Abstract
To date, there is little understanding of how contextual factors may influence the decisions individuals make regarding the adoption of options for hearing rehabilitation. This explorative retrospective study investigated whether hearing aid adoption and return rates are associated with the time of the day at which an appointment takes place. The study sample consisted of 24,842 patients experiencing their first audiology appointment. It was observed that hearing aid adoption was significantly associated with appointment times whereby lower hearing aid adoption rates were observed at noon and 4 p.m. It was also observed that hearing aid return rates were significantly associated with appointment times whereby lower return rates were observed at noon and 4 p.m. In light of the methodology employed in the study, it is not possible to unequivocally determine why time of day is associated with hearing aid adoption and return rates. Several possible explanations for the patterns of associations are discussed. In light of previous research observing that hunger lowers risk tolerance and glucose consumption increases risk tolerance, the results are consistent with an interpretation based on risk-aversion resulting from hunger. To establish causality between hunger and decision-making in audiology, additional research employing experimental methodologies are necessary.
Keywords: hearing aid adoption, decision-making, time of day, hearing loss, hearing rehabilitation
Introduction
Disabling hearing loss compromises the ability to fully participate in society and results in negative consequences in economic, physical, cognitive, psychosocial, emotional, and behavioral domains (Ciorba, Bianchini, Pelucchi, & Pastore, 2012; Dalton et al., 2003; Lin, Thorpe, Gordon-Salant, & Ferrucci, 2011). Hearing aids are often an essential component of hearing loss rehabilitation. A systematic review on the effects of hearing aid usage found that their use results in improved quality of life and decreased psychological and socioemotional consequences observed with hearing loss (Chisolm et al., 2007). Critically, the uptake of hearing aids remains low with only about 20% to 33% of individuals who could potentially benefit from hearing aids actually reporting current use of hearing aids (Abrams & Kihm, 2015; Bainbridge & Ramachandran, 2014; Kochkin, 2007).
There are several reviews of the factors associated with hearing aid adoption (Jenstad & Moon, 2011; Meyer & Hickson, 2012; Ng & Loke, 2015; Vestergaard Knudsen et al., 2010). Investigations attempting to identify correlates of hearing aid adoption tend to focus on variables associated with the patient. Such variables include age (Hartley, Rochtchina, Newall, Golding, & Mitchell, 2010), degree of audiometric hearing sensitivity (Garstecki & Erler, 1998; Popelka et al., 1998), race and socioeconomic status, (Gussekloo et al., 2003; Helvik, Wennberg, Jacobsen, & Halberg, 2008), sex (Popelka et al., 1998), years of formal education (Popelka et al., 1998), self-perceived hearing handicap (Palmer, Solodar, Hurley, Byrne, & Williams, 2009), expectations and attitudes toward hearing aids (Meister, Walger, Brehmer, von Wedel, & von Wedel, 2008; van den Brink, Wit, Kempen, & van Heuvelen, 1996), self-efficacy (Hickson, Meyer, Lovelock, Lampert, & Khan, 2014), personality (Cox, Alexander, & Gray, 2005), motivation (Ridgway, Hickson, & Lind, 2015), readiness for change (Ekberg, Grenness, & Hickson, 2016), use of information communication technologies (Gonsalves & Pichora-Fuller, 2008), stigma (Wallhagen, 2010), and manual dexterity (Humes, Wilson, & Humes, 2003).
In contrast, there has been less emphasis on understanding how factors external to the individual influence hearing aid adoption.1 One exception is the identification of the role of social relationships on hearing aid adoption. Correlational evidence suggests that significant others are positively associated with hearing aid adoption by providing social support (Hickson et al., 2014), attending audiology appointments (Singh & Launer, 2016), and communicating positive attitudes about hearing rehabilitation (Duijvestijn et al., 2003; Poost-Foroosh, Jennings, Shaw, Meston, & Cheesman, 2011). Recommendations to try or use hearing instruments when provided by audiologists; ear, nose, and throat surgeons; or family physicians are also positively correlated with hearing aid adoption (Kochkin, 2012). Finally, cost or affordability of hearing aids has been identified as a barrier to hearing aid adoption (Garstecki, 1996; Meister et al., 2008), the importance of which varies significantly depending on the research methodology employed. When self-report is used (i.e., when hearing aid nonadopters are asked to provide explanations for why they do not use hearing aids), 49% to 76% of survey respondents indicate cost as a relevant factor (Kochkin, 2007). In contrast, research comparing behavior (i.e., hearing aid adoption rates in countries where cost is either fully government subsidized or not) suggests that full subsidization of hearing aids in the United States would only increase hearing aid adoption rates by roughly 10% (Valente & Amlani, 2017).
Models of Behavior Change
Models of health behavior change attempt to conceptualize processes that govern decision-making and action in health-care contexts. Focused more at the level of the individual, three of the most common models of health behavior change include the transtheoretical model (Prochaska & DiClemente, 1983), the health belief model (Rosenstock, 1966), and the health action process approach (Schwarzer, Lippke, & Luszczynska, 2011). There are several examples of work applying models of behavior change at the level of the individual (e.g., Laplante-Lévesque, Hickson, & Worrall, 2013; Saunders, Frederick, Silverman, Nielsen, & Laplante-Lévesque, 2016). Generally, ecological models of health promotion tend to focus on individuals in broader social and environmental contexts so as to design systems that foster positive health decision-making (for a review, see Sallis & Owen, 1997). There have been several applications of ecological models to audiologic rehabilitation. Examples include community-based peer counselling provided by trained hearing-impaired individuals to help other seniors cope with hearing loss (Dahl, 1997), the provision of audiology rehabilitation in everyday living environments (i.e., residential care facilities) rather than in the clinic (Jennings & Head, 1994), and hearing conservation programs designed for work places (Reddy, Welch, Ameratunga, & Thorne, 2017; see also Carson & Pichora-Fuller, 1997).
Decision-Making
Often, decision-making is assumed to be a deliberate and conscious process. For decades, standard models of decision-making characterized individuals as rational deliberators who objectively weigh the pros and cons of decisions and behaviors. However, there is a great deal of consensus among psychologists that processes outside conscious awareness (priming, heuristics, and context) exert powerful influences on decision-making and subsequent behaviors (Nisbett & Wilson, 1977; Tversky & Kahneman, 1974; Wilson & Brekke, 1994; for a review, see Gilovich & Griffin, 2010). To our surprise, to date there has been minimal research investigating how such processes influence outcomes in audiology. This study consists of a retrospective exploratory investigation of a large dataset to determine whether hearing aid adoption is associated with one of these factors, namely, time of day.
Linkages Between Time of Day, Hunger, and Risk-Aversion
There is evidence from both laboratory-based experiments and analyses of real-world datasets, which suggests that decision-making may be influenced by time of day and hunger. For example, Danziger, Levav, and Avnaim-Pesso (2011) investigated decision-making in high-risk situations, namely, judicial board rulings for prisoner requests (i.e., requests for parole, removal of a tracking device, prison relocation, etc.). Remarkably, it was observed that decisions in favor of a prisoner’s request varied systematically in a sawtooth pattern over the course of a single day. At the start of each period after a meal was consumed (breakfast, lunch, and dinner), decisions in favor of the prisoner were granted roughly 65% of the time, then dropped to almost 0% prior to the consumption of the next meal, but increased back to approximately 65% after meal consumption. In complementary work, it has been demonstrated experimentally that, compared with sated individuals, individuals who are hungry are less willing to take risks on the Iowa Gambling Task (de Ridder, Kroese, Adriaanse, & Evers, 2014). When considered together, there appears to be evidence suggesting that under conditions of uncertainty with potentially risky outcomes, decision-making varies systematically with time of day. Specifically, it appears that decision makers exhibit lower risk tolerance (less willingness to take risks) under conditions of hunger and higher risk tolerance (i.e., more willingness to take risks) when sated.
