Abstract
This study aimed to document the perspective of patients with chronic obstructive pulmonary disease (COPD) who underwent home-based pulmonary rehabilitation (HBPR) in a clinical trial. In this qualitative study, open-ended questions explored participants’ views regarding HBPR. Thirteen semi-structured interviews were analysed using a thematic analysis approach. Major themes from interviews included the positive impact of HBPR on physical fitness, breathing and mood. Participants valued the flexibility and convenience of the programme. Participants also highlighted the importance of social support received, both from the physiotherapist over the phone and from family and friends who encouraged their participation. Reported challenges were difficulties in initiating exercise, lack of variety in training and physical incapability. While most participants supported the home setting, one participant would have preferred receiving supervised exercise training at the hospital. Participants also reported that HBPR had helped establish an exercise routine and improved their disease management. This study suggests that people with COPD valued the convenience of HBPR, experienced positive impacts on physical fitness and symptoms and felt supported by their community and programme staff. This highly structured HBPR model may be acceptable to some people with COPD as an alternative to centre-based pulmonary rehabilitation.
Keywords: Pulmonary disease, chronic obstructive, rehabilitation, home care services, motivational interviewing, qualitative research
Background
Chronic obstructive pulmonary disease (COPD) is characterised by dyspnoea upon exertion, physical limitations and chronic cough.1 Due to its progressive nature, COPD significantly impacts on exercise capacity,2 quality of life and mental well-being.3 In order to enhance exercise tolerance and reduce symptoms, strong evidence suggests that patients with COPD should undertake pulmonary rehabilitation (PR).4 Typically, outpatient PR is held at a health facility for a period of 6–8 weeks where biweekly sessions are run with supervision and feedback from healthcare professionals (HCPs).4 Although centre-based PR has outstanding effects on COPD outcomes,5 there are various well-documented barriers to uptake, attendance and completion of PR.6 Patient-related factors include travel burden, inconvenience in time and lack of perceived benefits.7,8
Home-based PR (HBPR) is an alternative model that has been shown to produce equivalent clinical outcomes to centre-based PR.9 Other studies of different HBPR models reported quantitative results that were similar to those produced by centre PR.10,11 However, the patient’s perspective regarding HBPR has not been documented. It is also unclear whether patients undergoing HBPR feel they receive adequate social support, which may have a critical impact on PR outcomes.12 This qualitative study aimed to report the perspective of patients who undertook HBPR.
Methods
Participants
All participants underwent an 8-week HBPR programme as part of the HomeBase trial. The HomeBase trial was a large multicentre randomised controlled trial (RCT) that examined clinical outcomes of HBPR in people with COPD.9 Eligibility criteria for participants included a confirmed diagnosis of COPD,1 at least 40 years of age and a smoking history of 10 pack years or more.
Following assessment, the HBPR programme was initiated with a home visit by a physiotherapist to discuss exercise goals, provide an exercise prescription and supervise the first session. Participants were encouraged to work towards a goal of at least 30 minutes of whole-body exercise on most days of the week and were provided with an exercise diary and a pedometer to document participation and goals. The home visit was followed by seven weekly phone calls from a physiotherapist. Using principles of motivational interviewing,13 the physiotherapist discussed exercise goals and delivered the self-management educational component of HBPR. Further information on the HBPR model utilised in the HomeBase trial is published separately.9
After ethics approval to conduct the interviews was received, consecutive home participants were asked whether they were interested in undertaking a short interview to report their perspective on undertaking home-based PR. Consenting participants undertook the interviews during the last week of rehabilitation, either in their own homes or through telephone calls as per their convenience.
Interviews
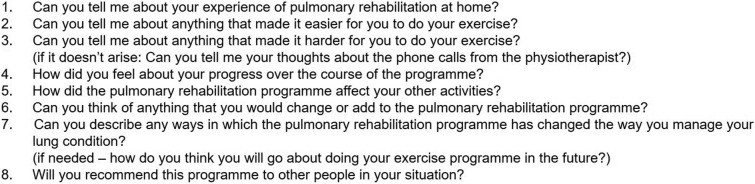
Semi-structured interviews with open-ended questions were designed to understand the perspectives of patients on HBPR (Box 1). The interviews were conducted based on principles of deductive thematic analysis.14 This approach obtained an in-depth exploration of viewpoints and feedback on the HBPR model. Questions explored possible facilitators and barriers to adherence to different HBPR components. Personal perspectives regarding the setting and design were also explored. Additionally, narrow questions regarding the programme’s impact on disease management, current daily activities and future exercise planning were set to explore broader aspects of the HBPR experience from participants’ perspective.14 Interviews were conducted by two authors (AL and AH) who had not been involved in delivery of the intervention. All interviews were audiotaped and transcribed verbatim, with transcripts checked for accuracy by a research assistant.
