Abstract
Hypertension and type 2 diabetes are common comorbidities. Hypertension is twice as frequent in patients with diabetes compared with those who do not have diabetes. Moreover, patients with hypertension often exhibit insulin resistance and are at greater risk of diabetes developing than are normotensive individuals. The major cause of morbidity and mortality in diabetes is cardiovascular disease, which is exacerbated by hypertension. Accordingly, diabetes and hypertension are closely interlinked because of similar risk factors, such as endothelial dysfunction, vascular inflammation, arterial remodelling, atherosclerosis, dyslipidemia, and obesity. There is also substantial overlap in the cardiovascular complications of diabetes and hypertension related primarily to microvascular and macrovascular disease. Common mechanisms, such as upregulation of the renin-angiotensin-aldosterone system, oxidative stress, inflammation, and activation of the immune system likely contribute to the close relationship between diabetes and hypertension. In this article we discuss diabetes and hypertension as comorbidities and discuss the pathophysiological features of vascular complications associated with these conditions. We also highlight some vascular mechanisms that predispose to both conditions, focusing on advanced glycation end products, oxidative stress, inflammation, the immune system, and microRNAs. Finally, we provide some insights into current therapies targeting diabetes and cardiovascular complications and introduce some new agents that may have vasoprotective therapeutic potential in diabetes.
Résumé
L’hypertension et le diabète de type 2 sont des affections concomitantes fréquentes. L’hypertension est deux fois plus fréquente chez les patients atteints de diabète que chez ceux qui n’en sont pas atteints. De plus, les patients atteints d’hypertension sont souvent résistants à l’insuline et sont plus susceptibles de souffrir de diabète que les personnes normotendues. Chez les diabétiques, la principale cause de morbidité et de mortalité est la maladie cardiovasculaire, qui est exacerbée par l’hypertension. En conséquence, le diabète et l’hypertension sont étroitement interreliés en raison de facteurs de risques similaires, comme la dysfonction endothéliale, l’inflammation vasculaire, le remodelage artériel, l’athérosclérose, la dyslipidémie et l’obésité. On observe un chevauchement important entre les complications cardiovasculaires du diabète et celles de l’hypertension liées principalement à des maladies microvasculaires et macrovasculaires. Des mécanismes communs, comme une stimulation du système rénine-angiotensine-aldostérone, un stress oxydatif, une inflammation et une activation du système immunitaire, sont susceptibles de contribuer à la relation étroite entre le diabète et l’hypertension. Dans cet article, nous abordons le diabète et l’hypertension comme des affections concomitantes et nous parlons des caractéristiques physiopathologiques des complications vasculaires associées à ces affections. Nous soulignons également certains mécanismes vasculaires qui prédisposent à ces deux affections, en mettant l’accent sur les produits finaux de glycation avancée, le stress oxydatif, l’inflammation, le système immunitaire et les micro-ARN. Finalement, nous présentons certaines connaissances sur les traitements actuels ciblant le diabète et les complications cardiovasculaires et nous présentons de nouveaux agents qui pourraient avoir un pouvoir vasoprotecteur chez les patients diabétiques.
Type 2 Diabetes Mellitus and Hypertension
The prevalence of obesity and type 2 diabetes (T2D) continues to rise worldwide as lifestyles associated with low energy expenditure and high caloric intake are increasingly adopted, particularly in lower-income and developing countries. It is predicted that the number of cases of T2D will rise from 415 million to 642 million by 2040.1 Hypertension is even more common, rising in prevalence in the same countries, with a recent worldwide estimate of 1.39 billion cases.2
Although T2D and hypertension can be simply diagnosed at the bedside, they are each complex and heterogeneous phenotypes associated with an elevated risk of life-threatening cardiovascular disease (CVD). Their frequent coexistence in the same individual is not a coincidence, because aspects of the pathophysiology are shared by both conditions, particularly those related to obesity and insulin resistance. For example, in the San Antonio Heart Study, 85% of those with T2D had hypertension by the fifth decade of life, whereas 50% of those with hypertension experienced impaired glucose tolerance or T2D.3
In health, insulin maintains glucose homeostasis by integrated actions on carbohydrate, protein, and lipid metabolism. Loss of sensitivity to aspects of insulin action (insulin resistance) principally affects the liver, muscle, and adipose tissues and is selective for glucose and lipid metabolism, eg, sparing insulin's action to retain sodium in the distal tubule.4, 5 Reduction in insulin-mediated glucose disposal leads to compensatory hypersecretion of insulin to maintain homeostasis: Glucose intolerance ensues if this endocrine pancreas response is inadequate, although some obese individuals avoid T2D by virtue of a supranormal B-cell response.6 Recently, the role of adipose tissue in these associations has been increasingly appreciated.7
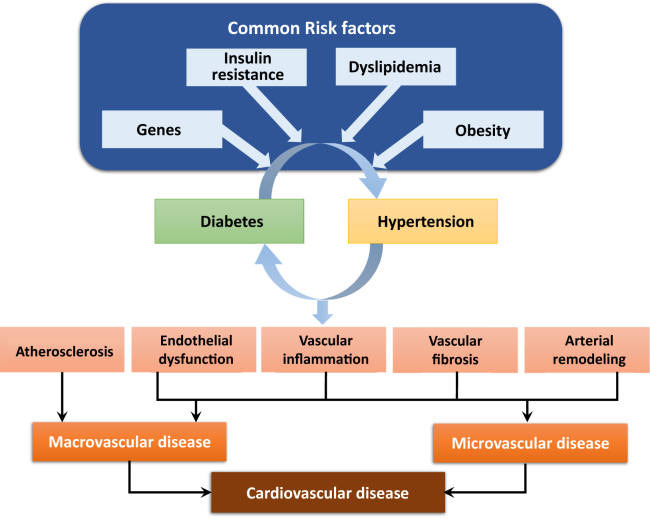
Diabetes is associated with both macrovascular (involving large arteries such as conduit vessels) and microvascular (involving small arteries and capillaries) disease. Chronic hyperglycemia and insulin resistance play an important role in the initiation of vascular complications of diabetes and involve a number of mechanisms including (1) increased formation of advanced glycation end products (AGEs) and activation of the receptor for advanced glycation end products (RAGE) AGE-RAGE axis, (2) oxidative stress, and (3) inflammation.8 In addition, emerging evidence suggests a role for microRNAs (miRNAs) in the vasculopathy of diabetes (see further on).9 Hypertension is an important risk factor for diabetes-associated vascular complications, because hypertension itself is characterized by vascular dysfunction and injury (Fig. 1).
Figure 1.
Vascular processes whereby diabetes and hypertension predispose to cardiovascular disease. Common risk factors promote diabetes and hypertension, which are associated with atherosclerosis, vascular inflammation, endothelial dysfunction, and structural remodelling, which lead to macrovascular and microvascular disease. Vascular damage and endothelial dysfunction is amplified when diabetes and hypertension coexist.
In this review, we focus on vascular complications of diabetes and discuss the impact of comorbidities, specifically hypertension. The role of oxidative stress and inflammation as “common soil” for metabolic and vascular disease are highlighted. We also discuss how some of the newer agents used in the treatment of T2D can influence blood pressure (BP) regulation and the risk of CVD, with an eye to future developments more specifically targeting vascular protection.
