AHP resulting from Ca2+-activated K+ channel inhibition causes sustained or increased firing frequencies (Weinreich and Wonderlin, 1987; Cordoba-Rodriguez et al., 1999). The contribution of the bradykinin-induced channel blockade to the alteration of nodose neuronal firing may reflect this paradigm (Oh and Weinreich, 2004).
CONCLUSIONS
Bradykinin is among the major pain mediators during inflammation. Peripherally produced bradykinin alters the electrical functions of nociceptor sensory neurons that are the forefront initiators of the ascending signals of the sensory neural pathway for pain perception. Bradykinin generally enhances their excitability, greatly contributing to the generation and exacerbation of pain. At the cellular level, bradykinin not only acutely excites the neurons but also electrically sensitizes them. Through intracellular signaling, mostly composed of G-protein coupled ones, it has been hypothesized that bradykinin may finally augment the depolarizing activities of some specific effector ion channels expressed in the nociceptor neurons. Currently, an array of ion channels have been shown to be affected in this paradigm. Here we overviewed six important ion channels in their role as a depolarizing effector. The opening of TRPV1, TRPA1, and ANO1 all seem to enact this role in the direct induction of neuronal firing by bradykinin. TRPV1 and TRPA1 also appear to be involved in sensitized neuronal function in a longer duration. PIEZO2 is an emerging ion channel that functions as a mechanical pain-specific sensitizing effector. KCNQ and Ca2+-activated K+ channels may contribute to the initial excitation through their functional downregulation. Linker signals between bradykinin receptor activation and depolarizing effectors are currently being revealed in greater depth (summarized in Fig. 1).
The consistent expansion of information has broadened the knowledge of the molecular nature of bradykinin-induced inflammatory pain and has validated bradykinin signaling as an analgesic target. In particular, the B2 receptor inhibitor HOE 140 and capsaicin-mediated TRPV1 incapacitation seem to have promising outcomes from a multitude of clinical researches (Backonja et al., 2008; Song et al., 2008). Nonetheless, efforts to establish the excitatory mechanism mediated by relatively recent found effectors such as ANO1 and K+ channels are still required. Further, unknown component may be present for the nociceptive neuronal actions of bradykinin. For example, pharmacological antagonism of purinergic P2X3 ion channel has once been shown to be effective specifically at bradykinin induced mechanical hyperalgesia, which needs to be confirmed by further molecular approaches (de Oliveira Fusaro et al., 2010). Among nociceptor-specific voltage-gated Na+ channels, Nav1.9 may particularly be affected under bradykinin-including pathologic condition but the mechanism remains elusive (Vaughn and Gold, 2010). Further accumulation of the knowledge will contribute to more precise understanding of the depolarization mechanisms and to development of more sophisticated painkilling strategies.
Acknowledgments
This work was supported by grants from the National Research Foundation of Korea (2017R1A2B2001817, 2017M3C7A1025600). SIC collected and analyzed the information and wrote the preliminary draft. SWH supervised the studies and wrote the manuscript. All authors read and approved the final manuscript. The authors declare that there is no conflict of interest regarding the publication of this article.
REFERENCES
- Akopian AN, Ruparel NB, Jeske NA, Hargreaves KM. Transient receptor potential TRPA1 channel desensitization in sensory neurons is agonist dependent and regulated by TRPV1-directed internalization. J Physiol. 2007;583:175–193. doi: 10.1113/jphysiol.2007.133231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen AC, Gammon CM, Ousley AH, McCarthy KD, Morell P. Bradykinin stimulates arachidonic acid release through the sequential actions of an sn-1 diacylglycerol lipase and a monoacylglycerol lipase. J Neurochem. 1992;58:1130–1139. doi: 10.1111/j.1471-4159.1992.tb09372.x. [DOI] [PubMed] [Google Scholar]
- Amaya F, Wang H, Costigan M, Allchorne AJ, Hatcher JP, Egerton J, Stean T, Morisset V, Grose D, Gunthorpe MJ, Chessell IP, Tate S, Green PJ, Woolf CJ. The voltage-gated sodium channel Na(v)1.9 is an effector of peripheral inflammatory pain hypersensitivity. J Neurosci. 2006;26:12852–12860. doi: 10.1523/JNEUROSCI.4015-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson DA, Gentry C, Moss S, Bevan S. Transient receptor potential A1 is a sensory receptor for multiple products of oxidative stress. J Neurosci. 2008;28:2485–2494. doi: 10.1523/JNEUROSCI.5369-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong D, Jepson J, Keele C, Stewart J. Pain-producing substance in human inflammatory exudates and plasma. J Physiol. 1957;135:350–370. doi: 10.1113/jphysiol.1957.sp005715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babenko V, Graven-Nielsen T, Svensson P, Drewes AM, Jensen TS, Arendt-Nielsen L. Experimental human muscle pain induced by intramuscular injections of bradykinin, serotonin, and substance P. Eur J Pain. 1999;3:93–102. doi: 10.1053/eujp.1998.0103. [DOI] [PubMed] [Google Scholar]
- Backonja M, Wallace MS, Blonsky ER, Cutler BJ, Malan P, Rauck R, Tobias J. NGX-4010, a high-concentration capsaicin patch, for the treatment of postherpetic neuralgia: a randomised, double-blind study. Lancet Neurol. 2008;7:1106–1112. doi: 10.1016/S1474-4422(08)70228-X. [DOI] [PubMed] [Google Scholar]
- Bae SW, Kim HS, Cha YN, Park YS, Jo SA, Jo I. Rapid increase in endothelial nitric oxide production by bradykinin is mediated by protein kinase A signaling pathway. Biochem Biophys Res Commun. 2003;306:981–987. doi: 10.1016/S0006-291X(03)01086-6. [DOI] [PubMed] [Google Scholar]
- Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, Earley TJ, Patapoutian A. Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron. 2004;41:849–857. doi: 10.1016/S0896-6273(04)00150-3. [DOI] [PubMed] [Google Scholar]
- Bang S, Hwang SW. Polymodal ligand sensitivity of TRPA1 and its modes of interactions. J Gen Physiol. 2009;133:257–262. doi: 10.1085/jgp.200810138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber LA, Vasko MR. Activation of protein kinase C augments peptide release from rat sensory neurons. J Neurochem. 1996;67:72–80. doi: 10.1046/j.1471-4159.1996.67010072.x. [DOI] [PubMed] [Google Scholar]
