Abstract
Introduction
Several studies suggest that the health of an individual is influenced by the socioeconomic status (SES) of the community in which he or she lives. This analysis seeks to understand the relationship between SES, tobacco store density and health outcomes at the neighbourhood level in a large urban community.
Methods
Data from the 55 neighbourhoods of Baltimore City were reviewed and parametric tests compared demographics and health outcomes for low-income and high-income neighbourhoods, defined by the 50th percentile in median household income. Summary statistics are expressed as median. Tobacco store density was evaluated as both an outcome and a predictor. Association between tobacco store densities and health outcomes was determined using Moran’s I and spatial regression analyses to account for autocorrelation.
Results
Compared with higher-income neighbourhoods, lower-income neighbourhoods had higher tobacco store densities (30.5 vs 16.5 stores per 10 000 persons, P=0.01), lower life expectancy (68.5 vs 74.9 years, P<0.001) and higher age-adjusted mortality (130.8 vs 102.1 deaths per 10 000 persons, P<0.001), even when controlling for other store densities, median household income, race, education status and age of residents.
Conclusion
In Baltimore City, median household income is inversely associated with tobacco store density, indicating poorer neighbourhoods in Baltimore City have greater accessibility to tobacco. Additionally, tobacco store density was linked to lower life expectancy, which underscores the necessity for interventions to reduce tobacco store densities.
INTRODUCTION
Socioeconomic status (SES) is a multidimensional construct comprising diverse socioeconomic factors.1,2 These factors may affect health outcomes at different moments of life and may operate at different levels, from individual to household to community.3–8 Growing evidence has recognised that neighbourhoods’ socioeconomic characteristics influence the health of an individual through multiple pathways.6–8 Therefore, when considering the complex relationships between community SES and health, evaluation of factors that co-localise with neighbourhood SES is necessary to better understand the potential influence on health outcomes.
One such factor is the sale of tobacco within residential areas. The high density of tobacco stores in low-income neighbourhoods has been documented9–12 and is the result of several factors, such as lower rental costs in low-income neighbourhoods. The high density of tobacco stores not only increases the supply of tobacco, but is likely to create a competitive local market with reduced product costs,9 which may result in an accessible and inexpensive product available to socioeconomically vulnerable populations. And while the impact of tobacco on an individual is well established in regards to health outcomes, the impact of density of tobacco stores on the health of a community remains unclear.
The objective of this study is to understand the relationship between the SES of neighbourhoods within an urban community (specifically, Baltimore City, the largest independent city in the USA13), tobacco store density and specific health outcomes, including life expectancy, age-adjusted mortality and death from chronic respiratory disease. It is hypothesised that characteristics of neighbourhoods, specifically lower SES and greater tobacco store densities, are associated with worse health outcomes.
METHODS
The Baltimore City data were obtained from the 2011 Neighborhood Health Profiles, a data set that compiles a variety of demographic (individual and community level) and outcome data from several sources (table 1).14 The purpose of the data was to highlight factors that may influence the health outcomes of Baltimore City’s neighbourhoods, attempting to identify objective variables that correlate with local health issues and concerns. The 2011 Neighborhood Health Profiles included data from the 2010 US Census, at which time the total Baltimore City population was 616 802 with a high minority population (60%). The Baltimore City Health Department organises neighbourhoods into community statistical areas (CSAs).14 The resulting 55 CSAs represent communities of similar social, demographic and economic characteristics. Each CSA (hereby referred to as neighbourhoods) must have a total population ranging from 5000 to 20 000 persons and allows for the collection and aggregation of a wide range of data for a relatively stable geography over time.
Table 1.