Macrovascular Disease
Clinical features
Macrovascular (or cardiovascular) disease of larger conduit arteries is a complex inflammatory process leading to myocardial infarction, stroke, and peripheral artery disease. The primary pathologic process associated with macrovascular disease is atherosclerosis, which in diabetes is accelerated with extensive distribution of vascular lesions.10 T2D confers an approximate 2-fold elevation in CVD risk, equivalent to that of a previous myocardial infarction.11, 12 Moreover, patients with T2D have poorer outcomes after an acute coronary syndrome and higher rates of reinfarction and heart failure.13
Elevation of CVD risk begins at the stage of prediabetes in association with insulin resistance and impaired glucose tolerance.14 As well as being the diagnostic hallmark of T2D, hyperglycemia is the principal determinant of microvascular complications of T2D and plays an important role in the pathogenesis of CVD. However, in established T2D, it is a relatively weak modifiable risk factor compared with hypertension, dyslipidemia, and (unfortunately in many populations) cigarette smoking.15, 16
Pathophysiological features
Insulin resistance is detectable for several years before the onset of T2D. It is associated with obesity, particularly central obesity, but may be present in lean individuals with hypertension.17 During calorie excess, adipocytes in obese humans—whether in subcutaneous or visceral areas—undergo hypertrophy. Visceral adipocytes are more susceptible to cellular death as they begin to enlarge and their stromal vascular fraction becomes infiltrated with macrophages.18
These macrophages around dead adipocytes form “crown-like structures,” a histologic appearance that is associated with expression of cytokines (including tumor necrosis factor-α [TNF-α], interleukin-6 [IL-6]), and inducible nitric oxide synthase.19 These changes have been shown to coincide with the onset of insulin resistance and provide a pathophysiological link between metabolic and vascular disease.20
In addition to these proinflammatory changes, adipocyte hypertrophy is associated with larger triglyceride stores, a higher lipolytic rate, and an atherogenic lipid profile: elevated concentrations of small dense low-density lipoprotein cholesterol, high concentrations of triglycerides, triglyceride-rich remnants, very low-density lipoprotein cholesterol, and apolipoprotein B, usually in combination with low levels of high-density lipoprotein cholesterol.7 This profile is associated with increased production of leptin, decreased production of adiponectin, higher circulating levels of nonesterified fatty acids (NEFAs), and activation of mitochondrial oxidative stress pathways in vascular endothelial cells.7
These proinflammatory and metabolic consequences of obesity and insulin resistance result in endothelial dysfunction, a key antecedent and modulator of atherosclerosis that has been demonstrated not only in hypertension but also in prediabetes,21 first-degree relatives of individuals with T2D,22 and even insulin-resistant healthy individuals.22, 23 It is characterized by disruption of the intricate physiological balance between vasoconstrictors (endothelin, angiotensin II) and vasodilators (nitric oxide, prostacyclin), growth promoting and inhibitory factors, proatherogenic and antiatherogenic factors, and procoagulant and anticoagulant factors.24, 25 A substantial body of evidence suggests that impaired endothelium-dependent vasodilation may in turn contribute to or exacerbate insulin resistance by limiting the delivery of substrate (glucose) to key target tissues.26
In addition to these functional changes, an associated low-grade inflammation in endothelial and smooth muscle cells of the vascular wall causes cell proliferation, hypertrophy, remodelling, and apoptosis.27 This accelerates disruption of the balance between the arterial wall scaffolding proteins elastin and collagen that determine vascular compliance, a form of “vascular aging,” which is a characteristic phenotype in hypertension.28, 29, 30, 31 Vascular stiffening leads to widening of arterial pulse pressure and increased pulsatile shear, exacerbating endothelial dysfunction and vascular disease.32
Microvascular Disease
Clinical features
Microvascular disease leads to retinopathy, nephropathy, and neuropathy, which are major causes of morbidity and mortality in patients with diabetes. In the United States, diabetic retinopathy affects about 28% of individuals with established T2D.33 Worldwide it is responsible for 10,000 cases of blindness every year.34, 35 Diabetic nephropathy affects about 25% of individuals with T2D and is the most common cause of renal failure in the United States.36 Neuropathy affects about 20% of these individuals, although it is estimated that about 50% have neuropathy at some point in their lives.36 Each of these organ-specific microvascular complications has its own unique clinical and histologic features, but all are common with increasing duration of hyperglycemia and are driven by its downstream cellular effects, including polyol accumulation (resulting from saturation of the hexokinase pathway and consequent increased activity of aldose reductase), AGE-induced injury, increased vascular permeability, and oxidative stress.8
Follow-up of the Action in Diabetes and Vascular Disease: Preterax and Diamicron Controlled Evaluation (ADVANCE) trial cohort has confirmed that the presence of microvascular complications increases the risk of cardiovascular complications in individuls with T2D.37 Moreover, the coexistence of hypertension and retinopathy is a risk factor for the progression of nephropathy. There is evidence that treatment of hypertension with angiotensin II receptor blockers can reduce the progression of retinopathy in addition to well-known effects on nephropathy.38
Pathophysiological features
Pathognomonic alterations of diabetic microangiopathy include capillary basement membrane thickening, increased endothelial permeability, and endothelial and vascular smooth muscle cell dysfunction. Hyperglycemia is the key stimulus for these processes by stimulating vasoinjurious signalling pathways, activating the polyol pathway, increasing oxidative stress, stimulating proinflammatory transcription factors, and activation of immune responses. Similar processes are induced by hypertension.39
Mechanisms of Vascular Complications in Diabetes and the Impact of Hypertension
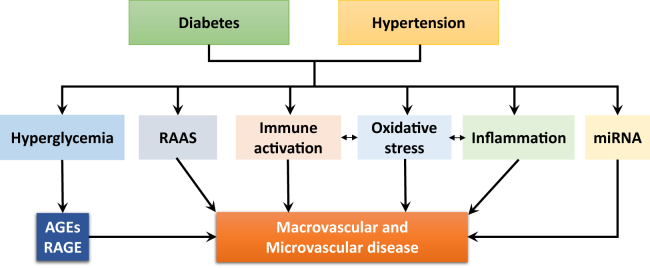
A number of interacting mechanisms are in play as summarized in the following sections (Fig. 2).
Figure 2.
Putative mechanisms whereby diabetes and hypertension cause vascular disease. Immune cell activation and inflammation are mediated through oxidative stress. AGEs, advanced glycation end products; RAAS, renin-angiotensin-aldosterone system; RAGE, receptor AGE.
