Abstract
Purpose of Review
Laser lithotripsy is increasingly used worldwide and is a continuously evolving field with new and extensive research being published every year.
Recent Findings
Variable pulse length Ho:YAG lithotripters allow new lithotripsy parameters to be manipulated, and there is an effort to integrate new technologies into lithotripters. Pulsed thulium lasers seem to be a viable alternative to holmium lasers. The performance of similar laser fibers varies from manufacturer to manufacturer. Special laser fibers and “cleaving only” fiber tip preparation can be beneficial for the lithotripsy procedure. Different laser settings and the surgical technique employed can have significant impact on the success of laser lithotripsy. When safely done, complications of laser lithotripsy are rare and concern the endoscopic nature of procedure, not the technology itself, making laser lithotripsy one of the safest tools in urology.
Summary
Laser lithotripsy has had several new developments and more insight has been gained in recent years with many more advances expected in the future.
Keywords: Laser lithotripsy, Endourology, Pulsed thulium lasers
Introduction
This year is the 50th birthday when lasers first made their debut in urology [1], as well as the 30th birthday when urinary laser lithotripsy began establishing itself as a method of urinary stone treatment [2, 3]. Similar to most technological advancements, laser lithotripsy has also advanced with ongoing new developments. We therefore review the latest advances in laser lithotripsy to keep up to date with them.
Material and Methods
A PubMed search was performed (December 2017) for papers including the terms “laser(s)” or “holmium” in association with any of the following terms “lithotripsy,” “lithiasis,” “stone(s),” “calculus,” “calculi,” “lithotripter(s),” “lithotrite(s),” “fiber(s),” “(endo)urology,” (endo)urologic(al),” or “intrarenal” in their title and published between the years 2015 and 2017, as well as 2018, to include already accepted, but not yet published papers. Additionally, the medical sections of ScienceDirect, Wiley, SpringerLink, and Mary Ann Liebert publishers where also searched for abstract presentations published in that time frame that were not indexed on PubMed. Moreover, key papers and other important studies on the subject were also included and cross-referenced, if they were considered noteworthy, despite being published before 2015. The authors adhered to PRISMA guidelines for this review [4]. All relevant data was identified, selected, and has been summarized below.
Bibliographic Search Results
The PubMed search returned 1255 articles. Most of these articles (845) relate to basic laser research not necessarily related to medicine. They include research of new laser media and fiber production, soliton and quantum research, down to communications, nanotubes, and random bit generators created with lasers, all of them published in journals specialized in the wide-raging field of optics, and hence indexed in PubMed. Other 108 articles relate to the use of lasers in non-urological medical specialties such as ophthalmology, gastroenterology, ENT, vascular and general surgery, interventional radiology, and pneumology, as well as dermatology. The other 302 articles relate to urology-related fields, of which 150 concern the use of lasers in a non-lithotripsy-related setting, such as HoLEP, Greenlight laser, or other laser ablative techniques. Finally, the last 152 articles relate to urological laser lithotripsy. More than half of these papers are about case series, single-surgeon series, and comparisons of laser lithotripsy to other lithotripsy methods or case reports.
The search in the medical sections of ScienceDirect, Wiley, SpringerLink, and Mary Ann Liebert returned 12,454 papers or abstract presentations, 759 of them related to urinary stone treatments, some of them already picked up in the PubMed search. All abstract presentations of the major urology congresses were also reviewed and included [5–16].
The relevant data of the publications and abstracts have been categorized into the following four main groups: laser lithotripters, laser fibers, laser settings and technique, and laser safety and related complications (Table 1).
Table 1.
Summary of the advances or technical aspects of laser lithotripsy, its complications, and their prevention
| Advancement or technical aspect | Benefit | Verdict | |
|---|---|---|---|
| Laser lithotripters | Long pulse length (pulse duration or pulse width) | • Less fiber tip degradation • Less stone retropulsion • Smaller residual fragments • Ideal for “dusting” |
Gradual rise in its use |
| Moses effect (modulated laser pulse) | • More ablative (in vitro) • Less retropulsion |
• No significant difference between lasing and procedural time in vivo • Limited availability (one manufacturer) • Costly |
|
| Burst laser lithotripsy | • Greater ablation volume | • Likely to be used more often • Limited availability (one manufacturer) |
|
| Thulium laser (pulsed) | • More ablative than Ho:YAG • Less retropulsion |
• New technology • Very limited availability • Lack of clinical studies |
|
| Laser fibers | Ball tip fiber | • Easier insertion in deflected scope | • Initial benefit lost after a few seconds with degradation |
| Tip cleaving tools | • All were equivalent | • Simple scissors are equally effective | |
| Leaving fibers coated | • Greater stone ablation • Easier to pass in the scope • Safer than stripped fiber |
• More advantageous than stripped fibers in several categories | |
| Stripping of fibers | • Debatable higher stone ablation | • Significantly less advantages than coated fibers | |
| Laser settings and technique | Fragmentation technique | • Faster ablation of primary stone | • Excellent for bladder or PCNL |
| Dusting technique | • No fragments (dust) • No basketing • Decreased ureteral access sheath use |
• Ablation itself takes more time, compensated by other time gains • Ultra-high-frequency lithotripters further shorten surgical time |
|
| Pop-corning | • Ideal for multiple smaller stone fragments in an enclosed space Avoids endless chase of fragments |
Helpful technique, complementing other lithotripsy methods | |
| Pop-dusting | • Similar to pop-corning, but creating more dust | • Helpful technique, complementing other lithotripsy methods | |
| Complication | Prevention | ||
| Laser safety and related complications | Fever, subcapsular hematoma | • Reduce operative time • Use low-pressure ureterorenoscopy Confirm negative urine culture |
|
| Local thermal damage | • Never close irrigation • Intermittent laser use • Cooled irrigation if necessary |
||
| Eye damage | • Use eye glasses (simple ones will do) • Avoid laser fibers near eyes |
||
| Collateral instrument damage | • Keep fibers coated for better identification and regularly cleave them • Respect the safety distance between scope and laser fiber tip • Avoid passage of fibers through deflected scopes or else use BT fiber or at least a coated fiber |
||
Laser Lithotripters
Laser technology was foreseen in 1917 and has been available and developed for 60 years [1, 17–19]. Most of the (initial) lasers emitted their laser energy in a continuous mode which has not been shown to be suited for lithotripsy [20], besides producing heat that can be harmful. On the contrary, pulsed lasers, e.g., the holmium:yttrium–aluminum–garnet (Ho:YAG) or the frequency-doubled double-pulse neodymium:YAG (FREDDY) laser [21, 22], deliver their energy in packets (pulses) that are suddenly released and very efficient at stone lithotripsy. Nevertheless, there are anecdotal reports of using Greenlight lasers for lithotripsy [23]. The reason for this difference in lithotripsy capabilities between continuous and pulsed lasers can be explained using the electric drill machine analogy: while trying to drill a hole in a wall, a continuous rotating drill is less efficient in perforating that wall and also generates much heat; on the contrary, a similar powered impact or percussion drill machine is much faster and efficient and also produces lower levels of heat. These features, together with its excellent safety profile, established and made the Ho:YAG laser ideal for laser lithotripsy in the last 30 years [2, 24, 25, 26••].
