Abstract
Objective
High anxiety sensitivity (AS) and poor attention control (AC) are established risk factors for post-traumatic stress symptoms (PTSS), but little is known about the combined influence of these variables. Consistent with dual systems models suggesting facets of executive function (e.g., AC) will modulate the effects of other risk factors (e.g., AS), the current study evaluated the singular and interactive effects of these variables on PTSD symptoms.
Method
In study 1, latent variable modeling was used to examine the unique and interactive effects of AS and AC on PTSS, controlling for trauma history, sex, and age, in a sample of trauma exposed, community adults (N = 670). In study 2, latent variable modeling is used to replicate these effects in a sample of trauma exposed, treatment seeking adults (N = 207).
Results
Findings from both studies demonstrated a significant and negative interaction between AS and AC predicting PTSS when controlling for trauma history, sex, and age. Moreover, results revealed that AS more strongly predicts PTSS among those with poor AC.
Conclusions
These findings suggest that impaired AC, one facet of executive function, may potentiate the effects of AS on PTSS and increasing levels of AS may enhance the effects of AC on PTSS. Results are discussed within the context of a dual-systems model of PTSS.
1. Introduction
Trauma exposure is highly prevalent and linked to a range of adverse psychological outcomes, most notably post-traumatic stress symptoms (PTSS) and the subsequent development of post-traumatic stress disorder (PTSD; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Until recently (Bardeen & Fergus, 2015), explanatory accounts of PTSS that have focused on cognitive-affective vulnerability (e.g., Elwood, Hahn, Olatunji, & Williams, 2009) or facets of executive function (e.g., Aupperle, Melrose, Stein, & Paulus, 2012; Vasterling et al., 2002) have neglected the potential ways in which these systems may interact to produce greater dysfunction (Beevers, 2005; Gyurak, Gross, & Etkin, 2011; Otto et al., 2016; Ouimet, Gawronski, & Dozois, 2009). To reinforce the critical value of studying these processes in tandem, the present study evaluated the unique and interactive effects of one cognitive-affective risk factor, elevated anxiety sensitivity (AS; Reiss, Peterson, Gursky, & McNally, 1986), and a facet of executive function, poor attentional control (AC; Derryberry & Reed, 2002), on PTSS among trauma-exposed community and clinical populations.
AS, referred to as the “fear of fear,” is a cognitive-affective risk factor that reflects the sensitivity to benign symptoms of physiological arousal (e.g., a racing heart) stemming from the faulty belief that these sensations are potentially harmful or dangerous. AS is believed to arise at least in part due to learned associations between anxiety-related symptoms and negative internal or external stimuli (Schmidt, Lerew, & Joiner, 2000) culminating in the rapid, automatic interpretation of these sensations as indicative of harm. This faulty interpretation subsequently amplifies the individual’s anxiety symptoms through a positive feedback loop in which they react fearfully to sensations of anxiety, thereby producing more anxiety. Thus, AS is comprised of both a cognitive component (i.e., automatic, faulty interpretations) and affective component (i.e., anxiety-related symptomology).
AS is believed to contribute to PTSS via amplified anxious arousal during the traumatic event as well as in response to subsequent trauma cues (Taylor, 2003). Several studies have empirically demonstrated the relationship between AS and PTSS (e.g., Lang, Kennedy, & Stein, 2002; Norr, Albanese, Boffa, Short, & Schmidt, 2016). For instance, Olatunji and Fan (2015) showed that higher AS predicts elevated physiological arousal while viewing a trauma-film and greater trauma-related intrusive thoughts throughout a 1-week follow-up. Moreover, Boffa et al. (2016) revealed that AS prior to a campus shooting prospectively predicts the development of PTSS.
AC is conceptualized as a facet of executive function, and reflects the ability to willfully direct attention towards or away from specific stimuli (Eyesenk, Derakshan, Santos, & Calvo, 2007; Miyake et al., 2000). Weak AC is believed to confer risk for PTSS via a diminished capacity to direct attention away from threatening stimuli, resulting in greater anxious arousal and decreased recovery when confronted with trauma reminders (Aupperle et al., 2012). Empirical studies have demonstrated AC impairments to be associated with PTSS (Pineles, Shipherd, Mostoufi, Abramovitz, & Yovel, 2009; Pineles, Shipherd, Welch, & Yovel, 2007; Vasterling et al., 2002). For instance, Pineles et al. (2007) found that veterans with high PTSS displayed greater difficulties disengaging attention from threat-relevant words than veterans with low PTSS. A follow-up study by Pineles et al. (2009) found that difficulties disengaging attention from trauma-relevant words differentiated sexual assault survivors with high PTSS from those with low PTSS. Thus, both theoretical models (Aupperle et al., 2012) and empirical evidence (e.g., Pineles et al., 2009; Pineles et al., 2007) support that AC is one facet of executive control that contributes to PTSS.
It is plausible that AC has a moderating influence on AS, such that the relationship between AS and PTSS may be strongest at low levels of AC. If supported, this moderating influence of AC would be consistent with dual-systems models of psychopathology. Dual-systems models suggest that the influence of automatic processing (e.g., cognitive-affective factors such as AS) on clinical phenomena is greater among those with a poor ability to control information processing (e.g., facets of executive function such as AC). For example, Gyurak et al. (2011) reviewed literature demonstrating that emotion dysregulation is the product of strong automatic processing of emotional material and poor ability to engage in top-down, controlled processing. Similarly, Beevers (2005) proposed a dual-systems model in which depression is predicted by the interplay of depression-relevant automatic processing (i.e., cognitive-affective responses to stressors) and the capacity to control information processing. Finally, (Ouimet et al., 2009) proposed that pathological anxiety is, in part, the product of anxiety-relevant automatic and controlled processing.