AGE-RAGE axis
AGEs are compounds that have undergone irreversible posttranslational modifications because of reactions between sugars and amino groups on proteins and nucleic acids. Hyperglycemia accelerates formation of AGEs, which accumulate in the extracellular matrix of vessels and contribute to vascular damage in diabetes.40 AGEs stimulate production of reactive oxygen species (ROS), which in turn further enhance AGE formation. AGEs are also antigenic and hence induce immune responses.40 In addition to AGEs, dicarbonyl methylglyoxal, a by-product of glycolysis, accumulates in tissues and contributes to diabetes-associated vascular damage.41
AGEs interact with 2 main types of cell surface receptors: (1) scavenger receptors, which remove and degrade AGEs, and (2) receptors for AGEs (RAGE), which trigger specific cellular signalling responses on AGE binding. RAGE is a member of the immunoglobulin family and binds many ligands besides AGEs, such as high mobility group protein B1, S100 calcium-binding proteins (including calgranulin), amyloid-β-protein, and amphotericin. AGE-RAGE signals through transforming growth factor (TGF)-β, NF-κB, mitogen-activated protein kinases (MAPK; ERK1/2, p38MAPK), and nicotinamide adenine dinucleotide phosphate (NADPH) oxidases (Nox) and induces expression of vascular adhesion molecule 1, E-selectin, vascular endothelial growth factor, and proinflammatory cytokines (IL-1β, IL-6, TNF-α).42 In diabetes, activation of these signalling pathways is increased in vascular smooth muscle cells, leading to vascular fibrosis, calcification, inflammation, prothrombotic effects, and vascular damage, processes underlying diabetic nephropathy, retinopathy, neuropathy, and atherosclerotic CVD.43 Coexisting hypertension amplifies these complications and contributes to the accelerated vasculopathy in diabetes.44 Patients with diabetes have increased tissue and circulating concentrations of AGEs and soluble RAGE, which is predictive of cardiovascular events and all-cause mortality. As such, urinary and plasma AGE levels and soluble RAGE may act as biomarkers for vascular disease in diabetes.45
Targeting AGE-RAGE has been considered a potential therapeutic strategy to reduce or prevent CVD in diabetes. A number of large clinical trials investigating cardiovascular benefits of alagebrium (ALT-711), which reduces accumulation of AGEs by cleaving AGE cross-links, have been undertaken. They include Distensibility Improvement and Remodeling in Diastolic Heart Failure (DIAMOND; NCT00043836), Systolic and Pulse Pressure Hemodynamic Improvement By Restoring Elasticity (SAPPHIRE; NCT00045981), Systolic Hypertension Interaction With Left Ventricular Remodeling (SILVER; NCT00045994), Systolic Pressure Efficacy and Safety Trial of Alagebrium (SPECTRA; NCT00089713), Beginning a Randomized Evaluation of the AGE Breaker Alagebrium in Diastolic Heart Failure I (BREAK-DHF-I; NCT00662116), and Evaluating the Efficacy and Safety of Alagebrium (ALT-711) in Patients With Chronic Heart Failure (BENEFICIAL; NCT00516646). However few data have been published from these studies. Some small clinical studies demonstrated cardiovascular benefit in patients with diabetes and hypertension.46 In particular, alagebrium improved endothelial function, reduced aortic stiffness, and increased vascular compliance.47
Oxidative stress and Nox
Oxidative stress is a key mechanism of glucotoxicity in diabetes, as evidenced by increased vascular ROS generation in response to hyperglycemia and accumulation of oxidation by-products of lipids, proteins, and nucleic acids.27 NADPH oxidases and dysfunctional endothelial nitric oxide synthase are principal sources of increased ROS in human vasculature in T2D.48, 49 ROS interact with DNA and stimulate many redox-sensitive signalling pathways that lead to inflammation, fibrosis, and vascular damage. Increased vascular oxidative stress in diabetes and hypertension promotes posttranslational oxidative modification of proteins, causing cellular damage and vascular dysfunction. Hyperglycemia also induces activation of redox-sensitive protein kinase C and polyol and hexosamine pathways, further contributing to mitochondrial dysfunction, oxidative stress, endoplasmic reticulum stress, and consequent cellular damage.50 Oxidative stress is also associated with reduced bioavailability of the vasodilator nitric oxide, causing endothelial dysfunction.
Diabetes-induced oxidative stress is caused by numerous processes, including glucose-stimulated mitochondrial respiration, endoplasmic reticulum stress, activation of the renin-angiotensin system (which is pro-oxidant), decreased vascular antioxidant capacity, reduced activity of the master antioxidant transcription factor nuclear factor-erythroid 2-related factor (Nrf-2), and activation of Nox isoforms.51 Of these mechanisms activation of Nox types is particularly important. Four Nox isoforms have been demonstrated in human vessels, including Nox1, Nox2, Nox4, and Nox5. Nox-derived ROS influence redox-sensitive signalling pathways in vascular cells such as MAPKs, protein tyrosine phosphatases, transcription factors, Ca2+ channels, ion transporters, and proinflammatory genes.52 In diabetes and hypertension, oxidative stress (increased ROS bioavailability) promotes vascular inflammation, fibrosis, and injury, processes that are normalized by Nox inhibitors or ROS scavengers, or both. Nox1, but not Nox4, seems to be important in atherosclerosis in diabetes, as we demonstrated in Nox1-deficient mice on the atherosclerosis-prone ApoE−/− background made diabetic with streptozotocin.53 Nox4 has been implicated in renal injury in mouse models of diabetes, effects that are ameliorated with Nox1/4 inhibitors and in mice deficient in Nox4.54, 55 Nox5 may also be important in diabetes-associated vascular injury and nephropathy. We demonstrated that renal Nox5 expression is increased in patients with diabetic nephropathy. Moreover, in transgenic mice with podocyte-specific expression of human Nox5, renal injury was amplified by diabetes.56 Similar findings were observed in mice expressing human Nox5 in a vascular smooth muscle cell-specific manner.57 Although extensive experimental evidence showed a renoprotective effect of Nox4 inhibition in diabetes, a recent clinical study using GKT137831, a Nox1/4 inhibitor, failed to show improvement in renal function in patients with diabetic nephropathy.58 Whether targeting Nox5 may have better clinical outcomes is unclear, because to date there are no Nox5 inhibitors available.
Inflammation and the immune system
Links between inflammation and the immune system with metabolic dysfunction, hypertension, and cardiovascular morbidity are supported by extensive experimental data.59 This encompasses a number of immune metabolic aspects, including the key role of the tricarboxylic cycle or sphingosine-1-phosphate in the regulation of vascular inflammation.59, 60 Clinical studies have shown that patients with T2D have increased total leukocyte counts, particularly neutrophils and lymphocytes, that correlate with insulin sensitivity,61 which is in part mediated by inflammatory changes of adipose tissue.62 Inflammatory biomarkers are also useful in developing targeted cardiovascular therapies in the context of metabolic dysfunction.63 The link between inflammation and T2D is further supported by genetic studies and clinical trials showing protective effects of immune-targeted therapies and anti-inflammatory actions of classic antidiabetes drugs.64 Circulating and locally produced effector cytokines such as TNF-α, interferon-γ, IL-1β, and IL-12 may influence insulin sensitivity of peripheral tissues and can modulate insulin release in the pancreatic islets.65, 66, 67, 68 Increased glucotoxicity and lipotoxicity have been associated with immune cell infiltration of target tissues, thereby affecting diabetes-associated target organ damage and cardiovascular complications,68, 69 including the development of metabolic cardiomyopathy.70, 71 Inflammation is a key modulator of metabolic and diabetic CVD.
Genetic evidence
Although genome-wide association studies (GWAS) for insulin resistance or T2D have not shown strong associations with immune-related genes, numerous metabolic traits are linked to immune-related loci.72 Studies integrating metabochip approaches with GWAS have shown that classic immunometabolic genes including JNK signalling pathways (such as MAP3K1), nuclear factor kappa B (NF-κB) regulators (MACROD1), inflammasome activators (NRF3), and interferon-γ receptor genes associate with T2D.73, 74 This also corresponds to results of recent large T2D GWAS that identified genes related to macrophage function and antigen presentation (MAEA, ST6GAL1), and T-cell signalling (CMIP or PTPRJ).72, 75 While trying to interpret these important studies, it should be appreciated that GWAS approaches have limitations, because only a small component of heritability of complex traits is directly explainable by single-gene variability.76
Clinical evidence
Increasing clinical evidence indicates an immune component in T2D and its cardiovascular complications. Immune-targeted therapies currently available for the treatment of rheumatoid arthritis and autoimmune disorders, including anti-TNF therapies, may prevent insulin resistance as well as cardiovascular risk.64, 77 A recent meta-analysis of studies with anti-TNF agents supports an overall protective effect of anti-TNF therapies on lifetime risk of diabetes as well as insulin sensitivity and obesity.74
A recent large proof of concept trial of anti-inflammatory therapy in patients after myocardial infarction (A Randomized, Double-blind, Placebo-controlled, Event-driven Trial of Quarterly Subcutaneous Canakinumab in the Prevention of Recurrent Cardiovascular Events Among Stable Post-Myocardial Infarction Patients With Elevated hsCRP [CANTOS]; canakinumab targeting IL-1β) showed a clear reduction in the rate of cardiovascular events, albeit with an associated increase in the rate of severe infections.78 These results were particularly evident in high-risk patients, although effects on metabolic profile remain unclear.78 However, evidence that IL-1β targeting may have significant metabolic benefits has been well established, as evidenced by improved profile insulin sensitivity in response to IL1-β blockade.79 The potential beneficial effects of anti-inflammatory and immune-modulating agents in T2D and its complications may relate to direct vasoprotective effects. These studies have led to the rapid development of the concept of immunometabolism, clearly linking metabolic changes in the tissues to the regulation of inflammation as well as metabolic status of immune cells to their activation.28, 56 The latter can be characterized by a switch between oxidative phosphorylation and anaerobic glycolysis, which is observed in macrophages and T cells.30, 59 This also emphasizes the importance of the interplay between vascular oxidative stress and the development of inflammation in adipose tissue and the vasculature.