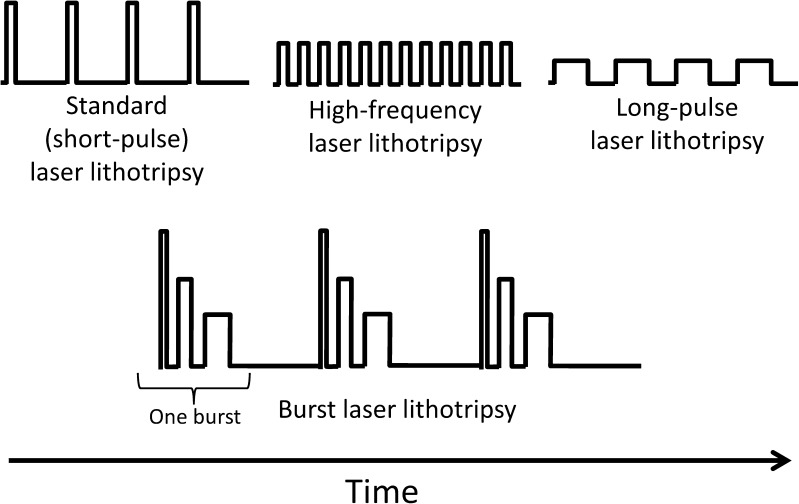
Despite the launch of more powerful and high-frequency Ho:YAG lithotripters over the years [27], they still only allowed the urologist to manipulate two parameters: pulse energy and pulse frequency. It took more than 20 years for holmium laser lithotripters to get their first, true technological upgrade, i.e., the ability to change pulse length, aka pulse duration or pulse width [26••]. Standard Ho:YAG lithotripters were restricted to short pulse lengths, while the newer lithotripters, besides short pulse, were now also capable of doing long-pulse lithotripsy (Fig. 1). Although all other lithotripter parameters (pulse energy, pulse frequency, and consequently total energy delivered) remain unchanged, in short-pulse mode, the energy delivered by a single laser pulse occurs during a short period of time (approximately 300 μs), while in long-pulse mode, that same amount of energy is distributed over a longer period of time (approximately 600 μs or more) [26••]. Pulse length was shown to be inversely correlated with ablation volume, i.e., the shorter the pulse length, the more ablative is the setting. Extreme pulse length comparisons of ultra-short and long-pulse mode (150 vs 800 μs) showed an average 60.6% higher ablation volume difference favoring ultra-short-pulse mode [28]. Despite this apparent lower efficiency, long-pulse mode showed to produce less fiber tip degradation and stone retropulsion [26••, 29, 30, 31•]. However, there is still some controversy in the subject, with some authors considering long pulse to be as ablative as short pulse [32•], or studies showing short-pulse lithotripters producing less retropulsion than more powerful long-pulse lithotripters [33]. There is also the general belief that long pulse produces smaller residual fragments and promotes a more “dusting” technique.
Fig. 1.
Graphic representation of differences between standard (short-pulse) laser lithotripsy, high-frequency laser lithotripsy, long-pulse laser lithotripsy, and burst laser lithotripsy over time
Regardless of the Ho:YAG lithotripsy domination, thulium laser technology, known for its usefulness in prostate ablation using continuous laser emission, and consequently considered unsuited for lithotripsy, has evolved and is now capable of pulsed laser emission. Although its usefulness in lithotripsy was demonstrated back in 2005 [34], only recently has it gained more attention. It has shown to be 2- to 4-fold faster without any significant heat increase and also producing three times less retropulsion, sometimes none at all, in comparison to Ho:YAG lithotripsy [35–37, 38•]. Pulsed thulium lithotripsy looks promising; however, true clinical studies are still lacking.
There is a new technology developed for a high-power 120-W Ho:YAG lithotripter, called the Moses effect. The theory is that this lithotripsy mode emits a modulated laser pulse whose first part divides the water between laser fiber tip and the stone, allowing the second part of the pulse to hit the stone unobstructed, more efficiently and with less retropulsion. However, on a closer look at the official high-speed videos, it reveals to be made of two separate laser pulses with a short time interval between them, rather than a single “modulated” laser pulse. Surgical opinions and in vitro experiments have indeed shown that this Moses effect reduced retropulsion [39, 40] and is significantly more ablative; however, in vivo experiments did not show any significant differences in terms of lasing and procedural times between regular and Moses lithotripsy techniques [40].
Recently, a novel Ho:YAG laser lithotripsy mode has been developed: burst laser lithotripsy (Fig. 1). Each burst consists of three individual laser pulses, the first one being the more energy intense while the last one the least energy intense, having successive increasing pulse lengths and which are emitted in a rapid succession after one another [41•, 42, 43]. The novel burst mode is significantly more ablative, achieving 60% higher ablation volumes than standard lithotripsy at similar power and energy settings [41•]. Possibly, the synchronized continuous variation of pulse energy and pulse length of high-frequency burst pulses, throughout the same lithotripter setting, might improve and speed up laser lithotripsy procedures in the future.
There have been also some efforts to incorporate useful auxiliary technologies into laser lithotripters. These include real-time stone/tissue differentiation using autofluorescence preventing the laser from firing against any structure other than the stone surface [44], or the attempt of in vivo analysis of urinary stone composition [45]. Some manufacturers are also trying to make carefully designed user interfaces, because most lithotripters are not as user friendly [46•].
Laser Fibers
Besides the lithotripter, the laser fiber used also plays a vital role in the lithotripsy procedure. It is already known that larger laser fibers hinder the flow of irrigation fluid, limit the flexibility of instruments, and produce more retropulsion as well as larger stone fragments [26••, 47, 48•, 49, 50]; hence, the urologists prefer for small-diameter laser fibers, especially in flexible ureterorenoscopy. Additionally, there is emerging evidence about significant performance differences (e.g., on flexibility, degradation, ablation capabilities) among laser fiber manufacturers and no single fiber seems to be an ideal performer in every situation [51••, 52••] corroborating older studies on the subject [53•]. These performance differences should also be considered together with the manufacturers’ misinformation and mislabeling issues about laser fiber diameters, which were discussed not so long ago and these issues are far from being settled [48•, 54]. Even small-diameter changes can have a critical impact, because they indirectly affect accessibility, visibility, efficiency, total surgical time, and the lithotripsy procedure as a whole [48•]. On the other hand, pulsed thulium lasers are able to use smaller diameter laser fibers, than the ones used with the Ho:YAG lasers, representing a clear advantage and affecting favorably on the abovementioned aspects [55].
Lately, much attention has been given to ball-shaped tip (BT) laser fibers. BT laser fibers are particularly interesting because of their reduced insertion force in a completely deflected working channel without damaging it [56]. However, those features are lost as soon as laser emission occurs, because of the laser fiber tip degradation, the so called “burn-back” effect. Hence, most of these BT fibers should be only used once for a single, deflected working channel passage and at the very beginning of the surgery, because after several seconds of laser emission, they exhibit exactly the same characteristics as standard laser fibers [57]. Additionally, no better ablation properties where found on these special (and more costly) designed fiber tips in comparison to single-use standard fibers [56, 57]. Regarding reusable fibers, they show exactly the same tip morphology and degradation as new single-use standard fibers, as well as similar performances as long as they are not damaged along their length or at the connector. Although reusable fibers are more expensive than standard single-use fibers, they decrease fiber costs after the third and subsequent uses [57]. Yet other authors have shown that the use of single-use laser fibers can help decrease the overall cost of flexible ureterorenoscopy [58].
Still, laser fiber degradation, fiber fracture with smaller bend diameters or burn-back at its tip, affects every fiber, regardless of its shape or type (single-use or reusable fibers). It has been demonstrated that higher pulse energies, shorter pulse lengths, or harder stone material are more detrimental to laser fibers, in particular to their tips [26••, 29, 59•]. But there are also some conflicting results from other authors claiming that there is a trend for less fiber fracture with higher pulse energies [52••].