Box 1. Interview questions.
Data analysis
All de-identified transcripts of the interviews were analysed by two researchers independently, one with 15 years of experience conducting PR (AH) and a second with 3 years (AL). Deductive thematic analysis was used due to its flexibility and ability to identify patterned meaning based on reflective data.15 Line-by-line coding was performed and descriptive codes were generated to represent the data.14 Related codes were collapsed into defining subthemes. Constant comparisons were used to compare codes and categories with new transcribed data.16 The researchers then agreed on major themes based on theoretical associations between subthemes. Any disagreement was resolved by discussions. Participants’ verbatim quotes were extracted from the transcripts to provide supportive data for subthemes. Data collection ceased when data saturation was reached.17 Data saturation was reached after 10 interview transcripts were coded, when no more themes were emerging from the data set.18 Three additional interviews were conducted to confirm saturation.
Results
Invitations to participate in interviews commenced in August 2013 and data collection ceased in March 2014. A total of 14 participants were invited to participate in this study and 13 participants agreed to take part. One potential participant chose not to participate in the interview due to personal reasons unrelated to the study or the intervention. Participant demographics are presented in Table 1. Twelve interviews were conducted face-to-face and one was carried out through the telephone. Box 2 summarises major themes and subthemes derived from the interviews.
Table 1.
Demographic characteristics of interviewed participants.
| Participant code | Gender | Age (years) | Smoking | Pack years | FEV1 (l) | FEV1% predicted | Completed centre PR before | Baseline 6MWD | Baseline mMRC | Post home PR 6MWD | Post Home PR mMRC | Completed home PR | Number of completed home PR sessions (total of eight) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 66 | Current | 48 | 1.00 | 44 | N | 435 | 1 | 475 | 1 | Y | 8 |
| 2 | Female | 57 | Quit | 40 | 0.85 | 34.8 | N | 525 | 1 | 575 | 2 | Y | 7 |
| 3 | Male | 73 | Quit | 33 | 1.04 | 36 | Y | 478 | 1 | 505 | 1 | Y | 8 |
| 4 | Female | 74 | Quit | 80 | 1.15 | 63 | N | 410 | 1 | 428 | 1 | Y | 8 |
| 5 | Female | 75 | Quit | 38 | 0.97 | 48 | N | 271 | 3 | 383 | 3 | Y | 8 |
| 6 | Female | 73 | Quit | 25 | 1.45 | 70 | N | 535 | 1 | 570 | 1 | Y | 8 |
| 7 | Female | 65 | Quit | 18 | 0.81 | 39 | N | 463 | 2 | 455 | 1 | Y | 8 |
| 8 | Female | 68 | Quit | 40 | 1.90 | 91 | N | 585 | 1 | 635 | 0 | Y | 7 |
| 9 | Male | 66 | Current | 42 | 2.28 | 68 | N | 546 | 1 | 668 | 1 | Y | 8 |
| 10 | Male | 49 | Current | 40 | 1.00 | 25 | N | 528 | 1 | 582 | 1 | Y | 8 |
| 11 | Female | 69 | Quit | 25 | 0.82 | 42 | N | 552 | 2 | 579 | 1 | Y | 8 |
| 12 | Female | 67 | Quit | 15 | 1.73 | 85 | N | 551 | 0 | a | 0 | Y | 7 |
| 13 | Female | 61 | Quit | 15 | 2.22 | 84 | N | 539 | 1 | 576 | 1 | Y | 8 |
FEV1: forced expiratory volume in 1 s; 6MWD: 6-minute walk distance; mMRC: modified Medical Research Council Dyspnoea Scale; PR: pulmonary rehabilitation; Y: yes; N: no.
aMissing data.
Box 2. Themes and subthemes associated with the experience of undertaking HBPR.
