Abstract
Introduction
Studies of authorship provide a barometer of local research capacity and ownership of research, considered key to defining appropriate research priorities, developing contextualised responses to health problems and ensuring that research informs policy and practice. This paper reports on an analysis of patterns of research authorship of the now substantial literature on community health workers (CHWs) in low-and-middle-income countries (LMICs) for the 5-year period: 2012–2016.
Methods
A search of five databases identified a total of 649 indexed publications reporting on CHWs in LMICs and meeting the inclusion criteria. The country, region and income classification of studies, affiliations (country, organisation) of lead (first) and last authors, proportions of all authors locally affiliated, programme area (eg, maternal child health) and funding source were extracted.
Results
The 649 papers reported experiences from 51 countries, 55% from middle-income countries (MICs) and 32% from low-income countries (LICs), with the remaining 13% multicountry studies. Overall, 47% and 54% of all the papers had a high-income country (HIC) lead and last author, respectively. Authorship followed three patterns: (1) a concentrated HIC pattern, with US-based authors numerically dominating LIC-based and multicountry studies; (2) an MIC pattern of autonomy, with a handful of countries—India, South Africa and Brazil, in particular—leading >70% of their CHW publications and (3) a pattern of unevenness among LICs in their lead authorship of publications varying from 14% (Malawi) to 54% (Uganda). Region, programme area and funding source were all associated with the distribution of authorship across country income categories.
Conclusion
The findings in this analysis mirror closely that of other authorship studies in global health. Collectively these provide a common message—that investments in global health programmes in the Millennium Development Goal era may have benefited health but not necessarily capacity for knowledge generation in LMICs.
Keywords: descriptive study, health systems, health services research
Key questions.
What is already known?
There is a growing body of work examining global inequalities in authorship of research outputs on health priorities in low-and-middle-income countries (LMICs).
All of these studies, examining maternal and child health, HIV/AIDS, malaria, tuberculosis and health policy and systems research more broadly, have produced a similar finding, namely that around half the publications are first authored (led) by an author whose primary affiliation is an LMIC institution. The remainder are led by high-income country-based authors.
What are the new findings?
This study adds to the literature by examining and characterising the patterns of authorship underlying these global inequalities and the factors influencing these patterns.
The paper highlights not only enduring inequalities, but also the concentration of knowledge generation on community health workers (CHWs) and CHW programmes.
What do the new findings imply?
The findings point to the need for closer examination of funding and research practices in the global north, more deliberate investment in building LMIC research institutions, beyond the training of individual researchers and leveraging existing strengths within LMICs to promote south–south knowledge exchange and research collaboration.
Background
Since the landmark Commission on Health Research in 1990, there has been much interest in who drives, leads and funds research in low-and-middle-income countries (LMICs). The Commission described the ‘10/90 gap’: 10% of global research funding is devoted to the 90% share of the global disease burden in the South.1 Despite numerous research capacity strengthening initiatives,1 especially following the adoption of the Millennium Development Goals (MDGs), global inequities in research production remain significant.2 As has been noted by many, locally led research is key to defining appropriate research priorities, developing contextualised and adapted responses to health problems, and ensuring that research informs policy and practice.3–6
A body of work examining patterns in research output and distribution of authorship has emerged in recent times as a barometer of research capacity and local ownership. In a review of publications on maternal health interventions in LMICs over 13 years (2000–2012), Chersich et al7 found that only 56.6% of papers were first-authored by researchers affiliated to an LMIC, a proportion which did not change significantly over the period. Similarly, Kelaher et al8 conducted an inventory of 1593 articles on randomised controlled trials for HIV/AIDS, malaria and tuberculosis (TB) in LMICs from 1990 to 2013, of which just under one half (49.8%) had an LMIC lead. As with the Chersich et al7 review, they documented significant year-on-year increases in the numbers of published studies, especially from the African continent, but the number and proportion of high-income country (HIC) lead authors grew much more rapidly. This phenomenon follows the rise of global health as a field in northern academic institutions and has been described by one commentator as the ‘20th century scramble for Africa’.9 In health policy and systems research (HPSR), the trends have been similar, although with a greater proportion of LMIC first authors as the numbers of publications have increased.10
The overall pattern from these studies reflects a considerable growth of health research in LMICs, but not a fundamental change in the global relations of research production.1 11 The playing fields remain deeply unequal, even if most global health researchers would consider baldly ‘parasitic’12 or ‘parachute’1 research practices, where HIC authors extract data and publish findings on LMICs without their involvement, as unacceptable.13 In addition, approaches to capacity building have been dominated by vertical research projects, focused on training individual researchers, rather than institution and network building.11 13 Funding is allocated to internationally designated ‘spotlight’ issues rather than local priorities,1 and research outputs remain poorly aligned to health needs.14
However, behind these broad global patterns are specific dynamics that provide a more nuanced understanding of global relations and signal where action to reshape the field of knowledge production is needed.11 This is most evident when research authorship is broken down by country income levels,7 10 by region and by countries within regions. Across regions, middle-income countries (MICs) are more likely to lead their research publications than low-income countries (LICs).2 7 10 12 In West Africa, research output on HPSR is almost all accounted for by three countries: Nigeria, Ghana and Burkina Faso, possibly reflecting particular institutional histories and nodes of research leadership.15
On the other side of the equation, HIC lead authors of LMIC studies are most commonly from the USA,2 7 also the largest funder of global health research.10 Funding sources influence authorship patterns: for instance, Chersich et al7 reported that the United States Agency for International Development and European Union-funded studies were more likely to be led by authors from HICs than studies funded by other bilateral donors or domestic sources. Finally, forms of research are another relevant consideration. Multicountry studies, systematic reviews and publications in high-impact journals remain largely the preserve of HIC lead authors.7
This paper reports on an analysis of patterns of research authorship of the now substantial literature on community health workers (CHWs) in LMICs. The paper specifically analyses the distribution of authorship of publications of CHW programmes in LMICs by country income group (high, middle, low) for the 5-year period 2012–2016 and examines how these patterns vary by region, programme orientation (eg, maternal child health (MCH), HIV), funding and organisational affiliation.