Related to these degradation issues is laser fiber tip preparation. This old, but still current practice of laser fiber preparation can be done before and during the procedure (to “renew” the fiber tip) and consists of stripping off the terminal portion of the plastic fiber coating and then cleaving several millimeters off the end of the glassy fiber components using special instruments (e.g., laser fiber stripper, ceramic scissors) [60–62, 63••]. One publication compared several cleaving methods, demonstrating that the “scribe pen” cleaving tool produced the highest average power output. However, these measurements were done without any laser emission, thus without considering any degradation issues over time [64]. Another paper analyzed the influence of stripping and cleaving methods of laser fibers on lithotripsy performance. The authors concluded that coated fibers outperformed stripped fibers; were not exposed to possible initial cladding damage caused by stripping; prevented damage caused by tip cleavage; and avoided cladding or other silica components to break off during lithotripsy as well as being more visible during the treatment. They also concluded that simple cleaving methods such as using a metallic surgical scissor were as good as more costly methods, as long as the fibers remain coated [63••]. Some of these results favoring coated fibers have been confirmed by other researchers [65]. Another advantage of keeping the fibers coated is that most of these fibers are able to pass through all angles of deflections in most scopes, while stripped fibers cannot without being harmful to the scopes’ working channel [66]. However, there is also evidence that initial advantages of certain cleaving methods over another level themselves out and the fibers become quite similar in performance in the first minutes of lithotripsy, because of equal, short-term fiber degradation [65, 67, 68•]. However, even over this topic, there is controversy among researchers, with some advocating against routine cleaving [67], others endorsing fiber tip preparation and renewal after 15 min or 10,000 J of laser emission, which is also important for reusable fibers [63••, 68•, 69], while still others claim that stripped fibers achieve greater stone ablation [65].
There are also other developments that can change the laser fiber as we know it. One of them is a miniaturized integrated thulium laser fiber and a stone basket. This device may minimize stone retropulsion, increase scope flexibility, allow higher saline irrigation rates through the working channel, reduce material degradation compared with separate fiber and basket manipulation, and reduce laser-induced nitinol wire damage [70]. The other is a more peculiar development: a fiber optic muzzle brake tip made of stainless steel to apply on thulium laser fibers. Similar to muzzle brakes used in rifles and artillery canons to reduce recoil and redirect propellant gases sideways, this laser fiber muzzle brake not only reduces stone retropulsion by 85%, but also provides minimal fiber degradation and an efficient stone ablation [71].
Laser Settings and Technique
Most experts agree that fragmentation settings with higher pulse energies (> 0.5 J) and shorter pulse lengths have advantages, because they speed up the process of breaking up a large stone into smaller pieces. This can be speedy and useful in the bladder or in kidney stones with a large caliber percutaneous approach. However in ureterorenoscopy, this technique may also turn a single large problem into multiple, more time-consuming smaller problems. This is the reason why many urologists prefer to use a “dusting” technique [72–74]. Although dusting settings with low pulse energies (0.2–0.5 J), higher frequencies, and preferably longer pulse lengths ablate less stone material per unit time, it has several advantages: it decreases the use of ureteral access sheaths and therefore reduces potential ureteral trauma [75••, 76]; basket-associated complications are reduced because dust is naturally eliminated [73]; in the long run, it even reduces operative time by 20–40% by avoiding lengthy extraction procedures [73, 75••, 76]. Besides using low pulse energies for dusting, some authors also recommend keeping the laser fiber slightly away from the stone to “defocus” it and produce smaller fragments [75••]. With the recent arrival of high-powered high-frequency long-pulse Ho:YAG lithotripters, ultra-high pulse frequencies are available (up to 80 Hz), further speeding up the dusting lithotripsy procedure [77–79]. Despite all this evidence, according to an international survey, most urologists still use lithotripter settings around 10 Hz and 0.8 J [80]. However, it must also be acknowledged that if the dust does not evacuate spontaneously, stone-free rates in patients can be lower and this increases the risk of future stone-related events [75••, 81].
All the aforementioned settings and modalities relate to contact lithotripsy, which constitutes the first (and usually the only) stage of the lithotripsy procedure. However, when numerous smaller fragments result, which are still big enough to need treatment, but too time-consuming to chase individually, a second stage (completion) non-contact lithotripsy can be performed. The aim of non-contact lithotripsy is to pulverize these fragments and allow their spontaneous passage [82], preferably in a smaller and enclosed space such as a calix to increase the efficiency [83]. Two different techniques can be employed. One is the “pop-corn” technique, whose optimal settings have been confirmed by using a higher pulse energy (≈ 1.5 J), usually associated with a high-frequency (20–40 Hz), long-pulse mode, as well as a small-diameter laser fiber, and taking as much time as possible to produce clinically insignificant fragments [84•]. The other one is the “pop-dusting” technique, quite similar to the pop-corn technique but using a lower pulse energy (0.5 J), resulting in finer fragments without compromising fiber tip burn-back [82].
However, fragment size may not only be related to laser lithotripter settings, but also on the surgical technique employed, i.e., how the surgeon approaches the stone with the laser, i.e., “perforating,” “chipping,” “cutting into pieces” vs working uniformly and tangentially on the surface, by “dancing” or “painting” the stone with the laser and taking care not to break off large fragments from the main stone [26••, 75••, 85, 86]. Thus, even the best dusting setting, when used improperly, can produce large stone fragments.
Concerning settings and technique, it is the authors’ opinion that one should use lower pulse energy levels, with long pulse length (thus achieving smaller residual fragments and minimizing retropulsion, as well as reducing laser fiber degradation), and very high frequencies as technically possible to “go faster” and speed up the procedure. The laser fiber should be moved uniformly over the stone, without chipping or fragmenting the stone. The surgeon should be aware of the resulting fragment size, and if necessary adjust the settings, or even use a pop-corn technique to finish the procedure.
Laser Safety and Related Complications
Ho:YAG laser lithotripsy is an efficient and safe technology for the treatment of urinary stones in almost any patient group, ranging from young children to adults and older patients, pregnant women to spinal cord injury patients, from solitary to allograft kidneys, or patients on certain medications and anticoagulants. Its safety profile has been largely demonstrated and still is in countless and recent safety-oriented studies [87•, 88•, 89, 90•, 91–98, 99•, 100, 101•]. Yet there are still some direct and indirect complications and safety concerns about laser lithotripsy, which have been recently researched.
The most frequent complication in laser lithotripsy is fever [102]. Renal backflow and infected urine fluid reabsorption can be one of the causes, and curiously retrograde intrarenal surgery (RIRS) has higher total fluid absorption than percutaneous nephrolithotomy (PCNL) procedures [103], which makes sense considering the enclosed space in RIRS. The presence of a preoperative stent, obstructive pyelonephritis, a positive preoperative bladder urine culture result, female gender, increased stone size, or lengthy operating time are significantly associated with postoperative fever and risk of sepsis [104, 105]. Spinal cord injury or patients with severe motor disabilities are in particular risk of sepsis (27%) after laser lithotripsy [106].
Bleeding is also a concern and several cases of renal subcapsular hematomas have been reported with Ho:YAG laser lithotripsy [102, 107, 108]. Yet it is questionable that these infections or bleeding complications were exclusively related to the Ho:YAG technology itself, because they are also known to occur in ureterorenoscopy without the use of laser lithotripsy [109]. On the other hand, one should bear in mind that there are at least three reported mortalities resulting from ureteral perforation and retroperitoneal bleeding using the Ho:YAG laser, although it is not specified if it was during a lithotripsy or endoureterotomy procedure [110]. In any case, the risk of subcapsular hematoma can be reduced by avoiding prolonged endoscopy and performing ureterorenoscopy under low pressure [111, 112], and the importance of always having a negative urine culture before any RIRS cannot be overemphasized.
Lately, attention has been given to local temperature rise at the site of laser lithotripsy, i.e., in the ureter or the kidney. Multiple authors and papers have confirmed that holmium laser emission in long bursts, even at lower power settings, does indeed rise fluid temperatures (up to 70 °C or more), particularly when irrigation is closed, potentially causing tissue injury [113•, 114•, 115•]. Since thulium laser has comparable absorption properties in water, it also shows similar temperature rises as the Ho:YAG laser [116, 117]. Considering that only 4.18 J of energy is needed to rise the temperature of 1 mL of water by 1 °C [118], and that holmium laser energy is highly absorbed by water, it comes as no surprise, that even with modest lithotripter settings providing dozens of Joules per second to a few milliliters of water enclosed in a very small space (e.g., a segment of the ureter or a renal calyx), the temperature is able to rise considerably and literally cook the surrounding tissues. Therefore, an endourologist should be aware of the risk of temperature rise during laser emission and implement a variety of techniques (higher irrigation flow rates, intermittent laser activation, and potentially cooled irrigation fluid) to control and mitigate thermal effects during laser lithotripsy and avoid unnecessary damage of the surrounding tissues [113•, 114•, 119].