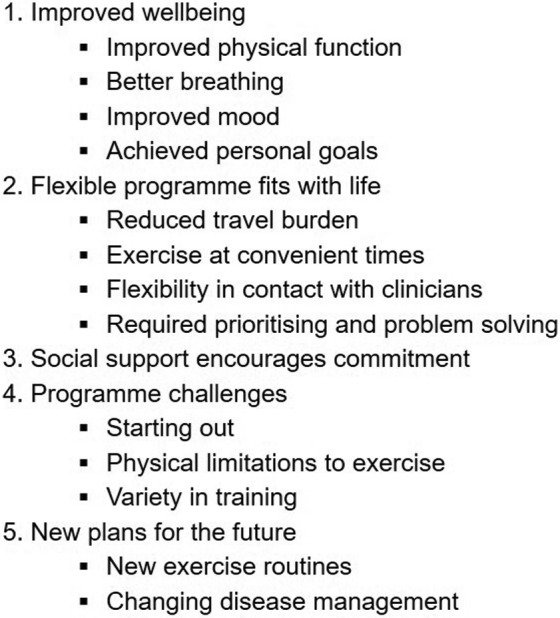
Theme 1: Improved well-being
Participants reported a positive impact on their physical function, symptoms and mood.
Improved physical function
Many described that, as a result of participation in HBPR, they perceived improvement in their symptoms and therefore were now able to undertake activities that had not previously been possible.
I found walking up hills…whereas, you know, before you get just about exhausted when you get to the top of the hill, whereas, now I can sort of keep walking. (p. 10)
Some participants were able to explore their new capabilities and enhanced physical function through participating in new activities.
I was able to go for a bush walk with friends and be able to talk as well as walk!…and keep up and they weren’t waiting for me so that was fantastic. That showed me clearly how much better I am! (p. 02)
Better breathing
Many participants had developed strategies to cope with breathlessness and were more confident in managing their symptoms. Better breathing control had also helped participants build confidence while exercise training and walking.
Well, I can walk a bit further now and I am thinking to myself ‘Breathe! Breathe! You can do it!’ so I talk to myself down the street. I am going a bit better with my breathing. (p. 07)
Improved mood
The majority of participants felt that completion of HBPR had improved their mood and provided hope. Engaging in new activities and noticing improvements helped them aspire to a better lifestyle.
I was sitting on the couch there for a while, a little too much, but now physically and mentally I am in a better state. (p. 11)
Achieved personal goals
Personal goals had functioned as motivators to help commit to HBPR, in particular to exercise. This was highlighted by a participant with multiple comorbidities:
…and doing the walking every day or attempting to walk every day is really good for the chronic fatigue also and for my osteoporosis as well as my emphysema so it has been great and I have noticed lots of small changes in my walking. (p. 02)
Theme 2: Flexible programme fits with life
The value of HBPR flexibility and convenience was a strong emerging theme. Participants reported a number of programme features that made participation accessible and feasible.
Reduced travel burden
Many participants perceived that attending centre-based PR would have been difficult due to burdens of using public transport and/or costs of travel. Participants felt that these burdens may have limited their ability to attend a centre-based programme.
See, I’m close to the hospital but it takes a hell of a lot to get there by public transport! You know, and then if you miss the tram you’ve got to wait twenty minutes for another one and I wouldn’t drive over because the parking is too hard to get and if you park in the car park it will cost you a small fortune. (p. 04)
Exercise at a convenient time
All participants pointed to the flexibility of training and the advantages of doing exercises at a time convenient for them. Flexibility in training time was perceived to encourage their commitment to an exercise routine.
To do walking just in my own time where I can fit it in is much more establishing, something that I can keep on doing. (p. 02)
Exercising at home allowed participants to proceed with daily routines without significant alterations caused by attending a twice-weekly hospital-based programme. Less interruption to daily activities had led some participants to develop time management and exercise prioritisation techniques.
When I have doctors’ appointments and I do volunteer work once a fortnight, I just work around it and make sure I do my exercises before I go or when I come home when it’s an early appointment. (p. 05)
Flexibility in contact with the physiotherapist
Participants had a regular weekly time for their telephone call with the physiotherapist, but appreciated that HBPR allowed some flexibility. Effective communication through telephone calls was perceived to have increased participants attendance.
The contact with people was very good, I mean they are very polite and a couple of times I had to be late so I rang up and they worked in with me so that has been no stress; so that is very good. (p. 11)
Weekly contact with the physiotherapist had allowed them to receive timely, personalised advice regarding their programme.
She (the physiotherapist) is very informative! She taught me over the phone as far as breathing exercises go. More so, she told me how to relax myself properly before I breathe. (p. 06)
Required prioritising and problem-solving
Although participants appreciated the flexible HBPR programme model, some participants mentioned that personal factors including social commitments, weather and prioritisation of activities affected their commitment to HBPR.
