Abstract
Background
Measles supplementary immunization activities (SIAs) are vaccination campaigns that supplement routine vaccination programs with a recommended second dose opportunity to children of different ages regardless of their previous history of measles vaccination. They are conducted every 2–4 years and over a few weeks in many low- and middle-income countries. While SIAs have high vaccination coverage, it is unclear whether they reach the children who miss their routine measles vaccine dose. Determining who is reached by SIAs is vital to understanding their effectiveness, as well as measure progress towards measles control.
Methods
We examined SIAs in low- and middle-income countries from 2000 to 2014 using data from the Demographic and Health Surveys. Conditional on a child’s routine measles vaccination status, we examined whether children participated in the most recent measles SIA.
Results
The average proportion of zero-dose children (no previous routine measles vaccination defined as no vaccination date before the SIA) reached by SIAs across 14 countries was 66%, ranging from 28% in São Tomé and Príncipe to 91% in Nigeria. However, when also including all children with routine measles vaccination data, this proportion decreased to 12% and to 58% when imputing data for children with vaccination reported by the mother and vaccination marks on the vaccination card across countries. Overall, the proportions of zero-dose children reached by SIAs declined with increasing household wealth.
Conclusions
Some countries appeared to reach a higher proportion of zero-dose children using SIAs than others, with proportions reached varying according to the definition of measles vaccination (e.g., vaccination dates on the vaccination card, vaccination marks on the vaccination card, and/or self-reported data). This suggests that some countries could improve their targeting of SIAs to children who miss other measles vaccine opportunities. Across all countries, SIAs played an important role in reaching children from poor households.
Keywords: measles, vaccination, supplementary immunization activities, equity, low- and middle-income countries
INTRODUCTION
At the turn of the 21st century, measles was the leading cause of vaccine-preventable child mortality, with an estimated global mortality burden of 535,000 deaths in the year 2000 [1]; it was then a leading cause of death among post-neonates, causing 4 to 5% of deaths in this age group [2]. While substantial progress to reduce measles mortality has been made in recent years, measles still caused an estimated 115,000 deaths globally in 2014 [3]. Despite the availability of a safe and effective vaccine, routine vaccination programs worldwide only reached approximately 85% of children under the age of one with the first dose of the measles vaccine in 2014 [3]. This coverage also varies by region, ranging from a low average of 83% in the World Health Organization (WHO) African Region to a high average of 93% in the Americas Region [4]. Routine measles vaccination coverage decreases further with the recommended second dose to approximately 35% for children under two and 53% at older ages globally [3, 5]. WHO recommends that all countries include a second routine dose of measles-containing vaccine (MCV) [6]. However, in practice, the second dose of MCV is offered through routine vaccination programs, supplementary immunization activities (SIAs), or both. The administration of the second dose of measles vaccine can vary by type of delivery and recommended age of vaccination according to health system infrastructure and measles endemicity. Countries with high levels of vaccination coverage, typically due to strong health systems, rely on routine services for delivery, whereas countries with low levels of coverage use SIAs to close the gaps in target coverage from the routine program [6]. In order to supplement those routine vaccination efforts, organizations such as the Measles & Rubella Initiative (partners including the American Red Cross, the United Nations Foundation, the U.S. Centers for Disease Control and Prevention, UNICEF and the WHO) and Gavi, the Vaccine Alliance, currently provide support and co-financing for measles SIAs every two to four years in low- and middle-income countries. SIAs are mass campaigns lasting up to three weeks during which health workers provide vaccinations directly to targeted children, regardless of their history of vaccination [7–9]. However, despite this widespread support, many countries have still not achieved the WHO target of a 95% reduction in measles mortality between 2000 and 2015 [3].
In order to achieve the current goal of eliminating measles in at least five of the six WHO regions by 2020 [10], efforts must focus both on strengthening the routine vaccination program and addressing missed measles vaccination opportunities in the routine program through SIAs to achieve the necessary very high levels of measles vaccination coverage required for population immunity [11]. Achieving high levels of vaccination coverage necessitates effective implementation of SIAs in countries that continue to experience high measles burden, with the success of these campaigns contingent upon high coverage of target populations likely to be missed by the routine vaccination program [12].
In this respect, measuring the overlap between routine measles vaccination coverage and measles SIAs is necessary to ensure the accurate estimation of the impact of countries’ full vaccination program, which can subsequently help policymakers in the selection between routine and SIA strategies for the second dose of measles vaccine to establish effective measles control. In addition, the lowest measles vaccination coverage and greatest risk of measles mortality are often concentrated in populations that are the most marginalized and disadvantaged economically [13]. Hence ensuring equitable coverage of measles vaccination is a further objective of SIAs.
Despite the widespread implementation of SIAs, marginalized populations that are not vaccinated through routine health services are often missed in vaccination campaigns, requiring additional efforts to serve these hard-to-reach populations [14–16]. A key question regarding coverage of marginalized populations is the degree to which current SIA outreach efforts have proven to be effective. To what extent are the children targeted and covered by measles SIAs previously unvaccinated and what are the characteristics of these children, as compared to those covered by the routine vaccination program? In other words, how many and what children who have not previously received a measles vaccine dose are reached by SIAs? Our analysis aims to address these questions using Demographic and Health Survey (DHS) data.
METHODS
The analysis focused on low- and middle-income countries (as classified by the World Bank) for which years and dates of SIAs were available from the WHO [17, 18]. A full list of all the countries with measles SIAs reviewed is included in the supplementary appendix (Table A). We relied on DHS data to determine the routine and SIA vaccination status of children. The DHS are nationally representative household-based surveys conducted periodically in more than 90 countries [19]. Each country survey includes a vaccination history for children under 5 years of age at the time of the survey. The interviewing approach of the DHS, which reconstructs the child’s history of vaccination according to the child’s health card and/or maternal reports of prior vaccination, is currently the best practice to determine the proportion of children covered by each vaccine at the time of the survey [20]. Specifically, for routine vaccination, if the health card of the child is available, DHS interviewers ask to see the card and transcribe the dates of each vaccination recorded on the card and also ask if the child has obtained other vaccinations that are not recorded. If the card is not available, interviewers ask the mother/guardian whether the child has received doses of each vaccine at any time before the survey, and, if so, how many doses [21].
