Abstract
Objectives
To report the burden of cardiovascular diseases (CVD) in the Eastern Mediterranean Region (EMR) during 1990–2015.
Methods
We used the 2015 Global Burden of Disease study for estimates of mortality and disability-adjusted life years (DALYs) of different CVD in 22 countries of EMR.
Results
A total of 1.4 million CVD deaths (95% UI: 1.3–1.5) occurred in 2015 in the EMR, with the highest number of deaths in Pakistan (465,116) and the lowest number of deaths in Qatar (723). The age-standardized DALY rate per 100,000 decreased from 10,080 in 1990 to 8606 in 2015 (14.6% decrease). Afghanistan had the highest age-standardized DALY rate of CVD in both 1990 and 2015. Kuwait and Qatar had the lowest age-standardized DALY rates of CVD in 1990 and 2015, respectively. High blood pressure, high total cholesterol, and high body mass index were the leading risk factors for CVD.
Conclusions
The age-standardized DALY rates in the EMR are considerably higher than the global average. These findings call for a comprehensive approach to prevent and control the burden of CVD in the region.
Electronic supplementary material
The online version of this article (doi:10.1007/s00038-017-1012-3) contains supplementary material, which is available to authorized users.
Keywords: Cardiovascular disease, Burden of disease, Eastern Mediterranean Region
Introduction
The Global Burden of Disease (GBD) study documented that cardiovascular diseases (CVD) have been the leading cause of global mortality since 1980 (Institute for Health Metrics and Evaluation 2017; Mortality and Causes of Death 2016). CVD accounted for nearly one-third of all deaths worldwide in 2015. Meanwhile, the principal components of CVD, namely stroke and ischemic heart disease, accounted for 85.1% (95% uncertainty interval (UI): 84.7–85.5) of all deaths in the CVD category in 2015 (Mortality and Causes of Death 2016).
Although the age-standardized mortality rates of CVD have fallen by 27.3% in the last 25 years, the absolute number of deaths due to CVD increased globally by 42.4% between 1990 and 2015 (2017). Most CVD deaths occur in low- and middle-income countries (Mensah et al. 2015). The decline in age-standardized rates is mainly due to preventive interventions and better access to quality treatment for acute cardiovascular conditions such as myocardial infarction and stroke (Smith 2011). CVD also impose a high economic burden on health systems and society. For instance, CVD personal spending in the United States was estimated to be 231.1 billion USD in 2013 and was the largest disease category of personal health care spending (Dieleman et al. 2016).
The Eastern Mediterranean Region (EMR) comprises 22 countries with a population of nearly 580 million people, with a diverse range in per capita gross national product (maximum 83,990 USD for Qatar, minimum 610 USD for Afghanistan) (World Development Indicators database 2017). To the best of our knowledge, there is no comprehensive report on the burden and mortality of CVD in the EMR.
This study aimed to report findings on cardiovascular diseases between 1990 and 2015, from the Global Burden of Diseases, Injuries and Risk Factors Study (GBD 2015) in the 22 countries of the EMR. This would be help us better understand the burden of CVD and interventions needed to control these diseases.
Methods
GBD 2015 covers 195 countries, 21 regions, and seven super-regions from 1990 to 2015 for 315 diseases and injuries, 2619 unique sequelae, and 79 risk factors by age and sex. Detailed descriptions of the general methodological approach of GBD 2015 and specific methodology used for CVD have been provided elsewhere (GBD 2015 DALYs and Collaborators 2016; GBD 2015 Disease and Injury Prevalence Collaborators 2016; GBD 2015 Mortality and Causes of Death Collaborators 2016).
We evaluated the burden of CVD in the Eastern Mediterranean Region (EMR), which contains 22 countries: Afghanistan, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, the United Arab Emirates (UAE), and Yemen.
The category of CVD includes the ten most common global causes of CVD-related death: rheumatic heart disease, ischemic heart disease, cerebrovascular disease (ischemic stroke and hemorrhagic stroke), hypertensive heart disease, cardiomyopathy and myocarditis, atrial fibrillation and flutter, aortic aneurysm, peripheral vascular disease, endocarditis, and “other cardiovascular and circulatory diseases.” Electronic supplementary table S1 shows the International Classification of Diseases (ICD-10) codes for each of the cardiovascular causes.
To estimate the number of deaths due to CVD, we estimated all-cause mortality envelopes (total number of deaths) for each country-year during 1990–2015; we used all accessible data such as vital registration systems, sample registration data, and household recall of deaths. These sources were used as inputs for cause of death models. We used cause of death ensemble modeling (CODEm) to estimate the number of deaths for each CVD by age, sex, country, and year. The number of deaths for each cause and life tables for all-cause mortality were used to calculate years of life lost (YLLs) (GBD 2015 Morality and Causes of Death Collaborators 2016; Roth et al. 2015a, b).
We updated our previous systematic reviews for the GBD study separately for each of the non-fatal sequelae of CVD. Data on epidemiologic measures (incidence, prevalence, and case fatality) were extracted from 170 data sources. List of all sources (by cause and location) are available at the Institute for Health Metrics and Evaluation’s website (IHME 2016).
Bayesian meta-regression analysis through DisMod-MR 2.1 was used for disease modeling. Model-based prevalence estimates, in combination with disability weights, were used to calculate cause-specific years lived with disability (YLDs) for each age, sex, location, and year. Disability-adjusted life years (DALYs) were calculated through summation of YLLs and YLDs (DALYs and Collaborators 2016; Disease et al. 2016).
We report 95% uncertainty intervals (UI) for each estimate, including rates, numbers of deaths, and DALYs. We estimated UIs by taking 1000 samples from the posterior distribution of each quantity and using the 25th- and 975th-ordered draws of the uncertainty distribution.
Results
Mortality
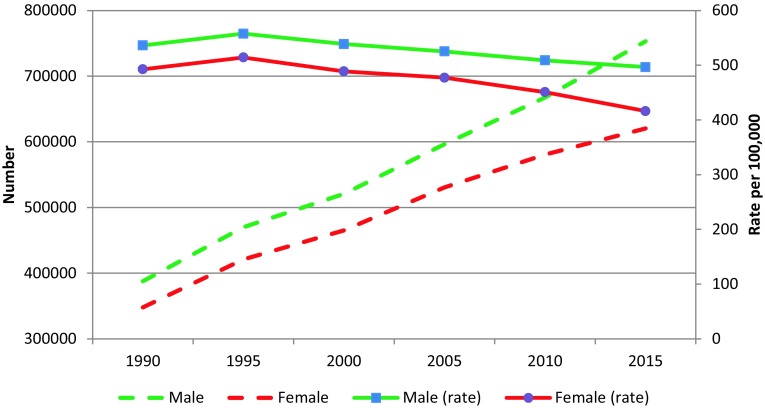
The CVD death rate per 100,000 population in the EMR decreased from 515.1 (95% UI: 491.7–541.5) in 1990 to 456.5 (95% UI: 431.5–484.2) in 2015 (Table 1). A total of 1,373,329 CVD deaths (95% UI: 1,290,959–1,465,047) occurred in 2015 in the EMR, 54.8% of which were among males. These deaths accounted for 34.1% (95% UI: 33.1–35.1) of all deaths in the region in 2015, compared to 30.2% (95% UI: 29.5–30.9) of all deaths in 1990. The number of men dying from CVD was consistently higher than the number of women during 1990–2015 (Fig. 1).
Table 1.
Total number of deaths and age-standardized mortality rates for cardiovascular diseases in 1990 and 2015, and percentage change, Global Burden of Disease study, Eastern Mediterranean Region, 1990–2015
| Cause | Number of deaths | Age-standardized death rate per 100,000 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | % Change | 1990 | 2105 | % Change | |||||
| Number | 95% UI | Number | 95% UI | Rate | 95% UI | Rate | 95% UI | |||
| Cardiovascular diseases | 735,689 | 700,875–773,593 | 1,373,329 | 1,290,959–1,465,047 | 86.7 | 515.1 | 491.7–541.5 | 456.5 | 431.5–484.2 | −11.4 |
| Rheumatic heart disease | 18,350 | 16,029–21,037 | 27,046 | 22,945–31,078 | 47.4 | 9.1 | 7.8–10.7 | 6.8 | 5.7–7.8 | −25.5 |
| Ischemic heart disease | 403,355 | 379,184–425,913 | 802,078 | 750,839–859,266 | 98.9 | 294.0 | 276.9–310.3 | 269.1 | 252.5–286.9 | −8.5 |
| Ischemic stroke | 92,230 | 79,786–106,780 | 174,760 | 158,325–190,197 | 89.5 | 75.5 | 65.5–87.8 | 65.6 | 59.7–71.2 | −13.1 |
| Hemorrhagic stroke | 117,813 | 105,731–133,751 | 200,113 | 182,283–230,479 | 69.9 | 71.5 | 61–82.5 | 60.6 | 55.4–69.6 | −15.3 |
| Hypertensive heart disease | 36,179 | 30,771–46,101 | 62,663 | 55,680–71,029 | 73.2 | 27.0 | 22.7–35.2 | 21.4 | 19–24.1 | −20.7 |
| Cardiomyopathy and myocarditis | 18,025 | 15,031–20,571 | 27,128 | 24,612–29,553 | 50.5 | 8.7 | 7.2–10 | 7.3 | 6.5–7.9 | −16.6 |
| Atrial fibrillation and flutter | 3513 | 2654–4487 | 7535 | 5707–9666 | 114.5 | 3.9 | 2.9–5.1 | 3.5 | 2.6–4.5 | −11.0 |
| Aortic aneurysm | 2694 | 2163–3414 | 6941 | 6291–7580 | 157.6 | 2.0 | 1.6–2.5 | 2.3 | 2.1–2.5 | 14.9 |
| Peripheral artery disease | 114 | 68–151 | 424 | 365–508 | 272.4 | 0.1 | 0.1–0.1 | 0.2 | 0.1–0.2 | 65.9 |
| Endocarditis | 5172 | 4167–7067 | 9016 | 7833–12,719 | 74.3 | 2.9 | 2.3–4.2 | 2.6 | 2.3–3.9 | −8.3 |
| Other cardiovascular and circulatory diseases | 38,243 | 34,519–42,477 | 55,625 | 51,621–60,292 | 45.5 | 20.3 | 18.5–22.2 | 17.1 | 15.9–18.6 | −15.7 |
Fig. 1.
Trend of number of deaths and age-standardized mortality rate from cardiovascular diseases in males and females, Global Burden of Disease study, Eastern Mediterranean Region, 1990–2015
The total number of deaths from ischemic heart disease (IHD) was 802,078 in 2015, which accounted for 58.4% of the total number of deaths due to CVD in the EMR. There were 637,640 additional deaths in 2015 compared to 1990, out of which 62.5% was contributed by IHD.