The analysis builds on, and extends, a scoping review of publication trends on CHWs for the period 2005–2014.16 The key findings of this review were a sevenfold increase in the number of publications on CHWs over the period, driven principally by responses to HIV and the renewed focus on child and maternal survival in the MDGs. Specific agendas such as that of integrated Community Case Management (iCCM), formulated in a highly networked international ‘epistemic’ community,17 were particularly influential during this period. The iCCM strategy spawned multicountry research and intervention initiatives across the African continent.18 These developments coincided with a growing number of studies documenting and evaluating established national CHW programmes from, among others, Brazil,19 Ethiopia,20 Malawi21 and India.22 The literature on CHWs has thus emerged from different quarters and provides a valuable window on the contemporary global dynamics of health systems research in LMICs.
Methods
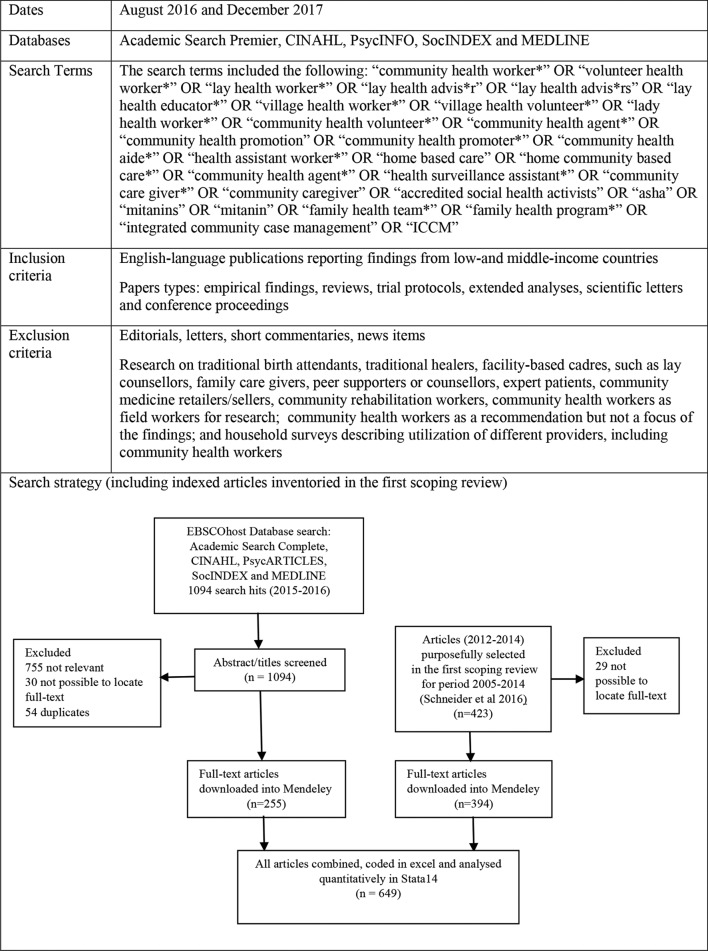
An analysis of 649 indexed journal articles on CHWs over the 5-year period 2012–2016 was conducted. The analysis included 394 articles inventoried in the first scoping review for the period 2005–201416 and 255 articles from an updated search of all 2015/2016 publications, using the exact same databases and search terms as the first review. The updated search was conducted by NM in August 2016 and again in December 2017. The review excluded articles where it was not possible to locate full-text versions required for the analysis. The two authors independently reviewed the 1094 titles and abstracts obtained from the updated search, removing duplicates and publications that did not meet the inclusion criteria. Decisions on disagreements were made through a joint review process. Full-text versions of the 649 publications from 2012 to 2016 were downloaded into a Mendeley database.
