Abstract
Introduction
Many studies suggest that Tai Chi exercise is a safe and appropriate mind-body exercise for older people and effectively slows down age-related cognitive decline. A set of bespoke Tai Chi exercise named ‘Cognition Protecting Tai Chi’ (CPT) has been created for older people with cognitive impairments by the research team of geriatricians, neurologists, rehabilitation specialists, experts of sports medicine and experienced practitioners of traditional Chinese medicine. This trial is designed to evaluate its effects on cognitive function, behaviour/moods, risk of falls and activities of daily living of the participants with mild dementia.
Methods and analysis
A randomised controlled study will be conducted. Eighty participants with mild dementia will be recruited and randomly allocated to an intervention group and a control group. The intervention group will practice the CPT exercise three times a week for 20 min each time under the guidance of professional therapists. The control group will continue receiving their routine treatments. The duration of this study will be 10 months. All participants will be assessed with a battery of neuropsychological and functional evaluations, which include Mini Mental State Examination, Montreal Cognitive Assessment, the WHO-University of California Los Angeles-Auditory Verbal Learning test (WHO-UCLA-AVLT), Trail Making Test (TMT), Geriatric Depression Scale, Neuropsychological Inventory and Barthel Index, at the baseline, 5 and 10 months during the study period. Fall incident will also be recorded. The primary outcome will be the WHO-UCLA-AVLT delayed recall score. The secondary outcome will be the TMT score.
Ethics and dissemination
This study has been approved by the ethical review committee of the Beijing Geriatric Hospital (protocol number: 2015–021). Informed consent will be obtained from all participants or their guardians. The authors intend to submit the findings of the study to peer-reviewed journals or academic conferences to be published.
Trial registration number
ChiCTR-INR-16009872; Pre-results.
Keywords: dementia, Tai Chi, cognitive function
Strengths and limitations of this study.
The bespoke Cognition Protecting Tai Chi is specially designed for older people with mild dementia by the research team of multidisciplinary professionals.
The randomised controlled trial design minimises the risk of selection bias.
As the sample size is calculated based on the primary outcome, this study may fail to demonstrate statistical differences of secondary outcomes.
An open-label study design is often viewed as leaning towards bias; however, it is not feasible to achieve a blinded intervention for this study.
Introduction
There are various clinical symptoms of people with dementia, which usually start with cognitive impairments, such as memory loss, and then complaints of inattention, miscalculation, lack of logical reasoning and disorientation.1 Besides cognitive impairments, people with dementia may also experience some changes psychologically and physically. There might be changes in personality, mood swings, ability to communicate and behaviours. It is often observed that patients with dementia feel anxious, depressed and may become verbally and physically aggressive. As the disease progresses, these symptoms gradually affect their ability in maintaining their activities of daily living, which leads to loss of independence. Current pharmacological interventions used to maintain cognitive function, such as acetylcholinesterase inhibitors and memantine, have limited efficacy, and there are usually side effects.2–5 Meanwhile, typical and atypical antipsychotics for dementia have the same or even severe side effects.
According to neuroplasticity theory, the repetition of stimulate-reflect training can help patients with dementia in preservation and restoration of brain functions, even when the brain has pathological damage to some extent.6 There has been a considerable focus on the non-pharmacological approach to enhancing cognition. Many studies suggest that mind-body exercise can efficiently prevent the onset of dementia by delaying age-related cognitive decline, and benefit the prognosis of dementia.7–10