There also exists precedent for conceptualizing AS within a dual-systems framework. AS is characterized by the rapid and catastrophic association of anxiety-related sensations with danger or harm (Reiss & McNally, 1985), suggesting that this cognitive-affective risk factor is marked by automatic, associative processing. Indeed, Otto et al. (2016) proposed a dual-systems model of negative health behaviors in which AS was positioned as a facet of automatic processing that drives cognitive-affective reactivity that the influence of AS is moderated by a facet of executive function (i.e., working memory). Though Otto et al.’s (2016) proposal has yet to be empirically evaluated, their model highlights the potential utility of conceptualizing risk conferred by high AS within a dual-systems framework.
An interaction of AS and AC would also be consistent with the AC theory (Eysenck, Derakshan, Santos, & Calvo, 2007). AC theory postulates that increasing levels of anxiety results in poorer processing efficiency, such that greater cognitive resources are required to perform tasks effectively for individuals experiencing elevated anxiety. In line with this theory, individuals with high AS, who are likely to experience amplified arousal when confronted with a trauma reminder, may need to recruit greater cognitive resources to disengage attention from the trauma reminder and their subsequent anxiety-related sensations. Those with good AC may benefit from a greater capacity to disengage attention from trauma reminders and anxiety symptoms, thereby muting the amplification of anxiety by AS. However, poor AC (i.e., fewer baseline cognitive resources) may result in sustained attention on the trauma reminders and anxiety symptoms, and thus further amplification of the anxiety via high AS.
Consistent with a dual-system model relating AS and AC in PTSS, Bardeen and Fergus (2015) examined the interactive effects of AS and AC on PTSS in a large, trauma exposed sample recruited from an online crowd-sourcing marketplace. Results of this study found a marginally significant interaction suggesting that individuals with high AS and weak AC expressed the greatest overall PTSS. However, there are notable limitations to this study that may have prohibited magnitude of the interactive effect. First, these data were collected exclusively through an online crowdsourcing marketplace, which may not be representative of clinical populations with elevated PTSS. Second, the authors did not account for demographic covariates such as age and sex, which have consistently demonstrated associations with PTSS (e.g., Kessler et al., 1995; Norr et al., 2016). Lastly, the authors tested the interaction using manifest variables, as opposed to latent variables, which may have reduced power to detect a significant interaction effect. Testing interactions using latent variables has many advantages over the use of manifest variables, such as less measurement error and more sensitivity to detect interactive effects (Muthén & Muthén, 2009).
The current study was designed to test a dual-systems model of PTSD by testing the unique and interactive effects of AS and AC on PTSS. To replicate the findings by Bardeen and Fergus (2015), we initially evaluated whether AS and AC interact to predict greater PTSS among a large sample of trauma-exposed community adults recruited from a crowdsourcing marketplace (study 1). We then evaluated the proposed interaction in a clinical sample of treatment-seeking, trauma-exposed adults (study 2). Based on prior research demonstrating that AS and AC exert direct effects on PTSS (e.g., Aupperle et al., 2012; Boffa et al., 2016) and preliminary evidence that AC and AS may have a modest interactive effect (Bardeen & Fergus, 2015), it was hypothesized that AS and AC would uniquely predict PTSS and that a significant and negative interaction between AS and AC would emerge in each sample. Specifically, it was predicted that individuals with high AS and low AC would display the greatest PTSS.
2. Study 1 - Method
2.1. Sample and setting
The sample in this study consisted of 670 trauma-exposed individuals recruited through an online crowd-sourcing marketplace through two studies with overlapping self-report measures. In this sample, ages ranged from 18 to 77 (M = 36.76, SD = 13.04). Participants were primarily female (69.6%). The racial/ethnic breakdown is as follows: 87.8% Caucasian, 6.3% African American, 2.8% Asian, 0.6% American Indian/Alaskan Native, 0.1% Native Hawaiian/Other Pacific Islander, and 2.4 % other.
2.2. Procedure
Participants were recruited to complete an online survey examining risk factors for anxiety and related pathology via Amazon’s Mechanical Turk (MTurk) at two time points conducted approximately one year apart. From this larger sample, a subset of trauma exposed participants were selected for the present investigation. Inclusion criteria for both studies were as follows: 18 years of age or older, living in the United States of America, and a record of high quality work on previous MTurk tasks as indexed by a Human Intelligence Task rating (a measure of data quality provided on prior tasks) greater than 90% (Paolacci & Chandler, 2014). Previous research has shown data collected through MTurk to be diverse and of high quality (Buhrmester, Kwang, & Gosling, 2011; Paolacci & Chandler, 2014). Further, samples recruited through this medium are considerably more diverse than typical student samples (Buhrmester et al., 2011). To ensure high quality data, validity items (e.g., “Are you reading this questionnaire?”) were included in the survey to detect random responding. Informed consent was obtained prior to data collection. All procedures were approved by the university’s institutional review board.
2.3 Measures
Anxiety Sensitivity Index – 3 (ASI-3)
The ASI-3 (Taylor et al., 2007) is an 18-item self-report measure that indexes the extent to which participants fear anxiety-related sensations (e.g., “It scares me when my heart beats rapidly”). Respondents indicate the degree to which they agree with each item on a 5-point Likert-type scale ranging from 0 (very little) to 5 (very much). The ASI-3 was adapted from the original ASI (Reiss et al., 1986) to provide improved psychometrics of the three most well-replicated subfactors of AS: cognitive concerns, physical concerns, and social concerns (Taylor et al., 2007). In the present study, only the ASI-3 total score was used. The ASI-3 has demonstrated strong psychometrics in previous research (Taylor et al., 2007). In this sample, the ASI-3 total score (α = .95) demonstrated excellent internal consistency.