The search terms and review flow chart are provided in figure 1.
Figure 1.
Search and review strategy.
The authors independently coded the 649 papers in an Excel spreadsheet extracting the following data:
Publication year and type of study (empirical, analysis or review).
Programmatic focus: MCH, HIV/TB, malaria, reproductive health, non-communicable diseases (NCDs), mental health, other and comprehensive (if two or more programmatic foci were mentioned in the publication).
Geography: region, country and country income classification (following the 2017 World Bank classification) of study: LIC, lower middle-income (LowerMIC), upper middle-income (UMIC), high-income (H) and LMICs if a study was conducted in multiple countries.
Authorship: country and organisational affiliation of lead/first and last/senior author (hereafter referred to as ‘lead’ and ‘last’), total number of authors in a publication and the proportion of local authors. Last author was considered as a proxy for principal investigator, as ‘the first author is the most valuable position in a paper, while specifically in the clinical and biomedical sciences the last author was seen as the indication of seniority or a supervisory role on the research project’.23 Organisational affiliation was categorised into university, research institute, bilateral and multilateral agencies, non-governmental organisations (NGOs) and health service. Multiple affiliations were recorded, although only the first is reported in the paper.
Funding source, if named. Following the approach of Kelaher et al,8 funding patterns were classified into domestic, bilateral, multilateral, private/philanthropic and none if not specified or declared.
The Excel spreadsheet was exported to Stata/IC V.14 for analysis. In analysing whether the lead and last author were affiliated to an organisation in the country of study (ie, a local lead, local last author), the 56 multicountry studies reporting research or reviews on more than five countries were excluded. Given the relatively small numbers in each category, LowerMIC and UMIC were combined in several of the analyses. χ2 (Fisher’s exact in cells with less than five observations) tests examining the association between LMIC authorship (lead and last) and various factors (country income, region, programme area, funding source and organisational base) were conducted. Comparisons of mean values (total number authors/proportion local) between income groups were computed using one-way analysis of variance with Bonferroni correction tests.
Results
Profile of publications
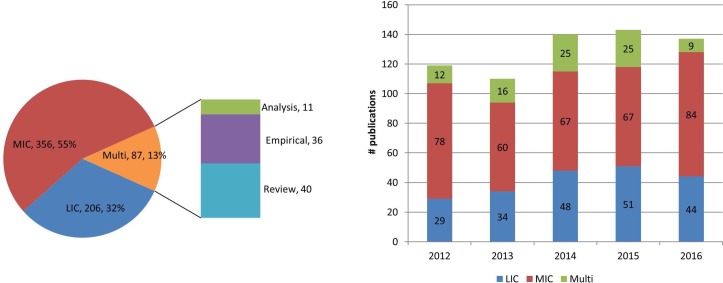
The 649 papers reported CHW programme experiences in 51 countries: 19 LICs, 23 LowerMIC and 9 UMICs, representing 61%, 43% and 16% of all countries in the three income categories, respectively. Publications on MIC CHW programmes made up more than half (55%), and those on LICs a third (32%) of the total. The remaining 87 (13%) were multicountry studies, nearly half (n=40) of which were review papers (figure 2). Fifteen countries (listed in online supplementary file 1) contributed 10 or more publications and accounted for 81% of the 562 single-country studies.
Figure 2.
Distribution of publications on community health workers by country income category and year (n=649). LIC, low-income country; MIC, middle-income country.
bmjgh-2018-000797supp001.pdf (93.4KB, pdf)
There was a trend towards an increased annual number of publications over the 5-year period (figure 2), with an annual average of 115 in 2012–2013 compared with 140 in 2014–2016. Multicountry studies were most prominent in 2014 and 2015 (figure 2).