As one of traditional Chinese martial arts, Tai Chi is an aerobic mind-body exercise with mild-to-moderate physical movements that are safe for older people.11 Tai Chi requires mind concentration and shifting the balance of body in accordance with gentle and smooth movements and steady breathing. In the theory of traditional Chinese medicine, Qi (Qi is one of the fixed technical terms in traditional Chinese medicine, referring to behavioural patterns seen to occur through the spatial extension of a physical medium, which is both activity and active substance) and blood are the two most fundamental materials to maintain human life activities. Qi and blood can both be mobilised coordinately when practising Tai Chi, which helps maintain the balance of Yin and Yang (the two opposite properties of all natural things in traditional Chinese medicine) and improves harmony of human body.12 As the nature of Tai Chi exercise strengthens the muscles of lower limbs of the body, it helps improve stability and minimise the risk of falls.11 Tai Chi is a recommended exercise for fall prevention in older people by the American Geriatrics Society, because it improves muscular strength, coordination and balance, and is an enjoyable activity with a potential as a long-term exercise regime.13 A randomised trial in older Chinese people without dementia carried out by Mortimer et al suggest that Tai Chi increases brain volume and improves cognitive function more effectively than the intervention of social interaction.14 Evidence has also shown that Tai Chi is an appropriate exercise for individuals with dementia in early stages, which helps improve quality of life, brain function inducing reconstruction of neurons and Tai Chi could become an emerging alternative therapy for people with dementia.15–17 Other studies reported that physical exercise like Tai Chi improved mood and alleviated psychiatric problems in early or middle stages of dementia and also significantly reduced caregiver distresses.18 For example, Sticky Hands Tai Chi, a special Tai Chi training technique practised with a partner, promoted a comforting intimate interaction between the two persons and improved exercise adherence and mood in older people with dementia.15
China has the largest number of older people with dementia19 and Tai Chi is originated from China. Tai Chi experts in China have developed various programmes of Tai Chi, but none is especially designed for older people with cognitive impairments. Therefore, a set of Tai Chi programme named ‘Cognition Protecting Tai Chi’ (CPT) has been designed by the research team of multidisciplinary professionals in the first stage of this study. The second stage of this study is to test the effectiveness of the CPT programme in improving cognitive function, and to evaluate its effects and impacts on psychological behaviour, mood swings, risk of falls and ability in maintaining activities of daily living for people with mild dementia with comparison to usual care. If results are positive, it would demonstrate the potential to become a routine cost-effective exercise for older people with mild dementia.
Methods
Settings
This study is designed at Center for Cognitive Disorders of Beijing Geriatric Hospital (BGH). The Case Report Forms will be kept and research data will be analysed by BGH. This hospital is a tertiary hospital, which is the highest rank in China’s hospital system in terms of capacity of beds and research capability. BGH has 900 inpatient beds and is located in Haidian District of Beijing. The Center for Cognitive Disorders of BGH is a department serving older people with cognitive impairments. It is also the Guidance Center for Cognitive Rehabilitation of Haidian District. The recruitment, assessment, intervention and follow-ups of participants will be conducted at three long-term care facilities near BGH where the participants reside.
Study design
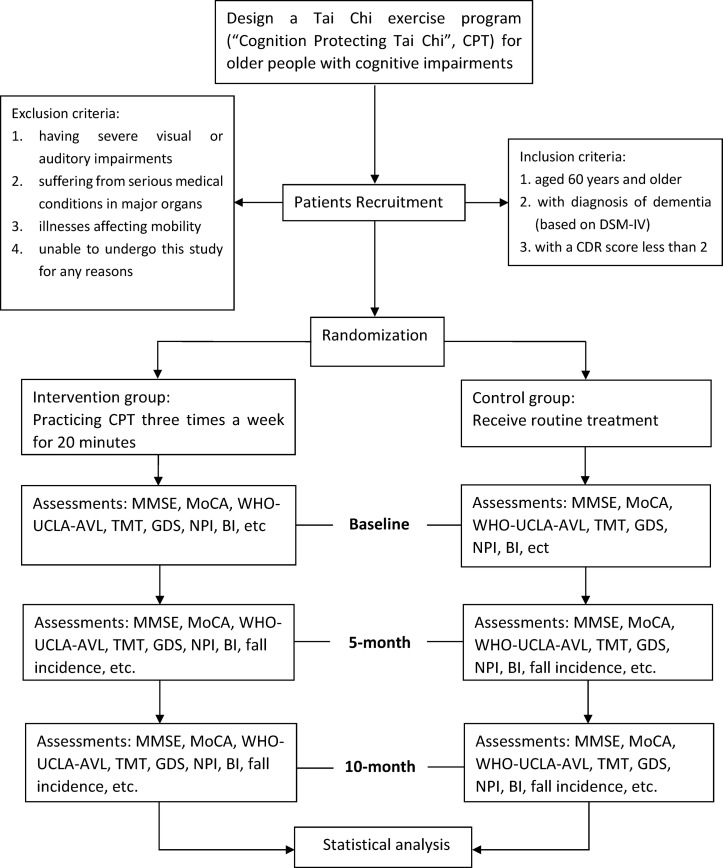
There are two stages in this study design (figure 1).
Figure 1.
