Abstract
The recently released 2013 ACC/AHA guidelines for management of blood cholesterol have substantially increased the number of adults who are eligible for preventive statin therapy. We sought to determine whether eligibility for statin therapy as determined by the 2013 ACC/AHA guideline recommendation is better aligned with the actual presence of coronary artery disease (CAD) as detected by coronary CT angiography (CCTA) when compared to prior guidelines including the 2004 NCEP ATP III and 2011 ESC/EAS guidelines.
In this secondary analysis of the prospective observational ROMICAT I (Rule Out Myocardial Infarction with Computer Assisted Tomography) cohort study, we included all men and women aged 40–79 years presenting with acute chest pain but not diagnosed with acute coronary syndrome nor on admission statin. Based on risk factor assessment and lipid data, we determined guideline-based eligibility for statin therapy by the 2013 ACC/AHA, the 2004 NCEP ATP II, and the 2011 ESC/EAS guidelines. We determined the presence and severity of CAD as detected by CCTA.
The 2013 ACC/AHA algorithm identified nearly twice as many individuals as eligible for statins (n=77/189; 41%) as compared to the 2004 ATPIII criteria: (n=41/189; 22%), (P<.0001) In addition, the 2013 ACC/AHA guidelines were more sensitive for treatment of CCTA-detected CAD than the 2004 ATP III guidelines [53.4% (42.5–64.1) vs 27.3% (18.3–37.8), p<.001] and the 2011 ESC/EAE guidelines [53.4% (42.5–64.1) vs 34.1% (24.3–45.0), p<.001]. However, the specificity of these guidelines was modestly reduced compared to the 2004 ATP III guidelines [70.3 (60.4–79.0) vs 83.2 (74.4–89.9), p<.001] and the 2011 ESC/EAE guidelines [70.3 (60.4–79.0) vs 86.1 (77.8–92.2), p<.001], suggesting increased treatment of subjects without CCTA-detected CAD. Overall, the 2013 ACC/AHA guidelines are more sensitive to identify patients who have CAD detected by CCTA eligible for statin therapy as compared with prior guidelines, with an acceptable trade-off in specificity for recommending statin therapy in those without CAD.
Keywords: prevention, guidelines, atherosclerosis, computed tomography, statin
Introduction
The recently released 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for management of blood cholesterol represent a shift in the treatment paradigm for primary prevention of cardiovascular disease.1,2 In comparison to the 2004 Adult Treatment Panel III Update (ATPIII), the ACC/AHA guidelines focus more on treating absolute cardiovascular risk by estimating 10-year atherosclerotic cardiovascular disease (ASCVD), as opposed to substantial reliance on risk-based low-density lipoprotein (LDL) thresholds for treatment. 3
Despite a more simplified approach to preventive therapy, significant controversy has surrounded the new cholesterol guidelines and the associated risk estimation tool. 4,5 Foremost, there has been concern as to whether the 2013 ACC/AHA blood cholesterol guidelines have set too low an absolute 10-year ASCVD risk threshold for eligibility of statin therapy. Furthermore, there has been concern regarding calibration of the new risk estimation tool when applied to other primary prevention cohorts.6 These concerns have resulted in discrepant viewpoints regarding adoption of the new cholesterol guidelines for initiating statin therapy. 7
The presence and extent of coronary artery disease (CAD) detected by coronary CT angiography (CCTA) is an excellent predictor of future cardiovascular events.8 Hence, we sought to evaluate the alignment of the 2004 ATPIII and 2013 ACC/AHA guideline recommendations for statin therapy with the presence of CAD as detected by CCTA in patients presenting with acute chest pain (ACP) in whom acute coronary syndrome (ACS) was excluded. We hypothesized that the 2013 ACC/AHA guidelines because of their focus on absolute cardiac risk would improve alignment of the recommendation for statin with the presence of CAD as detected by CCTA compared to the 2004 ATPIII guidelines.
Methods
Design, Setting and Participants
We utilized a well-characterized, previously described patient cohort from the Rule Out Myocardial Infarction with Computer Assisted Tomography (ROMICAT I) trial.9 In this prospective observational cohort study, patients (n=368, 53±12yrs, 61% male) who presented to the Emergency Department (ED) without a prior history of CAD or objective signs of myocardial ischemia or necrosis underwent CCTA after negative initial troponin.
