Abstract
The American College of Physicians (ACP) recently identified cognitive behavioral therapy for insomnia (CBT-I) as the first-line treatment for insomnia. Although CBT-I improves sleep outcomes and reduces the risks associated with reliance on hypnotics, patients are rarely referred to this treatment, especially in primary care where most insomnia treatment is provided. We reviewed the evidence about barriers to CBT-I referrals and efforts to increase the use of CBT-I services. PubMed, PsycINFO, and Embase were searched on January 11, 2018; additional titles were added based on a review of bibliographies and expert opinion and 51 articles were included in the results of this narrative review. Implementation research testing specific interventions to increase routine and sustained use of CBT-I was lacking. Most research focused on pre-implementation work that revealed the complexity of delivering CBT-I in routine healthcare settings due to three distinct categories of barriers. First, system barriers result in limited access to CBT-I and behavioral sleep medicine (BSM) providers. Second, primary care providers are not adequately screening for sleep issues and referring appropriately due to a lack of knowledge, treatment beliefs, and a lack of motivation to assess and treat insomnia. Finally, patient barriers, including a lack of knowledge, treatment beliefs, and limited access, prevent patients from engaging in CBT-I. These findings are organized using a conceptual model to represent the many challenges inherent in providing guideline-concordant insomnia care. We conclude with an agenda for future implementation research to systematically address these challenges.
Electronic supplementary material
The online version of this article (10.1007/s11606-018-4390-1) contains supplementary material, which is available to authorized users.
KEY WORDS: insomnia, implementation, guidelines, cognitive behavioral therapy for insomnia
INTRODUCTION
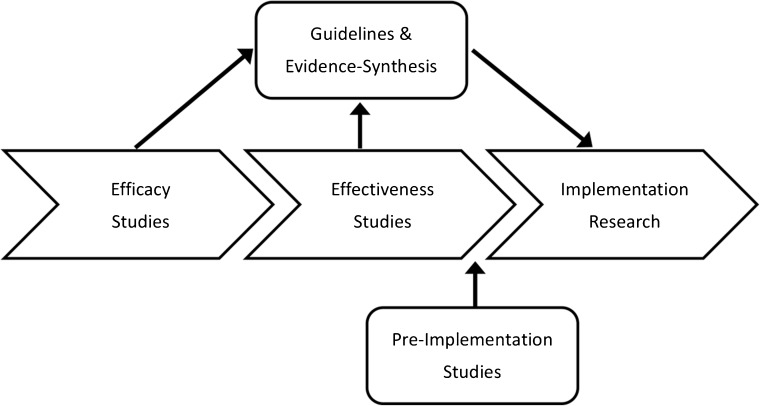
Insomnia is a common and debilitating public health concern that affects nearly 25% of the general population, with economic costs exceeding $100 billion USD per year in poor workplace performance and health care utilization.1,2 Insomnia exacts a great personal cost as well, impairing cognitive, physical, and emotional functioning and greatly reducing quality of life.3 The American College of Physicians (ACP) guidelines for management of chronic insomnia recommend that all patients receive cognitive behavioral therapy for insomnia (CBT-I) as the initial treatment, yet patients are rarely referred to this treatment.4–6 CBT-I is an evidence-based psychotherapy that employs behavioral interventions to regularize sleep cycles and cognitive interventions to address maladaptive thoughts about sleep, reducing the needs and hazards of excessive reliance on hypnotics. The purpose of this review is to explore the gap between guideline recommendations and practice, with the goal of increasing CBT-I access and utilization. As shown in Figure 1, we review pre-implementation studies identifying barriers to CBT-I referrals and implementation studies aiming to increase the use of CBT-I services using implementation interventions (methods designed to enhance adoption of a clinical treatment).7–9
Fig. 1.
Two previous reviews have focused on barriers for implementation of CBT-I.6,10 Cheung et al.10 reviewed the role of patient perceptions of insomnia treatment, but did not discuss provider- and system-level variables. Araujo et al.6 reviewed patient and provider barriers to CBT-I uptake, but limited their review to qualitative studies. This review extends the depth and breadth of this previous work by including pre-implementation and implementation work at system, provider, and patient levels. We develop a conceptual model representing multi-level barriers to implementing CBT-I, concluding with a discussion of promising future directions for implementation work.
METHODS
We collaborated with a biomedical librarian to conduct a search in PubMed, PsycINFO, and Embase for articles pertaining to CBT-I implementation and barriers to use experienced by physicians and patients. Searches began with the year of comprehensive indexing in each database, 1946, 1806, and 1947, respectively, to January 11, 2018. The search included all publication types (full search strategy is presented in the online appendix in the ESM). Inclusion criteria included studies written in English which focused on implementation and dissemination of CBT-I and patient and provider knowledge/beliefs about CBT-I. Additional articles were included based on review of the bibliographies of selected articles (3) and expert opinion (16). Investigators reviewed titles and abstracts of the 2625 articles and selected those that met the inclusion criteria listed above. A total of 2545 articles were deemed out of scope (see online appendix in the ESM for reasons). The remaining 80 articles were reviewed for relevance to CBT-I implementation, with 51 cited in the qualitative synthesis below.
RESULTS
Research on CBT-I implementation is extremely limited and most studies are confined to pre-implementation work within primary care settings. The most robust evidence was for three distinct barriers to CBT-I utilization: (1) system barriers resulting in limited access to CBT-I referral resources, (2) clinician barriers resulting in underutilization of CBT-I services, and (3) patient barriers resulting in under-engagement with CBT-I.
