Abstract
Background and Objectives
Coping with predeath grief (PDG) is an unmet need in caregivers of persons with dementia (PWD). The Marwit-Meuser Caregiver Grief Inventory (MM-CGI) and its abbreviated MM-CGI-Short-Form (MM-CGI-SF) are among the few empirically developed scales that detect PDG, yet they have not been substantially validated outside United States. We evaluated the reliability and validity of the PDG scales in a multiethnic Asian population distinct from that of United States.
Research Design and Methods
Family caregivers of community-dwelling PWD (n = 300) completed self-administered questionnaires containing MM-CGI and other scales of related construct. Sixty percent of the participants repeated the questionnaires 1 week later for test-retest reliability. Internal-consistency reliability was assessed by Cronbach’s α, test-retest reliability by intraclass-correlation-coefficient, construct validity by Spearman’s correlation-coefficient, and factorial validity by confirmatory factor analysis (CFA). Cohen’s κ was used to compare the agreement between MM-CGI and a commonly-used caregiver burden scale (Zarit Burden Interview).
Results
MM-CGI and MM-CGI-SF demonstrated internal-consistency reliability, test-retest reliability, construct validity, and known-group validity. In CFA, MM-CGI showed modest model-fit (comparative-fit-index, CFI = .80; Tucker-Lewis-index, TLI = .79), whereas MM-CGI-SF showed better model-fit (CFI = .91; TLI = .90). Eighty-six percent of the caregivers reported average or high levels of PDG, with 18% reporting high PDG. High scores in the caregiver burden scale only showed modest agreement with high scores in MM-CGI (κ = .47).
Discussion and Implications
MM-CGI and MM-CGI-SF demonstrated adequate psychometric properties and utility, beyond that of a caregiver burden scale, in detecting high PDG in a multiethnic Asian population. They open the way for PDG intervention in clinical care, as well as further exploration in caregiver research.
Keywords: Caregiver burden, Dementia, Marwit-Meuser Caregiver Grief Inventory, Predeath grief, Reliability, Validity
Caregiver stress in dementia has been much explored, with various interventions tailored to reduce the perceived burden of caregivers and improve their coping skills (Lazarus & Folkman, 1984). This approach has translated into services such as day care, respite care, caregiver education program and caregiver skills training. However, there are other emotions that caregivers contend with, including guilt, denial, sadness, and anger, which are not sufficiently addressed by interventions that focus primarily on the perceived burden or the coping skills of caregivers. A recent systematic review in the British Journal of Psychiatry (Feast et al., 2016) drew attention to the unmet emotional needs of family caregivers under the rubric of “feeling bereft,” thus highlighting the experience of loss and grief in the predeath context in caregivers of person with dementia (PWD). Similarly, another recent systematic review of the qualitative studies (Pozzebon, Douglas, & Ames, 2016) also reflected such experiences of loss and grief and highlighted the theme of “loss of partner” as central to the lived experience of spousal caregivers of PWD.
The experience of loss and grief in the predeath context is an emerging concept in the literature of dementia caregiving (Lindauer & Harvath, 2014). It has been described by various terms in the literature, such as “latent grief” (Dempsey & Baago, 1998), “anticipatory grief” (Chan, Livingston, Jones, & Sampson, 2013), “ambiguous loss” (Large & Slinger, 2015), “caregiver grief” (Large & Slinger, 2015), “dementia grief” (Blandin & Pepin, 2015), “feeling bereft” (Feast et al., 2016) and “predeath grief” (Lindauer & Harvath, 2014), with each term as an attempt to relate to the complex experience. In this paper, we opted for the generic term of “predeath grief” to include all the experience of loss and grief in the predeath context, as well as to contrast with the traditionally known grief which occurs postdeath. While there has not yet been a clear consensus on the definition of predeath grief (PDG), it possibly encompasses the range of emotional responses of caregivers as they mourn the current losses which are related to the caregiving role and the psychological death of PWD (a unique phenomenon in dementia whereby the PWD is still physically present but emotionally absent), and anticipate future losses with the physical death of the PWD.
PDG in dementia caregiving can have a complicated nature due to the protracted and uncertain disease trajectory, the disrupted communication and lost opportunity to reaffirm relationships, and the nature of grief which is disenfranchised and not socially sanctioned (Lindauer & Harvath, 2014). When the experience of losses in dementia caregiving is not recognized, caregivers may attempt to fight the inevitable decline in the PWD and become paternalistic towards the PWD. This may result in unequal dyadic relationships with caregivers feeling progressively more frustrated and helpless, while the PWD loses autonomy and becomes more dependent (Piiparinen & Whitlatch, 2011). Not surprisingly, caregivers with PDG have been shown to suffer from negative effects such as caregiver burden (Holley & Mast, 2009) and depression (Chan et al., 2013), and desire to institutionalize the PWD prematurely (Walker & Pomeroy, 1997). Considering the potential implications of PDG, a convenient instrument that can aid in its identification in clinical care is much needed.
The Marwit-Meuser Caregiver Grief Inventory (MM-CGI) and its abbreviated MM-CGI-Short-Form (MM-CGI-SF) are among the few empirically developed scales that measure PDG (Chan et al., 2013; Lindauer & Harvath, 2014). However, they have not been substantially validated outside the United States (Chan et al., 2013). As literature suggests that the expression of grief can be influenced by culture (Eisenbruch, 1984) (similarly reflected in our previous pilot study [Liew, 2016]), we sought to evaluate whether these PDG scales remain valid and reliable even in a multiethnic Asian population which is distinct from that of the United States (primary aim). We also had a secondary aim to assess whether these scales provide added utility in identifying caregivers with high PDG, beyond what is detectable by a commonly used caregiver burden scale (i.e., the Zarit Burden Interview which measures the perceived burden of caregivers).
Methods
Participants and Procedures
We consecutively sampled caregivers who accompanied the PWD to the dementia care service of two tertiary hospitals in the North-East of Singapore. Our inclusion criteria comprised: (a) spouses or children of PWD, (b) caring for PWD who is residing in the community, (c) able to read in English, and (d) age ≥21 years. At the point of recruitment, participants completed on-site a set of self-administered questionnaires comprising MM-CGI (Marwit & Meuser, 2002), a caregiver burden scale (Zarit Burden Interview, ZBI) (Zarit, Reever, & Bach-Peterson, 1980), a depression scale (Centre for Epidemiologic Studies Depression scale [CES-D]) (Radloff, 1977) and questions capturing demographic information. Participants were also asked to mail back a second set of questionnaires after they completed it at home one week later for the purpose of assessing test-retest reliability, of which sixty percent of the participants did so.