- Bautista DM, Jordt S-E, Nikai T, Tsuruda PR, Read AJ, Poblete J, Yamoah EN, Basbaum AI, Julius D. TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell. 2006;124:1269–1282. doi: 10.1016/j.cell.2006.02.023. [DOI] [PubMed] [Google Scholar]
- Beck PW, Handwerker HO. Bradykinin and serotonin effects on various types of cutaneous nerve fibres. Pflugers Arch. 1974;347:209–222. doi: 10.1007/BF00592598. [DOI] [PubMed] [Google Scholar]
- Bhave G, Hu H-J, Glauner KS, Zhu W, Wang H, Brasier D, Oxford GS, Gereau RW. Protein kinase C phosphorylation sensitizes but does not activate the capsaicin receptor transient receptor potential vanilloid 1 (TRPV1). Proc Natl Acad Sci USA. 2003;100:12480–12485. doi: 10.1073/pnas.2032100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brierley S, Jones R, Xu L, Gebhart G, Blackshaw L. Activation of splanchnic and pelvic colonic afferents by bradykinin in mice. Neurogastroenterol Motil. 2005;17:854–862. doi: 10.1111/j.1365-2982.2005.00710.x. [DOI] [PubMed] [Google Scholar]
- Brierley SM, Hughes PA, Page AJ, Kwan KY, Martin CM, O’Donnell TA, Cooper NJ, Harrington AM, Adam B, Liebregts T. The ion channel TRPA1 is required for normal mechanosensation and is modulated by algesic stimuli. Gastroenterology. 2009;137:2084–2095.e3. doi: 10.1053/j.gastro.2009.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burch RM, Axelrod J. Dissociation of bradykinin-induced prostaglandin formation from phosphatidylinositol turnover in Swiss 3T3 fibroblasts: evidence for G protein regulation of phospholipase A2. Proc Natl Acad Sci USA. 1987;84:6374–6378. doi: 10.1073/pnas.84.18.6374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess GM, Mullaney I, McNeill M, Dunn PM, Rang HP. Second messengers involved in the mechanism of action of bradykinin in sensory neurons in culture. J Neurosci. 1989;9:3314–3325. doi: 10.1523/JNEUROSCI.09-09-03314.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camprubi-Robles M, Planells-Cases R, Ferrer-Montiel A. Differential contribution of SNARE-dependent exocytosis to inflammatory potentiation of TRPV1 in nociceptors. FASEB J. 2009;23:3722–3733. doi: 10.1096/fj.09-134346. [DOI] [PubMed] [Google Scholar]
- Carr MJ, Kollarik M, Meeker SN, Undem BJ. A role for TRPV1 in bradykinin-induced excitation of vagal airway afferent nerve terminals. J Pharmacol Exp Ther. 2003;304:1275–1279. doi: 10.1124/jpet.102.043422. [DOI] [PubMed] [Google Scholar]
- Cavanaugh DJ, Lee H, Lo L, Shields SD, Zylka MJ, Basbaum AI, Anderson DJ. Distinct subsets of unmyelinated primary sensory fibers mediate behavioral responses to noxious thermal and mechanical stimuli. Proc Natl Acad Sci USA. 2009;106:9075–9080. doi: 10.1073/pnas.0901507106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesare P, Dekker LV, Sardini A, Parker PJ, McNaughton PA. Specific involvement of PKC-ε in sensitization of the neuronal response to painful heat. Neuron. 1999;23:617–624. doi: 10.1016/S0896-6273(00)80813-2. [DOI] [PubMed] [Google Scholar]
- Cesare P, McNaughton P. A novel heat-activated current in nociceptive neurons and its sensitization by bradykinin. Proc Natl Acad Sci USA. 1996;93:15435–15439. doi: 10.1073/pnas.93.26.15435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chahl LA, Iggo A. The effects of bradykinin and prostaglandin E1 on rat cutaneous afferent nerve activity. Br J Pharmacol. 1977;59:343–347. doi: 10.1111/j.1476-5381.1977.tb07498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SI, Yoo S, Lim JY, Hwang SW. Are sensory TRP channels biological alarms for lipid peroxidation? Int J Mol Sci. 2014;15:16430–16457. doi: 10.3390/ijms150916430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang H-h, Prescott ED, Kong H, Shields S, Jordt S-E, Basbaum AI, Chao MV, Julius D. Bradykinin and nerve growth factor release the capsaicin receptor from PtdIns (4, 5) P2-mediated inhibition. Nature. 2001;411:957–962. doi: 10.1038/35082088. [DOI] [PubMed] [Google Scholar]
- Cordoba-Rodriguez R, Moore KA, Kao JP, Weinreich D. Calcium regulation of a slow post-spike hyperpolarization in vagal afferent neurons. Proc Natl Acad Sci USA. 1999;96:7650–7657. doi: 10.1073/pnas.96.14.7650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa R, Bicca MA, Manjavachi MN, Segat GC, Dias FC, Fernandes ES, Calixto JB. Kinin receptors sensitize TRPV4 channel and induce mechanical hyperalgesia: relevance to paclitaxel-induced peripheral neuropathy in mice. Mol Neurobiol. 2018;55:2150–2161. doi: 10.1007/s12035-017-0475-9. [DOI] [PubMed] [Google Scholar]
- Costello A, Hargreaves K. Suppression of carrageenan-induced hyperalgesia, hyperthermia and edema by a bradykinin antagonist. Eur J Pharmacol. 1989;171:259–263. doi: 10.1016/0014-2999(89)90118-0. [DOI] [PubMed] [Google Scholar]
- Crandall M, Kwash J, Yu W, White G. Activation of protein kinase C sensitizes human VR1 to capsaicin and to moderate decreases in pH at physiological temperatures in Xenopus oocytes. Pain. 2002;98:109–117. doi: 10.1016/S0304-3959(02)00034-9. [DOI] [PubMed] [Google Scholar]
- Cunha TM, Verri WA, Fukada SY, Guerrero AT, Santodomingo-Garzón T, Poole S, Parada CA, Ferreira SH, Cunha FQ. TNF-α and IL-1β mediate inflammatory hypernociception in mice triggered by B 1 but not B 2 kinin receptor. Eur J Pharmacol. 2007;573:221–229. doi: 10.1016/j.ejphar.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Dai Y, Wang S, Tominaga M, Yamamoto S, Fukuoka T, Higashi T, Kobayashi K, Obata K, Yamanaka H, Noguchi K. Sensitization of TRPA1 by PAR2 contributes to the sensation of inflammatory pain. J Clin Invest. 2007;117:1979–1987. doi: 10.1172/JCI30951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Campos R, Henriques M, Calixto J. Systemic treatment with Mycobacterium bovis bacillus calmette-guerin (BCG) potentiates kinin B 1 receptor agonist-induced nociception and oedema formation in the formalin test in mice. Neuropeptides. 1998;32:393–403. doi: 10.1016/S0143-4179(98)90062-2. [DOI] [PubMed] [Google Scholar]
- de Oliveira Fusaro MCG, Pelegrini-da-Silva A, Araldi D, Parada CA, Tambeli CH. P2X3 and P2X2/3 receptors mediate mechanical hyperalgesia induced by bradykinin, but not by proinflammatory cytokines, PGE 2 or dopamine. Eur J Pharmacol. 2010;649:177–182. doi: 10.1016/j.ejphar.2010.09.037. [DOI] [PubMed] [Google Scholar]
- Delmas P, Brown DA. Pathways modulating neural KCNQ/M (Kv7) potassium channels. Nat Rev Neurosci. 2005;6:850–862. doi: 10.1038/nrn1785. [DOI] [PubMed] [Google Scholar]
