Supplemental digital content is available in the text.
Key Words: disclosure, malpractice claims, risk management, Mcare, serious events, adverse events
Abstract
Objective
This study aimed to determine whether Pennsylvania ACT 13 of 2002 (Mcare) requiring the written and verbal disclosure of “serious events” was accompanied by increased malpractice claims or compensation costs in a large U.S. health system.
Main Outcomes and Measures
The primary outcome was the rate of malpractice claims. The secondary outcome was the amount paid for compensation of malpractice claims. The analyses tested the relationship between the rate of serious event disclosures and the outcome variables, adjusted for the year of the event, category of claim, and the degree of “harm” related to the event.
Results
There were 15,028 serious event disclosures and 1302 total malpractice claims among 1,587,842 patients admitted to UPMC hospitals from May 17, 2002, to June 30, 2011. As the number of serious event disclosures increased, the number of malpractice claims per 1000 admissions remained between 0.62 and 1.03. Based on a matched analysis of claims that were disclosed and those that were not (195 pairs), disclosure status was significantly associated with increased claim payout (disclosures had 2.71 times the payout; 95% confidence interval, 1.56–4.72). Claims with higher harm levels H and I were independently associated with higher payouts than claims with lower harm levels A to D (11.15 times the payout; 95% confidence interval, 2.30–54.07).
Conclusions and Relevance
Implementation of a mandated serious event disclosure law in Pennsylvania was not associated with an overall increase in malpractice claims filed. Among events of similar degree of harm, disclosed events had higher compensation paid compared with those that had not been disclosed.
The 1999 Institute of Medicine report To Err Is Human1 had the desired effect of focusing attention on medical errors within health care facilities worldwide. News headlines have repeatedly focused on the large number of deaths that occur as a consequence of these errors. These revelations have put physicians and hospitals under pressure to disclose errors in care, which contribute to adverse outcomes to patients and families. Two major reasons are cited in support of disclosure: the ethical imperative to tell the truth and the need to develop safer systems of health care delivery.2 Several institutions have reported a further benefit of open disclosure, namely, that the costs of litigation are reduced by prompt disclosure and apology to patients for medical error.3–7 Others have contested these findings. Studdert et al8 modeled litigation consequences of disclosure and forecasted that litigation volume and cost would increase because of disclosure. Many states in the United States have passed laws mandating disclosure of medical errors.9,10 Despite this, there are limited data on the effects of disclosure on malpractice claim volumes.11,12
In March 2002, Pennsylvania enacted Act 13, the Medical Care Availability and Reduction of Error Act (Mcare) 40 P.S. section 1303.101 et seq.13 This legislation requires disclosure of all “serious events.” A serious event is defined as “an event, occurrence, or situation involving the clinical care of a patient in a medical facility that results in death or compromises patient safety and results in an unanticipated injury requiring the delivery of additional health care services” (Table 1). Verbal disclosure of serious events to the patient or family must take place within 24 hours of the event and written confirmation within 7 days. The serious event determination must be reported electronically to the Pennsylvania Patient Safety Authority (PSA).13,14
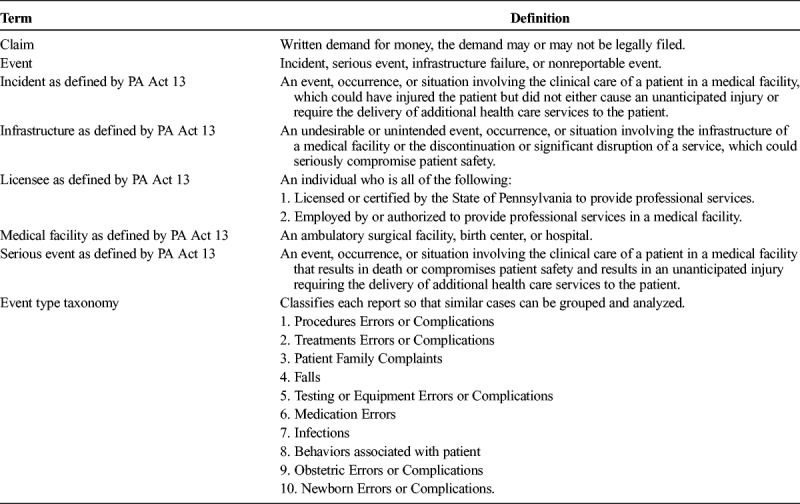
TABLE 1.
Definition of Terms
Although the requirements have been in effect for more than a decade, no study has addressed the question of whether this or other state-mandated serious event written disclosure encourages the filing of malpractice claims or alters degrees of compensation. The University of Pittsburgh and UPMC, a large health care system in southwestern Pennsylvania, supports and has implemented transparency in reporting medical error in compliance with Act 13. The purpose of this article was to report the relationship of written serious event disclosure with malpractice compensation claims filed against the health care system.
METHODS
This was a retrospective review of event reports and closed malpractice claims. The study was approved by the UPMC Quality Improvement Review Committee, in accordance with our institutional review board policy.