Prior to the start of the quantitative data collection, we also reviewed the clarity and comprehension of the items in MM-CGI using qualitative methods (such as cognitive interviews) as recommended by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) (Wild et al., 2009), with an intention to propose amendments to those items which may not be as clear to caregivers (see Supplementary Material 1 for details of the qualitative methods). Such approach of cross-cultural adaptation has been recommended by ISPOR when a scale is newly introduced across different populations (Wild et al., 2009).
The Domain Specific Review Board of the National Healthcare Group Singapore granted ethical approval for the study.
Measures
The Marwit-Meuser Caregiver Grief Inventory (MM-CGI) is a PDG scale that was developed in the United States through extensive focus-group interviews with caregivers of PWD (Marwit & Meuser, 2002). Its 50 items are assessed with 5-point Likert scales, and summed to generate a total score. Using the mean and standard deviation (SD) of MM-CGI in a study population, PDG can be classified into: Low (1 SD below mean), Average (within 1 SD from mean) and High (1 SD above mean). In the original study with 166 participants from the United States, this translated into cutoff scores of less than 113 to indicate low PDG, 113–175 to indicate average PDG and greater than 175 to indicate high PDG (Marwit & Meuser, 2002). In this study, we utilized both the original cutoff scores and a new set of cutoff scores derived from our study’s mean and SD.
The original validation study (Marwit & Meuser, 2002) also revealed three dimensions of loss in the exploratory factor analysis—Personal Sacrifice Burden, Heartfelt Sadness and Longing, and Worry and Felt Isolation. The Personal Sacrifice Burden dimension captures the personal aspect of losses experienced by caregivers (such as loss of personal freedom, sleep and physical health), the Heartfelt Sadness and Longing dimension captures the traditional concept of grief (i.e., one’s intrapersonal reactions to lost relationship) and the Worry and Felt Isolation dimension captures the feelings of losing connection with others and the worry about future losses. As recommended by the original authors, the three dimensions of loss in MM-CGI can be useful to guide the approach and the focus in our interventions for PDG (Meuser, Marwit, & Sanders, 2004).
The Marwit-Meuser Caregiver Grief Inventory-Short Form (MM-CGI-SF) is the shorter version of MM-CGI, using only the 18 most representative items for ease of administration (Marwit & Meuser, 2005). The Zarit Burden Interview (ZBI) is a 22-item scale that assesses the perceived burden experienced by caregivers of older persons (Zarit et al., 1980). The items are rated on 5-point Likert scales and summed to generate a total score ranging from 0 to 88, with scores above 60 being considered as high caregiver burden (Zarit & Zarit, 1987). ZBI contains five domains – Burden in the Relationship, Emotional Well-being, Social and Family Life, Finances, and Loss of Control over one’s life (Rankin, Haut, Keefover, & Franzen, 1994). CES-D comprises 20 items which measure depressive symptomatology using 4-point Likert scales. CES-D contains four domains—Depressed affect, Positive Affect, Somatic Symptoms, and Interpersonal Problems (Radloff, 1977). The ZBI (Seng et al., 2010) and CES-D (Stahl et al., 2008) have previously been validated in Singapore.
To obtain a brief measure of the stage of dementia, we used the three dementia severities described in the revised third edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) (American Psychiatric Association, 1987). From the three options, participants chose the description that best described the PWD—still capable of independent living (mild stage), needs some assistance with daily living (moderate stage), or needs round the clock supervision (severe stage). This brief measure was previously shown to have reasonable agreement with Clinical Dementia Rating Scale (κ = .56–.6) (Forsell, Fratiglioni, Grut, Viitanen, & Winblad, 1992; Juva et al., 1994; Morris, 1993).
Statistical Analyses
Overall, we conducted the following analyses: internal-consistency reliability, test-retest reliability, construct validity, known-group validity, and factorial validity. The details of each analysis are described in the paragraphs below.
Internal-consistency reliability was assessed with Cronbach’s α, whereas test-retest reliability was examined with intraclass correlation coefficient (ICC). The reliability indices of ≥.70 are considered good and represent the minimally acceptable reliability to allow group comparison (Nunnally & Bernstein, 1994), whereas values ≥.90 indicate suitability for individual-level measurements in clinical care (Fayers & Machin, 2007; Nunnally & Bernstein, 1994; Weiner & Stewart, 1984).
Construct validity was assessed by correlation with ZBI and CES-D, using the Spearman’s correlation coefficient (ρ). Correlation coefficient of >.50 are considered strong, whereas values ≤.50 are considered weak or moderate (Juniper, Guyatt, & Jaeschke, 1996). We made four hypotheses regarding construct validity:
MM-CGI would correlate strongly (ρ > .50) (Juniper et al., 1996) with the scales for caregiver burden (ZBI) and caregiver depression (CES-D). This is consistent with the original studies of MM-CGI (Marwit & Meuser, 2002, 2005) which have demonstrated the correlation of MM-CGI with caregiver burden and depression scales, with the reported correlation coefficients ranging between .51 and .76. This is expected because PDG, caregiver burden and caregiver depression are three related, though discriminable, phenomena in caregiving.
MM-CGI would correlate less strongly (ρ ≤ .50) (Juniper et al., 1996) with the Finances subscale of ZBI. The Finances subscale of ZBI, which comprises item 15 (do you feel that you don’t have enough money to take care of your relative), is not expected to show concordance with the experience of PDG measured by MM-CGI.
MM-CGI would correlate less strongly with the Positive Affect subscale of CES-D because each of them measures a distinct construct, the former on the feelings of loss and grief and the latter on positive feelings.
MM-CGI would correlate less strongly with the Interpersonal Problems subscale of CES-D. The Interpersonal Problems subscale of CES-D describes the feeling of critical reactions from others (item 15 of CES-D: people were unfriendly; item 19 of CES-D: I felt that people dislike me). Although such feelings can possibly be experienced by caregivers, they may not be reasonable correlates of caregivers who are grieving.
