Abstract
Myotonic Dystrophy type 1 (DM1) is the most common muscular dystrophy in adult life characterized by muscle dysfunction and cardiac conduction abnormalities. Atrial fibrillation frequently occurs in DM1 patients. It’s related to the discontinuous and inhomogeneous propagation of sinus impulses and to the prolongation of atrial conduction time, caused by progressive fibrosis and fatty replacement of the myocardium. AF predisposes to a hyper-coagulable state and to an increased risk of thromboembolism. We report the first case of complete resolution of left atrial appendage thrombosis with oral dabigatran etexilate in a myotonic dystrophy type I patient with atrial fibrillation scheduled for transesophageal echocardiogram-guided direct current cardioversion.
Key-words: myotonic dystrophy, atrial fibrillation, dabigatran etexilate, atrial thrombus
Introduction
Myotonic dystrophy type 1 (DM1) is the most common muscular dystrophy in adult life with an incidence of 1:8000 births and a worldwide prevalence ranging from 2.1 to 14.3/100.000 inhabitants. Cardiac involvement is noticed in about 80% of cases, and it often precedes the skeletal muscle one (1). Paroxysmal atrial arrhythmias (atrial fibrillation, atrial flutter, atrial tachycardia) frequently occur in DM1 patients with a prevalence up to 25% (2) and seem to increase mortality in this population (3). Modern pacemakers (PMs) and implantable cardiac defibrillators (ICDs) include detailed algorithms and functions to facilitate the diagnosis and management of frequent paroxysmal atrial tachy-arrhythmias often undetected during conventional clinical follow-up (4-11). Atrial fibrillation (AF) predisposes to a hypercoagulable state and an increased risk of thromboembolism (TE) (12, 13). The incidence of left atrial appendage thrombosis before direct current cardioversion (DCC) has been widely studied in AF population, ranging from 6 to 18% (14, 15). Non-Vitamin K Antagonist oral anticoagulants (NOAC) are increasingly used for the prevention and treatment of thrombi formation owing to the inherent limitations of Vitamin K antagonist oral anticoagulants (VKAs) (16). We report the first case of a left atrial appendage thrombosis effectively treated by dabigatran etexilate, a direct inhibitor of thrombin, in a DM1 patient with AF scheduled for transesophageal echocardiogram (TEE)-guided direct current cardioversion (DCC).
Case report
A 45-year-old DM1 woman with arterial hypertension, previously implanted with a dual chambers pacemaker for advanced atrioventricular block, came to our observation for PM check and cardiologic therapy optimization before cataract surgery. She was taking perindopril (4 mg/die) and magnesium pidolate (2.25 g/die). She referred a recent onset of palpitations and dyspnea. Standard (12-lead electrocardiogram) ECG confirmed the diagnosis of atrial fibrillation with a mean ventricular rate of 160 bpm (Fig. 1). PM interrogation showed atrial high rate electrograms (AHRE) faster than 220 bpm, that lasted longer than 5 minutes with irregularity and incoherence of RR intervals (Fig. 2) and arose five days before the cardiologic evaluation. Transthoracic echocardiogram showed a slightly reduced left ventricular systolic function (Simpson’s biplane ejection fraction: 48%) and a mild left atrial enlargement (left atrial volume index: 29 mL/m2). Considering the patients’ symptoms and the need to restore sinus rhythm before surgical procedure, a TEE-guided DCC was performed, which showed the presence of a thrombus in left atrial appendage (Fig. 3). The patient started a beta-blocker therapy for rate control (bisoprolol 2.5 mg/die) and oral anticoagulant therapy (warfarin 5 mg/die) to dissolve the thrombus and prevent the risk of systemic thrombo-embolic events. However, at one-month follow-up, due to a non-optimal response to warfarin therapy, evaluated by the International Normalized Ratio (INR) of the prothrombin time, a switch form VKA to NOAC therapy with dabigatran was performed at a dosage of 150 mg/bid. Eight weeks after, TEE revealed the complete resolution of the left atrial appendage thrombus (Fig. 4), allowing us to perform a safe and successful direct current cardioversion, that restored the sinus rhythm at 65 bpm. The therapy with dabigatran was prolonged for 4 weeks after cardioversion due to the high risk of thromboembolic events (CHA2DS2-Vasc Score: 2). At the date, twelve months after DCC procedure, no bleeding events or side-effects are reported.