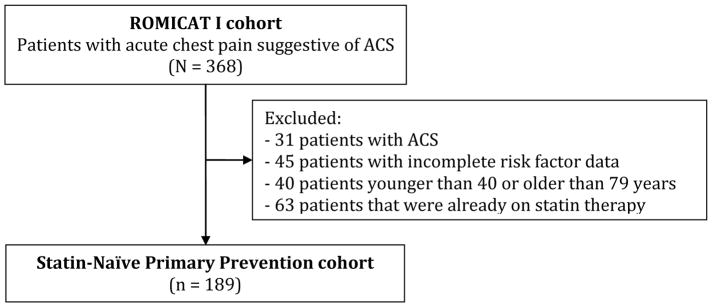
For this analysis, only patients who were diagnosed by their care-providers to have non-cardiac cause of chest pain, and thus subject to application of primary prevention guidelines, were included. (Figure 1) Patients ultimately diagnosed with ACS were excluded since these patients would be subject to secondary prevention initiatives. Those with incomplete risk factor data to determine guideline-based candidacy for statin were excluded. Also, subjects that were not between the ages of 40 and 79 years, and those on statins at the time of ED presentation were excluded.
Figure 1. Study Flow Diagram.
The original ROMICAT I (Rule out Myocardial Infarction with Computer-Assisted Tomography) consisted of 368 low-intermediate risk patients presenting with symptoms suggestive of acute coronary syndrome (ACS) to the ED. Patients with ACS, incomplete risk factor data, and patients that were already on statin therapy were excluded to generate the “primary prevention” cohort of patients (n=189).
Risk Factors and Guideline-Based Candidacy for Initiating/Intensifying Statin Therapy
Risk Factors
Risk factors were assessed at the time of subject enrollment, based on self-report as well as review of medical records for the index hospitalization. Hypertension was defined as a systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg or current anti-hypertensive treatment. Diabetes mellitus was defined as a fasting plasma glucose >=126 or treatment with a hypoglycemic agent. Peripheral vascular disease was defined as having a history transient ischemic attack, cerebrovascular event, or peripheral arterial disease. Family history of CAD was defined as having a first-degree female (<65 years of age) or male (<55 years of age) relative with a documented history of myocardial infarction or sudden cardiac death. Subjects were classified as smokers if they had smoked at least 1 cigarette per day in the year before the study. Lipid profiles were collected as part of the study protocol, and complete lipid data was available in 341/368 (93%) of patients.
2004 ATPIII Guidelines
To assess whether primary prevention statin was indicated per the 2004 Updated Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III), we applied the algorithm based on risk factors, Framingham risk score, and LDL-cutoff levels. 3,10
2013 ACC/AHA Guidelines
For the 2013 ACC/AHA guidelines, we identified candidates for statin based on four delineated benefit groups outlined in the document: (1) clinical ASCVD, (2) LDL≥190 mg/dl, (3) diabetes 40–75 years and LDL 70–189 mg/dl, or (4) without clinical ASCVD or diabetes, LDL 70–189 mg/dl, and estimated ASCVD risk ≥7.5%. ASCVD risk was determined using the pooled cohort calculator.
2013 ACC/AHA Guidelines Using Pooled Cohort Calculator 5% Threshold
In addition, we performed an analysis evaluating in addition to above the “optional” Class IIa recommendation for statin therapy in those without clinical ASCVD or diabetes, LDL 70–189, and estimated ASCVD risk of between 5%–7.5%.
2011 European Prevention Guidelines
To determine eligibility for statin therapy we applied the respective algorithm as delineated in the 2011 European Prevention Guidelines, which takes into account risk factors and the European SCORE risk based on the HeartScore calculator. The SCORE is a 10-year risk of fatal CVD based upon smoking status, systolic blood pressure, total and HDL cholesterol, and gender. 11,12
Coronary CT Angiography (CCTA)
The CCTA protocol in the ROMICAT I study has previously been described. 9 Briefly, this was performed using a 64-slice CT scanner (Sensation 64, Siemens Medical Solutions, Forchheim, Germany). CCTA results were blinded to care-providers, and patients were managed according to standard-of-care. CCTA-detected CAD was categorized as none, non-obstructive (<50% stenosis), or obstructive (≥50% stenosis).