Table 2 provides the total number of deaths and the age-standardized death rates from CVD in 1990 and 2015 for all EMR countries. In 2015, Afghanistan had the highest age-standardized death rate from CVD, followed by Iraq and Yemen. In most of the EMR countries, age-standardized death rates for CVD decreased between 1990 and 2015, with the highest decreases in Bahrain, Qatar, Lebanon, and Jordan.
Table 2.
Total number of deaths and age-standardized mortality rates for cardiovascular disease causes of death in 1990 and 2015, and percent change, Global Burden of Disease study, Eastern Mediterranean Region, 1990–2015
| Country | Number of deaths | Age-standardized death rate per 100,000 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | % Change | 1990 | 2015 | % Change | |||||
| Number | 95% UI | Number | 95% UI | Rate | 95% UI | Rate | 95% UI | |||
| EMR | 735,689 | 700,875–773,593 | 1,373,329 | 1,290,959–1,465,047 | 86.7 | 515.1 | 491.7–541.5 | 456.5 | 431.5–484.2 | −11.4 |
| Afghanistan | 34,755 | 27,217–42,776 | 10,1572 | 81,113–125,962 | 192.2 | 1048.1 | 860.6–1235.4 | 1042.5 | 865–1227.9 | −0.5 |
| Bahrain | 614 | 547–681 | 792 | 671–933 | 29.0 | 414.1 | 371.4–456.9 | 186.1 | 162.1–210.2 | −55.1 |
| Djibouti | 683 | 434–1025 | 1402 | 762–-2395 | 105.3 | 393.4 | 265.8–568.8 | 360.9 | 212.6–590.1 | −8.3 |
| Egypt | 153,214 | 147,677–157,026 | 226,457 | 219,738–234,235 | 47.8 | 544.9 | 530.1–556.7 | 465.2 | 451.7–479.2 | −14.6 |
| Iran | 96,775 | 86,347–107,587 | 176,299 | 148,576–203,480 | 82.2 | 499.2 | 451.4–547.5 | 402.2 | 344–456.9 | −19.4 |
| Iraq | 44,476 | 38,326–51,342 | 75,604 | 61,673–91,552 | 70.0 | 657.6 | 569.1–755.1 | 604.4 | 503.7–715.3 | −8.1 |
| Jordan | 4869 | 4319–5684 | 6788 | 6108–7611 | 39.4 | 416.0 | 370.2–481.4 | 236.9 | 214.1–264.4 | −43.1 |
| Kuwait | 1262 | 1192–1324 | 2367 | 2040–2747 | 87.6 | 258.5 | 245–271.3 | 209.7 | 185–237 | −18.9 |
| Lebanon | 7397 | 6206–8674 | 11,632 | 8967–14,195 | 57.3 | 464.2 | 391.3–540.9 | 252.1 | 196–305.1 | −45.7 |
| Libya | 4864 | 4354–5397 | 9301 | 8130–10,535 | 91.2 | 310.3 | 276.6–344 | 299.7 | 263.3–339.3 | −3.4 |
| Morocco | 36,293 | 32,487–40,581 | 59,824 | 47,641–75,972 | 64.8 | 362.1 | 327.5–400.4 | 268.3 | 216.5–336.6 | −25.9 |
| Oman | 2108 | 1688–2552 | 4000 | 3336–4583 | 89.7 | 378.8 | 300.7–461.2 | 300.3 | 255.4–336.8 | −20.7 |
| Pakistan | 216,936 | 191,002–247,476 | 465,116 | 407,279–528,666 | 114.4 | 513.1 | 454.9–578 | 530.9 | 469–599.1 | 3.5 |
| Palestine | 2333 | 1902–2925 | 5805 | 4683–6954 | 148.8 | 443.1 | 366.5–542 | 394.9 | 326.3–462.4 | −10.9 |
| Qatar | 338 | 297–383 | 723 | 568–924 | 114.3 | 342.4 | 303.1–380.4 | 180.6 | 149.6–221.8 | −47.3 |
| Saudi Arabia | 13,222 | 11,931–14,651 | 25,845 | 23,532–28,503 | 95.5 | 288.0 | 260.4–317.9 | 231.6 | 213.2–-253.4 | −19.6 |
| Somalia | 11,706 | 3957–22,825 | 15,080 | 5270–31,505 | 28.8 | 508.9 | 192.7–890.2 | 439.7 | 172.6–813.3 | −13.6 |
| Sudan | 42,922 | 35,852–51,825 | 74,648 | 56,697–97,015 | 73.9 | 611.3 | 512.7–738.5 | 501.9 | 388.7–634.1 | −17.9 |
| Syria | 23,049 | 20,307–26,719 | 33,044 | 28,488–36,934 | 43.4 | 554.8 | 494.8–634.9 | 401.0 | 348.7–446.9 | −27.7 |
| Tunisia | 10,747 | 9970–11,633 | 18,423 | 14,973–21,952 | 71.4 | 285.3 | 263.3–308.9 | 204.0 | 166.5–242.6 | −28.5 |
| UAE | 1641 | 1260–2230 | 8563 | 6337–11,314 | 421.9 | 406.5 | 327.3–501.8 | 333.4 | 279.6–403.7 | −18.0 |
| Yemen | 25,485 | 16,534–36,647 | 50,043 | 30,637–78,838 | 96.4 | 700.0 | 461.6–991.9 | 592.1 | 383–888.5 | −15.4 |
Electronic supplementary figure S1 shows the top-ranked death rates for different CVD in EMR countries. Ischemic heart disease was the leading cause of CVD mortality in 20 countries of the EMR; the exceptions were Djibouti and Somalia, where cerebrovascular disease (both hemorrhagic and ischemic stroke) was the leading cause of cardiovascular-related death.
YLLs
The age-standardized YLL rate decreased 15.3%, from 9618.7 (9148.6–10,141.7) per 100,000 in 1990–8145.0 (7628.6–8744.3) per 100,000 in 2015 (Electronic supplementary table S2). In the region, Afghanistan had the highest age-standardized YLL rate at 21,426.2 (17,105.2–26,544.7), followed by Yemen and Iraq (Electronic supplementary table S2). In all countries of the EMR except Pakistan, age-standardized YLL rates decreased from 1990 to 2015 (Electronic supplementary table S2).
YLDs
The years lived with disability caused by CVD in the EMR increased from 1,058,839 (95% UI: 746,613–1409,913) in 1990 to 1,966,111 (95% UI: 1398,373–2597,819) in 2015. The rate of YLD increased by 85.7% during 1990–2015 in the EMR.
The age-standardized YLD rate in the EMR was 460.6 (329.2–603.6) per 100,000 in 2015, which showed very little decrease compared to 1990 (461.1 per 100,000) (Electronic supplementary table S2). Oman had the highest age-standardized YLD rate in the region in both 1990 and 2015: it was 1261 (874.6–1722.1) per 100,000 in 2015, which was about 2.7 times higher than the regional average. United Arab Emirates had the lowest age-standardized YLD rate in the EMR, 296.8 per 100,000 in 1990 and 285.8 per 100,000 in 2015. Age-standardized YLD rates of CVD decreased between 1990 and 2015 in six countries of the region: Iran, United Arab Emirates, Jordan, Djibouti, Somalia, and Afghanistan. The biggest decline was seen in Iran (4.6%), and the smallest reduction was in Afghanistan (0.5%). Among the remaining 16 countries of the region that showed increases in age-standardized YLD rates of CVD, Syria’s was the greatest, at 9.1%.
DALYs
The rate of DALYs from CVD per 100,000 population decreased from 5447.8 (95% UI: 5168.2–5739.0) in 1990–5109.8 (95% UI: 4771.3–5511.1) in 2015, a 6.2% decrease—compared to an 8.4% reduction in the DALY rate for all other non-communicable diseases in the EMR. The age-standardized DALY rate also decreased 14.6% during 1990–2015 (Table 3). Table 3 reports numbers and age-standardized rates of DALYs for different CVD in the EMR in 1990 and 2015. The age-standardized DALY rate of CVD for men and women in the EMR in 2015 was higher than in other WHO regions. It was 1.51 times the global rate for males and 1.86 times the global rate for females. Electronic supplementary figure S2 shows the age-standardized rates of DALYs for different CVD in men and women. As shown, ischemic heart disease caused the highest number of DALYs both in men (5771.9 per 100,000) and women (3931.2 per 100,000), followed by hemorrhagic stroke and ischemic stroke.
Table 3.
Total disability-adjusted life years (DALY) and age-standardized disability-adjusted life years rates for component cardiovascular causes of death in 1990 and 2015, and percent change, Global Burden of Disease study, Eastern Mediterranean Region, 1990–2015
| Cause | Number of DALYs | Age-standardized DALY rate per 100,000 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | % Change | 1990 | 2015 | % Change | |||||
| Number | 95% UI | Number | 95% UI | Rate | 95% UI | Rate | 95% UI | |||
| Cardiovascular diseases | 20,164,206 | 19,129,504–21,242,151 | 33,131,948 | 30,937,166–35,734,353 | 64.3 | 10,079.8 | 9594.7–10,603.6 | 8605.6 | 8074.6–9219.3 | −14.6 |
| Rheumatic heart disease | 876,838 | 770,813–986,361 | 1153,351 | 993,217–1333,219 | 31.5 | 302.1 | 265.1–344.5 | 215.8 | 185.2–248.4 | −28.5 |
| Ischemic heart disease | 9323,188 | 8770,306–9877,741 | 17,827,201 | 16,511,324–19,368,534 | 91.2 | 5370.1 | 5052.6–5672.7 | 4865.0 | 4533.1–5231.4 | −9.4 |
| Ischemic stroke | 1879,679 | 1649,862–2128,711 | 3272,789 | 2963,211–3568,718 | 74.1 | 1183.5 | 1031.4–1361 | 997.6 | 903.8–1085.4 | −15.7 |
| Hemorrhagic stroke | 3941,327 | 3658,523–4323,670 | 5565,221 | 5091,084–6337,446 | 41.2 | 1649.0 | 1485.2–1870.5 | 1303.2 | 1193.9–1493 | −21.0 |
| Hypertensive heart disease | 822,728 | 711,712–1011,157 | 1366,662 | 1201,763–1571,258 | 66.1 | 479.4 | 411.3–603 | 371.0 | 328.2–422.5 | −22.6 |
| Cardiomyopathy and myocarditis | 833,292 | 693,153–982,453 | 1001,334 | 891,780–1097,777 | 20.2 | 247.2 | 206.1–281.7 | 188.0 | 170.3–204.4 | −24.0 |
| Atrial fibrillation and flutter | 77,777 | 61,867–94,926 | 161,328 | 129,867–199,493 | 107.4 | 63.3 | 51.4–77 | 58.2 | 47–71 | −8.0 |
| Aortic aneurysm | 63,221 | 50,928–80,451 | 163,304 | 146,635–180,105 | 158.3 | 35.4 | 28.5–45 | 41.6 | 37.6–45.6 | 17.6 |
| Peripheral artery disease | 13,954 | 7359–24,367 | 32,852 | 18,777–56,064 | 135.4 | 10.1 | 5.3–17.9 | 11.2 | 6.4–19.3 | 11.3 |
| Endocarditis | 217,347 | 160,723–291,718 | 292,842 | 248,013–378,079 | 34.7 | 68.4 | 55–92.5 | 58.5 | 50.9–80.3 | −14.4 |
| Other CVD | 2114,855 | 1844,679–2463,667 | 2295,064 | 2018,478–2613,017 | 8.5 | 671.3 | 599.3–755.3 | 495.4 | 440.4–555.8 | −26.2 |
Electronic supplementary figure S3 shows DALY rates for each CVD in different age groups. As shown, the highest DALY rates for IHD, hemorrhagic stroke, ischemic stroke, and hypertensive heart disease were observed in people aged 50–69 years. IHD, hemorrhagic stroke, and rheumatic heart disease showed the highest number of DALYs in the 15–49 years age group.