We first examined the schedule of SIAs in the identified countries from 2000 to 2014 [18]. We then selected available survey years from the DHS that occurred one to two years following measles SIAs [22]. The survey data was inspected for availability of the “vaccinated during campaign” indicator, in order to determine if SIA (campaign) vaccination status was included in addition to routine vaccination status during the administration of the survey. In the included surveys, mothers were asked whether their children participated in a specific SIA (with possible answers being “yes,” “no,” or “don’t know”) for which the date of implementation was available [18]. While the mother/guardian is asked if additional doses not included on the vaccination card were received as described above, we do not rely on this question to classify children as vaccinated through routine or SIA, but instead we have only selected surveys where specific questions about SIAs are asked. Data included both routine and SIA vaccination status, child age at time of vaccination, and household wealth quintile. We also estimated the 95% confidence intervals (CIs) using a logit transform for the proportion of children receiving routine measles vaccination for each country in the analysis [23].
In order to estimate the proportion of children reached for each measles vaccination campaign among children with no previous history of vaccination, we first examined these children according to whether or not they were covered by the most recent measles SIA prior to the survey round in the DHS-derived dataset. We then examined the routine vaccination status of the children, according to the child’s vaccination card. There are several approaches to defining receipt of routine measles vaccination prior to the SIA with this dataset, including utilizing vaccination card information, either dates or check marks, and self-reported data. Of the children who reported routine measles vaccination coverage (MCV1) in the DHS dataset, approximately 55.6% have vaccination dates on their vaccination card, approximately 43.7% have self-reported vaccination, and 0.7% have marks on the vaccination card. Our preference in this analysis was to identify children with a measles vaccination date marked on the vaccination card prior to the initial date of the measles SIA, i.e. children with a history of measles vaccination prior to the SIA. This approach enabled us to estimate the proportion of SIA doses that reach children with no prior doses of measles vaccine (i.e., “zero-dose children”) before the initial date of the SIA. In order to estimate this proportion, for each scenario, the denominator was the number of children under five years of age reported as receiving a specific SIA measles vaccine. The numerator varied according to the definition of routine measles vaccination prior to the SIA within this dataset in order to find the children who received both measles SIA and routine vaccines, as described above.
The probability of reaching zero-dose children with measles SIAs was subsequently measured by household wealth quintile, according to the DHS wealth index defined as: poorest, poorer, middle, richer, richest [22]. We then tested for “trend” of SIA vaccination status by wealth quintile, relying on Cuzick’s nonparametric test for trend across ordered groups in STATA [24]. Additionally, we examined how SIAs might improve population immunity using standardized assumptions for vaccine efficacy: 85% for the first dose of measles vaccine before one year of age and 98% for the second dose at age one year or later [25–27].
We also compared two additional scenarios. First, we examined the proportion of zero-dose children including all children with routine measles vaccination, including those with vaccination date on the vaccination card, vaccination reported by mother, or vaccination marked on the vaccination card. Second, we examined the proportion of zero-dose children using imputed binary values (0 = zero-dose at time of SIA, 1 = already routinely vaccinated at time of SIA) for vaccination reported by mother and vaccination marked on the vaccination card. For the latter scenario, we rely on the multiple imputation (mi) command of a logistic regression in STATA and averaged over ten imputations. Multiple imputation utilizes the distribution of the observed data to correctly reproduce the variance/covariance matrix that would have been observed in a dataset without missing values [28, 29]. Using the weights provided with the DHS datasets, we also obtained a representative sample of children in order to better compare the estimated SIA coverage with routine measles vaccination coverage.
Finally, in a simple attempt to understand country determinants, we conducted further statistical analysis to examine what might be possible determinants of the estimated proportions of zero-dose children reached, using multivariate linear regression to analyze the impact of covariates relevant to the country contexts. These analyses were conducted at the country level. We examined the correlations between covariates and tested the covariates for significance at the 5% level (p-value < 0.05) both individually (with likelihood ratio testing) and as a set (with a nested models F-test). The examined covariates included MCV1, gross domestic product (GDP) per capita, population density, percentage of population in urban areas, health care expenditure per capita, WHO region, and World Bank income level. We included MCV1 coverage under the hypothesis that countries with lower MCV1 coverage might be more likely to have zero-dose children reached by SIAs. The remaining covariates were ones that would likely be associated with the accessibility and strength of the health system, which would also impact the numbers of zero-dose children. All analyses were implemented using STATA, version 12.
RESULTS
The comparison of the schedule of SIAs and available survey years from DHS yielded 49 potential countries with measles SIAs that occurred one to two years prior to the survey from an initial set of 111 countries with both measles SIA and DHS data available (Figure 1) [18, 22]. Following examination of this DHS data, 14 countries and 15 survey-years were identified with campaign vaccination information. The final 14 countries included in the analysis had DHS surveys ranging from 2002 to 2008. The full details of the relevant measles SIAs conducted are presented in Table 1.
Figure 1. Selection of the countries included in the analysis.
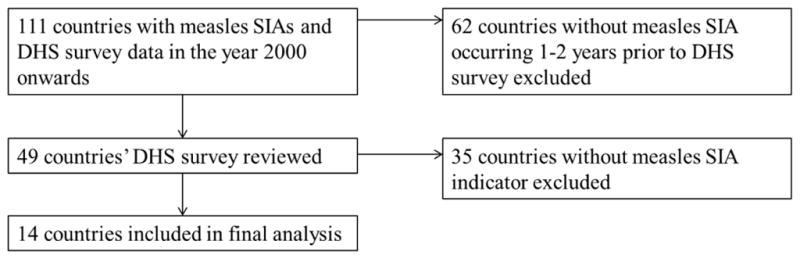
SIA = supplementary immunization activity; DHS = Demographic and Health Survey.
Table 1.