Known-group validity was assessed by comparing the mean scores of MM-CGI, using one-way analysis of variance (ANOVA), between groups which are known to differ in PDG levels. In the existing literature, later stage of dementia and spousal caregivers have been reported to be associated with the prominence of PDG (Chan et al., 2013; Liew, 2016; Pozzebon et al., 2016). Hence, the stage of dementia and the relationship with the PWD are the two demographic information that we used in the assessment of known-group validity to contrast the MM-CGI scores. The association between PDG and stage of dementia is understandable because with increasing severity of dementia, the psychological death of the PWD becomes more palpable to caregivers while the physical death of the PWD is more closely anticipated by caregivers. Likewise, the association between PDG and spousal caregivers is also understandable because spousal caregivers, who generally have longer and closer bonds with the PWD, will probably experience more grief reaction with the loss of the relationship.
Factorial validity was assessed with confirmatory factor analysis (CFA). We chose to conduct CFA for MM-CGI because CFA is generally the recommended approach “when the instrument was not new and when the authors had knowledge of the factor structure of scores from a previous administration of the instrument” (Henson & Roberts, 2006). We conducted the CFA using the maximum-likelihood estimation method in structural equation modeling. We compared the model fit between the original 3-factor model and a 1-factor model (which indicates MM-CGI as a unidimensional grief scale), and between MM-CGI and MM-CGI-SF. We used the following model-fit indices in CFA, with the values in parenthesis indicating good model-fit: root mean square error of approximation (RMSEA < .08), standardized root mean square residual (SRMR < .08), comparative fit index (CFI > .90), and Tucker-Lewis index (TLI > .90) (Marsh, Hau, & Grayson, 2005). Additionally, we also used the Akaike Information Criterion (AIC) in model comparison and AIC values which are lesser by at least 10 points indicate better model fit (Burnham & Anderson, 2003).
In the event of poor model-fit in CFA, we would further conduct exploratory analyses to examine possible reasons of poor fit. Specifically, we would conduct exploratory factor analysis (EFA) with maximum-likelihood estimation methods and oblique rotation (oblimin), to investigate whether the scale has three factors as originally reported, and whether the scale items loaded in the original factors (with factor loading of at least 0.30). To assess the appropriateness of the data for EFA, we would compute the Kaiser–Meyer–Olkin measure of sampling adequacy (with values closer to 1 indicating appropriateness, while values < .5 indicating inappropriateness of EFA) and Bartlett’s test of sphericity (with p < .05 indicating appropriateness of EFA). To assess the appropriate number of factors in EFA, we would use two methods, the Cattell’s scree test (Cattell, 1966) and Horn’s parallel analysis (Horn, 1965), to seek convergence in the results. The use of more than one method to determine the number of factors in EFA has been the recommended approach in recent literature (Henson & Roberts, 2006). Cattell’s scree test is a popular method which determines the number of factors to retain by examining the scree plot for a sharp break. On the other hand, Horn’s parallel analysis has received strong consensus in the literature as a more accurate method (Courtney, 2015; Dinno, 2009; Gaskin & Happell, 2014). Parallel analysis is implemented by generating a large number of data matrices from random data and factors are retained as long as they are greater than the mean eigenvalue generated from random data matrices (Courtney, 2015).
Additionally, we assessed the comparability between MM-CGI and MM-CGI-SF. The proportion of variance in MM-CGI which could be explained by MM-CGI-SF was examined with the coefficient of determination (r2). The agreement between MM-CGI and MM-CGI-SF in identifying PDG cases was examined with Cohen’s κ. Lastly, we also assessed whether high scores in a routinely used caregiver burden scale (ZBI) would have been sufficient to identify those with high PDG. Using Cohen’s κ, we compared the agreement between high ZBI scores (based on the cutoff score of >60) (Zarit & Zarit, 1987) and high MM-CGI scores (based on the cutoff score of >175) (Marwit & Meuser, 2002).
All analyses were performed using the Stata statistical software package, version 13 (Statacorp, 2013).
Results
We recruited 300 participants in this study, with 265 children and 35 spousal caregivers. The recruitment process had a response rate of 87.8%. The demographic information of the participants is shown in Table 1. Our participants comprised multiple ethnicities with the Chinese ethnicity being the largest group (82.3%). Prior to the start of quantitative data collection, we used recommended qualitative methods (such as cognitive interviews) (Wild et al., 2009) to review the clarity and comprehension of MM-CGI, and proposed three amendments to the scale items (see Supplementary Material 1 for details of the specific amendments). We incorporated the three amendments of MM-CGI into our study questionnaire and administered this updated version of questionnaire to all the study participants.
Table 1.
Demographic Information of the Caregivers and the Persons With Dementia They Cared for (n = 300)
| Variable | n (%) |
|---|---|
| Variables related to caregivers | |
| Age, mean (SD) | 52.1 (11.0) |
| Female gender, n (%) | 180 (60.0) |
| Ethnic, n (%) | |
| Chinese | 247 (82.3) |
| Malay | 25 (8.3) |
| Indian | 18 (6.0) |
| Eurasian/others | 10 (3.3) |
| Marital status, n (%) | |
| Single | 76 (25.3) |
| Married | 203 (67.7) |
| Widowed/divorced/separated | 21 (7.0) |
| Employment status, n (%) | |
| Working full-time | 179 (59.7) |
| Working part-time | 36 (12.0) |
| Not working | 85 (28.3) |
| Highest education, n (%) | |
| Tertiary | 110 (36.7) |
| Secondary | 182 (60.7) |
| Primary or no formal education | 8 (2.7) |
| Relationship with the PWD, n (%) | |
| Child | 265 (88.3) |
| Spouse | 35 (11.7) |
| Staying with the PWD, n (%) | 199 (66.3) |
| Duration of caregiving in years, mean (SD) | 6.6 (6.7) |
| Frequency of caregiving, n (%) | |
| Daily, for at least 4 hr a day | 156 (52.0) |
| Daily, but less than 4 hr a day | 64 (21.3) |
| At least once a week | 64 (21.3) |
| Less than once a week | 16 (5.3) |
| Primary caregiving role, n (%) | 218 (72.7) |
| MM-CGI score, mean (SD) | 140.0 (35.4) |
| MM-CGI-SF score, mean (SD) | 51.3 (13.4) |
| ZBI score, mean (SD) | 35.1 (17.5) |
| CES-D score, mean (SD) | 15.0 (10.7) |
| Variables related to PWD | |
| Age, mean (SD) | 79.5 (8.1) |
| Female gender, n (%) | 214 (71.3) |
| Age at dementia diagnosis, mean (SD) | 75.5 (8.3) |
| Duration of dementia diagnosis in years, mean (SD) | 4.5 (3.5) |
| Stage of dementia, n (%) | |
| Mild | 49 (16.3) |
| Moderate | 127 (42.3) |
| Severe | 124 (41.3) |
Note: CES-D = Centre for Epidemiologic Studies Depression scale; MM-CGI = Marwit-Meuser Caregiver Grief Inventory; MM-CGI-SF = Marwit-Meuser Caregiver Grief Inventory-Short Form; PWD = Persons with dementia; SD = Standard deviation; ZBI = Zarit Burden Interview.