System Barriers
Following ACP guidelines, several commentaries cited limited access to CBT-I providers as a key system barrier to guideline-concordant care.11,12 Demand for CBT-I providers drastically exceeds supply. A recent survey identified just 752 CBT-I specialists worldwide, 88% of whom are unequally distributed across the USA.13 Access barriers have been explored thoroughly in the US Department of Veterans Affairs (VA), where the gap between supply and demand for CBT-I is particularly pronounced. Veterans are one of the most vulnerable groups for developing insomnia, with an estimated 90% reporting sleep disturbances and nearly half above clinical cutoffs for insomnia.14–16 Based on rapidly increasing insomnia prevalence in the VA, an estimated half million veterans already diagnosed with insomnia would likely significantly benefit from CBT-I by the year 2020, with potentially hundreds of thousands more undiagnosed veterans who would also benefit.17–19
Despite the demonstrated need, resources for the evaluation and treatment of sleep disorders within the VA system are extremely limited. The 2012 VA sleep inventory revealed only 112 physician and psychologist full-time employment equivalents across all VA sleep medicine programs.19 VA sleep medicine clinics, where available, are often overwhelmed with assessment and diagnosis of sleep apnea, a condition that has increased in prevalence with increasing rates of obesity.18 Only half of VA sleep medicine programs had access to CBT-I resources in 2012, rendered primarily by employees who did not have full-time employment equivalent allocated to sleep.19
Access problems in the VA are partially addressed by ongoing CBT-I rollout training.20 To date, approximately 700–800 clinicians have been trained as part of the rollout, primarily providing CBT-I outside of sleep medicine programs in behavioral/mental health and primary care; however, it is unknown how many CBT-I-trained providers continue to practice or how many veterans they treat. Most providers are psychologists, psychiatrists, mental health nurses, and social workers and predominantly focus their clinical time treating other mental health conditions. Long-term sustainability and maintenance of treatment fidelity is unknown.20
Clinician Barriers
Research has identified three key clinician barriers leading to underutilization of CBT-I services: lack of knowledge, treatment beliefs, and lack of motivation. In marked contrast to ACP guidelines, the most commonly used treatments remain hypnotic medications and sleep hygiene, a psycho-education approach with insufficient evidence as a stand-alone treatment for chronic insomnia (e.g., avoid stimulants near bedtime, keep bedroom dark and quiet).4,6,21,22 In an online survey with international general health practitioners, the most commonly used sleep treatments were sleep hygiene (88%), pharmacotherapy (63%), and relaxation therapy (44%), and 80% of providers incorrectly believed that sleep hygiene was an efficacious monotherapy.23 A survey study with physicians at university medical centers in the USA demonstrated that less than 10% of patients with a likely diagnosis of insomnia are referred to CBT-I.24 In a survey with VA primary care providers who worked in medical centers with access to CBT-I, only 29% reported utilizing CBT-I to treat insomnia.25 In contrast, over 70% of these providers depended on medications and sleep hygiene.
A common theme in studies with clinicians is that they lack familiarity with CBT-I treatment components and are unsure of the effectiveness.4,6,25–30 In a survey study with Belgian family physicians, only 35% indicated that their knowledge of nonpharmacologic approaches to insomnia was sufficient.30 This finding was replicated in a VA survey study in which 82% of primary care providers had some familiarity with CBT-I, but only 10% had a good understanding and use it in their practice.25 Understandably, clinicians are reluctant to refer to a treatment they do not understand, particularly when they are unsure about the effectiveness of the treatment.31 Moreover, these knowledge gaps make it difficult for primary care clinicians to describe the treatment to patients in a compelling manner. Clinicians are also unsure about referral pathways and how to access CBT-I services.4,27 In the VA, 43% of primary care providers did not know that CBT-I was an available service in their facility.25
A second clinician barrier is treatment beliefs about the utility and acceptability of CBT-I. Traditionally, insomnia has been conceptualized as a symptom rather than a disorder. Many clinicians prioritize treatment of anxiety, depression, pain, or other conditions over insomnia. In a semi-structured interview study with Australian general practitioners, 54% indicated that they treat underlying causes of insomnia first.32 Similarly, a survey study in VA primary care settings shows that clinicians believe that insomnia will resolve sometimes (49%) or often (45%) following treatment of depression and PTSD.25 This barrier stems from a lack of knowledge of insomnia etiology and how it progresses to a chronic disorder. Current diagnostic taxonomies have moved away from classifying insomnia as a secondary disorder since insomnia frequently becomes an independent condition maintained by perpetuating compensatory behaviors and beliefs.33,34
Qualitative studies have shown that even if clinicians think CBT-I would be helpful, they often mistakenly believe that patients would be reluctant to engage and would prefer a medication quick fix.6 A survey study with Australian general practitioners indicated that the most commonly endorsed barrier to using nonpharmacological treatment for insomnia were patients wanting/expecting medication (31%), followed by non-compliance due to the effort required for nonpharmacological treatment (21%).27 Similarly, 39% of general practitioners in a UK survey study indicated that patient demand is the reason they use pharmacological treatments for insomnia35 and 49% of Belgian family physicians indicated that it is too difficult to motivate patients for nonpharmacological treatment for insomnia.30