I just get tired! I am tired now because I have been up early every day this week. And I haven’t had a chance, I’ve had visitors and gone out. (p. 04)
However, other participants reported problem-solving and planning had helped so that they could participate in HBPR regardless of personal commitments or health status.
…But I have been doing the exercises, some days I have missed but the other days I have made up for more. (p. 03)
Yes! I get a little bit puffy in the mornings, so I do them in the afternoons. (p. 07)
Theme 3: Social support encouraged commitment
One of the positive features of HBPR was the regular contact with physiotherapists who provided social support and showed special interest in participants’ lives which was possible through one-on-one interactions.
I feel quite comfortable talking to her, she is quite easy to talk to! It is not only about the programme, she asks me about myself and how I am coping with family. (p. 12)
Many participants spoke of the support that they had received from friends and family who witnessed their participation in HBPR and saw their improvement over time. One participant felt very proud when a friend acknowledged his new capabilities.
Well my friend over there knows that I can walk so much further now! (p. 03)
Others enjoyed having new opportunities to go outdoors to perform their exercise and engage in casual conversations with strangers. Connection with people and nature appeared to have positive impact on well-being and commitment.
I found that it was lovely to just walk past gardens and, you know, just see what is going on around and even people will speak with you, you know. It just cheers you up for the day and you look at life differently. (p. 08)
Although the overwhelming majority of participants perceived the social support received through the programme to be sufficient, one participant felt that HBPR would have been easier with more direct supervision and peer support in a group environment.
I think it (the supervision) gives you that sense that you can do it and you can do it a bit more because I think when you are at home you think ‘Oh I can’t be bothered with it’, It gives you a bit more fun to do it with the people. (p. 07)
Theme 4: Programme challenges
Participants identified minor challenges encountered when undertaking HBPR.
Starting out
A number of participants reported that it was challenging to adapt to daily exercises when they first initiated HBPR due to their prolonged sedentary lifestyle.
The first two weeks. I couldn’t get my head around it because I haven’t exercised before and I had to put myself out which is something that I’ve never really had to do. (p. 08)
Physical limitations to exercise
Some participants reported physical limitations that significantly affected their ability to exercise.
Well, the upper body (exercises) I’ve only done one because I have a spinal fusion in the neck so I did not do too much then because I don’t want to push that. (p. 13)
Variety in training
Some participants reported that having a similar daily exercise routine was a challenge to their engagement and commitment.
Probably a bit more variations I think! It gets a bit boring when you do the same every time so you split up like you might go on the bike this time and then you do your weights and then the next time you walk on the walking machine. (p. 07)
Theme 5: New plans for the future
Participants reported that HBPR had a long-term effect on their lives and future plans.
New exercise routine
The majority of participants pointed out that HBPR had helped in establishing a new exercise routine. Having a clear understanding of their exercise plan had helped participants take with long-term continuation.
When I finish the programme, I can continually keep walking which I do like to walk anyway so that is not going to be an issue. (p. 11)
Changing disease management
Participants also reported that HBPR had improved their disease management skills. Many participants explained their new way of managing exacerbations.
Before I would leave it for a week and I’d think I will get better but I know I don’t. So when it does flare up, nip it in the bud straight away and get onto the antibiotics and do the right thing. (p. 03)
Discussion
This study documents qualitative data about participants’ perspectives regarding their experience of HBPR. Reported results showed that there are multiple perceived benefits to this model. Participants described improvements in well-being through enhancement to physical and psychological status. Many participants disclosed that HBPR helped them feel stronger and achieve personal goals. Time-convenience and flexibility in training were strongly highlighted as essential features of HBPR. The programme design facilitated access to social support which provided motivation to participants. Although challenges were faced throughout HBPR, many participants had actively engaged in problem-solving and prioritising to enable continued participation.
A previous qualitative study analysing the barriers to uptake and completion of centre-based PR found that difficulties in transportation and cost of travel made attendance challenging.8 Disruption of established routines was also highlighted as a barrier to completion.19,20 Another qualitative study showed that the main barriers to participation in exercise were either environmental, including weather and distance, or personal, such as physical factors and boredom.21 Recommendations from previous studies entailed the development of a more flexible and equivalent programme model that facilitates accessibility and overcomes well-reported barriers. The perspectives of participants in this study suggest that HBPR can overcome many of these barriers in the short term and provide additional perceived benefits to people with COPD.
