Abstract
Context:
The nature of Australian rules football (Australian football) predisposes both unique and common injuries compared with those sustained in other football codes. The game involves a combination of tackling, kicking, high-speed running (more than other football codes), and jumping. Two decades of injury surveillance has identified common injuries at the professional level (Australian Football League [AFL]).
Objective:
To provide an overview of injuries in Australian rules football, including injury rates, patterns, and mechanisms across all levels of play.
Study Design:
A narrative review of AFL injuries, football injury epidemiology, and biomechanical and physiological attributes of relevant injuries.
Results:
The overall injury incidence in the 2015 season was 41.7 injuries per club per season, with a prevalence of 156.2 missed games per club per season. Lower limb injuries are most prevalent, with hamstring strains accounting for 19.1 missed games per club per season. Hamstring strains relate to the volume of high-speed running required in addition to at times having to collect the ball while running in a position of hip flexion and knee extension. Anterior cruciate ligament injuries are also prevalent and can result from contact and noncontact incidents. In the upper limb, shoulder sprains and dislocations account for 11.5 missed games per club per season and largely resulted from tackling and contact. Concussion is less common in AFL than other tackling sports but remains an important injury, which has notably become more prevalent in recent years, theorized to be due to a more conservative approach to management. Although there are less injury surveillance data for non-AFL players (women, community-level, children), many of these injuries appear to also be common across all levels of play.
Clinical Relevance:
An understanding of injury profiles and mechanisms in Australian football is crucial in identifying methods to reduce injury risk and prepare players for the demands of the game.
Keywords: AFL, injury prevention, injury surveillance
Australian rules football (Australian football) is a unique code of football played widely in Australia. It attracts participants from across a broad level, from children to the community to the national professional competition known as the Australian Football League (AFL). Across Australia, the number participating in Australian football is estimated to exceed 1.2 million, including almost 320,000 female participants.3 Female football play has been growing rapidly, with a 25% increase from 2014 from 2015.3
Australian football is a contact, winter sport played on natural grass with an oval ball made of leather. There are 18 players on the field plus 4 additional players on the bench (with 90 allowed rotations per match at the AFL level). Most playing fields are also used for cricket in the summer and are larger than those used by other football codes, varying from 135 to 185 m in length and 110 to 155 m in width.4 The sport requires a mix of endurance and high-speed running, kicking, ball-handling skills, and tackling (Figure 1).
Figure 1.

Overview of professional men’s Australian football.2
In the AFL, 18 men’s teams compete weekly across a season that lasts 22 rounds, with 4 additional weeks of finals. Clubs had an average of 45.4 players on their player lists in 2015.1 Until recently, the national level has been predominantly played by men, but the AFL launched a semiprofessional, national-level, female competition in 2017 with 8 teams.3
As with all other football codes, there is a risk of injury associated with participation in the sport. While many injuries may be somewhat preventable with implementation of suitable strategies, performance factors tend to drive injury rates upward.46 To inform such efforts, it is first important to understand both the common and unique injuries associated with the sport.22 The purpose of this review was to draw upon 2 decades of published injury surveillance data at the professional level to provide an overview of injuries of particular relevance to AFL players. This was supplemented with what is known about injuries across other competition levels from a variety of published sources.
Methods
A literature search was conducted using the SPORTDiscus, MEDLINE, and Google Scholar databases to find relevant articles pertaining to AFL injuries, football injury epidemiology, and biomechanical and physiological attributes of relevant injuries. Injury data pertaining to football codes were also sought from injury and annual reports published by respective sport organizations. Narrative review methods were used to synthesize data.
Injury Surveillance in Australian Football
Professional/AFL
The AFL has publicly released an annual injury report covering its national elite male competition since 1996, with 100% compliance since 1997.53 The AFL is believed to be the first professional football code to publish an annual injury report for its entire professional league.53 Player contracts include consent for players’ injury records to be used anonymously for research purposes, including injury surveillance. At times, the AFL Research Board commissions specific injury-focused studies (eg, anterior cruciate ligament [ACL] and soft tissue injury audits) using these data; however, for this to occur, the players must provide further consent.56
The AFL has defined injury as any physical or medical condition that cause a player to be unavailable for a match in the regular season or finals.53 This definition is used to create uniformity across clubs and allow reliable comparison, negating observational bias. AFL clubs are required to record why any player is not playing for that week, and if injured, record the diagnosis using the Orchard sports injury classifications system (OSICS).56,58 These data do not delineate between training and match injuries, as it was thought that due to the high proportion of overuse injuries this would be problematic.52
The overall injury incidence for the 2015 season was 41.7 injuries per club per season,1 equivalent to just under 1 injury per player. This has been fairly consistent over time, ranging from 37.6 (1993) to 48.1 (1997) since records began.