Sources for the 2011 Neighborhood Health Profiles provided by the Baltimore City Health Department
| Section | Variables | Source(s) |
|---|---|---|
| Demographics | Age, race | 2010 US Census |
| Socioeconomic characteristics | Income, education | American Community Survey 2005–2009 |
| Education | Baltimore City Public Schools Work Sampling System of the Maryland Model for School Readiness Baltimore Neighborhood Indicators Alliance from the Baltimore City Public Schools American Community Survey 2005–2009 |
|
| Community built and social environment | Alcohol store density Tobacco store density |
Baltimore City Liquor Board Baltimore City Comptroller Baltimore Neighborhood Indicators Alliance from the Baltimore City Police Department Baltimore City Police Department |
| Food environment | Fast food store density | Baltimore City Health Department Open Food Facilities Permit/License Database The Johns Hopkins Center for a Livable Future |
| Health outcomes | Death from chronic lower respiratory disease Life expectancy, age-adjusted mortality |
2010 US Census Maryland State Vital Statistics Administration 2005–2009 Maryland Department of Environment, Lead Poisoning Prevention Program |
The Neighborhood Health Profiles consist of seven sections, with the three sections providing an overview of demographic and community data and the four sections providing data on social determinants of health by neighbourhood. Demographic data included age (percentage of adults >65 years), gender, race/ethnicity (white, black or African-American, Hispanic or Latino, other race, or two or more races). As ‘white’ and ‘black or African-American’ represented >99% of the population, all other race variables were excluded from analyses. Socioeconomic characteristics included median household income while education variables included per cent of residents age 25 and older who have completed a bachelor’s degree or more. Community built and social environment characteristics included alcohol store density, tobacco store density and fast food store density. Tobacco stores are defined by the Baltimore City Health Department as ‘establishments that sell cigarettes or other tobacco products (cigars, pipe tobacco, chewing tobacco, roll-your-own tobacco, snuff, snus, and other smokeless tobacco products)’.15 In regards to health outcomes, data included life expectancy at birth (in years), age-adjusted mortality (deaths per 10 000 residents) and deaths due to chronic lower respiratory disease (per 10 000 residents).
The 55 neighbourhoods were categorised as lower income (n=28) or higher income (n=27) based on the 50th percentile of median household income. Results are presented as median with 25th to 75th percentiles. Neighbourhood characteristics and health outcomes between the two neighbourhood income categories were compared by t-tests for continuous variables and Fisher’s exact test for categorical variables. In sensitivity analyses, and to enhance generalisability or our findings to other national regions, we also dichotomised our data at the national median income of 2011 and separately by neighbourhoods with >20% of families below the federal poverty line (poor) or <20% of families below the poverty line.16 Pearson’s correlations were executed to evaluate the relationship between health outcomes of interest and tobacco store densities.
Given that there exists a strong concern for clustering when using cross-sectional data in regards to tobacco store densities in a geographic area,17 we ran spatial regression analyses to evaluate for spatial autocorrelation. Spatial autocorrelation refers to the measurement of correlation of a variable with itself in a given area, occurring when similar or dissimilar values occur near one another in that given space.17 Specifically, using Moran’s I and spatial regression, spatial autocorrelation was found for tobacco store densities in assessing its association with the health outcomes in unadjusted models and models adjusted for socioeconomic variables (race, percentage of population >65 years of age, percentage of population with a college degree age 25 years and older and median household income).
For consistency across all models, Moran’s I and spatial regression analyses were run for all univariate and multivariable models: unadjusted models, adjusted modes with tobacco store as the sole density measure and adjusted with density of all three store types including confounders. Comparing Moran’s I and spatial regression models with linear regression models (without adjustment for autocorrelation), the results were similar; therefore, only results for Moran’s I and spatial regression models are presented. One neighbourhood had significant higher tobacco store density (130.3) compared with others, and sensitivity analysis was performed excluding this outlier from analyses. Statistical analyses were conducted with SigmaPlot V.11.0 (San Jose, California, USA) and R software V.0.99.903 with a statistical significance level of 0.05.
RESULTS
Neighbourhood characteristics
The collective median household income of the 55 Baltimore City neighbourhoods was $36 362 (IQR $30 229–47 745). The median life expectancy was 71.9 (IQR 68.2–74.3) years, median aged-adjusted mortality was 115.7 (IQR 99.3–134.4) deaths per 10 000 residents and the median deaths from chronic lower respiratory disease was 3.7 (IQR 2.9–5.7) per 10 000 residents. Median tobacco store density was 22.5 (IQR 11.3–39.0) per 10 000 persons, which was greater than alcohol store density (4.5 (2.4–4.7)) or fast food density (1.5 (0.0–2.8)), both P<0.001.
Association of neighbourhood income with store densities and health outcomes
Lower household income neighbourhoods had a larger proportion of African-American residents and lower education with fewer adult (at least 25 years of age) residents with a bachelor’s degree. Lower household income neighbourhoods also had almost double the tobacco store density (30.5 vs 16.5 per 10 000 residents, P=0.01) and higher alcohol store density compared with higher household income neighbourhoods (table 2 and figure 1). Fast food store density did not differ between lower-income and higher-income neighbourhoods.
Table 2.