Table 4 summarizes age-standardized DALY rates for CVD in the EMR countries in 1990 and 2015. As shown, DALY rates decreased in all EMR countries except Pakistan from 1990 to 2015; the greatest reductions in DALY rates were seen in Bahrain (59.4%), Qatar (48.7%), and Jordan (47%). Afghanistan had the highest age-standardized CVD DALY rate in both 1990 and 2015. Kuwait had the lowest age-standardized DALY rate of CVD in 1990, and Qatar had the lowest in 2015.
Table 4.
Total number of disability-adjusted life years and age-standardized disability-adjusted life years rates for cardiovascular diseases in 1990 and 2015, and percent change, 1990–2015, in Eastern Mediterranean Region countries
| Country | Number of DALYs | Age-standardized DALY rate per 100,000 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | % Change | 1990 | 2015 | % Change | |||||
| Number | 95% UI | Number | 95% UI | Rate | 95% UI | Rate | 95% UI | |||
| EMR | 20,164,206 | 19,129,504–21,242,151 | 33,131,948 | 30,937,166–35,734,353 | 64.3 | 10,079.8 | 9594.7–10,603.6 | 8605.6 | 8074.6–9219.3 | −14.6 |
| Afghanistan | 1,019,023 | 7,93,590–1,278,676 | 2,865,062 | 2,239,466–3,635,800 | 181.2 | 22,258.2 | 17,615.6–27,186.7 | 21,864.3 | 17,591.4–27,024.5 | −1.8 |
| Bahrain | 18,578 | 16,524–20,639 | 23,376 | 19,748–27,808 | 25.8 | 8086.5 | 7206.4–8964 | 3281.4 | 2832.6–3769.2 | −59.4 |
| Djibouti | 19,979 | 13,027–-29,586 | 35,930 | 19,430–64,153 | 79.8 | 7891.5 | 5171.4–11,605.5 | 7112.8 | 4021.2–12,056.6 | −9.9 |
| Egypt | 4,373,017 | 4,109,349–4,595,897 | 5,436,416 | 5,216,937–5,700,475 | 24.3 | 11,230.6 | 10,762.9–11,583.1 | 8826.2 | 8508.6–9171.3 | −21.4 |
| Iran | 2,941,466 | 2,601,284–3,291,417 | 3,875,985 | 3,249,465-4,577,119 | 31.8 | 9849.9 | 8776.8–10,950.2 | 7179.6 | 6090.9–8340.9 | −27.1 |
| Iraq | 1,070,614 | 917,957–1248,583 | 1,875,448 | 1,489,313–2,315,419 | 75.2 | 12,513.4 | 10,678.3–14,669.9 | 11,244.0 | 9089.6–13,679.3 | −10.1 |
| Jordan | 109,195 | 95,903–127,032 | 154,251 | 137,970–172,312 | 41.3 | 7692.8 | 6771.4–8983.8 | 4077.5 | 3666.1–4533 | −47.0 |
| Kuwait | 40,918 | 38,315–43,123 | 75,385 | 65,509–87,507 | 84.2 | 4818.8 | 4558.7–5066.9 | 3884.1 | 3424.2–4417.1 | −19.4 |
| Lebanon | 167,913 | 140,761–199,069 | 211,244 | 159,897–264,585 | 25.8 | 8792.7 | 7390.6–10,364.6 | 4213.8 | 3210.3–5249.2 | −52.1 |
| Libya | 176,223 | 154,977–198,183 | 234,502 | 205,521–265,135 | 33.1 | 6384.4 | 5714.7–7050.6 | 5638.4 | 4957.2–6367.8 | −11.7 |
| Morocco | 1,103,861 | 980,405–1,235,540 | 1,332,750 | 1,078,637–1,670,227 | 20.7 | 7222.4 | 6511.3–8059.2 | 4977.5 | 4039.5–6209.9 | −31.1 |
| Oman | 93,965 | 76,349–115,695 | 135,300 | 114,087–155,337 | 44.0 | 8404.3 | 6832–10,016.2 | 5962.4 | 5071–6713.2 | −29.1 |
| Pakistan | 5,069,303 | 4,422,395–5,880,731 | 10,719,663 | 9,250,078–12,360,492 | 111.5 | 9446.3 | 8281–10,798.4 | 9928.0 | 8664.3–11,288.5 | 5.1 |
| Palestine | 68,438 | 55,953–85,314 | 150,510 | 120,084–183,652 | 119.9 | 8263.4 | 6749.8–10,377.3 | 7280.6 | 5868.1–8727.7 | −11.9 |
| Qatar | 10,556 | 9283–12,017 | 24,791 | 19,932–30,601 | 134.8 | 5873.6 | 5192.9–6542.3 | 3013.6 | 2466.4–3730 | −48.7 |
| Saudi Arabia | 359,601 | 320,837–401,588 | 663,879 | 600,438–732,764 | 84.6 | 5285.0 | 4727.5–5861.6 | 4003.3 | 3650.2–4393.1 | −24.3 |
| Somalia | 329,146 | 120,719–676,354 | 410,106 | 151,542–920,717 | 24.6 | 10,762.8 | 3851–21,078.4 | 9062.4 | 3379.7–18,999.5 | −15.8 |
| Sudan | 1,359,599 | 1,129,865–1,596,275 | 2,047,475 | 1,542,545–2,657,659 | 50.6 | 12,814.4 | 10,687.4–15,522.9 | 9823.7 | 7427.1–12,742.4 | −23.3 |
| Syria | 668,927 | 579,151–779,665 | 766,383 | 663,438–864,601 | 14.6 | 11,211.5 | 9876.4–13,008.3 | 7277.4 | 6299.5–8180.1 | −35.1 |
| Tunisia | 282,490 | 259,822–306,247 | 371,042 | 306,673–438,530 | 31.3 | 5367.9 | 4992.8–5778.7 | 3694.6 | 3055.8–4362 | −31.2 |
| UAE | 56,629 | 42,431–80,907 | 304,764 | 220,613–401,976 | 438.2 | 7978.3 | 6300–10,281.2 | 6184.6 | 4945.5–7774.5 | −22.5 |
| Yemen | 824,766 | 550,243–1,143,803 | 1,417,685 | 876,250–2,252,582 | 71.9 | 14,715.3 | 9437–21,422.1 | 11,692.8 | 7228.8–18,372.2 | −20.5 |
Analyzing the components of DALYs, CVD had a higher YLL rate compared to YLD rate: on average, YLLs were 17.7 times higher than YLDs in the EMR. The YLL/YLD ratio in the countries of the region showed a wide range of variation, from 48.9 in Afghanistan to 3.7 in Oman (Electronic supplementary table S2).
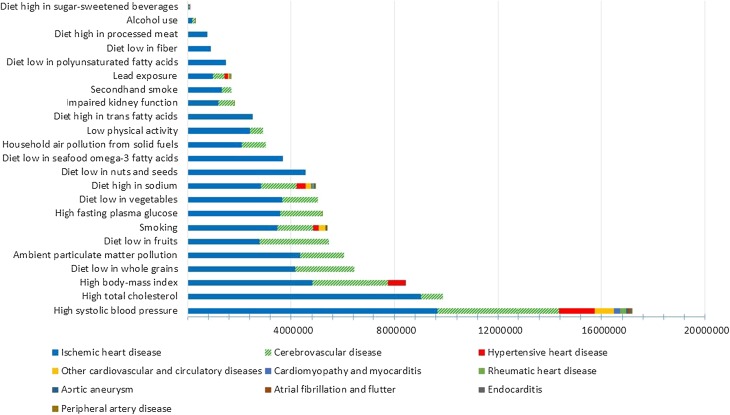
Risk factors
Figure 2 shows the contribution, in DALYs, of different risk factors to different CVD. High blood pressure, high total cholesterol, and high body mass index were the leading risk factors for CVD, accounting for 17,159,331 DALYs, 9852,820 DALYs, and 8427,021 DALYs, respectively.
Fig. 2.
Number of disability-adjusted life years for different cardiovascular diseases attributed to different risk factors, Global Burden of Disease study, Eastern Mediterranean Region, 2015
The cluster of all dietary risk factors accounts for 19,803,725 DALYs, making it the leading risk factor for CVD, higher than even high blood pressure. Low whole grains, low fruit, low vegetables, and high sodium intake were the most important dietary risk factors.
Discussion
This study shows that CVD are the leading cause of disease burden in the EMR as a whole and in most of the countries of the region. Close to 33 million years of life were lost due to premature mortality or disability from CVD, and more than 1.3 million people died in the EMR in 2015, accounting for around one-third of all deaths in the region. Previous studies have also reported CVD deaths as the main cause of death, for instance, 45% in the West Bank (Palestine), 45% in Aleppo (Syria), 35% in Jordan, and 25% in UAE (Barakat et al. 2012; Loney et al. 2013; Shara 2010). A study in Europe has reported CVD mortality as making up half of all deaths (Nichols et al. 2014).