Attentional Control Scale (ACS)
The ACS (Derryberry & Reed, 2002) is a 20-item self-report measure used to index individual differences in attentional control (e.g., “When trying to focus my attention on something, I have difficulty blocking out distractive thoughts”). Respondents indicate the degree to which each statement is consistent with their experience of attentional control on a 5-point Likert-type scale ranging from 1 (almost never) to 4 (always). Items are reverse-coded such that higher scores indicate greater attentional control. Two subscales comprise the ACS: Attentional Focus and Attentional Shifting (Judah, Grant, Mills, & Lechner, 2014). The ACS has demonstrated strong reliability (Derryberry & Reed, 2002) and convergent validity with behavioral and neural indices of attentional control and executive function (Judah et al., 2014; Mathews, Yiend, & Lawrence, 2004). Recent research has demonstrated that utilizing a subset of 11 of the original ACS items provides a better-fitting 2-factor structure, and that the 11-item ACS has strong psychometric properties (Judah et al., 2014). Thus, the abbreviated ACS was utilized in the current study. In the current study, the ACS total score (α = .84) demonstrated good internal consistency.
Post-traumatic Stress Disorder Checklist – Civilian (PCL-C)
The PCL-C (Weathers, Litz, Herman, Huska, & Keane, 1994) is a 17-item self-report measure used to assess the extent of PTSS experienced in the past month. Three subscales comprise the PCL-C: Avoidance, Hyperarousal, and Intrusions. Respondents indicate the degree to which they have experienced each item on a scale from 1 (not at all) to 5 (extremely), with greater scores reflecting greater PTSS [e.g., “Having physical reactions (e.g., heart pounding, trouble breathing, or sweating) when something reminded you of a stressful experience from the past?”]. The PCL-C was designed for use among civilian populations, and has shown strong reliability and internal consistency in previous research (Weathers et al., 1994). In the current study, the PCL-C total score (α = .96) demonstrated excellent internal consistency.
Post-traumatic Diagnostic Scale (PDS)
The PDS (Foa, 1995) includes a 12-item checklist of lifetime traumatic event exposure. Respondents were asked to indicate whether they experienced any of the 12 specified traumatic events [e.g., “Sexual assault by a stranger (for example, rape or attempted rape)”, “Military combat or war zone”]. In the current study, the PDS was used to screen individuals who reported experiencing a traumatic event from the parent sample as well as to provide a count of the number of types of traumatic events the individual has experienced to account for the effect of trauma history on PTSS (Foa, 1995).
2.4. Data Analytic Procedure
Descriptive statistics and correlations between all variables were first computed and reported using the scale scores. Confirmatory factor analysis (CFA) of item-level data was then used to fit the measurement models of AS (as indexed by the ASI-3), AC (as indexed by the ACS), and PTSS (as indexed by the PLC-C). CFAs were conducted using full information maximum likelihood and the robust maximum likelihood estimator (MLR) in Mplus (Muthén & Muthén, 2009). Fit for CFA and subsequent structural equation models (SEMs) were assessed using the likelihood ratio test (LRT). Fit indices were also examined to determine model fit because the LRT can be overly conservative (Kenny & McCoach, 2003; Moshagen, 2012). Fit indices included the comparative fit index (CFI), the standardized root mean square residual (SRMR), and the root mean square error of approximation (RMSEA) with accompanying 90% confidence intervals (CIs). CFI values above .90 indicated adequate fit. RMSEA values below .08 indicated adequate fit and values below .05 indicated good fit. In addition, RMSEA 90% CI values less than .05 indicated that a good-fitting model could not be rejected, and 90% CI values greater than .10 indicated that a poor-fitting model could not be rejected (Hu & Bentler, 1999; Kline, 2011).
Once measurement models were determined, SEMs were fit. SEMs were modeled using scale scores as indicators to maximize power. First, a SEM model to test the direct effects of AS and AC on PTSS was examined. Second, a SEM model testing the interaction of AS and AC was constructed. Because latent variable modeling with interactions is conducted using a quasi-maximum-likelihood design which does not provide the typical fit indices (Klein & Muthén, 2007), the necessity of the interaction term was determined by comparing the Y-B corrected -2loglikelihood values for the models with and without the interaction term (i.e., the baseline model), with a significant χ2 test of model fit indicating improved model fit with the inclusion of the interaction term. Finally, significant interactions were probed following procedures recommended by Aiken, West, and Reno (1991) in which the simple slopes of AS were examined 1 standard deviation above the mean, at the mean, and 1 standard deviation below the mean levels of AC. The simple slopes of AC were similarly examined at the corresponding levels of AS.
3. Study 1 - Results
3.2. Descriptive Statistics and Correlations
Descriptive statistics and correlations for scale scores for all measures can be found in Table 1. As anticipated, there were significant relations between AS, AC, and PTSS.
Table 1.
Study 1 – Community sample: Descriptives and Correlations
| Measures M (SD) | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. PCL-C 36.08 (18.64) |
1 | |||||
| 2. ASI-3 22.26 (17.30) |
.61*** | 1 | ||||
| 3. ACS 53.74 (10.82) |
−.36*** | −.48*** | 1 | |||
| 4. Number of Traumas 2.51 (1.66) |
.36*** | .08 | −.03 | 1 | ||
| 5. Age 36.76 (13.04) |
−.19*** | −.21*** | .17*** | .06 | 1 | |
| 6. Sex 69.6 (% female) |
.06 | .03 | −.03 | .05 | .07 | 1 |
Note. Post-Traumatic Stress Checklist – Civilian (PCL-C); Anxiety Sensitivity Index – 3 (ASI-3); Attentional Control Scale (ACS).