Details of measles supplementary immunization activities (SIAs) by country.
| Country | WHO Region | Gross domestic product per capita (2015 US$) | SIA year | DHS survey year |
|---|---|---|---|---|
| Benin | AFRO | $780 | 2005 | 2006 |
| Burkina Faso | AFRO | $620 | 2001 | 2003 |
| Democratic Republic of the Congo | AFRO | $480 | 2007 | 2007 |
| Ghana | AFRO | $1,360 | 2001 2002 |
2003 |
| Ghana | AFRO | $1,360 | 2006 | 2008 |
| Guinea | AFRO | $550 | 2002 2003 |
2005 |
| Haiti | AMRO | $810 | 2001 2002 |
2005 |
| Honduras | AMRO | $2,330 | 2004 | 2005 |
| Indonesia | SEARO | $3,340 | 2002 2002 |
2002 |
| Kenya | AFRO | $1,350 | 2002 | 2003 |
| Lesotho | AFRO | $1,070 | 2000 2003 |
2004 |
| Niger | AFRO | $360 | 2004 2005 |
2006 |
| Nigeria | AFRO | $2,660 | 2005 2006 |
2008 |
| São Tomé and Príncipe | AFRO | $1,630 | 2007 | 2008 |
| Sierra Leone | AFRO | $590 | 2003 2006 |
2008 |
DHS = Demographic and Health Survey. WHO=World Health Organization. AFRO=WHO Regional Office for Africa; AMRO=WHO Regional Office for the Americas; SEARO=WHO Regional Office for Southeast Asia.
The unweighted sample size of children both reached by the measles SIA and covered by the DHS ranged from 121 in Haiti to 9,620 in Indonesia. When restricting to children who received both a routine and SIA dose, the unweighted range changes to: (1) 108 – 7,505 without exclusions; (2) 46 – 1,500 excluding self-reported routine vaccination; and (3) 31 – 1,330 including only children with a measles vaccination date on their vaccination card. Table 2 provides the full range of sample sizes included in the analysis. Among these children, prior receipt of measles vaccine in the routine program was defined as having a date of measles vaccination on their vaccination card prior to the initial date of the measles SIA. For these children, the proportion of zero-dose children reached ranged from 28% (95% CI: 25–31%) in São Tomé and Príncipe to 91% (90–93%) in Nigeria. While not regionally representative, the two countries from the Americas, Haiti and Honduras, are nearly equal at 51% (43–60%) and 53% (51–55%), respectively; while Indonesia, as the lone country from Southeast Asia reaches approximately 86% (85–87%) zero-dose children with SIAs (Table 2).
Table 2.
Measles supplementary immunization activities (SIA) proportions of zero-dose children reached (95% confidence intervals in parentheses) – base case scenario*
| Country | DHS survey year | Number of children with immunization data | Number of children who received SIA measles vaccine | Number of children who received both measles SIA and routine vaccines** | Proportion of zero-dose children reached with SIA |
|---|---|---|---|---|---|
| Benin | 2006 | 8,331 | 3,000 | 908 | 70% (68–72%) |
| Burkina Faso | 2003 | 3,936 | 143 | 31 | 78% (70–86%) |
| Democratic Republic of the Congo | 2007 | 4,798 | 1,898 | 221 | 88% (87–90%) |
| Ghana | 2003 | 2,608 | 1,722 | 863 | 50% (48–52%) |
| Ghana | 2008 | 1,502 | 535 | 243 | 55% (51–59%) |
| Guinea | 2005 | 2,398 | 1,220 | 479 | 61% (58–63%) |
| Haiti | 2005 | 673 | 121 | 59 | 51% (43–60%) |
| Honduras | 2005 | 6,443 | 1,788 | 841 | 53% (51–55%) |
| Indonesia | 2002 | 11,939 | 9,620 | 1,330 | 86% (85–87%) |
| Kenya | 2003 | 3,527 | 1,464 | 444 | 70% (67–72%) |
| Lesotho | 2004 | 1,989 | 760 | 342 | 55% (52–59%) |
| Niger | 2006 | 4,176 | 2,425 | 710 | 71% (69–73%) |
| Nigeria | 2008 | 7,100 | 1,713 | 148 | 91% (90–93%) |
| São Tomé and Príncipe | 2008 | 1,333 | 614 | 442 | 28% (25–31%) |
| Sierra Leone | 2008 | 2,190 | 1,222 | 219 | 82% (79–85%) |
DHS = Demographic and Health Survey.
Unweighted sample sizes including only children who would have had the opportunity to be eligible for both SIA and routine vaccination prior to the SIA according to the WHO recommendation for routine measles vaccination at 9 months of age.
Routine measles vaccination with vaccination date on card prior to the initial date of the measles SIA.
Note: “Zero-dose children” are defined as children with no previous history of measles vaccination.
However, in the first scenario analysis, if vaccination reported by mother or marked on the vaccination card without a date was included, the proportion of zero-dose children reached by SIAs decreased to 12% overall, from as low as 1% (95% CI: 0–5%) in Honduras up to 22% (20–24%) in Indonesia (Table 3). In the second scenario analysis, relying on multiple imputation to simulate the self-reported data, the proportion of zero-dose children reached lay in between the base case analysis and the first scenario analysis at 58% overall. The proportion of zero-dose children reached ranged from 27% (20–34%) in São Tomé and Príncipe to 86% (86–87%) in Nigeria. We also show that the children in the DHS who do and do not receive SIA vaccination do not drastically differ by the type of routine measles vaccination data (Supplementary appendix, table B). In the supplementary appendix (Table C), we included an analysis of the maternal age, maternal education, wealth quintile, and percent of households in urban areas for those with and without a vaccination date on their vaccination card.
Table 3.