Act 13 requires any employee to report an event that could have injured a patient or compromised patient safety (Table 1 for definitions). At UPMC, once events are reported, they are triaged to the risk management department via a secure Web site, secure e-mail, or a dedicated telephone line. The events are automatically stored in an electronic risk management database. A risk manager reviews each event, classifies it using event type taxonomy, and triages it. The circumstances are investigated by chart review and personal interviews. The Patient Safety Quality Peer Review Committee reviews cases that could or did cause injury to the patient (Appendix A, Supplemental Digital Content 1, http://links.lww.com/JPS/A15). With the use of the PSA Harm Score, the Patient Safety Quality Peer Review Committee determines the degree of harm score (scale A-I) from among those listed in Table 2.15 For serious events with a harm score of E or greater, the attending physician is reminded to verbally disclose the event and document the disclosure in the medical chart. A letter is sent to the patient confirming the event and the verbal disclosure by the physician. The letter expresses regret for the incident and offers contact directions for further information. Neither a formal apology nor an offer of financial compensation is made.
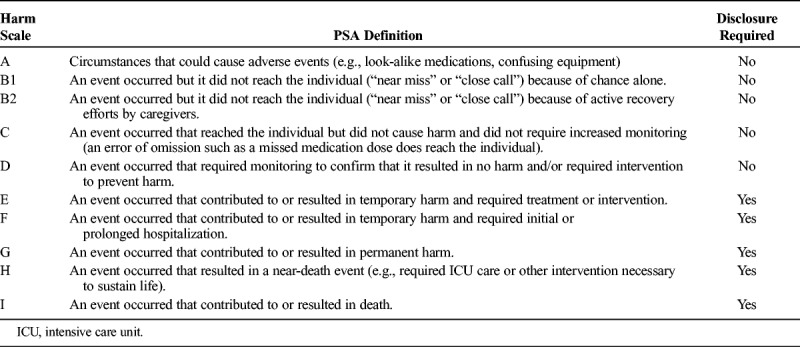
TABLE 2.
Harm Score Table as Defined by Pennsylvania PSA
The UPMC began issuing written serious event disclosure letters in accordance with the provision of the statute in May 2002. In the following decade, a number of hospitals joined the UPMC system. In 2007, the patient safety authority added hospital-acquired infections (HAI) to the list of serious events, which resulted in a marked increase in numbers of serious event disclosures.
In Pennsylvania, a medical malpractice claim is essentially a written demand for payment, asserting that the provider had a duty to the patient, that the duty was breached, and that the breach resulted in an injury to the patient. The statute of limitations is 2 years for adults and 18 years of age plus 2 years for children.16 The UPMC owns and operates a “captive” insurance company, which has the sole function of providing medical professional liability coverage to UPMC facilities, employees, and physicians. The UPMC is an integrated health system with 20 academic, specialty, and community hospitals and more than 4000 faculty or employed physicians. All malpractice claims for compensation are entered into the database of the captive insurer.
Malpractice claims obtained from the captive insurance database beginning January 1, 2000, and filed by June 30, 2013, were analyzed over a 13-year period and serious event disclosure data reported in the risk management database during the period of May 17, 2002, through June 30, 2011. The analytic data set included an additional 4 years of malpractice claims data to account for 2 years before and 2 years after disclosure for the statute of limitation for those events disclosed by June 30, 2011. Any claim in which no money was paid to a patient/plaintiff (because the claim was denied and not pursued, the case was dismissed, or a jury returned a verdict for the defense) was assigned a compensation amount of $0. We classified the degree of patient harm for all claims that were filed using the definitions approved by the PSA (Table 2).15 Malpractice claims solely against outpatient settings and extended care facilities were excluded.
Serious event disclosures were obtained from the risk management database for the period of May 17, 2002, to June 30, 2011. All serious event disclosures reported to the PSA were included. Excluded were patients who received care in other outpatient settings or extended care facilities. The data set could not capture errors that are not recognized by employees (failure to recognize or diagnose), events that caused harm but were not reported (failure to report), and verbal disclosures of unanticipated harm events that were not reported.
Statistical Analysis
We hypothesized that serious event disclosure would be associated with an increased likelihood of a malpractice claim but a decreased payout. Tests of association between serious event disclosures and claims, stratified by harm score, were performed using χ2 tests of independence or Fisher exact tests. Wilcoxon rank sum tests were used to test differences in the distributions of claim payout by serious event disclosure status by year and harm score. The trend in claim rates over time was tested using a Cochran-Armitage trend test. Bonferroni corrections for multiple comparisons were used when appropriate.