3.3. Confirmatory Factor Analysis Models of Anxiety Sensitivity, Attentional Control, and Post-traumatic Stress Symptoms
Second-order models were fit to demonstrate the proposed factor structure of each construct. A second-order model of AS, consisting of lower-order AS Cognitive Concerns, AS Physical Concerns, and AS Social Concerns factors, provided adequate fit to the data (Y-B χ2 = 712.51, df = 132, p < .001, CFI = .93, RMSEA = .08, 90% CI [.08, .09], SRMR = .05). Due to identification restraints, a correlated first-order model composed of lower-order Attention Focusing and Attention Shifting factors was assessed for model fit of AC. This model provided adequate model fit to the data (Y-B χ2 = 3564.28, df = 55, p < .001, CFI = .93, RMSEA = .09, 90% CI [.08, .10], SRMR = .06). A second-order model of PTSS, consisting of lower-order Avoidance, Hyperarousal, and Intrusions factors, provided adequate fit to the data (Y-B χ2 = 702.97, df = 116, p < .001, CFI = .94, RMSEA = .09, 90% CI [.08, .09], SRMR = .03).
3.4. Structural Equation Model Predicting Post-traumatic Stress Symptoms
To evaluate the unique effects of AC and AS on PTSS, a SEM model containing the AC factor, AS factor, trauma history, sex, and age was conducted. The main effects model examining the effects of AS, AC, trauma history and age on PTSS provided adequate fit to the data (Y-B χ2 = 174.55, df = 38, p < .001, CFI = .96, RMSEA = .07, 90% CI [.06, .08], SRMR = .06). PTSS shared significant associations with AS (B = .63, p < .001), trauma history (B = .33, p < .001), and age (B = −.08, p = .013). PTSS was marginally significantly associated with AC (B = −.08, p = .06) and was not significantly associated with sex (B = .04, p = .17).
3.5. Structural Equation Model Examining the Interactive Effects of Anxiety Sensitivity and Attentional Control
To evaluate the interactive effects of AS and AC on PTSS when accounting for trauma history, sex, and age, a SEM was conducted. Inclusion of the interaction term significantly improved model fit (adjusted χ2 = 5.612, p < .025). Results for the unique and interactive effects can be found in Table 2. In this model, PTSS was significantly and positively associated with AS (β = .60, p < .001), trauma history (β = .33, p < .001), and age (β = −.07, p = .01). PTSS was not significantly associated with AC (β = −.08, p = .15) or sex (β = .04, p = .13). The interaction between the AS and AC factors significantly predicted PTSS (β = −.07, p = .01; see Figure 1).
Table 2.
Study 1 – Community sample: Direct and Interactive Effects of Anxiety Sensitivity and Attentional Control on PTS Symptoms
| PTSS | ||
|---|---|---|
|
| ||
| B | SE | |
| AS | 0.60*** | 0.06 |
| AC | −0.08 | 0.06 |
| AS × AC | −0.07* | 0.03 |
| Number of Traumas | 0.33*** | 0.03 |
| Sex | 0.04 | 0.03 |
| Age | −0.07* | 0.03 |
Note. AS = anxiety sensitivity factor; AC = attentional control factor; PTSS = Post-traumatic stress symptoms factor; AS × AC = interaction term for AS and AC factors.
p < .05;
p < .001.
Figure 1.
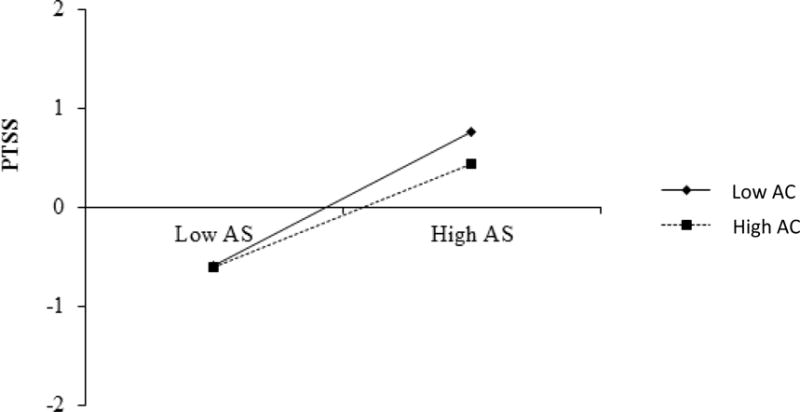
Study 1 – Community sample. The effects of Anxiety Sensitivity (AS) predicting PTSS (by standard deviations [SDs]) at Attentional Control levels 1 SD below the mean (Low ACS) and 1 SD above the mean (High ACS) in study 1.
Next, the simple slopes of each factor comprising the interaction were examined to probe the interactive effects. AS significantly and positively predicted PTSS at all levels of AC. Interestingly, AS was a more robust predictor of PTSS for individuals with weak AC (i.e., 1 standard deviation below the mean; β = .67, p < .001) compared to mean levels of AC (β = .60, p < .001) and good AC (i.e., 1 standard deviation above the mean; β = .53, p < .001). In contrast, AC significantly and negatively predicted PTSS at high levels of AS (i.e., 1 standard deviation above the mean; β = −.16, p = .03), but did not significantly predict PTSS at mean levels of AS (β = −.08, p = .14) or low levels of AS (i.e., 1 standard deviation below the mean; β = −.01, p = .84).