Previous studies of HBPR demonstrated effectiveness and equivalence to centre-based PR. A systematic review of 18 RCTs published in 2014 showed that HBPR significantly improved health-related quality of life and exercise tolerance with the recommendation of developing larger scale RCTs to provide robust conclusions.11 A recently published large RCT reported that HBPR improved exercise capacity and dyspnoea-related quality of life in people with COPD.9 Although HBPR appears to show promise, it is not yet widely available for patients nor clinically accepted. Our findings revealed that, according to patients’ perspectives, HBPR is acceptable, convenient and provides multiple perceived benefits. This may stimulate exploration of funding models which could make HBPR accessible for COPD care.
Although it is strongly believed that group-based PR provides social support among patients, this report showed that participants in HBPR also experienced support from various sources including friends, family and neighbours. Most patients found receiving support, motivation and education from the clinician over the telephone-facilitated adherence to this largely unsupervised programme. However, it must be acknowledged that some patients prefer a supervised group setting for support as indicated by one patient in the study. Despite this, remote interactions between HCP and patients are widely implemented. A recent qualitative analysis of the interaction stated that remote communication can be efficient and satisfying.22 Given the limited evidence in this area, future research should explore the effects of such communications through modern tele-healthcare interventions.
‘Starting out’ was one of the challenges faced during HBPR. Participants found it problematic to commence exercise after being prone to a relatively sedentary lifestyle.23 A similar theme was reported in a qualitative study documenting the experience of undergoing a hospital-based PR.24 Through a focus group of HCP and COPD patients, patients reported their tendency to rely on HCPs to keep them active and committed.24 However, themes emerging from HCPs implied that it is challenging to motivate patients to exercise. They reported that motivation often depends on providing clear reasons for different activities and acknowledging patients’ interests. HCPs also disclosed that motivation would increase if PR was set according to patients’ goals rather than professionals’ goals for patients. This is consistent with the principles of motivational interviewing utilised by the physiotherapist conducting telephone calls in HBPR which assist patients to find their own motivation to exercise and promote adoption of long-term active lifestyles.13
One of the main features of HBPR was its contribution to establishing a prolonged exercise routine. Many participants reported they had established a routine during HBPR that they were committed to proceeding with. This intention for ongoing exercise might indicate that HBPR can successfully promote long-term continuation of exercise training. However, this was not borne out in the larger trial, where improvement in exercise capacity and objectively measured physical activity were not sustained after 12 months of either home or centre-based PR.9 Further research is needed to establish whether embedding an exercise routine in daily life through HBPR could result in long-term gains in physical activity.25
Strengths and limitations
This is the first study to discuss the perspective of patients with COPD regarding their experience of HBPR. A strength of this research is that two researchers performed the analysis separately, then discussed their results to obtain consensus. Our findings explore participants’ views on future exercise plans and disease management, which documents perceptions regarding the new model’s impact on patients’ habitual activities. It should be acknowledged that despite the positive perceptions regarding future plans, this was not consistent with the lack of long-term (12 month) maintenance of benefits seen in the larger trial.9 Other weaknesses include the absence of perspectives of those who may not have chosen to undertake HBPR. In the RCT from which this sample was drawn, 54 people declined participation because they preferred a centre-based programme.9 To comprehensively understand various perspectives regarding HBPR, the views of those who did not complete the programme or declined participation should be explored.
Conclusion
In conclusion, this qualitative study suggests that HBPR is acceptable to people with COPD and may overcome some of the well-documented barriers to participation in centre-based PR. Participants reported that HBPR was convenient and fitted in with their lives. It also resulted in perceived health benefits in managing life with disability. Moreover, bringing PR from the hospital into the home made it easier and more accessible. Given the clinical benefits of HBPR and its acceptability to patients, consideration should be given to whether HBPR can be routinely incorporated into clinical care.
Acknowledgements
The authors would like to thank all the trial participants for taking part in this interview-based research.
Authors’ note: This is a sub-study of the HomeBase trial (cited in the manuscript).
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The HomeBase trial was funded by Lung Foundation Australia and the National Health and Medical Research Council in Australia under project grant 1046353.