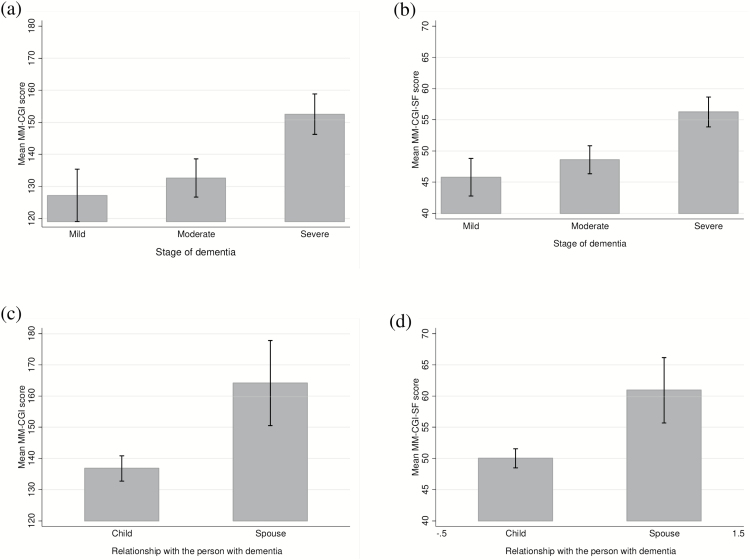
Both MM-CGI and MM-CGI-SF had high internal-consistency reliability (α = .98 and .94 respectively) and test-retest reliability (ICC = .90 and .88 respectively). As hypothesized, both scales correlated strongly with ZBI and CES-D (Spearman’s correlation coefficient, ρ = .72–.77) and correlated less strongly with Finance subscale of ZBI, Positive Affect subscale of CES-D and Interpersonal Problems subscale of CES-D (ρ = .36–.49) (Supplementary Table 2). In the assessment of known-group validity (Figure 1), the findings were consistent with what we had expected. The mean scores of the scales were significantly different among those caring for PWD at various stages of disease (p < .001 in ANOVA for both MM-CGI and MM-CGI-SF). In pairwise comparison, the mean scores of MM-CGI and MM-CGI-SF were significantly higher among those caring for PWD at severe stage compared to the mild stage (p < .001 after Bonferroni adjustment) or the moderate stage (p < .001 after Bonferroni adjustment). However, the mean scores were not significantly different between the mild stage and the moderate stage (after Bonferroni adjustment, p = 1.00 for MM-CGI and p = .584 for MM-CGI-SF). Similarly, spousal caregivers reported significantly higher mean scores than children caregivers (p < .001 for both MM-CGI and MM-CGI-SF).
Figure 1.
Comparison of the mean scores of Marwit-Meuser Caregiver Grief Inventory (MM-CGI) and Marwit-Meuser Caregiver Grief Inventory-Short Form (MM-CGI-SF) between groups which are known to differ in predeath grief level, in the assessment of known-group validity. Figure (a) and (b) shows the mean scores of MM-CGI and MM-CGI-SF respectively, at various stages of dementia. Figure (c) and (d) shows the mean scores of MM-CGI and MM-CGI-SF respectively, for child and spousal caregivers. The vertical lines of error bar indicate the 95% confidence interval of the scores.
In the CFA of MM-CGI and MM-CGI-SF, the original three-factor models had better fit indices than the one-factor models (Supplementary Table 3). The fit indices of the three-factor MM-CGI-SF were also generally better than those of the three-factor MM-CGI. In view of the modest model-fit of three-factor MM-CGI (RMSEA = .080, SRMR = .061, CFI = .80, TLI = .79), we proceeded to conduct EFA. The data was appropriate for EFA, with Kaiser–Meyer–Olkin measure of sampling adequacy of .96 and p value of less than .001 in Bartlett’s test of sphericity (χ2 = 11,701.1, df = 1,225). The scree plot is shown in Supplementary Figure 4, with the scree test and parallel analysis converging on a three-factor structure. In the EFA that retained three factors, the factor loadings of individual scale items are shown in Table 2. Most of the items in Factor 1 (Personal Sacrifice Burden) and Factor 2 (Heartfelt Sadness and Longing) loaded in their original factors. However, items in Factor 3 (Worry and Felt Isolation) appeared to be split between the “Worry” component and the “Felt Isolation” component—Items which relate to the “Felt Isolation” component still loaded in the original Factor 3 but items relating to the “Worry” component loaded in Factor 2 (Heartfelt Sadness and Longing) instead.
Table 2.