Comparison of lower-income and higher-income neighbourhood variables in Baltimore City, defined by median household income
| Characteristic | Overall | Low income (n=28) | High income (n=27) | P value* |
|---|---|---|---|---|
| Neighbourhood demographics† | ||||
| Median household income (US$) | 36 362 (30 229, 47 745) | 30 230 (25 050, 33 240) | 47 760 (41 220, 60 160) | <0.001 |
| African-Americans (%) | 76.2 (34.7, 92.8) | 91.1 (76.1, 95.8) | 49.7 (12.0, 74.4) | <0.001 |
| Whites (%) | 17.6 (3.8, 52.8) | 5.0 (1.7, 17.6) | 41.7 (20.3, 75.1) | <0.001 |
| Residents 25 years or older with a bachelor’s degree or more (%) | 17.7 (8.3, 32.2) | 9.4 (7.0, 17.4) | 30.4 (20.7, 49.1) | <0.001 |
| Percentage of population > 65 years of age (%) | 11.4 (9.0, 13.0) | 12.1 (9.1, 12.8) | 10.9 (9.0, 14.6) | 0.59 |
| Neighbourhood store densities | ||||
| Tobacco store (density per 10 000 residents) | 22.5 (11.3, 39.0) | 30.5 (19.7, 44.9) | 16.5 (9.1, 27.2) | 0.01 |
| Alcohol store (density per 10 000 residents) | 4.5 (2.4, 4.7) | 5.5 (4.0, 7.9) | 2.9 (2.1, 4.7) | 0.001 |
| Fast food density (per 10 000 residents) | 1.5 (0.0, 2.8) | 1.1 (0.0, 2.6) | 1.7 (0.8, 3.3) | 0.57 |
| Neighbourhood health outcomes | ||||
| Life expectancy at birth (years) | 71.9 (68.2, 74.3) | 68.2 (65.2, 71.7) | 74.3 (72.2, 76.5) | <0.001 |
| Aged-adjusted mortality (per 10 000 residents) | 115.7 (99.3, 134.4) | 130.8 (113.2, 143.8) | 102.1 (87.3, 118.4) | <0.001 |
| Deaths due to chronic lower respiratory disease (per 10 000 residents) | 3.7 (2.9, 5.7) | 3.7 (2.8, 4.9) | 4.5 (3.0, 6.6) | 0.35 |
Results are presented as median (25th, 75th percentiles).
P values represent comparisons between the two neighbourhood income categories, by t-tests for continuous variables or Fisher’s exact test for categorical variables, where appropriate.
Note that we only included African-American and white for race as other races made up <1% of the majority of the neighbourhoods.
Figure 1.
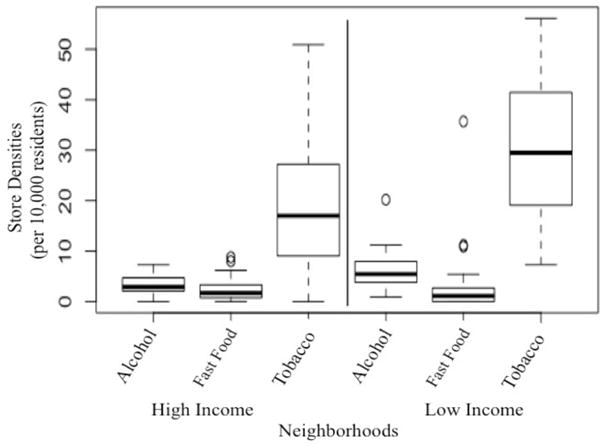
Comparison of store densities between high-income and low-income neighbourhoods. There was a statistically significant difference between alcohol (P=0.001) and tobacco (P=0.01) store densities, but not in fast food store densities (P=0.99). Neighbourhood with tobacco store density of 130.3 was excluded from the figure.
Lower household income neighbourhoods had lower life expectancy (68.2 vs 74.3 years; P<0.001) and higher age-adjusted mortality compared with higher household income neighbourhoods. There was no statistically significant difference between neighbourhood income and deaths from chronic lower respiratory disease (table 2).
These relationships were similar when dichotomising the neighbourhoods by values derived from national income and poverty values (see online supplementary tables 1 and 2).
Moran’s I and spatial regression models: neighbourhood characteristics, tobacco store densities and health outcomes
In unadjusted models, tobacco store density was associated with lower life expectancy (β =−0.14, P=0.01) and higher age-adjusted mortality (β =1.2, P=0.008) and death from chronic lower respiratory disease (β =0.46, P<0.001). Correlation of tobacco store densities and health outcomes is shown in figure 2. Lower median household income, African-American race, lower education and older age of residents were also associated with lower life expectancy, higher age-adjusted mortality and higher death from chronic respiratory disease, in univariate analyses. Only median household income and education did not reach statistical significance for association with death from chronic lower respiratory disease. Similarly, alcohol and fast food stores were also associated with worse health outcomes, except fast food store density had a borderline association with death from chronic lower respiratory disease (table 3).