In the AFL Injury Survey, injury prevalence is defined as the number of missed games per club per season. It is recognized that this is not the traditional epidemiological definition of prevalence, but it has been used for 2 decades as the AFL’s preferred measure of time missed through injury. The injury prevalence in the AFL for 2015 was 156.2 missed games per club per season, and this has ranged from 116.3 (1994) to 158.1 (2013) since records began. The game has evolved, with more high-speed running and increased size of players, causing higher injury rates despite improved conditioning and injury prevention practices.46
The most prevalent injuries in the AFL are hamstring strains (19.1 missed games/club/season in 2015), ACL injuries (16.7 missed games/club/season), shoulder sprains and dislocations (11.5 missed games/club/season), leg and foot stress fractures (8.6 missed games/club/season), and ankle sprains or joint injuries (7.2 missed games/club/season) (Table 1 in the Appendix, available in the online version of this article).1 Shoulder sprains and dislocations refer to the glenohumeral joint specifically, as acromioclavicular (AC) joint and clavicle pathology are categorized separately and cause fewer missed matches (AC joint injuries, 0.4; clavicle fractures, 0.1). Groin strains and osteitis pubis was previously the second-most common injury, with a prevalence of 17.5 in 2007; however, this had fallen to 7.1 in 2015, potentially related to a shift toward hip-related pathologies being diagnosed more frequently and possibly improved conditioning programs and management. Other leg/foot/ankle injuries had a prevalence of 14.0 in 2015; however, this was unusually high and thought to be a reflection of an interpretation/classification issue rather than a change in injury patterns.1
The mean time lost per injury for the common AFL injuries is outlined in Table 2 in the Appendix. However, these data should be interpreted with caution, as the AFL Injury Survey only includes injuries that result in missed matches. For example, the mean number of missed matches for ankle sprains will be artificially high because those that do not cause any missed matches are excluded. In addition, if a significant injury (eg, shoulder dislocation requiring surgery) occurs late in the season, the player may miss fewer matches because they are able to recover during the off-season.
Comparison With Other Football Codes
The injury profile of Australian football tends to be more contact-orientated than soccer but more noncontact-oriented than rugby union and related sports (American football and rugby league).52 This seems to reflect the less frequent and perhaps lower force of tackling compared with rugby codes as well as the more open and dynamic nature of Australian football, with larger playing fields, longer duration of matches (mean match length, 120 minutes [20-minute quarters plus stoppage time]), and more high-speed running. There is more continuous running in Australian football than other codes where there are more regular breaks for tackling, with AFL players running on average 13.20 km per match at a mean 7.23 km/h. This includes, on average, 5 minutes 16 seconds at greater than 18 km/h.70 By comparison, a study of elite European soccer players found they ran on average 10.86 km per match, and 1 minute 24 seconds at greater than 18 km/h.44 Professional rugby union players in England covered an average of 7.52 km per match, including 300 m at greater than 20 km/h (different units).41 In soccer, 87% of injuries affect the lower limbs, compared with 68% in Australian football.
Other Levels of Play
There is no routine collection of injury data for any level of play other than at the AFL. Although the rules are largely the same across all levels, at least in adults, there is a slower speed of game and variation in skill level, which contributes to different injury profiles in community and professional football. Injury surveillance in the adult male community leagues and junior leagues has been undertaken in a sample of clubs through specific research studies reported in the peer-reviewed literature.7,17,25,31,33,42,60,61 A recent review has summarized the methods used in these studies.25 These studies have generally used an injury definition encompassing both medical treatment and time-loss injuries occurring during both matches and training. The inclusion of either team-based or player-exposure measures have enabled calculations of injury rates. There have also been published reports of the profile of Australian football injuries treated in medical treatment settings, such as hospitals, but such studies have not allowed calculation of exposure-adjusted injury rates.18 More recently, the first profile of injuries in female Australian football players has been published from a compilation of the above sources29 and the first survey of injured players.27
Lower Limb Injuries
Irrespective of the level of play, the lower limbs are the most commonly injured body region. Almost all the community-level studies either did not collect or report specific injury diagnoses, so it was not possible to summarize those studies to this same level of detail. The exceptions were the amateur Australian football players, for whom provisional injury diagnoses were coded according to the OSICS.31 However, on a frequency basis, lower limb injuries account for 40% to 68% of all injuries in adult male community players and 42% to 49% of all injuries in children.25
Soft tissue injuries of the lower limb typically require less recovery time than bone and joint injuries; however, their collective time burden for a club over a season can be greater.1 The burden of soft tissue injuries is complicated by the high incidence of recurrent injuries and the prolonged recovery for recurrent injuries. Furthermore, this high soft tissue load injury rate has been fairly refractory over time1 despite advancement in imaging technology, improved anatomical and pathological understanding, and improved sports science and medicine practices, perhaps suggesting that game-related factors such as running loads are more relevant than prevention strategies in affecting incidence.20
Strain Injuries
Hamstring
The incidence of hamstring strain injury is high across all football codes19,71; however, it is the sport-specific demands that contribute to the particularly high risk of this injury in Australian football. Hamstring injuries were also the most common individual injury in the single community-level surveillance study reporting diagnostic detail.31 The substantial volume of high-speed running in the AFL70 is a known risk factor for hamstring strain injuries.16 Players also frequently collect the ball from the ground on the run in the vulnerable position of trunk flexion, hip flexion, and knee extension (Figure 2).39 This is often completed under stress from an opponent at the moment of ball collection, where the hamstring is particularly vulnerable to higher grade (proximal biceps femoris intramuscular tendon) strains.