Scenario analyses of measles supplementary immunization activities (SIA) proportions of zero-dose children reached (95% confidence intervals in parentheses).
| Country | DHS survey year | Proportion of zero-dose children reached with SIA | ||
|---|---|---|---|---|
|
| ||||
| Base case* | Scenario analysis 1** | Scenario analysis 2*** | ||
| Benin | 2006 | 70% (68–72%) | 19% (15–22%) | 67% (65–69%) |
| Burkina Faso | 2003 | 78% (70–86%) | 20% (3–36%) | 73% (66–79%) |
| Democratic Republic of the Congo | 2007 | 88% (87–90%) | 11% (8–15%) | 82% (81–83%) |
| Ghana | 2003 | 50% (48–52%) | 11% (7–15%) | 39% (36–43%) |
| Ghana | 2008 | 55% (51–59%) | 4% (0–12%) | 37% (33–41%) |
| Guinea | 2005 | 61% (58–63%) | 17% (10–22%) | 32% (29–34%) |
| Haiti | 2005 | 51% (43–60%) | 11% (0–30%) | 48% (41–55%) |
| Honduras | 2005 | 53% (51–55%) | 1% (0–5%) | 34% (32–36%) |
| Indonesia | 2002 | 86% (85–87%) | 22% (20–24%) | 75% (74–76%) |
| Kenya | 2003 | 70% (67–72%) | 13% (8–18%) | 57% (55–59%) |
| Lesotho | 2004 | 55% (52–59%) | 3% (1–10%) | 39% (36–43%) |
| Niger | 2006 | 71% (69–73%) | 16% (12–20%) | 69% (67–71%) |
| Nigeria | 2008 | 91% (90–93%) | 15% (10–18%) | 86% (86–87%) |
| São Tomé and Príncipe | 2008 | 28% (25–31%) | 6% (0–11%) | 27% (20–34%) |
| Sierra Leone | 2008 | 82% (79–85%) | 12% (6–18%) | 68% (65–71%) |
Measles vaccination defined as a measles vaccination date marked on the vaccination card prior to the initial date of the measles SIA.
Routine measles vaccination includes vaccination date on card, vaccination reported by mother, or vaccination marked on card.
Routine measles vaccination includes vaccination date on card and imputed values for vaccination reported by mother and vaccination marked on card.
DHS = Demographic and Health Survey.
Note: “Zero-dose children” are defined as children with no previous history of measles vaccination.
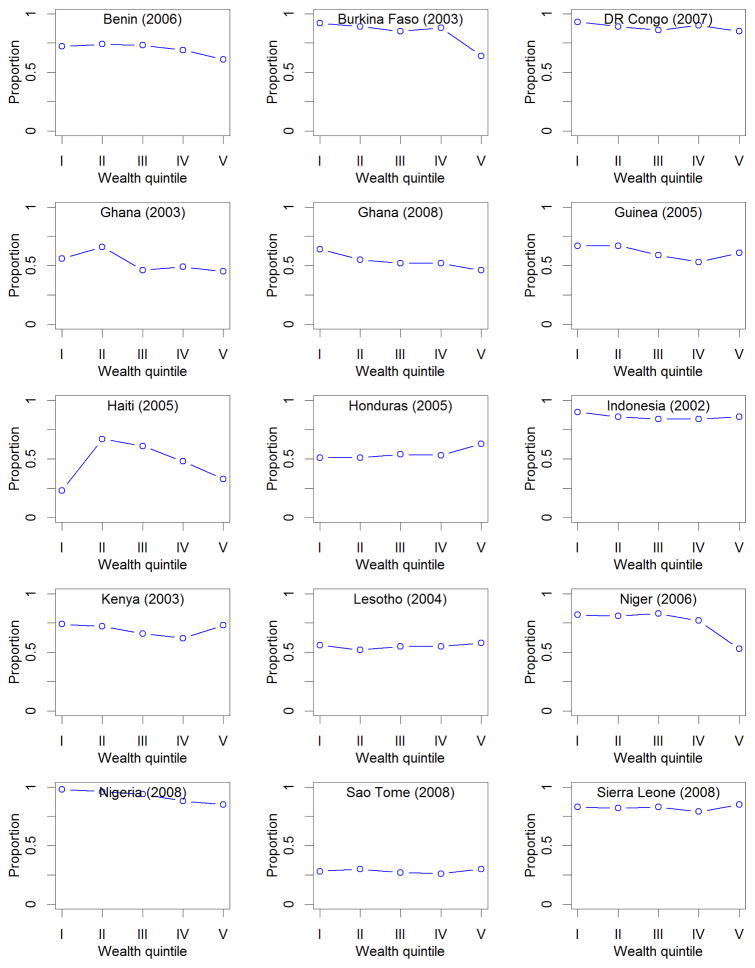
Figure 2 presents results for the proportion of zero-dose children reached with SIAs by household wealth quintile in each country. Generally, the proportions of zero-dose children reached declines with increasing wealth, with those from the poorest households being more likely to be reached by the SIA than those from the richest households. For example, in Burkina Faso, the SIA was 92% (95% CI: 88–95%) likely to reach zero-dose children from the poorest households while only 64% (60–67%) likely to reach children from the richest households; whereas, in the Democratic Republic of the Congo, the proportion ranged from 93% (89–97%) in the poorest to 85% (81–88%) in the richest. In testing for “trend” of SIA vaccination status by wealth quintile, we found a lack of trend in the majority of countries, indicating non-discriminatory SIAs. However, we found a significant trend that SIA vaccination declines with increasing wealth in Burkina Faso, Guinea, Haiti, Indonesia, and Niger, suggesting that SIAs in these countries would be pro-poor (Supplementary appendix, table D). No country had a significant trend in which SIA vaccination increased with increasing wealth.
Figure 2. Proportion of zero-dose children reached with supplementary immunization activities by household wealth quintile, in each of the countries studied (DHS survey year is indicated in parentheses).
DHS = Demographic and Health Survey.
Note: “Zero-dose children” are defined as children with no previous history of measles vaccination, defined as a measles vaccination date marked on the vaccination card prior to the initial date of the measles SIA.
Across the 14 countries in the analysis, SIAs could improve population immunity by 4% (95% CI: 3–5%) when defining measles vaccination as having a measles vaccination date on the vaccination card prior to the initial date of the measles SIA. When the definition is expanded to include vaccination reported by mother or marked on the vaccination card without a date, this improvement could increase to 11% (10–12%) (Supplementary appendix, table E).
In the country determinants analysis, none of the examined covariates – routine measles vaccination coverage, GDP per capita, health care expenditure per capita, population density, percentage of population in urban areas – were statistically significant in the prediction of the proportion of zero-dose children reached in the model (Table 4).
Table 4.