Statistical Analysis
Continuous variables were expressed as mean +/− standard deviation or median (inter-quartile range); categorical variables were described by frequency. McNemar’s test was used to compare paired proportions within strata of CCTA-detected CAD. Fisher’s exact test was used to compare proportion of patients “upgraded” to statin eligibility from the 2004 ATPIII to the 2013 ACC/AHA guidelines between strata of CCTA-detected CAD. For analysis of diagnostic characteristics such as sensitivity and specificity of guideline eligibility for treatment of CCTA-detected CAD, we grouped patients with non-obstructive and obstructive CAD together as having CAD. We used the balanced accuracy = (sensitivity + specificity)/2 as a summary measure of alignment between guideline-based statin eligibility and CCTA-detected CAD. McNemar’s test was used for comparisons of sensitivity and specificity. The Delong algorithm was used for the comparison of balanced accuracies. 13 All analyses were performed using Stata (Version 13.1, StatCorp, College Station, Texas).
Results
Of the 368 patients in the ROMICAT I cohort, we excluded 31 who were diagnosed with ACS on index hospitalization, 45 with incomplete risk factor data, 40 outside the age of 40–79 years, and 63 with admission statin use. Baseline characteristics of the final cohort of 189 subjects are as shown. (Table 1) The mean age of the cohort was 53 ± 9.2 years and was 43% female.
Table 1.
Baseline Demographics and Risk Factors
| Total (n=189) | |
|---|---|
| Age (years), mean ± SD | 53.3 ± 9.2 |
| Women, n (%) | 82 (43.4) |
| Current smoker, n (%) | 55 (29.1) |
| Hypertension, n (%) | 68 (36.0) |
| Diabetes mellitus, n (%) | 15 (7.9) |
| Peripheral Vascular Disease, n (%) | 4 (2.1) |
| Lipid Profile | |
| LDL, mean ± SD | 120.8 ± 36.6 |
| HDL, mean ± SD | 52.9 ± 13.9 |
| Total Cholesterol, mean ± SD | 201.3 ± 40.2 |
| Triglycerides, median (IQR) | 118.7 (85.9–173.6) |
| Framingham Risk Score (10 year CVD risk), median (IQR) | 4.9 (2.1–9.7) |
| 10-year ASCVD Risk Score, median (IQR) | 5.7 (2.8–11.4) |
| 10-year European CVD Risk Score, median (IQR) | 2.0 (1.0–3.0) |
Stratifying subjects by the presence and severity of CAD detected by CCTA, 101 (53%) patients had no CAD, 68 (36%) had non-obstructive CAD, and 20 (11%) had obstructive CAD. The 2013 ACC/AHA algorithm identified nearly twice as many individuals as eligible for statins (n=77/189; 41%) as compared to the 2004 ATPIII criteria (n=41/189; 22%), (P<.0001).
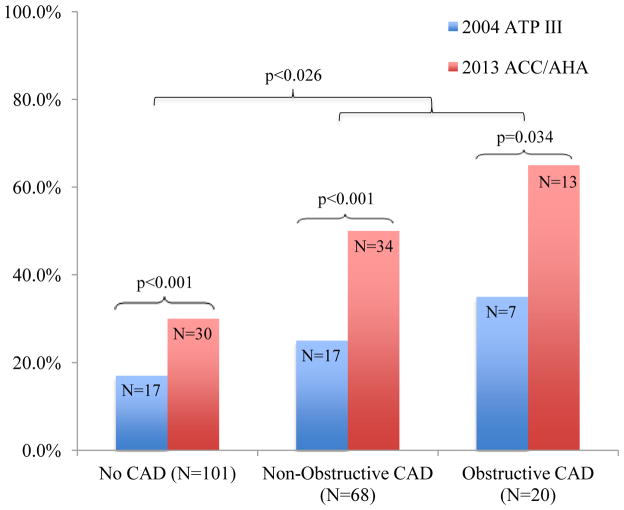
We found that among patients with CAD a higher proportion qualified for statin therapy using the 2013 ACC/AHA algorithm as compared to 2004 ATPIII criteria (p=.026) (Figure 2). Of note, the sensitivity of the 2013 ACC/AHA guidelines for treatment of CCTA-detected CAD was significantly higher than the 2004 ATP III guidelines: 53.4% (42.5–64.1) versus 27.3% (18.3–37.8), respectively; p<.001. This was at the expense of a modest drop in specificity: 70.3% (60.4–79.0) for the 2013 ACC/AHA guidelines versus 83.2%(74.4–89.9) for the ATP III guidelines (p<.001). In addition, our measure of overall alignment, the balanced accuracy, was significant higher with 2013 ACC/AHA guidelines compared to the 2004 ATP III guidelines: 61.9%(55.0–68.7) versus 55.2%(49.3–61.2), p=.03. (Table 2)
Figure 2.