- Dickenson A, Dray A. Selective antagonism of capsaicin by capsazepine: evidence for a spinal receptor site in capsaicin-induced antinociception. Br J Pharmacol. 1991;104:1045–1049. doi: 10.1111/j.1476-5381.1991.tb12547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dray A, Bettaney J, Forster P, Perkins M. Bradykinin-induced stimulation of afferent fibres is mediated through protein kinase C. Neurosci Lett. 1988;91:301–307. doi: 10.1016/0304-3940(88)90697-0. [DOI] [PubMed] [Google Scholar]
- Dray A, Forbes C, Burgess G. Ruthenium red blocks the capsaicin-induced increase in intracellular calcium and activation of membrane currents in sensory neurones as well as the activation of peripheral nociceptors in vitro. Neurosci Lett. 1990;110:52–59. doi: 10.1016/0304-3940(90)90786-9. [DOI] [PubMed] [Google Scholar]
- Dray A, Patel I, Perkins M, Rueff A. Bradykinin-induced activation of nociceptors: receptor and mechanistic studies on the neonatal rat spinal cord-tail preparation in vitro. Br J Pharmacol. 1992;107:1129–1134. doi: 10.1111/j.1476-5381.1992.tb13418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubin AE, Schmidt M, Mathur J, Petrus MJ, Xiao B, Coste B, Patapoutian A. Inflammatory signals enhance piezo2-mediated mechanosensitive currents. Cell Rep. 2012;2:511–517. doi: 10.1016/j.celrep.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira J, Beirith A, Mori MA, Araújo RC, Bader M, Pesquero JB, Calixto JB. Reduced nerve injury-induced neuropathic pain in kinin B1 receptor knock-out mice. J Neurosci. 2005;25:2405–2412. doi: 10.1523/JNEUROSCI.2466-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira J, Campos MM, Pesquero JB, Araújo RC, Bader M, Calixto JB. Evidence for the participation of kinins in Freund’s adjuvant-induced inflammatory and nociceptive responses in kinin B 1 and B 2 receptor knockout mice. Neuropharmacology. 2001;41:1006–1012. doi: 10.1016/S0028-3908(01)00142-3. [DOI] [PubMed] [Google Scholar]
- Ferreira J, Da Silva GL, Calixto JB. Contribution of vanilloid receptors to the overt nociception induced by B2 kinin receptor activation in mice. Br J Pharmacol. 2004;141:787–794. doi: 10.1038/sj.bjp.0705546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira S, Lorenzetti B, Cunha F, Poole S. Bradykinin release of TNF-α plays a key role in the development of inflammatory hyperalgesia. Agents Actions. 1993a;38:C7–C9. doi: 10.1007/BF01991120. [DOI] [PubMed] [Google Scholar]
- Ferreira S, Lorenzetti B, Poole S. Bradykinin initiates cytokine-mediated inflammatory hyperalgesia. Br J Pharmacol. 1993b;110:1227–1231. doi: 10.1111/j.1476-5381.1993.tb13946.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer MJ, Balasuriya D, Jeggle P, Goetze TA, McNaughton PA, Reeh PW, Edwardson JM. Direct evidence for functional TRPV1/TRPA1 heteromers. Pflugers Arch. 2014;466:2229–2241. doi: 10.1007/s00424-014-1497-z. [DOI] [PubMed] [Google Scholar]
- Fischer MJ, McNaughton PA. How anchoring proteins shape pain. Pharmacol Ther. 2014;143:316–322. doi: 10.1016/j.pharmthera.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Fox A, Barnes P, Urban L, Dray A. An in vitro study of the properties of single vagal afferents innervating guinea-pig airways. J Physiol. 1993;469:21–35. doi: 10.1113/jphysiol.1993.sp019802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox AJ, Lalloo UG, Belvisi MG, Bernareggi M, Chung KF, Barnes PJ. Bradykinin–evoked sensitization of airway sensory nerves: A mechanism for ACE–inhibitor cough. Nat Med. 1996;2:814–817. doi: 10.1038/nm0796-814. [DOI] [PubMed] [Google Scholar]
- Franco-Cereceda A. Prostaglandins and CGRP release from cardiac sensory nerves. Naunyn Schmiedebergs Arch Pharmacol. 1989;340:180–184. doi: 10.1007/BF00168966. [DOI] [PubMed] [Google Scholar]
- Füredi R, Bölcskei K, Szolcsányi J, Pethő G. Comparison of the peripheral mediator background of heat injury-and plantar incision-induced drop of the noxious heat threshold in the rat. Life Sci. 2010;86:244–250. doi: 10.1016/j.lfs.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Funk K, Woitecki A, Franjic-Würtz C, Gensch T, Möhrlen F, Frings S. Modulation of chloride homeostasis by inflammatory mediators in dorsal root ganglion neurons. Mol Pain. 2008;4:32. doi: 10.1186/1744-8069-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabra BH, Benrezzak O, Pheng L-H, Duta D, Daull P, Sirois P, Nantel F, Battistini B. Inhibition of type 1 diabetic hyperalgesia in streptozotocin-induced Wistar versus spontaneous gene-prone BB/Worchester rats: efficacy of a selective bradykinin B1 receptor antagonist. J Neuropathol Exp Neurol. 2005a;64:782–789. doi: 10.1097/01.jnen.0000178448.79713.5f. [DOI] [PubMed] [Google Scholar]
- Gabra BH, Merino VF, Bader M, Pesquero JB, Sirois P. Absence of diabetic hyperalgesia in bradykinin B1 receptor-knockout mice. Regul Pept. 2005b;127:245–248. doi: 10.1016/j.regpep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Gabra BH, Sirois P. Role of bradykinin B 1 receptors in diabetes-induced hyperalgesia in streptozotocin-treated mice. Eur J Pharmacol. 2002;457:115–124. doi: 10.1016/S0014-2999(02)02658-4. [DOI] [PubMed] [Google Scholar]
- Gabra BH, Sirois P. Beneficial effect of chronic treatment with the selective bradykinin B 1 receptor antagonists, R-715 and R-954, in attenuating streptozotocin-diabetic thermal hyperalgesia in mice. Peptides. 2003a;24:1131–1139. doi: 10.1016/j.peptides.2003.06.003. [DOI] [PubMed] [Google Scholar]
- Gabra BH, Sirois P. Kinin B 1 receptor antagonists inhibit diabetes-induced hyperalgesia in mice. Neuropeptides. 2003b;37:36–44. doi: 10.1016/S0143-4179(02)00148-8. [DOI] [PubMed] [Google Scholar]
- Gammon CM, Allen AC, Morell P. Bradykinin stimulates phosphoinositide hydrolysis and mobilization of arachidonic acid in dorsal root ganglion neurons. J Neurochem. 1989;53:95–101. doi: 10.1111/j.1471-4159.1989.tb07299.x. [DOI] [PubMed] [Google Scholar]
- Gao Y, Cao E, Julius D, Cheng Y. TRPV1 structures in nanodiscs reveal mechanisms of ligand and lipid action. Nature. 2016;534:347–351. doi: 10.1038/nature17964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson HE, Edwards JG, Page RS, Van Hook MJ, Kauer JA. TRPV1 channels mediate long-term depression at synapses on hippocampal interneurons. Neuron. 2008;57:746–759. doi: 10.1016/j.neuron.2007.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gougat J, Ferrari B, Sarran L, Planchenault C, Poncelet M, Maruani J, Alonso R, Cudennec A, Croci T, Guagnini F. SSR240612 [(2R)-2-[((3R)-3-(1, 3-benzodioxol-5-yl)-3-{[(6-methoxy-2-naphthyl) sulfonyl] amino} propanoyl) amino]-3-(4-{[2R, 6S)-2, 6-dimethylpiperidinyl] methyl} phenyl)-N-isopropyl-N-methylpropanamide hydrochloride], a new nonpeptide antagonist of the bradykinin B1 receptor: biochemical and pharmacological characterization. J Pharmacol Exp Ther. 2004;309:661–669. doi: 10.1124/jpet.103.059527. [DOI] [PubMed] [Google Scholar]