Propensity score matching17 was applied to compensate for potential confounding by indication and generate bias-corrected comparisons of payout for closed claims (n = 1051), which were disclosed (n = 257) versus not disclosed (n = 794). Propensity scores, defined as the estimated probabilities of being a disclosed claim, were computed using logistic regression with harm score (A-D, E, F, G, as well as H and I), event type taxonomy (procedures errors or complications, treatments errors or complications, patient family complaints, falls, testing or equipment errors or complications, medication errors, infections, behaviors associated with patient, obstetric errors or complications, newborn errors or complications) and year of event (2002–2011). These variables were chosen because of their known association with the likelihood of having received a disclosure.18–20 Propensity scores were used with exact matching on harm score and nearest neighbor matching within a caliper of 0.15 SDs of the propensity score without replacement based on claim year and category.21 Disclosed claims that did not have a match within this caliper were discarded, as were undisclosed claims that were not selected as a match (599 undisclosed claims and 62 disclosed claims). We matched 195 (75.9%) of the disclosed claims, with 195 (24.6%) of the nondisclosed claims. Balance was verified by assessing standardized differences between groups for all variables in the matched cohort with a target of less than 20%, histograms of propensity scores for the matched data, and standard tests of differences between variables and disclosure status. We used a negative binomial regression model to investigate the association between disclosure status and claim payout because of the presence of $0 payouts (dismissals, defense verdict). The model controlled for harm status, category, and year of claim because these variables could confound the relationship between disclosure status and total payout. Computations were performed in SAS version 9.3 and R version 3.0.2 (packages MatchIt).
RESULTS
Disclosed Events
For the 9-year study period, May 17, 2002, to June 30, 2011, there were 1,587,842 inpatient hospital admissions to UPMC hospitals for a total of 9,625,864 inpatient days. There were 15,028 unique patient disclosures of “serious” events. There were 223 (1.4%) serious event disclosures that were inadvertently made to the state although the harm score was D or lower (not considered to be serious events). Appendix B (Supplemental Digital Content 2, http://links.lww.com/JPS/A16) details the rate of serious event disclosures relative to the number of admissions over each of the years after the enactment of Act 13. Figure 1A illustrates the increase in serious events disclosure from 2007 after the redefinition of all health care–acquired infections as serious events. There was no significant change in the rate of serious event disclosures per 1000 admissions from 2005 to 2011 when HAIs were excluded (Fig. 1A).
FIGURE 1.
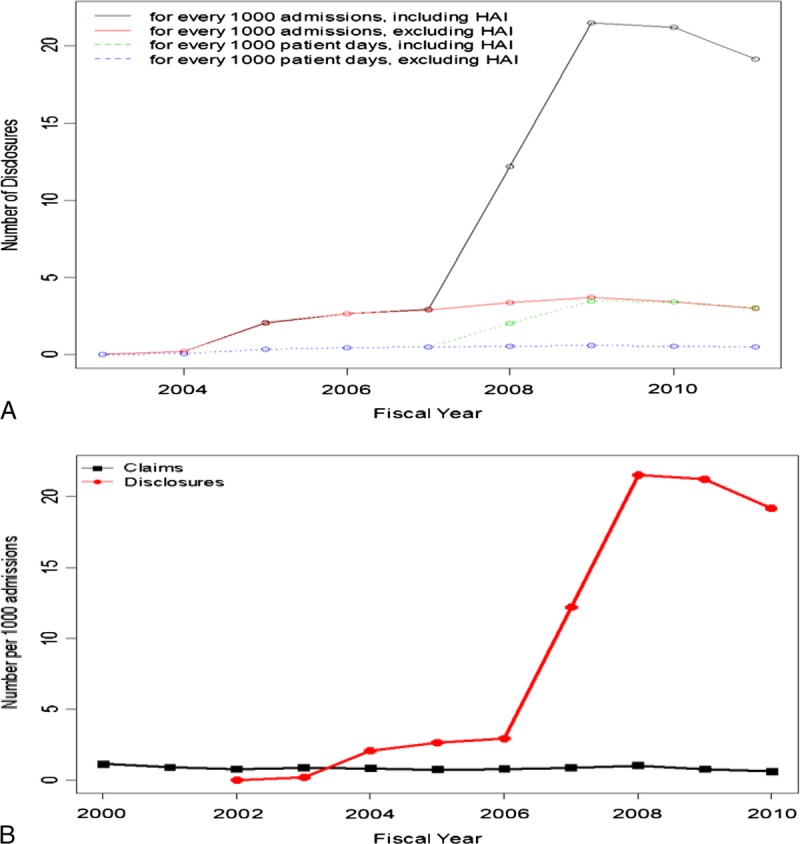
A, Number of serious events per fiscal year disclosed to patients and PA patient authority between May 17, 2002, and June 30, 2011. B, The rate of malpractice claims (black) remains stable between 0.62 and 1.14 per 1000 admissions from years 2000 to 2011.
Malpractice Claims
A total of 1302 claims were filed between May 17, 2002, and June 30, 2013, that corresponded to the written disclosure period. Of these, 993 claims (76%) had no disclosure and 309 had serious event disclosure. There were 1.14 total malpractice claims per 1000 admissions in the year before implementation of the Act 13 (Fig. 1B). There was a significant decrease in the rate of claims per 1000 admissions between 2000 and 2011 (from 1.14 to 0.62, P = 0.0002). There is no significant difference in total claim rates during the period of 2001 to 2010 (P = 0.09). In addition, there is no significant change in malpractice claim rates excluding HAI between 2002 and 2011 (P = 0.08). There was a brief increase in malpractice claims made for HAI coincident with the redefinition of HAI “serious event” in 2007 to 2009, but this was not evident the next year.