Exploratory Factor Analysis of the Marwit-Meuser Caregiver Grief Inventory and Factor Loadings of the Scale Items, Using Maximum-Likelihood Estimation and Oblique Rotation (Oblimin)
| Factors | |||
|---|---|---|---|
| MM-CGI items within their original factors | 1 | 2 | 3 |
| Factor 1: Personal sacrifice burden | |||
| 1. I’ve had to give up a great deal to be a caregivera. | 0.718 | ||
| 3. I feel I am losing my freedoma. | 0.911 | ||
| 4. My physical health has declined from the stress of being a caregiver. | 0.486 | 0.306 | |
| 7. I carry a lot of stress as a caregiver. | 0.563 | ||
| 11. My personal life has changed a great deal. | 0.623 | ||
| 17. I feel this constant sense of responsibility and it just never leaves. | 0.508 | ||
| 20. I can’t feel free in this situation. | 0.601 | ||
| 25. I feel so frustrated that I often ignore him/her. | 0.307 | ||
| 28. This is requiring more emotional energy and determination than I ever expected. | 0.409 | 0.452 | |
| 29. I will be tied up with this for who knows how longa. | 0.534 | 0.306 | |
| 35. His/her death will bring me renewed personal freedom to live my life. | 0.725 | −0.326 | |
| 39. Independence is what I’ve lost…I don’t have the freedom to go and do what I wanta. | 0.802 | ||
| 40. I’ve had to make some drastic changes in my life as a result of becoming a caregiver. | 0.773 | ||
| 41. I wish I had an hour or two to myself each day to pursue personal interestsa. | 0.619 | ||
| 42. I’m stuck in this caregiving world and there’s nothing I can do about ita. | 0.545 | ||
| 44. What upset me most are the things I have to give up. | 0.330 | 0.494 | |
| 21. I’m having trouble sleeping. | 0.472 | ||
| 49. The demands on me are growing faster than I ever expected. | 0.573 | ||
| Factor 2: Heartfelt sadness and longing | |||
| 9. I have this empty, sick feeling knowing that my loved one is “gone”a. | 0.645 | ||
| 14. I feel terrific sadness. | 0.821 | ||
| 15. This situation is totally unacceptable in my heart. | 0.826 | ||
| 18. I long for what was, what we had and shared in the pasta. | 0.648 | ||
| 19. I could deal with other serious disabilities better than with thisa. | 0.539 | ||
| 27. I’m angry at the disease for robbing me of so much. | 0.678 | ||
| 30. It hurts to put her/him to bed at night and realize that she/he is “gone”a. | 0.660 | ||
| 31. I feel very sad about what this disease has donea. | 0.702 | ||
| 36. I feel powerless. | 0.468 | ||
| 37. It’s frightening because you know doctors can’t cure this disease, so things only get worse. | 0.594 | ||
| 38. I’ve lost other people close to me, but the losses I’m experiencing now are much more troublinga. | 0.706 | ||
| 43. I can’t contain my sadness about all that’s happening. | 0.793 | ||
| 48. I’ve had a hard time accepting what is happening. | 0.851 | ||
| 50. I wish this was all a dream and I could wake up back in my old life. | 0.676 | ||
| 2. I miss so many of the activities we used to share. | 0.520 | ||
| Factor 3: Worry and felt isolation | |||
| 5. I have nobody to communicate witha. | 0.334 | 0.450 | |
| 8. I receive enough emotional support from othersb. | −0.417 | ||
| 24. My extended family has no idea what I go through in caring for him/her. | 0.375 | ||
| 34. The people closest to me do not understand what I’m going througha. | 0.371 | 0.353 | |
| 45. I’m managing pretty well overallb. | −0.308 | −0.305 | |
| 47. I get excellent support from members of my familyb. | −0.505 | ||
| 6. I don’t know what is happening. I feel confused and unsure. | 0.549 | ||
| 10. I feel anxious and scared. | 0.792 | ||
| 12. I spend a lot of time worrying about the bad things to comea. | 0.729 | ||
| 13. Dementia is like a double loss…I’ve lost the closeness with my loved one and connectedness with my familya. | 0.741 | ||
| 16. My friends simply don’t understand what I’m going througha. | 0.387 | ||
| 22. I’m at peace with myself and my situation in lifeb. | −0.301 | ||
| 23. It’s a life phase and I know we’ll get through itb. | −0.314 | ||
| 26. I am always worrying. | 0.673 | ||
| 32. I feel severe depression. | 0.810 | ||
| 33. I lay awake most nights worrying about what’s happening and how I’ll manage tomorrowa. | 0.776 | ||
| 46. I think I’m denying the full impact of this disease for my life. | 0.595 | ||
Note: Only factor loadings of ≥0.30 are shown in the table. Bold-faced factor loadings indicate those items which did not load into their original factors.
aItems used in MM-CGI-SF. bItems in reverse wordings.
MM-CGI-SF explained 96% of the variance in MM-CGI (based on the result from r2). The new and the original cutoff scores for MM-CGI produced similar proportions of PDG levels (Supplementary Table 5) and had good agreement between each other (κ = .85). However, the agreement between MM-CGI and MM-CGI-SF was better when we used the new cutoff scores (κ = .83), in contrast to that of the original cutoff scores (κ = .63). Using the new cutoff scores of MM-CGI, 86% of caregivers reported average or high levels of PDG (95% CI 82%–90%), with 18% reporting high PDG (95% CI 14%–22%). Similar prevalence was also seen with the new cutoff scores of MM-CGI-SF.
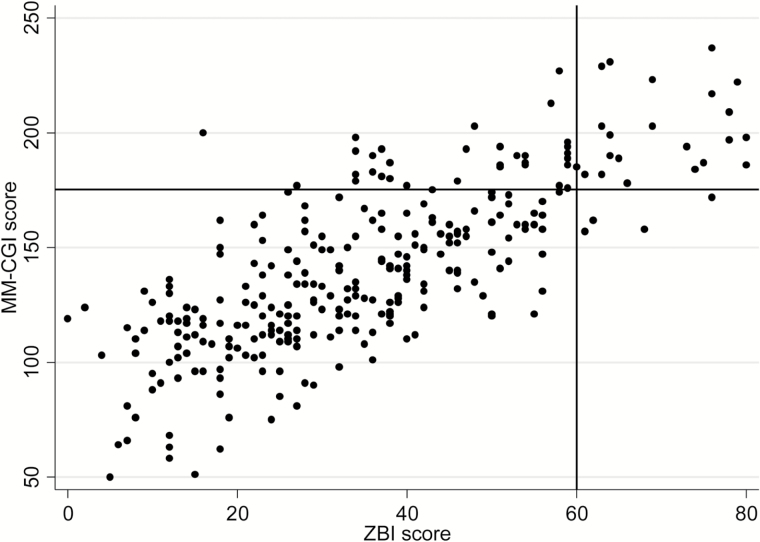
Many caregivers with high MM-CGI scores (>175) did not exhibit high ZBI scores (>60), as shown in Figure 2. The agreement between high MM-CGI scores and high ZBI scores was modest (κ = .47).