Figure 1.
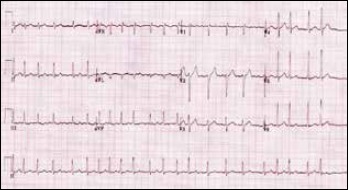
Atrial fibrillation detected by standard 12-lead electrocardiogram.
Figure 2.
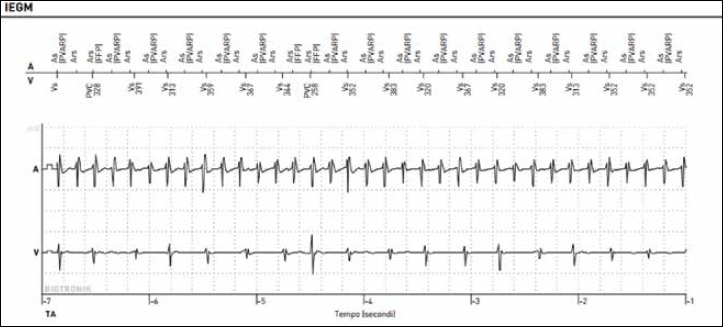
Atrial high rates electrograms detected by pacemaker diagnostics.
Figure 3.
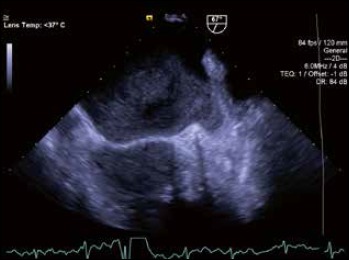
Transesophageal echocardiographic evaluation. See the presence of a thrombus in left atrial appendage.
Figure 4.

Transesophageal echocardiography evaluation eight weeks after treatment with dabigatran etexilate.
Discussion
Cardiac involvement in DM1 patients occurs as a degenerative process with progressive fibrosis and fatty replacement not only limited to the specialized conduction system, but also extended to initially unaffected areas of the atrial myocardium (17). This anatomo-pathological substrate, causing the discontinuous and inhomogeneous propagation of sinus impulses and the prolongation of atrial conduction time, may facilitate the onset and perpetuation of atrial arrhythmias in these patients (18-24), as usually happens in other clinical conditions (25-30). AF is one of the most common supraventricular arrhythmias observed in DM1 population, characterized by chaotic and uncoordinated atrial activity which predisposes to a hypercoagulable state and an increased risk of TE (12, 13). DCC quickly and effectively converts AF to sinus rhythm; however, it carries an inherent risk of stroke, which is substantially reduced by the administration of anticoagulation therapy. An early initiation of such therapy is important in all patients scheduled for cardioversion. Patients who have been in AF for periods longer than 48 h should start oral anticoagulation therapy at least 3 weeks before cardioversion and will continue it for at least 4 weeks afterwards (31). However, the difficulties in achieving an optimal anticoagulation with conventional warfarin therapy, likely related to several factors such as the slow onset of action, variable pharmacologic effects, numerous food and drug interactions and periodic closely target INR monitoring (32) make it difficult the therapeutic management in clinical practice and reduce the real-life patients’ compliance. All these challenges have prompted an extensive research and developed NOAC, now available for stroke prevention in AF patients and used in various clinical settings (33-38). Dabigatran etexilate, a direct inhibitor of thrombin, emerged as the first new generation oral anticoagulants potentially able to replace warfarin in preventing arterial TE in patients with AF (39-41). A post-hoc analysis of the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) study in patients who underwent cardioversion with or without TEE guidance, showed that dabigatran treatment has a low and comparable frequency of adverse events compared to warfarin (42). These results were confirmed by a long term propensity score matched study in real world setting (43). The potential thrombolytic effect of dabigatran has been previously described (43, 44) as it is able to create a easier and faster anticoagulation milieu while inhibiting thrombin binding to fibrin and fibrin degradation products. In contrast warfarin anticoagulation, in its loading phase, could also exert a transient thrombogenic action (45).