Results of country-level determinants analysis of the proportion of zero-dose children reached with supplementary immunization activities.
| Variable | Coefficient | Standard error | Regression p-value | Correlation coefficient | Correlation p-value |
|---|---|---|---|---|---|
| Constant | 1.078 | 0.287 | 0.01 | N/A | N/A |
| Routine measles immunization coverage | −0.004 | 0.005 | 0.46 | −0.495 | 0.06 |
| Gross domestic product per capita | 0.001 | 0.001 | 0.91 | −0.210 | 0.45 |
| Population density | −0.001 | 0.001 | 0.68 | −0.310 | 0.26 |
| Percent of urban population | −0.004 | 0.006 | 0.54 | −0.417 | 0.12 |
| Health care expenditure per capita | 0.002 | 0.005 | 0.79 | −0.255 | 0.36 |
| WHO Africa region fixed effect | (reference) | ||||
| WHO Americas region fixed effect | −0.083 | 0.195 | 0.69 | N/A | N/A |
| WHO Southeast Asia region fixed effect | 0.331 | 0.258 | 0.25 | N/A | N/A |
| Low-income country fixed effect | (reference) | ||||
| Lower middle-income country fixed effect | −0.113 | 0.179 | 0.55 | N/A | N/A |
WHO = World Health Organization. A full list of countries by WHO region is included in the supplementary appendix (Table A).
Note: “Zero-dose children” are defined as children with no previous history of measles vaccination.
The correlation between the proportion of zero-dose children reached and each covariate is generally low, with correlation coefficients ranging between −0.2 and −0.4, and insignificant. However, the proportion of zero-dose children reached and routine measles vaccination coverage were moderately correlated at −0.50 (95% CI: −0.80–0.02), indicating near significance at the 5% level (p-value = 0.06).
DISCUSSION
We examined the probability that measles SIAs reached children with no previous history of measles vaccination in fourteen low- and middle-income countries. Specifically, we found, in our base case scenario (defining measles vaccination as a measles vaccination date marked on the vaccination card prior to the initial date of the measles SIA) that the proportion of zero-dose children – children with no prior doses of measles vaccine – reached by SIAs ranged from a low 28% (95% CI: 25%–31%) in São Tomé and Príncipe to a high 91% (90–93%) in Nigeria (Table 2). Yet, recall the findings of the two scenario analyses, which showed a range of 1% (0–5%) in Honduras up to 22% (20–24%) in Indonesia in scenario one (adding vaccination marks on the vaccination card and vaccinated reported by the mother to the definition of measles vaccination) and a range of 27% (20–34%) in São Tomé and Príncipe to 86% (86–87%) in Nigeria in scenario two (imputing routine measles vaccination for vaccination marks on the vaccination card and vaccinated reported by the mother).
We also found that the proportion of zero-dose children reached by SIAs declined with increasing wealth on average, although these equity improvements were not seen in each country. In São Tomé and Príncipe, in our base case scenario, this proportion ranged from 28% (18%–37%) in the poorest wealth quintile to 30% (22%–37%) in the highest wealth quintile; while in Nigeria, the proportion ranged from 98% (95%–100%) in the poorest wealth quintile to 85% (83%–87%) in the highest (Figure 2).
This analysis examined how SIAs would strengthen measles control efforts and achieve their objective by identifying the zero-dose children reached compared with those children previously reached by routine vaccination efforts. This enables better assessment of the “real-world” impact of routine vaccination and SIA efforts in achieving the worldwide goals of measles control and elimination. In order to examine the probability of reaching zero-dose children, we defined SIA vaccination in the analysis as children with the vaccination date prior to the date of the SIA included on their vaccination card, as we had the greatest confidence of true MCV1 coverage with this approach. The ensuing proportion of zero-dose children reached is likely to be an overestimate, as children with the self-report of the mother or a mark on their vaccination card might also have received a routine vaccination prior to the campaign.
Therefore, we also examined the proportion of zero-dose children reached for all data types – vaccination date on the vaccination card, vaccination reported by mother, or vaccination marked on the vaccination card – as well as an imputation of vaccination reported by mother and vaccination marked on the vaccination card in scenario analyses (Table 3). In the first scenario analysis, we found that the proportion of zero-dose children reached by SIAs was much lower than the proportions in the primary analysis (12% vs. 66%), while the imputation showed a proportion of zero-dose children reached closer to that of the primary analysis (58% vs. 66%). While the first scenario analysis might overestimate MCV1 coverage, self-reported data is included in current estimates of routine measles vaccination coverage [30] and, therefore, it may be a more accurate reflection of the true overlap between routine and SIA vaccination efforts. However, there is inherent uncertainty in the data for children with a vaccination mark on the card (0.7% of data set) or self-reported data (43.7% of data set) [31]. Without a vaccination date provided, it is not clear whether a vaccination mark indicates a routine vaccination that did indeed take place before the SIA or whether a self-reported vaccination was received via routine vaccination or via measles SIA. Despite this uncertainty, the first scenario analysis provides a lower bound for the proportion of zero-dose children reached if all children reporting measles vaccination in the DHS are included. Additionally, it is important to note that the children who are and are not reached by SIA vaccination in the DHS do not drastically differ by the type of routine measles vaccination data (Supplementary appendix, table B). In other words, the children reached by SIAs are not necessarily more or less likely to have a vaccination date on their vaccination card than the children who were not reached. Furthermore, the proportion of zero-dose children reached with SIAs by household wealth quintile similarly declines with increasing wealth when self-reported data is included (Supplementary appendix, figure F), indicating that any differences of having vaccination cards by wealth quintile do not affect the general distributional impact of SIAs.
However, there may be demographic differences between children with a date on their vaccination card compared to those without, indicating that access might be affecting the numbers of zero-dose children. In the supplementary appendix (Table C), we included an analysis of the maternal age, maternal education, wealth quintile, and percent of households in urban areas for those with and without a vaccination date on their vaccination card. The percentage of households in urban areas does not appear to have a consistent relationship with the percentage of children with a vaccination date on their vaccination card, with 47% of countries having a greater percentage of households in urban areas among those with a vaccination date on their card compared to 43% of countries where there is a greater percentage among those without a vaccination date. While mean maternal age and mean years of maternal education do not differ by more than 7%, there are larger differences for mean wealth quintile for some countries. For mean wealth quintile, seven countries differ by less than 5%, six countries differ by less than 15%, and two countries (Niger and Nigeria) differ by 23% and 28%. Therefore, as we might expect, there appears to be differences in households being able to access routine health services according to wealth, borne out by the analyses of distributional impact of SIAs.