CVD age-standardized mortality was considerably higher than the global average (456 compared to 286 per 100,000); however it shows a declining trend over the past 25 years in most of the EMR countries. Countries with higher declines (Bahrain, Qatar, Lebanon, and Jordan) were among the countries in the fourth Socio-demographic Index quartile category. In another GBD study, we estimated an index for healthcare access and quality which is a composite index based on estimates of mortality amenable to personal health care and varies between 0 (worst) and 100 (best). The index showed substantial heterogeneity with a range between 32 (Afghanistan) and 85 (Qatar) in 2015 in the EMR. Linking these results to the findings of our study showed that the countries with lower age-standardized DALY rates due to CVD had a higher index for healthcare access and quality, and vice versa. This restates the importance of increasing access to and quality of health care to reduce CVD burden (Barber et al. 2017).
In the EMR, YLLs are the main component of CVD burden. A global-level assessment showed that for overall CVD, YLL rates were lowest in both the lowest and highest socio-demographic groups, with an increase for those in the middle of the socio-demographic rankings. It has been suggested that medical care in countries with the highest Socio-demographic Index might have increased life expectancy to the point where CVD is most prevalent, while people in the lowest socio-demographic group are dying from other competing conditions before reaching the common age for developing ischemic heart disease and stroke. Based on this hypothesis, people living in countries in the middle range of the socio-demographic rankings are surviving long enough to develop ischemic heart disease but do not have access to optimal medical or surgical treatment (GBD 2015 Mortality and Causes of Death Collaborators 2016).
These findings call for a comprehensive approach to prevent and control the burden of CVD in the region. This approach should include a road map for better monitoring of the burden in EMR countries, with a focus on potential variations in risk and care by regions within the countries. It should also include programs for increasing awareness among the general population of the importance of controlling CVD risk factors.
The United Nations has set targets to decrease mortality from non-communicable diseases (Sustainable Development Goals, target 3.4.1), and CVD is at the center of this target (GBD 2015 SDGs Collaborators 2016). The World Health Organization has suggested a package of essential non-communicable disease interventions for primary health care in low-resource settings (PEN). These interventions include a mixture of cost-effective population-wide and individual approaches to reduce the burden of major non-communicable diseases, such as methods for early detection and diagnosis using inexpensive technologies, non-pharmacological and pharmacological approaches for modification of risk factors, and affordable medications for prevention and treatment of heart attacks and strokes, diabetes, cancer, and asthma (World-Health-Organization 2010).
Our study showed that increased blood pressure is the most important risk factor for CVD in the EMR, followed by high total cholesterol and high body mass index. A Cochrane systematic review showed that multiple risk factor interventions may lower systolic and diastolic blood pressure, body mass index, and waist circumference in low- and middle-income countries (Uthman et al. 2015).
Previous studies show a high percentage of undiagnosed CVD risk factors, such as diabetes and hypertension, in the region (Abd El-Aty et al. 2015; El Bcheraoui et al. 2014a, b; Najafipour et al. 2014). The evidence shows that delayed detection and undiagnosed risk factors, especially diabetes, are strong predictors of fatal CVDs (Nakagami et al. 2006). Based on reports from the region, required care and services (such as medications) are underutilized in diagnosed cases, even in high-income countries like Saudi Arabia (Moradi-Lakeh et al. 2016). Underutilization of medications is a function of availability, accessibility, affordability, acceptability, and quality of medicines (and care), as well as adherence to medical recommendations (Behnood-Rod et al. 2016; Najafipour et al. 2014; van Mourik et al. 2010; Wirtz et al. 2016). The Prospective Urban Rural Epidemiology (PURE) study showed great variation in availability, affordability, and use of medications for CVD, between and within countries. Countries with less control over production, importation, distribution chains, and retail outlets are specifically at risk of substandard quality and falsification of medicines (Khatib et al. 2016). All these factors are important to achieve desired health outcomes in the field of CVD. CVD prevention and control programs should improve the perceived need and demand of the population for early detection and use of the prevention/control services. The study on CVD mortality forecast in 2015 has shown that the MENA region will not achieve the target of 25% reduction of CVD mortality by 2025 without achieving all major targets for risk factor reduction (i.e., reducing the prevalence of elevated systolic blood pressure by 25%, reducing the prevalence of smoking by 30%, halting the rise in elevated body mass index, and halting the rise in fasting plasma glucose). Moreover, reports of health system challenges in controlling and managing CVD in some of the EMR countries reemphasize the need for significant investment and improvement of access (Roth et al. 2015a, b; Romdhane et al. 2015; Ahmad et al. 2015).
Our study has some limitations; accurate data on cardiovascular events (especially non-fatal outcomes) are limited in many countries, including the EMR countries. We used the standard GBD methodology by using study- and country-level covariates for adjustment and estimation of epidemiologic measures. Our study does not account for variation within countries.
Conclusion
Most of the EMR countries have launched programs to reduce the burden of non-communicable disease, but they generally do not have widespread programs to combat CVD. This study calls for strengthening efforts to design and launch comprehensive programs to cover all aspects of prevention and control of CVDs through evidence-informed, efficient interventions. The countries should establish or improve information systems such as surveillance sy stems to provide valid and accurate information for policymaking and monitoring of the situation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators:
Ali H. Mokdad, PhD (corresponding author), Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Arash Tehrani-Banihashemi, PhD, Preventive Medicine and Public Health Research Center, Iran University of Medical Sciences, Tehran, Iran. Maziar Moradi-Lakeh, MD, Department of Community Medicine, Preventive Medicine Public Health Research Center, Gastrointestinal and Liver Disease Research Center (GILDRC), Iran University of Medical Sciences, Tehran, Iran. Charbel El Bcheraoui, PhD, Institute for Health Metrics and Evaluation, University of Washington. Raghid Charara, MD, American University of Beirut, Beirut, Lebanon. Ibrahim Khalil, MD, Institute for Health Metrics and Evaluation, University of Washington. Ashkan Afshin, MD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Michael Collison, BS, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Farah Daoud, BA/BS, Institute for Health Metrics and Evaluation, University of Washington. Kristopher J. Krohn, BA, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Adrienne Chew, ND, Institute for Health Metrics and Evaluation, University of Washington. Leslie Cornaby, BS, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Kyle J. Foreman, PhD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Imperial College London, London, UK. Joseph Frostad, Institute for Health Metrics and Evaluation, University of Washington. Nicholas J. Kassebaum, MD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States; Department of Anesthesiology and Pain Medicine, Seattle Children’s Hospital, Seattle, Washington, United States. Laura Kemmer, PhD, Institute for Health Metrics and Evaluation, University of Washington. Michael Kutz, BS, Institute for Health Metrics and Evaluation, University of Washington. Patrick Liu, BA, Institute for Health Metrics and Evaluation, University of Washington. Mojde Mirarefin, MPH, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States; Hunger Action Los Angeles, Los Angeles, CA, United States. Grant Nguyen, MPH, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Haidong Wang, PhD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Ben Zipkin, BS, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Amanuel Alemu Abajobir, MPH, School of Public Health, University of Queensland, Brisbane, QLD, Australia. Marian Abouzeid, DPH, Telethon Kids Institute, Perth, Australia. Niveen M.E. Abu-Rmeileh, PhD, Institute of Community and Public Health, Birzeit University, Ramallah, Palestine. Aliasghar Ahmad Kiadaliri, PhD, Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit, Lund University, Lund, Sweden. Muktar Beshir Ahmed, MPH, College of Health Sciences, Department of Epidemiology, ICT and e-Learning Coordinator, Jimma University, Jimma, Ethiopia. Baran Aksut, MD, Cleveland Clinic, Cleveland, United States. Khurshid Alam, PhD, Murdoch Childrens Research Institute, The University of Melbourne, Parkville, Victoria, Australia. The University of Melbourne, Melbourne, VIC, Australia, The University of Sydney, Sydney, NSW, Australia. Deena Alasfoor, MSc, Ministry of Health, Al Khuwair, Muscat, Oman. Raghib Ali, MSc, University of Oxford, Oxford, UK. Reza Alizadeh-Navaei, PhD, Gastrointestinal Cancer Research Center, Mazandaran University of Medical Sciences, Sari, Iran. Rajaa Al-Raddadi, PhD, Joint Program of Family and Community Medicine, Jeddah, Saudi Arabia. Ubai Alsharif, MPH, Charité Universitätsmedizin, Berlin, Germany. Khalid A. Altirkawi, MD, King Saud University, Riyadh, Saudi Arabia. Nelson Alvis-Guzman, PhD, Universidad de Cartagena, Colombia. Nahla Anber, PhD, Mansoura University, Mansoura, Egypt. Palwasha Anwari, MD, Self-employed, Kabul, Afghanistan. Johan Ärnlöv, PhD, Department of Neurobiology, Care Sciences and Society, Division of Family Medicine and Primary Care, Karolinska Institutet, Stockholm, Sweden, School of Health and Social Studies, Dalarna University, Falun, Sweden. Solomon Weldegebreal Asgedom, PhD, Mekelle University, Mekelle, Ethiopia. Tesfay Mehari Atey, MS, Mekelle University, Mekelle, Ethiopia. Ashish Awasthi, PhD, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India. Till Bärnighausen, MD, Department of Global Health and Population, Harvard T. H. Chan School of Public Health, Harvard University, Boston, MA, United States; Africa Health Research Institute, Mtubatuba, South Africa; Institute of Public Health, Heidelberg University, Heidelberg, Germany. Umar Bacha, PhD, School of Health Sciences, University of Management and Technology, Lahore, Pakistan. Aleksandra Barac, PhD, Faculty of Medicine, University of Belgrade, Belgrade, Serbia. Suzanne L. Barker-Collo, PhD, School of Psychology, University of Auckland, Auckland, New Zealand. Neeraj Bedi, MD, College of Public Health and Tropical Medicine, Jazan, Saudi Arabia. Derrick A. Bennett, PhD, Nuffield Department of Population Health, University of Oxford, Oxford, UK. Derbew Fikadu Berhe, MS, School of Pharmacy, Mekelle University, Mekelle, Ethiopia. Sibhatu Biadgilign, MPH, Independent Public Health Consultants, Addis Ababa, Ethiopia. Zahid A. Butt, PhD, Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan. Jonathan R. Carapetis, PhD, Telethon Kids Institute, Princess Margaret Hospital for Children, The University of Western Australia, Subiaco, Western Australia, Australia. Ruben Estanislao Castro, PhD, Universidad Diego Portales, Santiago, Region