Figure 2.
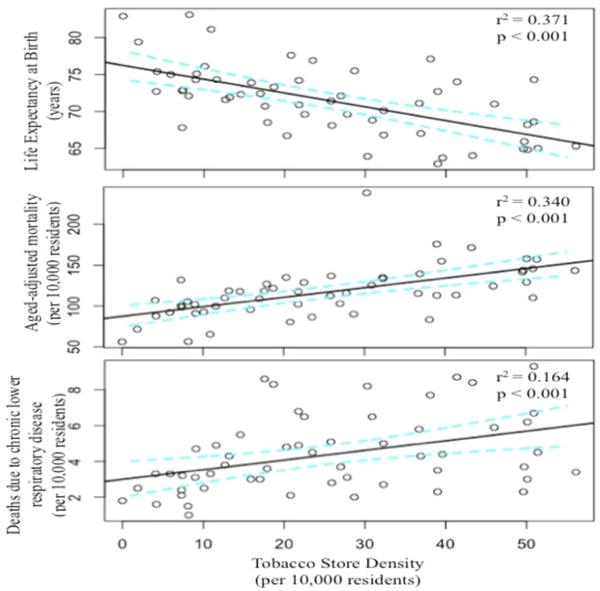
Correlation between tobacco store densities and health outcomes in univariate spatial regression analysis. Best fit line (solid black) and 95% CI (dashed blue line) are shown. Neighbourhood with tobacco store density of 130.3 was excluded from the figure.
Table 3.
Moran’s I and spatial lag regression model for select health outcomes and store densities, unadjusted and two adjusted models, of the 55 neighbourhoods of Baltimore City
| Life expectancy at birth | ||||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted† | Adjusted‡ | ||||
| Neighbourhood variables | β (95% CI) | P value | β (95% CI) | P value | β (95% CI) | P value |
| Tobacco store density | −0.13 (−0.05 to −0.22) | <0.001* | −0.12 (−0.03 to −0.17) | <0.001* | −0.10 (−0.02 to −0.23) | 0.004* |
| Alcohol store density | −0.81 (−0.55 to −1.02) | <0.001* | – | – | −0.32 (−0.13 to −0.52) | <0.001* |
| Fast food store density | −0.15 (−0.01 to −0.19) | 0.01* | – | – | −0.13 (−0.08 to 0.10) | −0.10 |
| Median household income § | 2.3 (3.7 to 120.0) | <0.001* | 0.17 (−32.4 to 2.1) | 0.59 | 0.1 (−0.12 to 0.21) | 0.49 |
| African-American (%) | −8.2 (−2.2 to −17.2) | <0.001* | −2.8 (−0.3 to −5.7) | 0.02* | −2.1 (−4.3 to 1.8) | 0.07 |
| Bachelor’s degree | 16.4 (9.8 to 25.9) | <0.001* | 11.8 (4.2 to 33.5) | <0.001* | 12.6 (7.2 to 29.3) | <0.001* |
| Age > 65 years (%) | 48.3 (30.1 to 67.2) | 0.006* | 14.2 (−0.03 to 22.2) | 0.06 | 12.9 (−10.2 to 21.2) | 0.13 |
| Age-adjusted mortality | ||||||
| Tobacco store density | 1.2 (0.7 to 2.5) | <0.001* | 1.0 (0.3 to 2.5) | <0.001* | 0.67 (0.32 to 0.87) | 0.002* |
| Alcohol store density | 6.7 (3.2 to 17.3) | <0.001* | – | – | 2.32 (2.01 to 7.1) | 0.03* |
| Fast food store density | 2.7 (0.4 to 9.2) | <0.001* | – | – | 0.59 (−3.1 to 1.1) | 0.24 |
| Median household income § | −1.2 (−4.1 to −8.1) | <0.001* | 0.26 (−93.0 to 0.71) | 0.92 | 0.70 (−0.06 to 0.91) | 0.37 |
| African-American (%) | 29.9 (14.3 to 55.3) | 0.01* | 12.7 (−22.1 to 41.2) | 0.14 | 10.7 (−20.9 to 17.2) | 0.11 |
| Bachelor’s degree | −68.7 (−41.7 to −98.2) | <0.001* | −50.8 (−37.7 to −86.2) | 0.005* | −65.5 (−40.3 to −72.1) | <0.001* |
| Age > 65 years (%) | −437.8 (−329.1 to −598.2) | <0.001* | −168.4 (−95.7 to −201.3) | 0.003* | −168.8 (−110.1 to −203.5) | <0.001* |
| Death from chronic lower respiratory disease | ||||||
| Tobacco store density | 0.46 (0.30 to 0.71) | <0.001* | 0.44 (0.33 to 0.82) | <0.001* | 0.40 (0.29 to 0.55) | 0.03* |
| Alcohol store density | 0.23 (0.15 to 0.39) | 0.002* | – | – | 0.09 (−2.4 to 0.5) | 0.52 |
| Fast food store density | 0.14 (−0.03 to 0.22) | 0.06 | – | – | 0.02 (−0.7 to 1×10−3) | 0.80 |
| Median household income § | 0.08 (−32.3 to 0.91) | 0.07 | 0.43 (−0.07 to 28.2) | 0.10 | 0.45 (−0.01 to 3.1) | 0.45 |
| African-American (%) | 2.7 (1.5 to 5.1) | 0.001* | 4.3 (3.0 to 7.5) | <0.001* | 4.4 (3.7 to 6.1) | 0.04* |
| Bachelor’s degree | −5.0 (−10.9 to 2.2) | 0.07 | −7.4 (−2.8 to −11.6) | 0.001* | −7.6 (−5.1 to −11.8) | 0.003* |