In summary, considering the aforementioned issues, and with very few exceptions, patient-related safety and complications are probably less dependent on the laser technology itself, but dependent on multiple other factors relating to the procedure, e.g., the surgeon’s skill, the use of ureteral access sheaths, basketing instead of dusting, good intraoperative visibility, and operative time [63••, 73, 75••, 110].
But laser safety is not only about patient-related problems, but also concerns the safety of urologists and other staff in the operating room (OR). Eye injury is one of the main concerns when lasers are used; however, it was demonstrated that Ho:YAG lasers can only cause damage when all the following three conditions are met: high-energy laser settings, at very close distances (0–5 cm), and with no eye protection. Simple eyeglasses are equally effective in preventing laser damage as special laser safety glasses, and should an eye burn still occur, it would be restricted to the cornea [120••]. Not surprisingly, no eye injuries were reported so far with the use of Ho:YAG lasers [110]. Considering all reported adverse events with Ho:YAG lasers, if there is harm, it is to the patient or the surgeon (minor skin burns for the latter), but never to non-medical operators [110].
Radiation exposure for the patient as for the surgeon is a familiar problem in laser lithotripsy. Studies have confirmed the positive correlation between stone burden and radiation exposure during laser lithotripsy. Hence, clinicians should consider strategies to reduce the total radiation exposure, such as using pulsed instead of continuous fluoroscopy [121], although there are even defenders of using no fluoroscopy at all [122].
Material-related safety is also an issue, because laser energy can be harmful to other instruments, in particular to the delicate scopes used in endourology. To prevent accidental material damage, several strategies are recommended: to keep the laser fiber tip coated for better identification and to know its whereabouts [63••] and at a reasonable safety distance from the optical end of the scope (approximately one fourth of the endoscope field of view) [123••]; to regularly cleave the fiber tip to prevent back burns and retrograde laser emission [69]; to avoid passing a laser fiber through a deflected ureterorenoscope, and if inevitable, it is better to opt for an unused BT fiber or a recently cleaved and coated (not stripped) laser fiber [57, 124]; to avoid narrowed scope deflections with active laser fibers, and if inevitable, to change to smaller core fibers since they are less likely to fracture [59•]; and to avoid laser emission adjacent to auxiliary instrument components such as guidewires or basket tip parts since they are susceptible to breakages [125, 126].
Conclusions
After 20 years of few technological developments, with the arrival of variable pulse length Ho:YAG lithotripters, new lithotripsy parameters can be manipulated to their advantage by the endourologist. There is an effort to integrate new lithotripsy modes and helpful technologies into lithotripters, including the use of pulsed thulium lasers instead of the Ho:YAG. Laser fibers from several manufactures perform significantly differently from one another and BT laser fibers have some short-lived advantages that can also be obtained with standard laser fibers. Laser fiber stripping is always detrimental for their performance and fiber cleavage can be done securely with simple metallic scissors. There are several settings for contact and non-contact laser lithotripsy, each with their own advantages and disadvantages, but the importance of the procedural movements of the laser fiber by the surgeon to deliver the laser energy to the stone should not be neglected. There are some reported complications with laser lithotripsy, but most of them are procedure-related and not with the laser technology itself. The remaining few safety issues can be prudently avoided, making laser lithotripters one of the safest instruments urologists can use in any patient group.
Compliance with Ethical Standards
Conflict of Interest
Peter Kronenberg and Bhaskar Somani each declares no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Endourology
Contributor Information
Peter Kronenberg, Email: peterkronenberg@gmail.com.
Bhaskar Somani, Email: b.k.somani@soton.ac.uk.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Parsons RL, Campbell JL, Thomley MW. Carcinoma of the penis treated by the ruby laser. J Urol. 1968;100(1):38–39. doi: 10.1016/s0022-5347(17)62468-6. [DOI] [PubMed] [Google Scholar]
- 2.Coptcoat MJ, Ison KT, Watson G, Wickham JE. Lasertripsy for ureteric stones in 120 cases: lessons learned. Br J Urol. 1988;61(6):487–489. doi: 10.1111/j.1464-410x.1988.tb05085.x. [DOI] [PubMed] [Google Scholar]
- 3.Hofmann R, Hartung R. Use of pulsed Nd:YAG laser in the ureter. Urol Clin North Am. 1988;15(3):369–375. [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.EAU15 – 30th Annual Congress of the European Association of Urology Abstracts. Eur Urol Suppl. 2015;14(2):e1-eV77.
- 6.EAU16 – 31st Annual Congress of the European Association of Urology Abstracts. Eur Urol Suppl. 2016;15(3):e1-eV79.
- 7.Abstracts EAU17 – 32nd Annual EAU Congress. Eur Urol Suppl. 2017;16(3):e1-e2160.
- 8.2015 Annual Meeting Program Abstracts. J Urol. 2015; 193(4):e1-e1118.
- 9.2016 Annual Meeting Program Abstracts. J Urol. 2016;195(4):e1-e1192.
- 10.2017 Annual Meeting Program Abstracts. J Urol. 2017;197(4):1–1376.
- 11.SIU 2015 Abstracts. World J Urol 2015;33(Suppl 1):1–256. 10.1007/s00345-015-1684-3. [DOI] [PMC free article] [PubMed]
- 12.Abstract SIU 2016 Buenos Aires, Argentina book. World J Urol. 2016; 34(Suppl 1):1–248. 10.1007/s00345-016-1931-2. [DOI] [PubMed]
- 13.Abstracts from the 37th Congress of the Société Internationale d'Urologie, Centro de Congressos de Lisboa, October 19-22, 2017. World J Urol. 2017;35(Suppl 1):1–360. 10.1007/s00345-017-2090-9. [DOI] [PMC free article] [PubMed]
- 14.Scientific Program of 33rd World Congress of Endourology & SWL Program Book. J Endourol. 2015;29(Suppl 1):P1-A457. 10.1089/end.2015.29003.abstracts. [DOI] [PubMed]
- 15.Scientific Program of 34th World Congress of Endourology & SWL Program Book and Abstracts. J Endourol. 2016;30(S2):P1-A464. 10.1089/end.2016.29020.abstracts. [DOI] [PubMed]
- 16.Scientific Program of 35th World Congress of Endourology Program Book and Abstracts. J Endourol. 2017;31(S2):P1-A474. 10.1089/end.2017.29029.abstracts. [DOI] [PubMed]
- 17.Einstein A. Zur Quantentheorie der Strahlung. Phys Z. 1917;18:121–128. [Google Scholar]
- 18.Schawlow AL, Townes CH. Infrared and optical masers. Phys Rev. 1958;112(6):1940–1949. [Google Scholar]
- 19.Maiman TH. Stimulated optical radiation in ruby. Nature. 1960;187(4736):493–494. [Google Scholar]
- 20.Pal D, Ghosh A, Sen R, Pal A. Continuous-wave and quasi-continuous wave thulium-doped all-fiber laser: implementation on kidney stone fragmentations. Appl Opt. 2016;55(23):6151–6155. doi: 10.1364/AO.55.006151. [DOI] [PubMed] [Google Scholar]
- 21.Zörcher T, Hochberger J, Schrott KM, Kühn R, Schafhauser W. In vitro study concerning the efficiency of the frequency-doubled double-pulse neodymium:YAG laser (FREDDY) for lithotripsy of calculi in the urinary tract. Lasers Surg Med. 1999;25(1):38–42. doi: 10.1002/(sici)1096-9101(1999)25:1<38::aid-lsm5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 22.Banús Gassol JM. Física del láser. Arch Esp Urol. 2008;61(9):961–964. doi: 10.4321/s0004-06142008000900003. [DOI] [PubMed] [Google Scholar]
- 23.Ow D, Bolton D, Lawrentschuk N, VID.38 Photovaporization of calculi as an alternative approach for vesical urolithiasis. World J Urol. 2015;33(Suppl 1):102–256. [Google Scholar]
- 24.Floratos DL, de la Rosette JJ. Lasers in urology. BJU Int. 1999;84(2):204–211. doi: 10.1046/j.1464-410x.1999.00163.x. [DOI] [PubMed] [Google Scholar]
- 25.Vicente Rodríguez JJ, Fernández González I, Hernández Fernández C, Santos García-Vaquero I, Rosales Bordes A. Láser en Urología. Actas Urol Esp. 2006;30:879–895. doi: 10.1016/s0210-4806(06)73554-9. [DOI] [PubMed] [Google Scholar]
- 26.Kronenberg P, Traxer O. Update on lasers in urology 2014: current assessment on holmium:yttrium-aluminum-garnet (Ho:YAG) laser lithotripter settings and laser fibers. World J Urol. 2015;33(4):463–469. doi: 10.1007/s00345-014-1395-1. [DOI] [PubMed] [Google Scholar]
- 27.Lumenis. VersaPulse PowerSuite Brochure; PB-1106750 Rev. B; 2013 [cited 2014 Jun 19]. Available from: URL:http://www.surgical.lumenis.com/pdf/PB-1106750_rB_VPPS_P20v_br_LowRes%20(1).pdf.