Trail flow chart. BI, Barthel Idex; CDR, Clinical Dementia Rating; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; GDS, Geriatric Depression Scale; MMSE, Mini Mental State Examination; MoCA, Montreal Cognitive Assessment; NPI, Neuropsychiatric Inventory; TMT, Trail Making Test; WHO-UCLA-AVLT, WHO-University of California Los Angeles Auditory Verbal Learning test.
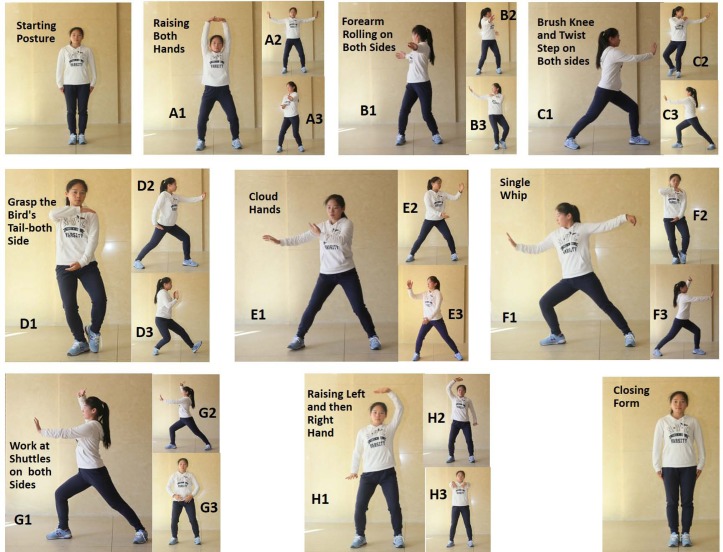
The first stage is the development of the CPT programme by the research team. The CPT programme was specifically designed for cognitively impaired patients by a research team of geriatricians, neurologists, rehabilitation specialists, experts of sports medicine and experienced practitioners of traditional Chinese medicine in 2016. The team has modified the traditional Chinese Tai Chi to suit people with mild dementia. Any unsafe and complex actions in the traditional eight style Tai Chi programme was removed, and some movements which were thought to be more beneficial for cognitive functions were added based on theories of traditional Chinese medical science. For example, the researchers removed the posture of standing on one foot and added some movements of rotating wrists and fingers in consideration of the suitability and safety aspects of the programme for people with dementia. The CPT programme contains eight styles of Tai Chi movements and each movement can be divided into three different manoeuvres. Between January 2017 and May 2017, the CPT has been performed in five patients with mild dementia who were invited to learn and practice the CPT programme for 4 weeks. The CPT has been further modified where necessary based on the comments and the feedback provided by the participants before the completion of final version of the CPT.
In addition to routine Starting Posture and Closing Form, there are eight styles of Tai Chi movements in the CPT, including raising both hands, forearm rolling on both sides, brush knee and twist step on both sides, grasp the bird’s tail-left side and then right side, cloud hands, single whip, work at shuttles on both sides and raising left and then right hand (figure 2).
Figure 2.
Main movements of the ‘Cognition Protecting Tai Chi’ (CPT). A1–A3: raising both hands. B1–B3: forearm rolling on both sides. C1–C3: brush knee and twist step on both sides. D1–D3: grasp the bird’s tail—left side and then right side, cloud hands. E1–E3: cloud hands. F1–F3: single whip. G1–G3: work at shuttles on both sides. H1–H3: raising left and then right hand.
The second stage is a randomised controlled trial, which will be conducted to test the effectiveness of the CPT programme.
Recruitment of participants
Participants will be recruited from long-term care facilities near BGH. These facilities are Wenquan nursing home, Lengquan nursing home and Hexihui nursing home. There are altogether >1000 older residents living in these nursing homes, thus sufficient samples can be provided. Residents who meet the inclusion criteria will be recruited.
Inclusion criteria
Residents aged 60 years or older with mild dementia (diagnosis is based on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition), who have a Clinical Dementia Rating score <2 will be enrolled into this study.
Exclusion criteria
Residents who have severe visual or auditory impairment, serious medical conditions in major organs (such as heart, lung, kidney, liver and so on), illnesses affecting mobility or are unable to accept assessments or interventions that are required in this study for any reasons.
Randomisation and allocation sequence
Participants will be enrolled by dementia specialists. The randomisation will be carried out by an independent research assistant who will not be involved in the enrolment, assessment or intervention of the participants. Random number sequences will be generated using SAS V.9.4 software. Sealed envelopes with the serial number outside and group number inside will be produced and kept in a locked drawer which will be inaccessible to all the researchers. The envelopes will be opened sequentially by the independent research assistant after baseline assessments and participants will be assigned to two groups (ie, one intervention group and one control group) at a ratio of 1:1 according to the group number printed inside the envelopes. Outcome evaluators and data analysts will be blinded to the group assignment.