References
- 1. Cox NS, Oliveria CC, Lahham A, et al. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the theoretical domains framework. J Physiother 2017; 63(2): 84–93. [DOI] [PubMed] [Google Scholar]
- 2. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. A statement of the American Thoracic Society and European Respiratory Society. Am J Resp Crit Care Med 1999; 159: S1–S40. [DOI] [PubMed] [Google Scholar]
- 3. Bratek A, Zawada K, Beil-Gawełczyk J, et al. Depressiveness, symptoms of anxiety and cognitive dysfunctions in patients with asthma and chronic obstructive pulmonary disease (COPD): possible associations with inflammation markers: a pilot study. J Neural Transm 2015; 122: 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Resp Crit Care Med 2013; 188: e13–e64. [DOI] [PubMed] [Google Scholar]
- 5. McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2: CD003793 Resource: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003793.pub3/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Johnston K, Grimmer-Somers K. Pulmonary rehabilitation: overwhelming evidence but lost in translation? Physiother Can 2010; 62: 368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chronic Respir Dis 2011; 8: 89–99. [DOI] [PubMed] [Google Scholar]
- 8. Keating A, Lee AL, Holland AE. Lack of perceived benefit and inadequate transport influence uptake and completion of pulmonary rehabilitation in people with chronic obstructive pulmonary disease: a qualitative study. J Physiother 2011; 57: 183–190. [DOI] [PubMed] [Google Scholar]
- 9. Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: a randomised, controlled equivalence trial. Thorax 2017; 72(1): 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dias FD, Sampaio LM, da Silva GA, et al. Home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized clinical trial. Int J Chron Obstruct Pulmon Dis 2013; 8: 537–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu XL, Tan JY, Wang T, et al. Effectiveness of home-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: a meta-analysis of randomized controlled trials. Rehabil Nurs 2014; 39: 36–59. [DOI] [PubMed] [Google Scholar]
- 12. Young P, Dewse M, Fergusson W, et al. Respiratory rehabilitation in chronic obstructive pulmonary disease: predictors of nonadherence. ERJ Open Res 1999; 13: 855–859. [DOI] [PubMed] [Google Scholar]
- 13. Rollnick S, Miller WR, Butler CC, et al. Motivational interviewing in health care: Helping patients change behavior. COPD J 2008; 5: 203–203. [Google Scholar]
- 14. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 15. Kohlbacher F. The use of qualitative content analysis in case study research. Forum Qualitative Sozialforschung / Forum: Qualitative Social Research 2006; 7 (1). [Google Scholar]
- 16. Suter WN. Introduction to educational research: A critical thinking approach. Thousand Oaks, US: SAGE, 2012, p. 528. [Google Scholar]
- 17. Walker JL. The use of saturation in qualitative research. Can J Cardiovasc Nurs 2012; 22: 5. [PubMed] [Google Scholar]
- 18. O’Reilly M, Parker N. ‘Unsatisfactory Saturation’: a critical exploration of the notion of saturated sample sizes in qualitative research. Qual Res 2013; 13: 190–197. [Google Scholar]
- 19. Alsubaiei M, Cafarella P, Frith P, et al. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann Thorac Med 2016; 11: 121–127. Original Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fischer MJ, Scharloo M, Abbink JJ, et al. Participation and drop-out in pulmonary rehabilitation: a qualitative analysis of the patient’s perspective. Clin Rehab 2007; 21: 212–221. [DOI] [PubMed] [Google Scholar]
- 21. O’Shea SD, Taylor NF, Paratz JD.…But watch out for the Weather: factors affecting adherence to progressive resistance exercise for persons with COPD. J Cardiopulm Rehabil Prev 2007; 27: 166–174. [DOI] [PubMed] [Google Scholar]
- 22. Dinesen B, Andersen SK, Hejlesen O, et al. Interaction between COPD patients and healthcare professionals in a cross-sector tele-rehabilitation programme. Stud Health Technol Inform 2011; 169: 28–32. [PubMed] [Google Scholar]
- 23. Pitta F TT, Spruit MA, Probst VS, et al. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Resp Crit Care Med 2005; 171: 972–977. [DOI] [PubMed] [Google Scholar]
- 24. Meis JJ, Bosma CB, Spruit MA, et al. A qualitative assessment of COPD patients’ experiences of pulmonary rehabilitation and guidance by healthcare professionals. Respir Med 2014; 108: 500–510. [DOI] [PubMed] [Google Scholar]
- 25. Lahham A, McDonald CF, Holland AE. Exercise training alone or with the addition of activity counselling improves physical activity levels in COPD: a systematic review and meta-analysis of randomized controlled trials. Int J Chron Obstruct Pulmon Dis 2016; 11: 3121–3136. [DOI] [PMC free article] [PubMed] [Google Scholar]