- 28.Kronenberg P, Traxer O. PI-05 ultra-short, short, medium and long-pulse laser lithotripsy performance. J Urol. 2016;195(4, Supplement):e410. [Google Scholar]
- 29.Wollin DA, Ackerman A, Yang C, Chen T, Simmons WN, Preminger GM, Lipkin ME. Variable pulse duration from a new holmium: YAG laser: the effect on stone comminution, fiber tip degradation, and retropulsion in a dusting model. Urology. 2017;103:47–51. doi: 10.1016/j.urology.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Bell JR, Penniston KL, Nakada SY. In vitro comparison of holmium lasers: evidence for shorter fragmentation time and decreased retropulsion using a modern variable-pulse laser. Urology. 2017;107:37–42. doi: 10.1016/j.urology.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 31.Sroka R, Pongratz T, Scheib G, Khoder W, Stief CG, Herrmann T, et al. Impact of pulse duration on Ho: YAG laser lithotripsy: treatment aspects on the single-pulse level. World J Urol. 2015;33(4):479–485. doi: 10.1007/s00345-015-1504-9. [DOI] [PubMed] [Google Scholar]
- 32.Bader MJ, Pongratz T, Khoder W, Stief CG, Herrmann T, Nagele U, et al. Impact of pulse duration on Ho: YAG laser lithotripsy: fragmentation and dusting performance. World J Urol. 2015;33(4):471–477. doi: 10.1007/s00345-014-1429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bell JR, Penniston KL, Nakada SY. In vitro comparison of stone fragmentation when using various settings with modern variable pulse holmium lasers. J Endourol. 2017;31(10):1067–1072. doi: 10.1089/end.2017.0351. [DOI] [PubMed] [Google Scholar]
- 34.Fried NM. Thulium fiber laser lithotripsy: an in vitro analysis of stone fragmentation using a modulated 110-watt thulium fiber laser at 1.94 microm. Lasers Surg Med. 2005;37(1):53–58. doi: 10.1002/lsm.20196. [DOI] [PubMed] [Google Scholar]
- 35.Platonova DV, Zamyatina VA, Dymov AM, Kovalenko AA, Vinarov AZ, Minaev VP. Laser lithotripsy. Urologiia (Moscow, Russia : 1999). 2015;(6):116–21. [PubMed]
- 36.Kamal W, Kallidonis P, Koukiou G, Amanatides L, Panagopoulos V, Ntasiotis P, Liatsikos E. Stone retropulsion with Ho: YAG and Tm: YAG lasers: a clinical practice-oriented experimental study. J Endourol. 2016;30(11):1145–1149. doi: 10.1089/end.2016.0212. [DOI] [PubMed] [Google Scholar]
- 37.Dymov A, Glybochko P, Alyaev Y, Vinarov A, Altshuler G, Zamyatina V, Sorokin N, Enikeev D, Lekarev V, Proskura A, Koshkarev A. V11-11 thulium lithotripsy: from experiment to clinical practice. J Urol. 2017;197((4):e1285. [Google Scholar]
- 38.Glybochko P, Altshuler G, Vinarov A, Rapoport L, Enikeev M, Grigoriev N, et al. 226 Comparison between the possibilities of holmium and thulium laser in lithotripsy in vitro. Eur Urol Suppl. 2017;16(3):e391–e392. [Google Scholar]
- 39.Mullerad M, Aguinaga JRA, Aro T, Kastin A, Goldin O, Kravtsov A, Assadi A, Badaan S, Amiel GE. Initial clinical experience with a modulated holmium laser pulse-Moses technology: does it enhance laser lithotripsy efficacy? Rambam Maimonides Med J. 2017;8(4):e0038. doi: 10.5041/RMMJ.10315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elhilali MM, Badaan S, Ibrahim A, Andonian S. Use of the Moses technology to improve holmium laser lithotripsy outcomes: a preclinical study. J Endourol. 2017;31(6):598–604. doi: 10.1089/end.2017.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kronenberg P, Traxer O. MP22-13 burst laser lithotripsy—a novel lithotripsy mode. J Urol. 2016;195(4, Supplement):e258. [Google Scholar]
- 42.Kronenberg P, Traxer O. Lithotripsie par laser en salves: Un nouveau mode de lithotripsie. Prog Urol. 2016;26(13):697–698. [Google Scholar]
- 43.CoolTouch - Syneron Candela. StoneLight 30 brochure: laser therapy. 2016.
- 44.Lange B, Jocham D, Brinkmann R, Cordes J. Stone/tissue differentiation for holmium laser lithotripsy using autofluorescence: clinical proof of concept study. Lasers Surg Med. 2017;49(4):361–365. doi: 10.1002/lsm.22611. [DOI] [PubMed] [Google Scholar]
- 45.Miernik A, Eilers Y, Nuese C, Bolwien C, Lambrecht A, Hesse A, Rassweiler JJ, Schlager D, Wilhelm K, Wetterauer U, Schoenthaler M. Is in vivo analysis of urinary stone composition feasible? Evaluation of an experimental setup of a Raman system coupled to commercial lithotripsy laser fibers. World J Urol. 2015;33(10):1593–1599. doi: 10.1007/s00345-014-1477-0. [DOI] [PubMed] [Google Scholar]
- 46.Dragos LB, Proietti S, Buttice S, Sener E, Tefik T, Emiliani E, et al. 82 - Lasers in flexible ureterorenoscopy. Are they user friendly enough? Eur Urol Suppl. 2016;15(11):e1449–e1450. [Google Scholar]
- 47.Kronenberg P, Traxer O. V1718 laser fibers, pulse energy and retropulsion—what we can see and what we can’t. J Urol. 2013;189((4):e707. [Google Scholar]
- 48.Kronenberg P, Traxer O. The truth about laser fiber diameters. Urology. 2014;84(6):1301–1307. doi: 10.1016/j.urology.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 49.Pasqui F, Dubosq F, Tchala K, Tligui M, Gattegno B, Thibault P, Traxer O. Impact on active scope deflection and irrigation flow of all endoscopic working tools during flexible ureteroscopy. Eur Urol. 2004;45(1):58–64. doi: 10.1016/j.eururo.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 50.Spore SS, Teichman JM, Corbin NS, Champion PC, Williamson EA, Glickman RD. Holmium: YAG lithotripsy: optimal power settings. J Endourol. 1999;13(8):559–566. doi: 10.1089/end.1999.13.559. [DOI] [PubMed] [Google Scholar]
- 51.Akar EC, Knudsen BE. Evaluation of 16 new holmium:yttrium-aluminum-garnet laser optical fibers for ureteroscopy. Urology. 2015;86(2):230–235. doi: 10.1016/j.urology.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 52.Lusch A, Heidari E, Okhunov Z, Osann K, Landman J. Evaluation of contemporary holmium laser fibers for performance characteristics. J Endourol. 2016;30(5):567–573. doi: 10.1089/end.2015.0600. [DOI] [PubMed] [Google Scholar]
- 53.Mues AC, Teichman JMH, Knudsen BE. Evaluation of 24 holmium:YAG laser optical fibers for flexible ureteroscopy. J Urol. 2009;182(1):348–354. doi: 10.1016/j.juro.2009.02.112. [DOI] [PubMed] [Google Scholar]
- 54.European Association of Urology. Information conveyed to urologists regarding laser fiber diameter is incorrect. ScienceDaily 2013 Sep 17 [cited 2014 Jul 17]. Available from: URL:http://www.sciencedaily.com/releases/2013/09/130917124821.htm.