Intervention
This study is designed as a 10-month-randomised controlled trial. In addition to their routine treatment and usual care for ADL, the intervention group will practice the CPT exercise three times a week for 20 min each time under the guidance of the professional therapists at where the participants reside. The intervention will be practised in groups with one therapist to five to eight participants. The control group will only receive routine treatments and usual care for ADL. The intervention to the participant should be discontinued if any complication that could affect the outcomes of the CPT occurs. The participants will be encouraged to complete follow-ups. The participants and their representatives have access to the research team anytime if they need to discuss any issues or concerns during the study period. The participants will be explained that they can discontinue with the intervention at any time during the period of the study. Demographic information of participants who withdraw from the study after randomisation and the reasons for their withdrawal will be collected.
Assessment
The trial will use the most commonly used tools (see below) that have been carefully selected to assess the efficacy of CPT. The Chinese version of Mini Mental State Examination (MMSE)20 is a 30-point questionnaire, which is used to measure cognitive impairments. It examines functions of attention, calculation, recall, language, ability to follow simple commands and orientation.
The Montreal Cognitive Assessment (MoCA) Beijing version (www.mocatest.org) is also a 30-point test for assessing cognitive function. MoCA includes cognitive domains for short-term memory recall, visuospatial abilities, multiple aspects of executive functions, attention, concentration and working memory, language and orientation to time and place. Because there are more difficult and multiple tasks in MoCA, MoCA is more sensitive to detect mild cognitive changes than MMSE does.21
The WHO-University of California Los Angeles-Auditory Verbal Learning test (WHO-UCLA-AVLT)22 is a tool to assess immediate recall and delayed recall with 15 words independent in meaning. Immediate recall is performed by asking the participants to remember and recall those 15 words just after each auditory learning, and this learning-recall process is repeated for three times to generate an average performance score. An average performance is recorded. Delayed recall is performed by asking the participants to recall those 15 words 30–45 min after the immediate recall has been completed.
The study uses the method of the Trail Making Test (TMT), which is a neuropsychological test of visual attention and task switching. It can provide information on visual search speed, scanning, speed of processing, mental flexibility as well as executive functioning. A Chinese version of Shape TMT was used in this study. This Shape TMT shows numbers from 1 to 25 twice, once in a circle and once in a square. The participants are asked to connect them in sequential order alternately between circles and squares (circle 1, square 1, circle 2, square 2, etc).23 This Shape TMT has been proved to be a sensitive test of visual search and sequencing.24
The Geriatric Depression Scale (GDS)25 is a 30-item self-report assessment used to identify depression in the elderly, of which questions are answered in a ‘yes’ or ‘no’ format. It is appropriate to test older individuals with mild or moderate cognitive impairment using GDS.
The Neuropsychiatric Inventory26 assesses common psychiatric and behavioural symptoms in dementia. Its items include hallucinations, delusions, agitation/aggression, dysphoria/depression, anxiety, irritability, disinhibition, euphoria, apathy, aberrant motor behaviour, sleep and night-time behaviour disturbance, appetite and eating disorders. Information can be obtained from caregivers who have in-depth knowledge of the patients’ performance. The caregivers will also be asked to rate their own distress level associated with daily care and support provided by them to the patients.
The Barthel Idex27 is an ordinal scale used to measure performance in ADL. The 10 variables describing ADL and mobility addressed in the Barthel scale are: presence or absence of faecal incontinence, urinary incontinence, grooming, toileting, feeding, transferring (eg, from chair to bed), walking, dressing, climbing stairs and bathing. The scoring is based on information provided by the participant’s informant, who can be his/her family members or caregivers.
All participants will undergo all above assessments at 0 (baseline), 5 and 10 months within the current study period. Fall incident will also be recorded. Fall will be defined as the experience of a sudden, involuntary, unintentional change of position, down on the ground or on a lower plane. When assessing a definite fall, the team will try to get an eyewitness account or records of security cameras (all the areas of the nursing homes where participants live will be monitored by 24 hours security cameras).