Anti-inflammatory properties of antidiabetic therapies
Classic approaches improving metabolic health, such as weight reduction and the use of metformin, statin drugs, pioglitazone, and insulin have been shown to have anti-inflammatory effects. Metformin reduces C-reactive protein levels by 13%. More recently, a novel anti-inflammatory mechanism of metformin affecting M1/M2 polarization of macrophages has been shown to reduce obesity-associated low-grade inflammation, possibly because of adenosine monophosphate-activated protein kinase (AMPK) activation. These effects were modulated by AMPK and the AMPK analogue 5-aminoimidazole-4-carboxamide ribonucleotide, effects that appear stronger than those of metformin.80 Recent studies have shown that salicylates have anti-inflammatory effects that involve inhibition of NF-κB and that they also prevent diabetes and improve insulin resistance in experimental models and humans.81, 82 Drugs such as glicazide and troglitazone, as well as N-acetylcysteine, decrease inflammatory markers in patients with diabetic nephropathy and diabetic retinopathy.83
Epigenetics is another mechanism that may influence inflammation and immunometabolism in diabetes.59 Histone deacetylase (HDAC) inhibitors cause NF-κB inhibition through acetylation of the p65 subunit. Givinostat (formerly ITF2357), an orally active HDAC inhibitor, has been shown to prevent the development of diabetes.84, 85 Similarly, activation of sirtuin1, which is involved in inflammation, metabolism, and aging, has been shown to have anti-inflammatory properties in diabetes.86
MiRNAs, Diabetes, and Vascular Complications
miRNAs are a group of noncoding RNAs that are multifunctional. They fine tune gene expression and have been implicated in various pathologic processes, including T2D and the development of diabetic vascular complications. A number of pancreatic B-cell–specific miRNAs have been identified, including miR-375, miR-124a, miR-96, miR-7a, miR7a2, miR-30d, miR-9, miR-200, miR-184, and let-7.87 These play a role in pancreatic function, insulin secretion, and glucose tolerance. Differential miRNA signatures have been identified among prediabetic individuals, patients with diabetes, and patients with diabetes and vascular complications, suggesting that miRNAs may be novel biomarkers. Diabetic cardiovascular complications are associated with increased levels of miR-223, miR-320, miR-501, miR504, and miR1 and decreased levels of miR-16, miR-133, miR-492, and miR-373.9 Whether these changes in miRNA are simply biomarkers of disease or whether they are directly involved in the vasculopathy of diabetes remains unclear.
Treatment of diabetes mellitus and its cardiovascular complications
Once T2D has been diagnosed, the aim of achieving glucose control is principally to avoid microvascular complications. There are some benefits with respect to macrovascular complications, but this is dependent on the profile of individual drug classes and even appears to be different for agents within the same class.88 The role of BP lowering to improve prognosis in T2D has been established since the UK Prospective Diabetes Study (UKPDS) in 1998.89, 90 However, more recently, more widespread use of glucose-lowering agents that reduce (rather than increase) weight, lower BP, and have beneficial “off-target” effects (as demonstrated in recent large cardiovascular outcome trials) facilitates cardiovascular risk factor control and is playing a role in improving the cardiovascular prognosis of T2D.91, 92
Achieving glucose control in T2D begins with weight management. Particularly in the first 8 years after diagnosis, normal glucose tolerance can be restored if radical weight reduction can be achieved, most effectively using a very low calorie liquid replacement diet.93 In obese patients, this can also occur after successful bariatric surgery, particularly the Roux-en-Y procedure.94 The mechanism may involve reduction in ectopic fat, and consequent relief from its proinflammatory effects, in and around the pancreatic islets of Langerhans.95
All current glucose-lowering guidelines suggest the early addition of metformin as first-line therapy. Unlike the sulphonylureas, which augment insulin secretion, metformin lowers blood glucose levels principally by decreasing hepatic glucose production and promoting weight reduction (with little effect on BP). Among the many proposed mechanisms of action of metformin is activation of AMPK: This is now thought to be a secondary effect of inhibition of the mitochondrial respiratory chain.96 Such effects of metformin may act directly (ie, independent of blood glucose lowering) on other tissues, including vascular endothelial cells. Metformin treatment is associated with improvements in endothelial biomarkers and reduction in plasma high-sensitivity C-reactive protein levels.97, 98 It was associated with cardiovascular benefit in the landmark UKPDS.99
Other second-line agents used in glucose lowering include pioglitazone, a thiazolidinedione that directly promotes the differentiation of adipocytes within subcutaneous adipose depots (by activation of peroxisome proliferator-activated receptor-γ), thus promoting storage of non-esterified fatty acids (NEFAs).100 Pioglitazone reverses many of the metabolic features associated with insulin resistance without much effect on BP. Anti-inflammatory effects have been demonstrated in human adipose tissue biopsy samples and also in some animal models.101 There was great hope in the 1990s that agents from this class would have major benefits for the cardiovascular system, a hypothesis that was to some extent supported by the results of the Prospective Pioglitazone Clinical Trial in Macrovascular Events (PROACTIVE) cardiovascular outcome trial, although beneficial effects were offset by weight gain and fluid retention.102
More recently introduced classes of glucose-lowering agents have heralded an exciting era in T2D pharmacotherapy because they are associated with weight reduction, BP reduction, and, importantly, reduced rates of major adverse events in long-term cardiovascular outcome trials.91, 92, 103
Glucagon-like peptide-1 agonists are injectable agents that augment glucose-dependent insulin secretion (the “incretin” effect), delay gastric emptying (enhancing satiety), and have central effects on hypothalamic nuclei to reduce appetite.104 Systolic BP is lowered beyond the effect that would be expected purely from weight loss, and there is an improvement in pulse-wave velocity, reflecting a reduction in arterial stiffness. However, the time course of cardiovascular event reduction in the Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results (LEADER) trial suggests a primary antiatherosclerotic rather than hemodynamic effect.91 Indeed, liraglutide has been shown to have anti-inflammatory actions on the cardiovascular system in a number of preclinical and clinical studies.103, 105
SGLT2 inhibitors promote lowering of the threshold for urinary glucose excretion: an additional glucose equivalent to 300 kcal per day is therefore cleared by the kidneys, promoting weight loss and a catabolic state with increased circulating ketone bodies and NEFAs.106 There are associated reductions in BP and plasma volume, which together may have been responsible for the early reduction in cardiovascular event rates seen with empagliflozin in Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) trial.91 A shift in fuel substrate metabolism from glucose to NEFAs and ketones, including by the myocardium, is 1 of the mechanisms by which SGLT2 inhibitors may provide cardiovascular protection,107 but studies in apoE knockout mice and Zucker diabetic fatty rats suggest that anti-inflammatory effects may also play a role.108
Diabetes, vasoprotection, and potential new therapies
Data from landmark clinical trials in T2D including UKPDS, ADVANCE, and Action to Control Cardiovascular Risk in Diabetes (ACCORD) demonstrate that treating comorbidities including hypertension and hypercholesterolemia is a more effective strategy for reducing cardiovascular complications than targeting blood glucose levels with conventional agents.109 Antihypertensive drugs such as angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, mineralocorticoid-receptor blockers, and calcium-channel blockers may have direct vasoprotective effects, and their use may contribute, at least in part, to reduced vascular complications in patients with diabetes and concomitant hypertension.110 Tight control of BP has been shown to reduce cardiovascular risk in T2D: most recent US and Canadian guidelines recommend a target of < 130/80 mm Hg.111, 112 Statin drugs and clopidrogel are also vasoprotective and may have extra benefit in patients with diabetes. Some of the beneficial effects of these drugs have been attributed to their antioxidant and anti-inflammatory properties.