2013 ACC/AHA versus 2004 ATP III Guidelines on Statin Recommendation across strata of presence and extent of coronary atherosclerosis as detected by CCTA in 189 patients without prior statin use presenting with acute chest pain in whom an acute coronary syndrome was excluded.
Table 2.
Diagnostic characteristics of Guideline-Based Statin Eligibility for CCTA-Detected CAD
| Sensitivity | Specificity | PPV | NPV | Balanced Accuracy* | |
|---|---|---|---|---|---|
| 2004 ATP III | 27.3 (18.3–37.8) |
83.2 (74.4–89.9) |
58.5 (42.1–73.7) |
56.8 (48.4–64.9) |
55.2 (49.3–61.2) |
|
2013 ACC/AHA (7.5%) |
53.4 (42.5–64.1) |
70.3 (60.4–79.0) |
61.0 (49.2–72.0) |
63.4 (53.8–72.3) |
61.9 (55.0–68.7) |
|
2013 ACC/AHA (5%) |
71.6 (61.0–80.7) |
61.4 (51.2–70.9) |
61.8 (51.6–71.2) |
71.3 (60.6–80.5) |
66.5 (59.8–73.2) |
| 2011 European | 34.1 (24.3–45.0) |
86.1 (77.8–92.2) |
68.2 (52.4–81.4) |
60.0 (51.5–68.0) |
60.1 (54.1–66.1) |
95% Confidence Intervals are in brackets;
Balanced Accuracy = Area under the receiver operating characteristic curve = (Sensitivity + Specificity)/2
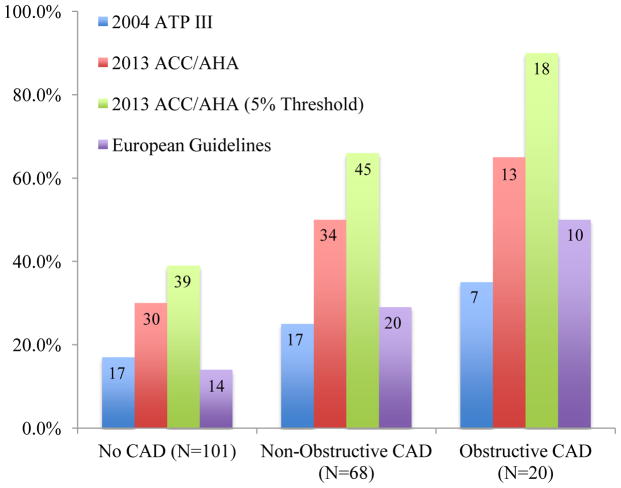
ACC/AHA Guidelines with optional 5% Threshold
Applying the ACC/AHA 2013 guidelines with the optional Class IIa recommendation of a risk threshold of 5% (instead of 7.5%), we found an even higher sensitivity of 71.6% (61.0–80.7), at the expense of a further decrease in specificity to 61.4% (49.2–72.0) compared to 2004 ATP III guidelines (p<.001). The alignment was significantly improved using the ACC/AHA 2013 (5% threshold) versus the 2004 ATP III guidelines: 66.5%(59.8–73.2) versus 55.2%(49.3–61.2), p<.001.
ESC/EAS (European) Guidelines
We also assessed the European ESC/EAS guidelines and found that applying these, the sensitivity for treatment of CCTA-detected CAD was 34.1% (24.3–45.0) and the specificity was 86.1% (77.8–92.2) which were not significantly different compared to the 2004 ATP III guidelines (p=.180 and p=.439, respectively). The overall alignment was also not significantly different from the 2004 ATP III guidelines: 60.1%(54.1–66.1) versus 55.2%(49.3–61.2), p=.12.
Discussion
Overall, our findings suggest that the 2013 ACC/AHA guidelines result in improved alignment of statin eligibility with the presence and extent of CCTA-detected CAD in patients presenting with ACP in whom ACS was excluded and who therefore are eligible for primary prevention. The sensitivity of these guidelines for the treatment of CCTA-detected CAD was significantly higher than that imparted by application of the 2004 ATPIII guidelines or the 2011 ESC/EAS guidelines. This occurred at the expense of a relatively modest reduction in specificity, that is the treatment of those patients with no evidence of CCTA-detected CAD. Furthermore using a 5% ASCVD risk threshold resulted in further increase in sensitivity (from 53% to 72%), with slight further reduction in specificity (70% to 61%).