Outcomes
The psychometric tools used in this study will be analysed to assess the efficacy of the CPT. The primary outcome is the WHO-UCLA-AVLT delayed recall score. The secondary outcome is the score of the TMT. The fall incident will be analysed to assess the safety of this Tai Chi programme. Complaints of medical symptoms related to the intervention will be documented and treated when necessary, including fatigue, pain, dizziness and so on.
Sample size
The sample size was calculated by Power Analysis and Sample Size Calculation Statistical Software V.13.0 based on the results of pre-experiment of this study. Using a type I error of 0.05 and a power of 80%, a mean difference of 2 points is expected between two groups after 10 months. The results show a sample size of 34 per groups is adequate for testing the primary outcome (WHO-UCLA-AVLT delayed recall score). Considering a 15% dropout rate, a total number of 80 participants will be recruited.
Quality control and quality assurance
At least three dementia specialists will work together to examine the participants and provide diagnosis for each participant. All data will be monitored and reviewed by the principal investigator or research coordinators. Training will be provided to all researchers. Consistency coefficients in scoring assessment scales between researchers should be no <0.85. Data entry will be verified by a second researcher in the team. To protect participants’ confidentiality, only supervisors, researchers of this study and the ethics committee will be authorised to have access to the personal information and medical records of the participants.
Statistical method
All analyses will be carried out using SPSS V.16.0. The variations of scores of psychometric assessments over time between two groups will be examined using repeated measurement of variance analysis. The association between intervention and incidence of falls will be analysed using χ2 test.
Ethics and dissemination
Information leaflets of the study will be available at the three long-term care facilities. The leaflets explain in full detail the aims and objectives of the study, selection criteria and the processes that the study will be adhering to. The research team will provide an individual face-to-face consultation to all applicants or their guardian to answer any questions they may have. The applicants can then discuss this with their family if they wish and make a decision to opt in or opt out the study prior to signing the consent form. Informed consent will be obtained from all participants or their guardians. The authors intend to submit the findings of the study to peer-reviewed journals or academic conferences to be published.
Patient and public involvement
The original research question and outcome measures were conceived by the authors and were modified based on the face-to-face screening interview with patients and their guardians by a research assistant. Five patients with mild dementia were invited to learn and practice the CPT programme prior to designing the RCT. The CPT was modified based on the comments and the feedback provided by the participants in order to ensure the safety and the applicability of the intervention. Both the burden and the potential benefit of the intervention will be assessed by patients and their advisors before the consent forms are signed. The findings of this study will be made available to the participants and their guardians.
Conclusion
This protocol outlined the objectives of the study and explained the CPT exercise developed by the research team including geriatricians, neurologists, rehabilitation specialists, experts of sports medicine and experienced practitioners of traditional Chinese medicine. The study is designed as a randomised controlled trial in order to evaluate the effects of this especially designed CPT on the participants with mild dementia.
Supplementary Material
Acknowledgments
The authors would like to thank Kai Hao (a staff of Publicity and Education Centre of BGH) for helping to improve the images of this article. The authors would also like to thank all the participants and their advisors for their cooperation.
Footnotes
Contributors: JL conceived the idea and supervised this study and is the guarantor. JL, XR, XC, FL, WL and LW were involved in the design. WL, NH and XR prepared draft manuscript. JL, MC and QX revised the manuscript. WL, ML and XR carried out the statistical calculation. All authors approved submission of this manuscript.