| Age > 65 years (%) | −26.6 (−12.9 to −41.8) | <0.001* | −13.4 (−4.6 to −22.1) | 0.03* | −13.4 (−9.3 to −21.9) | <0.001* |
Indicates statistically significant (P<0.05).
Adjusted model including tobacco store densities and neighbourhood demographic variables (median household income, percentage of population aged >65, percentage who have completed a bachelor’s degree and percentage of African-Americans).
Adjusted included all three store densities and neighbourhood demographic variables (median household income, percentage of population aged >65, percentage who have completed a bachelor’s degree and percentage of African-Americans).
Note that the median household income was scaled to $10 000.
After adjusting for median neighbourhood income, race, education and age, tobacco store density continued to be associated with a lower life expectancy (β =−0.12, P<0.001) and a higher age-adjusted mortality (β =1.0, P<0.001) and death from chronic lower respiratory disease (β =0.44, P<0.001). However, median household income no longer had a statistically significant association with life expectancy or age-adjusted mortality (table 3). When adjusting for the above covariates (ie, neighbourhood characteristics), in addition to alcohol and fast food store density, tobacco store density continued to have an independent statistically significant adverse link to life expectancy (β =−0.10, P<0.001), age-adjusted mortality (β =0.67, P=0.002) and death from chronic lower respiratory disease (β =0.40, P=0.03) (table 3). Alcohol store density was adversely associated with life expectancy and age-adjusted mortality but not death from chronic lower respiratory disease. Neighbourhood income and fast food store density were no longer associated with measured health outcomes.
In sensitivity analysis, excluding the neighbourhood with tobacco store density of 130.3 per 10 000 residents did not significantly change the results of the regression models (data not shown).
DISCUSSION
In this study of Baltimore City, lower-income neighbourhoods had higher density of tobacco stores and lower life expectancy, higher age-adjusted mortality and higher death from chronic lower respiratory disease. Importantly, this study showed that higher tobacco store density was independently associated with worse health outcomes, even after adjusting for spatial autocorrelation, alcohol and fast food store densities and neighbourhood characteristics such as race, education, income and age. Interestingly, in adjusted models, neighbourhood income was no longer statistically significantly associated with health outcomes, suggesting that the social gradient in health outcomes experienced by low-income communities is complex, multifactorial and explained in part by the social conditions of the neighbourhood, including presence of tobacco stores. Together, these findings highlight how efforts of medical initiatives alone will not be sufficient to overcome the health inequities experienced by socioeconomically disadvantaged communities.