- 55.Wilson CR, Hardy LA, Kennedy JD, Irby PB, Fried NM. Miniature ball-tip optical fibers for use in thulium fiber laser ablation of kidney stones. J Biomed Opt. 2016;21(1):18003. doi: 10.1117/1.JBO.21.1.018003. [DOI] [PubMed] [Google Scholar]
- 56.Shin RH, Lautz JM, Cabrera FJ, Shami CJ, Goldsmith ZG, Kuntz NJ, Kaplan AG, Neisius A, Simmons WN, Preminger GM, Lipkin ME. Evaluation of novel ball-tip holmium laser Fiber: impact on ureteroscope performance and fragmentation efficiency. J Endourol. 2016;30(2):189–194. doi: 10.1089/end.2015.0300. [DOI] [PubMed] [Google Scholar]
- 57.Kronenberg P, Traxer O. Lithotripsy performance of specially designed laser fiber tips. J Urol. 2016;195(5):1606–1612. doi: 10.1016/j.juro.2015.10.135. [DOI] [PubMed] [Google Scholar]
- 58.Chapman RA, Somani BK, Robertson A, Healy S, Kata SG. Decreasing cost of flexible ureterorenoscopy: single-use laser fiber cost analysis. Urology. 2014;83(5):1003–1005. doi: 10.1016/j.urology.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 59.Haddad M, Emiliani E, Rouchausse Y, Coste F, Doizi S, Berthe L, et al. Impact of the curve diameter and laser settings on laser fiber fracture. J Endourol. 2017;31(9):918–921. doi: 10.1089/end.2017.0006. [DOI] [PubMed] [Google Scholar]
- 60.Bagley DH, Das A. Endourologic use of the holmium laser. Teton NewMedia: Jackson; 2001. [Google Scholar]
- 61.Mues AC, Teichman JMH, Knudsen BE. Quantification of holmium:yttrium aluminum garnet optical tip degradation. J Endourol. 2009;23(9):1425–1428. doi: 10.1089/end.2009.0384. [DOI] [PubMed] [Google Scholar]
- 62.Sung C, Singh H, Schwartz M, Mirabile G, Hruby GW, Ryan CD, Landman J. Evaluation of efficacy of novel optically activated digital endoscope protection system against laser energy damage. Urology. 2008;72(1):57–60. doi: 10.1016/j.urology.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 63.Kronenberg P, Traxer O. Are we all doing it wrong? Influence of stripping and cleaving methods of laser fibers on laser lithotripsy performance. J Urol. 2015;193(3):1030–1035. doi: 10.1016/j.juro.2014.07.110. [DOI] [PubMed] [Google Scholar]
- 64.Vassantachart JM, Lightfoot M, Yeo A, Maldonado J, Li R, Alsyouf M, Martin J, Lee M, Olgin G, Baldwin DD. Laser fiber cleaving techniques: effects on tip morphology and power output. J Endourol. 2015;29(1):84–89. doi: 10.1089/end.2014.0175. [DOI] [PubMed] [Google Scholar]
- 65.Ritchie C, Yang P, Peplinski B, Keheila M, Cheriyan S, Abourbih S, Kelln W, Baldwin DD. Jackets off: the impact of laser fiber stripping on power output and stone degradation. J Endourol. 2017;31(8):780–785. doi: 10.1089/end.2017.0160. [DOI] [PubMed] [Google Scholar]
- 66.Baghdadi M, Emiliani E, Talso M, Servián P, Barreiro A, Orosa A, Proietti S, Traxer O. Comparison of laser fiber passage in ureteroscopic maximum deflection and their influence on deflection and irrigation: do we really need the ball tip concept? World J Urol. 2017;35(2):313–318. doi: 10.1007/s00345-016-1873-8. [DOI] [PubMed] [Google Scholar]
- 67.Peplinski B, Faaborg D, Miao E, Alsyouf M, Myklak K, Kelln W, Baldwin DD. The effect of laser fiber cleave technique and lithotripsy time on power output. J Endourol. 2016;30(6):678–684. doi: 10.1089/end.2015.0835. [DOI] [PubMed] [Google Scholar]
- 68.Haddad M, Emiliani E, Rouchausse Y, Coste F, Berthe L, Doizi S, et al. Impact of laser fiber tip cleavage on power output for ureteroscopy and stone treatment. World J Urol. 2017;35(11):1765–1770. doi: 10.1007/s00345-017-2053-1. [DOI] [PubMed] [Google Scholar]
- 69.Haddad M, Emiliani E, Traxer O. Re: The effect of laser fiber cleave technique and lithotripsy time on power output. J Endourol. 2016; 10.1089/end.2016.0492. [DOI] [PubMed]
- 70.Wilson CR, Hutchens TC, Hardy LA, Irby PB, Fried NM. A miniaturized, 1.9F integrated optical fiber and stone basket for use in thulium fiber laser lithotripsy. J Endourol. 2015;29(10):1110–1114. doi: 10.1089/end.2015.0124. [DOI] [PubMed] [Google Scholar]
- 71.Hutchens TC, Gonzalez DA, Irby PB, Fried NM. Fiber optic muzzle brake tip for reducing fiber burnback and stone retropulsion during thulium fiber laser lithotripsy. J Biomed Opt. 2017;22(1):18001. doi: 10.1117/1.JBO.22.1.018001. [DOI] [PubMed] [Google Scholar]
- 72.Wu Z, Gao P, Feng C, Wang L, Mao S, Ding Q, et al. MP-04.10 flexible ureteroscopic stone dusting with holmium: YAG laser for treatment of renal stones. World J Urol. 2016;34(Suppl 1):19. [Google Scholar]
- 73.Gamal W, Mamdouh A. MP28-04 flexible URS holmium laser stone dusting VS fragmentaion for 2 cm single renal stone. J Urol. 2015;193(4):e312–e313. [Google Scholar]
- 74.Singh A, Sabnis R, Ganpule A, Chhabra J, Desai M. MP-04.11 initial experience of using high power holmium laser for dusting of large bulk renal stones by RIRS. World J Urol. 2016;34(Suppl 1):20–248. [Google Scholar]
- 75.•• Matlaga BR, Chew B, Eisner B, Humphreys M, Knudsen B, Krambeck A, et al. Ureteroscopic laser lithotripsy: a review of dusting vs fragmentation with extraction. J Endourol. 2017; 10.1089/end.2017.0641. Key paper on dusting laser lithotripsy and its numerous advantages, as well as focusing on its technique. [DOI] [PubMed]
- 76.Santiago JE, Hollander AB, Soni SD, Link RE, Mayer WA. To dust or not to dust: a systematic review of ureteroscopic laser lithotripsy techniques. Curr Urol Rep. 2017;18(4):32. doi: 10.1007/s11934-017-0677-8. [DOI] [PubMed] [Google Scholar]
- 77.Tracey J, Gagin G, Morhardt D, Hollingsworth J, Ghani K. MP51-07 flexible ureteroscopy and laser lithotripsy for renal stones using ‘pop-dusting’: comparison of outcomes between traditional dusting settings versus ultra-high frequency settings. J Urol. 2016;195(4, Supplement):e683. [Google Scholar]
- 78.Tracey JM, Gagin G, Morhardt D, Hollingsworth JM, Ghani KR. Ureteroscopic high frequency dusting utilizing a 120-watt holmium laser. J Endourol. 2017; 10.1089/end.2017.0220. [DOI] [PubMed]
- 79.Teichman JMH. Editorial comment on: In vitro comparison of stone fragmentation when using various settings with modern variable pulse holmium lasers by Bell et al. (from: Bell JR, Penniston KL, Nakada SY, J Endourol 2017;31:1067-1072) J Endourol. 2017;31(12):1345–1346. doi: 10.1089/end.2017.0711. [DOI] [PubMed] [Google Scholar]