There are two dominant, and nonmutually exclusive, theoretical accounts for risk-aversion resulting from hunger. Ego depletion theory (Baumeister & Vohs, 2007) posits that decision-making draws upon a limited pool of cognitive resources that can deplete over time. Factors that can diminish the pool of available resources include antecedent factors (e.g., prior demands on resources such as that which occurs with sequential decision-making) and concurrent factors (e.g., body states). In contrast, hot-cold empathy gap theory (Loewenstein, 1996) suggests that decision-making can be state dependent whereby decision-making that takes place in psychologically hot states (e.g., hunger, sexual arousal, experiencing a craving associated with an addiction, etc.) may differ, sometimes drastically, from decisions made in psychologically cold states (i.e., calmness).
The Current Research
The primary objective of the current research is to determine whether there is an association between the time of day at which an audiology appointment is scheduled and hearing aid adoption. Two factors suggest a possible association between time of day and hearing aid adoption. First, there is evidence to suggest lower risk tolerance when decision makers are hungry (Danziger et al., 2011; de Ridder et al., 2014). Second, there is further evidence to suggest that, for many individuals, hearing aid adoption is considered a risk proposition (Kochkin, 2007). Risks include, but are not limited to, uncertainty regarding benefit, concerns about the cost of devices, and potential stigmatization (David & Werner, 2016; Southall, Gagné, & Jennings, 2010). Accordingly, it is hypothesized that lower hearing aid adoption will be observed at times of the day when meal consumption takes place (noon) or is about take place (4 p.m.) compared with all other times of the day. The influence of the day of the week on hearing aid adoption is also investigated, and it is hypothesized that no association will be observed between the day of the week and hearing aid adoption. Failure to observe a significant relationship between day of week and hearing aid adoption and observation of a significant relationship between time of day and hearing aid adoption would provide evidence of divergent validity between the two predictors.
The second objective of the study is to investigate whether hearing aid return rates are influenced by the time of day at which appointments are scheduled. It is hypothesized that lower return rates will be observed for groups of participants with appointments at times where meal consumption typically takes place (noon) or is about to take place (4 p.m.). Because risk-aversion resulting from hunger is assumed to dissuade individuals with noon and 4 p.m. appointments who are on the bubble (i.e., experience more uncertainty) regarding the decision to obtain hearing instruments, it is anticipated that those who persist and obtain hearing instruments at these times of day represent a subgroup that exhibits qualities (e.g., more motivation, more self-perceived hearing handicap, greater self-efficacy, etc.) that facilitates hearing aid adoption (i.e., hunger is not sufficient to deter this subgroup from becoming hearing aid adopters). For that reason, it is expected that lower return rates will be observed in the group of hearing aid adopters whose appointments are scheduled at noon and 4 p.m. than hearing aid adopters whose appointments are scheduled at any other time of the day.
Methods
Participants and Procedures
The study consists of a retrospective examination of 24,842 adult patient records obtained from a private chain of audiology clinics in Canada. The participants were first-time patients of the clinics. At the first appointment, participants completed a hearing assessment, and for all the participants in the sample, a recommendation for at least one hearing aid was provided. Information was collected whether the patient decided to try a hearing aid(s) (yes or no) or the patient decided to keep their hearing aid(s) (yes or no) beyond the trial period which was typically 30 days. Typically, a decision regarding whether or not to pursue amplification as a component of their audiologic rehabilitation is made at the conclusion of the appointment. None of the participants had previously worn hearing aids. The time of day of the appointment (9 a.m., 10 a.m., 11 a.m., noon, 1 p.m., 2 p.m., 3 p.m., and 4 p.m.) was recorded for each of the patients. Because there are multiple time zones in Canada, time zone conversions were completed so that all times are reported in a time that enables comparisons. Information was collected regarding the age and sex of each patient. Demographic information regarding the final sample is provided in Table 1. The study involved only deidentified data that were collected in the course of routine care, so no institutional review board approval was necessary.
Table 1.
Sample Demographics and Characteristics.
| %* | Mean age (years) | SD age (years) | |
|---|---|---|---|
| Total sample size (n = 24,842) | – | 75.4 | 13.5 |
| Female | 53.2 | 77.2 | 13.7 |
| Male | 39.0 | 73.3 | 12.9 |
| Unknown sex | 7.8 | 74.2 | 13.9 |
| Mild HL | 33.1 | 71.5 | 12.7 |
| Moderate HL | 37.4 | 76.9 | 13.0 |
| >Moderate HL | 29.5 | 78.1 | 14.0 |
| Adopters | 53.5 | 76.3 | 13.3 |
| Mild HL | 29.4 | 72.4 | 12.7 |
| Moderate HL | 38.5 | 77.4 | 12.8 |
| >Moderate HL | 32.1 | 78.6 | 13.8 |
| Monaural fittings | 29.2 | 76.5 | 14.5 |
| Binaural fittings | 70.8 | 76.3 | 12.8 |
| Nonadopters | 46.5 | 74.4 | 13.7 |
| Mild HL | 37.4 | 70.7 | 12.8 |
| Moderate HL | 36.1 | 76.2 | 13.3 |
| >Moderate HL | 26.5 | 77.4 | 14.3 |
| Returned HA(s) | 21.3 | 75.1 | 13.5 |
| Mild HL | 34.5 | 71.8 | 12.7 |
| Moderate HL | 37.4 | 76.5 | 13.2 |
| >Moderate HL | 28.1 | 77.2 | 13.9 |
| Did not return HA(s) | 78.7 | 75.5 | 13.5 |
| Mild HL | 32.8 | 71.4 | 12.7 |
| Moderate HL | 37.4 | 77.0 | 13.0 |
| >Moderate HL | 29.9 | 78.3 | 14.0 |
HL = hearing loss; HA = hearing aid.
non-italicized values represent percentages of the total sample; italicized values represent percentages of the sub-sample.
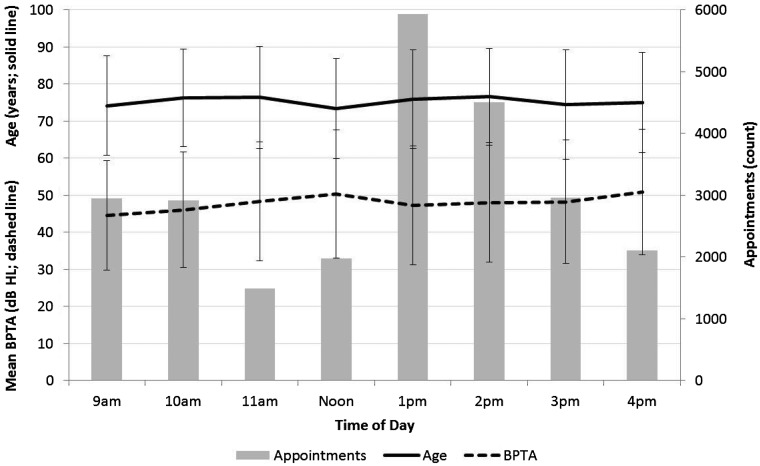
Pure-tone air-conduction audiometric threshold testing was conducted on all individuals; however, individual frequency audiometric threshold information was not available in the data set. Instead, for each ear, information regarding a three frequency (500, 1000, and 2000 Hz) pure-tone average (PTA) was available. The mean and standard deviation for age and binaural PTA (BPTA) of the participants are depicted by time of day in Figure 1 (referenced to left y-axis). Figure 1 also depicts the total number of appointments for each of the time bins (referenced to the right y-axis). A mean of 3,105.3 (SD =1,458.6; min = 1,489; max = 5,931) appointments was observed across the 8 times of day. Mean age across the 8 times of day was 75.4 years (SD = 13.5; minmean = 73.4; maxmean = 76.6).