Lead and last authorship
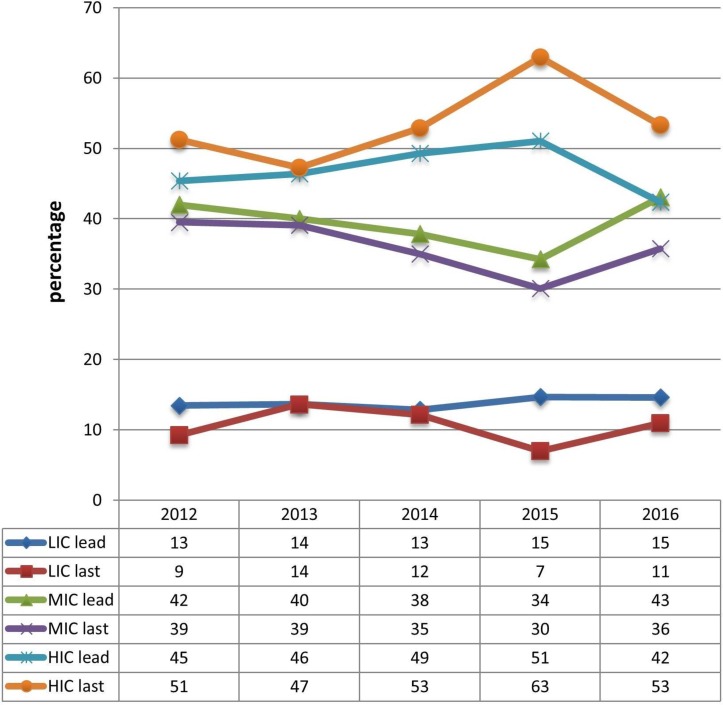
Overall, 47% and 54% of all the papers had an HIC lead and last author, respectively. Over the period, there was an initial trend towards increased HIC lead authorship, from 45% in 2012 to 51% in 2015, dropping back to earlier levels in 2016 (42%). Similarly, HIC last authorship rose from 51% to 63% in 2015, dropping to 53% in 2016 (figure 3). The relative decline in HIC lead and last authorship in 2016 matches a drop in the number of multicountry studies in that year (figure 2). Thirty-nine per cent of all studies had an MIC lead, while 14% had an LIC lead. The proportions of LIC lead and last authorship remained relatively static over the period (Figure 3).
Figure 3.
Percentage distribution of lead and last authorship of community health worker publications by income classification (n=649). HIC, high-income country; LIC, low-income country; MIC, middle-income country.
Publications were also examined by country, analysing the percentage of local lead and local last authors. Online supplementary file 1 lists the number of publications and authorship profiles of individual countries, categorised by income. In the publications emanating from LICs, 37% and 29% had a local lead and last author, respectively, rising progressively to 61% and 54% in LowerMICs, and 74% and 67% in UMICs.
There was considerable variation within country income categories. Lead authorship in three LICs (Malawi, Uganda and Ethiopia), which together contributed more than half the total publications in the low-income group, varied from 14% (Malawi) to 54% (Uganda). Among LowerMICs, percentage local lead authorship in countries with 10 or more publications varied from 48% (Zambia) to 78% (India). South Africa and Brazil, which together made up 81% of UMIC publications, had local lead authorship levels of 76% and 71%, respectively. In the subset of multicountry studies involving five or less countries (n=31), only 23% (n=7) had a lead author from one of the five countries, and similarly, 23% (n=20) of all the multicountry studies (n=87) had an LMIC lead.
Online supplementary file 2 reports the country distribution of the 304 and 350 HIC lead and last authors of CHW publications, respectively. Two-thirds (n=197, 65%) of lead authors had a primary affiliation to a US-based institution, followed by the UK (n=34, 11%) and Canada (n=20, 7%).
bmjgh-2018-000797supp002.pdf (36.1KB, pdf)
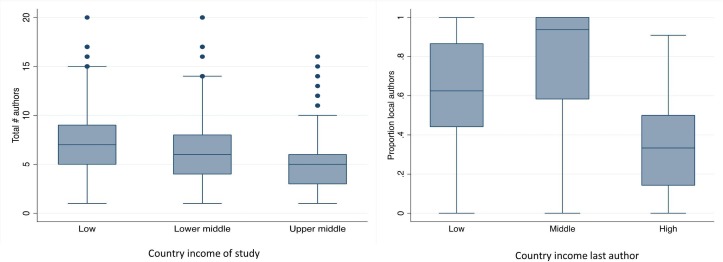
Number and local affiliations of all authors
In addition to lead and last author affiliations, we recorded the total number of authors per publication and the proportion who were based in the country of study (ie, local coauthors). The mean size of coauthorship teams in MIC publications was significantly lower than those of LIC publications (UMIC=5.4, LowerMIC=6.3, LIC=7.4, p=0.002), but not different from multicountry studies (mean=6.4) (figure 4). However, local coauthors made up a greater proportion of authorship teams in MIC publications than in LIC and multicountry publications (multicountry=0.41, LIC=0.43, LowerMIC=0.58, UMIC=0.70, p<0.001). In the subset of publications with three or more authors, 10% (52/544) did not include any local authors.
Figure 4.
Box plots (showing medians, 25%–75% quartile range and distribution) of total numbers of authors on publications by country income (n=649) and the proportion of local authors by country income of last author (n=593).
The proportion of local authors in authorship teams was strongly associated with the provenance of the last author (as an indicator of seniority or principal investigator status). Publications with HIC last authors had the lowest mean proportion of local authors (0.34) compared with 0.63 and 0.78 for publications with LIC and MIC last authors, respectively (p<0.001) (figure 4).