Conclusions
The present case is the first report of a complete left atrial appendage thrombosis resolution obtained by oral dabigatran etexilate in a DM1 patient with AF, scheduled for TEE guided direct electrical cardioversion. The use of NOAC therapy should be particularly useful in this population of patients, for their variable cognitive impairment and consequent poor compliance with periodic INR monitoring.
References
- 1.Nigro G, Comi LI, Politano L, et al. Cardiomyopathies associated with muscular dystrophies. Engel AG, Franzini-Armstrong C, Eds. Myology. 3rd ed New York: McGraw-Hill; 2004, pp. 1239-56. [Google Scholar]
- 2.Russo V, Rago A, Ciardiello C, et al. The role of the atrial electromechanical delay in predicting atrial fibrillation in myotonic dystrophy type 1 patients. J Cardiovasc Electrophysiol 2016;27:65-72. [DOI] [PubMed] [Google Scholar]
- 3.Petri H, Witting N, Ersbøll MK, et al. High prevalence of cardiac involvement in patients with myotonic dystrophy type 1: a crosssectional study. Int J Cardiol 2014;174:31-6. [DOI] [PubMed] [Google Scholar]
- 4.Lazarus A, Varin J, Babuty D, et al. Long-term follow-up of arrhythmias in patients with myotonic dystrophy treated by pacing: a multicenter diagnostic pacemaker study. JACC 2002;40:1645-52. [DOI] [PubMed] [Google Scholar]
- 5.Russo V, Rago A, Papa AA, et al. Does a high percentage of right ventricular pacing influence the incidence of paroxysmal atrial fibrillation in myotonic dystrophy type 1 patients? Kardiol Pol 2013;71:1147-53. [DOI] [PubMed] [Google Scholar]
- 6.Nigro G, Russo V, Politano L, et al. Does Bachmann’s bundle pacing prevent atrial fibrillation in myotonic dystrophy type 1 patients? A 12 months follow-up study. Europace 2010;12:1219-23. [DOI] [PubMed] [Google Scholar]
- 7.Russo V, Nigro G, Papa AA, et al. Far field R-wave sensing in myotonic dystrophy type 1: right atrial appendage versus Bachmann’s bundle region lead placement. Acta Myol 2014;33:94-9. [PMC free article] [PubMed] [Google Scholar]
- 8.Russo V, Rago A, Politano L, et al. The effect of atrial preference pacing on paroxysmal atrial fibrillation incidence in myotonic dystrophy type 1 patients: a prospective, randomized, single-bind cross over study. Europace 2012;14:486-9. [DOI] [PubMed] [Google Scholar]
- 9.Nigro G, Russo V, Rago A, et al. Right atrial preference pacing algorithm in the prevention of paroxysmal atrial fibrillation in myotonic dystrophy type 1 patients: a long term follow-up study. Acta Myologica 2012;31:139-43. [PMC free article] [PubMed] [Google Scholar]
- 10.Russo V, Nigro G, Rago A, et al. Atrial fibrillation burden in myotonic dystrophy type 1 patients implanted with dual chamber pacemaker: the efficacy of the overdrive atrial algorithm at 2 year follow-up. Acta Myologica 2013;32:142-7. [PMC free article] [PubMed] [Google Scholar]
- 11.Russo V, Nigro G, Meo F, et al. The effect of atrial preference pacing on atrial fibrillation electrophysiological substrate in myotonic dystrophy type 1 population. Acta Myologica 2014;33:127-35. [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart S, Hart CL, Hole DJ, et al. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart 2001;86:516-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet 2009;373:155-66. [DOI] [PubMed] [Google Scholar]
- 14.Roijer A, Eskilsson J, Olsson B. Transoesophageal echocardiography-guided cardioversion of atrial fibrillation or flutter. Selection of a low-risk group for immediate cardioversion. Eur Heart J 2000;21:837-47. [DOI] [PubMed] [Google Scholar]