We observed a range of proportions of zero-dose children reached by measles SIAs among the countries in this analysis, with some seemingly more effective at selective targeting than others, depending on the definition of measles vaccination being utilized (e.g., vaccination dates on the vaccination card, vaccination marks on the vaccination card, and/or self-reported data). It is likely that countries with relatively low coverage for measles in the routine vaccination program, such as Nigeria, might have higher proportions of zero-dose children reached. In fact, Nigeria has the lowest MCV1 coverage of the countries in our analysis at 43% around the years of its SIA (2005–6) [4]. In Table 5, we compare the weighted SIA coverage using the weights provided with each DHS dataset with MCV1 coverage. If we assume a representative sample using these weights, given national SIAs, we can likewise estimate the increase in measles coverage from SIAs (Table 5). We also examined the potential improvements in immunity levels due to SIAs, finding a 4–11% increase in immunity from SIAs (Supplementary appendix, table E). However, this broad estimation has been computed using standardized assumptions for vaccine efficacy (85% for the first dose of measles vaccine and 98% for the second dose) as country-level data is not available [25–27], which hides enormous heterogeneity across and within countries. Vaccine efficacy is also potentially reduced in the field as compared to facility-based routine settings, due to issues of climate, timeliness, and the quality of the cold chain. Without additional serological testing, the true immunity levels before and after SIAs remain uncertain [32]. Moreover, in countries with low routine vaccination coverage (at the time of the survey), the role of immunity due to natural infection may be more dramatic, such that the second dose of measles vaccine may not have as large of an impact as estimated in this analysis.
Table 5.
Comparison of supplementary immunization activity (SIA) weighted coverage reaching zero-dose children with coverage of routine measles first dose (MCV1)
| Country | DHS survey year | Weighted proportion of zero-dose children reached with SIA (95% CI) | MCV1 coverage during SIA* | Increase in measles vaccine coverage after SIA (95% CI)** |
|---|---|---|---|---|
| Benin | 2006 | 70% (68–72%) | 61% | 27% (26–29%) |
| Burkina Faso | 2003 | 74% (64–83%) | 63% | 27% (18–37%) |
| Democratic Republic of the Congo | 2007 | 89% (87–91%) | 68% | 28% (27–30%) |
| Ghana | 2003 | 51% (49–54%) | 78% | 11% (9–14%) |
| Ghana | 2008 | 53% (49–57%) | 85% | 8% (4–12%) |
| Guinea | 2005 | 60% (57–63%) | 47% | 32% (29–35%) |
| Haiti | 2005 | 47% (37–57%) | 56% | 21% (10–31%) |
| Honduras | 2005 | 59% (56–61%) | 92% | 5% (2–7%) |
| Indonesia | 2002 | 87% (86–88%) | 72% | 24% (23–26%) |
| Kenya | 2003 | 66% (63–69%) | 78% | 15% (12–17%) |
| Lesotho | 2004 | 56% (52–60%) | 80% | 11% (7–15%) |
| Niger | 2006 | 79% (77–81%) | 46% | 43% (41–45%) |
| Nigeria | 2008 | 90% (88–92%) | 43% | 51% (49–53%) |
| São Tomé and Príncipe | 2008 | 20% (16–24%) | 86% | 3% (0–7%) |
| Sierra Leone | 2008 | 83% (79–86%) | 69% | 26% (23–29%) |
The year of MCV1 coverage listed is the year during which the SIA took place. Source: World Health Organization. (2015). WHO/UNICEF coverage estimates for 1980–2014. Geneva: WHO/UNICEF. Last updated: 4 November 2015.
Assumes that the weighted SIA coverage addresses the current gap in MCV1 coverage, i.e., (1 – MCV1 coverage)*(Weighted proportion of zero-dose children reached with SIA).
Note: “Zero-dose children” are defined as children with no previous history of measles vaccination.
The correlation coefficient between the SIA proportion of zero-dose children reached and the routine measles first dose coverage was indeed −0.50, and is nearly significant (0.06) despite the small sample size. Meanwhile, in this analysis, the island nation of São Tomé and Príncipe, with both high routine coverage (86% in the year of the SIA) and a small population (less than 200,000), was unlikely to reach zero-dose children with SIAs, which may be true for other countries able to achieve a high level of routine coverage [4, 33]. Table G in the supplementary appendix provides routine coverage for MCV1 for the countries in this analysis from 2000 to 2014 [4].
Nevertheless, this analysis presents a number of limitations, which complicate drawing generalizable conclusions from its findings. First, the small sample size in the numbers of children with measles SIA data collected in the DHS is a limiting factor. Second, while information collected in DHS is subject to reporting and recall biases (although evidence from Egypt suggests that mothers’ reports can be of high quality [20]), we relied on the approach of estimating the proportion of zero-dose children reached with dates copied from the vaccination card in order to counteract these potential biases, but also pursued a number of additional scenario analyses (Table 3). Moreover, as all scenarios analyzed utilize a denominator derived from the DHS question on whether a “child was vaccinated during campaign,” there is additional uncertainty regarding the accuracy of the reported information, as it is similarly subject to reporting and recall biases. As DHS surveys use complex sampling and require weights for country-level estimates, but the primary analysis is unweighted, the estimated proportions may not be reflective of the proportion reached at the national level, and do not indicate coverage. However, the country-level weighted estimates in Table 5 do not greatly differ from the unweighted proportions in Table 2, as the same DHS weights are used to weight both the numerators and denominators to arrive at the estimates in Table 5. In analyzing what might be the country determinants of SIAs reaching zero-dose children, the lack of significance of the country-level covariates tested (Table 4) suggests that there would not be clear country-level predictors of success in reaching zero-dose children. We further compared the proportion of zero-dose children reached to routine measles vaccination coverage in the year of the SIA in order to confirm that there is indeed a clear correlation between this outcome and MCV1 (Table 5). However, the lack of significance may also be due to the small sample size of countries meeting our criteria for inclusion in the study. As additional empirical evidence on the overlap between routine and SIA delivery of measles vaccination becomes available, this type of analysis should be re-examined. For example, future research might include serosurveys using immunoassays examining measles antibodies to compare the presence of measles immunoglobulin before and after SIA rollout.