Figure 2.
Scatterplot between a commonly used caregiver burden scale (Zarit Burden Interview, ZBI) and Marwit-Meuser Caregiver Grief Inventory (MM-CGI) (n = 300). ZBI scores above 60 are considered high caregiver burden (vertical line), while MM-CGI scores above 175 are considered high predeath grief (horizontal line).
Discussion
To our knowledge, this is the first study that has provided substantial evidence of the validity and reliability of MM-CGI and MM-CGI-SF in a multiethnic Asian population which is outside and distinct from that of the United States. We showed that MM-CGI-SF may be a better choice than MM-CGI for routine use given its shorter length and administration time, better model-fit, and near-complete explanation of the variance in MM-CGI. We also proposed further improvements to the scales for our multiethnic Asian population, such as revisions to the scale items to improve clarity and a new set of cutoff scores to improve the agreement between MM-CGI and MM-CGI-SF. Using MM-CGI and MM-CGI-SF, we showed that PDG is not uncommon in caregivers of PWD. We also demonstrated the added utility of the scales in identifying a subgroup of caregivers with high PDG, beyond what a commonly used caregiver burden scale can detect. Had the MM-CGI or MM-CGI-SF not been used, we would have missed many caregivers who had high PDG but did not exhibit high burden.
In CFA, the modest model-fit of MM-CGI could possibly be contributed by the complex factor structure of the scale itself. As written by Marsh et al. (Marsh, Hau, & Wen, 2004), “Conventional CFA goodness of fit criteria are too restrictive when applied to most multifactor rating instruments. It is my experience that it is almost impossible to get an acceptable fit (e.g., CFI,RNI,TLI>0.9; RMSEA<0.05) for even “good” multifactor rating instruments when analyses are done at the item level and there are multiple factors (e.g., 5–10), each measured with a reasonable number of items (e.g., at least 5–10 per scale) so that there are at least 50 items overall. If this is the case, then I argue that “conventional” rules of thumb about acceptable fit are too restrictive (even though there has been a recent push for even stricter standards).” Another plausible explanation to the modest model-fit is that the original factor structures of MM-CGI may not be directly applicable outside the United States and its factor structure may need to be revisited in different populations. This is evident in our EFA which demonstrated a distinct pattern of deviation from the original factor structures. The original Factor 3 of Worry and Felt Isolation appeared to be split into two, with the “Worry” component more closely associated with the original Factor 2 of Heartfelt Sadness and Longing (which represents the traditional concept of grief, or one’s intrapersonal reactions to lost relationship). The result of EFA seems to reaffirm the known literature that the expression of grief can differ across cultures (Eisenbruch, 1984). At least in the context of our population, and possibly in the other Asian populations, the expression of worry may be a masquerade of the grief reaction of caregivers. Awareness of this association may help clinicians to look out for PDG whenever they are faced with caregivers who express much worries. Nevertheless, independent replication of this new finding in future studies is still necessary before we can draw any strong conclusion on the factor structure of MM-CGI. Regardless of the eventual conclusion on this factor structure, it should not have significant impact on the overall usefulness of MM-CGI. The utility of MM-CGI lies primarily in its total score (which is needed to detect PDG), while the subscales may have more relevance to guide subsequent approaches of intervention (as recommended by the original authors) (Meuser et al., 2004).
Most caregivers in this study reported average or high levels of PDG. This is consistent with published literature (Chan et al., 2013) that PDG is not uncommon in dementia caregiving. It also reaffirms the applicability of PDG outside of the United States (Liew, 2016), specifically in a multiethnic Asian population. Having a PDG scale that is validated both in- and outside of the United States sets the stage for future cross-cultural comparison of PDG to enrich our understanding of its characteristics and how it may affect dementia caregiving. In clinical settings, the finding calls for health care and social-care workers in contact with caregivers of PWD to be familiar with PDG, and actively provide opportunities for caregivers to talk about their difficult emotions and to review the implications of their losses (Parkes, 1998). This is when the caregivers can feel supported emotionally, even while they are faced with challenges in the caregiving journey.
A substantial proportion, nearly one-fifth, of caregivers experienced high PDG. These caregivers with high PDG, possibly representing a subgroup who has more severe intensity of PDG, may not be easily recognized considering that PDG is commonly disenfranchised (Lindauer & Harvath, 2014) and not readily talked about by caregivers. They may also be missed by other routinely used scales such as the caregiver burden scale, as seen in our results (Figure 2). By adding a brief PDG scale such as MM-CGI-SF in routine practice, clinicians will now be able to identify caregivers with high PDG who might possibly benefit from further clinical attention and interventions.
Although most of the literature on grief interventions focuses on the post-death context, some of the principles of interventions may possibly be similar in PDG and can be considered to guide our interventions for caregivers with high PDG. For instance, the focus in interventions may possibly include facilitating caregivers to adjust to life changes following the loss (Stroebe & Schut, 2010; William Worden, 2008), revisit the loss and its associated emotions (Stroebe & Schut, 2010; William Worden, 2008), reconstruct the meaning of the loss (Neimeyer, 2014), find continual connection with the lost relationship (Klass, Silverman, & Nickman, 1996; William Worden, 2008), and involve the whole family in the grieving process (Neimeyer, 2014; Stroebe & Schut, 2015). Through grief interventions, we may be better able to support caregivers to adapt to the losses and find new ways to maintain a meaningful relationship with the PWD who has changed. This approach is consistent with the understanding of what constitutes successful caregiving (Kahana & Young, 1990), with caregivers changing themselves to adapt to the PWD and fit into the new caregiving relationship. Regardless of the arguments for grief interventions in PDG, further research is still required in this area to evaluate the efficacy of any proposed interventions for high PDG. Such research opportunities are now easier outside the United States because we can confidently identify PDG with a validated scale.