4. Study 2 – Method
Two limitations of the Study 1 findings are that the participants were community adults uncharacterized with regard to psychopathology and that participants were predominantly Caucasian, representing less-than-desirable diversity. As a more stringent test of the interaction of the AS and AC factors predicting PTSS, we replicated these findings in a clinical sample of trauma-exposed individuals.
4.2. Sample and setting
The sample in this study consisted of 207 trauma-exposed individuals who presented for a study assessing a brief, computerized intervention. In this sample, ages ranged from 18 to 79 (M = 36.66, SD = 15.61). Participants were primarily female (56.0%). The racial/ethnic breakdown is as follows: 55.1% Caucasian, 29.5% African American, 1.9% Asian, 0.5% Native Hawaiian/Other Pacific Islander, and 13.0% other. Of the 207 participants, 57 individuals were determined to have PTSS severe enough to warrant a PTSD diagnosis as assessed using the Structured Clinical Interview for DSM-5 (SCID-5-RV; First et al., 2015).
4.3. Procedure
Participants were recruited from the community based on their report risk factors for suicidality to participate in a larger clinical trial of two interventions each consisting of one session of computerized psychoeducation followed by three sessions of cognitive bias modification training. Participants were recruited based on elevations on one of several risk factors for suicidality (AS cognitive concerns, thwarted belongingness, perceived burdensomeness; Daniel W. Capron et al., 2012; Van Orden et al., 2010) though suicidal ideation was not a necessary inclusionary criteria. All data used in the current study were collected prior to randomization and intervention. Interested participants responded to flyers, newspaper advertisements, and social media postings by calling the laboratory and completing a brief telephone screen. Those who were potentially eligible were scheduled for a baseline assessment, during which they completed the Structured Clinical Interview for DSM-5-Research Version (SCID-5-RV; First, Williams, Karg, & Spitzer, 2015), and a battery of self-report questionnaires. All participants provided written informed consent and all study procedures were approved by the university’s institutional review board.
4.4. Measures
Anxiety Sensitivity Index – 3 (ASI-3)
See previous description of the ASI-3 (Taylor et al., 2007). In this sample, the ASI-3 total score (α = .94) demonstrated excellent internal consistency.
Attentional Control Scale (ACS)
See previous description of the ACS (Derryberry & Reed, 2002). In the current study, the ACS total score (α = .88) demonstrated good internal consistency.
Post-traumatic Stress Checklist – Civilian (PCL-C)
See previous description of the PCL-C (Weathers et al., 1994). In the current study, the PCL-C total score (α = .95) demonstrated excellent internal consistency.
Post-traumatic Diagnostic Scale (PDS)
See previous description of the PDS (Foa, 1995).
Structured Clinical Interview for DSM-5 (SCID-5-RV)
PTSD diagnoses were determined using the SCID-5-RV (First et al., 2015). The SCID-5-RV was administered by trained doctoral level therapists who completed extensive training in SCID-5-RV administration and scoring. All results were reviewed by a licensed clinical psychologist to ensure accurate diagnoses.
3.5 Data Analytic Procedure
The data analytic procedure for Study 2 was identical to that of Study 1. See previous description for the full data analytic procedure.
5. Study 2 - Results
5.2. Descriptive Statistics and Correlations
Descriptive statistics and correlations for scale scores for all measures can be found in Table 3. As anticipated, there were significant relations between AS, AC, and PTSS.
Table 3.
Study 2 – Clinical Sample: Descriptives and Correlations
| Measures M (SD) | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. PCL-C 46.55 (17.22) |
1 | |||||
| 2. ASI-3 32.75 (17.34) |
.54*** | 1 | ||||
| 3. ACS 27.38 (5.97) |
−.40*** | −.43*** | 1 | |||
| 4. Number of Traumas 3.52 (2.16) |
.41*** | .18* | .09 | 1 | ||
| 5. Age 36.66 (15.61) |
.08 | −.01 | .13 | .45*** | 1 | |
| 6. Gender 56.0 (% female) |
.08 | .15* | −.18* | −.17* | −.25*** | 1 |
Note. Post-Traumatic Checklist – Civilian (PCL-C); Anxiety Sensitivity Index – 3 (ASI-3); Attentional Control Scale (ACS).
5.3. Confirmatory Factor Analysis Models of Anxiety Sensitivity, Attentional Control, and Post-traumatic Stress Symptoms
Second-order models were fit to demonstrate the proposed factor structure of each construct. A second-order model of AS, consisting of lower-order AS Cognitive Concerns, AS Physical Concerns, and AS Social Concerns factors, provided adequate fit to the data (Y-B χ2 = 275.59, df = 132, p < .001, CFI = .94, RMSEA = .07, 90% CI [.06, .09], SRMR = .06). The correlated first-order model composed of the attention focusing and attention shifting subfactors of AC provided adequate model fit to the data (Y-B χ2 = 72.85, df = 43, p = .003, CFI = .95, RMSEA = .06, 90% CI [.04, .09], SRMR = .05). A second-order model of PTSS, consisting of lower-order Avoidance, Hyperarousal, and Intrusions factors, provided adequate fit to the data (Y-B χ2 = 350.77, df = 114, p < .001, CFI = .90, RMSEA = .10, 90% CI [.09, .11], SRMR = .05).
5.4. Structural Equation Model Predicting Post-traumatic Stress Symptoms
To evaluate the unique effects of AC and AS on PTSS, a SEM model containing the AC factor, AS factor, trauma history, sex, and age was conducted. The main effects model examining the effects of AS, AC, trauma history and age on PTSS provided adequate fit to the data (Y-B χ2 = 79.83, df = 38, p < .001, CFI = .95, RMSEA = .07, 90% CI [.05, .10], SRMR = .07). PTSS shared significant associations with AS (β = .44, p < .001), AC (β = −.24, p = .009), and trauma history (β = .40, p < .001). PTSS was not significantly associated with age (β = −.06, p = .37) or sex (β = .03, p = .67).