Of note, the overall sensitivity, specificity and alignment were not significantly different between the 2011 ESC/EAS and the 2004 ATP III guidelines. Although there are nuances, all of these guidelines including the 2013 ACC/AHA guidelines are in relative agreement regarding the lower thresholds for statin initiation in those with diabetes, peripheral vascular disease, and primary hyperlipidemia. 14 However, the main difference which drives the increased sensitivity in the ACC/AHA guidelines is related to lower absolute ASCVD risk threshold of 7.5% which is calculated based on risk factors with the pooled cohort calculator. In addition, both the 2004 ATP III and (to a lesser extent) the 2011 ESC/EAS guidelines are more reliant on LDL cut-off values for treatment in addition to absolute risk for determining statin eligibility. When considering the impressive safety profile of statins, particularly with pravastatin and simvastatin15, it would appear that the modestly reduced specificity of the ACC/AHA guidelines may be an acceptable trade-off for the improved sensitivity in the treatment of actual CCTA-detected CAD.
However, it is still remarkable that despite an improvement of alignment of statin eligibility with the presence of CAD, roughly half of patients with non-obstructive CAD and a third of patients with obstructive CAD remain ineligible for statin therapy using the new ACC/AHA guidelines. We have chosen the alignment of statin recommendations with the presence and extent of CAD as a gold standard as numerous studies including the multicenter CONFIRM registry have demonstrated that the presence, extent, and severity of CAD detected by CCTA is a powerful predictor of outcomes.16 Conventional risk factor algorithms, which are based largely on traditional clinical risk factors, may not be sufficient for determination of risk (and therefore allocation of preventive medical therapy) in all patients, as we have shown. This is further supported by evidence from nearly 18,000 patients were followed for a median of 2.3 years for all-cause mortality in the Coronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter Registry (CONFIRM) in which CCTA extent and severity of CAD improved overall risk prediction beyond NCEP ATP III risk. 17
It should be noted that although CCTA has now become an accepted diagnostic evaluation for low-intermediate risk chest pain patients in the ED setting based on multiple randomized controlled trials, there is currently insufficient evidence for the use of CCTA to guide treatment decisions in a pure asymptomatic primary prevention setting, However, other imaging modalities including coronary calcium scoring have been suggested in cholesterol treatment guidelines to help direct or influence statin treatment decisions. 18
Our study is not without limitations. Although the application of primary prevention rules to our cohort seems atypical, our patient cohort had no history of clinically apparent CAD and hence, once ACS was ruled out they were classified as having non-cardiac chest pain, and thus return to the group of patients eligible for primary prevention. Although our cohort may have a higher prevalence of traditional coronary atherosclerosis risk factors, and therefore a higher prevalence of CCTA-detected CAD, we have made our comparisons between guidelines in terms of sensitivity, specificity, and balanced accuracy, all which are considered to be independent of disease prevalence. Our other limitation is the relatively small sample size in which to apply these guidelines. However, the cohort is well-characterized, all the patients underwent CCTA to provide a “gold standard” of the severity and extent of CAD, and the proportion of patients with and without CAD were well-balanced.
The 2013 ACC/AHA are more sensitive than prior guidelines in identifying candidates for statin therapy who actually do have CAD as detected by CCTA, with an acceptable trade-off in specificity for those without CAD being recommended for therapy. Further longitudinal studies or randomized controlled trials are needed to determine whether changes in eligibility for statin therapy by the 2013 guidelines result in favorable down-stream health benefits.
Figure 3.
Schematic depicting the proportion of subjects eligible for statin therapy per the 2004 ATP III Guidelines, the 2013 ACC/AHA Guidelines, the 2013 ACC/AHA Guidelines using a 5.0% threshold, and the 2011 European Prevention Guidelines across strata of the presence and extent of coronary atherosclerosis as detected by CCTA in 189 patients without prior statin use presenting with acute chest pain in whom an acute coronary syndrome was excluded.
Acknowledgments
Funding and Disclosures:
This work was supported by grants from the National Heart, Lung, and Blood Institute (R01 HL080053 and 5K24HL113128)
Dr. Pursnani received support from NIH T32 HL076136.