Figure 1.
Mean age (solid line; referenced to left y-axis) and binaural three frequency (500, 1000, and 2000 Hz) PTA (dashed line; referenced to left y-axis) and total number of appointments (gray bars; referenced to right y-axis) depicted by time of day. Error bars represent standard deviations. BPTA = binaural pure-tone average.
Outcome Measures
The decision to purchase and possibly return the hearing aids was quantified as follows. Hearing aid adoption is defined as the proportion of the sample who made the decision to include hearing instruments (1 or 2 hearing aids) as a component of their rehabilitation. Return rate is defined as the proportion of the sample who ultimately returned the hearing aids before the conclusion of the trial period.
Statistical Analyses
To better understand which factors were associated with hearing aid adoption and the decision to return hearing aids before the conclusion of a trial period across the time of day, hierarchical binary logistic regressions were conducted in order to statistically control for the possibly confounding influence of age and degree of hearing loss on hearing aid adoption (Wong & Mason, 1985). The effect of time of day on hearing aid adoption (yes or no) was assessed by entering participant age and BPTA into Block 1 of the analysis. Entered into Block 2 of the analysis was time of day (9 a.m., 10 a.m., 11 a.m., noon, 1 p.m., 2 p.m., 3 p.m., and 4 p.m.) and two interaction terms (Time of Day × BPTA and Time of Day × Age). To explore the possible influence of day of week on hearing aid adoption (yes or no), a binary logistic regression was conducted whereby the day of the week (Monday, Tuesday, Wednesday, Thursday, and Friday) was entered as a predictor variable.
A hierarchical binary logistic regression was conducted in order to assess the effect of time of day on return rate (returned or did not return). This was assessed by entering participant age and BPTA into Block 1 and time of day (9 a.m., 10 a.m., 11 a.m., noon, 1 p.m., 2 p.m., 3 p.m., and 4 p.m.) into Block 2. Also entered into Block 2 was the Time of Day × BPTA and Time of Day × Age Interaction Terms.
For all regression analyses, variables needed to have a value of p < .05 to remain in the model. There was no evidence of multicollinearity as all predictor variables exhibited weak correlations (all rs < 0.2) with each other. Post hoc testing consisted of chi-square analyses assessing hearing aid adoption (or return rates; yes or no) for the 8 appointment times of the day (9 a.m., 10 a.m., 11 a.m., noon, 1 p.m., 2 p.m., 3 p.m., and 4 p.m.) and were conducted using methods outlined by Beasley and Schumacker (1995). The null hypothesis was that equivalent hearing aid adoption (or return rates) would be observed for each of the 8 times of the day investigated in the study. For all significant effects, we report odds ratio (OR), a measure of the association between the relevant variable (e.g., time of day) and the relevant outcome measure (e.g., hearing aid adoption). All analyses were conducted using IBM® SPSS® statistics software (version 24).
Results
Hearing Aid Adoption
In contrast to the null hypothesis that there would be no time of day effects on hearing aid adoption and return rates, we observed that hearing aid adoption and return rates fluctuate in a theoretically predictable fashion throughout the day. It was observed that there are times of the day when hearing aid adoption and return rates deviate positively and are higher than one would expect, there are times of the day when hearing aid adoption and return rates deviate negatively and are lower than one would expect, and that there are times of the day when hearing aid adoption and return rates are not significantly different in either direction.
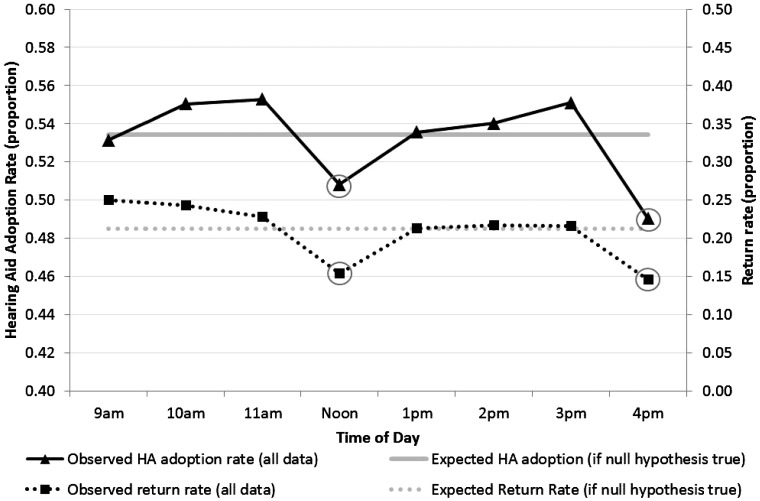
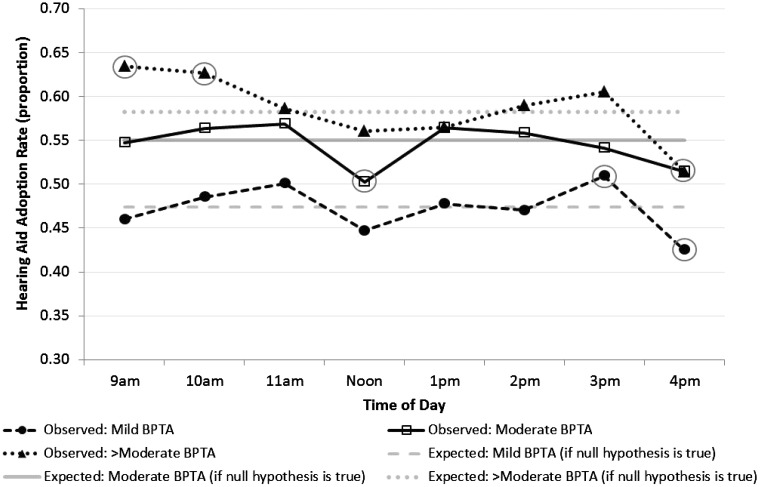
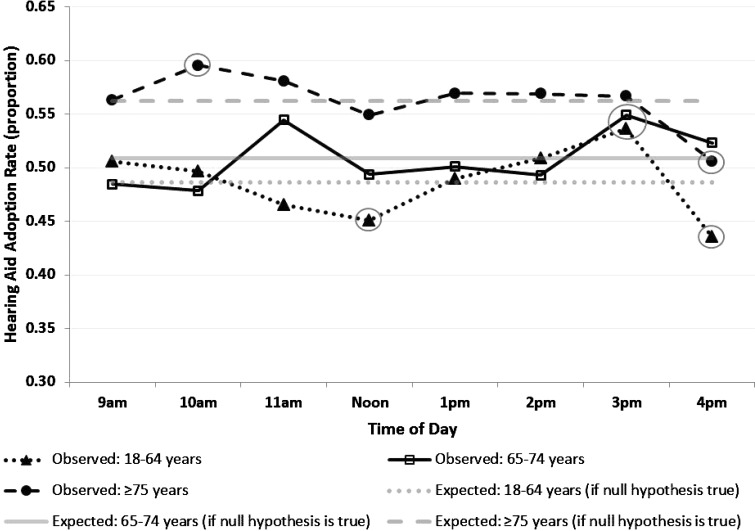
The first objective of the study was to assess hearing aid adoption rates across the time of day. A significant association was observed (−2 log likelihood = 33,059.73, χ2 = 286.99, Nagelkerke R2 = .02, p < .001). As predicted, post hoc testing revealed that poorer hearing aid adoption was observed at noon and at 4 p.m. (see Figure 2, solid black line) than at 9 to 11 a.m. and 1 to 3 p.m.; hence, the null hypothesis that equivalent hearing aid adoption would be observed across all times of the day was rejected (solid gray line; OR = 1.12; 95% CI [1.04, 1.20], p < .01). Significant main effects of age (OR = 1.01; 95% CI [1.01, 1.02], p < .001) and BPTA (OR = 1.02; 95% CI [1.01, 1.02], p < .001) were also observed whereby greater hearing aid adoption was observed for older compared with younger adults and for individuals with poorer compared with better hearing thresholds. We further examined whether the degree of hearing loss influenced the relationship between hearing aid adoption rates and appointment times. A significant BPTA by time of day interaction was observed (OR = 1.00; 95% CI [0.99, 1.00], p < .01). Post hoc testing revealed that (a) higher than expected hearing aid adoption rates were observed at 9 and 10 a.m. for the group with greater than moderate hearing losses and at 3 p.m. for the group with mild hearing losses, and (b) lower than expected hearing aid adoption rates were observed at noon for the group with moderate hearing losses and 4 p.m. for the groups with mild and greater than moderate hearing losses (see Figure 3). We also examined whether age influenced the relationship between hearing aid adoption rates and appointment times. A significant age by time of day interaction was observed (OR = 1.00; 95% CI [0.99, 1.00], p < .05). Post hoc testing revealed that (a) higher than expected hearing aid adoption was observed at 10 a.m. for the group ≥ 75 years of age and at 3 p.m. for the groups 18 to 64 and 65 to 74 years of age, and that lower than expected hearing aid adoption was observed at noon for the group 18 to 64 years of age and at 4 p.m. for the groups 65 to 74 and ≥75 years of age (see Figure 4).