5.5. Structural Equation Model Examining the Interactive Effects of Anxiety Sensitivity and Attentional Control
To evaluate the interactive effects of AS and AC on PTSS when accounting for trauma history, sex, and age, a SEM was conducted. Inclusion of the interaction term significantly improved model fit (adjusted χ2 = 4.42, p < .05). Results for the unique and interactive effects can be found in Table 4. In this model, PTSS was significantly and positively associated with AS (β = .43, p < .001), AC (β = −.25, p = .007), and trauma history (β = .42, p < .001). PTSS was not significantly associated with age (β = −.09, p = .17) or sex (β = .02, p = .73). The interaction between the AS and AC factors significantly predicted PTSS (β = −.14, p = .02; see Figure 2).
Table 4.
Study 2 – Clinical Sample: Direct and Interactive Effects of Anxiety Sensitivity and Attentional Control on PTS Symptoms
| PTSS
|
||
|---|---|---|
| B | SE | |
| AS | 0.43*** | 0.09 |
| AC | −0.25** | 0.09 |
| AS × AC | −0.14* | 0.06 |
| Number of Traumas | 0.42*** | 0.07 |
| Sex | 0.02 | 0.06 |
| Age | −0.09 | 0.06 |
Note. AS = anxiety sensitivity factor; AC = attentional control factor; PTSS = Post-traumatic stress symptoms factor; AS × AC = interaction term for AS and AC factors.
p < .05;
p < .01;
p < .001.
Figure 2.
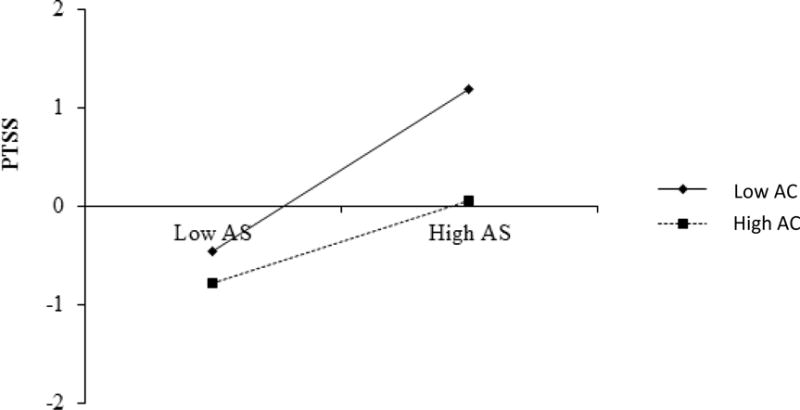
Study 2 – Clinical sample. The effects of Anxiety Sensitivity (AS) predicting PTSS (by standard deviations [SDs]) at Attentional Control levels 1 SD below the mean (Low ACS) and 1 SD above the mean (High ACS) in study 2.
Next, the simple slopes of each factor comprising the interaction were examined to probe the interactive effects. AS significantly and positively predicted PTSS at all levels of AC. Results demonstrated that AS was a more robust predictor of PTSS for individuals with weak AC (i.e., 1 standard deviation below the mean; β = .56, p < .001) compared to mean levels of AC (β = .43, p < .001) and good AC (i.e., 1 standard deviation above the mean; β = .29, p = .009). In contrast, AC significantly and negatively predicted PTSS at high levels of AS (i.e., 1 standard deviation above the mean; β = −.39, p = .001) and mean levels of AS (β = −.25, p = .01) but was not a significant predictor of PTSS at low levels of AS (i.e., 1 standard deviation below the mean; β = −.11, p = .35).
6. Discussion
The results of this study indicate that AS more robustly predicts PTSS among those with poor AC in community (study 1) and clinical (study 2) trauma-exposed populations. These findings add to literature by independently associating AS and AC with PTSS (e.g., Aupperle et al., 2012; Boffa et al., 2016) and extend prior research examining the interactive effects of AS and AC (Bardeen & Fergus, 2015). Importantly, the observed interaction was stronger among a trauma-exposed clinical sample (study 2; PCL-C M = 46.55, SD = 17.22) relative to a trauma-exposed community sample (study 1; PCL-C M = 36.08, SD = 18.64), suggesting that the moderating effects of poor AC on AS are stronger among those with more severe presentations (i.e., greater PTSS) or who are actively seeking treatment. This finding may help explain the previously reported marginally significant interactive effect reported by Bardeen and Fergus (2015) in a community sample.
It is plausible that individuals with high AS and weak AC experience more pronounced difficulty directing their attention away from salient, anxiety-related sensations to engage in regulatory coping strategies, effectively maintaining attention on threatening internal stimuli which further amplifies anxious arousal. In fact, one study demonstrated that poor AC enhanced fearful responding to anxiety-related sensations provoked using a biological challenge for trait anxious individuals (CO2 inhalation) and concluded that those with poor AC are likely to have greater difficulty disengaging attention from interoceptive threat (Richey, Keough, & Schmidt, 2012). Thus, the enhancement of AS-related risk among those with poor AC may influence PTSS through the amplification of emotionality when faced with trauma reminders and intrusive thoughts.
Further, it is reasonable to suggest that the heightened emotional responding stemming from the combination of high AS and weak AC may fuel avoidance of provocative stimuli, thereby prolonging and enhancing PTSS (Salters-Pedneault, Tull, & Roemer, 2004). This interpretation is consistent with other data showing that poor AC may inflate the influence of other vulnerabilities on anxiety symptoms and that good AC may act as a buffer against risk for anxiety pathology (Bardeen & Fergus, 2015) as well as broader dual-systems models of psychopathology (e.g., Beevers, 2005; Gyurak et al., 2011; Otto et al., 2016; Ouimet et al., 2009).