- 80.Bell J, Philip J, Rane A, Nakada SY. MP39-16 international holmium laser lithotripsy settings: an international survey of endourologists. J Endourol. 2016;30(S2):A336–A464. [Google Scholar]
- 81.Shah O, Chew B, Humphreys M, Sur R, Knudsen BE, Matlaga B, et al. MP46-13 dusting vs basketing during ureteroscopic lithotripsy—what is more efficacious? A multi-centre prospective trial from the EDGE Research Consortium. J Endourol. 2015;29(Suppl 1):A351. [Google Scholar]
- 82.Aldoukhi AH, Roberts WW, Hall TL, Ghani KR. Holmium laser lithotripsy in the new stone age: dust or bust? Front Surg. 2017;4:57. doi: 10.3389/fsurg.2017.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wollin D, Jiang R, Tom W, Radvak D, Simmons WN, Preminger G, et al. PD35-05 how do you like your popcorn? An evaluation of laser settings and location in the efficiency of the popcorn effect. J Urol. 2017;197(4, Supplement):e664. doi: 10.1007/s00240-018-1066-6. [DOI] [PubMed] [Google Scholar]
- 84.Emiliani E, Talso M, Cho S-Y, Baghdadi M, Mahmoud S, Pinheiro H, et al. Optimal settings for the noncontact holmium:YAG stone fragmentation popcorn technique. J Urol. 2017;198(3):702–706. doi: 10.1016/j.juro.2017.02.3371. [DOI] [PubMed] [Google Scholar]
- 85.Al-Kandari AM, Desai M, Shokeir AA, Shoma AM, Smith AD. Difficult cases in endourology. London: Springer; 2013. [Google Scholar]
- 86.Hecht SL, Wolf JS., Jr Techniques for holmium laser lithotripsy of intrarenal calculi. Urology. 2013;81(2):442–445. doi: 10.1016/j.urology.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 87.Ishii H, Griffin S, Somani BK. Ureteroscopy for stone disease in the paediatric population: a systematic review. BJU Int. 2015;115(6):867–873. doi: 10.1111/bju.12927. [DOI] [PubMed] [Google Scholar]
- 88.Ghosh A, Somani BK. Safety and feasibility of day case ureteroscopy and laser lithotripsy (URSL) in patients with a solitary kidney. Centr Eur J Urol. 2016;69(1):91–95. doi: 10.5173/ceju.2016.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.El-Nahas AR, Elshal AM, El-Tabey NA, El-Assmy AM, Shokeir AA. Percutaneous nephrolithotomy for staghorn stones: a randomised trial comparing high-power holmium laser versus ultrasonic lithotripsy. BJU Int. 2016;118(2):307–312. doi: 10.1111/bju.13418. [DOI] [PubMed] [Google Scholar]
- 90.Ishii H, Aboumarzouk OM, Somani BK. Current status of ureteroscopy for stone disease in pregnancy. Urolithiasis. 2014;42(1):1–7. doi: 10.1007/s00240-013-0635-y. [DOI] [PubMed] [Google Scholar]
- 91.Aboulela W, ElSheemy MS, Shoukry AI, Shouman AM, Elshenoufy A, Daw K, et al. Transurethral holmium laser cystolithotripsy in children: single center experience. J Endourol. 2015;29(6):661–665. doi: 10.1089/end.2014.0636. [DOI] [PubMed] [Google Scholar]
- 92.Altay B, Erkurt B, Albayrak S. A review study to evaluate holmium:YAG laser lithotripsy with flexible ureteroscopy in patients on ongoing oral anticoagulant therapy. Lasers Med Sci. 2017;32(7):1615–1619. doi: 10.1007/s10103-017-2289-4. [DOI] [PubMed] [Google Scholar]
- 93.Bujons A, Millán F, Centeno C, Emiliani E, Sánchez Martín F, Angerri O, Caffaratti J, Villavicencio H. Mini-percutaneous nephrolithotomy with high-power holmium YAG laser in pediatric patients with staghorn and complex calculi. J Pediatr Urol. 2016;12(4):253.e1–253.e5. doi: 10.1016/j.jpurol.2016.04.027. [DOI] [PubMed] [Google Scholar]
- 94.Ilic P, Djordjevic M, Kojovic V, Dzambasanovic S. Laser lithotripsy in the treatment of renal stones in children. A single-center experience. Ann Ital Chir. 2016;87:326–332. [PubMed] [Google Scholar]
- 95.Sevinc C, Balaban M, Ozkaptan O, Karadeniz T. Flexible ureterorenoscopy and laser lithotripsy for the treatment of allograft kidney lithiasis. Transplant Proc. 2015;47(6):1766–1771. doi: 10.1016/j.transproceed.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 96.Dołowy Ł, Krajewski W, Dembowski J, Zdrojowy R, Kołodziej A. The role of lasers in modern urology. Centr Eur J Urol. 2015;68(2):175–182. doi: 10.5173/ceju.2015.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Abedi AR, Allameh F, Razzaghi MR, Fadavi B, Qashqai H, Najafi S, Ranjbar A, Bashirian M. The efficacy and safety of laser lithotripsy in pregnancy. J Lasers Med Sci. 2017;8(2):84–87. doi: 10.15171/jlms.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tepeler A, Sninsky BC, Nakada SY. Flexible ureteroscopic laser lithotripsy for upper urinary tract stone disease in patients with spinal cord injury. Urolithiasis. 2015;43(6):501–505. doi: 10.1007/s00240-015-0786-0. [DOI] [PubMed] [Google Scholar]
- 99.• Prattley S, Cheng S, Voss J, Geraghty R, Jones P, Somani BK. Ureteroscopy and stone treatment in the elderly (≥70 years): prospective outcomes over 5-years with a review of literature. Int Braz J Urol. 2018; (In Press). One of the several key papers on the safety of ureterorenoscopy and laser lithotripsy for specific patient populations. [DOI] [PMC free article] [PubMed]
- 100.Yoshioka T, Otsuki H, Uehara S, Shimizu T, Murao W, Fujio K, Fujio K, Wada K, Araki M, Nasu Y. Effectiveness and safety of ureteroscopic holmium laser lithotripsy for upper urinary tract calculi in elderly patients. Acta Med Okayama. 2016;70(3):159–166. doi: 10.18926/AMO/54414. [DOI] [PubMed] [Google Scholar]
- 101.Sharaf A, Amer T, Somani BK, Aboumarzouk OM. Ureteroscopy in patients with bleeding diatheses, anticoagulated, and on anti-platelet agents: a systematic review and meta-analysis of the literature. J Endourol. 2017;31(12):1217–1225. doi: 10.1089/end.2017.0253. [DOI] [PubMed] [Google Scholar]
- 102.Zhang P, Hu W-L. Sudden onset of a huge subcapsular renal hematoma following minimally invasive ureteroscopic holmium laser lithotripsy: a case report. Exp Ther Med. 2015;10(1):335–337. doi: 10.3892/etm.2015.2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guzelburc V, Balasar M, Colakogullari M, Guven S, Kandemir A, Ozturk A, et al. Comparison of absorbed irrigation fluid volumes during retrograde intrarenal surgery and percutaneous nephrolithotomy for the treatment of kidney stones larger than 2 cm. SpringerPlus. 2016;5(1):1707. doi: 10.1186/s40064-016-3383-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Uchida Y, Takazawa R, Kitayama S, Tsujii T. Predictive risk factors for systemic inflammatory response syndrome following ureteroscopic laser lithotripsy. Urolithiasis. 2017; 10.1007/s00240-017-1000-3. [DOI] [PubMed]