Figure 2.
Mean observed (solid black line) and expected (solid gray line) hearing aid adoption rates (referenced to the left y-axis) and mean observed (dotted black line) and expected (dotted gray line) return rates (referenced to the right y-axis) depicted by the time of day. Circles highlight data points where there are significant differences between observed and corresponding expected performance. HA = hearing aid.
Figure 3.
Mean observed (black lines) and expected (gray lines) hearing aid adoption rates for the groups with mild (dashed lines), moderate (solid lines), and greater than moderate (dotted lines) hearing loss depicted by the time of day. Circles highlight data points where there are significant differences between observed and corresponding expected performance. BPTA = binaural pure-tone average.
Figure 4.
Mean observed (black lines) and expected (gray lines) hearing aid adoption rates for the group of participants ages 18 to 64 years (dotted lines), 65 to 74 years (solid lines), and ≥ 75 years (dashed lines) depicted by the time of day. Circles highlight data points where there are significant differences between observed and corresponding expected performance.
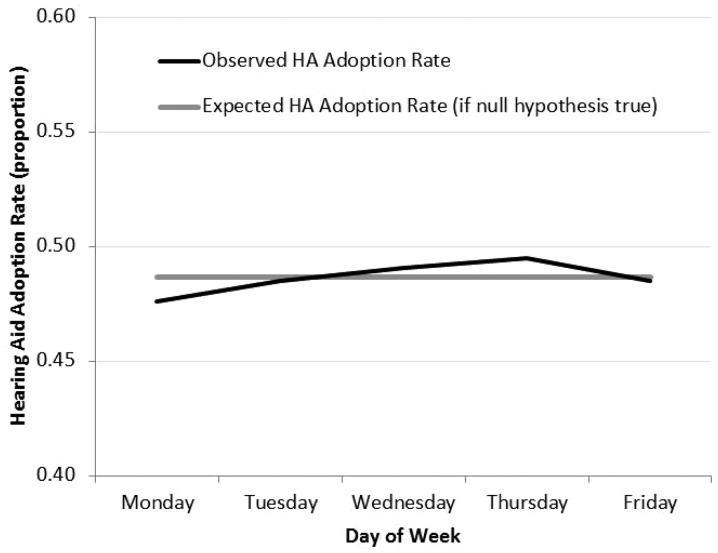
In contrast to the differences in hearing aid adoption rates hypothesized across the time of day, we did not expect to observe an association between hearing aid adoption and the day of the week. As expected, similar hearing aid adoption rates were observed from Monday to Friday (p > .05; see Figure 5).
Figure 5.
Mean observed (black line) and expected (gray line) hearing aid adoption rates depicted by the day of week.
Return Rates
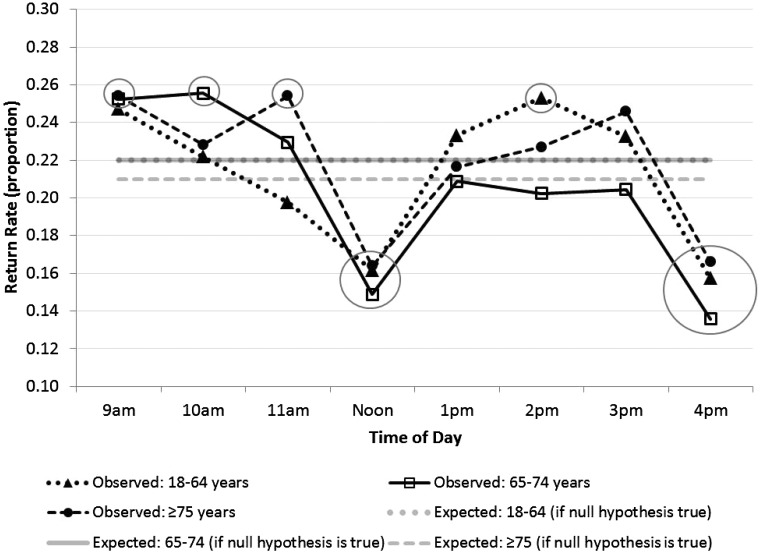
The second objective of the study was to assess whether hearing aid return rates vary systematically across the time of day. The null hypothesis is that equivalent return rates will be observed across all times of the day. A significant association was observed (−2 log likelihood = 25,011.05, χ2 = 71.47, Nagelkerke R2 = .01, p < .001). As predicted, a significant main effect of time of day was observed (OR = 1.11; 95% CI [1.02, 1.21], p < .05). Post hoc testing revealed equivalent return rates between observed (dotted black line) and expected (dotted gray line) performance at all times except noon and 4 p.m. where return rates were lower than expected (see Figure 2). A significant main effect of Age (OR = 1.01; 95% CI [1.00, 1.01], p < .05) was also observed whereby return rates were higher for younger compared with older adults. Finally, a significant Time of Day by Age interaction was observed (OR = 0.99; 95% CI [0.99, 1.00], p < .001). Post hoc testing revealed that (a) higher than expected hearing aid return rates were observed at 9 a.m., 10 a.m., 11 a.m., and 2 p.m. for the group(s) ≥ 65, 65 to 74, ≥ 75, and 18 to 64 years of age, respectively and (b) lower than expected hearing aid return rates were observed at noon and 4 p.m. for all age-groups (see Figure 6).
Figure 6.
Mean observed (black lines) and expected (gray lines) hearing aid return rates for the group of participants ages 18 to 64 years (dotted lines), 65 to 74 years (solid lines), and ≥75 years (dashed lines) depicted by the time of day. Circles highlight data points where there are significant differences between observed and corresponding expected performance.