The current study found that AC, one facet of executive function, moderated the effect of AS on PTSS. However, it remains unclear if other facets of executive function will have a similar or more robust effect. For instance, Otto et al. (2016) postulate that working memory may have similar moderating effects on AS due to the role of working memory in regulating emotional reactivity to maintain adaptive, goal-directed behaviors. It is plausible that the combination of high AS with less capacity to regulate emotional and behavioral reactions to stressors would result in greater fear reactivity to and subsequent avoidance of trauma reminders. Given that working memory has also been linked with PTSS (Aupperle et al., 2012), it is important that future research evaluate this as an alternate moderator of the effect of AS on PTSS.
These results may help inform the development and utilization of targeted interventions for PTSS. Brief interventions (e.g., Capron & Schmidt, 2016; Clerkin, Beard, Fisher, & Schofield, 2015) that include both psychoeducation about the nature of anxiety-symptoms and exposure to previously feared anxiety symptoms have been shown to be an effective and potent method for reducing AS. Further, one study has shown that reductions in AS following a brief AS intervention significantly mediated reductions in PTSS (Allan, Short, Albanese, Keough, & Schmidt, 2015). Results showing that AS has a stronger relationship with PTSS among those with weak AC suggests that individuals with low AC may have more opportunity for PTSS reduction from AS interventions. Further, there is some evidence for the efficacy of interventions targeting AC through repeated engagement in tasks requiring AC engagement (Bherer et al., 2005). Given the limited efficacy of PTSD treatments (Resick, Nishith, Weaver, Astin, & Feuer, 2002), future research should evaluate the benefits of using both AS and AC training programs for individuals seeking PTSD amelioration.
6.1 Limitations
Several limitations to the current study should be noted, which point to opportunities for additional work. First, the present data are cross-sectional in nature, indicating that causality cannot be inferred. Future research should seek to extend this work by using longitudinal and experimental designs that allow researchers to test the temporal influence of the unique and interactive effects of AS and AC on PTSS. Second, not all participants in study 2 met full diagnostic criteria for PTSD. Though this allowed the researchers to utilize a broader range of PTSS severity, future research should evaluate if the interaction of AS and AC predicts symptom severity using larger samples of patients meeting criteria for PTSD. Lastly, the exclusive reliance on self-reported measures introduces potential reporting biases, which may be mitigated in future research through the use of behavioral and neural indices of AS and AC.
6.2 Conclusions
Despite these limitations, the present study contributes novel findings to a growing body of literature assessing risk factors for PTSS, and is the first to propose a dual-systems account of PTSS. Moreover, the importance and difficulty in replicating interactions (Jaccard & Wan, 1995) underscores the integrity of the interactive effect that the present study demonstrated in two distinct samples. Further evaluation of the utility of a dual-systems approach to PTSS is warranted, particularly with regard to the moderation of AS by other facets of executive control implicated in PTSS, such as working memory capacity (Otto et al., 2016). Future research may also investigate the influence of AS on PTSS among individuals at high and low risk for weak AC, such as those with a history of traumatic brain injury (Aupperle et al., 2012).
References
- Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- Allan NP, Short NA, Albanese BJ, Keough ME, Schmidt NB. Direct and mediating effects of an anxiety sensitivity intervention on posttraumatic stress disorder symptoms in trauma-exposed individuals. Cognitive Behaviour Therapy. 2015;44(6):512–524. doi: 10.1080/16506073.2015.1075227. [DOI] [PubMed] [Google Scholar]
- Aupperle RL, Melrose AJ, Stein MB, Paulus MP. Executive function and PTSD: disengaging from trauma. Neuropharmacology. 2012;62(2):686–694. doi: 10.1016/j.neuropharm.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA. Emotional distress intolerance, experiential avoidance, and anxiety sensitivity: The buffering effect of attentional control on associations with posttraumatic stress symptoms. Journal of Psychopathology and Behavioral Assessment. 2015:1–10. [Google Scholar]
- Beevers CG. Cognitive vulnerability to depression: A dual process model. Clinical Psychology Review. 2005;25(7):975–1002. doi: 10.1016/j.cpr.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Bherer L, Kramer AF, Peterson MS, Colcombe S, Erickson K, Becic E. Training effects on dual-task performance: are there age-related differences in plasticity of attentional control? Psychology and aging. 2005;20(4):695. doi: 10.1037/0882-7974.20.4.695. [DOI] [PubMed] [Google Scholar]
- Boffa JW, Norr AM, Raines AM, Albanese BJ, Short NA, Schmidt NB. Anxiety sensitivity prospectively predicts posttraumatic stress symptoms following a campus shooting. Behavior Therapy. 2016;47(3):367–376. doi: 10.1016/j.beth.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on psychological science. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Capron DW, Fitch K, Medley A, Blagg C, Mallott M, Joiner T. Role of anxiety sensitivity subfactors in suicidal ideation and suicide attempt history. Depression and Anxiety. 2012;29(3):195–201. doi: 10.1002/da.20871. [DOI] [PubMed] [Google Scholar]
- Capron DW, Schmidt NB. Development and randomized trial evaluation of a novel computer-delivered anxiety sensitivity intervention. Behaviour Research and Therapy. 2016;81:47–55. doi: 10.1016/j.brat.2016.04.001. [DOI] [PubMed] [Google Scholar]