Figure 2.
Picking up a ground ball on the run results in hip flexion and knee extension (Source: Australian Football League).
The biceps femoris is the predominant affected muscle,32 with frequent involvement of the intramuscular tendon.8,10 Such injuries have also recently been identified as the most common types of subsequent injury in AFL players.24
Quadriceps
Quadriceps strain injuries occur predominantly in the rectus femoris of the kicking leg.8 As for hamstring strain injuries, tendon involvement is important to consider for return-to-play planning.12 Strain events in the other 3 quadriceps muscles do not cause as much concern, as they tend to settle quickly.12
Calf
Calf strain injuries are less common, yet their prevalence/incidence has increased over time. This may be attributed to the introduction of 1 bench injury substitute in 2011, with 1 less player being freely available to interchange (1 injury substitute plus 3 free interchange players, previously 4 interchange players and no substitute), although hamstring strains were noted to drop concurrently.1 The substitute was removed in 2016. Musculotendinous junction and intramuscular tendon soleus injuries are more likely to result in missed games.67 The gastrocnemius is less commonly involved in strain events in the AFL.67
Adductor
Adductor strain injuries (included in the hip and groin grouping in the AFL Injury Survey) as a group are neither frequently encountered nor a cause for long-term absence1 compared with insertional tendinopathy at the pubic symphysis. This possibly reflects the absence of kicking in the abducted foot position relative to soccer and possibly the absence of intramuscular tendon involvement.
Contusions
Contusions commonly occur to the lateral thigh (predominantly vastus lateralis and intermedialis) and less often in the leg muscle groups.43 While impact can arise from all hard surfaces or body parts, if the knee and high speed are involved, the severity can be underestimated and result in a more protracted or complicated outcome. Contusion and other soft tissue injuries are very common in players from the community forms of the game.25
Joint/Ligament Injuries
Ankle Sprain
The AFL injury report details a 10-year mean of 8.9 games missed per club per season from all ankle joint injuries. In 2015, there was a mean 2.3 new ankle injuries causing 7.2 missed games per AFL club.1 Undoubtedly, there are a significant number of low-grade ankle injuries not resulting in missed matches that were not included in these statistics.
The majority of reported ankle sprains in both the AFL and community forms of the game are lateral ankle sprains. Syndesmosis ankle sprains may be less common than in other sports such as rugby union, where they are a large cause of morbidity,21 but they still represent a significant proportion of the overall morbidity.
Typical mechanisms of ankle sprains include marking contests, where a player may land on another player’s foot, similar to other sports such as basketball and netball, causing either an inversion injury or less commonly an eversion and external rotation injury. A player’s foot could also become trapped and twisted into eversion as the “pack” falls to the ground, but one can also see how rugby union players would be more often exposed to a loaded rotation mechanism with multiple players in scrums and tackles. Another common mechanism is the player who has the foot planted and is rotating to pass the ball while being tackled.
Anterior Cruciate Ligament
The incidence of ACL injuries over the previous 2 decades is 0.7 per AFL club per season.1,56,58 The incidence decreased from the 1990s to 2012,58 possibly due to improved strength and conditioning practices and changes in ground preparation aimed to reduce shoe-surface traction injuries.53,54 ACL injuries typically occur early in the playing season and preseason training,54,55 with 2014 being an unexplained anomaly to this trend.56
ACL injuries are expensive, both in terms of treatment costs and missed matches.35 They are treated surgically, with a mean return to play of 10 to 12 months.48 Hence, AFL players are unlikely to return to play in the same playing season.54,65
Australia has the highest incidence of ACL reconstructions per 100,000 person-years as compared with other Western countries, and in Australia, at the population level, Australian football has the second-highest incidence of ACL injuries per participant after skiing.35 A greater incidence of ACL injuries in the AFL occurs in warmer regions,1,49,55 a finding consistent with European soccer.66 This is hypothesized to be due to the higher traction forces encountered playing on warm season grasses.50,59 Injury risk has also been demonstrated to be related to ground hardness in community football.64
Noncontact mechanisms account for 56% of ACL ruptures in Australian football.9 Side-stepping and landing on an extended knee appear to be the most common mechanisms of noncontact ACL injuries in the league, as identified on video analysis.9 Risk factors include speed and change of direction, knee instability, angle of landing, and studded boots increasing friction with the ground.65 A recent randomized controlled trial has demonstrated that targeted exercise training programs for community Australian football can reduce the risk of knee injury by up to 50% and the risk of all lower limb injury by 22%.26
Female athletes are at greater risk of ACL rupture than males, with a 2- to 3-fold increase observed in other football codes.27 Data do not currently exist for this cohort in Australian football; however, the Women’s Injury Surveillance Extension (FootyWISE) was established to address this gap.27 The first analysis of injury data in women players was not able to confirm an excess of ACL ruptures because of a low number of reported injuries.27,29
Posterior Cruciate Ligament
Posterior cruciate ligament (PCL) injuries have earned the colloquial label “ruckman’s curse” due to their prevalence in AFL ruckmen. Opposing ruckmen jump to contest the ball when it is bounced up or thrown in at a stoppage in play.57 The 2 opposing ruckmen will usually run at each other while the ball is in flight, potentially colliding with a flexed knee. The most widely reported mechanism of PCL injury is a fall on the flexed knee with the foot in plantar flexion or direct force blow to the anterior tibia63; however, a ruckman can also collide with a flexed knee while “rucking.”