Discussion
The current explorative retrospective study provides evidence that when patients make decisions regarding hearing rehabilitation, there is a significant tendency to not pursue hearing aids at noon and 4 p.m. (see Figures 2 and 3). The study also provides evidence of an association between time of day and the decision to return hearing instruments before the conclusion of a trial period whereby return rates were associated with the time of day at which the patient made the decision to pursue hearing aids. Specifically, lower return rates were observed at noon and at 4 p.m. compared to all other times of the day (see Figures 2, 4, and 6). As predicted, an association between hearing aid adoption and the day of the week was not observed in the study (see Figure 5).
Due to the nonexperimental nature of the methodology employed in the study, it is not possible to establish the causal mechanism that accounts for the reduced hearing aid adoption rates and return rates observed at noon and 4 p.m. than at other times of the day. Seemingly, the lower rates observed at these times arise from factors related to the patient, the clinician, and/or some other factor such as environment or context. Despite these methodological limitations and the shortage of measures directly assessing internal states, we feel it is helpful to propose potential explanations of the data so as to provide frameworks for future research. Hence, we next consider three hypotheses (the risk-aversion hypothesis, the clinician behavior hypothesis, and the preexisting differences hypothesis) regarding the patterns of data observed in the study.
Risk-Aversion Hypothesis
The risk-aversion hypothesis posits that when decision-making occurs at times of the day when food consumption takes or is about to take place, resource scarcity (i.e., hunger) promotes risk-aversion. This hypothesis is based on previous research suggesting that hunger and resource scarcity inhibits risk tolerance for complex behaviors with delayed gratification2 (Danziger et al., 2011; de Ridder et al., 2014). Indeed, for some, the decision to pursue hearing instruments represents a risk proposition (i.e., hesitation stemming from factors such as uncertainty regarding benefit, cost of hearing instruments, concerns regarding stigmatization, etc.).
An account based on altered risk-aversion resulting from hunger is consistent with the patterns of hearing aid adoption found in the study, namely, that lower hearing aid adoption was observed when appointments are scheduled at times of the day when food consumption typically, or is about to, take place (see Figures 2 and 3). This pattern of data is also consistent with the sawtooth pattern rates of parole decisions observed in Danziger et al. (2011) and the observation that hunger is associated with decreased risk tolerance (de Ridder et al., 2014). Moreover, recent work investigating the availability of glucose on risk tolerance supports the risk-aversion hypothesis. Compared to placebo, Pfundmair, Lermer, and Frey (2017) found that a dose of glucose (i.e., consumption of a sugar-containing beverage) was found to increase risk-taking on both cognitive and behavioral tasks.
Additional evidence in support of the risk-aversion hypothesis stems from the return rate data. If this hypothesis accounts for the patterns of findings observed in the study, it is likely the case that risk-aversion resulting from hunger would alter the behavior of individuals who experience more uncertainty about hearing aids (i.e., individuals who are on-the-bubble regarding their decision) than individuals who are more certain that they want to pursue hearing aids. Further still, this would imply that, on average, the individuals who actually go ahead and obtain hearing instruments at noon and 4 p.m. (despite experiencing risk-aversion resulting from hunger) likely differ along dimensions that facilitate hearing aid adoption (e.g., motivation, self-perceived hearing handicap, personality, etc.). Put another way, if risk-aversion resulting from hunger deterred a proportion of the on-the-bubble individuals from some groups (i.e., noon and 4 p.m.) but not from others (i.e., 9–11 a.m. and 1–3 p.m.), one should expect to observe differences in return rates between these two sets of hearing aid adopters. Specifically, lower return rates should be observed for hearing aid adopters with appointments at noon and 4 p.m. (groups containing relatively fewer on-the-bubble individuals) than hearing aid adopters with appointments at any other time of the day (groups containing relatively more on-the-bubble individuals); this is precisely the pattern of results that was observed in the study (see Figures 2 and 6). Hence, the pattern of return rates observed in the study is consistent with an account based on risk-aversion resulting from hunger.
Clinician Behavior Hypothesis
The clinician behavior hypothesis states that, rather than influencing patients directly, time of the day indirectly influences hearing aid adoption rates by altering the behaviors of clinicians. For example, it could be that at certain times of the day, clinicians exhibit behaviors (or fail to exhibit behaviors) that negatively (or positively) influence hearing aid adoption. Perhaps lower hearing aid adoption takes place at noon or 4 p.m. because fatigue sets in or clinicians find themselves in a hurry to depart for lunch or the day. The authors are unaware of any research in audiology that investigates how time of day and work scheduling influences the behavior of hearing care professionals. More broadly, research examining the effect of rest breaks on workplace performance observes that accident risk is predicted by taking breaks (Greiner, Krause, Ragland, & Fisher, 1998), particularly if food is consumed during the break (Lisper & Eriksson, 1980; for a review, see Tucker, 2003).
A second way that clinician behaviors may influence hearing aid adoption is that clinicians may spend more time with patients first thing in the morning and first thing after lunch, than with patients whose appointments are scheduled just before lunch or end of work day. Because the study did not measure actual appointment duration, but scheduled appointment duration, clinicians may have spent more time with some patients and not others. Similarly, this behavior pattern by clinicians may have influenced patient behavior because wait times for patients may be longer for appointments scheduled just before lunch or end of work day than for patients with appointments scheduled first thing in the morning and first thing after lunch. In research conducted with physicians, there is evidence that longer waiting times are negatively associated with patient satisfaction (Miceli & Wolosin, 2004).
As with the risk-aversion hypothesis, if time of day influences clinicians so that they spend less time with some patients and not others and engage in fewer behaviors that encourage hearing aid adoption, it may be the case that such behaviors would have greatest impact for patients who are on-the-bubble regarding their decision to pursue hearing instruments. Therefore, similar to the risk-aversion hypothesis, one should expect to observe lower return rates at the same times of day when appointment times negatively influence hearing aid adoption rates. This is also the pattern observed in the study. Hence, the return rate data are consistent with an account based on the clinician behavior hypothesis.
Preexisting Differences Hypothesis
The preexisting differences hypothesis states that there are differences between those who select appointment times at noon and 4 p.m. compared to other times of the day, and that such differences account for the lower hearing aid adoption rates observed at certain times of the day. For example, it could be that younger individuals, a group which exhibits lower rates of hearing aid adoption, tend to schedule appointments at noon and 4 p.m. because they have less flexibility in their schedule, and appointments at noon and 4 p.m. are more suitable for a standard work day. The data reported in Figure 2, however, suggest that the group of participants at noon and 4 p.m. were similar to the group of participants at all other times of the day both in terms of age and hearing thresholds, thus providing less support for the preexisting differences hypothesis.
If it is the case that the group who scheduled appointments at noon and 4 p.m. differ in some fashion that systematically predisposes them to adopt hearing instruments at a lower rate than at other times of the day (the preexisting differences hypothesis), it is less obvious why such a group would also be predisposed to keep their hearing aids after trying them at a higher rate than groups more inclined to obtain hearing aids (such as those who scheduled appointments between 9–11 a.m. and 1–3 p.m.). Hence, the return rate data would also suggest less support for the preexisting differences hypothesis.