Factors associated with the distribution of lead and last authorship by income
The relationship between the distribution of lead and last authorship and the study setting (LIC, MIC, multicountry), region, programme area and funding was examined (table 1). HIC lead and last authors were particularly prominent in LIC and multicountry publications. The vast majority (+95%) of LMIC lead/last authors were also local leads/last authors with minimal cross-over of authorship between countries and income groupings.
Table 1.
Factors associated with lead and last authorship (n=649)
| LIC lead (%)† | MIC lead (%) | HIC lead (%) | P values* | LIC last (%) | MIC last (%) | HIC last (%) | P values* | Total | |
| Country classification | |||||||||
| LIC study | 77 (37%) | 5 (3%) | 124 (60%) | <0.001 | 59 (29%) | 5 (2%) | 142 (69%) | <0.001 | 206 |
| MIC study | 3 (1%) | 240 (67%) | 113 (32%) | 1 (1%) | 215 (60%) | 140 (39%) | 356 | ||
| Multicountry study | 10 (12%) | 10 (12%) | 67 (77%) | 8 (9%) | 11 (13%) | 68 (78%) | 87 | ||
| Total | 90 (14%) | 255 (39%) | 304 (47%) | 68 (10%) | 231 (36%) | 350 (54%) | 649 | ||
| Region | |||||||||
| Africa | 77 (21%) | 110 (29%) | 187 (50%) | <0.001 | 59 (16%) | 90 (24%) | 225 (60%) | <0.001 | 374 |
| Asia | 7 (4%) | 110 (62%) | 59 (34%) | 6 (3%) | 104 (59%) | 66 (38%) | 176 | ||
| Americas | 1 (2%) | 27 (54%) | 22 (44%) | 0 | 27 (54%) | 23 (46%) | 50 | ||
| Middle East | 0 | 3 (75%) | 1 (25%) | 0 | 3 (75%) | 1 (25%) | 4 | ||
| Cross-region | 5 (11%) | 5 (11%) | 35 (78%) | 3 (7%) | 7 (16%) | 35 (78%) | 45 | ||
| Programme area | |||||||||
| Maternal-child health | 44 (17%) | 90 (35%) | 123 (48%) | <0.001 | 34 (13%) | 70 (27%) | 153 (60%) | <0.001 | 257 |
| HIV/TB | 7 (10%) | 31 (42%) | 35 (48%) | 5 (7%) | 30 (41%) | 38 (52%) | 73 | ||
| Malaria | 16 (26%) | 21 (35%) | 24 (39%) | 7 (11%) | 17 (28%) | 37 (61%) | 61 | ||
| Reproductive health | 5 (16%) | 8 (26%) | 18 (58%) | 5 (16%) | 9 (29%) | 17 (55%) | 31 | ||
| NCD | 1 (3%) | 22 (69%) | 9 (28%) | 0 | 21 (66%) | 11 (34%) | 32 | ||
| Mental health | 2 (9%) | 9 (43%) | 10 (48%) | 2 (10%) | 10 (48%) | 9 (42%) | 21 | ||
| Other | 1 (2%) | 24 (53%) | 20 (45%) | 3 (7%) | 23 (51%) | 19 (42%) | 45 | ||
| Comprehensive | 13 (12%) | 39 (37%) | 54 (51%) | 12 (11%) | 38 (36%) | 56 (53%) | 106 | ||
| Not specified | 1 (4%) | 11 (48%) | 11 (48%) | 0 | 13 (57%) | 10 (43%) | 23 | ||
| Funders | |||||||||
| US bilateral | 12 (9%) | 28 (21%) | 93 (70%) | <0.001 | 14 (11%) | 31 (23%) | 88 (66%) | <0.001 | 133 |
| Other bilateral | 18 (20%) | 25 (27%) | 49 (53%) | 10 (11%) | 23 (25%) | 59 (64%) | 92 | ||
| Multilateral | 6 (25%) | 3 (12%) | 15 (63%) | 1 (4%) | 6 (25%) | 17 (71%) | 24 | ||
| BMGF | 17 (23%) | 23 (31%) | 35 (47%) | 9 (12%) | 16 (21%) | 50 (67%) | 75 | ||
| Wellcome Trust | 0 | 6 (75%) | 2 (25%) | 1 (13%) | 4 (50%) | 3 (37%) | 8 | ||
| Domestic | 8 (12%) | 52 (78%) | 7 (10%) | 8 (12%) | 50 (75%) | 9 (13%) | 67 | ||
| Multiple | 13 (13%) | 44 (42%) | 47 (45%) | 12 (12%) | 31 (30%) | 61 (58%) | 104 | ||
| None or not specified | 16 (11%) | 74 (51%) | 56 (38%) | 13 (9%) | 70 (48%) | 63 (43%) | 146 | ||
*χ2or Fisher’s exact where cells<5.