- 15.Stoddard MF, Dawkins P, Prince CR, et al. Transesophageal echocardiographic guidance of cardioversion in patients with atrial fibrillation. Am Heart J 1995;129:1204-15. [DOI] [PubMed] [Google Scholar]
- 16.Russo V, Rago A, Proietti R, et al. Efficacy and safety of the target-specific oral anticoagulants for stroke prevention in atrial fibrillation: the real-life evidence. Ther Adv Drug Saf 2017;8:67-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russo V, Meo F, Rago A, et al. Paroxysmal atrial fibrillation in myotonic dystrophy type 1 patients: P wave duration and dispersion analysis. Eur Rev Med Pharmacol Sci 2015;19:1241-8. [PubMed] [Google Scholar]
- 18.Russo V, Rago A, Nigro G. Atrial electromechanical delay in myotonic dystrophy type 1 patients. Eur Rev Med Pharmacol Sci 2015;19:3991-2. [PubMed] [Google Scholar]
- 19.Russo V, Rago A, Nigro G. Sudden cardiac death in neuromuscolar disorders: time to establish shared protocols for cardiac pacing. Int J Cardiol 2016;207:284-5. [DOI] [PubMed] [Google Scholar]
- 20.Russo V, Nigro G, Papa AA, et al. Adenosine-induced sinus tachycardia in a patient with myotonic dystrophy type 1. Acta Myologica 2014;33:104-6. [PMC free article] [PubMed] [Google Scholar]
- 21.Russo V, Rago A, Meo F, et al. Ventricular fibrillation induced by coagulating mode bipolar electrocautery during pacemaker implantation in myotonic dystrophy type 1 patient. Acta Myologica 2014;33:149-51. [PMC free article] [PubMed] [Google Scholar]
- 22.Russo V, Rago A, D’Andrea A, et al. Early onset “electrical” heart failure in myotonic dystrophy type 1 patient: the role of ICD biventricular pacing. Anadolu Kardiyol Derg 2012;12:517-9. [DOI] [PubMed] [Google Scholar]
- 23.Nigro G, Russo V, Vergara P, et al. Optimal site for atrial lead implantation in myotonic dystrophy patients.The role of Bachmann’s Bundle stimulation. PACE 2008;31:1463-6. [DOI] [PubMed] [Google Scholar]
- 24.Nigro G, Russo V, Politano L, et al. Right atrial appendage versus Bachmann’s bundle stimulation: a two year comparative study of electrical parameters in myotonic dystrophy type 1 patients. PACE 2009;32:1192-7. [DOI] [PubMed] [Google Scholar]
- 25.Rago A, Russo V, Papa AA, et al. The role of the atrial electromechanical delay in predicting atrial fibrillation in beta thalassemia major patients. JICE 2016;48:147-57. [DOI] [PubMed] [Google Scholar]
- 26.Russo V, Di Meo F, Rago A, et al. Impact of continuous positive airway pressure therapy on atrial electromechanical delay in obesity-hypoventilation syndrome patients. J Cardiovasc Electrophysiol 2016;27:327-34. [DOI] [PubMed] [Google Scholar]
- 27.Russo V, Rago A, Di Meo F, et al. Atrial septal aneurysms and supraventricular arrhythmias: the role of atrial electromechanical delay. Echocardiography 2015;32:1504-14. [DOI] [PubMed] [Google Scholar]
- 28.Russo V, Rago A, Pannone B, et al. Atrial fibrillation and beta thalassemia major: the predictive role of the 12-lead electrocardiogram analysis. Indian Pacing Electrophysiol J 2014;25:121-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Russo V, Rago A, Pannone B, et al. Early electrocardiographic evaluation of atrial fibrillation risk in beta-thalassemia major patients. Int J Hematol 2011;93:446-51. [DOI] [PubMed] [Google Scholar]
- 30.Kirchhof P, Benussi S, Kotecha D, et at. ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur Heart J 2016;7,2893-962. [DOI] [PubMed] [Google Scholar]