These clinician beliefs are not supported by research. Although patients acknowledge the appeal of a “magic bullet” to treat insomnia, they are well aware of the limitations of medications.10,36,37 Patients with insomnia perceive nonpharmacological approaches like CBT-I as healthier and preferable to medications for managing insomnia over the long-term.6,27,38–42 In a Norwegian epidemiological study, 80% of respondents who had used sleeping medication indicated that they would prefer nonpharmacological treatment, but only 10% had been offered it.38 Even patients who are already taking hypnotics for insomnia express openness to alternative nonpharmacological treatments.43
A final clinician barrier is a lack of motivation to assess and treat insomnia. Surveys with primary care clinicians suggest that diagnosis and management of insomnia is a low priority compared to other health conditions. One survey in an Australian primary care setting found 83% of clinicians do not proactively assess insomnia, believing patients will raise the issue themselves if they have sleep problems;32 however, nearly 70% of patients with insomnia never discuss their sleep problems with their clinicians.44 Even when patients ask for insomnia treatment, they may not get it. In a UK survey study, nearly 25% of patients with insomnia indicated that they spoke with their doctor about their sleep problem but that their clinician did not seem to think anything could be done about it.45 Qualitative research has shown that most patients learn about CBT-I through extensive research on their own rather than mainstream health services and have to explicitly raise the issue of referral to CBT-I during appointments.36 Clinicians may also be more likely to defer to mental health, especially if they incorrectly believe that insomnia is a symptom of PTSD or depression rather than an independent condition that needs targeted treatment.25
Finally, qualitative interviews with US internal medicine physicians at a university medical center suggested that clinicians may be more likely to prescribe medications to ensure that “the really important business of the clinic visit” takes place, rather than taking time to discuss nonpharmacological options.46 Insomnia is seen as less urgent than other medical symptoms, perhaps due to underestimating the adverse health consequences of poor sleep.6 It is likely that the lack of motivation to properly assess insomnia is related to other barriers discussed above, including limited time, a lack of knowledge about insomnia and nonpharmacological treatments, and insufficient access or knowledge about referral resources.
Patient Barriers
Research has identified several key barriers that prevent patients from engaging with CBT-I, namely knowledge, beliefs, and access. As few as 5% of patients will seek sleep treatment.44 A lack of knowledge or awareness about nonpharmacological treatment options and their effectiveness is one of the top barriers. For example, a survey study with people with insomnia in the UK indicated that 52% of participants did not seek treatment since they thought sleeping pills were the only treatment.45 The most common category of not seeking treatment was the belief that their sleep problems were benign, trivial, or something they felt they should be able to cope with alone (57%).45
Other practical barriers related to access contribute to a reluctance for patients to seek care and engage with CBT-I. One survey study in the UK reported that patients identify times constraints as a significant barrier to seeking insomnia treatment (35%).45 Veterans with insomnia have indicated a preference for “easy” insomnia treatments that accommodate their busy lives; standard CBT-I, delivered over 4–6 weekly or bi-weekly hour-long sessions, may not be feasible for many.47 Additionally, long wait times to get into treatment, as well as long distances to travel, may deter patients from engaging in CBT-I.48 Arranging for child or elder care and requiring appointment times before or after work can further complicate engagement with treatment. Finally, for those with access to care, changing sleep habits and schedules, key aspects of CBT-I, is hard work and far more challenging than taking a pill.11 Qualitative research with patients involved in CBT-I has highlighted the degree of effort and self-discipline needed to fully commit to the therapy.49–51 Up to 40% of patients prematurely drop out of CBT-I in clinical practice,52 and consistent adherence to treatment recommendations generally falls around 47–52%.53–55 Fortunately, an appreciable number of patients who complete treatment benefit, with 70–80% experiencing significant improvements in sleep.56–58
DISCUSSION
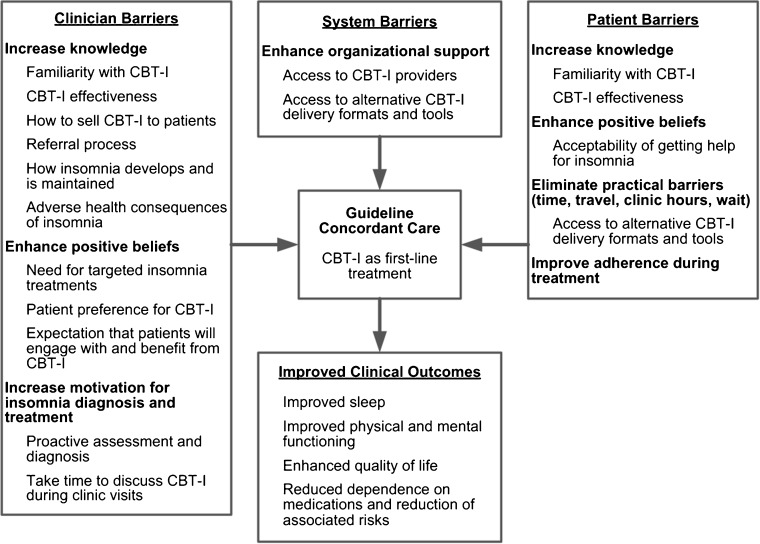
Increasing delivery of CBT-I to patients in real-world settings requires a thoughtful and systematic program of research to develop and test implementation interventions at multiple levels. We present a conceptual model in Figure 2 as a framework for this research, drawing from previous work, including Cabana et al.’s conceptual model of barriers to physician adherence to practice guidelines and Anthierens et al.’s multi-level model of barriers to nonpharmacological treatment of stress, anxiety, and insomnia.30,59 Our model highlights promising intervention targets for future implementation work, which are discussed in more detail below.
Fig. 2.
Intervention targets to increase guideline-concordant management of insomnia in primary care.