† All percentages are reported across rows.
BMGF, Bill and Melinda Gates Foundation; HIC, high-income country; LIC, low-income country; MIC, middle-income country; NCD, non-communicable diseases; TB, tuberculosis.
Authorship varied by region: 34% of publications from Asian countries had an HIC lead compared with 50% from African countries and 78% of cross-regional publications. Among the programme areas, MIC leads dominated in publications with an NCD focus (69%). The percentage of LIC leads was highest in malaria-related publications (26%), although only 11% had an LIC last author. In the largest programme category, MCH, 48% and 61% of publications had HIC lead and last authors, respectively.
Funding source played a significant role in the distribution of lead/last authorship. While only 10% of publications funded through domestic sources had an HIC lead, this rose to 70% of publications reporting US bilateral funding (directly or through intermediaries such as the Centers for Disease Control), also the most commonly listed source of funding (n=133, 20%). In contrast, 53% of publications supported by other bilateral funders (grouped together) had HIC leads. The Bill and Melinda Gates Foundation was listed as the main funder in 12% (n=75) of publications, of which 47% had an HIC lead author.
Across all country income groups, the main organisational affiliation of lead and last authors was a university or research institute: 63% and 70% of LIC, 77% and 77% of MIC, and 76% and 73% of HIC lead and last authors, respectively. Thirty-seven per cent of LIC leads were based in health services, NGOs or donor organisations, compared with 24% of HIC leads (table 2).
Table 2.
Organisational base of lead and last author by country classification (n=649)
| LIC lead | MIC lead | HIC lead | LIC last | MIC last | HIC last | |
| University | 45 (50%) | 135 (53%) | 212 (70%) | 37 (55%) | 132 (57%) | 223 (63%) |
| Research institute | 12 (13%) | 60 (24%) | 19 (6%) | 11 (16%) | 46 (20%) | 34 (10%) |
| Health service | 10 (11%) | 26 (10%) | 14 (5%) | 5 (7%) | 22 (10%) | 23 (7%) |
| Other* | 23 (26%) | 34 (13%) | 59 (19%) | 15 (22%) | 31 (13%) | 70 (20%) |
| Total | 90 (100%) | 254 (100%) | 305 (100%) | 68 (100%) | 231 (100%) | 350 (100%) |
*Local or international non-governmental organisation, bilateral, multilateral agency.
HIC, high-income country; LIC, low-income country; MIC, middle-income country.
Discussion
The findings in this analysis mirror closely those of other authorship studies in global health, with the proportions of LMIC lead and last authors very similar to that found in the fields of maternal health,7 HIV/TB,8child health12 and HPSR.10 Approximately half the indexed publications on CHW programmes are first authored by LMIC authors. As with other authorship studies, LMIC research leadership (whether first or last author) increases as countries move from LIC, to LowerMIC and UMIC status. The growth in research output on CHW programmes has been driven mostly by HIC-based scholars, with the USA being by far the most significant source of lead/last authors and funding for research in the field. Collectively these various authorship studies provide a common message—that investments in global health programmes in the MDG era may have led to a growth in health research and benefited health,24 25 but not necessarily institutional capacity for knowledge generation in LMICs. The finding that 1 in 10 multiauthor publications on CHW programmes had no local coauthors further suggests that ‘parachute’ research practices continue to exist, although in the absence of historical comparisons it is not possible to assess trends in this phenomenon.
Insofar as the analysis of authorship provides a window into the conduct of research on CHWs, it can be summarised into three overall patterns of scholarship:
A concentrated (USA) high-income country pattern, setting research agendas through funding and mobilisation of HIC-based scholars, and numerically dominating LIC-based and multicountry studies.
An MIC pattern of autonomy, with a handful of countries—India, South Africa, Brazil and Pakistan—driving significant levels of research on their CHW programmes. However, this research is almost all single country and locally focused, with smaller research teams (as judged by the size of their authorship teams), and relatively little multicountry or south–south collaboration evident.
A pattern of unevenness among LICs in their capacity to lead research on their own CHW programmes.
The inequalities in scholarship between HICs and MICs and LICs are likely to have been underplayed in this analysis, which did not examine scope or type of study (descriptive, experimental, etc), journal (local, international), impact factors and citations. The power of HIC-driven research extends to institutional connections with bodies such as WHO and Unicef, which, among others, enabled the formulation of the iCCM strategy.17 However, as pointed out by Sheikh et al5 ‘the most excellent research study or Global Health program risks failure unless it is informed and contextualised by the people close to where change is sought’. One-size-fits-all, technical approaches such as iCCM have been assimilated with difficulty in the everyday reality of country health systems, each with their own particular needs, histories, cultures and contexts.18 26 Implementation and scale-up require robust ‘embedded’ country research conducted through sufficiently capacitated national institutions working in close collaboration with policymakers and implementers.6 27
The analysis suggests that many MICs and some LICs have the potential to drive research agendas around their own CHW programmes. This could be due to greater institutional capacity or access to domestic research funding and different programmatic emphases, both of which were associated with authorship patterns. Research on community-based NCD care, which until recently was not a major theme of funding or research in global health, has been driven predominantly by MICs. In contrast, MCH was a major focus of attention in global health in the MDG era. The relatively even distribution of lead (although not last) authors in community-based malaria research is an interesting observation and could point to different operating norms in this field.