In prior analyses, SIAs have not only been shown to be effective at providing a second opportunity for measles vaccination, but also more equitable measles vaccination coverage by strengthening coverage among children from lower socio-economic status [21, 34]. A previous analysis also found that the percentage of zero-dose children vaccinated in SIAs declined with increasing wealth, such that the largest proportions were from the poorest households [34]. On the other hand, another analysis suggests that SIAs are often biased towards those with previous high access to vaccination, estimating an effective coverage level (i.e., proportion of the remaining susceptible population immunized by the campaign) up to 50% [35]. While these two analyses examine SIA impact in a single country (Kenya and Malawi, respectively), this analysis goes a step further in examining the impact across fourteen low- and middle-income countries. Our analysis generally follows the former storyline, with the proportions of zero-dose children reached being highest among the poorest households on average. These results provide evidence of the impact of measles SIAs overall leading to more equitable measles vaccination coverage.
This research is also a starting point to examine what might be the impact of ‘vertical’ delivery of specific health interventions on the ‘horizontal’ delivery of primary and preventive services in the health system, and the broader benefits and disadvantages of SIAs. Our analysis shows improvements in measles coverage due to SIAs, thus supplementing the efforts of routine vaccination, and increases in equity by reaching children from poorer households. But beyond the scope of our analysis and measles vaccination, previous work examining the impact of measles SIAs on the broader health system have ranged from positive to negative associations with system functioning [36–40]. For example, there remains the potential for challenges to the health system if measles SIAs are relied upon as a replacement for weak routine vaccination programs rather than as a supplementary improvement to routine vaccination services. Some have recommended that SIAs must have “reached, and sustained, a predetermined level” in order to counteract the potential for these efforts to supplant or mask weak routine vaccination programs [41]. Furthermore, others have proposed that continued efforts towards measles control should focus specifically on strengthening the routine vaccination program, integrating vaccination with other health services, and encouraging donor support of primary health care [42].
As decision-makers evaluate measles control decisions, the ability to accurately demonstrate what future efforts are needed for measles control will be critical. This research can serve to elucidate some, but not all, of the uncertainty around the SIA impact by providing information in specific country contexts that can be used to evaluate measles control achievements. By estimating the real-world effectiveness of SIAs reaching those children not always reached by routine health systems, we can provide valuable insight into the estimation of public health impact towards measles control and elimination. Additionally, this paper also highlights the important role that SIAs can play in improving equity by increasing vaccination coverage beyond routine levels and reaching children from poorer households.
Supplementary Material
Highlights.
SIAs improve equity by increasing coverage beyond routine levels
We quantified the likelihood that SIAs reach those w/no prior measles vaccination
The average proportion of zero-dose children reached by SIAs was 66%
The likelihood of reaching zero-dose children declined with increasing wealth
Acknowledgments
Earlier versions of this paper were presented at the Harvard T.H. Chan School of Public Health, and we received valuable comments from seminar participants, including Barry Bloom and Till Bärnighausen.
Footnotes
Disclaimer: This research was supported by Gavi, the Vaccine Alliance and by a grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R03HD082443. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Gavi.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Simons E, Ferrari M, Fricks J, et al. Assessment of the 2010 global measles mortality reduction goal: results from a model of surveillance data. Lancet. 2012;379(9832):2173–2178. doi: 10.1016/S0140-6736(12)60522-4. [DOI] [PubMed] [Google Scholar]
- 2.Bryce J, Boschi-Pinto C, Shibuya K, et al. WHO estimates of the causes of death in children. Lancet. 2005;365(9465):1147–1152. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Measles. World Health Organization Fact Sheet No. 286. 2015 Last updated November 2015. Available at: http://www.who.int/mediacentre/factsheets/fs286/en/
- 4.World Health Organization. WHO/UNICEF coverage estimates for 1980–2014. Geneva: WHO/UNICEF; 2015. Last updated: 4 November 2015. Available at: http://www.who.int/immunization/monitoring_surveillance/routine/coverage/en/index4.html. [Google Scholar]
- 5.Harris JB, Gacic-Dobo M, Eggers R, et al. Global routine vaccination coverage, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(46):1055–1058. [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Measles vaccines: WHO position paper – April 2017. Weekly epidemiological record. No 17. 2017;92:205–228. Available at: http://www.who.int/wer. [Google Scholar]
- 7.Dowdle WR. The principles of disease elimination and eradication. Bull World Health Organ. 1998;76(Suppl 2):22–25. [PMC free article] [PubMed] [Google Scholar]
- 8.Heymann DL. Control, elimination, eradication and re-emergence of infectious diseases: getting the message right. Bull World Health Organ. 2006;84(2):82. doi: 10.2471/blt.05.029512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melgaard B, Creese A, Aylward B, et al. Disease eradication and health systems development. Morbidity and Mortality weekly Report (MMR) Supplement--global disease elimination and eradication as public health strategies. 1999;48:28–35. [Google Scholar]
- 10.World Health Organization. Global Vaccine Action Plan, 2011–2020. Geneva: 2013. Available at: http://www.unicef.org/immunization/files/GVAP(1).pdf. [Google Scholar]
- 11.World Health Organization. Global measles and rubella strategic plan: 2012–2020. Geneva: 2012. Available at: http://measlesrubellainitiative.org/learn/the-solution/the-strategy/ [Google Scholar]