- Gregus AM, Doolen S, Dumlao DS, Buczynski MW, Takasusuki T, Fitzsimmons BL, Hua X-Y, Taylor BK, Dennis EA, Yaksh TL. Spinal 12-lipoxygenase-derived hepoxilin A3 contributes to inflammatory hyperalgesia via activation of TRPV1 and TRPA1 receptors. Proc Natl Acad Sci USA. 2012;109:6721–6726. doi: 10.1073/pnas.1110460109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesbacher T, Amann R, Sametz W, Diethart S, Juan H. The nonpeptide B2 receptor antagonist FR173657: inhibition of effects of bradykinin related to its role in nociception. Br J Pharmacol. 1998;124:1328–1334. doi: 10.1038/sj.bjp.0701938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z-L, Fu L-W, Symons JD, Longhurst JC. Signal transduction in activation of ischemically sensitive abdominal visceral afferents: role of PKC. Am J Physiol. 1998;275:H1024–H1031. doi: 10.1152/ajpheart.1998.275.3.H1024. [DOI] [PubMed] [Google Scholar]
- Guo Z-L, Symons JD, Longhurst JC. Activation of visceral afferents by bradykinin and ischemia: independent roles of PKC and prostaglandins. Am J Physiol. 1999;276:H1884–H1891. doi: 10.1152/ajpheart.1999.276.6.H1884. [DOI] [PubMed] [Google Scholar]
- Haake B, Liang Y, Reeh P. Bradykinin effects and receptor subtypes in rat cutaneous nociceptors, in vitro. Pflugers Arch. 1996;431:R15. [Google Scholar]
- Hinman A, Chuang H-h, Bautista DM, Julius D. TRP channel activation by reversible covalent modification. Proc Natl Acad Sci USA. 2006;103:19564–19568. doi: 10.1073/pnas.0609598103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Y, Abbott F. Behavioural effects of intraplantar injection of inflammatory mediators in the rat. Neuroscience. 1994;63:827–836. doi: 10.1016/0306-4522(94)90527-4. [DOI] [PubMed] [Google Scholar]
- Hwang SW, Cho H, Kwak J, Lee S-Y, Kang C-J, Jung J, Cho S, Min KH, Suh Y-G, Kim D. Direct activation of capsaicin receptors by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci USA. 2000;97:6155–6160. doi: 10.1073/pnas.97.11.6155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda Y, Ueno A, Naraba H, Oh-ishi S. Evidence for bradykinin mediation of carrageenin-induced inflammatory pain: a study using kininogen-deficient Brown Norway Katholiek rats. Biochem Pharmacol. 2001a;61:911–914. doi: 10.1016/S0006-2952(01)00536-6. [DOI] [PubMed] [Google Scholar]
- Ikeda Y, Ueno A, Naraba H, Oh-ishi S. Involvement of vanilloid receptor VR1 and prostanoids in the acid-induced writhing responses of mice. Life Sci. 2001b;69:2911–2919. doi: 10.1016/S0024-3205(01)01374-1. [DOI] [PubMed] [Google Scholar]
- Inoue A, Iwasa M, Nishikura Y, Ogawa S, Nakasuka A, Nakata Y. The long-term exposure of rat cultured dorsal root ganglion cells to bradykinin induced the release of prostaglandin E2 by the activation of cyclooxygenase-2. Neurosci Lett. 2006;401:242–247. doi: 10.1016/j.neulet.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Jackson JG, Usachev YM, Thayer SA. Bradykinin-induced nuclear factor of activated T-cells-dependent transcription in rat dorsal root ganglion neurons. Mol Pharmacol. 2007;72:303–310. doi: 10.1124/mol.107.035048. [DOI] [PubMed] [Google Scholar]
- Jenkins DW, Sellers LA, Feniuk W, Humphrey PP. Characterization of bradykinin-induced prostaglandin E2 release from cultured rat trigeminal ganglion neurones. Eur J Pharmacol. 2003;469:29–36. doi: 10.1016/S0014-2999(03)01732-1. [DOI] [PubMed] [Google Scholar]
- Jin X, Shah S, Liu Y, Zhang H, Lees M, Fu Z, Lippiat JD, Beech DJ, Sivaprasadarao A, Baldwin SA. Activation of the Cl− channel ANO1 by localized calcium signals in nociceptive sensory neurons requires coupling with the IP3 receptor. Sci Signal. 2013;6 doi: 10.1126/scisignal.2004184. ra73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan H. Mechanism of action of bradykinin-induced release of prostaglandin E. Naunyn Schmiedebergs Arch Pharmacol. 1977;300:77–85. doi: 10.1007/BF00505082. [DOI] [PubMed] [Google Scholar]
- Juan H, Lembeck F. Action of peptides and other algesic agents on paravascular pain receptors of the isolated perfused rabbit ear. Naunyn Schmiedebergs Arch Pharmacol. 1974;283:151–164. doi: 10.1007/BF00501142. [DOI] [PubMed] [Google Scholar]
- Kajekar R, Proud D, Myers AC, Meeker SN, Undem BJ. Characterization of vagal afferent subtypes stimulated by bradykinin in guinea pig trachea. J Pharmacol Exp Ther. 1999;289:682–687. [PubMed] [Google Scholar]
- Kano M, Kawakami T, Hikawa N, Hori H, Takenaka T, Gotoh H. Bradykinin-responsive cells of dorsal root ganglia in culture: cell size, firing, cytosolic calcium, and substance P. Cell Mol Neurobiol. 1994;14:49–57. doi: 10.1007/BF02088588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karashima Y, Prenen J, Meseguer V, Owsianik G, Voets T, Nilius B. Modulation of the transient receptor potential channel TRPA1 by phosphatidylinositol 4,5-biphosphate manipulators. Pflugers Arch. 2008;457:77. doi: 10.1007/s00424-008-0493-6. [DOI] [PubMed] [Google Scholar]
- Katanosaka K, Banik RK, Giron R, Higashi T, Tominaga M, Mizumura K. Contribution of TRPV1 to the bradykinin-evoked nociceptive behavior and excitation of cutaneous sensory neurons. Neurosci Res. 2008;62:168–175. doi: 10.1016/j.neures.2008.08.004. [DOI] [PubMed] [Google Scholar]
- Khan AA, Raja SN, Manning DC, Campbell JN, Meyer RA. The effects of bradykinin and sequence-related analogs on the response properties of cutaneous nociceptors in monkeys. Somatosens Mot Res. 1992;9:97–106. doi: 10.3109/08990229209144765. [DOI] [PubMed] [Google Scholar]
- Khasar SG, Green PG, Levine JD. Comparison of intradermal and subcutaneous hyperalgesic effects of inflammatory mediators in the rat. Neurosci Lett. 1993;153:215–218. doi: 10.1016/0304-3940(93)90325-F. [DOI] [PubMed] [Google Scholar]
- Kim D, Cavanaugh EJ. Requirement of a soluble intracellular factor for activation of transient receptor potential A1 by pungent chemicals: role of inorganic polyphosphates. J Neurosci. 2007;27:6500–6509. doi: 10.1523/JNEUROSCI.0623-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Cavanaugh EJ, Simkin D. Inhibition of transient receptor potential A1 channel by phosphatidylinositol-4, 5-bisphosphate. Am J Physiol Cell Physiol. 2008;295:C92–C99. doi: 10.1152/ajpcell.00023.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindgen-Milles D, Klement W, Arndt J. The nociceptive systems of skin, paravascular tissue and hand veins of humans and their sensitivity to bradykinin. Neurosci Lett. 1994;181:39–42. doi: 10.1016/0304-3940(94)90555-X. [DOI] [PubMed] [Google Scholar]