Dr. Ferencik was supported by a grant from the American Heart Association (13FTF16450001).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, McBride P, Eckel RH, Schwartz JS, Goldberg AC, Shero ST, Gordon D, Smith SC, Jr, Levy D, Watson K, Wilson PW. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Goff DC, Jr, Lloyd-Jones DM, Bennett G, O’Donnell CJ, Coady S, Robinson J, D’Agostino RB, Sr, Schwartz JS, Gibbons R, Shero ST, Greenland P, Smith SC, Jr, Lackland DT, Sorlie P, Levy D, Stone NJ, Wilson PW. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013 doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Guallar E, Laine C. Controversy Over Clinical Guidelines: Listen to the Evidence, Not the Noise. Ann Intern Med. 2014 doi: 10.7326/M14-0112. [DOI] [PubMed] [Google Scholar]
- 5.Martin SS, Blumenthal RS. Concepts and Controversies: The 2013 American College of Cardiology/American Heart Association Risk Assessment and Cholesterol Treatment Guidelines. Ann Intern Med. 2014 doi: 10.7326/M13-2805. [DOI] [PubMed] [Google Scholar]
- 6.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–1765. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 7.Schulte JM, Rothaus CS, Adler JN. Clinical decisions. Starting statins--polling results. N Engl J Med. 2014;371:e6. doi: 10.1056/NEJMclde1407177. [DOI] [PubMed] [Google Scholar]
- 8.Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;57:1237–1247. doi: 10.1016/j.jacc.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS, Seneviratne SK, Truong QA, Cury RC, Abbara S, Shapiro MD, Moloo J, Butler J, Ferencik M, Lee H, Jang IK, Parry BA, Brown DF, Udelson JE, Achenbach S, Brady TJ, Nagurney JT. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol. 2009;53:1642–1650. doi: 10.1016/j.jacc.2009.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 11.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WM, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F. European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Int J Behav Med. 2012;19:403–488. doi: 10.1007/s12529-012-9242-5. [DOI] [PubMed] [Google Scholar]
- 12.Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Eur Heart J. 2011;32:1769–1818. doi: 10.1093/eurheartj/ehr158. [DOI] [PubMed] [Google Scholar]
- 13.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 14.Ray KK, Kastelein JJ, Boekholdt SM, Nicholls SJ, Khaw KT, Ballantyne CM, Catapano AL, Reiner Z, Luscher TF. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35:960–968. doi: 10.1093/eurheartj/ehu107. [DOI] [PubMed] [Google Scholar]
- 15.Naci H, Brugts J, Ades T. Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials. Circ Cardiovasc Qual Outcomes. 2013;6:390–399. doi: 10.1161/CIRCOUTCOMES.111.000071. [DOI] [PubMed] [Google Scholar]
- 16.Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, Lippolis NJ, Berman DS, Callister TQ. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50:1161–1170. doi: 10.1016/j.jacc.2007.03.067. [DOI] [PubMed] [Google Scholar]
- 17.Hadamitzky M, Achenbach S, Al-Mallah M, Berman D, Budoff M, Cademartiri F, Callister T, Chang HJ, Cheng V, Chinnaiyan K, Chow BJ, Cury R, Delago A, Dunning A, Feuchtner G, Gomez M, Kaufmann P, Kim YJ, Leipsic J, Lin FY, Maffei E, Min JK, Raff G, Shaw LJ, Villines TC, Hausleiter J. Optimized prognostic score for coronary computed tomographic angiography: results from the CONFIRM registry (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter Registry) J Am Coll Cardiol. 2013;62:468–476. doi: 10.1016/j.jacc.2013.04.064. [DOI] [PubMed] [Google Scholar]
- 18.Perrone-Filardi P, Achenbach S, Mohlenkamp S, Reiner Z, Sambuceti G, Schuijf JD, Van der Wall E, Kaufmann PA, Knuuti J, Schroeder S, Zellweger MJ. Cardiac computed tomography and myocardial perfusion scintigraphy for risk stratification in asymptomatic individuals without known cardiovascular disease: a position statement of the Working Group on Nuclear Cardiology and Cardiac CT of the European Society of Cardiology. Eur Heart J. 2011;32:1986–1993. 1993a, 1993b. doi: 10.1093/eurheartj/ehq235. [DOI] [PubMed] [Google Scholar]