- Clerkin EM, Beard C, Fisher CR, Schofield CA. An attempt to target anxiety sensitivity via cognitive bias modification. PLoS One. 2015;10(2):e0114578. doi: 10.1371/journal.pone.0114578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology. 2002;111(2):225–236. doi: 10.1037/0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- Elwood LS, Hahn KS, Olatunji BO, Williams NL. Cognitive vulnerabilities to the development of PTSD: A review of four vulnerabilities and the proposal of an integrative vulnerability model. Clinical Psychology Review. 2009;29(1):87–100. doi: 10.1016/j.cpr.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: Attentional control theory. Emotion. 2007;7(2):336–353. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5 - Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) Arlington, VA: American Psychiatric Association; 2015. [Google Scholar]
- Foa EB. Posttraumatic stress diagnostic scale manual. United States of America: National Computer Systems: Inc; 1995. [Google Scholar]
- Gyurak A, Gross JJ, Etkin A. Explicit and implicit emotion regulation: a dual-process framework. Cognition and Emotion. 2011;25(3):400–412. doi: 10.1080/02699931.2010.544160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Jaccard J, Wan CK. Measurement error in the analysis of interaction effects between continuous predictors using multiple regression: Multiple indicator and structural equation approaches. Psychological bulletin. 1995;117(2):348. [Google Scholar]
- Judah MR, Grant DM, Mills AC, Lechner WV. Factor structure and validation of the attentional control scale. Cognition & Emotion. 2014;28(3):433–451. doi: 10.1080/02699931.2013.835254. [DOI] [PubMed] [Google Scholar]
- Kenny DA, McCoach DB. Effect of the number of variables on measures of fit in structural equation modeling. Structural equation modeling. 2003;10(3):333–351. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klein AG, Muthén BO. Quasi-maximum likelihood estimation of structural equation models with multiple interaction and quadratic effects. Multivariate behavioral research. 2007;42(4):647–673. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford press; 2011. [Google Scholar]
- Lang AJ, Kennedy CM, Stein MB. Anxiety sensitivity and PTSD among female victims of intimate partner violence. Depression and Anxiety. 2002;16(2):77–83. doi: 10.1002/da.10062. [DOI] [PubMed] [Google Scholar]
- Mathews A, Yiend J, Lawrence AD. Individual differences in the modulation of fear-related brain activation by attentional control. Journal of Cognitive Neuroscience. 2004;16(10):1683–1694. doi: 10.1162/0898929042947810. [DOI] [PubMed] [Google Scholar]
- Moshagen M. The model size effect in SEM: Inflated goodness-of-fit statistics are due to the size of the covariance matrix. Structural Equation Modeling: A Multidisciplinary Journal. 2012;19(1):86–98. [Google Scholar]
- Muthén B, Muthén B. Statistical analysis with latent variables. Wiley; Hoboken: 2009. [Google Scholar]
- Norr AM, Albanese BJ, Boffa JW, Short NA, Schmidt NB. The relationship between gender and PTSD symptoms: Anxiety sensitivity as a mechanism. Personality and Individual Differences. 2016;90:210–213. [Google Scholar]
- Olatunji B, Fan Q. Anxiety sensitivity and post-traumatic stress reactions: Evidence for intrusions and physiological arousal as mediating and moderating mechanisms. Journal of Anxiety Disorders. 2015;34:76–85. doi: 10.1016/j.janxdis.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Otto MW, Eastman A, Lo S, Hearon BA, Bickel WK, Zvolensky M, Doan SN. Anxiety sensitivity and working memory capacity: Risk factors and targets for health behavior promotion. Clinical Psychology Review. 2016 doi: 10.1016/j.cpr.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Ouimet AJ, Gawronski B, Dozois DJ. Cognitive vulnerability to anxiety: A review and an integrative model. Clinical Psychology Review. 2009;29(6):459–470. doi: 10.1016/j.cpr.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Paolacci G, Chandler J. Inside the turk understanding mechanical turk as a participant pool. Current Directions in Psychological Science. 2014;23(3):184–188. [Google Scholar]
- Pineles SL, Shipherd JC, Mostoufi SM, Abramovitz SM, Yovel I. Attentional biases in PTSD: More evidence for interference. Behaviour Research and Therapy. 2009;47(12):1050–1057. doi: 10.1016/j.brat.2009.08.001. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Shipherd JC, Welch LP, Yovel I. The role of attentional biases in PTSD: Is it interference or facilitation? Behaviour Research and Therapy. 2007;45(8):1903–1913. doi: 10.1016/j.brat.2006.08.021. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. Theoretical Issues in Behavior Therapy. 1985:107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. http://dx.doi.org/10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70(4):867. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richey JA, Keough ME, Schmidt NB. Attentional control moderates fearful responding to a 35% CO 2 Challenge. Behavior Therapy. 2012;43(2):285–299. doi: 10.1016/j.beth.2011.06.004. [DOI] [PubMed] [Google Scholar]
- Salters-Pedneault K, Tull MT, Roemer L. The role of avoidance of emotional material in the anxiety disorders. Applied and Preventive Psychology. 2004;11(2):95–114. [Google Scholar]
- Schmidt NB, Lerew DR, Joiner TE. Prospective evaluation of the etiology of anxiety sensitivity: test of a scar model. Behaviour Research and Therapy. 2000;38(11):1083–1095. doi: 10.1016/s0005-7967(99)00138-2. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity and its implications for understanding and treating PTSD. Journal of Cognitive Psychotherapy. 2003;17(2):179–186. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. 2010;117(2):575. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasterling JJ, Duke LM, Brailey K, Constans JI, Allain AN, Sutker PB. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16(1):5. doi: 10.1037//0894-4105.16.1.5. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist-civilian version (PCL-C) Boston, MA: National Center for PTSD; 1994. [Google Scholar]