New therapeutic approaches targeting oxidative stress, inflammation, and fibrosis are currently being developed to treat diabetes-associated cardiovascular complications.113 In particular, drugs that increase Nrf-2 activity, such as bardoxolone methyl, and strategies to inhibit the pyrin domain containing 3 (NLRP3) inflammasome, may have therapeutic potential. A novel bardoxolone methyl derivative, dh404, has been shown to attenuate endothelial dysfunction, reduce Nox1 expression, decrease oxidative stress, and inhibit inflammation in diabetic mice, suggesting that upregulation of Nrf2 may have therapeutic potential to limit diabetes-associated vascular damage.114 Another example includes inhibition of dipeptidyl peptidase-4 by linagliptin, which reduces obesity-related insulin resistance and inflammation by regulating M1/M2 macrophage status.115 Other therapies on the horizon for the treatment of cardiovascular complications of diabetes include pentoxifylline (methylxanthine derivative and nonspecific phosphodiesterase inhibitor with anti-inflammatory and antifibrotic effects), ruboxistaurin (selective protein kinase C-β inhibitor), pirfenidone (TGF-β inhibitor), bindarit (MCP-1/CCL2 inhibitor), sulodexide (an oral formulation composed of 2 glycosaminoglycans), AKB-9778 (Tie2 activator), baricitinib (JAK/STAT inhibitor), and Nox inhibitors.116 The clinical benefit of these compounds awaits further confirmation, and novel nanotherapeutic approaches are being developed to target inflammation.117
Conclusions
Diabetes is associated with an increased risk of CVD, which is exaggerated with coexistent hypertension. Many of the underlying molecular mechanisms, including oxidative stress, inflammation, and fibrosis causing microvascular and macrovascular complications of diabetes, also cause vascular remodelling and dysfunction in hypertension. Controlling comorbidities, especially hypertension, and targeting strategies to promote vascular health, may be especially important in reducing the microvascular and macrovascular complications of diabetes.
Funding Sources
This work was supported by grants from the British Heart Foundation (RG/13/7/30099, RE/13/5/30177), the Wellcome Trust Senior Biomedical Fellowship (to T.J.G.), and the National Science Centre of Poland (2011/03/B/NZ4/02454).
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 581 for disclosure information.
References
- 1.Ogurtsova K., da Rocha Fernandes J.D., Huang Y. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 2.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitchell B.D., Stern M.P., Haffner S.M., Hazuda H.P., Patterson J.K. Risk factors for cardiovascular mortality in Mexican Americans and non-Hispanic whites. San Antonio Heart Study. Am J Epidemiol. 1990;131:423–433. doi: 10.1093/oxfordjournals.aje.a115517. [DOI] [PubMed] [Google Scholar]
- 4.Defronzo R.A. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58:773–795. doi: 10.2337/db09-9028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeFronzo R.A., Cooke C.R., Andres R., Faloona G.R., Davis P.J. The effect of insulin on renal handling of sodium, potassium, calcium, and phosphate in man. J Clin Invest. 1975;55:845–855. doi: 10.1172/JCI107996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrannini E., Mari A. β-cell function in type 2 diabetes. Metabolism. 2014;63:1217–1227. doi: 10.1016/j.metabol.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Jung U.J., Choi M.S. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15:6184–6223. doi: 10.3390/ijms15046184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615–1625. doi: 10.2337/diabetes.54.6.1615. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y., Sun X., Icli B., Feinberg M.W. Emerging roles for microRNAs in diabetic microvascular disease: novel targets for therapy. Endocr Rev. 2017;38:145–168. doi: 10.1210/er.2016-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kattoor A.J., Pothineni N.V.K., Palagiri D., Mehta J.L. Oxidative stress in atherosclerosis. Curr Atheroscler Rep. 2017;19:42. doi: 10.1007/s11883-017-0678-6. [DOI] [PubMed] [Google Scholar]
- 11.Juutilainen A., Lehto S., Rönnemaa T., Pyörälä K., Laakso M. Type 2 diabetes as a “coronary heart disease equivalent”: an 18-year prospective population-based study in Finnish subjects. Diabetes Care. 2005;28:2901–2907. doi: 10.2337/diacare.28.12.2901. [DOI] [PubMed] [Google Scholar]
- 12.Haffner S.M., Lehto S., Ronnemaa T., Pyorala K., Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 13.Abbott R.D., Donahue R.P., Kannel W.B., Wilson P.W. The impact of diabetes on survival following myocardial infarction in men vs women. The Framingham Study. JAMA. 1988;260:3456–3460. [PubMed] [Google Scholar]
- 14.Balkau B., Eschwège E., Papoz L. Risk factors for early death in non-insulin dependent diabetes and men with known glucose tolerance status. BMJ. 1993;307:295–299. doi: 10.1136/bmj.307.6899.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller M.E., Williamson J.D., Gerstein H.C. Effects of randomization to intensive glucose control on adverse events, cardiovascular disease, and mortality in older versus younger adults in the ACCORD trial. Diabetes Care. 2014;37:634–643. doi: 10.2337/dc13-1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gæde P., Oellgaard J., Carstensen B. Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia. 2016;59:2298–2307. doi: 10.1007/s00125-016-4065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrannini E., Buzzigoli G., Bonadonna R. Insulin resistance in essential hypertension. N Engl J Med. 1987;317:350–357. doi: 10.1056/NEJM198708063170605. [DOI] [PubMed] [Google Scholar]
- 18.Giordano A., Murano I., Mondini E. Obese adipocytes show ultrastructural features of stressed cells and die of pyroptosis. J Lipid Res. 2013;54:2423–2436. doi: 10.1194/jlr.M038638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Antoniades C. ‘Dysfunctional’ adipose tissue in cardiovascular disease: a reprogrammable target or an innocent bystander? Cardiovasc Res. 2017;113:997–998. doi: 10.1093/cvr/cvx116. [DOI] [PubMed] [Google Scholar]
- 20.Camastra S., Vitali A., Anselmino M. Muscle and adipose tissue morphology, insulin sensitivity and beta-cell function in diabetic and nondiabetic obese patients: effects of bariatric surgery. Sci Rep. 2017;7:9007. doi: 10.1038/s41598-017-08444-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su Y., Liu X.M., Sun Y.M. Endothelial dysfunction in impaired fasting glycemia, impaired glucose tolerance, and type 2 diabetes mellitus. Am J Cardiol. 2008;102:497–498. doi: 10.1016/j.amjcard.2008.03.087. [DOI] [PubMed] [Google Scholar]
- 22.Scuteri A., Tesauro M., Rizza S. Endothelial function and arterial stiffness in normotensive normoglycemic first-degree relatives of diabetic patients are independent of the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2008;18:349–356. doi: 10.1016/j.numecd.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 23.Petrie J.R., Ueda S., Webb D.J., Elliott H.L., Connell J.M. Endothelial nitric oxide production and insulin sensitivity. A physiological link with implications for pathogenesis of cardiovascular disease. Circulation. 1996;93:1331–1333. doi: 10.1161/01.cir.93.7.1331. [DOI] [PubMed] [Google Scholar]