Serious Events, Malpractice Claims, and Harm Score
Most of the serious event disclosures and malpractice claims were made for events causing temporary harm and requiring initial or prolonged treatment associated with a harm score of E or F. Ninety percent (90%) of serious event disclosures issued were for cases with a temporary harm score E, with the remaining 10% for all other harm scores. Most malpractice claims were made in harm scores E and F; however, 27% of the malpractice claims had harm scores of A to D, which are considered no harm by the PSA.
Financial compensation to the plaintiff was highly skewed, with a few malpractice claims each year resulting in large payouts (Appendix C, Supplemental Digital Content 3, http://links.lww.com/JPS/A17). Considering all closed claims only by year, there was no increase in claim payout per claim with implementation of the disclosure law. The median payout decreased substantially since 2007 ($49,332 for 128 claims in 2007, $5000 in 2008 for 139 claims, $2500 in 2009 for 85 claims, and $259 in 2010 from 44 claims).
Considering claims by year and disclosure status, the median claim payout was significantly higher for claims that had been disclosed than for events that had no disclosure for all years (2004, 2005, 2008, and 2009; P = 0.0011, 0.0007, 0.0002, and 0.002 respectively). In these years, more than 50% of disclosed claim payments were more than $50,000 versus less than $7500 for undisclosed claims (Appendix D, Supplemental Digital Content 4, http://links.lww.com/JPS/A18). Considering the claims by harm level and disclosure status, the median payment per claim tended to increase as the degree of harm increased for both disclosed and undisclosed events (Fig. 2 and Appendix E, Supplemental Digital Content 2, http://links.lww.com/JPS/A16). When comparing payment stratified by harm score, aside from a single claim payout for a serious disclosed event with harm score A, payouts were 2 to 3 times higher for claims related to serious event disclosures when compared with undisclosed events of equivalent degrees of harm.
FIGURE 2.
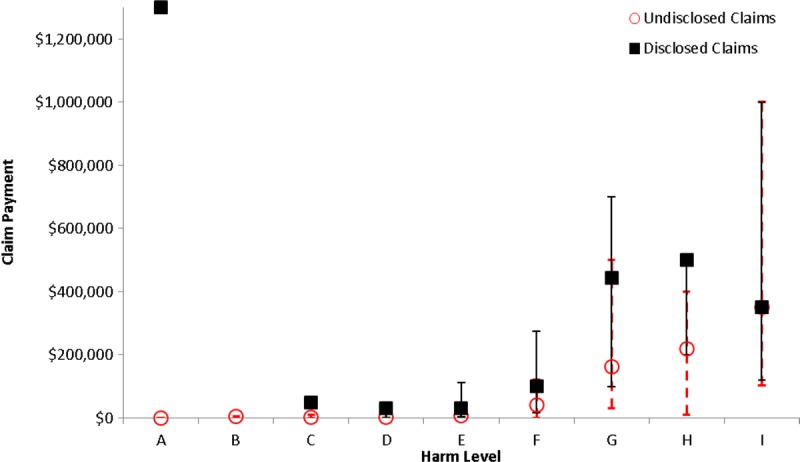
Median malpractice claim payout for undisclosed (red circle) versus serious event disclosed (black square) events for each harm level for all closed claims (n = 1051). Error bars represent the 25th to 75th percentiles of claim payout *Significant difference P ≤ 0.001.