Metropolitana, Chile. Abdulaal A. Chitheer, MD, Ministry of Health, Baghdad, Iraq. Kairat Davletov, PhD, Republican Institute of Cardiology and Internal Diseases, Almaty, Kazakhstan, School of Public Health, Kazakh National Medical University, Almaty, Kazakhstan. Samath D. Dharmaratne, MD, Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka. Shirin Djalalinia, PhD, Undersecretary for Research and Technology, Ministry of Health and Medical Education, Tehran, Iran. Huyen Phuc Do, MSc, Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam. Manisha Dubey, MPhil, International Institute for Population Sciences, Mumbai, India. Hedyeh Ebrahimi, MD, Non-communicable Diseases Research Center, Tehran University of Medical Sciences, Tehran, Iran; Liver and Pancreaticobiliary Diseases Research Center, Digestive Disease Research Institute, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Tehran, Iran. Babak Eshrati, PhD, Ministry of Health and Medical Education, Tehran, Iran, Arak University of Medical Sciences, Arak, Iran. Alireza Esteghamati, MD, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran. Maryam S. Farvid, PhD, Department of Nutrition, Harvard T. H. Chan School of Public Health, Harvard University, Boston, MA, United States, Harvard/MGH Center on Genomics, Vulnerable Populations, and Health Disparities, Mongan Institute for Health Policy, Massachusetts General Hospital, Boston, MA, United States. Seyed-Mohammad Fereshtehnejad, PhD, Department of Neurobiology, Care Sciences and Society (NVS), Karolinska Institutet, Stockholm, Sweden. Florian Fischer, PhD, School of Public Health, Bielefeld University, Bielefeld, Germany. Solomon Weldemariam Gebrehiwot, MS, College of Health Sciences, Mekelle University, Mekelle, Ethiopia. Tsegaye Tewelde Gebrehiwot, MPH, Jimma University, Jimma, Ethiopia. Richard F. Gillum, MD, Howard University, Washington, DC, United States. Philimon N. Gona, PhD, University of Massachusetts Boston, Boston, Massachusetts, United States. Rajeev Gupta, PhD, Eternal Heart Care Centre and Research Institute, Jaipur, India. Nima Hafezi-Nejad, MD, Endocrinology and Metabolism Research Center, Tehran University of Medical Sciences, Tehran, Iran. Randah Ribhi Hamadeh, DPhil, Arabian Gulf University, Manama, Bahrain. Samer Hamidi, DrPH, Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates. Mohamed Hsairi, MD, Department of Epidemiology, Salah Azaiz Institute, Tunis, Tunisia. Sun Ha Jee, PhD, Graduate School of Public Health, Yonsei University, Seoul, South Korea. Jost B. Jonas, MD, Department of Ophthalmology, Medical Faculty Mannheim, Ruprecht-Karls-University Heidelberg, Mannheim, Germany. Chante Karimkhani, MD, Case Western University Hospitals, Cleveland, Ohio, United States. Amir Kasaeian, PhD, Hematology-Oncology and Stem Cell Transplantation Research Center, Tehran University of Medical Sciences, Tehran, Iran; Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran. Yousef Saleh Khader, ScD, Department of Community Medicine, Public Health and Family Medicine, Jordan University of Science and Technology, Irbid, Jordan. Ejaz Ahmad Khan, MD, Health Services Academy, Islamabad, Pakistan. Daniel Kim, DrPH, Department of Health Sciences, Northeastern University, Boston, Massachusetts, United States. Dharmesh Kumar Lal, MD, Public Health Foundation of India, Gurgaon, India. Heidi J. Larson, PhD, Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, UK; Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Asma Abdul Latif, PhD, Department of Zoology, Lahore College for Women University, Lahore, Pakistan. Shai Linn, MD, University of Haifa, Haifa, Israel. Paulo A. Lotufo, DrPH, University of São Paulo, São Paulo, Brazil. Raimundas Lunevicius, PhD, Aintree University Hospital National Health Service Foundation Trust, Liverpool, UK; School of Medicine, University of Liverpool, Liverpool, UK. Hassan Magdy Abd El Razek, MBBCH, Mansoura Faculty of Medicine, Mansoura, Egypt. Azeem Majeed, MD, Department of Primary Care and Public Health, Imperial College London, London, UK. Reza Malekzadeh, MD, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran. Deborah Carvalho Malta, PhD, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil. Toni Meier, PhD, Martin Luther University Halle-Wittenberg, Halle (Saale), Germany. Peter Memiah, PhD, University of West Florida, Pensacola, FL, United States. Ziad A. Memish, MD, Saudi Ministry of Health, Riyadh, Saudi Arabia; College of Medicine, Alfaisal University, Riyadh, Saudi Arabia. Walter Mendoza, MD, United Nations Population Fund, Lima, Peru. George A. Mensah, MD, Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, United States. Atte Meretoja, PhD, Department of Medicine, The University of Melbourne, Melbourne, Victoria, Australia, Department of Neurology, Helsinki University Hospital, Helsinki, Finland. Ted R. Miller, PhD, Pacific Institute for Research and Evaluation, Calverton, MD, United States; Centre for Population Health, Curtin University, Perth, WA, Australia. Erkin M. Mirrakhimov, PhD, Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan; National Center of Cardiology and Internal Disease, Bishkek, Kyrgyzstan. Shafiu Mohammed, PhD, Health Systems and Policy Research Unit, Ahmadu Bello University, Zaria, Nigeria; Institute of Public Health, Heidelberg University, Heidelberg, Germany. Quyen Le Nguyen, MD, Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam. Vuong Minh Nong, MSc, Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam. Jonathan Pearson-Stuttard, MD, Imperial College London, London, UK. Farhad Pishgar, MD, Non-communicable Diseases Research Center, Tehran University of Medical Sciences, Tehran, Iran; Uro-Oncology Research Center, Tehran University of Medical Sciences, Tehran, Iran. Farshad Pourmalek, PhD, University of British Columbia, Vancouver, British Columbia, Canada. Mostafa Qorbani, PhD, Non-communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran. Amir Radfar, MD, A T Still University, Kirksville, MO, United States. Anwar Rafay, MS, Contech International Health Consultants, Lahore, Pakistan; Contech School of Public Health, Lahore, Pakistan. Vafa Rahimi-Movaghar, MD, Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, Tehran, Iran. Rajesh Kumar Rai, MPH, Society for Health and Demographic Surveillance, Suri, India. Saleem M. Rana, PhD, Contech School of Public Health, Lahore, Pakistan, Contech International Health Consultants, Lahore, Pakistan. David Laith Rawaf, MD, WHO Collaborating Centre, Imperial College London, London, UK, North Hampshire Hospitals, Basingstroke, UK; University College London Hospitals, London, UK. Salman Rawaf, MD, Imperial College London, London, UK. Andre M. N. Renzaho, PhD, Western Sydney University, Penrith, NSW, Australia. Satar Rezaei, PhD, School of Public Health, Kermanshah University of Medical Sciences, Kermanshah, Iran. Kedir Teji Roba, PhD, Haramaya University, Harar, Ethiopia. Gholamreza Roshandel, PhD, Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran; Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran. Mahdi Safdarian, MD, Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, Tehran, Iran. Sare Safi, MS, Ophthalmic Epidemiology Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Saeid, Safiri, PhD, Managerial Epidemiology Research Center, Department of Public Health, School of Nursing and Midwifery, Maragheh University of Medical Sciences, Maragheh, Iran. Mohammad Ali Sahraian, MD, MS Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran. Payman Salamati, MD, Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, Tehran, Iran. Abdallah M. Samy, PhD, Ain Shams University, Cairo, Egypt. Milena M. Santric Milicevic, PhD, Institute of Social Medicine, Faculty of Medicine, University of Belgrade, Belgrade, Serbia, Centre School of Public Health and Health Management, Faculty of Medicine, University of Belgrade, Belgrade, Serbia. Benn Sartorius, PhD, Public Health Medicine, School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa; UKZN Gastrointestinal Cancer Research Centre, South African Medical Research Council (SAMRC), Durban, South Africa. Sadaf G, Sepanlou, PhD, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran. Masood Ali Shaikh, PhD, Independent Consultant, Karachi, Pakistan. Diego Augusto Santos Silva, Federal University of Santa Catarina, Florianopolis, Brazil. Jasvinder A. Singh, MD, University of Alabama at Birmingham and Birmingham Veterans Affairs Medical Center, Birmingham, Alabama, United States. Badr H. A Sobaih, MD, King Saud University, Riyadh, Saudi Arabia. Konstantinos Stroumpoulis, PhD, Alexandra General Hospital of Athens, Athens, Greece; Centre Hospitalier Public du Cotentin, Cherbourg, France. Rizwan Suliankatchi Abdulkader, MD, Ministry of Health, Kingdom of Saudi Arabia, Riyadh, Saudi Arabia. Cassandra E. I. Szoeke, PhD, Institute of Health and Ageing, The University of Melbourne, Melbourne, Victoria, Australia. Mohamad-Hani Temsah, MD, King Saud University, Riyadh, Saudi Arabia. Bach Xuan Tran, PhD, Johns Hopkins University, Baltimore, Maryland, United States; Hanoi Medical University, Hanoi, Vietnam. Kingsley Nnanna Ukwaja, MD, Department of Internal Medicine, Federal Teaching Hospital, Abakaliki, Ebonyi State, Nigeria. Olalekan A. Uthman, PhD, Warwick Medical School, University of Warwick, Coventry, UK. Tommi Vasankari, PhD, UKK Institute for Health Promotion Research, Tampere, Finland. Vasiliy Victorovich Vlassov, MD, National Research University Higher School of Economics, Moscow, Russia. Stein Emil Vollset, DrPH, Center for Disease Burden, Norwegian Institute of Public Health, Bergen, Norway; Department of Global Public Health and Primary Care, University of Bergen, Bergen, Norway; Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, United States. Tolassa Wakayo, MS, Jimma University, Jimma, Ethiopia. Robert G. Weintraub, MBBS, Royal Children's Hospital, Melbourne, VIC, Australia, The University of Melbourne, Melbourne, VIC, Australia, Murdoch Children's Research Institute, Melbourne, VIC, Australia. Priscilla R. Wessly, MD, Internal Medicine Department, Howard University Hospital, Washington, DC, United States. Tissa Wijeratne, MD, Western Health, Footscray, Victoria, Australia, University of Melbourne, Footscray, Victoria, Australia. Charles D.A. Wolfe, MD, Division of Health and Social Care Research, King's College London, London, UK; National Institute for Health Research Comprehensive Biomedical Research Centre, Guy’s and St. Thomas’ NHS Foundation Trust and King’s College London, London, UK. Abdulhalik Workicho, MPH, Jimma University, Jimma, Ethiopia, Ghent University, Ghent, Belgium. Mohsen Yaghoubi, MSc, School of Public Health, University of Saskatchewan, Saskatoon, Saskatchewan, Canada. Yuichiro Yano, MD, Department of Preventive Medicine, Northwestern University, Chicago, Illinois, United States. Mehdi Yaseri, PhD, Tehran University of Medical Sciences, Terhan, Iran; Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Naohiro Yonemoto, MPH, Department of Biostatistics, School of Public Health, Kyoto University, Kyoto, Japan. Mustafa Z. Younis, Jackson State University, Jackson, MS, United States. Chuanhua Yu, PhD, Department of Epidemiology and Biostatistics, School of Public Health, Wuhan University, Wuhan, China; Global Health Institute, Wuhan University, Wuhan, China. Maysaa El Sayed Zaki, PhD, Faculty of Medicine, Mansoura University, Mansoura, Egypt. Aisha O. Jumaan, PhD, Independent Consultant, Seattle, Washington, United States. Theo Vos, PhD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Gregory A. Roth, MD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Simon I. Hay, DSc, Oxford Big Data Institute, Li Ka Shing Centre for Health Information and Discovery, University of Oxford, Oxford, UK; Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Mohsen Naghavi, PhD, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States. Christopher J. L Murray, DPhil, Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, United States.