Because of a spike in PCL ruptures in ruckmen,57 the center circle rule was developed in 2005, which led to the creation of a 10-meter outer circle that the ruckmen had to start in at a center bounce. The rule change was aimed at decreasing the run-up distance and acceleration, which would then translate into decreasing impact forces.51 A cohort study in 2009 demonstrated that the rule change was successful in reducing the overall ruck-related PCL injuries in general and those due to the center bounce mechanism.51,55,57 A further rule change was introduced in 2013 to increase the separation of ruckmen at stoppages; however, the efficacy of this rule cannot yet be established.51 The reduction in ground hardness could be a possible confounder in decreased injury rates due to non-ruck-related mechanisms.45
The incidence of PCL injuries for the latest 2015 AFL injury surveillance data was 0.5 new injuries, in keeping with historically low averages since the introduction of the center circle rule.1
Upper Limb Injuries
The upper limb is the second-most common body region of injuries in Australian football in children, with 18% to 22% of all injuries, compared with 13% to 27% of injuries in adult male community players.25 Such injuries are also common in female players.27 Upper limb injuries are more commonly reported in treatment-based data collections than in club surveillance in community football because of their nature (commonly involving the wrist, fingers, and hands) and immediate assessment needs.17
Shoulder
Shoulder injuries in all forms of Australian football occur due to the contact/collision nature of the sport. Glenohumeral instability has the greatest incidence and time lost to injury (1.0 to 1.8 new injuries/club/year resulting in 7.1 to 21.1 missed games/club/season).1 Recurrence rates are typically between 9% and 15% but have been much higher (54% in 2014).1
The first injury pattern relates to the contested overhead mark (mean, 11.4 per AFL club/game).2 This action involves the arm being placed in full abduction and at the limit of shoulder external rotation during an attempt to catch/mark the ball against an opponent who is attempting to disrupt the mark, usually by punching or knocking the ball away concurrently. Unique to Australian football is the height at which this can occur, which is greater than other codes because of the allowed technique of jumping onto another player to increase elevation. This mechanism can result in hyperexternal rotation of the abducted arm, with resultant glenohumeral joint anterior instability injury patterns.
The second injury pattern involves players competing for the ball while at ground level, even lying on the ground. This can occur when a player in the prone position reaches forward into full flexion and external rotation toward the ball and another player impacts on the posterior aspect of the scapula or shoulder, forcing the arm into hyperflexion/external rotation, also creating anterior instability.
Third, glenohumeral instability may result after a tackle. While tackling is more prevalent in other football codes (eg, the mean number per club per game in the Australian National Rugby League in 2016 was 32647), it is also a prominent feature of AFL, with a mean 69.6 tackles per game in 2016.2 Tackling a player head-on with the arm abducted at 90° risks anterior dislocation force similar to that seen in other tackling sports. In Australian football, the lack of an offside rule means players can be tackled from any direction, and tackles more often occur by chasing a player down rather than head-on. This frequently leaves the arms of the tackled player free. A tackle that takes the player to the ground in this way can result in forced abduction and external rotation and a greater likelihood of glenohumeral instability injury compared with rugby, in which the arms are often pinned to the player and resultant impact results more frequently in an AC joint injury.
Preventative/protective taping and bracing of the shoulder is less effective in Australian football players than in other tackling football codes, as every player in the team is required to be able to freely reach overhead repetitively during the game. Taping is commonly used in Australian football players; however, the effect is largely proprioceptive rather than providing structural restraint.5
Posterior instability injuries in Australian football mimic those of other football codes, caused by a direct anterior impact to the shoulder or the player either falling onto the elbow or fending off another player with the shoulder forward flexed and resultant posteriorly directed forces applied to the joint. Posterior dislocation is far less common than anterior dislocation62 and appears to present more commonly with subluxation symptoms rather than frank dislocations.