Funding: This work is supported by Beijing Clinical Characteristics Project of Beijing Municipal Science and Technology Commission (Project number Z151100004015023) and Major Clinical Medicine Development Plan of Beijing Municipal Administration of Hospitals (Project number ZYXL201834).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: This study was approved by the ethical review committee of the Beijing Geriatric Hospital (protocol number: 2015–021).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Bassil N, Mollaei C. Alzheimer’s dementia: a brief review. J Med Liban 2012;60:192–9. [PubMed] [Google Scholar]
- 2. Qaseem A, Snow V, Cross JT, et al. Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med 2008;148:370–8. 10.7326/0003-4819-148-5-200803040-00008 [DOI] [PubMed] [Google Scholar]
- 3. Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA 2005;294:1934–43. 10.1001/jama.294.15.1934 [DOI] [PubMed] [Google Scholar]
- 4. Schneider LS, Tariot PN, Dagerman KS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N Engl J Med 2006;355:1525–38. 10.1056/NEJMoa061240 [DOI] [PubMed] [Google Scholar]
- 5. Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry 2006;14:191–210. 10.1097/01.JGP.0000200589.01396.6d [DOI] [PubMed] [Google Scholar]
- 6. Smith GS. Aging and neuroplasticity. Dialogues Clin Neurosci 2013;15:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Collaborating Centre for Mental Health. Dementia: a NICE–SCIE guideline on supporting people with dementia and their carers in health and social care. London: British Psychological Society, 2007. [PubMed] [Google Scholar]
- 8. Cheng ST, Chow PK, Yu EC, et al. Leisure activities alleviate depressive symptoms in nursing home residents with very mild or mild dementia. Am J Geriatr Psychiatry 2012;20:904–8. 10.1097/JGP.0b013e3182423988 [DOI] [PubMed] [Google Scholar]
- 9. Knapp M, Thorgrimsen L, Patel A, et al. Cognitive stimulation therapy for people with dementia: cost-effectiveness analysis. Br J Psychiatry 2006;188:574–80. 10.1192/bjp.bp.105.010561 [DOI] [PubMed] [Google Scholar]
- 10. Orrell M, Spector A, Thorgrimsen L, et al. A pilot study examining the effectiveness of maintenance Cognitive Stimulation Therapy (MCST) for people with dementia. Int J Geriatr Psychiatry 2005;20:446–51. 10.1002/gps.1304 [DOI] [PubMed] [Google Scholar]
- 11. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yuan S. The mechanisms of Tai Chi Traing. Healthcare Science and education 2016;45:38. [Google Scholar]
- 13. Society AG, Society G, Of AA, et al. Guideline for the prevention of falls in older persons. J Am Geriatr Soc 2001;49:664–72. 10.1046/j.1532-5415.2001.49115.x [DOI] [PubMed] [Google Scholar]
- 14. Mortimer JA, Ding D, Borenstein AR, et al. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. J Alzheimers Dis 2012;30:757–66. 10.3233/JAD-2012-120079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yao L, Giordani B, Alexander NB. Developing a positive emotion-motivated Tai Chi (PEM-TC) exercise program for older adults with dementia. Res Theory Nurs Pract 2008;22:241–55. 10.1891/1541-6577.22.4.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Klein PJ. Tai Chi Chuan in the management of Parkinson’s disease and Alzheimer’s disease. Med Sport Sci 2008;52:173–81. 10.1159/000134298 [DOI] [PubMed] [Google Scholar]
- 17. Cheng ST, Chow PK, Song YQ, et al. Mental and physical activities delay cognitive decline in older persons with dementia. Am J Geriatr Psychiatry 2014;22:63–74. 10.1016/j.jagp.2013.01.060 [DOI] [PubMed] [Google Scholar]
- 18. Tai SY, Hsu CL, Huang SW, et al. Effects of multiple training modalities in patients with Alzheimer’s disease: a pilot study. Neuropsychiatr Dis Treat 2016;12:2843–9. 10.2147/NDT.S116257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jia J, Wang F, Wei C, et al. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement 2014;10:1–9. 10.1016/j.jalz.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 20. Wang ZY, Zhang MY, Gy Q, et al. Application of Chinese version of the Mini-Mental State Examination (MMSE). Shanghai Arch Psychiatry 1989;7:108–11. [Google Scholar]
- 21. Lu J, Li D, Li F, et al. Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. J Geriatr Psychiatry Neurol 2011;24:184–90. 10.1177/0891988711422528 [DOI] [PubMed] [Google Scholar]
- 22. Maj M, Satz P, Janssen R, et al. WHO Neuropsychiatric AIDS study, cross-sectional phase II. Neuropsychological and neurological findings. Arch Gen Psychiatry 1994;51:51–61. [DOI] [PubMed] [Google Scholar]
- 23. Zhao Q, Guo Q, Li F, et al. The Shape Trail Test: application of a new variant of the Trail making test. PLoS One 2013;8:e57333 10.1371/journal.pone.0057333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lu QHG C, Hong Z. Trail making test used by Chinese elderly patients with mild cognitive impairment and mild Alzheimer dementia. Chinese Journal of Clinical Psychology 2016;14:118–21. [Google Scholar]
- 25. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1982-83;17:37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 26. Wang T, Xiao S, Li X, et al. Reliability and validity of the Chinese version of the neuropsychiatric inventory in mainland China. Int J Geriatr Psychiatry 2012;27:539–44. 10.1002/gps.2757 [DOI] [PubMed] [Google Scholar]
- 27. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61–5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.