- 24.Creager M.A., Lüscher T.F., Cosentino F., Beckman J.A. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Circulation. 2003;108:1527–1532. doi: 10.1161/01.CIR.0000091257.27563.32. [DOI] [PubMed] [Google Scholar]
- 25.Weiss N., Keller C., Hoffmann U., Loscalzo J. Endothelial dysfunction and atherothrombosis in mild hyperhomocysteinemia. Vasc Med. 2002;7:227–239. doi: 10.1191/1358863x02vm428ra. [DOI] [PubMed] [Google Scholar]
- 26.Meijer R.I., De Boer M.P., Groen M.R. Insulin-induced microvascular recruitment in skin and muscle are related and both are associated with whole-body glucose uptake. Microcirculation. 2012;19:494–500. doi: 10.1111/j.1549-8719.2012.00174.x. [DOI] [PubMed] [Google Scholar]
- 27.Savoia C., Sada L., Zezza L. Vascular inflammation and endothelial dysfunction in experimental hypertension. Int J Hypertens. 2011:281240. doi: 10.4061/2011/281240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harvey A., Montezano A.C., Touyz R.M. Vascular biology of ageing-Implications in hypertension. J Mol Cell Cardiol. 2015;83:112–121. doi: 10.1016/j.yjmcc.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guzik T.J., Touyz R.M. Oxidative stress, inflammation, and vascular aging in hypertension. Hypertension. 2017;70:660–667. doi: 10.1161/HYPERTENSIONAHA.117.07802. [DOI] [PubMed] [Google Scholar]
- 30.Barton M., Husmann M., Meyer M.R. Accelerated vascular aging as a paradigm for hypertensive vascular disease: prevention and therapy. Can J Cardiol. 2016;32:680–686. doi: 10.1016/j.cjca.2016.02.062. [DOI] [PubMed] [Google Scholar]
- 31.Yin H., Pickering J.G. Cellular senescence and vascular disease: novel routes to better understanding and therapy. Can J Cardiol. 2016;32:612–623. doi: 10.1016/j.cjca.2016.02.051. [DOI] [PubMed] [Google Scholar]
- 32.Zieman S.J., Melenovsky V., Kass D.A. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25:932–943. doi: 10.1161/01.ATV.0000160548.78317.29. [DOI] [PubMed] [Google Scholar]
- 33.Zhang X., Saaddine J.B., Chou C.F. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010;304:649–656. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fong D.S., Aiello L.P., Ferris F.L., 3rd, Klein R. Diabetic retinopathy. Diabetes Care. 2004;27:2540–2553. doi: 10.2337/diacare.27.10.2540. [DOI] [PubMed] [Google Scholar]
- 35.Ruta L.M., Magliano D.J., Lemesurier R. Prevalence of diabetic retinopathy in type 2 diabetes in developing and developed countries. Diabet Med. 2013;30:387–398. doi: 10.1111/dme.12119. [DOI] [PubMed] [Google Scholar]
- 36.Pantalone K.M., Hobbs T.M., Wells B.J. Clinical characteristics, complications, comorbidities and treatment patterns among patients with type 2 diabetes mellitus in a large integrated health system. BMJ Open Diabetes Res Care. 2015;3:e000093. doi: 10.1136/bmjdrc-2015-000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mohammedi K., Woodward M., Marre M. Comparative effects of microvascular and macrovascular disease on the risk of major outcomes in patients with type 2 diabetes. Cardiovasc Diabetol. 2017;16:95. doi: 10.1186/s12933-017-0574-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sjølie A.K., Klein R., Porta M. Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet. 2008;372:1385–1393. doi: 10.1016/S0140-6736(08)61411-7. [DOI] [PubMed] [Google Scholar]
- 39.Madonna R., Balistreri C.R., Geng Y.J., De Caterina R. Diabetic microangiopathy: pathogenetic insights and novel therapeutic approaches. Vascul Pharmacol. 2017;90:1–7. doi: 10.1016/j.vph.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 40.Vlassara H., Uribarri J. Advanced glycation end products (AGE) and diabetes: cause, effect, or both? Curr Diab Rep. 2014;14(1):453. doi: 10.1007/s11892-013-0453-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nigro C., Leone A., Raciti G.A. Methylglyoxal-glyoxalase 1 balance: the root of vascular damage. Int J Mol Sci. 2017;18:188–202. doi: 10.3390/ijms18010188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manigrasso M.B., Juranek J., Ramasamy R., Schmidt A.M. Unlocking the biology of RAGE in diabetic microvascular complications. Trends Endocrinol Metab. 2014;25:15–22. doi: 10.1016/j.tem.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koulis C., Watson A.M., Gray S.P., Jandeleit-Dahm K.A. Linking RAGE and Nox in diabetic micro- and macrovascular complications. Diabetes Metab. 2015;41:272–281. doi: 10.1016/j.diabet.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Frimat M., Daroux M., Litke R. Kidney, heart and brain: three organs targeted by ageing and glycation. Clin Sci (Lond) 2017;131:1069–1092. doi: 10.1042/CS20160823. [DOI] [PubMed] [Google Scholar]
- 45.Schmidt A.M. 2016 ATVB Plenary Lecture: receptor for advanced glycation endproducts and implications for the pathogenesis an treatment of cardiometabolic disorders: spotlight on the macrophage. Arterioscler Thromb Vasc Biol. 2017;37:613–621. doi: 10.1161/ATVBAHA.117.307263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nenna A., Nappi F., Avtaar Singh S.S. Pharmacologic approaches against advanced glycation end products (AGEs) in diabetic cardiovascular disease. Res Cardiovasc Med. 2015;4:e26949. doi: 10.5812/cardiovascmed.4(2)2015.26949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kass D.A., Shapiro E.P., Kawaguchi M. Improved arterial compliance by a novel advanced glycation end-product crosslink breaker. Circulation. 2001;104:1464–1470. doi: 10.1161/hc3801.097806. [DOI] [PubMed] [Google Scholar]
- 48.Guzik T.J., Mussa S., Gastaldi D. Mechanisms of increased vascular superoxide production in human diabetes mellitus: role of NAD(P)H oxidase and endothelial nitric oxide synthase. Circulation. 2002;105:1656–1662. doi: 10.1161/01.cir.0000012748.58444.08. [DOI] [PubMed] [Google Scholar]
- 49.Adeshara K.A., Diwan A.G., Tupe R.S. Diabetes and complications: cellular signaling pathways, current understanding and targeted therapies. Curr Drug Targets. 2016;17:1309–1328. doi: 10.2174/1389450117666151209124007. [DOI] [PubMed] [Google Scholar]
- 50.Sedeek M., Montezano A.C., Hebert R.L. Oxidative stress, Nox isoforms and complications of diabetes-potential targets for novel therapies. J Cardiovasc Transl Res. 2012;5:509–518. doi: 10.1007/s12265-012-9387-2. [DOI] [PubMed] [Google Scholar]
- 51.Newsholme P., Cruzat V.F., Keane K.N., Carlessi R., de Bittencourt P.I., Jr. Molecular mechanisms of ROS production and oxidative stress in diabetes. Biochem J. 2016;473:4527–4550. doi: 10.1042/BCJ20160503C. [DOI] [PubMed] [Google Scholar]
- 52.Gray S.P., Di Marco E., Okabe J. NADPH oxidase 1 plays a key role in diabetes mellitus accelerated atherosclerosis. Circulation. 2013;127:1888–1902. doi: 10.1161/CIRCULATIONAHA.112.132159. [DOI] [PubMed] [Google Scholar]
- 53.Gray S.P., Di Marco E., Kennedy K. Reactive oxygen species can provide atheroprotection via NOX4-dependent inhibition of inflammation and vascular remodeling. Arterioscler Thromb Vasc Biol. 2016;36:295–307. doi: 10.1161/ATVBAHA.115.307012. [DOI] [PubMed] [Google Scholar]