Some limitations of the study are noteworthy. First, the scales were self-administered; therefore caregivers with lower literacy were probably under-represented. Second, a number of the spousal caregivers in our population could not speak English and hence, could not participate in this study. It is also more common for children caregivers to accompany the PWD for clinical follow-up, and hence there were less opportunities to recruit the spousal caregivers. Had more spousal caregivers been recruited, the average scores and prevalence of PDG might possibly be higher considering a recent systematic review (Pozzebon et al., 2016) that highlighted the experience of loss as the central theme for spousal caregivers. Third, as MM-CGI-SF was embedded as part of MM-CGI, its properties could possibly be different if it had been administered separately on its own. Forth, the cutoff scores of MM-CGI and MM-CGI-SF are meant as indications of the need for further evaluations, and should not be used to indicate the definite presence or absence of PDG. The new cutoff scores that we proposed may benefit from further validation in future studies to assess whether they are replicable in different populations, or whether we need population-specific cutoff scores to reflect the varying experience of PDG in different cultures.
In conclusion, PDG, with its complexity of emotions, is not uncommon in caregivers of PWD. It provides an additional opportunity to understand and support the emotional needs of caregivers. The MM-CGI and MM-CGI-SF have demonstrated adequate psychometric properties, although the subscales of MM-CGI may need to be interpreted with caution in different cultures. The scales have also demonstrated their utility, beyond that of a caregiver burden scale, in identifying a subgroup of caregivers with high PDG. They open the way for PDG assessment and intervention in clinical care, as well as further exploration in caregiver research.
Supplementary Material
Supplementary data are available at The Gerontologist online.
Previous Presentation
Presented orally in preliminary form at the Alzheimer’s Association International Conference (Toronto, July 2016).
Funding
This research was supported by the Singapore Ministry of Health’s National Medical Research Council under the Centre Grant Program (Grant No.: NMRC/CG/004/2013). It also received pilot funding from the National University of Singapore. Separately, the first author (T.M.L.) was supported by a research fellowship under the Singapore Ministry of Health’s National Medical Research Council (Grant No.: NMRC/Fellowship/0030/2016). The funding sources had no involvement in any part of the project.
Supplementary Material
Acknowledgments
The authors thank Associate Professor Thomas M. Meuser for providing the original scales, and the participants for their support of this research.
Conflict of Interest
The authors declare no conflict of interest.
References
- American Psychiatric Association.(1987). Diagnostic and statistical manual of mental disorders: DSM-III-R.Washington: American Psychiatric Association. [Google Scholar]
- Blandin K., & Pepin R (2015). Dementia grief: A theoretical model of a unique grief experience. Dementia (London), 16, 67–78. doi:10.1177/1471301215581081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham K. P., & Anderson D. R (2003). Model selection and multimodel inference: A practical information-theoretic approach. New York: Springer. [Google Scholar]
- Cattell R. B. (1966). The scree test for the number of factors. Multivariate Behavioral Research, 1, 245–276. doi:10.1207/s15327906mbr0102_10 [DOI] [PubMed] [Google Scholar]
- Chan D., Livingston G., Jones L. & Sampson E. L (2013). Grief reactions in dementia carers: A systematic review. International Journal of Geriatric Psychiatry, 28, 1–17. doi:10.1002/gps.3795 [DOI] [PubMed] [Google Scholar]
- Courtney M. G. R. (2015). Determining the number of factors to retain in EFA: Using the SPSS R-Menu v2.0 to make more judicious estimations. Practical Assessment, Research & Evaluation, 18, 1–14. [Google Scholar]
- Dempsey M., & Baago S (1998). Latent grief: The unique and hidden grief of carers of loved ones with dementia. American Journal of Alzheimer’s Disease and Other Dementias, 13, 84–91. doi:10.1177/153331759801300206 [Google Scholar]
- Dinno A. (2009). Exploring the sensitivity of Horn’s parallel analysis to the distributional form of random data. Multivariate Behavioral Research, 44, 362–388. doi:10.1080/00273170902938969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenbruch M. (1984). Cross-cultural aspects of bereavement. II: Ethnic and cultural variations in the development of bereavement practices. Culture, Medicine and Psychiatry, 8, 315–347. doi:10.1007/bf00114661 [DOI] [PubMed] [Google Scholar]
- Fayers P. M., & Machin D (2007). Quality of life: The assessment, analysis and interpretation of patient-reported outcomes. England: Wiley. [Google Scholar]
- Feast A., Orrell M., Charlesworth G., Melunsky N., Poland F. & Moniz-Cook E (2016). Behavioural and psychological symptoms in dementia and the challenges for family carers: Systematic review. The British Journal of Psychiatry: The Journal of Mental Science, 208, 429–434. doi:10.1192/bjp.bp.114.153684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsell Y., Fratiglioni L., Grut M., Viitanen M. & Winblad B (1992). Clinical staging of dementia in a population survey: Comparison of DSM-III-R and the Washington University Clinical Dementia Rating Scale. Acta Psychiatrica Scandinavica, 86, 49–54. doi:10.1111/j.1600-0447.1992.tb03225.x [DOI] [PubMed] [Google Scholar]
- Gaskin C. J., & Happell B (2014). On exploratory factor analysis: A review of recent evidence, an assessment of current practice, and recommendations for future use. International Journal of Nursing Studies, 51, 511–521. doi:10.1016/j.ijnurstu.2013.10.005 [DOI] [PubMed] [Google Scholar]
- Henson R. K., & Roberts J. K (2006). Use of exploratory factor analysis in published research. Educational and Psychological Measurement, 66, 393–416. doi:10.1177/0013164405282485 [Google Scholar]
- Holley C. K. & Mast B. T (2009). The impact of anticipatory grief on caregiver burden in dementia caregivers. The Gerontologist, 49, 388–396. doi:10.1093/geront/gnp061 [DOI] [PubMed] [Google Scholar]
- Horn J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika, 30, 179–185. doi:10.1007/bf02289447 [DOI] [PubMed] [Google Scholar]