Compliance with ethical standards
Ethical standards
This manuscript reflects original work that has not previously been published in whole or in part and is not under consideration elsewhere. All authors have read the manuscript and have agreed that the work is ready for submission and accept responsibility for its contents. The authors of this paper have complied with all ethical standards and do not have any conflicts of interest to disclose at the time of submission. The funding source played no role in the design of the study, the analysis and interpretation of data, and the writing of the paper. The study did not involve human participants and/or animals; therefore, no informed consent was needed.
Funding
This research was funded by the Bill & Melinda Gates Foundation.
Conflict of interest
The authors declare that they have no conflicts of interest at this time.
Footnotes
This article is part of the supplement “The state of health in the Eastern Mediterranean Region, 1990–2015”.
The members of GBD (Global Burden of Disease) 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators are listed at the end of the article. Ali H. Mokdad, on behalf of GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators, is the corresponding author.
Contributor Information
GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators, Email: mokdaa@uw.edu
GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators:
Arash Tehrani-Banihashemi, Maziar Moradi-Lakeh, Charbel El Bcheraoui, Raghid Charara, Ibrahim Khalil, Ashkan Afshin, Michael Collison, Farah Daoud, Kristopher J. Krohn, Adrienne Chew, Leslie Cornaby, Kyle J. Foreman, Joseph Frostad, Nicholas J. Kassebaum, Laura Kemmer, Michael Kutz, Patrick Liu, Mojde Mirarefin, Grant Nguyen, Haidong Wang, Ben Zipkin, Amanuel Alemu Abajobir, Marian Abouzeid, Niveen M. E. Abu-Rmeileh, Aliasghar Ahmad Kiadaliri, Muktar Beshir Ahmed, Baran Aksut, Khurshid Alam, Deena Alasfoor, Raghib Ali, Reza Alizadeh-Navaei, Rajaa Al-Raddadi, Ubai Alsharif, Khalid A. Altirkawi, Nelson Alvis-Guzman, Nahla Anber, Palwasha Anwari, Johan Ärnlöv, Solomon Weldegebreal Asgedom, Tesfay Mehari Atey, Ashish Awasthi, Till Bärnighausen, Umar Bacha, Aleksandra Barac, Suzanne L. Barker-Collo, Neeraj Bedi, Derrick A. Bennett, Derbew Fikadu Berhe, Sibhatu Biadgilign, Zahid A. Butt, Jonathan R. Carapetis, Ruben Estanislao Castro, Abdulaal A. Chitheer, Kairat Davletov, Samath D. Dharmaratne, Shirin Djalalinia, Huyen Phuc Do, Manisha Dubey, Hedyeh Ebrahimi, Babak Eshrati, Alireza Esteghamati, Maryam S Farvid, Seyed-Mohammad Fereshtehnejad, Florian Fischer, Solomon Weldemariam Gebrehiwot, Tsegaye Tewelde Gebrehiwot, Richard F. Gillum, Philimon N. Gona, Rajeev Gupta, Nima Hafezi-Nejad, Randah Ribhi Hamadeh, Samer Hamidi, Mohamed Hsairi, Sun Ha Jee, Jost B. Jonas, Chante Karimkhani, Amir Kasaeian, Yousef Saleh Khader, Ejaz Ahmad Khan, Daniel Kim, Dharmesh Kumar Lal, Heidi J. Larson, Asma Abdul Latif, Shai Linn, Paulo A. Lotufo, Raimundas Lunevicius, Hassan Magdy Abd El Razek, Azeem Majeed, Reza Malekzadeh, Deborah Carvalho Malta, Toni Meier, Peter Memiah, Ziad A. Memish, Walter Mendoza, George A. Mensah, Atte Meretoja, Ted R. Miller, Erkin M. Mirrakhimov, Shafiu Mohammed, Quyen Le Nguyen, Vuong Minh Nong, Jonathan Pearson-Stuttard, Farhad Pishgar, Farshad Pourmalek, Mostafa Qorbani, Amir Radfar, Anwar Rafay, Vafa Rahimi-Movaghar, Rajesh Kumar Rai, Saleem M. Rana, David Laith Rawaf, Salman Rawaf, Andre M. N. Renzaho, Satar Rezaei, Kedir Teji Roba, Gholamreza Roshandel, Mahdi Safdarian, Sare Safi, Saeid Safiri, Mohammad Ali Sahraian, Payman Salamati, Abdallah M. Samy, Milena M. Santric Milicevic, Benn Sartorius, Sadaf G. Sepanlou, Masood Ali Shaikh, Diego Augusto Santos Silva, Jasvinder A. Singh, Badr H. A. Sobaih, Konstantinos Stroumpoulis, Rizwan Suliankatchi Abdulkader, Cassandra E. I. Szoeke, Mohamad-Hani Temsah, Bach Xuan Tran, Kingsley Nnanna Ukwaja, Olalekan A. Uthman, Tommi Vasankari, Vasiliy Victorovich Vlassov, Stein Emil Vollset, Tolassa Wakayo, Robert G. Weintraub, Priscilla R. Wessly, Tissa Wijeratne, Charles D. A. Wolfe, Abdulhalik Workicho, Mohsen Yaghoubi, Yuichiro Yano, Mehdi Yaseri, Naohiro Yonemoto, Mustafa Z. Younis, Chuanhua Yu, Maysaa El Sayed Zaki, Aisha O. Jumaan, Theo Vos, Gregory A. Roth, Simon I. Hay, Mohsen Naghavi, Christopher J. L. Murray, and Ali H. Mokdad
References
- Abd El-Aty MA, Meky FA, Morsi MM, Al-Lawati JA, El Sayed MK. Hypertension in the adult Omani population: predictors for unawareness and uncontrolled hypertension. J Egypt Public Health Assoc. 2015;90(3):125–132. doi: 10.1097/01.EPX.0000470547.32952.cf. [DOI] [PubMed] [Google Scholar]
- Ahmad B, Fouad FM, Elias M, Zaman S, Phillimore P, Maziak W. Health system challenges for the management of cardiovascular disease and diabetes: an empirical qualitative study from Syria. Int J Public Health. 2015;60(S1):55–62. doi: 10.1007/s00038-014-0594-2. [DOI] [PubMed] [Google Scholar]
- Barakat H, Barakat H, Baaj MK. CVD and obesity in transitional Syria: a perspective from the Middle East. Vasc Health Risk Manag. 2012;8:145–150. doi: 10.2147/VHRM.S28691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber Ryan M, Fullman Nancy, Sorensen Reed J D, Bollyky Thomas, McKee Martin, Nolte Ellen, Abajobir Amanuel Alemu, Abate Kalkidan Hassen, Abbafati Cristiana, Abbas Kaja M, Abd-Allah Foad, Abdulle Abdishakur M, Abdurahman Ahmed Abdulahi, Abera Semaw Ferede, Abraham Biju, Abreha Girmatsion Fisseha, Adane Kelemework, Adelekan Ademola Lukman, Adetifa Ifedayo Morayo O, Afshin Ashkan, Agarwal Arnav, Agarwal Sanjay Kumar, Agarwal Sunilkumar, Agrawal Anurag, Kiadaliri Aliasghar Ahmad, Ahmadi Alireza, Ahmed Kedir Yimam, Ahmed Muktar Beshir, Akinyemi Rufus Olusola, Akinyemiju Tomi F, Akseer Nadia, Al-Aly Ziyad, Alam Khurshid, Alam Noore, Alam Sayed Saidul, Alemu Zewdie Aderaw, Alene Kefyalew Addis, Alexander Lily, Ali Raghib, Ali Syed Danish, Alizadeh-Navaei Reza, Alkerwi Ala'a, Alla François, Allebeck Peter, Allen Christine, Al-Raddadi Rajaa, Alsharif Ubai, Altirkawi Khalid A, Martin Elena Alvarez, Alvis-Guzman Nelson, Amare Azmeraw T, Amini Erfan, Ammar Walid, Amo-Adjei Joshu, Amoako Yaw Ampem, Anderson Benjamin O, Androudi Sofia, Ansari Hossein, Ansha Mustafa Geleto, Antonio Carl Abelardo T, Ärnlöv Johan, Artaman Al, Asayesh Hamid, Assadi Reza, Astatkie Ayalew, Atey Tesfay Mehari, Atique Suleman, Atnafu Niguse Tadele, Atre Sachin R, Avila-Burgos Leticia, Avokpaho Euripide Frinel G Arthur, Quintanilla Beatriz Paulina Ayala, Awasthi Ashish, Ayele Nebiyu Negussu, Azzopardi Peter, Saleem Huda Omer Ba, Bärnighausen Till, Bacha Umar, Badawi Alaa, Banerjee Amitava, Barac Aleksandra, Barboza Miguel A, Barker-Collo Suzanne L, Barrero Lope H, Basu Sanjay, Baune Bernhard T, Baye Kaleab, Bayou Yibeltal Tebekaw, Bazargan-Hejazi Shahrzad, Bedi Neeraj, Beghi Ettore, Béjot Yannick, Bello Aminu K, Bennett Derrick A, Bensenor Isabela M, Berhane Adugnaw, Bernabé Eduardo, Bernal Oscar Alberto, Beyene Addisu Shunu, Beyene Tariku Jibat, Bhutta Zulfiqar A, Biadgilign Sibhatu, Bikbov Boris, Birlik Sait Mentes, Birungi Charles, Biryukov Stan, Bisanzio Donal, Bizuayehu Habtamu Mellie, Bose Dipan, Brainin Michael, Brauer Michael, Brazinova Alexandra, Breitborde Nicholas J K, Brenner Hermann, Butt Zahid A, Cárdenas Rosario, Cahuana-Hurtado Lucero, Campos-Nonato Ismael Ricardo, Car Josip, Carrero Juan Jesus, Casey Daniel, Caso Valeria, Castañeda-Orjuela Carlos A, Rivas Jacqueline Castillo, Catalá-López Ferrán, Cecilio Pedro, Cercy Kelly, Charlson Fiona J, Chen Alan Z, Chew Adrienne, Chibalabala Mirriam, Chibueze Chioma Ezinne, Chisumpa Vesper Hichilombwe, Chitheer Abdulaal A, Chowdhury Rajiv, Christensen Hanne, Christopher Devasahayam Jesudas, Ciobanu Liliana G, Cirillo Massimo, Coggeshall Megan S, Cooper Leslie Trumbull, Cortinovis