Enhancing Knowledge and Beliefs
Clinicians have clearly expressed a desire for improved education about insomnia treatment;4,26 knowledge gaps that could be targeted with educational interventions include the development and maintenance of insomnia, adverse health and functional outcomes associated with insomnia, CBT-I effectiveness, and patient preference for CBT-I, as well as ways to convincingly sell this treatment to patients. It is recommended that education, both early in the training process (e.g., medical school, residency) and throughout the career (e.g., conferences workshops), is crucial for instigating and sustaining change in healthcare systems.60
Some early work has been done in this area. For example, 137 general practitioners in Australia were randomized to receive a 15-min educational intervention in which a doctor or pharmacist visited during office hours to provide education and patient materials pertaining to nonpharmacological treatment of insomnia.61 This significantly reduced the percentage of benzodiazepine prescriptions for newly diagnosed insomnia over the 7-month follow up (85 to 48%).62 Similarly, a promising pilot program within the VA delivers sleep medicine education to rural primary care providers using video-teleconferencing technology.63 This program involves 10 stand-alone 1-h sessions delivered by specialists in sleep, psychology, and pharmacy, and 80% of participants reported increased comfort with the use of nonpharmacological management for insomnia, although they also identified scheduling conflicts and a lack of protected time as substantial participation barriers.
We are currently developing a social marketing campaign to increase knowledge and positive beliefs/attitudes about CBT-I. This approach goes beyond providing educational materials by focusing on strategic marketing of messages to a target audience.64 We anticipate that informational materials for primary care providers will include best practice guidelines, referral information for CBT-I, and recommended talking points for describing CBT-I to patients, presented at monthly clinic meetings. We are also considering CBT-I “champions” within primary care to answer questions about CBT-I and provide feedback about patients who benefit from CBT-I.
Patient education will be an important counterpoint to these clinician-focused efforts, including efforts to reduce the stigma of discussing insomnia with a provider and making information about the effectiveness of CBT-I easily accessible. There is evidence from a preliminary study with 40 primary care patients in Canada that educational brochures about the harms and hazards of hypnotics provided in outpatient waiting rooms significantly improve knowledge, with 45% of patients intending to discuss low-value hypnotic care with their clinicians after reading these brochures.65 Additional work is needed to develop and test targeted educational interventions for patients with chronic use of hypnotics, such as online videos with “expert patients” who have benefited from CBT-I or pamphlets provided through mail or in-person at clinic appointments discussing the benefits of CBT-I vs. hypnotics. This education is necessary to counteract pervasive advertising by pharmaceutical companies and the compelling but unrealistic desire for a “magic bullet” to improve sleep.46,66
Increasing CBT-I Access
Research has demonstrated a vast gap between supply of CBT-I providers and demand for CBT-I providers; lessons learned during national efforts by the VA to train CBT-I providers can be applied to other healthcare settings. For example, participant feedback during this training was used to extend the training workshop (3 vs. 1.5 days) and increase the focus on implementing CBT-I for patients with medical and mental health comorbidities, as well as the development of virtual office hours to provide continued consultation and support for newly trained CBT-I providers.20 Program materials, including competency rating scales and patient materials developed during this initiative, can be used and adapted in future dissemination programs.
Stepped-care models, where different levels of care can be delivered in different settings (e.g., mild to moderate insomnia in primary care, severe comorbid insomnia in specialty mental health) will help those with insomnia get the appropriate level of care by the appropriate provider.67 In order to implement stepped-care models, the VA and other healthcare systems also need to increase access not only to CBT-I providers, but to professionals with expertise in behavioral sleep medicine (BSM) more broadly. These professionals, often psychologists with further specialized training, are a valuable resource for both CBT-I providers and primary care clinicians to help manage patients with more complex comorbidities for whom CBT-I may be contraindicated and for whom other evidence-based approaches are needed (e.g., circadian rhythm disorder, shift work disorder, seizure disorder, traumatic brain injury, bipolar disorder, poorly-managed sleep apnea).
Increased access to CBT-I can also enhance clinician motivation to assess, diagnose, and refer for treatment of insomnia. Simple insomnia screening tools are available, although they are not yet widely integrated into routine clinical care.7 The Insomnia Severity Index, a 7-item patient reported outcome measure, could identify potentially appropriate candidates for CBT-I in primary care, using cut scores of 11 or higher.11,68,69 If brief insomnia screens are not feasible in busy primary care settings, clinicians can defer to trained CBT-I providers to assess patients with an insomnia or sleep complaint and help make decisions about treatment.
Developing and Testing Alternative Delivery Formats for CBT-I
Work is ongoing to develop and test alternative delivery formats for CBT-I to increase access and minimize patient burden and use of healthcare resources. For example, self-management (i.e., self-help) approaches utilizing books, web-based programs, and mobile applications allow patients to stay at home, eliminating both transportation and time barriers.45,70 These approaches also partially address the problem of too few trained CBT-I providers, although qualitative interviews with patients suggest that they prefer to have some form of contact with a CBT-I provider.70 Developing alternative delivery formats for CBT-I may also enhance adherence and improve outcomes, increasing the use of CBT-I by patients and providers. Meta-analyses have found that self-management CBT-I approaches to treating insomnia are efficacious compared to inactive control,71,72 but few studies have compared these approaches to standard CBT-I.