Because the study sample was not randomly assigned to appointment times, it is not possible to rule out the preexisting differences hypothesis. For example, research on diurnal variation (i.e., circadian rhythms) in humans observes that individuals report preferences in peak alertness (Horne & Östberg, 1976) and exhibit differences in cognitive performance that vary with time of day (May, Hasher, & Stolzfus, 1993). In general, older adults tend to function better earlier in the day (i.e., morning types), whereas younger adults function better later in the day (i.e., evening types; Kripke et al., 2005). While there has been some exploration of time of day effects on auditory performance (Ezzatian, Pichora-Fuller, & Schneider, 2010; Veneman, Gordon-Salant, Matthews, & Dubno, 2013), the authors know of no research investigating how such diurnal variation influences decisions regarding hearing aid adoption. In order to reject the preexisting differences hypothesis account of the data, it would be necessary to employ an experimental methodology whereby matched groups of patients are randomly assigned to appointment times and to observe how time of day influences hearing aid adoption rates.
Notably, the size of the effects observed in the current study is small but meaningful. Compared to appointments that were scheduled at noon and 4 p.m., hearing aid adoption rates were 9% higher when appointments were scheduled at any other time of the day. Such effects are relatively small in light of other research investigating hearing aid adoption (e.g., Singh & Launer, 2016); however, it is remarkable that a seemingly extraneous factor such as appointment time can potentially exert as much influence as was observed in the current study. In contrast, the association between time of day and the effect on return rates was comparatively larger. Although the mean return rate was 23% for hearing aid purchasers whose appointments were scheduled between 9 and 11 a.m. and 1 and 3 p.m., it was on average 15% for the group whose appointments were scheduled at either noon or 4 p.m.
Time of day was associated with a differential effect on hearing aid adoption for groups with mild, moderate, and greater than moderate binaural hearing loss. All three groups exhibited lower than expected hearing aid adoption at noon, at 4 p.m., or at both times, a pattern of findings consistent with both the risk-aversion and clinician behavior hypotheses. Notably, greater than expected hearing aid adoption was observed at 9 a.m. and 10 a.m. for the group with greater than moderate hearing loss, and at 3 p.m. for the group with mild hearing loss. Of the theoretical accounts described in the article, seemingly no account can fully explain the time of day by BPTA interaction. However, the pattern of data is somewhat consistent with what one might speculate based on age-related diurnal variation. One possibility is that morning types (who tend to be older adults) may be more likely to adopt hearing aids at appointments scheduled earlier in the day, and evening types (who tend to be younger adults) may be more likely to adopt hearing aids at appointment scheduled later in the day. Indeed, the mean age of the group with greater than moderate hearing loss was 84.5 years (SD = 5.9) and the mean age of the group with mild hearing loss was 54.1 years (SD = 9.6 years). Because higher than expected hearing aid adoption was observed for the group with greater than moderate hearing loss earlier in the day (a relatively older adult group) and higher than expected hearing aid adoption was observed later in the day (i.e., 3 p.m.) for the group with mild hearing loss (a relatively younger adult group), this raises the possibility that age-related diurnal variation may be a relevant factor regarding hearing aid adoption.
Study Limitations, Strengths, and Future research
There are (at least) three notable shortcomings associated with the study. First, the study employed a retrospective design. While retrospective designs are not a weakness in and of themselves, within this context, we consider it a weakness because it did not allow for the random assignment of patients and clinicians to appointments at specific times of the day. A second notable weakness of the study is that there were few measures assessing characteristics of the sample (i.e., demographic, auditory, behavioral, and psychological variables). This is problematic as it is not possible to unequivocally determine possible mechanisms underlying the association between time of day and hearing aid adoption and the association between time of day and hearing aid return rates. A third shortcoming is that measures assessing appointment length were not available. Accordingly, wait times may have differed between individuals with appointments scheduled at the beginning of the day or after lunch than those with appointments scheduled to begin just before lunch or the end of the day.
There are (at least) three notable strengths of the study. First, in a large-scale sample of 24,842 first-time patients of hearing health-care clinics, a new variable (i.e., the time at which an appointment is scheduled) has been identified as a significant correlate of both hearing aid adoption and return rates. Second, the article describes several mechanisms (risk-aversion, clinician behavior, and preexisting differences) that may be relevant in order to better understand hearing aid adoption. Third, and more broadly, the study draws attention to the need to better understand the influence of contextual (possibly nonconscious) influences on clinical behaviors and outcomes.
As possible future research, we suggest more systematic experimentation investigating the influence of time of day on hearing aid adoption, with an eye to sorting out the various explanations offered of the observed pattern of relationships found in the current study. Furthermore, the current study puts forward the idea that risk-aversion may influence hearing aid adoption. Accordingly, it may be of value if future research explores patient decision-making and behaviors in experiments that consider the possible influence of risk perceptions.
The reporting of associations between time of day and hearing aid adoption or return rates sheds light on factors that may influence hearing health-care rehabilitation. One clinical implication regarding the findings observed in the study is that decision-making in audiology and other health-care contexts may be influenced by seemingly extraneous variables such as the time of an appointment. This application of the study findings may be influenced by a myriad of motivations including the desire to address untreated hearing loss, improve quality of life, and the goal to improve business outcomes. In the interest of transparent communication, such as that provided when care is provided from a Family-Centered Care perspective (Singh et al., 2016; Singh, Lau, & Pichora-Fuller, 2015), the authors advocate open dialogue whereby patients are informed of the factors that may or may not influence decision-making.
Conclusion
Research in audiology typically examines auditory, psychosocial, demographic, or clinical influences on help-seeking and hearing aid adoption. In contrast, less is known about contextual (possibly nonconscious) influences on behavior in hearing rehabilitation. This retrospective study provides quantitative evidence in a large sample that the time of day at which an appointment is scheduled is significantly associated with both hearing aid adoption and the decision to return hearing aids before the conclusion of a trial period. There are several potential explanations for the pattern of data observed in the study which should be investigated further in future research.
Notes
In fact, the authors are unaware of any experiments which systematically investigate the role of such external factors in the decision to pursue audiologic treatment options.
Interestingly, hunger is also associated with increased risk taking in several species (e.g., fish) when the risk involves foraging behaviors (Killen, Marras, & McKenzie, 2011).