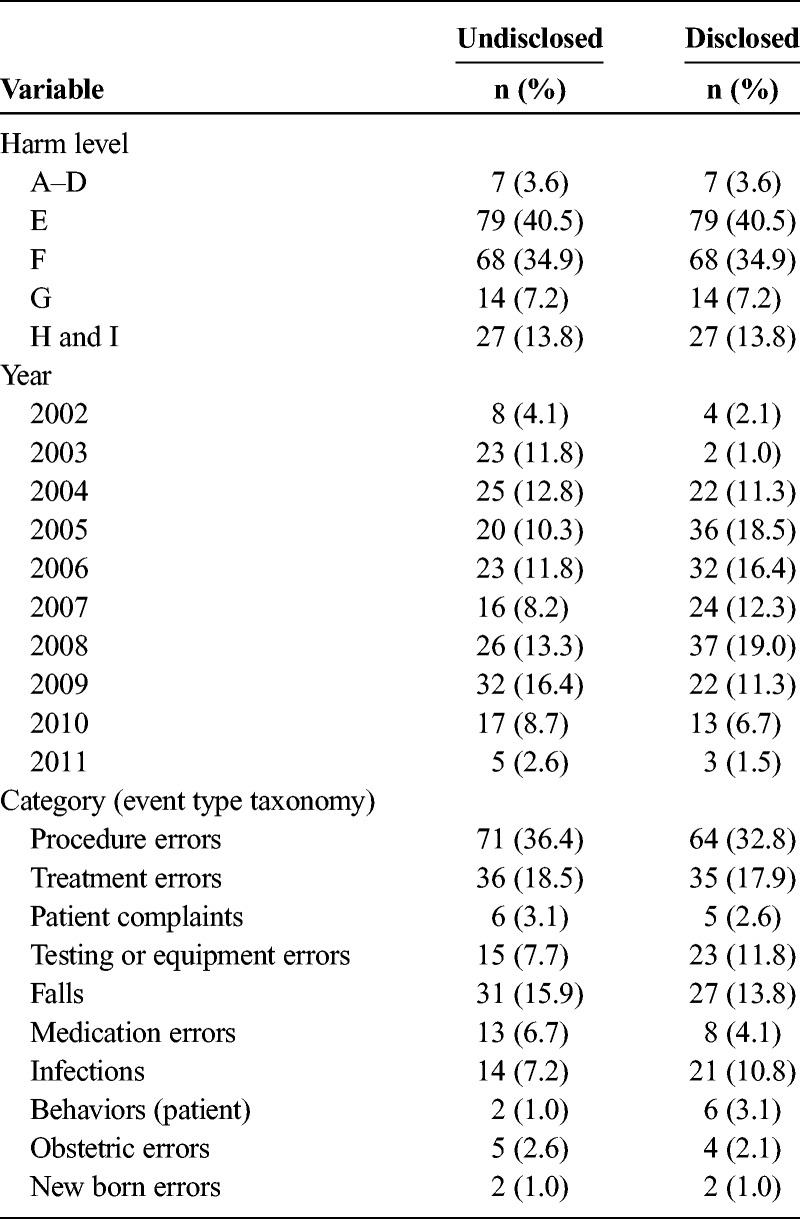
To further investigate the relationship among claim payout, serious event disclosure, and harm score for closed malpractice claims (n = 1051), we completed a propensity score–matched analysis on 195 matched pairs (Table 3). Both higher harm levels and being disclosed were significantly associated with higher total claim payout. Specifically, controlling for harm, category, and year, a claim that has been disclosed has 2.71 times (95% confidence interval, 1.56–4.72; P = 0.0004) the total payout than claims that have not been disclosed. Claims with harm levels H to I have 11.15 times (95% confidence interval, 2.30–54.07; P = 0.003) the payout than claims with harm levels A to D. Harm levels E, F, and G did not differ significantly in payout from harm levels A to D controlling for the other variables (P = 0.90, 0.24, and 0.06, respectively). Category and year of claim were not significantly associated with payout; P = 0.56 and 0.85, respectively.
TABLE 3.
Frequencies of Harm Level, Category, and Year for Closed Claims Used in Matched Pairs Analysis (n = 195 Matched Pairs)
DISCUSSION
In 2007, Studdert et al8 modeled the litigation consequences of disclosure and predicted that routine disclosure would more likely expand litigation and costs rather than reduce them. Our results do not support the hypothesis that written disclosure will increase the numbers of claims. However, we did find that compensation was significantly increased for claim events that were disclosed. This study is important because it is the first to provide empirical evidence on the relationship between mandatory disclosure regulations and malpractice claims and costs.
A search of PubMed.gov revealed more than 1300 publications on the topic of “medical error disclosure” during the period 1973 to March 2013. In the past decade, more than 100 articles have appeared on this subject every year. There is near-universal agreement of the ethical duty of health care providers to disclose harmful medical mistakes to the patients.22 Most articles emphasized that disclosure of a medical error to a patient encourages self-evaluation and peer review so that errors can be analyzed for the purpose of minimizing such problems in the future.23–26 Many professional organizations including the American College of Physicians,27 the Joint Commission,28 and the American Medical Association29 support the idea that “timely and candid disclosure should be standard practice.”
A number of states including Pennsylvania have enacted statutes requiring or encouraging disclosure.30 Some states however have declined to enact such laws. There is disagreement over what constitutes an error, the nature of the apology, and what degree of liability is generated by such disclosure statements.31 Surveys reveal that many health care professionals are concerned that ambiguities inherent in an open approach will undermine patients' confidence in the quality of care. Ethical opinions assert that disclosure will support the relationships between physicians and patients.32–37 There is evidence that frank explanations of all types of adverse outcome, with expressions of regret and apology, are the exception rather than the rule, although this is the kind of disclosure desired by patients.
Two frequently cited studies support the idea that prompt reporting of harmful events, when accompanied by apologies, actually decreases litigation and the size of resulting financial settlements. Both studies described voluntary efforts to provide not only disclosure but also apology and compensatory financial offers sometimes called “disclosure, apology, and offer (DA&O)” programs.4–6,23,36,37 The Lexington Veterans Affairs Medical Center began a practice in 1987 in which disclosure was accompanied by apology to the patient. There were a larger number of claims, but lower average settlement amounts compared with a group of comparable VA hospitals.4–6 A similar policy at the University of Michigan offered prompt financial compensation after an injury and found a reduction from 262 claims in 2001 to less than 100 in 2005. More recent updates confirmed that since the initiation of the program, the number of claims, time from claim to resolution, total liability costs, patient compensation, and related legal costs have all significantly decreased.5
No previous study has addressed the implementation of a state mandated disclosure law on malpractice claims or levels of financial compensation. The present study focuses on a single large multihospital health care system in western Pennsylvania after the state mandated disclosure of serious events to the patient and the Pennsylvania Safety Authority. More than 15,000 written disclosures were made without an overall increase in claims. A prompt and sustained decrease in malpractice claims was observed.