Telephone-delivered CBT-I is a promising approach that minimizes practical barriers (e.g., travel) while providing the desired contact with a trained CBT-I provider; a recent randomized clinical trial demonstrated significant improvement in sleep following a brief, telephone-based CBT-I relative to an education control.73 Within the VA, video telehealth is already used to provide CBT-I to veterans in rural areas, and work is ongoing to develop mobile applications that can be used independently and in conjunction with in-person CBT-I, as well as self-management approaches for insomnia treatment with telephone-based provider support.74–76 These treatments are still in the pilot phase and comparative effectiveness relative to standard CBT-I is unknown.
In primary care settings, brief behavioral treatment for insomnia (BBTI), group CBT-I, and classroom settings have been investigated as a way to deliver the treatment to more patients using fewer resources.77–79 A BBTI protocol with two in-person sessions and two telephone sessions has demonstrated efficacy compared to control groups in veteran populations80,81 and is currently being directly compared to CBT-I.82 Overall, there are a number of promising alternatives to standard CBT-I that have demonstrated efficacy; it is now time to move along the continuum toward effectiveness and implementation trials. Hybrid implementation-effectiveness trials can be used to test the comparative effectiveness of different CBT-I delivery methods under real-world conditions, while simultaneously exploring barriers/facilitators to the uptake and sustainability of these treatments in routine care settings.7,8
CONCLUSIONS
Primary care providers are ideally positioned to make referrals to CBT-I as the first-line treatment for insomnia. Crucial next steps will include developing and testing implementation interventions, including targeted materials marketing CBT-I to patients and providers. Additional efforts are needed in community healthcare settings to adapt and implement existing training models, like those used in the VA, to increase access to CBT-I providers. Although standard CBT-I is a highly effective treatment, the capacity to delivery it cannot begin to meet demand. Comparative effectiveness research testing alternative delivery formats for CBT-I is a necessary part of implementation and will also help establish stepped-care models. Efforts to establish the sustained and routine use of CBT-I will benefit clinicians and patients through the delivery of safe and effective insomnia care for the vast numbers of patients struggling with insomnia.
Electronic Supplementary Material
(DOCX 38 kb)
Acknowledgements
We would like to thank Jonathan Koffel, MSI, for his assistance constructing the search strategy. This material was the result of work supported with resources and the use of facilities at the Minneapolis VA Health Care System, Minneapolis, MN, VA, Pittsburgh Healthcare System, Pittsburgh, PA, and Durham VA Medical Center, Durham, NC. The views expressed in this article are those of the authors and do not reflect the official policy or position of the US Department of Veterans Affairs or the US Government.
Funding Information
Drs. Koffel, Ulmer, and Bramoweth were supported by the Department of Veterans Affairs Health Services Research and Development Service Career Development Awards (CDA 15-063, 09-218, and 13-260, respectively) while working on this manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69(6):592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 2.Wickwire EM, Shaya FT, Scharf SM. Health economics of insomnia treatments: the return on investment for a good night’s sleep. Sleep Med Rev. 2016;30:72–82. doi: 10.1016/j.smrv.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Kyle SD, Espie CA, Morgan K. “...Not just a minor thing, it is something major, which stops you from functioning daily”: quality of life and daytime functioning in insomnia. Behav Sleep Med. 2010;8(3):123–140. doi: 10.1080/15402002.2010.487450. [DOI] [PubMed] [Google Scholar]
- 4.Cheung JM, Atternas K, Melchior M, Marshall NS, Fois RA, Saini B. Primary health care practitioner perspectives on the management of insomnia: a pilot study. Aust J Prim Health. 2014;20(1):103–112. doi: 10.1071/PY12021. [DOI] [PubMed] [Google Scholar]
- 5.Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- 6.Araujo T, Jarrin DC, Leanza Y, Vallieres A, Morin CM. Qualitative studies of insomnia: current state of knowledge in the field. Sleep Med Rev. 2017;31:58–69. doi: 10.1016/j.smrv.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parthasarathy S, Carskadon MA, Jean-Louis G, et al. Implementation of sleep and circadian science: recommendations from the sleep research society and national institutes of health workshop. Sleep. 2016;39(12):2061–2075. doi: 10.5665/sleep.6300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mittman BS. Introduction to implementation science in VA. Enhancing Implementation Science in VA 2012, Introductory Program 2012; https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/eis-050312.pdf. Accessed 1 Feb 2018.