Clavicular and AC joint injury patterns in Australian football mimic those seen in other contact sports such as rugby, with direct impact during a tackle or with the player falling to the ground with the arm by the side and a direct lateral impact to the shoulder.11 No shoulder padding is worn. In Australian football, “bumping” (deliberately impacting an opposing player with the hip and shoulder) is a legal means of dispossessing a player with the ball and can also result in impact injury to the shoulder. Whereas AC joint injury is the most common shoulder injury in rugby,34 glenohumeral instability is more common than AC joint injury in the AFL.1
Concussion
Concussion in the AFL appears less common than in head-on tackling sports such as rugby union, with 6 per 1000 player-hours in Australian football compared with 13.4 in rugby union.1,21 Both statistics include all concussions, regardless of whether they resulted in missed matches. By contrast, statistics from the annual AFL Injury Survey only includes injuries causing missed matches. The AFL Injury Survey incidence of concussion (new injuries/AFL club/season) has increased over the past decade, from 0.3 in 2006 to 1.5 in 2015,1 particularly since 2011, when a rule was introduced that players could not return in a match after suffering a concussion.51
The prevalence of concussion in the AFL (missed games/AFL club/season) has also increased, with a notable spike from 1.6 in 2014 to 4.2 in 2015. However, the 2014 and 2015 surveys suggest that the increase in observed rates of concussion and missed time may be a reflection of better recognition and increasingly conservative approaches toward concussions, with players being more likely to miss a game, as opposed to a recent true increase in prevalence.1,56
Concussion rates have also been reported in community forms of the game. In an adult male league, they accounted for 19% of all head/neck/orofacial injuries.6 In a secondary analysis of data from a randomized controlled trial, concussion rates in community football were 4.9 per 1000 game-hours.36 An analysis of hospital admissions data over a 9-year period prior to mid-2011 reported a relatively stable rate of concussion-related admissions from Australian football, with a mean 80.3 cases per 100,000 participants aged 15+ years.23 In a survey of injured female players, concussion was ranked as the most commonly reported worst injury by 33% of survey respondents.27
The nature of Australian football places players at risk of concussion from unique mechanisms during play. Opponents can tackle players from any angle, and since there are 36 players on the ground at any time, there is a considerable risk of accidental collision. The rules of the game aim to protect players from being struck in the head; however, head contact still does occur both within and outside the rules of the game.4 In a study involving male adults from community leagues in 2 states, 63% of the concussions were sustained within game rules.30
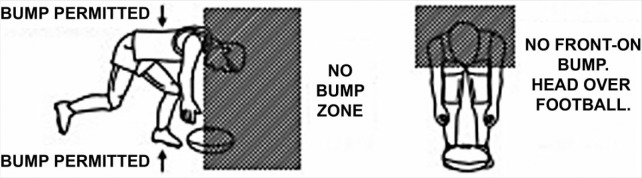
Examples of at-risk plays include a player jumping for the ball and being punched in the back of the head by a player trying to “spoil” the ball who misjudges (or maliciously judges) their approach. Players may try to jump and mark a ball while running backward, which puts them at risk of hitting the back of their head on the pitch from a significant height or colliding with an opposition player. Players who are running to tackle a player with the ball may be “bumped” by opposition players who may deliberately obstruct them if they are within 5 meters of the player with the ball. A “bump” is similar to a block in American football (which is legal in this code) or a shoulder charge in the rugby codes (which is now illegal in both rugby codes). A player who is tackled is often “wrapped up” with the ball to secure a free kick. Therefore, players and coaches have adopted a tackling style that involves tackling a player around their arms, which leaves the head unprotected (Figure 3).
Figure 3.

Wrapping up arms in a tackle can leave a player’s head unprotected (Source: Australian Football League).
There can be a large size differential between players who are valuable to their team in different roles. Smaller, faster players are often utilized to pick up the ball when it goes to the ground while larger players are important for the aerial contests. Therefore, not only is a large size differential a risk to smaller players, but these smaller players are more often trying to pick up the ball from the ground while running fast such that their head is vulnerable to impact. Players must show a duty of care to other players who are bending to pick up the ball, and avoid any contact above the neck (Figure 4),4 which can be difficult if a player puts their head in a low or vulnerable position.
Figure 4.
The “no bump zone” (Source: Australian Football League).
In accordance with the 2012 Zurich consensus guidelines,40 the current policy of the AFL mandates off-field assessment whenever concussion is suspected. This requires a player to be removed from play and rested for a period of 10 minutes before a multimodal Standardized Concussion Assessment Tool (SCAT 3) is completed. An additional tool for clinical assessment and diagnosis of concussion is video replay footage, which is instantly available. Observable clinical signs of concussion have been shown to be highly correlated with concussion diagnosis, with good to excellent interrater reliability (among experienced clinicians) for observable clinical signs of concussion.13,38 No signs had both a high sensitivity and specificity for concussion, emphasizing the need for multimodal clinical assessment. These guidelines work well for the professional form of the game but, as has been reportedly the case for many other sports, compliance with concussion guidelines is hard to achieve in the community forms of the sport, and there are many challenges to overcome to ensure they are consistently implemented.15,36,68,69
Fatal Injuries
While death is not common during Australian football participation, insurance claims in community-level Australian football over a 10-year period from 2004 to 2013 found 18 of these deaths occurring during football matches or training, and 16 of those were in players. The most common causes of on-field death were cardiac and unconfirmed causes.28 Of the unconfirmed causes, many were listed as “collapsed,” so it is suspected that the number of cardiac causes may be underestimated. Within the limitations of the study, no contact-related or other physical injury deaths were identified in the Australian football players. A 2-year study of injury-related hospitalizations, which overlapped the same period, identified 2 in-hospital deaths related to match play.37
Conclusion
Two decades of injury surveillance in the AFL has provided valuable insight into injury patterns. The most prevalent injuries, and hence most costly from a time-loss perspective, are hamstring strains, ACL ruptures, and glenohumeral dislocations. Common injuries in the AFL can be attributed to the nature of the game, which includes contesting for a ball and tackling/being tackled from all directions, plus more high-speed running that other football codes. At the community level, there are no directly comparable data with the AFL; however, the most common injuries appear to be similar. Factors such as sports ground conditions, availability of sports medicine professionals at games, and formal implementation of safety practices may influence injury profiles at the community level.