Tobacco use continues to be the leading cause of preventable morbidity and mortality in the USA.18 Through policies and campaigns that both raise the awareness of tobacco health harms and challenge tobacco accessibility, there has been a decline in cigarette smoking over the past several decades among adults in the USA, reaching the current nadir of 16.8% of smokers in the general population.19 However, this decline has not been met uniformly among the American population, with socioeconomic disparities existing in cigarette smoking and secondhand exposure. For instance, 30% of adults living below poverty smoke well above the general average, and secondhand smoke remains higher in children living in poverty.15,19,20
There are several factors that may contribute to the higher smoking and secondhand smoke rates in low-income settings. One possible explanation is the higher tobacco store density in neighbourhoods with lower SES, demonstrated in our study and others.12,21–23 In addition to the current work, Fakunle et al showed a similar inverse relationship between median household income and tobacco store density in another mid-Atlantic region—Prince George’s County, Maryland.24 It is unclear if and how the presence of tobacco stores directly leads to higher rates of tobacco use in the neighbourhood, but it is likely that the high density of tobacco stores results in the local increase of supply of tobacco products. In addition, it may also create a competitive local market with reduced product costs, resulting in an accessible and inexpensive product available to socioeconomically vulnerable populations. Further, it is probable that the high density of tobacco stores influences local neighbourhood norms that support smoking13 and smoking consumption.25,26
Importantly, this study builds on prior publications of tobacco store density neighbourhood distribution by highlighting that the presence of higher tobacco store densities was also associated with worse health outcomes. Tobacco store density was associated with these health outcomes, including lower life expectancy and higher age-adjusted mortality, even after adjusting for other store densities and neighbourhood demographics. In addition, tobacco store density, but not alcohol or fast food density, was also associated with higher death from chronic lower respiratory disease. This is not surprising as tobacco smoking is the leading cause of chronic obstructive pulmonary disease and is a known contributor to asthma and lower respiratory infections. Furthermore, understanding modifiable contributions to death from chronic lower respiratory disease is a priority as it is a prevalent cause of death in all of the 55 neighbourhoods (and the number 5 cause of death in Baltimore City as a whole in the 2011 Neighborhood Profile Data).14
These results illustrate that disproportionate access to tobacco products in low-income neighbourhoods is associated with significant negative health outcomes. Given these findings, attention towards implementing public health policies targeting reduction of tobacco stores in such communities may be warranted. There is a comparable analogy regarding alcohol access and alcohol consumption and its impact on morbidity and mortality in diverse communities.27 Policies have been implemented in order to reduce alcohol access in socioeconomically disadvantaged communities, resulting in positive health and social outcomes from diverse areas.27–29 Baltimore City implemented an alcohol zoning policy in 1971, and a liquor zoning law passed in 2016, aimed at removing liquor stores from residential neighbourhoods.30 Yet, for tobacco stores and retailers, similar policies do not exist in Baltimore City, resulting in some neighbourhoods with tobacco store densities that is more than five times that of the collective median for alcohol store density. The Institute of Medicine and several other organisations have called for a restriction on the number of tobacco stores allowed in communities.31 Such advocacy has the potential to address the health disparities influenced by tobacco.
Interestingly, income did not retain its statistical significance in our adjusted models on health outcomes. Income inequality has been linked with negative effects on a community’s overall health,32,33 but conflicting data to this conclusion have emerged.34–36 In a recent systematic review, the author argues that other demographic variables (such as age) and the health outcome variable of interest impact how income inequality relates to aggregate health.37 For example, in our study, other neighbourhood characteristics, in particular tobacco store density, offset income’s influence on a neighbourhood’s total health. Further, another socioeconomic variable, neighbourhood education, retained a significant association with life expectancy and age-adjusted mortality in the majority of regression models, suggesting that other demographic characteristics linked to income levels may explain a large proportion of the income-based health disparities. Education, for instance, may reflect certain non-socioeconomic characteristics that impact health outcomes (eg, problem-solving skills), which may be able to offset adversities posed by poverty itself.38 Therefore, how income impacts health outcomes in the sense of disease and disease management must be taken into account with other socioeconomic variables, both at the individual (educational status) and community (tobacco store densities) levels.
The findings of this study must be viewed in the context of the following limitations. First, individual behaviours were not addressed. While an increase in availability likely leads to acceptance of the usage of products, causal relationships cannot be determined. Second, the proximity of tobacco store retailers with homes, public housing units and schools was not defined, and such information may provide further insight into behaviour and marketing. Also store size and hours of operation were not reported, which may influence purchasing behaviours. Finally, information on other health-related outcomes, such as cancer and cardiac disease, was not included in our analysis, but warrants investigation as tobacco has been shown to be a risk factor for several morbidities. However, commonly used measures of community health outcomes including life expectancy and age-adjusted mortality were reported. Life expectancy estimated at birth is defined as the mean number of years a person born in a given year is expected to live.39 It is based on the mortality rates among a population within a given age group of a predefined area, while assuming these current age-specific mortality rates remain constant over time.39 Age-adjusted mortality, on the other hand, represents the number of deaths per 10 000 people per year, adjusted for neighbourhoods with a proportionally large number of elderly people.18 The association between tobacco store densities and death from chronic lower respiratory disease was not surprising as the negative impact by tobacco use on the lungs has been well documented.15,19,20 These results are consistent across different measures which shows the robustness and likely validity of our findings.