- 10.Cheung JM, Bartlett DJ, Armour CL, Saini B. Treating insomnia: a review of patient perceptions toward treatment. Behav Sleep Med. 2016;14:235–266. doi: 10.1080/15402002.2014.981818. [DOI] [PubMed] [Google Scholar]
- 11.Kathol RG, Arnedt JT. Cognitive behavioral therapy for chronic insomnia: confronting the challenges to implementation. Ann Intern Med. 2016;165(2):149–150. doi: 10.7326/M16-0359. [DOI] [PubMed] [Google Scholar]
- 12.Schmitz MF. The ACP guidelines for treatment of chronic insomnia: the challenge of implementation. Behav Sleep Med. 2016;14(6):699–700. doi: 10.1080/15402002.2016.1220131. [DOI] [PubMed] [Google Scholar]
- 13.Thomas A, Grandner M, Nowakowski S, Nesom G, Corbitt C, Perlis ML. Where are the behavioral sleep medicine providers and where are they needed? A geographic assessment. Behav Sleep Med. 2016;14(6):687–698. doi: 10.1080/15402002.2016.1173551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SP. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38(10):1547–1554. doi: 10.5665/sleep.5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Culver NC, Song Y, Kate McGowan S, et al. Acceptability of medication and nonmedication treatment for insomnia among female veterans: effects of age, insomnia severity, and psychiatric symptoms. Clin Ther. 2016;38(11):2373–2385. doi: 10.1016/j.clinthera.2016.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plumb TR, Peachey JT, Zelman DC. Sleep disturbance is common among servicemembers and veterans of Operations Enduring Freedom and Iraqi Freedom. Psychol Serv. 2014;11(2):209–219. doi: 10.1037/a0034958. [DOI] [PubMed] [Google Scholar]
- 17.Martin JL. What to do about the growing number of veterans diagnosed with sleep disorders? Sleep. 2016;39(7):1331–1332. doi: 10.5665/sleep.5956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander M, Ray MA, Hebert JR, et al. The national veteran sleep disorder study: descriptive epidemiology and secular trends, 2000-2010. Sleep. 2016;39(7):1399–1410. doi: 10.5665/sleep.5972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarmiento K, Rossettie J, Stepnowsky C, Atwood C, Calvitti A. The state of veterans affairs sleep medicine programs: 2012 inventory results. Sleep Breath. 2016;20(1):379–382. doi: 10.1007/s11325-015-1184-0. [DOI] [PubMed] [Google Scholar]
- 20.Manber R, Carney C, Edinger J, et al. Dissemination of CBTI to the non-sleep specialist: protocol development and training issues. J Clin Sleep Med. 2012;8:209–218. doi: 10.5664/jcsm.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung KF, Lee CT, Yeung WF, Chan MS, Chung EW, Lin WL. Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract. 2017. [DOI] [PubMed]
- 22.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504. [PMC free article] [PubMed] [Google Scholar]
- 23.Moss TG, Lachowski AM, Carney CE. What all treatment providers should know about sleep hygiene recommendations. The Behavior Therapist. 2013;36(4):76–83. [Google Scholar]
- 24.Conroy DA, Ebben MR. Referral practices for cognitive behavioral therapy for insomnia: a survey study. Behav Neurol. 2015. [DOI] [PMC free article] [PubMed]
- 25.Ulmer CS, Bosworth HB, Beckham JC, et al. Veterans affairs primary care provider perceptions of insomnia treatment. J Clin Sleep Med. 2017;13(8):991–999. doi: 10.5664/jcsm.6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davy Z, Middlemass J, Siriwardena AN. Patients’ and clinicians’ experiences and perceptions of the primary care management of insomnia: qualitative study. Health Expect. 2013;18(5):1371–1383. doi: 10.1111/hex.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dollman WB, LeBlanc VT, Roughead EE. Managing insomnia in the elderly - what prevents us using non-drug options? J Clin Pharm Ther. 2003;28(6):485–491. doi: 10.1046/j.0269-4727.2003.00523.x. [DOI] [PubMed] [Google Scholar]
- 28.Everitt H, McDermott L, Leydon G, Yules H, Baldwin D, Little P. GPs’ management strategies for patients with insomnia: a survey and qualitative interview study. Br J Gen Pract. 2014;64(619):e112–119. doi: 10.3399/bjgp14X677176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sirdifield C, Anthierens S, Creupelandt H, Chipchase SY, Christiaens T, Siriwardena AN. General practitioners’ experiences and perceptions of benzodiazepine prescribing: systematic review and meta-synthesis. BMC Fam Pract. 2013;14:191. doi: 10.1186/1471-2296-14-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anthierens S, Pasteels I, Habraken H, Steinberg P, Declercq T, Christiaens T. Barriers to nonpharmacologic treatments for stress, anxiety, and insomnia: family physicians’ attitudes toward benzodiazepine prescribing. Can Fam Physician. 2010;56(11):e398–406. [PMC free article] [PubMed] [Google Scholar]
- 31.Lugtenberg M, Zegers-van Schaick JM, Westert GP, Burgers JS. Why don’t physicians adhere to guideline recommendations in practice? An analysis of barriers among Dutch general practitioners. Implement Sci. 2009;4:54. doi: 10.1186/1748-5908-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sake FT, Wong K, Bartlett DJ, Saini B. Insomnia management in the Australian primary care setting. Behav Sleep Med. 2017;18:1–15. doi: 10.1080/15402002.2016.1266491. [DOI] [PubMed] [Google Scholar]
- 33.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- 34.American Academy of Sleep Medicine . International classification of sleep disorders. 3. Darien: Author; 2014. [Google Scholar]
- 35.Siriwardena AN, Apekey T, Tilling M, Dyas JV, Middleton H, Orner R. General practitioners’ preferences for managing insomnia and opportunities for reducing hypnotic prescribing. J Eval Clin Pract. 2010;16(4):731–737. doi: 10.1111/j.1365-2753.2009.01186.x. [DOI] [PubMed] [Google Scholar]