Supplementary Material
Footnotes
The following authors declared potential conflicts of interest: Tanusha Cardoso is consulting as a sport and exercise medicine registrar at Alphington Sports Medicine Clinic, Victoria; John W. Orchard was the paid Injury Surveillance Coordinator for the Australian Football League for the period 1992-2014 inclusive.
References
- 1. Australian Football League. AFL Injury Survey 2015. Melbourne, Victoria, Australia: AFL Doctors Association, AFL Physiotherapists Association, AFL Football Operations Department; 2015. [Google Scholar]
- 2. Australian Football League. AFL player and match statistics. 2016. http://www.afl.com.au/stats. Accessed December 19, 2016.
- 3. Australian Football League. Australian Football League Annual Report 2015. Melbourne, Victoria, Australia: Australian Football League; 2015. [Google Scholar]
- 4. Australian Football League. Laws of Australian Football. Melbourne, Victoria, Australia: Australian Football League; 2016. [Google Scholar]
- 5. Bradley T, Baldwick C, Fischer D, Murrell GA. Effect of taping on the shoulders of Australian Football players. Br J Sports Med. 2009;43:735-738. [DOI] [PubMed] [Google Scholar]
- 6. Braham R, Finch CF, McCrory P. The incidence of head/neck/orofacial injuries in non-elite Australian Football. J Sci Med Sport. 2004;7:451-453. [DOI] [PubMed] [Google Scholar]
- 7. Braham R, Finch CF, McIntosh A, McCrory P. Community level Australian Football: a profile of injuries. J Sci Med Sport. 2004;7:96-105. [DOI] [PubMed] [Google Scholar]
- 8. Brukner P, Connell D. ‘Serious thigh muscle strains’: beware the intramuscular tendon which plays an important role in difficult hamstring and quadriceps muscle strains. Br J Sports Med. 2016;50:205-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cochrane JL, Lloyd DG, Buttfield A, Seward H, McGivern J. Characteristics of anterior cruciate ligament injuries in Australian Football. J Sci Med Sport. 2007;10:96-104. [DOI] [PubMed] [Google Scholar]
- 10. Comin J, Malliaras P, Baquie P, Barbour T, Connell D. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med. 2013;41:111-115. [DOI] [PubMed] [Google Scholar]
- 11. Crichton J, Jones DR, Funk L. Mechanisms of traumatic shoulder injury in elite rugby players. Br J Sports Med. 2012;46:538-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32:710-719. [DOI] [PubMed] [Google Scholar]
- 13. Davis G, Makdissi M. Use of video to facilitate sideline concussion diagnosis and management decision-making. J Sci Med Sport. 2016;19:898-902. [DOI] [PubMed] [Google Scholar]
- 14. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42:221-233. [PMC free article] [PubMed] [Google Scholar]
- 15. Donaldson A, Newton J, McCrory P, et al. Translating guidelines for the diagnosis and management of sports-related concussion into practice. Am J Lifestyle Med. 2016;10:120-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duhig S, Shield AJ, Opar D, Gabbett TJ, Ferguson C, Williams M. Effect of high-speed running on hamstring strain injury risk. Br J Sports Med. 2016;50:1536-1540. [DOI] [PubMed] [Google Scholar]
- 17. Ekegren CL, Gabbe BJ, Donaldson A, Cook J, Lloyd D, Finch CF. Injuries in community-level Australian football: results from a club-based injury surveillance system. J Sci Med Sport. 2015;18:651-655. [DOI] [PubMed] [Google Scholar]
- 18. Ekegren CL, Gabbe BJ, Finch CF. Medical-attention injuries in community Australian football: a review of 30 years of surveillance dtat from treatment sources. Clin J Sport Med. 2015;25:162-172. [DOI] [PubMed] [Google Scholar]
- 19. Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39:1226-1232. [DOI] [PubMed] [Google Scholar]
- 20. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45:553-558. [DOI] [PubMed] [Google Scholar]
- 21. EPRISP. England Professional Rugby Injury Surveillance Project: 2014-15 Season Report. Twickenham, England: Rugby Football Union; 2016. [Google Scholar]
- 22. Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006;9:3-9. [DOI] [PubMed] [Google Scholar]
- 23. Finch CF, Clapperton AJ, McCrory P. Increasing incidence of hospitalisation for sport-related concussion in Victoria, Australia. Med J Aust. 2013;198:427-430. [DOI] [PubMed] [Google Scholar]
- 24. Finch CF, Cook J, Kunstler BE, Akram M, Kunstler B, Orchard J. Subsequent injuries are more common than injury recurrences. An analysis of 1 season of prospectively collected injuries in professional Australian Football. Am J Sports Med. 2017;45:1921-1927. [DOI] [PubMed] [Google Scholar]