North–south research collaborations vary in their willingness to reflect on their partnership practices,28 and donors may differ in the extent to which they prioritise local ownership and leadership of research. For example, Crane et al,13 in a case study of an US-Ugandan research partnership, point to the common practice of establishing ‘shell’ non-profit organisations in LMICs in order to meet US federal government fiscal requirements, rather than channelling funds through local universities. The authors concluded that ‘U.S. fiscal administrative practices may drain rather than build capacity at African universities’.
An analysis of affiliations of lead and last (as opposed to all) authors may underestimate the extent of south–south research collaborations in CHW research. However, the relative absence of LMIC lead and last authors in multicountry studies suggests an implicit international hierarchy in the field. Namely, that cross-national generalisable knowledge is still the preserve of HIC researchers, who are able to speak about multiple settings, whereas LMIC researchers may be perceived as country specialists generating contextual knowledge that offers limited lessons for other jurisdictions.
Conclusions
Research authorship in the field of CHW programmes, as in other areas of global health, is heavily skewed towards HIC institutions, scholars and sources of funding. This has implications for research prioritisation, the capacity to generate relevant knowledge required to strengthen CHW programmes and local ownership. These patterns point to the need for closer examination of funding and research practices in the global north, including the nature of incentive structures in academic institutions; more deliberate investment in building research institutions in the global south,29 beyond the training of individual researchers,11 and leveraging existing strengths within LMICs to promote south–south knowledge exchange and research collaboration. Detailed case studies of donor practices and research partnerships, especially in LICs, may also shed light on harmful or beneficial approaches to developing more equitable playing fields in research on CHW programmes in LMICs.
Acknowledgments
The authors thank their colleagues Asha George, Uta Lehmann and Wolde Amde for their contributions to this analysis. An anonymous reviewer provided the important comment, included verbatim, on the implicit hierarchy in multicountry studies.
Footnotes
Handling editor: Stephanie M Topp
Contributors: HS and NM jointly conceptualised the study. Both authors independently coded and jointly conducted the analysis and drafted the manuscript. Both authors approved the final version of the manuscript.
Funding: This work is based on the research supported by the South African Research Chairs Initiative of the Department of Science and Technology and National Research Foundation of South Africa (grant no. 98918).
Disclaimer: Any opinion, finding and conclusion or recommendation expressed in this material is that of the author(s) and the NRF does not accept any liability in this regard.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Franzen SRP, Chandler C, Lang T. Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ Open 2017;7:e012332–16. 10.1136/bmjopen-2016-012332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasnida A, Borst RA, Johnson AM, et al. Making health systems research work: time to shift funding to locally-led research in the South. Lancet Glob Health 2017;5:e22–e24. 10.1016/S2214-109X(16)30331-X [DOI] [PubMed] [Google Scholar]
- 3.Costello A, Zumla A. Moving to research partnerships in developing countries. BMJ 2000;321:827–9. 10.1136/bmj.321.7264.827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Tracking Universal Health Coverage: 2017 Global Monitoring Report. Geneva: World Health Organization, 2017. [Google Scholar]
- 5.Sheikh K, Bennett SC, El Jardali F, et al. Privilege and inclusivity in shaping Global Health agendas. Health Policy Plan 2017;32:303–4. 10.1093/heapol/czw146 [DOI] [PubMed] [Google Scholar]
- 6.Ghaffar A, Langlois EV, Rasanathan K, et al. Strengthening health systems through embedded research. Bull World Health Organ 2017;95:87 10.2471/BLT.16.189126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chersich MF, Blaauw D, Dumbaugh M, et al. Local and foreign authorship of maternal health interventional research in low- and middle-income countries: systematic mapping of publications 2000-2012. Global Health 2016;12:1–15. 10.1186/s12992-016-0172-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelaher M, Ng L, Knight K, et al. Equity in global health research in the new millennium : trends in first-authorship for randomized controlled trials among low- and middle-income country researchers 1990-2013. Int J Epidemiol 2017;0:1–10. [DOI] [PubMed] [Google Scholar]
- 9.Crane J. Scrambling for Africa? Universities and global health. Lancet 2011;377:1388–90. 10.1016/S0140-6736(10)61920-4 [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. World Report On Health Policy and Systems Research (HPSR). Geneva: World Health Organization, 2017. [Google Scholar]