In conclusion, the relationships between neighbourhood SES, tobacco store density and major health outcomes are demonstrated in this study. These findings add to the growing body of evidence that poorer neighbourhoods have greater accessibility to tobacco products. However, further insight is provided into the association between tobacco store density and health outcomes, including neighbourhood life expectancy, age-adjusted mortality and death from chronic lower respiratory disease. Policies addressing not only financial inequities of neighbourhoods, but also tobacco store distribution, are likely needed to impact health. These results suggest that health inequities must be approached in a multidisciplinary fashion to offset the socioeconomic disparities that in turn impact health outcomes.
Supplementary Material
What this paper adds.
-
►
The high density of tobacco stores in low-income neighbourhoods has been well documented. Substantial evidence has recognised that communities’ socioeconomic characteristics influence the health of an individual through multiple pathways. However, whether the density of tobacco stores is associated with the health of a community is not known.
-
►
This paper shows that tobacco store density was associated with specific health outcomes, such as life expectancy, age-adjusted mortality and death from chronic lower respiratory disease. Such findings highlight how efforts of medical initiatives alone will not be sufficient to overcome the health disparities experienced by socioeconomically disadvantaged communities.
Footnotes
Additional material is published online only. To view please visit the journal online (http://dx.doi.org/10.1136/tobaccocontrol-2017-053945).
Contributors: All authors contributed to the writing of this manuscript. PG and NH prepared the concept, writing and review of the preliminary manuscripts. CR, MM, EB and NP all contributed in reviewing the data and discussing of the conclusions. PG, CK, SH and JP prepared and analysed the data.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Our data are drawn from the Baltimore City Health Department. Data may be made available upon request via email.
References
- 1.Abramson JH, Gofin R, Habib J, et al. Indicators of social class. A comparative appraisal of measures for use in epidemiological studies. Soc Sci Med. 1982;16:1739–46. doi: 10.1016/0277-9536(82)90267-2. [DOI] [PubMed] [Google Scholar]
- 2.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 3.Smith GD, Hart C, Blane D, et al. Adverse socioeconomic conditions in childhood and cause specific adult mortality: prospective observational study. BMJ. 1998;316:1631–5. doi: 10.1136/bmj.316.7145.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahkonen O, Lahelma E, Huuhka M. Past or present? Childhood living conditions and current socioeconomic status as determinants of adult health. Soc Sci Med. 1997;44:327–36. doi: 10.1016/s0277-9536(96)00102-5. [DOI] [PubMed] [Google Scholar]
- 5.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 6.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55:111–22. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: social processes and new directions in research. Annu Rev Sociol. 2002;28:443–78. [Google Scholar]
- 8.Marmot M. Inequalities in health. N Engl J Med. 2001;345:134–6. doi: 10.1056/NEJM200107123450210. [DOI] [PubMed] [Google Scholar]
- 9.Yu D, Peterson NA, Sheffer MA, et al. Tobacco outlet density and demographics: analysing the relationships with a spatial regression approach. Public Health. 2010;124:412–6. doi: 10.1016/j.puhe.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Wood LJ, Pereira G, Middleton N, et al. Socioeconomic area disparities in tobacco retail outlet density: a Western Australian analysis. Med J Aust. 2013;198:489–91. doi: 10.5694/mja12.11539. [DOI] [PubMed] [Google Scholar]
- 11.Shortt NK, Tisch C, Pearce J, et al. A cross-sectional analysis of the relationship between tobacco and alcohol outlet density and neighbourhood deprivation. BMC Public Health. 2015;15:1014. doi: 10.1186/s12889-015-2321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marashi-Pour S, Cretikos M, Lyons C, et al. The association between the density of retail tobacco outlets, individual smoking status, neighbourhood socioeconomic status and school locations in New South Wales, Australia. Spat Spatiotemporal Epidemiol. 2015;12:1–7. doi: 10.1016/j.sste.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 13.HubPages. Independent cities of the United States. http://hubpages.com/travel/Independent-Cities-of-the-United-States (accessed 30 Oct 2016).
- 14.BaltimoreCity Health Department. Neighborhood health profiles. http://health.baltimorecity.gov/stats-and-data (accessed 13 May 2016).