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Abrams H. B., Kihm J. (2015) An introduction to MarkeTrak IX: A new baseline for the hearing aid market. Hearing Review 22: 16 Retrieved from http://www.hearingreview.com/2015/05/introduction-marketrak-ix-new-baseline-hearing-aid-market/. [Google Scholar]
- Bainbridge K. E., Ramachandran V. (2014) Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005-2006 and 2009-2010. Ear and Hearing 35: 289–294. doi:10.1097/01.aud.0000441036.40169.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister R. F., Vohs K. (2007) Self-regulation, ego depletion, and motivation. Social and Personality Psychology Compass 1: 115–128. doi:10.1111/j.1751-9004.2007.00001.x. [Google Scholar]
- Beasley T. M., Schumacker R. E. (1995) Multiple regression approach to analyzing contingency tables; Post hoc and planned comparison procedures. Journal of Experimental Education 64: 79–93. doi:10.1080/00220973.1995.9943797. [Google Scholar]
- Carson A. J., Pichora-Fuller M. K. (1997) Health promotion and audiology: The community-clinic link. Journal of the Academy of Rehabilitative Audiology 30: 29–51. [Google Scholar]
- Chisolm T. H., Johnson C. E., Danhauer J. L., Portz L. J. P., Abrams H. B., Lesner S., et al. (2007) A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology Task Force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology 18: 151–183. https://doi.org/10.3766/jaaa.18.2.7. [DOI] [PubMed] [Google Scholar]
- Ciorba A., Bianchini C., Pelucchi S., Pastore A. (2012) The impact of hearing loss on the quality of life of elderly adults. Clinical Interventions in Aging 7: 159–63. doi:10.2147/CIA.S26059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox R., Alexander G., Gray G. (2005) Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear and Hearing 26: 12–26. doi:10.1097/00003446-200502000-00002. [DOI] [PubMed] [Google Scholar]
- Dahl M. (1997) To Hear Again: A volunteer program in hearing health care for hard-of-hearing seniors. Journal of Speech-Language Pathology and Audiology 21: 153–159. [Google Scholar]
- Dalton D. S., Cruickshanks K. J., Klein B. E., Klein R., Wiley T. L., Nondahl D. M. (2003) The impact of hearing loss on quality of life in older adults. Gerontologist 43: 661–668. doi:10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- Danziger S., Levav J., Avnaim-Pesso L. (2011) Extraneous factors in judicial decisions. Proceedings of the National Academy of Sciences 108: 6889–6892. doi:10.1073/pnas.1018033108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David D., Werner P. (2016) Stigma regarding hearing loss and hearing aids: A scoping review. Stigma and Health 1(2): 59–71. doi:10.1037/sah0000022. [Google Scholar]
- de Ridder D., Kroese F., Adriaanse M., Evers C. (2014) Always Gamble on an Empty Stomach: Hunger Is Associated with Advantageous Decision Making. PLoS ONE 9(10): e111081 doi:10.1371/journal.pone.0111081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duijvestijn J., Anteunis L., Hoek C., Van Den Brink R. H., Chenault M. N., Manni J. J. (2003) Help-seeking behavior of hearing-impaired persons aged > or = 55 years: Effect of complaints, significant others and hearing aid image. Acta Oto-laryngologica 123: 846–850. doi:10.1080/0001648031000719. [DOI] [PubMed] [Google Scholar]
- Ekberg K., Grenness C., Hickson L. (2016) Application of the transtheoretical model of behaviour change for identifying older clients’ readiness for hearing rehabilitation during history-taking in audiology appointments. International Journal of Audiology 55: s42–s51. doi:10.3109/14992027.2015.1136080. [DOI] [PubMed] [Google Scholar]
- Ezzatian P., Pichora-Fuller M. K., Schneider B. A. (2010) Do circadian rhythms affect adult age-related differences in auditory performance? Canadian Journal of Aging 29(2): 215–221. doi:10.1017/S0714980810000139. [DOI] [PubMed] [Google Scholar]
- Garstecki D. C. (1996) Older adults: Hearing handicap and hearing-aid management. American Journal of Audiology 5: 25–33. doi: 10.1044/1059-0889.0503.25. [Google Scholar]
- Garstecki D. C., Erler S. F. (1998) Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, and Hearing Research 41(3): 527–537. doi:10.1044/jslhr.4103.527. [DOI] [PubMed] [Google Scholar]
- Gilovich, T. D., & Griffin, D. W. (2010) Judgment and decision making. In S.T. Fiske, D.T. Gilbert, & G. Lindzey (Eds.), Handbook of social psychology, 5th ed. (vol I, pp. 542–88). New York: Wiley. https://doi.org/10.1002/9780470561119.socpsy001015.
- Gonsalves C., Pichora-Fuller M. K. (2008) The effect of hearing loss and hearing aids on the use of information and communication technologies by community-living older adults. Can J Aging 27: 145–157. doi:10.3138/cja.27.2.145. [DOI] [PubMed] [Google Scholar]
- Greiner B., Krause N., Ragland D. R., Fisher J. M. (1998) Objective stress factors, accidents, and absentee-ism in transit operators: A theoretical framework and empirical evidence. Journal of Occupational Health Psychology 3: 130–146. doi:10.1037/1076-8998.3.2.130. [DOI] [PubMed] [Google Scholar]
- Gussekloo J., de Bont L. E. A., von Faber M., Eekhof J. A. H., de Laat J. A. P.M., Hulshof J. H., et al. (2003) Auditory rehabilitation of older people from the general population-The Leiden 85-plus Study. British Journal of General Practice 53: 536–540. Retrieved from http://bjgp.org. [PMC free article] [PubMed] [Google Scholar]
- Hartley D., Rochtchina E., Newall P., Golding M., Mitchell P. (2010) Use of hearing aids and assistive listening devices in an older Australian population. Journal of the American Academy of Audiology 21: 642–653. doi: 10.3766/jaaa.21.10.4. [DOI] [PubMed] [Google Scholar]
- Helvik A.-S., Wennberg S., Jacobsen G., Hallberg L. (2008) Why do some individuals with objectively verified hearing loss reject hearing aids? Audiological Medicine 6: 141–148. https://doi.org/10.1080/16513860802178692. [Google Scholar]
- Hickson L., Meyer C., Lovelock K., Lampert M., Khan A. (2014) Factors associated with success with hearing aids in older adults. International Journal of Audiology 53: 18–27. doi: 10.3109/14992027.2013.860488. [DOI] [PubMed] [Google Scholar]
- Horne J. A., Östberg O. (1976) A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology 4: 97–110. [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Humes A. C. (2003) Examinations of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss and gender. International Journal of Audiology 42: 432–441. https://doi.org/10.3109/14992020309080053. [DOI] [PubMed] [Google Scholar]
- Jennings M. B., Head B. G. (1994) Development of an ecological audiologic rehabilitation program in a home-for-the-aged. Journal of the Academy of Rehabilitative Audiology 27: 73–88. [Google Scholar]
- Jenstad L., Moon J. (2011) Systematic review of barriers and facilitators to hearing-aid uptake in older adults. Audiology Research 1: e25, 91–96. . doi: 10.4081/audiores.2011.e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen S. S., Marras S., McKenzie D. J. (2011) Fuel, fasting, fear: routine metabolic rate and food deprivation exert synergistic effects on risk-taking in individual juvenile European sea bass. Journal of Animal Ecology 80: 1024–1033. doi:10.1111/j.1365-2656.2011.01844.x. [DOI] [PubMed] [Google Scholar]
- Kochkin, S. (2007, April). MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. Hearing Journal, 60(4), 27-43. Retrieved from http://www.betterhearing.org/hearingpedia/marketrak-publications/marketrak-vii-obstacles-adult-non-user-adoption-hearing-aids.
- Kochkin, S. (2012, March). MarkeTrak VIII: The key influencing factors in hearing aid purchase intent. Hearing Review, 19(3), 12-25. Retrieved from http://www.betterhearing.org/hearingpedia/marketrak-publications/marketrak-viii-key-influencing-factors-hearing-aid-purchase.