- 12.Mbabazi WB, Nanyunja M, Makumbi I, et al. Achieving measles control: lessons from the 2002–06 measles control strategy for Uganda. Health Policy Plan. 2009;24(4):261–269. doi: 10.1093/heapol/czp008. [DOI] [PubMed] [Google Scholar]
- 13.Johri M, Verguet S, Morris SK, et al. Adding interventions to mass measles vaccinations in India. Bull World Health Organ. 2016;94(10):718–727. doi: 10.2471/BLT.15.160044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doumtsop JG, Malano ER, Diallo IT, et al. An evaluation of the 2012 measles mass vaccination campaign in Guinea. Pan Afr Med J. 2014;17:4. doi: 10.11604/pamj.2014.17.4.2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu X, Xiao S, Chen B, et al. Gaps in the 2010 measles SIA coverage among migrant children in Beijing: evidence from a parental survey. Vaccine. 2012;30(39):5721–5725. doi: 10.1016/j.vaccine.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 16.McBean AM, Foster SO, Herrmann KL, et al. Evaluation of a mass measles immunization campaign in Yaounde, Cameroun. Trans R Soc Trop Med Hyg. 1976;70(3):206–212. doi: 10.1016/0035-9203(76)90040-7. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Proceedings of the Global Technical Consultation to assess the feasibility of measles eradication, 28–30 July 2010. J Infect Dis. 2011;204(Suppl 1):S4–13. doi: 10.1093/infdis/jir100. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Immunization Vaccines and Biologicals (IVB) World Health Organization; Retrospective Measles Data on Supplementary Immunization Activities 2000–2014. Data source: WHO/IVB Database, last updated 30 October 2014. [Google Scholar]
- 19.Corsi DJ, Neuman M, Finlay JE, et al. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41(6):1602–1613. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 20.Langsten R, Hill K. The accuracy of mothers’ reports of child vaccination: evidence from rural Egypt. Soc Sci Med. 1998;46(9):1205–1212. doi: 10.1016/s0277-9536(97)10049-1. [DOI] [PubMed] [Google Scholar]
- 21.Helleringer S, Abdelwahab J, Vandenent M. Polio supplementary immunization activities and equity in access to vaccination: evidence from the demographic and health surveys. J Infect Dis. 2014;210(Suppl 1):S531–539. doi: 10.1093/infdis/jiu278. [DOI] [PubMed] [Google Scholar]
- 22.ICF International. Demographic and Health Surveys (various) [Datasets] Calverton, Maryland: ICF International [Distributor]; 2015. 2003–2008. [Google Scholar]
- 23.StataCorp. Stata 13 Base Reference Manual. College Station, TX: Stata Press; 2013. [Google Scholar]
- 24.Cuzick J. A Wilcoxon-type test for trend. Statistics in Medicine. 1985;4(1):87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 25.Sudfeld CR, Navar AM, Halsey NA. Effectiveness of measles vaccination and vitamin A treatment. Int J Epidemiol. 2010;39(Suppl 1):i48–55. doi: 10.1093/ije/dyq021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clements CJ, Strassburg M, Cutts FT, et al. The epidemiology of measles. World Health Stat Q. 1992;45(2–3):285–291. [PubMed] [Google Scholar]
- 27.Orenstein WA, Markowitz LE, Atkinson WL, et al. Worldwide measles prevention. Isr J Med Sci. 1994;30(5–6):469–481. [PubMed] [Google Scholar]
- 28.Johnson DR, Young R. Towards Best Practices in analyzing Datasets with Missing Data: Comparisons and Recommendations. Journal of Marriage and Family. 2011;73(5):926–945. [Google Scholar]
- 29.White IR. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine. 2011;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 30.Burton A, Monasch R, Lautenbach B, et al. WHO and UNICEF estimates of national infant immunization coverage: methods and processes. Bull World Health Organ. 2009;87(7):535–541. doi: 10.2471/BLT.08.053819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murray CJ, Shengelia B, Gupta N, et al. Validity of reported vaccination coverage in 45 countries. Lancet. 2003;362(9389):1022–1027. doi: 10.1016/S0140-6736(03)14411-X. [DOI] [PubMed] [Google Scholar]
- 32.Colson KE, Zuniga-Brenes P, Rios-Zertuche D, et al. Comparative Estimates of Crude and Effective Coverage of Measles Immunization in Low-Resource Settings: Findings from Salud Mesoamerica 2015. PLoS One. 2015;10(7):e0130697. doi: 10.1371/journal.pone.0130697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Bank. World development indicators. Washington, DC: The World Bank; 2015. (Last updated: 16-Dec-2015). Available at: http://data.worldbank.org/ [Google Scholar]
- 34.Vijayaraghavan M, Martin RM, Sangrujee N, et al. Measles supplemental immunization activities improve measles vaccine coverage and equity: Evidence from Kenya, 2002. Health Policy. 2007;83(1):27–36. doi: 10.1016/j.healthpol.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Minetti A, Hurtado N, Grais RF, et al. Reaching hard-to-reach individuals: Nonselective versus targeted outbreak response vaccination for measles. Am J Epidemiol. 2014;179(2):245–251. doi: 10.1093/aje/kwt236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verguet S, Jassat W, Hedberg C, et al. Measles control in Sub-Saharan Africa: South Africa as a case study. Vaccine. 2012;30(9):1594–1600. doi: 10.1016/j.vaccine.2011.12.123. [DOI] [PubMed] [Google Scholar]
- 37.Verguet S, Jassat W, Bertram MY, et al. Impact of supplemental immunisation activity (SIA) campaigns on health systems: findings from South Africa. J Epidemiol Community Health. 2013;67(11):947–952. doi: 10.1136/jech-2012-202216. [DOI] [PubMed] [Google Scholar]
- 38.Hanvoravongchai P, Mounier-Jack S, Oliveira Cruz V, et al. Impact of measles elimination activities on immunization services and health systems: findings from six countries. J Infect Dis. 2011;204(Suppl 1):S82–89. doi: 10.1093/infdis/jir091. [DOI] [PubMed] [Google Scholar]
- 39.Koehlmoos TP, Uddin J, Sarma H. Impact of measles eradication activities on routine immunization services and health systems in Bangladesh. J Infect Dis. 2011;204(Suppl 1):S90–97. doi: 10.1093/infdis/jir086. [DOI] [PubMed] [Google Scholar]
- 40.Mounier-Jack S, Edengue JM, Lagarde M, et al. One year of campaigns in Cameroon: effects on routine health services. Health Policy Plan. 2016;31(9):1225–1231. doi: 10.1093/heapol/czw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heymann DL, Fine PE, Griffiths UK, et al. Measles eradication: past is prologue. Lancet. 2010;376(9754):1719–1720. doi: 10.1016/S0140-6736(10)61934-4. [DOI] [PubMed] [Google Scholar]
- 42.Griffiths UK, Mounier-Jack S, Oliveira-Cruz V, et al. How can measles eradication strengthen health care systems? J Infect Dis. 2011;204(Suppl 1):S78–81. doi: 10.1093/infdis/jir090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.