- Kollarik M, Undem B. Activation of bronchopulmonary vagal afferent nerves with bradykinin, acid and vanilloid receptor agonists in wild-type and TRPV1−/−mice. J Physiol. 2004;555:115–123. doi: 10.1113/jphysiol.2003.054890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koltzenburg M, Kress M, Reeh P. The nociceptor sensitization by bradykinin does not depend on sympathetic neurons. Neuroscience. 1992;46:465–473. doi: 10.1016/0306-4522(92)90066-B. [DOI] [PubMed] [Google Scholar]
- Kozaki Y, Kambe F, Hayashi Y, Ohmori S, Seo H, Kumazawa T, Mizumura K. Molecular cloning of prostaglandin EP3 receptors from canine sensory ganglia and their facilitatory action on bradykinin-induced mobilization of intracellular calcium. J Neurochem. 2007;100:1636–1647. doi: 10.1111/j.1471-4159.2006.04320.x. [DOI] [PubMed] [Google Scholar]
- Kumazawa T, Mizumura K. The polymodal C-fiber receptor in the muscle of the dog. Brain Res. 1976;101:589–593. doi: 10.1016/0006-8993(76)90483-2. [DOI] [PubMed] [Google Scholar]
- Kumazawa T, Mizumura K, Minagawa M, Tsujii Y. Sensitizing effects of bradykinin on the heat responses of the visceral nociceptor. J Neurophysiol. 1991;66:1819–1824. doi: 10.1152/jn.1991.66.6.1819. [DOI] [PubMed] [Google Scholar]
- Kwan KY, Allchorne AJ, Vollrath MA, Christensen AP, Zhang D-S, Woolf CJ, Corey DP. TRPA1 contributes to cold, mechanical, and chemical nociception but is not essential for hair-cell transduction. Neuron. 2006;50:277–289. doi: 10.1016/j.neuron.2006.03.042. [DOI] [PubMed] [Google Scholar]
- Kwan KY, Glazer JM, Corey DP, Rice FL, Stucky CL. TRPA1 modulates mechanotransduction in cutaneous sensory neurons. J Neurosci. 2009;29:4808–4819. doi: 10.1523/JNEUROSCI.5380-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrakakis C, Tong CK, Weissman T, Torsney C, MacDermott AB. Localization and function of ATP and GABAA receptors expressed by nociceptors and other postnatal sensory neurons in rat. J Physiol. 2003;549:131–142. doi: 10.1113/jphysiol.2002.031963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang E, Novak A, Reeh P, Handwerker H. Chemosensitivity of fine afferents from rat skin in vitro. J Neurophysiol. 1990;63:887–901. doi: 10.1152/jn.1990.63.4.887. [DOI] [PubMed] [Google Scholar]
- Lee MG, MacGlashan DW, Undem BJ. Role of chloride channels in bradykinin-induced guinea pig airway vagal C-+fibre activation. J Physiol. 2005a;566:205–212. doi: 10.1113/jphysiol.2005.087577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S-Y, Lee J-H, Kang KK, Hwang S-Y, Choi KD, Oh U. Sensitization of vanilloid receptor involves an increase in the phosphorylated form of the channel. Arch Pharm Res. 2005b;28:405–412. doi: 10.1007/BF02977669. [DOI] [PubMed] [Google Scholar]
- Lee B, Cho H, Jung J, Yang YD, Yang DJ, Oh U. Anoctamin 1 contributes to inflammatory and nerve-injury induced hypersensitivity. Mol Pain. 2014;10:5. doi: 10.1186/1744-8069-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lembeck F, Juan H. Interaction of prostaglandins and indomethacin with algesic substances. Naunyn Schmiedebergs Arch Pharmacol. 1974;285:301–313. doi: 10.1007/BF00501460. [DOI] [PubMed] [Google Scholar]
- Lembeck F, Popper H, Juan H. Release of prostaglandins by bradykinin as an intrinsic mechanism of its algesic effect. Naunyn Schmiedebergs Arch Pharmacol. 1976;294:69–73. doi: 10.1007/BF00692786. [DOI] [PubMed] [Google Scholar]
- Leonard PA, Arunkumar R, Brennan TJ. Bradykinin antagonists have no analgesic effect on incisional pain. Anesth Analg. 2004;99:1166–1172. doi: 10.1213/01.ANE.0000130348.85587.BE. [DOI] [PubMed] [Google Scholar]
- Levy D, Zochodne DW. Increased mRNA expression of the B1 and B2 bradykinin receptors and antinociceptive effects of their antagonists in an animal model of neuropathic pain. Pain. 2000;86:265–271. doi: 10.1016/S0304-3959(00)00256-6. [DOI] [PubMed] [Google Scholar]
- Liang YF, Haake B, Reeh PW. Sustained sensitization and recruitment of rat cutaneous nociceptors by bradykinin and a novel theory of its excitatory action. J Physiol. 2001;532:229–239. doi: 10.1111/j.1469-7793.2001.0229g.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebmann C, Graness A, Ludwig B, Adomeit A, Boehmer A, Boehmer F-D, Nürnberg B, Wetzker R. Dual bradykinin B2 receptor signalling in A431 human epidermoid carcinoma cells: activation of protein kinase C is counteracted by a GS-mediated stimulation of the cyclic AMP pathway. Biochem J. 1996;313:109–118. doi: 10.1042/bj3130109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, Linley JE, Du X, Zhang X, Ooi L, Zhang H, Gamper N. The acute nociceptive signals induced by bradykinin in rat sensory neurons are mediated by inhibition of M-type K+ channels and activation of Ca 2+-activated Cl−channels. J Clin Invest. 2010;120:1240–1252. doi: 10.1172/JCI41084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luiz AP, Schroeder SD, Chichorro JG, Calixto JB, Zampronio AR, Rae GA. Kinin B 1 and B 2 receptors contribute to orofacial heat hyperalgesia induced by infraorbital nerve constriction injury in mice and rats. Neuropeptides. 2010;44:87–92. doi: 10.1016/j.npep.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Lukacs V, Thyagarajan B, Varnai P, Balla A, Balla T, Rohacs T. Dual regulation of TRPV1 by phosphoinositides. J Neurosci. 2007;27:7070–7080. doi: 10.1523/JNEUROSCI.1866-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macpherson LJ, Dubin AE, Evans MJ, Marr F, Schultz PG, Cravatt BF, Patapoutian A. Noxious compounds activate TRPA1 ion channels through covalent modification of cysteines. Nature. 2007;445:541–545. doi: 10.1038/nature05544. [DOI] [PubMed] [Google Scholar]
- Manning DC, Raja SN, Meyer RA, Campbell JN. Pain and hyperalgesia after intradermal injection of bradykinin in humans. Clin Pharmacol Ther. 1991;50:721–729. doi: 10.1038/clpt.1991.212. [DOI] [PubMed] [Google Scholar]