- 54.Jha J.C., Gray S.P., Barit D. Genetic targeting or pharmacologic inhibition of NADPH oxidase nox4 provides renoprotection in long-term diabetic nephropathy. J Am Soc Nephrol. 2014;25:1237–1254. doi: 10.1681/ASN.2013070810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sedeek M., Gutsol A., Montezano A.C. Renoprotective effects of a novel Nox1/4 inhibitor in a mouse model of Type 2 diabetes. Clin Sci (Lond) 2013;124:191–202. doi: 10.1042/CS20120330. [DOI] [PubMed] [Google Scholar]
- 56.Holterman C.E., Thibodeau J.F., Towaij C. Nephropathy and elevated BP in mice with podocyte-specific NADPH oxidase 5 expression. J Am Soc Nephrol. 2014;25:784–797. doi: 10.1681/ASN.2013040371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jha J.C., Banal C., Okabe J. NADPH oxidase Nox5 accelerates renal injury in diabetic nephropathy. Diabetes. 2017;66:2691–2703. doi: 10.2337/db16-1585. [DOI] [PubMed] [Google Scholar]
- 58.Mooradian A.D. Targeting select cellular stress pathways to prevent hyperglycemia-related complications: shifting the paradigm. Drugs. 2016;76:1081–1091. doi: 10.1007/s40265-016-0609-9. [DOI] [PubMed] [Google Scholar]
- 59.Guzik TJ, Cosentino F. Epigenetics and immunometabolism in diabetes and aging [e-pub ahead of print]. Antiox Redox Signal https://doi.org/10.1089/ars.2017.7299. [DOI] [PMC free article] [PubMed]
- 60.Meissner A., Miro F., Jimenez-Altayo F. Sphingosine-1-phosphate signalling-a key player in the pathogenesis of angiotensin II-induced hypertension. Cardiovasc Res. 2017;113:123–133. doi: 10.1093/cvr/cvw256. [DOI] [PubMed] [Google Scholar]
- 61.Lorenzo C., Hanley A.J., Haffner S.M. Differential white cell count and incident type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetologia. 2014;57:83–92. doi: 10.1007/s00125-013-3080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vacca M., Di Eusanio M., Cariello M. Integrative miRNA and whole-genome analyses of epicardial adipose tissue in patients with coronary atherosclerosis. Cardiovasc Res. 2016;109:228–239. doi: 10.1093/cvr/cvv266. [DOI] [PubMed] [Google Scholar]
- 63.Passacquale G., Di Giosia P., Ferro A. The role of inflammatory biomarkers in developing targeted cardiovascular therapies: lessons from the cardiovascular inflammation reduction trials. Cardiovasc Res. 2016;109:9–23. doi: 10.1093/cvr/cvv227. [DOI] [PubMed] [Google Scholar]
- 64.Donath M.Y. Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat Rev Drug Discov. 2014;13:465–476. doi: 10.1038/nrd4275. [DOI] [PubMed] [Google Scholar]
- 65.Banerjee M., Saxena M. Interleukin-1 (IL-1) family of cytokines: role in type 2 diabetes. Clin Chim Acta. 2012;413:1163–1170. doi: 10.1016/j.cca.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 66.Mishra M., Kumar H., Bajpai S., Singh R.K., Tripathi K. Level of serum IL-12 and its correlation with endothelial dysfunction, insulin resistance, proinflammatory cytokines and lipid profile in newly diagnosed type 2 diabetes. Diabetes Res Clin Pract. 2011;94:255–261. doi: 10.1016/j.diabres.2011.07.037. [DOI] [PubMed] [Google Scholar]
- 67.Guest C.B., Park M.J., Johnson D.R., Freund G.G. The implication of proinflammatory cytokines in type 2 diabetes. Front Biosci. 2008;13:5187–5194. doi: 10.2741/3074. [DOI] [PubMed] [Google Scholar]
- 68.Hasnain S.Z., Borg D.J., Harcourt B.E. Glycemic control in diabetes is restored by therapeutic manipulation of cytokines that regulate beta cell stress. Nat Med. 2014;20:1417–1426. doi: 10.1038/nm.3705. [DOI] [PubMed] [Google Scholar]
- 69.Su S.C., Pei D., Hsieh C.H. Circulating pro-inflammatory cytokines and adiponectin in young men with type 2 diabetes. Acta Diabetol. 2011;48:113–119. doi: 10.1007/s00592-009-0171-y. [DOI] [PubMed] [Google Scholar]
- 70.Nishida K., Otsu K. Inflammation and metabolic cardiomyopathy. Cardiovasc Res. 2017;113:389–398. doi: 10.1093/cvr/cvx012. [DOI] [PubMed] [Google Scholar]
- 71.Frati G., Schirone L., Chimenti I. An overview of the inflammatory signalling mechanisms in the myocardium underlying the development of diabetic cardiomyopathy. Cardiovasc Res. 2017;113:378–388. doi: 10.1093/cvr/cvx011. [DOI] [PubMed] [Google Scholar]
- 72.Nath A.P., Ritchie S.C., Byars S.G. An interaction map of circulating metabolites, immune gene networks, and their genetic regulation. Genome Biol. 2017;18:146. doi: 10.1186/s13059-017-1279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Voight B.F., Kang H.M., Ding J. The metabochip, a custom genotyping array for genetic studies of metabolic, cardiovascular, and anthropometric traits. PLoS Genet. 2012;8:e1002793. doi: 10.1371/journal.pgen.1002793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hotamisligil G.S. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542:177–185. doi: 10.1038/nature21363. [DOI] [PubMed] [Google Scholar]
- 75.Strawbridge R.J., Laumen H., Hamsten A. Effects of genetic loci associated with central obesity on adipocyte lipolysis. PLoS One. 2016;11:e0153990. doi: 10.1371/journal.pone.0153990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nikpay M., Stewart A.F., McPherson R. Partitioning the heritability of coronary artery disease highlights the importance of immune-mediated processes and epigenetic sites associated with transcriptional activity. Cardiovasc Res. 2017;113:973–983. doi: 10.1093/cvr/cvx019. [DOI] [PubMed] [Google Scholar]
- 77.Guzik T.J., Skiba D., Touyz R.M., Harrison D.G. The role of infiltrating immune cells in dysfunctional adipose tissue. Cardiovasc Res. 2017;113:1009–1023. doi: 10.1093/cvr/cvx108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ridker P.M., Everett B.M., Thuren T. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 79.Sloan-Lancaster J., Abu-Raddad E., Polzer J. Double-blind, randomized study evaluating the glycemic and anti-inflammatory effects of subcutaneous LY2189102, a neutralizing IL-1beta antibody, in patients with type 2 diabetes. Diabetes Care. 2013;36:2239–2246. doi: 10.2337/dc12-1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jing Y., Wu F., Li D. Metformin improves obesity-associated inflammation by altering macrophages polarization. Mol Cell Endocrinol. 2018;461:256–264. doi: 10.1016/j.mce.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 81.Yin M.J., Yamamoto Y., Gaynor R.B. The anti-inflammatory agents aspirin and salicylate inhibit the activity of I(kappa)B kinase-beta. Nature. 1998;396:77–80. doi: 10.1038/23948. [DOI] [PubMed] [Google Scholar]
- 82.Baye E., Naderpoor N., Misso M. Treatment with high dose salicylates improves cardiometabolic parameters: meta-analysis of randomized controlled trials. Metabolism. 2017;71:94–106. doi: 10.1016/j.metabol.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 83.Agrawal N.K., Kant S. Targeting inflammation in diabetes: newer therapeutic options. World J Diabetes. 2014;5:697–710. doi: 10.4239/wjd.v5.i5.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Besancon A., Goncalves T., Valette F. Oral histone deacetylase inhibitor synergises with T cell targeted immunotherapy to preserve beta cell metabolic function and induce stable remission of new-onset autoimmune diabetes in NOD mice. Diabetologia. 2018;61:389–398. doi: 10.1007/s00125-017-4459-0. [DOI] [PubMed] [Google Scholar]