Complicating interpretation of all retrospective studies, including those from Michigan and western Pennsylvania, is the overall decline in malpractice claims during this period that has occurred nationally.9,10 Elsewhere in Pennsylvania, where written disclosure was mandated, malpractice claims decreased 44% between 2000 and 2011.38 Although our program does not include apology and offer, these combined results give some support to the VA and Michigan studies that disclosure does not increase the number of claims. Many factors may contribute to the decrease in number of claims and the implementation of a disclosure law may or may not be one of them.
Of the many malpractice claims filed, it is well-known that few such claims are resolved by a jury trial. Most malpractice claims end in settlements negotiated between defendant and plaintiff. For example, in 2012, only 10 cases ended in a jury verdict in Allegheny County, Pennsylvania, although the number of malpractice claims filed annually in the previous 3 years ranged from 263 to 326.38 Therefore, providing letters of disclosure confirming that serious events had occurred during hospitalizations potentially arm plaintiffs' lawyers with written statements from hospitals that the standard of care may have been violated. Such statements, although in our experience never introduced into evidence in cases, can be interpreted as admissions by the hospitals and provide an advantage to the patients' lawyers in settlement discussions. This may in turn lead to higher settlements.
This study had several limitations. This was a retrospective observational study of the outcomes of a number of uncontrollable processes that underlie compliance with a single state law and single health system. The results may not be generalizable to other states with differing laws relating to disclosure. Some states have passed apology laws that protect the disclosure from being interpreted by the courts as an admission of guilt,39 and few states mandate disclosure. Tort reform, quality improvement, and patient safety efforts have taken many varied approaches, and there has been no analysis of the reasons for the national decrease in malpractice claims.
The claims made and compensation amounts paid are influenced by many factors not measured in this study, including age, occupation, dependents, comorbidities, education, geographic location, and earning capacity.39–41 The propensity score–based matching that we used would not be able to adjust for these unmeasured confounders. Despite these limitations, the results are contrary to the prediction of the model by Studdert et al8 stating that the number of claims would increase but do seem to be in line with their prediction of an increase in costs of claims if disclosure laws were widely enforced.
Notwithstanding Act 13, three-quarters of the claims filed were for events that were never disclosed, reflecting findings that the vast majority of errors go unreported.42 Many harmful events represent delayed and missed diagnoses or other judgment errors not recognized as errors by providers. However, few physicians file reports42; those that are filed are usually by nurses who may feel compelled to report obvious errors with easily recognized harm. Disclosures inevitably carry both verbal and nonverbal messages and are delivered under differing circumstances, by hundreds of different providers.43–48 Another unmeasured confounder is the quality of the disclosure discussion. The only common element of the disclosure process in Pennsylvania was requirements of a written letter confirming disclosure. It is possible that many of the mandated disclosure discussion may not have been performed skillfully, perhaps because of inadequate institutional support of clinicians. The lack of apology, a component of disclosure universally expected by patients, may have blunted the effectiveness of some of the required discussions.2,33 These factors could have prevented the potential benefits of disclosure in mitigating anger and awards from being realized.
Mandated disclosure has important advantages recently reviewed by Kachalia23: the process reinforces the ethical imperative to tell the whole truth; it encourages the difficult conversation between provider and patient to occur, even if a formal apology is not offered; and it may increase efforts to develop a curriculum designed to improve patient-physician communication. Furthermore, the process facilitates both major and more subtle changes in care, which might avoid the complication or error in the future. It encourages the culture of safety in which educational and system improvements can occur. Indeed, this was the principle goal of Act 13 and other mandates of this type.42
CONCLUSIONS
Serious event disclosures do not open the litigation floodgates and increase the number of claims. Disclosure, however, coincided with an increase in both the rate of financial compensation and the average payout per claim even after controlling for the extent of harm. Act 13 may be judged a success in that it has increased openness with patients about adverse events without increasing the number of malpractice claims. Although the costs attributed to claims where disclosure occurred were higher than claims where there was no disclosure, this is not unexpected. The circumstances of the disclosed situations were clear enough for the incidents to be labeled as serious events, thus giving the claimants the upper hand in negotiating settlements. Undisclosed situations were not so clear cut and thus more amenable to being contested which lowers settlement values. Further research is needed on whether disclosure discussions contribute to the propensity to file claims or to the value of claims when filed.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the following: Patricia Buddmeyer, data analyst, UPMC Corporate and Captive Insurance Program, data collection, no compensation awarded; Tisha Cannone, insurance analyst, UPMC Corporate and Captive Insurance, data collection, no compensation awarded; Samantha Curtis, health information student, University of Pittsburgh, data collection, no compensation awarded; Nancy DeRiggi, executive assistant, UPMC Corporate Risk Management, proof reading, no compensation awarded; Matthew Doherty, legal intern, UPMC Legal Intern, legal literature search, no compensation awarded; Charles Schwabenbauer, financial analyst, UPMC, data collection, no compensation awarded; Margaret Sims, senior systems analyst, UPMC Corporate Risk Management, data collection, no compensation awarded; Joanne Frazier, senior risk specialist, UPMC Corporate Risk Management, proof reading, no compensation awarded; Derek Angus, chair, Department of Critical Care Medicine, secondary appointments in medicine, health policy and management, and clinical and translational science, director, CRISMA Center, Department of Critical Care Medicine, University of Pittsburgh Schools of the Health Sciences and UPMC Health System, reading and suggestions, no compensation awarded; Lyda Dye, senior director, UPMC Revenue Cycle, proof reading, no compensation awarded; Rebecca Moss, nursing student, proof reading, no compensation awarded; and Elizabeth Stuart, associate professor, Department of Mental Health, Department of Biostatistics, Johns Hopkins Bloomberg School of Public Health, statistical consult, no compensation awarded.