- Kripke D. F., Youngstedt S. D., Elliott J. A., Tuunainen A., Rex K. M., Hauger R. L., et al. (2005) Circadian phase in adults of contrasting ages. Chronobiology International 22: 695–709. doi: 10.1080/07420520500180439. [DOI] [PubMed] [Google Scholar]
- Laplante-Lévesque A., Hickson L., Worrall L. (2013) Stages of change in adults with acquired hearing impairment seeking help for the first time: application of the transtheoretical model in audiologic rehabilitation. Ear and Hearing 34: 447–457. doi: 10.1097/AUD.0b013e3182772c49. [DOI] [PubMed] [Google Scholar]
- Lin F. R., Thorpe R., Gordon-Salant S., Ferrucci L. (2011) Hearing loss prevalence and risk factors among older adults in the United States. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 66: 582–590. doi: 10.1093/gerona/glr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisper H.-O., Eriksson B. (1980) Effects of the length of a rest break and food intake on subsidiary reaction-time performance in an 8-hour driving task. Journal of Applied Psychology 65: 117–122. http://dx.doi.org/10.1037/0021-9010.65.1.117. [PubMed] [Google Scholar]
- Loewenstein G. (1996) Out of control: Visceral influences on behavior. Organizational Behavior and Human Decision Processes 65: 272–292. doi:10.1006/obhd.1996.0028. [Google Scholar]
- May C. P., Hasher L., Stolzfus E. R. (1993) Optimal time of day and the magnitude of age differences in memory. Psycholological Sciences 4: 326–330. https://doi.org/10.1111/j.1467-9280.1993.tb00573.x. [Google Scholar]
- Meister H., Walger M., Brehmer D., von Wedel U. C., von Wedel H. (2008) The relationship between pre-fitting expectations and willingness to use hearing aids. International Journal of Audiology 47: 153–159. doi: 10.1080/14992020701843111. [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L. (2012) What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? International Journal of Audiology 51(2): 66–74. doi: 10.3109/14992027.2011.611178. [DOI] [PubMed] [Google Scholar]
- Miceli P. J., Wolosin R. J. (2004) You’re “running late”—now what?: Patient satisfaction, wait time and physician behavior, Orlando, FL: The World Organization of National Colleges, Academies, and Academic Associations of General Practitioners/Family Physicians. [Google Scholar]
- Ng J. H.-Y., Loke A. Y. (2015) Determinants of hearing-aid adoption and use among the elderly: A systematic review. International Journal of Audiology 54: 21–30. https://doi.org/10.3109/14992027.2014.966922. [DOI] [PubMed] [Google Scholar]
- Nisbett R. E., Wilson T. D. (1977) Telling more than we can know: Verbal reports on mental processes. Psychological Review 84: 231–259. http://dx.doi.org/10.1037/0033-295X.84.3.231. [Google Scholar]
- Palmer C. V., Solodar H. S., Hurley W. R., Byrne D. C., Williams K. O. (2009) Self-perception of hearing ability as a strong predictor of hearing aid purchase. J Am Acad Audiol 20: 341–347. https://doi.org/10.3766/jaaa.20.6.2. [DOI] [PubMed] [Google Scholar]
- Pfundmair M., Lermer E., Frey D. (2017) Glucose increases risky behavior and attitudes in people low in self-control. Social Psychology 48: 47–53. http://dx.doi.org/10.1027/1864-9335/a000290. [Google Scholar]
- Poost-Foroosh L., Jennings M. B., Shaw L., Meston C. N., Cheesman M. F. (2011) Factors in client-clinician interaction that influence hearing aid adoption. Trends in Amplification 15(3): 127–139. https://doi.org/10.1177/1084713811430217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popelka M. M., Cruickshanks K. J., Wiley T. L., Tweed T. S., Klein B. E. K., Klein R. (1998) Low prevalence of hearing aid use among older adults with hearing loss: The epidemiology of hearing loss study. Journal of the American Geriatrics Society 46: 1075–1078. https://doi.org/10.1111/j.1532-5415.1998.tb06643.x. [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., DiClemente C. C. (1983) Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology 51: 390–395. [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., Velicer W. F. (1997) The transtheoretical model of health behavior change. American Journal of Health Promotion 12: 38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Reddy R., Welch D., Ameratunga S., Thorne P. (2017) An ecological approach to hearing health promotion in workplaces. International Journal of Audiology 12: 1–12. doi: 10.1080/14992027.2016.1271467. [DOI] [PubMed] [Google Scholar]
- Ridgway J., Hickson L., Lind C. (2015) Autonomous motivation is associated with hearing aid adoption. International Journal of Audiology 54: 476–484. doi: 10.3109/14992027.2015.1007213. [DOI] [PubMed] [Google Scholar]
- Rosenstock I. M. (1966) Why people use health services. Milbank Mem Fund Q 44(Suppl): S94–S127 https://doi.org/10.2307/3348967. [PubMed] [Google Scholar]
- Sallis J. F., Owen N. (1997) Ecological Models. In: Glanz K., Lewis F. M., Rimer B. K. (eds) Health Behavior and Health Education: Theory, Research, and Practice, 2nd ed San Francisco, Calif: Jossey-Bass, pp. 403–424. [Google Scholar]
- Saunders G. H., Frederick M. T., Silverman S. C., Nielsen C., Laplante-Lévesques A. (2016) Description of adults seeking hearing help for the first time according to two health behavior change approaches: Transtheoretical mode (stages of change) and health belief model. Ear and Hearing 37: 324–333. doi: 10.1097/AUD.0000000000000268. [DOI] [PubMed] [Google Scholar]
- Schwarzer R., Lippke S., Luszczynska A. (2011) Mechanisms of health behavior change in persons with chronic illness or disability: The health action process approach (HAPA). Rehabilitation Psychology 56: 161–170. doi: 10.1037/a0024509. [DOI] [PubMed] [Google Scholar]
- Singh G., Hickson L., English K., Scherpiet S., Lemke U., Timmer B., et al. (2016) Family-centered adult audiologic care: A Phonak position statement. Hearing Review 23: 16–20. Retrieved from http://www.hearingreview.com/2016/03/family-centered-adult-audiologic-care-phonak-position-statement/. [Google Scholar]
- Singh G., Lau S.-T., Pichora-Fuller M. K. (2015) Social support and hearing aid satisfaction. Ear and Hearing 36: 664–676. doi: 10.1097/AUD.0000000000000182. [DOI] [PubMed] [Google Scholar]
- Singh G., Launer S. (2016) Social context and hearing aid adoption. Trends in Hearing 20: 1–10. https://doi.org/10.1177/2331216516673833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southall K., Gagné J., Jennings M. (2010) Stigma: A negative and a positive influence on help-seeking for adults withacquired hearing loss. International Journal of Audiology 49: 804–814. doi: 10.3109/14992027.2010.498447. [DOI] [PubMed] [Google Scholar]
- Tucker P. (2003) The impact of rest breaks upon accident risk, fatigue and performance: A review. Work & Stress 17: 123–137. https://doi.org/10.1080/0267837031000155949. [Google Scholar]
- Tversky A., Kahneman D. (1974) Judgment under uncertainty: Heuristics and biases. Science 185(4157): 1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- Valente M., Amlani A. M. (2017) Cost as a barrier for hearing aid adoption. JAMA Otolaryngology - Head & Neck Surgery 143: 647–648. doi:10.1001/jamaoto.2017.0245. [DOI] [PubMed] [Google Scholar]
- van den Brink R., Wit H., Kempen G., van Heuvelen (1996) Attitude and help-seeking for hearing impairment. Br J Audiol 30: 313–324. https://doi.org/10.3109/03005369609076779. [DOI] [PubMed] [Google Scholar]
- Veneman C. E., Gordon-Salant S., Matthews L. J., Dubno J. R. (2013) Age and measurement time-of-day effects on speech recognition in noise. Ear and Hearing 34: 288–299. doi: 10.1097/AUD.0b013e31826d0b81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vestergaard Knudsen L., Öberg M., Nielsen C., Naylor G., Kramer S. E. (2010) Factors influencing help-seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification 14: 127–154. doi: 10.1177/1084713810385712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallhagen M. I. (2010) The stigma of hearing loss. Gerontologist 50: 66–75. https://doi.org/10.1093/geront/gnp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong G. Y., Mason W. M. (1985) The hierarchical logistic regression model for multilevel analysis. Journal of the American Statistical Association 80: 513–524. doi: 10.1080/01621459.1985.10478148. [Google Scholar]
- Wilson T. D., Brekke N. (1994) Mental contamination and mental correction: Unwanted influences on judgments and evaluations. Psychological Bulletin 116: 117–142. http://dx.doi.org/10.1037/0033-2909.116.1.117. [DOI] [PubMed] [Google Scholar]