- 31.Proietti R, Joza J, Arensi A, et al. Novel nonpharmacologic approaches for stroke prevention in atrial fibrillation: results from clinical trials. Med Devices (Auckl) 2015;8:103-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Danna P, Proietti R, Sagone A, et al. Does left atrial appendage closure with a cardiac plug system reduce the stroke risk in nonvalvular atrial fibrillation patients? A single-center case series. Pacing Clin Electrophysiol 2013;36:347-53. [DOI] [PubMed] [Google Scholar]
- 33.Russo V, Rago A, Papa AA, et al. Use of non-vitamin K antagonist oral anticoagulants in atrial fibrillation with malignancy: clinical practice experience in a single institution and literature review. Semin Thromb Hemost 2017. December 8. doi: 10.1055/s-0037-1607436. [DOI] [PubMed] [Google Scholar]
- 34.Russo V, Rago A, Papa AA, et al. Budget impact analysis of rivaroxaban vs warfarin anticoagulation strategy for direct current cardioversion in non-valvular atrial fibrillation patients: the MonaldiVert economic study. Minerva Cardioangiol 2017;66:1-5. [DOI] [PubMed] [Google Scholar]
- 35.Russo V, Di Napoli L, Bianchi V, et al. A new integrated strategy for direct current cardioversion in non-valvular atrial fibrillation patients using short term rivaroxaban administration: The MonaldiVert real life experience. Int J Cardiol 2016;1;224:454-5. [DOI] [PubMed] [Google Scholar]
- 36.Stabile G, Russo V, Rapacciuolo A, et al. Transesophageal echocardiograpy in patients with persistent atrial fibrillation undergoing electrical cardioversion on new oral anticoagulants: a multi center registry. Int J Cardiol 2015;184:283-4. [DOI] [PubMed] [Google Scholar]
- 37.Bertaglia E, Anselmino M, Zorzi A, et al. NOACs and atrial fibrillation: incidence and predictors of left atrial thrombus in the real world. Int J Cardiol 2017;249:179-83. [DOI] [PubMed] [Google Scholar]
- 38.Connolly SJ, Ezekowitz MD, Yusuf S, et al. RE-LY steering committee and investigators dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139-51. [DOI] [PubMed] [Google Scholar]
- 39.Russo V, Bianchi V, Cavallaro C, et al. Efficacy and safety of dabigatran in a “real-life” population at high thromboembolic risk and hemorrhagic risk: data from Monaldi Care registry. Eur Rev Pharmacol Sci 2015;19:3961-7. [PubMed] [Google Scholar]
- 40.Russo V, Rago A, D’Onofrio A, et al. The clinical performance of dabigatran in the Italian real-life experience. J Cardiovasc Med (Hagerstown) 2017;18:922-3. [DOI] [PubMed] [Google Scholar]
- 41.Nagarakanti R, Ezekowitz MD, Oldgren J, et al. Dabigatran versus warfarin in patients with atrial fibrillation: an analysis of patients undergoing cardioversion. Circulation 2011;123:131-6. [DOI] [PubMed] [Google Scholar]
- 42.Russo V, Rago A, Papa AA, et al. Efficacy and safety of dabigatran in patients with atrial fibrillazion scheduled for transesophageal echocardiogram-guided direct electrical current cardioversion: a prospective propensity score-matched cohort study. J Thromb Thrombolysis 2018;45:206-12. [DOI] [PubMed] [Google Scholar]
- 43.Vidal A, Vanerio G. Dabigatran and left atrial appendage thrombus. J Thromb Thrombolysis 2012;34:545-7. [DOI] [PubMed] [Google Scholar]
- 44.Morita S, Ajiro Y, Uchida Y. Dabigatran for left atrial thrombus. Eur Heart J 2013;34:2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Azoulay L, Dell’Aniello S, Simon TA. Initiation of warfarin in patients with atrial fibrillation: early effects on ischaemic strokes. Eur Heart J 2013;35:1881-7. [DOI] [PubMed] [Google Scholar]