Footnotes
The authors disclose no conflict of interest.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.journalpatientsafety.com).
REFERENCES
- 1.Kohn LT, Corrigan J, Donaldson MS . Washington, DC: National Academy Press, 2000. [Google Scholar]
- 2.Wu AW, Cavanaugh TA, McPhee SJ, et al. To tell the truth: ethical and practical issues in disclosing medical mistakes to patients. . 1997;12:770–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boothman RC, Blackwell AC, Campbell DA, Jr, et al. A better approach to medical malpractice claims? The University of Michigan experience. . 2009;2:125–159. [PubMed] [Google Scholar]
- 4.Kachalia A, Shojania KG, Hofer TP, et al. Does full disclosure of medical errors affect malpractice liability? The jury is still out. . 2003;29:503–511. [DOI] [PubMed] [Google Scholar]
- 5.Kachalia A, Kaufman SR, Boothman R, et al. Liability claims and costs before and after implementation of a medical error disclosure program. . 2010;153:213–221. [DOI] [PubMed] [Google Scholar]
- 6.Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. . 1999;131:963–967. [DOI] [PubMed] [Google Scholar]
- 7.Mitka M. Disclosing medical errors does not mean greater liability costs, new study finds. . 2010;304:1656–1657. [DOI] [PubMed] [Google Scholar]
- 8.Studdert DM, Mello MM, Gawande AA, et al. Disclosure of medical injury to patients: an improbable risk management strategy. . 2007;26:215–226. [DOI] [PubMed] [Google Scholar]
- 9.Marchev M. Medical malpractice and medical error disclosure: balancing facts and fears. December 2003. Available at: http://www.nashp.org/sites/default/files/balancing_facts_fears.pdf. Accessed November 21, 2013. [Google Scholar]
- 10.Weinberg J, Hilborne LE, Nguyen QT. Regulation of health policy: patient safety and the states. Available at: http://www.ncbi.nlm.nih.gov/books/NBK20479/. Accessed November 21, 2013. [PubMed]
- 11.Gallagher TH, Studdert D, Levinson W. Disclosing harmful medical errors to patients. . 2007;356:2713–2719. [DOI] [PubMed] [Google Scholar]
- 12.Murtagh L, Gallagher TH, Andrew P, et al. Disclosure-and-resolution programs that include generous compensation offers may prompt a complex patient response. . 2012;31:2681–2689. [DOI] [PubMed] [Google Scholar]
- 13. Medical Care Availability and Reduction of Error (MCARE) Act, 40 P.S. §1303.101 et seq. [Google Scholar]
- 14.Commonwealth of Pennsylvania Patient Safety Authority. Pennsylvania patient safety authority issues annual report for 2012. Available at: http://patientsafetyauthority.org/NewsAndInformation/PressReleases/2013/Pages/pr_April_30_2013.aspx. Accessed July 1, 2013.
- 15.Commonwealth of Pennsylvania Patient Safety Authority. Automated data interface XML specifications part 3 of 3 appendix. Available at: http://patientsafetyauthority.org/PA-PSRS/Documents/part3-appendix.pdf. Accessed November 21, 2013.
- 16. Pennsylvania Judiciary and Judicial Procedures 42 Pa.C.S.A. §§5524, 5533. [Google Scholar]
- 17.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. . 1985;39:33–38. [Google Scholar]
- 18.Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. . 1996;335:1963–1967. [DOI] [PubMed] [Google Scholar]
- 19.Mehstun WT, Ibrahim AM, Diener-West M, et al. Surgical never events in the United States. . 2013;153:465–472. [DOI] [PubMed] [Google Scholar]
- 20.Luce JM. Medical malpractice and the chest physicians. . 2008;134:1044–1050. [DOI] [PubMed] [Google Scholar]
- 21.Ho D, Imai K, King G, et al. MatchIt: nonparametric preprocessing for parametric causal inference. Available at: http://gking.harvard.edu/files/matchp.pdf. Accessed December 21, 2007.