- 25. Finch CF, Gabbe B, White P, et al. Priorities for investment in injury prevention in community Australian football. Clin J Sport Med. 2013;23:430-438. [DOI] [PubMed] [Google Scholar]
- 26. Finch CF, Twomey DM, Fortington LV, et al. Preventing Australian football injuries with a targeted neuromuscular control exercise program: comparative injury rates from a training intervention delivered in a clustered randomised controlled trial. Inj Prev. 2016;22:123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fortington LV, Donaldson A, Finch CF. Self-reported worst injuries in women’s Australian football identify lower limb injuries as a prevention priority. BMJ Open Sport Exerc Med. 2016;2:e000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fortington LV, Finch CF. Death in community Australian football: a ten year national insurance claims report. PLoS One. 2016;11:e0159008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fortington LV, Finch CF. Priorities for injury prevention in women’s Australian football: a compilation of national data from different sources. BMJ Open Sport Exerc Med. 2016;2:e000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fortington LV, Twomey DM, Finch CF. Concussion in community Australian football—epidemiological monitoring of the causes and immediate impact on play. Inj Epidemiol. 2015;2:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gabbe B, Finch C, Wajswelner H, Bennell K. Australian football: injury profile at the community level. J Sci Med Sport. 2002;5:149-160. [DOI] [PubMed] [Google Scholar]
- 32. Gibbs N, Cross T, Cameron M, Houang M. The accuracy of MRI in predicting recovery and recurrence of acute grade one hamstring muscle strains within the same season in Australian Rules football players. J Sci Med Sport. 2004;7:248-258. [DOI] [PubMed] [Google Scholar]
- 33. Grimmer K, Williams J. Injury in junior Australian rules footballers. J Sci Med Sport. 2003;6:328-338. [DOI] [PubMed] [Google Scholar]
- 34. Headey J, Brooks JH, Kemp SP. The epidemiology of shoulder injuries in English professional rugby union. Am J Sports Med. 2007;35:1537-1543. [DOI] [PubMed] [Google Scholar]
- 35. Janssen K, Orchard J, Driscoll T, Van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003-2004 to 2007-2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports. 2012;22:495-501. [DOI] [PubMed] [Google Scholar]
- 36. Kemp J, Newton J, White P, Finch C. Implementation of concussion guidelines in community Australian Football and Rugby League—the experiences and challenges faced by coaches and sports trainers. J Sci Med Sport. 2016;19:305-310. [DOI] [PubMed] [Google Scholar]
- 37. Kreisfeld R, Harrison JE, Pointer SC. Australian Sports Injury Hospitalisations: 2011-2012. Canberra, ACT: Australian Institute of Health and Welfare; 2014. [Google Scholar]
- 38. Makdissi M, Davis G. The reliability and validity of video analysis for the assessment of the clinical signs of concussion in Australian football. J Sci Med Sport. 2016;19:859-863. [DOI] [PubMed] [Google Scholar]
- 39. Marovic P, Koulouris G. Imaging of the hamstring muscle complex in elite athletes. Aspetar Sports Med J. 2016;5:364-369. [Google Scholar]
- 40. McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 2013;47:250-258. [DOI] [PubMed] [Google Scholar]
- 41. McLaren SJ, Weston M, Smith A, Cramb R, Portas MD. Variability of physical performance and player match loads in professional rugby union. J Sci Med Sport. 2016;19:493-497. [DOI] [PubMed] [Google Scholar]
- 42. McMahon KA, Nolan T, Bennett CM, Carlin JB. Australian Rules football injuries in children and adolescents. Med J Aust. 1993;159:301-306. [DOI] [PubMed] [Google Scholar]
- 43. Mitchell B. Efficacy of thing protectors in preventing thigh haematomas. J Sci Med Sport. 2000;3:30-34. [DOI] [PubMed] [Google Scholar]
- 44. Mohr M, Krustrup P, Bangsbo J. Match performance of high-standard soccer players with special reference to development of fatigue. J Sports Sci. 2003;21:519-528. [DOI] [PubMed] [Google Scholar]
- 45. Norton K, Schwerdt S, Lange K. Evidence for the aetiology of injuries in Australian Football. Br J Sports Med. 2001;35:418-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Norton KI, Craig N, Olds T. The evolution of Australian Football. J Sci Med Sport. 1999;2:389-404. [DOI] [PubMed] [Google Scholar]
- 47. NRL. NRL Telstra Premiership Club Statistics. 2016. http://www.nrl.com/stats/telstrapremiership/clubstatistics/tabid/10254/default.aspx. Accessed December 19, 2016.