- 105.Fan S, Gong B, Hao Z, Zhang L, Zhou J, Zhang Y, Liang C. Risk factors of infectious complications following flexible ureteroscope with a holmium laser: a retrospective study. Int J Clin Exp Med. 2015;8(7):11252–11259. [PMC free article] [PubMed] [Google Scholar]
- 106.Madec F-X, Suply E, Luyckx F, Nedelec M, Chowaniec Y, Branchereau J, le Normand L, Glemain P. L’urétérorénoscopie souple avec fragmentation laser dans le traitement des calculs du haut appareil urinaire chez les patients atteints d’une maladie du système nerveux avec un handicap moteur sévère. Prog Urol. 2017;27(6):369–374. doi: 10.1016/j.purol.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 107.Tao W, Cai CJ, Sun CY, Xue BX, Shan YX. Subcapsular renal hematoma after ureteroscopy with holmium:yttrium-aluminum-garnet laser lithotripsy. Lasers Med Sci. 2015;30(5):1527–1532. doi: 10.1007/s10103-015-1760-3. [DOI] [PubMed] [Google Scholar]
- 108.Paiva MM, da Silva RD, Jaworski P, Kim FJ, Molina WR. Subcapsular hematoma after ureteroscopy and laser lithotripsy. Can J Urol. 2016;23(4):8385–8387. [PubMed] [Google Scholar]
- 109.Chouhan JD, Zhao HH, Magee B, McNeil BK. Retroperitoneal hemorrhage after ureteroscopy without laser lithotripsy: an extreme example of an underreported event? Can J Urol. 2016;23(3):8324–8328. [PubMed] [Google Scholar]
- 110.Althunayan AM, Elkoushy MA, Elhilali MM, Andonian S. Adverse events resulting from lasers used in urology. J Endourol. 2014;28(2):256–260. doi: 10.1089/end.2013.0451. [DOI] [PubMed] [Google Scholar]
- 111.Whitehurst LA, Somani BK. Perirenal hematoma after ureteroscopy: a systematic review. J Endourol. 2017;31(5):438–445. doi: 10.1089/end.2016.0832. [DOI] [PubMed] [Google Scholar]
- 112.Vaidyanathan S, Samsudin A, Singh G, Hughes PL, Soni BM, Selmi F. Large subcapsular hematoma following ureteroscopic laser lithotripsy of renal calculi in a spina bifida patient: lessons we learn. Int Med Case Rep J. 2016;9:253–259. doi: 10.2147/IMCRJ.S99960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Aldoukhi AH, Ghani KR, Hall TL, Roberts WW. Thermal response to high-power holmium laser lithotripsy. J Endourol. 2017;31(12):1308–1312. doi: 10.1089/end.2017.0679. [DOI] [PubMed] [Google Scholar]
- 114.Butticè S, Sener TE, Proietti S, Dragos L, Tefik T, Doizi S, et al. Temperature changes inside the kidney: what happens during holmium:yttrium-aluminium-garnet laser usage? J Endourol. 2016;30(5):574–579. doi: 10.1089/end.2015.0747. [DOI] [PubMed] [Google Scholar]
- 115.• Wollin DA, Carlos EC, Tom WR, Simmons WN, Preminger GM, Lipkin ME. Effect of laser settings and irrigation rates on ureteral temperature during holmium laser lithotripsy, an in vitro model. J Endourol. 2017; 10.1089/end.2017.0658. One of the several scary papers about possible and significantly harmful temperature increases during laser lithotripsy. [DOI] [PubMed]
- 116.Lange BI, Brendel T, Hüttmann G. Temperature dependence of light absorption in water at holmium and thulium laser wavelengths. Appl Opt. 2002;41(27):5797–5803. doi: 10.1364/ao.41.005797. [DOI] [PubMed] [Google Scholar]
- 117.Kallidonis P, Amanatides L, Panagopoulos V, Kyriazis I, Vrettos T, Fligou F, Kamal W, Liatsikos EN. Does the heat generation by the thulium:yttrium aluminum garnet laser in the irrigation fluid allow its use on the upper urinary tract? An experimental study. J Endourol. 2016;30(4):422–427. doi: 10.1089/end.2015.0252. [DOI] [PubMed] [Google Scholar]
- 118.Rossini FD. Excursion in chemical thermodynamics, from the past into the future. Pure Appl Chem. 1964;8(2):95–112. [Google Scholar]
- 119.Gross AJ, Netsch C. Editorial comment on: Thermal response to high-power holmium laser lithotripsy by Aldoukhi et al. J Endourol. 2017;31(12):1313. doi: 10.1089/end.2017.0809. [DOI] [PubMed] [Google Scholar]
- 120.Villa L, Cloutier J, Compérat E, Kronemberg P, Charlotte F, Berthe L, et al. Do we really need to wear proper eye protection when using holmium:YAG laser during endourologic procedures? Results from an ex vivo animal model on pig eyes. J Endourol. 2016;30(3):332–337. doi: 10.1089/end.2015.0232. [DOI] [PubMed] [Google Scholar]
- 121.Hadjipavlou M, Lam V, Seth J, Anjum F, Sriprasad S. MP28-18 predicting radiation exposure in ureterorenoscopy and laser lithotripsy: an analysis of patient and stone characteristics. J Urol. 2015;193(4, Supplement):e317. doi: 10.1159/000486345. [DOI] [PubMed] [Google Scholar]
- 122.Aboutaleb H. Fluoroscopy free flexible ureteroscopy with holmium: yttrium-aluminium-garnet laser lithotripsy for removal of renal calculi. Arab J Urol. 2016;14(2):123–130. doi: 10.1016/j.aju.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Talso M, Emiliani E, Haddad M, Berthe L, Baghdadi M, Montanari E, et al. Laser fiber and flexible ureterorenoscopy: the safety distance concept. J Endourol. 2016;30(12):1269–1274. doi: 10.1089/end.2016.0209. [DOI] [PubMed] [Google Scholar]
- 124.Emiliani E, Talso M, Traxer O. Re: Evaluation of novel ball-tip holmium laser fiber: impact on ureteroscope performance and fragmentation efficiency (from: Shin RH, Lautz JM, Cabrera FJ, et al. J Endourol 2016;30:189-194) J Endourol. 2017;31(6):618. doi: 10.1089/end.2016.0208. [DOI] [PubMed] [Google Scholar]
- 125.Bagbanci S. Holmium: yttrium aluminum garnet laser and guidewires: is there a durability difference among guidewires against laser energy? An in vitro experimental study. J Endourol. 2017;31(5):528–532. doi: 10.1089/end.2016.0883. [DOI] [PubMed] [Google Scholar]
- 126.Huang Z, Fu F, Zhong Z, Xu R, Zhang L, Deng G, et al. Zebra guidewire damage by holmium: YAG laser and management of removal. Int J Clin Exp Med. 2015;8(8):14251–14253. [PMC free article] [PubMed] [Google Scholar]