- 22.Vogel J, Delgado R. To tell the truth: physician's duty to disclose medical mistakes. . 1980;28:52–94. [PubMed] [Google Scholar]
- 23.Kachalia A. Improving patient safety through transparency. . 2013;369:1677–1679. [DOI] [PubMed] [Google Scholar]
- 24.O'Conner E, Coates HM, Yardley IE, et al. Disclosure of patient safety incidents: a comprehensive review. . 2010;22:371–379. [DOI] [PubMed] [Google Scholar]
- 25.Hebert PC, Levin AV, Robertson G. Bioethics for clinicians: 23. Disclosure of medical error. . 2001;164:509–513. [PMC free article] [PubMed] [Google Scholar]
- 26.Wu AW, Boyle DJ, Wallace G, et al. Disclosure of adverse events in the United States and Canada: an update, and a proposed framework for improvement. . 2013:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American College of Physicians Ethics Manual. Third edition. . 1992;117:947–960. [DOI] [PubMed] [Google Scholar]
- 28.The Joint Commission. Health care at the crossroads: strategies for improving the medical liability system and preventing patient injury. 2005. Available at: www.jointcommission.org/assets/1/18/Medical_Liability.pdf. Accessed July 8, 2013. [Google Scholar]
- 29.AMA council on ethics. Available at: http://www.amednews.com/article/20120706/profession/307069996.
- 30.Pelt JL, Faldmo LP. Physician error and disclosure. . 2008;51:700–708. [DOI] [PubMed] [Google Scholar]
- 31.Saitta N, Hodge S., Jr Efficacy of a physician's words of empathy: an overview of state apology laws. . 2012;112:302–306. [DOI] [PubMed] [Google Scholar]
- 32.McIntyre N, Popper K. The critical attitude in medicine: the need for a new ethics. . 1983;287:1919–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu AW, Huang IC, Stokes S, et al. Disclosing medical errors to patients: it's not what you say, it's what they hear. . 2009;24:1012–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lazare A. Apology in medical practice: an emerging clinical skill. . 2006;296:1401–1404. [DOI] [PubMed] [Google Scholar]
- 35.Bell SK, Smulowitz PB, Woodward AC, et al. Disclosure, apology and offer programs: stakeholders' views of barriers to and strategies for broad implementations. . 2012;90:682–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pelletier E, Robson R. Giving back the pen: disclosure, apology and early compensation discussions after harm in the healthcare setting. . 2008;11:85–90. [DOI] [PubMed] [Google Scholar]
- 37.Supreme Court of Pennsylvania Medical Malpractice Filings Report 2000-2012. Available at: http://www.pacourts.us/assets/files/setting-2929/file-2300.pdf?cb=71be06. Accessed November 13, 2013.
- 38.Mastroianni AC, Mello MM, Sommer S, et al. The flaws in state ‘apology’ and ‘disclosure’ laws dilute their intended impact on malpractice suits. . 2010;29:1611–1619. [DOI] [PubMed] [Google Scholar]
- 39.Orosco RK, Talamini J, Chang DC, et al. Surgical malpractice in the United States 1990-2006. . 2012;215:480–488. [DOI] [PubMed] [Google Scholar]
- 40.Saber Tehrani AS, Lee H, Mathews SC, et al. 25-year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. . 2013;22:672–680. [DOI] [PubMed] [Google Scholar]
- 41.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. . 2006;354:2024–2033. [DOI] [PubMed] [Google Scholar]
- 42.Levtzion-Korach O, Frankel A, Alcalai H, et al. Integrating incident data from five reporting systems to assess patient safety: making sense of the elephant. . 2010;36:402–410. [DOI] [PubMed] [Google Scholar]
- 43.Conway J, Federico F, Stewart K, et al. Respectful Management of Serious Clinical Adverse Events (Second Edition). IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2011. Available at: www.IHI.org. Accessed July 1, 2013. [Google Scholar]
- 44.Hannawa AF. Shedding light on the dark side of doctor-patient interactions: verbal and nonverbal messages physicians communicate during error disclosures. . 2011;84:344–351. [DOI] [PubMed] [Google Scholar]
- 45.Hannawa AF, Beckman H, Mazor KM, et al. Building bridges: future directions for medical error disclosure research. . 2013;92:319–327. [DOI] [PubMed] [Google Scholar]
- 46.Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. . 1996;156:2565–2569. [PubMed] [Google Scholar]
- 47.Kaldjian LC, Jones EW, Rosenthal GE, et al. An empirically derived taxonomy of factors affecting physicians' willingness to disclose medical errors. . 2006;21:942–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gallagher TH, Waterman AD, Ebers AG, et al. Patients' and physicians' attitudes regarding the disclosure of medical errors. . 2003;289:1001–1007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