- Materazzi S, Nassini R, Andrè E, Campi B, Amadesi S, Trevisani M, Bunnett NW, Patacchini R, Geppetti P. Cox-dependent fatty acid metabolites cause pain through activation of the irritant receptor TRPA1. Proc Natl Acad Sci USA. 2008;105:12045–12050. doi: 10.1073/pnas.0802354105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathivanan S, Devesa I, Changeux JP, Ferrer-Montiel A. Bradykinin induces TRPV1 exocytotic recruitment in peptidergic nociceptors. Front Pharmacol. 2016;7:178. doi: 10.3389/fphar.2016.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maubach KA, Grundy D. The role of prostaglandins in the bradykinin-induced activation of serosal afferents of the rat jejunum in vitro. J Physiol. 1999;515:277–285. doi: 10.1111/j.1469-7793.1999.277ad.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer S, Izydorczyk I, Reeh PW, Grubb BD. Bradykinin-induced nociceptor sensitisation to heat depends on cox-1 and cox-2 in isolated rat skin. Pain. 2007;130:14–24. doi: 10.1016/j.pain.2006.10.027. [DOI] [PubMed] [Google Scholar]
- Mcgehee DS, Oxford GS. Bradykinin modulates the electrophysiology of cultured rat sensory neurons through a pertussis toxin-insensitive G protein. Mol Cell Neurosci. 1991;2:21–30. doi: 10.1016/1044-7431(91)90036-N. [DOI] [PubMed] [Google Scholar]
- McGuirk S, Dolphin A. G-protein mediation in nociceptive signal transduction: an investigation into the excitatory action of bradykinin in a subpopulation of cultured rat sensory neurons. Neuroscience. 1992;49:117–128. doi: 10.1016/0306-4522(92)90079-H. [DOI] [PubMed] [Google Scholar]
- McGuirk S, Vallis Y, Pasternak C, Dolphin A. Bradykinin enhances excitability in cultured rat sensory neurones by a GTP-dependent mechanisms. Neurosci Lett. 1989;99:85–89. doi: 10.1016/0304-3940(89)90269-3. [DOI] [PubMed] [Google Scholar]
- Meotti FC, Figueiredo CP, Manjavachi M, Calixto JB. The transient receptor potential ankyrin-1 mediates mechanical hyperalgesia induced by the activation of B1 receptor in mice. Biochem Pharmacol. 2017;125:75–83. doi: 10.1016/j.bcp.2016.11.003. [DOI] [PubMed] [Google Scholar]
- Meyer RA, Davis KD, Raja SN, Campbell JN. Sympathectomy does not abolish bradykinin-induced cutaneous hyperalgesia in man. Pain. 1992;51:323–327. doi: 10.1016/0304-3959(92)90217-Y. [DOI] [PubMed] [Google Scholar]
- Mizumura K, Koda H, Kumazawa T. Evidence that protein kinase C activation is involved in the excitatory and facilitatory effects of bradykinin on canine visceral nociceptors in vitro. Neurosci Lett. 1997;237:29–32. doi: 10.1016/S0304-3940(97)00793-3. [DOI] [PubMed] [Google Scholar]
- Mizumura K, Sato J, Kumazawa T. Effects of prostaglandins and other putative chemical intermediaries on the activity of canine testicular polymodal receptors studied in vitro. Pflugers Arch. 1987;408:565–572. doi: 10.1007/BF00581157. [DOI] [PubMed] [Google Scholar]
- Mizumura K, Sugiura T, Katanosaka K, Banik RK, Kozaki Y. Excitation and sensitization of nociceptors by bradykinin: what do we know? Exp Brain Res. 2009;196:53–65. doi: 10.1007/s00221-009-1814-5. [DOI] [PubMed] [Google Scholar]
- Moriyama T, Higashi T, Togashi K, Iida T, Segi E, Sugimoto Y, Tominaga T, Narumiya S, Tominaga M. Sensitization of TRPV1 by EP 1 and IP reveals peripheral nociceptive mechanism of prostaglandins. Mol Pain. 2005;1:3. doi: 10.1186/1744-8069-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura A, Fujita M, Shiomi H. Involvement of endogenous nitric oxide in the mechanism of bradykinin-induced peripheral hyperalgesia. Br J Pharmacol. 1996;117:407–412. doi: 10.1111/j.1476-5381.1996.tb15205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Numazaki M, Tominaga T, Toyooka H, Tominaga M. Direct phosphorylation of capsaicin receptor VR1 by protein kinase Cε and identification of two target serine residues. J Biol Chem. 2002;277:13375–13378. doi: 10.1074/jbc.C200104200. [DOI] [PubMed] [Google Scholar]
- Oh EJ, Weinreich D. Bradykinin decreases K+ and increases Cl− conductances in vagal afferent neurones of the guinea pig. J Physiol. 2004;558:513–526. doi: 10.1113/jphysiol.2004.066381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshita K, Inoue A, Tang H-B, Nakata Y, Kawamoto M, Yuge O. CB1 cannabinoid receptor stimulation modulates transient receptor potential vanilloid receptor 1 activities in calcium influx and substance P release in cultured rat dorsal root ganglion cells. J Pharmacol Sci. 2005;97:377–385. doi: 10.1254/jphs.FP0040872. [DOI] [PubMed] [Google Scholar]
- Pan H-L, Chen S-R. Sensing tissue ischemia. Circulation. 2004;110:1826–1831. doi: 10.1161/01.CIR.0000142618.20278.7A. [DOI] [PubMed] [Google Scholar]
- Patapoutian A, Tate S, Woolf CJ. Transient receptor potential channels: targeting pain at the source. Nat Rev Drug Discov. 2009;8:55–68. doi: 10.1038/nrd2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris M, Hockley JR, Reed DE, Smith ESJ, Bulmer DC, Blackshaw LA. Peripheral KV7 channels regulate visceral sensory function in mouse and human colon. Mol Pain. 2017;13 doi: 10.1177/1744806917709371. 1744806917709371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins M, Kelly D. Induction of bradykinin B1 receptors in vivo in a model of ultra-violet irradiation-induced thermal hyperalgesia in the rat. Br J Pharmacol. 1993;110:1441–1444. doi: 10.1111/j.1476-5381.1993.tb13982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins MN, Campbell E, Dray A. Antinociceptive activity of the bradykinin B1 and B2 receptor antagonists, des-Arg 9,[Leu 8]-BK and HOE 140, in two models of persistent hyperalgesia in the rat. Pain. 1993;53:191–197. doi: 10.1016/0304-3959(93)90080-9. [DOI] [PubMed] [Google Scholar]
- Petcu M, Dias J, Ongali B, Thibault G, Neugebauer W, Couture R. Role of kinin B1 and B2 receptors in a rat model of neuropathic pain. Int Immunopharmacol. 2008;8:188–196. doi: 10.1016/j.intimp.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Pethö G, Derow A, Reeh PW. Bradykinin-induced nociceptor sensitization to heat is mediated by cyclooxygenase products in isolated rat skin. Eur J Neurosci. 2001;14:210–218. doi: 10.1046/j.0953-816x.2001.01651.x. [DOI] [PubMed] [Google Scholar]
- Petho G, Reeh PW. Sensory and signaling mechanisms of bradykinin, eicosanoids, platelet-activating factor, and nitric oxide in peripheral nociceptors. Physiol Rev. 2012;92:1699–1775. doi: 10.1152/physrev.00048.2010. [DOI] [PubMed] [Google Scholar]
- Petrus M, Peier AM, Bandell M, Hwang SW, Huynh T, Olney N, Jegla T, Patapoutian A. A role of TRPA1 in mechanical hyperalgesia is revealed by pharmacological inhibition. Mol Pain. 2007;3:40. doi: 10.1186/1744-8069-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole S, Lorenzetti B, Cunha J, Cunha F, Ferreira S. Bradykinin B1 and B2 receptors, tumour necrosis factor α and inflammatory hyperalgesia. Br J Pharmacol. 1999;126:649–656. doi: 10.1038/sj.bjp.0702347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porreca F, Vanderah TW, Guo W, Barth M, Dodey P, Peyrou V, Luccarini J, Junien J-L, Pruneau D. Antinociceptive pharmacology of N-[[4-(4, 5-dihydro-1H-imidazol-2-yl) phenyl] methyl]-2-[2-[[(4-methoxy-2, 6-dimethylphenyl) sulfonyl] methylamino] ethoxy]-N-methylacetamide, fumarate (LF22-0542), a novel nonpeptidic bradykinin B1 receptor antagonist. J Pharmacol Exp Ther. 2006;318:195–205. doi: 10.1124/jpet.105.098368. [DOI] [PubMed] [Google Scholar]