- Juniper E. F., Guyatt G. H., & Jaeschke R (1996). How to develop and validate a new health-related quality of life instrument. In B., Spilker (Ed.), Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia: Lippincott-Raven. [Google Scholar]
- Juva K., Sulkava R., Erkinjuntti T., Ylikoski R., Valvanne J. & Tilvis R (1994). Staging the severity of dementia: Comparison of clinical (CDR, DSM-III-R), functional (ADL, IADL) and cognitive (MMSE) scales. Acta Neurologica Scandinavica, 90, 293–298. doi:10.1111/j.1600-0404.1994.tb02724.x [DOI] [PubMed] [Google Scholar]
- Kahana E., & Young R (1990). Clarifying the caregiving paradigm: Challenges for the future. In D. E. Biegel, & A. Blum (Eds.), Aging and caregiving: Theory, research, and policy (pp. 76–97). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Klass D., Silverman P. R., & Nickman S. L (1996). Continuing bonds: New understandings of grief. New York: Taylor & Francis. [Google Scholar]
- Large S. & Slinger R (2015). Grief in caregivers of persons with Alzheimer’s disease and related dementia: A qualitative synthesis. Dementia (London, England), 14, 164–183. doi:10.1177/1471301213494511 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., & Folkman S (1984). Stress, appraisal, and coping. New York: Springer Publishing Company. [Google Scholar]
- Liew T. M. (2016). Applicability of the pre-death grief concept to dementia family caregivers in Asia. International Journal of Geriatric Psychiatry, 31, 749–754. doi:10.1002/gps.4387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindauer A. & Harvath T. A (2014). Pre-death grief in the context of dementia caregiving: A concept analysis. Journal of Advanced Nursing, 70, 2196–2207. doi:10.1111/jan.12411 [DOI] [PubMed] [Google Scholar]
- Marsh H. W., Hau K.-T., & Wen Z (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling: A Multidisciplinary Journal, 11, 320–341. doi:10.1207/s15328007sem1103_2 [Google Scholar]
- Marsh H. W., Hau K. T., & Grayson D (2005). Goodness of fit in structural equation models. In R. P. McDonald A. Maydeu-Olivares, & J. J. McArdle (Eds.), Contemporary psychometrics: A Festschrift for Roderick P. McDonald. New Jersey: Lawrence Erlbaum Associates. [Google Scholar]
- Marwit S. J. & Meuser T. M (2002). Development and initial validation of an inventory to assess grief in caregivers of persons with Alzheimer’s disease. The Gerontologist, 42, 751–765. doi:10.1093/geront/42.6.751 [DOI] [PubMed] [Google Scholar]
- Marwit S. J. & Meuser T. M (2005). Development of a short form inventory to assess grief in caregivers of dementia patients. Death studies, 29, 191–205. doi:10.1080/07481180590916335 [DOI] [PubMed] [Google Scholar]
- Meuser T. M., Marwit S. J., & Sanders S (2004). Assessing grief in family caregivers. In K. J., Doka (Ed.), Living with grief: Alzheimer’s disease (pp. 169–195). Washington, DC: Hospice Foundation of America. [Google Scholar]
- Morris J. C. (1993). The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology, 43, 2412–2414. doi:10.1212/wnl.43.11.2412-a [DOI] [PubMed] [Google Scholar]
- Neimeyer R. A. (2014). The changing face of grief: Contemporary directions in theory, research, and practice. Progress in Palliative Care, 22, 125–130. doi:10.1179/1743291x13y.0000000075 [Google Scholar]
- Nunnally J. C., & Bernstein I. H (1994). Psychometric theory. New York: McGraw-Hill. [Google Scholar]
- Parkes C. M. (1998). Facing loss. BMJ (Clinical research ed.), 316, 1521–1524. doi:10.1136/bmj.316.7143.1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piiparinen R., & Whitlatch C. J (2011). Existential loss as a determinant to well-being in the dementia caregiving dyad: A conceptual model. Dementia, 10, 185–201. doi:10.1177/ 1471301211398989 [Google Scholar]
- Pozzebon M., Douglas J. & Ames D (2016). Spouses’ experience of living with a partner diagnosed with a dementia: A synthesis of the qualitative research. International Psychogeriatrics, 28, 537–556. doi:10.1017/S1041610215002239 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Rankin E. D., Haut M. W., Keefover R. W. & Franzen M. D (1994). The establishment of clinical cutoffs in measuring caregiver burden in dementia. The Gerontologist, 34, 828–832. doi:10.1093/geront/34.6.828 [DOI] [PubMed] [Google Scholar]
- Seng B. K., Luo N., Ng W. Y., Lim J., Chionh H. L., Goh J. & Yap P (2010). Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Annals of the Academy of Medicine, Singapore, 39, 758–763. [PubMed] [Google Scholar]
- Stahl D., Sum C. F., Lum S. S., Liow P. H., Chan Y. H., Verma S.,… Chong S. A (2008). Screening for depressive symptoms: Validation of the center for epidemiologic studies depression scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care, 31, 1118–1119. doi:10.2337/dc07-2019 [DOI] [PubMed] [Google Scholar]
- Stroebe M. & Schut H (2010). The dual process model of coping with bereavement: A decade on. OMEGA, 61, 273–289. doi:10.2190/OM.61.4.b [DOI] [PubMed] [Google Scholar]
- Stroebe M. & Schut H (2015). Family matters in bereavement: Toward an integrative intra-interpersonal coping model. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 10, 873–879. doi:10.1177/1745691615598517 [DOI] [PubMed] [Google Scholar]
- Walker R. J. & Pomeroy E. C (1997). The impact of anticipatory grief on caregivers of persons with Alzheimer’s disease. Home Health Care Services Quarterly, 16, 55–76. doi:10.1300/J027v16n01_05 [DOI] [PubMed] [Google Scholar]
- Weiner E. A., & Stewart B. J (1984). Assessing individuals: Psychological and educational tests and measurements. New York: Little, Brown. [Google Scholar]
- Wild D., Eremenco S., Mear I., Martin M., Houchin C., Gawlicki M.,… Molsen E (2009). Multinational trials-recommendations on the translations required, approaches to using the same language in different countries, and the approaches to support pooling the data: The ISPOR Patient-Reported Outcomes Translation and Linguistic Validation Good Research Practices Task Force report. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 12, 430–440. doi:10.1111/j.1524-4733.2008.00471.x [DOI] [PubMed] [Google Scholar]
- William Worden J. (2008). Grief counseling and grief therapy, fourth edition: A handbook for the mental health practitioner. New York: Springer Publishing Company. [Google Scholar]
- Zarit S. H., Reever K. E. & Bach-Peterson J (1980). Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist, 20, 649–655. doi:10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]
- Zarit S. H., & Zarit J. M (1987). Instructions for the burden interview.University Park, PA: Pennsylvania State University. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.