- 48. Orchard J. ACL prevention in Norway and Australia. Sport Health. 2008;26(2):17-22. [Google Scholar]
- 49. Orchard J. The ‘northern bias’ for injuries in the Australian Football League. Aust Turfgrass Manage. 2000;23:36-42. [Google Scholar]
- 50. Orchard J, Chivers I, Aldous D, Bennell K, Seward H. Rye grass is associated with fewer non-contact anterior cruciate ligament injuries than bermuda grass. Br J Sports Med. 2005;39:704-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Orchard J, McCrory P, Makdissi M. Use of rule changes to reduce injury in the Australian Football League. Minerva Ortop Trauma. 2014;65:355-364. [Google Scholar]
- 52. Orchard J, Seward H. Comparing AFL Injury Surveillance to other codes. Sport Health. 2009;27(2):38-41. [Google Scholar]
- 53. Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36:39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196-200. [DOI] [PubMed] [Google Scholar]
- 55. Orchard J, Seward H, Orchard JJ. AFL Injury Survey 2013. Melbourne, Victoria, Australia: AFL Doctors Association, AFL Physiotherapists Association, AFL Football Operations Department; 2013. [Google Scholar]
- 56. Orchard J, Seward H, Orchard JJ. AFL Injury Survey 2014. Melbourne, Victoria, Australia: AFL Doctors Association, AFL Physiotherapists Association, AFL Football Operations Department; 2014. [Google Scholar]
- 57. Orchard JW, Seward H. Decreased incidence of knee posterior cruciate ligament injury in Australian Football League after ruck rule change. Br J Sports Med. 2009;43:1026-1030. [DOI] [PubMed] [Google Scholar]
- 58. Orchard JW, Seward H, Orchard JJ. Results of 2 decades of injury surveillance and public release of data in the Australian Football League. Am J Sports Med. 2013;41:734-741. [DOI] [PubMed] [Google Scholar]
- 59. Orchard JW, Waldén M, Hägglund M, et al. Comparison of injury incidences between football teams playing in different climatic regions. Open Access J Sports Med. 2013;4:251-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Romiti M, Finch CF, Gabbe B. A prospective cohort study of the incidence of injuries among junior Australian football players: evidence for an effect of playing-age level. Br J Sports Med. 2008;42:441-446. [DOI] [PubMed] [Google Scholar]
- 61. Shawdon A, Brukner P. Injury profile of amateur Australian rules footballers. Aust J Sci Med Sport. 1994;26:59-61. [PubMed] [Google Scholar]
- 62. Tannenbaum EP, Sekiya JK. Posterior shoulder instability in the contact athlete. Clin Sports Med. 2013;32:781-796. [DOI] [PubMed] [Google Scholar]
- 63. Tsikouris G. Posterior cruciate ligament injuries in sports: treatment options. Br J Sports Med. 2011;45:e2. [Google Scholar]
- 64. Twomey DM, Finch CF, Lloyd DG, Elliott BC, Doyle TLA. Ground hardness and injury risk in community level Australian football. J Sci Med Sport. 2012;15:305-310. [DOI] [PubMed] [Google Scholar]
- 65. Verrall MG, Esterman A, Hewett ET. Analysis of the three most prevalent injuries in Australian Football demonstrates a season to season association between groin/hip/osteitis pubis injuries with ACL knee injuries. Asian J Sports Med. 2014;5:e23072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Waldén M, Hägglund M, Orchard J, Kristenson K, Ekstrand J. Regional differences in injury incidence in European professional football. Scand J Med Sci Sports. 2013;23:424-430. [DOI] [PubMed] [Google Scholar]
- 67. Waterworth G, Wein S, Gorelik A, Rotstein A. MRI assessment of calf injuries in Australian Football League players: findings that influence return to play. Skeletal Radiol. 2017;46:343-350. [DOI] [PubMed] [Google Scholar]
- 68. White P, Donaldson A, Sullivan S, Newton J, Finch C. Australian Football League concussion guidelines: what do community players think? BMJ Open Sport Exerc Med. 2016;2:e000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. White PE, Newton JD, Makdissi M, et al. Knowledge about sports-related concussion: is the message getting through to coaches and trainers? Br J Sports Med. 2014;48:119-124. [DOI] [PubMed] [Google Scholar]
- 70. Wisbey B, Montgomery P. Quantifying Changes in AFL Player Game Demands Using GPS Tracking: 2015 AFL Season. Melbourne, Victoria, Australia: Austrian Football League; 2016. [Google Scholar]
- 71. Woods C, Hawkins R, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of hamstring injuries. Br J Sports Med. 2004;38:36-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.