- 36.Cheung JM, Bartlett DJ, Armour CL, Glozier N, Saini B. Insomnia patients’ help-seeking experiences. Behav Sleep Med. 2014;12(2):106–122. doi: 10.1080/15402002.2013.764529. [DOI] [PubMed] [Google Scholar]
- 37.Cheung JMY, Bartlett DJ, Armour CL, Laba TL, Saini B. To drug or not to drug: a qualitative study of patients’ decision-making processes for managing insomnia. Behav Sleep Med. 2016;16:1–26. doi: 10.1080/15402002.2016.1163702. [DOI] [PubMed] [Google Scholar]
- 38.Omvik S, Pallesen S, Bjorvatn B, Sivertsen B, Havik OE, Nordhus IH. Patient characteristics and predictors of sleep medication use. Int Clin Psychopharmacol. 2010;25(2):91–100. doi: 10.1097/YIC.0b013e328334e5e6. [DOI] [PubMed] [Google Scholar]
- 39.Morin CM, Gaulier B, Barry T, Kowatch RA. Patients’ acceptance of psychological and pharmacological therapies for insomnia. Sleep. 1992;15(4):302–305. doi: 10.1093/sleep/15.4.302. [DOI] [PubMed] [Google Scholar]
- 40.Azad N, Byszewski A, Sarazin FF, McLean W, Koziarz P. Hospitalized patients’ preference in the treatment of insomnia: pharmacological versus non-pharmacological. Can J Clin Pharmacol. 2003;10(2):89–92. [PubMed] [Google Scholar]
- 41.Siriwardena AN, Qureshi MZ, Dyas JV, Middleton H, Orner R. Magic bullets for insomnia? Patients’ use and experiences of newer (Z drugs) versus older (benzodiazepine) hypnotics for sleep problems in primary care. Br J Gen Pract. 2008;58(551):417–422. doi: 10.3399/bjgp08X299290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vincent N, Lionberg C. Treatment preference and patient satisfaction in chronic insomnia. Sleep. 2001;24(4):411–417. doi: 10.1093/sleep/24.4.411. [DOI] [PubMed] [Google Scholar]
- 43.Dyas JV, Apekey TA, Tilling M, Orner R, Middleton H, Siriwardena AN. Patients’ and clinicians’ experiences of consultations in primary care for sleep problems and insomnia: a focus group study. Br J Gen Pract. 2010;60(574):e180–200. doi: 10.3399/bjgp10X484183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Culpepper L. Insomnia: a primary care perspective. J Clin Psychiatry. 2005;66 Suppl 9:14–17; quiz 42-13. [PubMed]
- 45.Stinson K, Tang NK, Harvey AG. Barriers to treatment seeking in primary insomnia in the United Kingdom: a cross-sectional perspective. Sleep. 2006;29(12):1643–1646. doi: 10.1093/sleep/29.12.1643. [DOI] [PubMed] [Google Scholar]
- 46.Moloney ME. ‘Sometimes, it’s easier to write the prescription’: physician and patient accounts of the reluctant medicalisation of sleeplessness. Sociol Health Illn. 2017;39(3):333–348. doi: 10.1111/1467-9566.12485. [DOI] [PubMed] [Google Scholar]
- 47.Epstein DR, Babcock-Parziale JL, Haynes PL, Herb CA. Insomnia treatment acceptability and preferences of male Iraq and Afghanistan combat veterans and their healthcare providers. J Rehabil Res Dev. 2012;49(6):867–878. doi: 10.1682/JRRD.2011.06.0114. [DOI] [PubMed] [Google Scholar]
- 48.Pizer SD, Prentice JC. What are the consequences of waiting for health care in the veteran population? J Gen Intern Med. 2011;26(Suppl 2):676–682. doi: 10.1007/s11606-011-1819-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kyle SD, Morgan K, Spiegelhalder K, Espie CA. No pain, no gain: an exploratory within-subjects mixed-methods evaluation of the patient experience of sleep restriction therapy (SRT) for insomnia. Sleep Med. 2011;12(8):735–747. doi: 10.1016/j.sleep.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 50.Faulkner S, Bee P. Perspectives on sleep, sleep problems, and their treatment, in people with serious mental illnesses: a systematic review. PLoS One. 2016;11(9):e0163486. doi: 10.1371/journal.pone.0163486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barnes GL, Lawrence V, Khondoker M, Stewart R, Brown JSL. Participant experiences of attending a community CBT workshop for insomnia: a qualitative six-year follow-up. Behav Sleep Med. 2017;7:1–20. doi: 10.1080/15402002.2017.1301942. [DOI] [PubMed] [Google Scholar]
- 52.Ong JC, Kuo TF, Manber R. Who is at risk for dropout from group cognitive-behavior therapy for insomnia? J Psychosom Res. 2008;64:419–425. doi: 10.1016/j.jpsychores.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vincent N, Hameed H. Relation between adherence and outcome in the group treatment of insomnia. Behav Sleep Med. 2003;1(3):125–139. doi: 10.1207/S15402010BSM0103_1. [DOI] [PubMed] [Google Scholar]
- 54.McChargue DE, Sankaranarayanan J, Visovsky CG, Matthews EE, Highland KB, Berger AM. Predictors of adherence to a behavioral therapy sleep intervention during breast cancer chemotherapy. Support Care Cancer. 2012;20(2):245–252. doi: 10.1007/s00520-010-1060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruiter Petrov ME, Lichstein KL, Huisingh CE, Bradley LA. Predictors of adherence to a brief behavioral insomnia intervention: daily process analysis. Behav Ther. 2014;45(3):430–442. doi: 10.1016/j.beth.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 56.Brasure M, Fuchs E, MacDonald R, et al. Psychological and behavioral interventions for managing insomnia disorder: an evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2016;165:113–124. doi: 10.7326/M15-1782. [DOI] [PubMed] [Google Scholar]
- 57.Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 1999;22(8):1134–1156. doi: 10.1093/sleep/22.8.1134. [DOI] [PubMed] [Google Scholar]