Monica, Crump John A, Dalal Koustuv, Danawi Hadi, Dandona Lalit, Dandona Rakhi, Dargan Paul I, das Neves Jose, Davey Gail, Davitoiu Dragos V, Davletov Kairat, De Leo Diego, Del Gobbo Liana C, del Pozo-Cruz Borja, Dellavalle Robert P, Deribe Kebede, Deribew Amare, Des Jarlais Don C, Dey Subhojit, Dharmaratne Samath D, Dicker Daniel, Ding Eric L, Dokova Klara, Dorsey E Ray, Doyle Kerrie E, Dubey Manisha, Ehrenkranz Rebecca, Ellingsen Christian Lycke, Elyazar Iqbal, Enayati Ahmadali, Ermakov Sergey Petrovich, Eshrati Babak, Esteghamati Alireza, Estep Kara, Fürst Thomas, Faghmous Imad D A, Fanuel Fanuel Belayneh Bekele, Faraon Emerito Jose Aquino, Farid Talha A, Farinha Carla Sofia e Sa, Faro Andre, Farvid Maryam S, Farzadfar Farshad, Feigin Valery L, Feigl Andrea B, Fereshtehnejad Seyed-Mohammad, Fernandes Jefferson G, Fernandes João C, Feyissa Tesfaye Regassa, Fischer Florian, Fitzmaurice Christina, Fleming Thomas D, Foigt Nataliya, Foreman Kyle J, Forouzanfar Mohammad H, Franklin Richard C, Frostad Joseph, G/hiwot Tsegaye Tewelde, Gakidou Emmanuela, Gambashidze Ketevan, Gamkrelidze Amiran, Gao Wayne, Garcia-Basteiro Alberto L, Gebre Teshome, Gebremedhin Amanuel Tesfay, Gebremichael Mengistu Welday, Gebru Alemseged Aregay, Gelaye Amha Admasie, Geleijnse Johanna M, Genova-Maleras Ricard, Gibney Katherine B, Giref Ababi Zergaw, Gishu Melkamu Dedefo, Giussani Giorgia, Godwin William W, Gold Audra, Goldberg Ellen M, Gona Philimon N, Goodridge Amador, Gopalani Sameer Vali, Goto Atsushi, Graetz Nicholas, Greaves Felix, Griswold Max, Guban Peter Imre, Gugnani Harish Chander, Gupta Prakash C, Gupta Rahul, Gupta Rajeev, Gupta Tanush, Gupta Vipin, Habtewold Tesfa Dejenie, Hafezi-Nejad Nima, Haile Demewoz, Hailu Alemayehu Desalegne, Hailu Gessessew Bugssa, Hakuzimana Alex, Hamadeh Randah Ribhi, Hambisa Mitiku Teshome, Hamidi Samer, Hammami Mouhanad, Hankey Graeme J, Hao Yuantao, Harb Hilda L, Hareri Habtamu Abera, Haro Josep Maria, Hassanvand Mohammad Sadegh, Havmoeller Rasmus, Hay Roderick J, Hay Simon I, Hendrie Delia, Heredia-Pi Ileana Beatriz, Hoek Hans W, Horino Masako, Horita Nobuyuki, Hosgood H Dean, Htet Aung Soe, Hu Guoqing, Huang Hsiang, Huang John J, Huntley Bethany M, Huynh Chantal, Iburg Kim Moesgaard, Ileanu Bogdan Vasile, Innos Kaire, Irenso Asnake Ararsa, Jahanmehr Nader, Jakovljevic Mihajlo B, James Peter, James Spencer Lewis, Javanbakht Mehdi, Jayaraman Sudha P, Jayatilleke Achala Upendra, Jeemon Panniyammakal, Jha Vivekanand, John Denny, Johnson Catherine, Johnson Sarah C, Jonas Jost B, Juel Knud, Kabir Zubair, Kalkonde Yogeshwar, Kamal Ritul, Kan Haidong, Karch Andre, Karema Corine Kakizi, Karimi Seyed M, Kasaeian Amir, Kassebaum Nicholas J, Kastor Anshul, Katikireddi Srinivasa Vittal, Kazanjan Konstantin, Keiyoro Peter Njenga, Kemmer Laura, Kemp Andrew Haddon, Kengne Andre Pascal, Kerbo Amene Abebe, Kereselidze Maia, Kesavachandran Chandrasekharan Nair, Khader Yousef Saleh, Khalil Ibrahim, Khan Abdur Rahman, Khan Ejaz Ahmad, Khan Gulfaraz, Khang Young-Ho, Khoja Abdullah Tawfih Abdullah, Khonelidze Irma, Khubchandani Jagdish, Kibret Getiye Dejenu, Kim Daniel, Kim Pauline, Kim Yun Jin, Kimokoti Ruth W, Kinfu Yohannes, Kissoon Niranjan, Kivipelto Miia, Kokubo Yoshihiro, Kolk Anneli, Kolte Dhaval, Kopec Jacek A, Kosen Soewarta, Koul Parvaiz A, Koyanagi Ai, Kravchenko Michael, Krishnaswami Sanjay, Krohn Kristopher J, Defo Barthelemy Kuate, Bicer Burcu Kucuk, Kuipers Ernst J, Kulkarni Veena S, Kumar G Anil, Kumsa Fekede Asefa, Kutz Michael, Kyu Hmwe H, Lager Anton Carl Jonas, Lal Aparna, Lal Dharmesh Kumar, Lalloo Ratilal, Lallukka Tea, Lan Qing, Langan Sinead M, Lansingh Van C, Larson Heidi J, Larsson Anders, Laryea Dennis Odai, Latif Asma Abdul, Lawrynowicz Alicia Elena Beatriz, Leasher Janet L, Leigh James, Leinsalu Mall, Leshargie Cheru Tesema, Leung Janni, Leung Ricky, Levi Miriam, Liang Xiaofeng, Lim Stephen S, Lind Margaret, Linn Shai, Lipshultz Steven E, Liu Patrick, Liu Yang, Lo Loon-Tzian, Logroscino Giancarlo, Lopez Alan D, Lorch Scott A, Lotufo Paulo A, Lozano Rafael, Lunevicius Raimundas, Lyons Ronan A, Macarayan Erlyn Rachelle King, Mackay Mark T, El Razek Hassan Magdy Abd, El Razek Mohammed Magdy Abd, Mahdavi Mahdi, Majeed Azeem, Malekzadeh Reza, Malta Deborah Carvalho, Mantovani Lorenzo G, Manyazewal Tsegahun, Mapoma Chabila C, Marcenes Wagner, Marks Guy B, Marquez Neal, Martinez-Raga Jose, Marzan Melvin Barrientos, Massano João, Mathur Manu Raj, Maulik Pallab K, Mazidi Mohsen, McAlinden Colm, McGrath John J, McNellan Claire, Meaney Peter A, Mehari Alem, Mehndiratta Man Mohan, Meier Toni, Mekonnen Alemayehu B, Meles Kidanu Gebremariam, Memish Ziad A, Mengesha Melkamu Merid, Mengiste Desalegn Tadese, Mengistie Mubarek Abera, Menota Bereket Gebremichael, Mensah George A, Mereta Seid Tiku, Meretoja Atte, Meretoja Tuomo J, Mezgebe Haftay Berhane, Micha Renata, Millear Anoushka, Mills Edward J, Minnig Shawn, Mirarefin Mojde, Mirrakhimov Erkin M, Mock Charles N, Mohammad Karzan Abdulmuhsin, Mohammed Shafiu, Mohanty Sanjay K, Mokdad Ali H, Mola Glen Liddell D, Molokhia Mariam, Monasta Lorenzo, Montico Marcella, Moradi-Lakeh Maziar, Moraga Paula, Morawska Lidia, Mori Rintaro, Moses Mark, Mueller Ulrich O, Murthy Srinivas, Musa Kamarul Imran, Nachega Jean B, Nagata Chie, Nagel Gabriele, Naghavi Mohsen, Naheed Aliya, Naldi Luigi, Nangia Vinay, Nascimento Bruno Ramos, Negoi Ionut, Neupane Sudan Prasad, Newton Charles R, Ng Marie, Ngalesoni Frida Namnyak, Ngunjiri Josephine Wanjiku, Nguyen Grant, Ningrum Dina Nur Anggraini, Nolte Sandra, Nomura Marika, Norheim Ole F, Norrving Bo, Noubiap Jean Jacques N, Obermeyer Carla Makhlouf, Ogbo Felix Akpojene, Oh In-Hwan, Okoro Anselm, Oladimeji Olanrewaju, Olagunju Andrew Toyin, Olivares Pedro R, Olsen Helen E, Olusanya Bolajoko Olubukunola, Olusanya Jacob Olusegun, Opio John Nelson, Oren Eyal, Ortiz Alberto, Osborne Richard H, Osman Majdi, Owolabi Mayowa O, PA Mahesh, Pain Amanda W, Pakhale Smita, Castillo Elizabeth Palomares, Pana Adrian, Papachristou Christina, Parsaeian Mahboubeh, Patel Tejas, Patton George C, Paudel Deepak, Paul Vinod K, Pearce Neil, Pereira David M, Perez-Padilla Rogelio, Perez-Ruiz Fernando, Perico Norberto, Pesudovs Konrad, Petzold Max, Phillips Michael Robert, Pigott David M, Pillay Julian David, Pinho Christine, Polinder Suzanne, Pond Constance D, Prakash V, Purwar Manorama, Qorbani Mostafa, Quistberg D Alex, Radfar Amir, Rafay Anwar, Rahimi Kazem, Rahimi-Movaghar Vafa, Rahman Mahfuzar, Rahman Mohammad Hifz Ur, Rai Rajesh Kumar, Ram Usha, Rana Saleem M, Rankin Zane, Rao Paturi Vishnupriya, Rao Puja C, Rawaf Salman, Rego Maria Albertina Santiago, Reitsma Marissa, Remuzzi Giuseppe, Renzaho Andre M N N, Resnikoff Serge, Rezaei Satar, Rezai Mohammad Sadegh, Ribeiro Antonio L, Roba Hirbo Shore, Rokni Mohammad Bagher, Ronfani Luca, Roshandel Gholamreza, Roth Gregory A, Rothenbacher Dietrich, Roy Nawal K, Sachdev Perminder S, Sackey Ben Benasco, Saeedi Mohammad Yahya, Safiri Saeid, Sagar Rajesh, Sahraian Mohammad Ali, Saleh Muhammad Muhammad, Salomon Joshua A, Samy Abdallah M, Sanabria Juan Ramon, Sanchez-Niño Maria Dolores, Sandar Logan, Santos Itamar S, Santos João Vasco, Milicevic Milena M Santric, Sarmiento-Suarez Rodrigo, Sartorius Benn, Satpathy Maheswar, Savic Miloje, Sawhney Monika, Saylan Mete I, Schöttker Ben, Schutte Aletta E, Schwebel David C, Seedat Soraya, Seid Abdulbasit Musa, Seifu Canaan Negash, Sepanlou Sadaf G, Serdar Berrin, Servan-Mori Edson E, Setegn Tesfaye, Shackelford Katya Anne, Shaheen Amira, Shahraz Saeid, Shaikh Masood Ali, Shakh-Nazarova Marina, Shamsipour Mansour, Islam Sheikh Mohammed Shariful, Sharma Jayendra, Sharma Rajesh, She Jun, Sheikhbahaei Sara, Shen Jiabin, Shi Peilin, Shigematsu Mika, Shin Min-Jeong, Shiri Rahman, Shoman Haitham, Shrime Mark G, Sibamo Ephrem Lejore Sibamo, Sigfusdottir