- 11.Ager A, Zarowsky C. Balancing the personal, local, institutional, and global: multiple case study and multidimensional scaling analysis of African experiences in addressing complexity and political economy in health research capacity strengthening. Health Res Policy Syst 2015;13:1–9. 10.1186/1478-4505-13-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rees CA, Lukolyo H, Keating EM, et al. Authorship in paediatric research conducted in low- and middle-income countries: parity or parasitism? Trop Med Int Health 2017;22:1362–70. 10.1111/tmi.12966 [DOI] [PubMed] [Google Scholar]
- 13.Crane JT, Andia Biraro I, Fouad TM, et al. The ’indirect costs' of underfunding foreign partners in global health research: A case study. Glob Public Health 2017;16:1–8. 10.1080/17441692.2017.1372504 [DOI] [PubMed] [Google Scholar]
- 14.Chersich M, Blaauw D, Dumbaugh M, et al. Mapping of research on maternal health interventions in low- and middle-income countries: a review of 2292 publications between 2000 and 2012. Global Health 2016;12:1–16. 10.1186/s12992-016-0189-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Defor S, Kwamie A, Agyepong IA. Understanding the state of health policy and systems research in West Africa and capacity strengthening needs: scoping of peer-reviewed publications trends and patterns 1990–2015. Health Res Policy Syst 2017;15(S1):102–38. 10.1186/s12961-017-0215-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneider H, Okello D, Lehmann U. The global pendulum swing towards community health workers in low- and middle-income countries: a scoping review of trends, geographical distribution and programmatic orientations, 2005 to 2014. Hum Resour Health 2016;14:1–12. 10.1186/s12960-016-0163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalglish SL, George A, Shearer JC, et al. Epistemic communities in global health and the development of child survival policy: a case study of iCCM. Health Policy Plan 2015;30 Suppl 2:ii12–ii25. 10.1093/heapol/czv043 [DOI] [PubMed] [Google Scholar]
- 18.Bennett S, George A, Rodriguez D, et al. Policy challenges facing integrated community case management in Sub-Saharan Africa. Trop Med Int Health 2014;19:872–82. 10.1111/tmi.12319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giugliani C, Harzheim E, Duncan MS, et al. Effectiveness of community health workers in Brazil: a systematic review. J Ambul Care Manage 2011;34:326–38. 10.1097/JAC.0b013e31822cbdfd [DOI] [PubMed] [Google Scholar]
- 20.Medhanyie A, Spigt M, Kifle Y, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res 2012;12:1–9. 10.1186/1472-6963-12-352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rodríguez DC, Banda H, Namakhoma I. Integrated community case management in Malawi: an analysis of innovation and institutional characteristics for policy adoption. Health Policy Plan 2015;30 Suppl 2:ii74–ii83. 10.1093/heapol/czv063 [DOI] [PubMed] [Google Scholar]
- 22.Sundararaman T, Ved R, Gupta G, et al. Determinants of functionality and effectiveness of community health workers: results from evaluation of ASHA program in eight Indian states. BMC Proc 2012;6(Suppl 5):O30–2. 10.1186/1753-6561-6-S5-O30 [DOI] [Google Scholar]
- 23.Street JM, Rogers WA, Israel M, et al. Credit where credit is due? Regulation, research integrity and the attribution of authorship in the health sciences. Soc Sci Med 2010;70:1458–65. 10.1016/j.socscimed.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 24.Murray CJ, Ortblad KF, Guinovart C, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:1005–70. 10.1016/S0140-6736(14)60844-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moucheraud C, Owen H, Singh NS, et al. Countdown to 2015 country case studies: what have we learned about processes and progress towards MDGs 4 and 5? BMC Public Health 2016;16 Suppl 2(Suppl 2):794 10.1186/s12889-016-3401-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olivier de Sardan JP, Diarra A, Moha M. Travelling models and the challenge of pragmatic contexts and practical norms: the case of maternal health. Health Res Policy Syst 2017;15(Suppl 1):71–138. 10.1186/s12961-017-0213-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization. Changing Mindsets: Strategy on Health Policy and Systems Research. Geneva: World Health Organization, 2012. [Google Scholar]
- 28.Citrin D, Mehanni S, Acharya B, et al. Power, potential, and pitfalls in global health academic partnerships: review and reflections on an approach in Nepal. Glob Health Action 2017;10:1367161–10. 10.1080/16549716.2017.1367161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sombié I, Aidam J, Montorzi G. Evaluation of regional project to strengthen national health research systems in four countries in West Africa: lessons learned. Health Res Policy Syst 2017;15(Suppl 1):90–138. 10.1186/s12961-017-0214-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2018-000797supp001.pdf (93.4KB, pdf)
bmjgh-2018-000797supp002.pdf (36.1KB, pdf)