- 58.Trockel M, Karlin BE, Taylor CB, Manber R. Cognitive behavioral therapy for insomnia with veterans: evaluation of effectiveness and correlates of treatment outcomes. Behav Res Ther. 2014;53:41–46. doi: 10.1016/j.brat.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 59.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 60.Grol R, Wensing M. Dissemination of innovations. In: Eccles M, Davis D, editors. Improving patient care: the implementation of change in health care. Chichester: Wiley; 2013. pp. 185–196. [Google Scholar]
- 61.Yeo GT, de Burgh SP, Letton T, et al. Educational visiting and hypnosedative prescribing in general practice. Fam Pract. 1994;11(1):57–61. doi: 10.1093/fampra/11.1.57. [DOI] [PubMed] [Google Scholar]
- 62.Mant A, de Burgh S, Mattick RP, Donnelly N, Hall W. Insomnia in general practice. Results from NSW general practice survey 1991-1992. Aust Fam Physician. 1996;25(Suppl 1):S15–18. [PubMed] [Google Scholar]
- 63.Parsons EC, Mattox EA, Beste LA, et al. Development of a sleep telementorship program for rural department of veterans affairs primary care providers: sleep veterans affairs extension for community healthcare outcomes. Ann Am Thorac Soc. 2017;14(2):267–274. doi: 10.1513/AnnalsATS.201605-361BC. [DOI] [PubMed] [Google Scholar]
- 64.Evans WD. How social marketing works in health care. BMJ. 2006;332(7551):1207–1210. doi: 10.1136/bmj.332.7551.1207-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Silverstein W, Lass E, Born K, Morinville A, Levinson W, Tannenbaum C. A survey of primary care patients’ readiness to engage in the de-adoption practices recommended by Choosing Wisely Canada. BMC Res Notes. 2016;9:301. doi: 10.1186/s13104-016-2103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vitiello MV, McCurry SM, Rybarczyk BD. The future of cognitive behavioral therapy for insomnia: what important research remains to be done? J Clin Psychol. 2013;69(10):1013–1021. doi: 10.1002/jclp.21948. [DOI] [PubMed] [Google Scholar]
- 67.Espie CA. “Stepped care”: a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep. 2009;32(12):1549–1558. doi: 10.1093/sleep/32.12.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gagnon C, Belanger L, Ivers H, Morin CM. Validation of the Insomnia Severity Index in primary care. J Am Board Fam Med. 2013;26(6):701–710. doi: 10.3122/jabfm.2013.06.130064. [DOI] [PubMed] [Google Scholar]
- 69.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cheung JMY, Bartlett DJ, Armour CL, Laba TL, Saini B. Patient perceptions of treatment delivery platforms for cognitive behavioral therapy for insomnia. Behav Sleep Med. 2017;21:1–19. doi: 10.1080/15402002.2017.1293539. [DOI] [PubMed] [Google Scholar]
- 71.Ho FY, Chung KF, Yeung WF, et al. Self-help cognitive-behavioral therapy for insomnia: a meta-analysis of randomized controlled trials. Sleep Med Rev. 2015;19:17–28. doi: 10.1016/j.smrv.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 72.Seyffert M, Lagisetty P, Landgraf J, et al. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PLoS One. 2016;11(2):e0149139. doi: 10.1371/journal.pone.0149139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McCurry SM, Guthrie KA, Morin CM, et al. Telephone-based cognitive behavioral therapy for insomnia in perimenopausal and postmenopausal women with vasomotor symptoms: a MsFLASH randomized clinical trial. JAMA Intern Med. 2016;176(7):913–920. doi: 10.1001/jamainternmed.2016.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Koffel E, Kuhn E, Petsoulis N, et al. A randomized controlled pilot study of CBT-I Coach: feasibility, acceptability, and potential impact of a mobile phone application for patients in cognitive behavioral therapy for insomnia. Health Informatics J. 2016. [DOI] [PubMed]
- 75.Hermes ED, Rosenheck RA. Implementing computer-based psychotherapy among veterans in outpatient treatment for substance use disorders. Psychiatr Serv. 2016;67(2):176–183. doi: 10.1176/appi.ps.201400532. [DOI] [PubMed] [Google Scholar]
- 76.Kuhn E, Weiss BJ, Taylor KL, et al. CBT-I coach: a description and provider perceptions of a mobile app for cognitive behavioral therapy for insomnia. J Clin Sleep Med. 2016;12(4):597–606. doi: 10.5664/jcsm.5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ellis JG, Cushing T, Germain A. Treating acute insomnia: a randomized controlled trial of a “Single-Shot” of cognitive behavioral therapy for insomnia. Sleep. 2015;38(6):971–978. doi: 10.5665/sleep.4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Buysse DJ, Germain A, Moul DE, et al. Efficacy of brief behavioral treatment for chronic insomnia in older adults. Arch Intern Med. 2011;171(10):887–895. doi: 10.1001/archinternmed.2010.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Koffel E, Koffel J, Gehrman P. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med Rev. 2015;19:6–16. doi: 10.1016/j.smrv.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Germain A, Richardson R, Stocker R, et al. Treatment for insomnia in combat-exposed OEF/OIF/OND military veterans: preliminary randomized controlled trial. Behav Res Ther. 2014;61:78–88. doi: 10.1016/j.brat.2014.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pigeon WR, Funderburk J, Bishop TM, Crean HF. Brief cognitive behavioral therapy for insomnia delivered to depressed veterans receiving primary care services: a pilot study. J Affect Disord. 2017;217:105–111. doi: 10.1016/j.jad.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 82.Bramoweth AD, Germain A, Youk AO, Rodriguez KL, Chinman MJ. A hybrid type I trial to increase Veterans' access to insomnia care: study protocol for a randomized controlled trial. Trials. 2018. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 38 kb)