- 15.Homa DM, Neff LJ, King BA, et al. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke–United States, 1999-2012. MMWR Morb Mortal Wkly Rep. 2015;64:103–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Zager S, Mendu ML, Chang D, et al. Neighborhood poverty rate and mortality in patients receiving critical care in the academic medical center setting. Chest. 2011;139:1368–79. doi: 10.1378/chest.10-2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anselin L, Rey S. Properties of tests for spatial dependence in linear regression models. Geogr Anal. 1991;23:112–31. [Google Scholar]
- 18.Klein RJ, Schoenborn CA. Age-adjustmentusing the 2000 projected US population Healthy people statistical notes. Hyattsville, Maryland: National Center for Health Statistics; 2001. https://www.cdc.gov/nchs/data/statnt/statnt20.pdf (accessed 27 Feb 2017). [Google Scholar]
- 19.The health consequences of smoking – 50 years of progress: a report of the surgeon general. Atlanta: US Department of Health and Human Services; 2014. [Google Scholar]
- 20.Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep. 2015;64:1233–40. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- 21.Loomis BR, Kim AE, Goetz JL, et al. Density of tobacco retailers and its association with sociodemographic characteristics of communities across New York. Public Health. 2013;127:333–8. doi: 10.1016/j.puhe.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Duncan DT, Kawachi I, Melly SJ, et al. Demographic disparities in the tobacco retail environment in Boston: a citywide spatial analysis. Public Health Rep. 2014;129:209–15. doi: 10.1177/003335491412900217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JG, Sun DL, Schleicher NM, et al. Inequalities in tobacco outlet density by race, ethnicity and socioeconomic status, 2012, USA: results from the ASPiRE Study. J Epidemiol Community Health. 2017;71:487–92. doi: 10.1136/jech-2016-208475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fakunle DO, Milam AJ, Furr-Holden CD, et al. The inequitable distribution of tobacco outlet density: the role of income in two Black Mid-Atlantic geopolitical areas. Public Health. 2016;136:35–40. doi: 10.1016/j.puhe.2016.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Novak SP, Reardon SF, Raudenbush SW, et al. Retail tobacco outlet density and youth cigarette smoking: a propensity-modeling approach. Am J Public Health. 2006;96:670–6. doi: 10.2105/AJPH.2004.061622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reitzel LR, Cromley EK, Li Y, et al. The effect of tobacco outlet density and proximity on smoking cessation. Am J Public Health. 2011;101:315–20. doi: 10.2105/AJPH.2010.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fone D, Dunstan F, White J, et al. Change in alcohol outlet density and alcohol-related harm to population health (CHALICE) BMC Public Health. 2012;12:428. doi: 10.1186/1471-2458-12-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Hatcher B, Clarkson L, et al. Changes in density of on-premises alcohol outlets and impact on violent crime, Atlanta, Georgia, 1997-2007. Prev Chronic Dis. 2015;12:E84. doi: 10.5888/pcd12.140317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fitterer JL, Nelson TA, Stockwell T. A review of existing studies reporting the negative effects of alcohol access and positive effects of alcohol control policies on interpersonal violence. Front Public Health. 2015;3:253. doi: 10.3389/fpubh.2015.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Broadwater L. Overobjections, Baltimore city council OKs historic rewrite of zoningcode. 2016 http://www.baltimoresun.com/news/maryland/baltimorecity/bs-md-ci-rezoning-20161024-story.html (accessed 13 Dec 2016).
- 31.Institute of Medicine. Ending the tobacco problem: a blueprint for the nation. Washington, DC: Institute of Medicine of the National Academies; 2007. [Google Scholar]
- 32.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304:165–8. doi: 10.1136/bmj.304.6820.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnston R, Jen M-H, Jones K. On inequality and health, again: a response to Bernburg, and Barford, Dorling and Pickett. Soc Sci Med. 2010;70:498–500. [Google Scholar]
- 34.Marmot M. Social determinants of health inequalities. The Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 35.Macinko JA, Shi L, Starfield B, et al. Income inequality and health: a critical review of the literature. Med Care Res Rev. 2003;60:407–52. doi: 10.1177/1077558703257169. [DOI] [PubMed] [Google Scholar]
- 36.Lynch J, Smith GD, Harper S, et al. Is income inequality a determinant of population health? Part 1. a systematic review. Milbank Q. 2004;82:5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim KT. The relationships between income inequality, welfare regimes and aggregate health: a systematic review. Eur J Public Health. 2017;27:397–404. doi: 10.1093/eurpub/ckx055. [DOI] [PubMed] [Google Scholar]
- 38.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–88. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 39.Silcocks PB, Jenner DA, Reza R. Life expectancy as a summary of mortality in a population: statistical considerations and suitability for use by health authorities. J Epidemiol Community Health. 2001;55:38–43. doi: 10.1136/jech.55.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