- 85.Christensen D.P., Dahllof M., Lundh M. Histone deacetylase (HDAC) inhibition as a novel treatment for diabetes mellitus. Mol Med. 2011;17:378–390. doi: 10.2119/molmed.2011.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gillum M.P., Kotas M.E., Erion D.M. SirT1 regulates adipose tissue inflammation. Diabetes. 2011;60:3235–3245. doi: 10.2337/db11-0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Banerjee J., Nema V., Dhas Y., Mishra N. Role of microRNAs in type 2 diabetes and associated vascular complications. Biochimie. 2017;139:9–19. doi: 10.1016/j.biochi.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 88.Ferrannini E., DeFronzo R.A. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J. 2015;36:2288–2296. doi: 10.1093/eurheartj/ehv239. [DOI] [PubMed] [Google Scholar]
- 89.Adler A.I., Stratton I.M., Neil H.A. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:706–713. [PMC free article] [PubMed] [Google Scholar]
- 91.Zinman B., Wanner C., Lachin J.M. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 92.Marso S.P., Daniels G.H., Brown-Frandsen K. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–322. doi: 10.1056/NEJMoa1603827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Steven S., Taylor R. Restoring normoglycaemia by use of a very low calorie diet in long- and short-duration Type 2 diabetes. Diabet Med. 2015;32:1149–1155. doi: 10.1111/dme.12722. [DOI] [PubMed] [Google Scholar]
- 94.Mingrone G., Panunzi S., De Gaetano A. Bariatric surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–973. doi: 10.1016/S0140-6736(15)00075-6. [DOI] [PubMed] [Google Scholar]
- 95.Steven S., Hollingsworth K.G., Small P.K. Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes. Diabetes Care. 2016;39:158–165. doi: 10.2337/dc15-0750. [DOI] [PubMed] [Google Scholar]
- 96.Rena G., Hardie D.G., Pearson E.R. The mechanisms of action of metformin. Diabetologia. 2017;60:1577–1585. doi: 10.1007/s00125-017-4342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.de Jager J., Kooy A., Schalkwijk C. Long-term effects of metformin on endothelial function in type 2 diabetes: a randomized controlled trial. J Intern Med. 2014;275:59–70. doi: 10.1111/joim.12128. [DOI] [PubMed] [Google Scholar]
- 98.de Jager J., Kooy A., Lehert P. Effects of short-term treatment with metformin on markers of endothelial function and inflammatory activity in type 2 diabetes mellitus: a randomized, placebo-controlled trial. J Intern Med. 2005;257:100–109. doi: 10.1111/j.1365-2796.2004.01420.x. [DOI] [PubMed] [Google Scholar]
- 99.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 100.Libby P., Plutzky J. Inflammation in diabetes mellitus: role of peroxisome proliferator-activated receptor-alpha and peroxisome proliferator-activated receptor-gamma agonists. Am J Cardiol. 2007;99(4A):27B–40B. doi: 10.1016/j.amjcard.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 101.Spencer M., Yang L., Adu A. Pioglitazone treatment reduces adipose tissue inflammation through reduction of mast cell and macrophage number and by improving vascularity. PLoS One. 2014;9:e102190. doi: 10.1371/journal.pone.0102190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dormandy J.A., Charbonnel B., Eckland D.J. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366:1279–1289. doi: 10.1016/S0140-6736(05)67528-9. [DOI] [PubMed] [Google Scholar]
- 103.Petrie J.R. The cardiovascular safety of incretin-based therapies: a review of the evidence. Cardiovasc Diabetol. 2013;12:130. doi: 10.1186/1475-2840-12-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Drucker D.J. The cardiovascular biology of glucagon-like peptide-1. Cell Metab. 2016;24:15–30. doi: 10.1016/j.cmet.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 105.von Scholten B.J., Persson F., Rosenlund S. Effects of liraglutide on cardiovascular risk biomarkers in patients with type 2 diabetes and albuminuria: a sub-analysis of a randomized, placebo-controlled, double-blind, crossover trial. Diabetes Obes Metab. 2017;19:901–905. doi: 10.1111/dom.12884. [DOI] [PubMed] [Google Scholar]
- 106.Ferrannini E. Sodium-glucose co-transporters and their inhibition: clinical physiology. Cell Metab. 2017;26:27–38. doi: 10.1016/j.cmet.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 107.Ferrannini E., Mark M., Mayoux E. CV protection in the EMPA-REG OUTCOME trial: a “thrifty substrate” hypothesis. Diabetes Care. 2016;39:1108–1114. doi: 10.2337/dc16-0330. [DOI] [PubMed] [Google Scholar]
- 108.Steven S., Oelze M., Hanf A. The SGLT2 inhibitor empagliflozin improves the primary diabetic complications in ZDF rats. Redox Biol. 2017;13:370–385. doi: 10.1016/j.redox.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mannucci E., Dicembrini I., Lauria A., Pozzilli P. Is glucose control important for prevention of cardiovascular disease in diabetes? Diabetes Care. 2013;36(suppl 2):S259–S263. doi: 10.2337/dcS13-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cameron A.C., Lang N.N., Touyz R.M. Drug treatment of hypertension: focus on vascular health. Drugs. 2016;76:1529–1550. doi: 10.1007/s40265-016-0642-8. [DOI] [PubMed] [Google Scholar]
- 111.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [e-pub ahead of print]. J Am Coll Cardiol https://doi.org/10.1016/j.jacc.2017.11.006. [DOI] [PubMed]
- 112.Leung A.A., Daskalopoulou S.S., Dasgupta K. Hypertension Canada's 2017 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. Can J Cardiol. 2017;33:557–576. doi: 10.1016/j.cjca.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 113.Yonchuk J.G., Foley J.P., Bolognese B.J. Characterization of the potent, selective Nrf2 activator, 3-(pyridin-3-ylsulfonyl)-5-(trifluoromethyl)-2h-chromen-2-one, in cellular and in vivo models of pulmonary oxidative stress. J Pharmacol Exp Ther. 2017;363:114–125. doi: 10.1124/jpet.117.241794. [DOI] [PubMed] [Google Scholar]
- 114.Sharma A., Rizky L., Stefanovic N. The nuclear factor (erythroid-derived 2)-like 2 (Nrf2) activator dh404 protects against diabetes-induced endothelial dysfunction. Cardiovasc Diabetol. 2017;16:33. doi: 10.1186/s12933-017-0513-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhuge F., Ni Y., Nagashimada M. DPP-4 inhibition by linagliptin attenuates obesity-related inflammation and insulin resistance by regulating M1/M2 macrophage polarization. Diabetes. 2016;65:2966–2979. doi: 10.2337/db16-0317. [DOI] [PubMed] [Google Scholar]
- 116.Khan S.S., Quaggin S.E. Therapies on the horizon for diabetic kidney disease. Curr Diab Rep. 2015;15:111. doi: 10.1007/s11892-015-0685-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lewis D.R., Petersen L.K., York A.W. Nanotherapeutics for inhibition of atherogenesis and modulation of inflammation in atherosclerotic plaques. Cardiovasc Res. 2016;109:283–293. doi: 10.1093/cvr/cvv237. [DOI] [PMC free article] [PubMed] [Google Scholar]