- Premkumar LS, Ahern GP. Induction of vanilloid receptor channel activity by protein kinase C. Nature. 2000;408:985–990. doi: 10.1038/35050121. [DOI] [PubMed] [Google Scholar]
- Prescott ED, Julius D. A modular PIP2 binding site as a determinant of capsaicin receptor sensitivity. Science. 2003;300:1284–1288. doi: 10.1126/science.1083646. [DOI] [PubMed] [Google Scholar]
- Price TJ, Cervero F, Gold MS, Hammond DL, Prescott SA. Chloride regulation in the pain pathway. Brain Res Rev. 2009;60:149–170. doi: 10.1016/j.brainresrev.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C, Farber JP, Miller KE, Foreman RD. Responses of thoracic spinal neurons to activation and desensitization of cardiac TRPV1-containing afferents in rats. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1700–R1707. doi: 10.1152/ajpregu.00231.2006. [DOI] [PubMed] [Google Scholar]
- Quintão NL, Passos GF, Medeiros R, Paszcuk AF, Motta FL, Pesquero JB, Campos MM, Calixto JB. Neuropathic pain-like behavior after brachial plexus avulsion in mice: the relevance of kinin B1 and B2 receptors. J Neurosci. 2008;28:2856–2863. doi: 10.1523/JNEUROSCI.4389-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rang H, Ritchie J. Depolarization of nonmyelinated fibers of the rat vagus nerve produced by activation of protein kinase C. J Neurosci. 1988;8:2606–2617. doi: 10.1523/JNEUROSCI.08-07-02606.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeh PW, Pethö G. Nociceptor excitation by thermal sensitization—a hypothesis. Prog Brain Res. 2000;129:39–50. doi: 10.1016/S0079-6123(00)29004-3. [DOI] [PubMed] [Google Scholar]
- Rong W, Hillsley K, Davis JB, Hicks G, Winchester WJ, Grundy D. Jejunal afferent nerve sensitivity in wild-type and TRPV1 knockout mice. J Physiol. 2004;560:867–881. doi: 10.1113/jphysiol.2004.071746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueff A, Dray A. Sensitization of peripheral afferent fibres in the in vitro neonatal rat spinal cord-tail by bradykinin and prostaglandins. Neuroscience. 1993;54:527–535. doi: 10.1016/0306-4522(93)90272-H. [DOI] [PubMed] [Google Scholar]
- Rupniak NM, Boyce S, Webb JK, Williams AR, Carlson EJ, Hill RG, Borkowski JA, Hess JF. Effects of the bradykinin B 1 receptor antagonist des-Arg 9 [Leu 8] bradykinin and genetic disruption of the B2 receptor on nociception in rats and mice. Pain. 1997;71:89–97. doi: 10.1016/S0304-3959(97)03343-5. [DOI] [PubMed] [Google Scholar]
- Sauer S, Schäfer D, Kress M, Reeh P. Stimulated prostaglandin E 2 release from rat skin, in vitro. Life Sci. 1998;62:2045–2055. doi: 10.1016/S0024-3205(98)00176-3. [DOI] [PubMed] [Google Scholar]
- Sauer SK, Averbeck B, Reeh PW. Denervation and NKI receptor block modulate stimulated CGRP and PGE2 release from rat skin. Neuroreport. 2000;11:283–286. doi: 10.1097/00001756-200002070-00012. [DOI] [PubMed] [Google Scholar]
- Schuligoi R, Donnerer J, Amann R. Bradykinin-induced sensitization of afferent neurons in the rat paw. Neuroscience. 1994;59:211–215. doi: 10.1016/0306-4522(94)90111-2. [DOI] [PubMed] [Google Scholar]
- Shin J, Cho H, Hwang SW, Jung J, Shin CY, Lee S-Y, Kim SH, Lee MG, Choi YH, Kim J. Bradykinin-12-lipoxygenase-VR1 signaling pathway for inflammatory hyperalgesia. Proc Natl Acad Sci USA. 2002;99:10150–10155. doi: 10.1073/pnas.152002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song I, Althoff C, Hermann K, Scheel A, Knetsch T, Burmester G, Backhaus M. Contrast-enhanced ultrasound in monitoring the efficacy of a bradykinin receptor 2 antagonist in painful knee osteoarthritis compared with MRI. Ann Rheum Dis. 2008;68:75–83. doi: 10.1136/ard.2007.080382. [DOI] [PubMed] [Google Scholar]
- Soukhova-O’Hare GK, Zhang JW, Gozal D, Yu J. Bradykinin B 2 receptors mediate pulmonary sympathetic afferents induced reflexes in rabbits. Life Sci. 2006;78:1990–1997. doi: 10.1016/j.lfs.2005.08.035. [DOI] [PubMed] [Google Scholar]
- Staruschenko A, Jeske NA, Akopian AN. Contribution of TRPV1-TRPA1 interaction to the single channel properties of the TRPA1 channel. J Biol Chem. 2010;285:15167–15177. doi: 10.1074/jbc.M110.106153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steranka LR, Manning DC, DeHaas CJ, Ferkany JW, Borosky SA, Connor JR, Vavrek RJ, Stewart JM, Snyder SH. Bradykinin as a pain mediator: receptors are localized to sensory neurons, and antagonists have analgesic actions. Proc Natl Acad Sci USA. 1988;85:3245–3249. doi: 10.1073/pnas.85.9.3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens PA, Pyne S, Grady M, Pyne NJ. Bradykinin-dependent activation of adenylate cyclase activity and cyclic AMP accumulation in tracheal smooth muscle occurs via protein kinase C-dependent and-independent pathways. Biochem J. 1994;297:233–239. doi: 10.1042/bj2970233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stucky C, Abrahams L, Seybold V. Bradykinin increases the proportion of neonatal rat dorsal root ganglion neurons that respond to capsaicin and protons. Neuroscience. 1998;84:1257–1265. doi: 10.1016/S0306-4522(97)00572-1. [DOI] [PubMed] [Google Scholar]
- Sugiura T, Tominaga M, Katsuya H, Mizumura K. Bradykinin lowers the threshold temperature for heat activation of vanilloid receptor 1. J Neurophysiol. 2002;88:544–548. doi: 10.1152/jn.2002.88.1.544. [DOI] [PubMed] [Google Scholar]
- Sung K-W, Kirby M, McDonald MP, Lovinger DM, Delpire E. Abnormal GABAA receptor-mediated currents in dorsal root ganglion neurons isolated from Na−K−2Cl cotransporter null mice. J Neurosci. 2000;20:7531–7538. doi: 10.1523/JNEUROSCI.20-20-07531.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taiwo Y, Heller P, Levine J. Characterization of distinct phospholipases mediating bradykinin and noradrenaline hyperalgesia. Neuroscience. 1990;39:523–531. doi: 10.1016/0306-4522(90)90288-F. [DOI] [PubMed] [Google Scholar]
- Taiwo YO, Levine JD. Characterization of the arachidonic acid metabolites mediating bradykinin and noradrenaline hyperalgesia. Brain Res. 1988;458:402–406. doi: 10.1016/0006-8993(88)90487-8. [DOI] [PubMed] [Google Scholar]