Inga Dora, Silva Diego Augusto Santos, Silveira Dayane Gabriele Alves, Sindi Shireen, Singh Abhishek, Singh Jasvinder A, Singh Om Prakash, Singh Prashant Kumar, Singh Virendra, Sinke Abiy Hiruye, Sinshaw Aklilu Endalamaw, Skirbekk Vegard, Sliwa Karen, Smith Alison, Sobngwi Eugene, Soneji Samir, Soriano Joan B, Sousa Tatiane Cristina Moraes, Sposato Luciano A, Sreeramareddy Chandrashekhar T, Stathopoulou Vasiliki, Steel Nicholas, Steiner Caitlyn, Steinke Sabine, Stokes Mark Andrew, Stranges Saverio, Strong Mark, Stroumpoulis Konstantinos, Sturua Lela, Sufiyan Muawiyyah Babale, Suliankatchi Rizwan Abdulkader, Sun Jiandong, Sur Patrick, Swaminathan Soumya, Sykes Bryan L, Tabarés-Seisdedos Rafael, Tabb Karen M, Taffere Getachew Redae, Talongwa Roberto Tchio, Tarajia Musharaf, Tavakkoli Mohammad, Taveira Nuno, Teeple Stephanie, Tegegne Teketo Kassaw, Tehrani-Banihashemi Arash, Tekelab Tesfalidet, Tekle Dejen Yemane, Shifa Girma Temam, Terkawi Abdullah Sulieman, Tesema Azeb Gebresilassie, Thakur JS, Thomson Alan J, Tillmann Taavi, Tiruye Tenaw Yimer, Tobe-Gai Ruoyan, Tonelli Marcello, Topor-Madry Roman, Tortajada Miguel, Troeger Christopher, Truelsen Thomas, Tura Abera Kenay, Uchendu Uche S, Ukwaja Kingsley N, Undurraga Eduardo A, Uneke Chigozie Jesse, Uthman Olalekan A, van Boven Job F M, Van Dingenen Rita, Varughese Santosh, Vasankari Tommi, Venketasubramanian Narayanaswamy, Violante Francesco S, Vladimirov Sergey K, Vlassov Vasiliy Victorovich, Vollset Stein Emil, Vos Theo, Wagner Joseph A, Wakayo Tolassa, Waller Stephen G, Walson Judd L, Wang Haidong, Wang Yuan-Pang, Watkins David A, Weiderpass Elisabete, Weintraub Robert G, Wen Chi-Pang, Werdecker Andrea, Wesana Joshua, Westerman Ronny, Whiteford Harvey A, Wilkinson James D, Wiysonge Charles Shey, Woldeyes Belete Getahun, Wolfe Charles D A, Won Sungho, Workicho Abdulhalik, Workie Shimelash Bitew, Wubshet Mamo, Xavier Denis, Xu Gelin, Yadav Ajit Kumar, Yaghoubi Mohsen, Yakob Bereket, Yan Lijing L, Yano Yuichiro, Yaseri Mehdi, Yimam Hassen Hamid, Yip Paul, Yonemoto Naohiro, Yoon Seok-Jun, Younis Mustafa Z, Yu Chuanhua, Zaidi Zoubida, El Sayed Zaki Maysaa, Zambrana-Torrelio Carlos, Zapata Tomas, Zenebe Zerihun Menlkalew, Zodpey Sanjay, Zoeckler Leo, Zuhlke Liesl Joanna, Murray Christopher J L. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. The Lancet. 2017;390(10091):231–266. doi: 10.1016/S0140-6736(17)30818-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnood-Rod A, Rabbanifar O, Pourzargar P, et al. Adherence to Antihypertensive Medications in Iranian Patients. Int J Hypertens. 2016;2016:1508752. doi: 10.1155/2016/1508752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman JL, Baral R, Birger M, et al. US Spending on Personal Health Care and Public Health, 1996–2013. JAMA. 2016;316:2627–2646. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Bcheraoui C, Basulaiman M, Tuffaha M, et al. Status of the diabetes epidemic in the Kingdom of Saudi Arabia, 2013. Int J Public Health. 2014;59:1011–1021. doi: 10.1007/s00038-014-0612-4. [DOI] [PubMed] [Google Scholar]
- El Bcheraoui C, Memish ZA, Tuffaha M, et al. Hypertension and its associated risk factors in the kingdom of saudi arabia, 2013: a national survey. Int J Hypertens. 2014;2014:564679. doi: 10.1155/2014/564679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 DALYs/HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 SDGs Collaborators Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1813–1850. doi: 10.1016/S0140-6736(16)31467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IHME (2016) Global Burden of Disease Study 2015 (GBD 2015) Data input sources tool. http://ghdx.healthdata.org/gbd-2015/data-input-sources?locations=137&components=3&causes=491. Accessed 10 June 2017
- Institute for Health Metrics and Evaluation (IHME) (2017) GBD Compare Data Visualization https://vizhub.healthdata.org/gbd-compare. Accessed 4 April 2017
- Khatib R, McKee M, Shannon H, et al. Availability and affordability of cardiovascular disease medicines and their effect on use in high-income, middle-income, and low-income countries: an analysis of the PURE study data. The Lancet. 2016;387:61–69. doi: 10.1016/S0140-6736(15)00469-9. [DOI] [PubMed] [Google Scholar]
- Loney T, Aw T-C, Handysides DG, et al. An analysis of the health status of the United Arab Emirates: the ‘Big 4’ public health issues. Global Health Action. 2013;6(1):20100. doi: 10.3402/gha.v6i0.20100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah GA, Roth GA, Sampson UKA, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26:S6–10. doi: 10.5830/CVJA-2015-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi-Lakeh M, El Bcheraoui C, Daoud F, et al. Medication use for chronic health conditions among adults in Saudi Arabia: findings from a national household survey. Pharmacoepidemiol Drug Saf. 2016;25:73–81. doi: 10.1002/pds.3904. [DOI] [PubMed] [Google Scholar]
- Najafipour H, Nasri HR, Afshari M, et al. Hypertension: diagnosis, control status and its predictors in general population aged between 15 and 75 years: a community-based study in southeastern Iran. Int J Public Health. 2014;59:999–1009. doi: 10.1007/s00038-014-0602-6. [DOI] [PubMed] [Google Scholar]
- Nakagami T, Qiao Q, Tuomilehto J, et al. Screen-detected diabetes, hypertension and hypercholesterolemia as predictors of cardiovascular mortality in five populations of Asian origin: the DECODA study. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2006;13:555–561. doi: 10.1097/01.hjr.0000183916.28354.69. [DOI] [PubMed] [Google Scholar]
- Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35(42):2950–2959. doi: 10.1093/eurheartj/ehu299. [DOI] [PubMed] [Google Scholar]
- Romdhane HB, Tlili F, Skhiri A, Zaman S, Phillimore P. Health system challenges of NCDs in Tunisia. Int J Public Health. 2015;60(S1):39–46. doi: 10.1007/s00038-014-0616-0. [DOI] [PubMed] [Google Scholar]
- Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–1678. doi: 10.1161/CIRCULATIONAHA.114.008720. [DOI] [PubMed] [Google Scholar]
- Roth GA, Nguyen G, Forouzanfar MH, Mokdad AH, Naghavi M, Murray CJ. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation. 2015;132(13):1270–1282. doi: 10.1161/CIRCULATIONAHA.115.016021. [DOI] [PubMed] [Google Scholar]
- Shara NM. Cardiovascular disease in Middle Eastern women. Nutr Metabol Cardiovasc Dis. 2010;20(6):412–418. doi: 10.1016/j.numecd.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Smith SC., Jr Reducing the global burden of ischemic heart disease and stroke: a challenge for the cardiovascular community and the United Nations. Circulation. 2011;124(3):278–279. doi: 10.1161/CIRCULATIONAHA.111.040170. [DOI] [PubMed] [Google Scholar]
- Uthman OA, Hartley L, Rees K, Taylor F, Ebrahim S, Clarke A. Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD011163.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Mourik MS, Cameron A, Ewen M, Laing RO. Availability, price and affordability of cardiovascular medicines: a comparison across 36 countries using WHO/HAI data. BMC Cardiovasc Disord. 2010;10:25. doi: 10.1186/1471-2261-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirtz VJ, Kaplan WA, Kwan GF, Laing RO. Access to medications for cardiovascular diseases in low- and middle-income countries. Circulation. 2016;133(21):2076–2085. doi: 10.1161/CIRCULATIONAHA.115.008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Development Indicators database WB (2017) Gross national income per capita 2015, Atlas method and PPP. http://databank.worldbank.org/data/download/GNIPC.pdf. Accessed 10 June 2017
- World-Health-Organization (2010) Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. http://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf. Accessed 4 Apr 2017
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.