- Tang H-B, Inoue A, Oshita K, Hirate K, Nakata Y. Zaltoprofen inhibits bradykinin-induced responses by blocking the activation of second messenger signaling cascades in rat dorsal root ganglion cells. Neuropharmacology. 2005;48:1035–1042. doi: 10.1016/j.neuropharm.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Tang H-B, Inoue A, Oshita K, Nakata Y. Sensitization of vanilloid receptor 1 induced by bradykinin via the activation of second messenger signaling cascades in rat primary afferent neurons. Eur J Pharmacol. 2004;498:37–43. doi: 10.1016/j.ejphar.2004.07.076. [DOI] [PubMed] [Google Scholar]
- Tang HB, Inoue A, Iwasa M, Hide I, Nakata Y. Substance P release evoked by capsaicin or potassium from rat cultured dorsal root ganglion neurons is conversely modulated with bradykinin. J Neurochem. 2006;97:1412–1418. doi: 10.1111/j.1471-4159.2006.03830.x. [DOI] [PubMed] [Google Scholar]
- Thayer SA, Perney TM, Miller RJ. Regulation of calcium homeostasis in sensory neurons by bradykinin. J Neurosci. 1988;8:4089–4097. doi: 10.1523/JNEUROSCI.08-11-04089.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasko M, Campbell W, Waite K. Prostaglandin E2 enhances bradykinin-stimulated release of neuropeptides from rat sensory neurons in culture. J Neurosci. 1994;14:4987–4997. doi: 10.1523/JNEUROSCI.14-08-04987.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn AH, Gold MS. Ionic mechanisms underlying inflammatory mediator-induced sensitization of dural afferents. J Neurosci. 2010;30:7878–7888. doi: 10.1523/JNEUROSCI.6053-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellani V, Mapplebeck S, Moriondo A, Davis JB, McNaughton PA. Protein kinase C activation potentiates gating of the vanilloid receptor VR1 by capsaicin, protons, heat and anandamide. J Physiol. 2001;534:813–825. doi: 10.1111/j.1469-7793.2001.00813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellani V, Zachrisson O, McNaughton PA. Functional bradykinin B1 receptors are expressed in nociceptive neurones and are upregulated by the neurotrophin GDNF. J Physiol. 2004;560:391–401. doi: 10.1113/jphysiol.2004.067462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voets T, Droogmans G, Wissenbach U, Janssens A, Flockerzi V, Nilius B. The principle of temperature-dependent gating in cold-and heat-sensitive TRP channels. Nature. 2004;430:748–754. doi: 10.1038/nature02732. [DOI] [PubMed] [Google Scholar]
- Vyklický L, Vlachova V, Vitaskova Z, Dittert I, Kabat M, Orkand R. Temperature coefficient of membrane currents induced by noxious heat in sensory neurones in the rat. J Physiol. 1999;517:181–192. doi: 10.1111/j.1469-7793.1999.0181z.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter T, Chau T, Weichman B. Effects of analgesics on bradykinin-induced writhing in mice presensitized with PGE 2. Agents Actions. 1989;27:375–377. doi: 10.1007/BF01972826. [DOI] [PubMed] [Google Scholar]
- Wang MM, Reynaud D, Pace-Asciak CR. In vivo stimulation of 12(S)-lipoxygenase in the rat skin by bradykinin and platelet activating factor: formation of 12(S)-HETE and hepoxilins, and actions on vascular permeability. Biochim Biophys Acta. 1999;1436:354–362. doi: 10.1016/S0005-2760(98)00128-3. [DOI] [PubMed] [Google Scholar]
- Wang S, Dai Y, Fukuoka T, Yamanaka H, Kobayashi K, Obata K, Cui X, Tominaga M, Noguchi K. Phospholipase C and protein kinase A mediate bradykinin sensitization of TRPA1: a molecular mechanism of inflammatory pain. Brain. 2008;131:1241–1251. doi: 10.1093/brain/awn060. [DOI] [PubMed] [Google Scholar]
- Wang S, Joseph J, Ro JY, Chung MK. Modality-specific mechanisms of protein kinase C-induced hypersensitivity of TRPV1: S800 is a polymodal sensitization site. Pain. 2015;156:931–941. doi: 10.1097/j.pain.0000000000000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreich D, Koschorke G, Undem B, Taylor G. Prevention of the excitatory actions of bradykinin by inhibition of PGI2 formation in nodose neurones of the guinea-pig. J Physiol. 1995;483:735–746. doi: 10.1113/jphysiol.1995.sp020618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreich D, Wonderlin W. Inhibition of calcium-dependent spike after-hyperpolarization increases excitability of rabbit visceral sensory neurones. J Physiol. 1987;394:415–427. doi: 10.1113/jphysiol.1987.sp016878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng H-J, Patel KN, Jeske NA, Bierbower SM, Zou W, Tiwari V, Zheng Q, Tang Z, Mo GC, Wang Y. Tmem100 is a regulator of TRPA1-TRPV1 complex and contributes to persistent pain. Neuron. 2015;85:833–846. doi: 10.1016/j.neuron.2014.12.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whalley E, Clegg S, Stewart J, Vavrek R. The effect of kinin agonists and antagonists on the pain response of the human blister base. Naunyn Schmiedebergs Arch Pharmacol. 1987;336:652–655. doi: 10.1007/BF00165756. [DOI] [PubMed] [Google Scholar]
- Wu Z-Z, Pan H-L. Role of TRPV1 and intracellular Ca2+ in excitation of cardiac sensory neurons by bradykinin. Am J Physiol Regul Integr Comp Physiol. 2007;293:R276–R283. doi: 10.1152/ajpregu.00094.2007. [DOI] [PubMed] [Google Scholar]
- Yamaguchi-Sase S, Hayashi I, Okamoto H, Nara Y, Matsuzaki S, Hoka S, Majima M. Amelioration of hyperalgesia by kinin receptor antagonists or kininogen deficiency in chronic constriction nerve injury in rats. Inflamm Res. 2003;52:164–169. doi: 10.1007/s000110300067. [DOI] [PubMed] [Google Scholar]
- Yanaga F, Hirata M, Koga T. Evidence for coupling of bradykinin receptors to a guanine-nucleotide binding protein to stimulate arachidonate liberation in the osteoblast-like cell line, MC3T3-E1. Biochim Biophys Acta. 1991;1094:139–146. doi: 10.1016/0167-4889(91)90001-E. [DOI] [PubMed] [Google Scholar]
- Yu S, Ouyang A. TRPA1 in bradykinin-induced mechanical hypersensitivity of vagal C fibers in guinea pig esophagus. Am J Physiol Gastrointest Liver Physiol. 2009;296:G255–G265. doi: 10.1152/ajpgi.90530.2008. [DOI] [PubMed] [Google Scholar]
- Zahner MR, Li DP, Chen SR, Pan HL. Cardiac vanilloid receptor 1-expressing afferent nerves and their role in the cardiogenic sympathetic reflex in rats. J Physiol. 2003;551:515–523. doi: 10.1113/jphysiol.2003.048207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Li L, McNaughton PA. Proinflammatory mediators modulate the heat-activated ion channel TRPV1 via the scaffolding protein AKAP79/150. Neuron. 2008;59:450–461. doi: 10.1016/j.neuron.2008.05.015. [DOI] [PubMed] [Google Scholar]
- Zylka MJ, Rice FL, Anderson DJ. Topographically distinct epidermal nociceptive circuits revealed by axonal tracers targeted to Mrgprd. Neuron. 2005;45:17–25. doi: 10.1016/j.neuron.2004.12.015. [DOI] [PubMed] [Google Scholar]