Abstract
Background
Climate change is expected to result in more heat-related, but potentially fewer cold-related, emergency department visits and deaths. The net effect of projected changes in temperature on morbidity and mortality remains incompletely understood. We estimated the change in temperature-related morbidity and mortality at two sites in southern New England, USA through the end of the 21st century.
Methods
We used distributed lag Poisson regression models to estimate the present-day associations between daily mean temperature and all-cause emergency department visits and deaths in Rhode Island and in Boston, Massachusetts. We estimated the change in temperature-related visits and deaths in 2045–2054 and 2085–2094 (relative to 2001–2010) under two greenhouse gas emissions scenarios (RCP4.5 and RCP8.5) using downscaled projections from an ensemble of over 40 climate models, assuming all other factors remain constant.
Results
We observed U-shaped relationships between temperature and morbidity and mortality in Rhode Island, with minima at 10.9 °C and 22.5 °C, respectively. We estimate that, if this population were exposed to the future temperatures projected under RCP8.5 for 2085–2094, there would be 5976 (95% eCI: 1630, 11,379) more emergency department visits but 218 (95% eCI: −551, 43) fewer deaths annually. Results were similar in Boston, and similar but less pronounced in the 2050s and under RCP4.5.
Conclusions
We estimate that in the absence of further adaptation, if the current southern New England population were exposed to the higher temperatures projected for future decades, temperature-related emergency department visits would increase, but temperature-related deaths would not.
Keywords: Hot Temperature, Cold Temperature, Climate Change, Death, Emergency Service, Hospital, New England, Rhode Island, Massachusetts, Boston
Introduction
Global ambient temperatures are projected to rise over the coming decades due to climate change.1 Given the established relationship between high outdoor temperatures (i.e., “heat”) and increased risk of both mortality2,3 and morbidity,4–6 the impact of warmer temperatures on human health has become an area of increasing public health concern.
Studies linking present-day associations between heat and health to output from global climate models suggest that the future burden of mortality and morbidity attributable to heat is likely to increase over the 21st century, all other factors held constant.7–9 However, large analyses examining the impact of temperatures across the calendar year have documented a U-shaped association between temperature and mortality, characterized by a location-specific minimum mortality temperature at which mortality risk is lowest, and elevated risks at temperatures both warmer and colder than the minimum mortality temperature.10,11 Cold temperatures are also associated with higher rates of morbidity,12,13 and recent work suggests a U-shaped association between temperature and all-cause emergency department visits.14 As a result, future increases in heat-related mortality and morbidity due to warming temperatures may be at least partially offset by decreases in cold-related events.
Few studies have projected the impact of changes in temperature across the year on health. Furthermore, work to date in this area15–19 has been primarily focused on mortality rather than morbidity, and has yet to incorporate temperature projections from the Coupled Model Intercomparison Project Phase 5 (CMIP5),20 the state-of-the-art ensemble of coupled ocean-atmosphere circulation models used in the most recent Intergovernmental Panel on Climate Change (IPCC) assessment.1 Accordingly, we estimated the net change in all-cause emergency department visits and deaths attributable to changes in temperature projected for 2045–2054 and 2085–2095 in Rhode Island (RI), a small, coastal state in the New England region of the United States. Specifically, we first estimated present-day exposure-response curves for the association between daily mean temperature and daily counts of emergency department visits and deaths. We then combined these exposure–response curves with downscaled CMIP5 temperature projections under two different sets of assumptions about future greenhouse gas emissions to estimate the change in heat-related, cold-related, and total temperature-related morbidity and mortality. Finally, we replicated our findings at a second study site in New England among residents living in and around Boston, Massachusetts.
Methods
Study Sites
We carried out this analysis at two sites in southern New England, a region located in the northeastern United States. Our primary study site was the state of RI, which had a population in 2010 of 1,052,567.21 For the purpose of replication, we repeated our analysis in the area around and including Boston, a large city located approximately 46 miles to the northeast of the centroid of RI in the adjacent state of Massachusetts (MA). We defined the Boston area (hereafter referred to simply as “Boston”) as all zip codes fully or partially contained within a 10-mile radius of a weather station located in Jamaica Plain, a neighborhood just southwest of the city center. This area, which encompasses the city of Boston as well as some of the surrounding neighborhoods, contained an estimated 1,661,468 people in 2010.22
Exposure Assessment
We obtained historical measurements of daily mean ambient temperature observed at T.F. Green Airport in Warwick, RI (41.7225°, −71.4325°) and in Jamaica Plain, MA (42.3031°, −71.1240°) between 1999 and 2015 from the National Oceanic and Atmospheric Administration’s Climate Data Online database.23 T.F. Green Airport is located approximately 9 km from the geographic centroid of RI and approximately 14 km from downtown Providence, the state’s capital and largest city. We used data from a second Boston weather station located at Logan International Airport (42.3631°, −71.0064°) to impute temperature values for a limited number of days (0.5% of all days 1999–2015) with missing data at Jamaica Plain.
Outcome Assessment
We constructed time series of daily all-cause emergency department visits and deaths at each study site from individual-level data. For RI, we obtained data on emergency department visits (2005–2014) and deaths (1999–2011) from the RI Department of Health. Individual-level emergency department data included visits to all RI hospitals except the Veterans Affairs Hospital and psychiatric hospitals. Individual-level death data included all deaths occurring in RI. We excluded individuals whose state of residence was not RI.
For Boston, we obtained data on emergency department visits (2011–2015) from the MA All-Payer Claims Database maintained by the Center for Health Information and Analysis (CHIA). These data included all individuals who presented for care in an emergency department in MA, as captured by CHIA’s Case Mix dataset, and whose primary residence was within the Boston area, as defined above. We obtained data on deaths (2000–2012) among people 65 years or older living in the Boston area from the Centers for Medicare and Medicaid Services. This study was approved by the Northeastern University and Tufts University institutional review boards. The Brown University institutional review board determined that this work did not constitute human subjects research.
Temperature Projections
We obtained projections of historical and future temperatures from the CMIP5 multi-model ensemble24 for three decades: 2001–2010, 2045–2054 and 2085–2094 (hereafter referred to as 2005, 2050, and 2090). We obtained daily projections for minimum and maximum temperature from approximately 40 models from the CMIP5 ensemble, downscaled to the 1/8° grid cell corresponding to the centroid of RI and to the coordinates of the Jamaica Plain weather station in MA using the bias-correction and constructed analogs approach.25 We estimated mean daily temperature as the averaged daily values of projected minimum and maximum temperature.
To reflect a range of possible future climate policies, models contributing to CMIP5 were run using four Representative Concentration Pathways (RCPs), each of which uses a set of assumptions about future radiative forcing due to anticipated greenhouse gas emissions and other factors. For this study, we used temperature projections under RCP4.5 and RCP8.5. Under RCP8.5, a relatively high emissions scenario, atmospheric carbon dioxide (CO2) concentrations are projected to increase throughout the 21st century and reach 936 ppm by 2100, more than double today’s concentration.26 Under RCP4.5, CO2 concentrations are assumed to stabilize and reach only 538 ppm by 2100.1,27 Daily bias correction and constructed analogue-downscaled temperature projections were available from 42 models for RCP4.5 and from 41 models for RCP8.5 (eTable 1).
Statistical Analysis
Present-day association
We estimated the present-day association between mean daily temperature and both outcomes at each study site as previously described.10 Briefly, we modeled the cumulative association between mean daily temperature and each outcome using distributed lag non-linear models with an over-dispersed Poisson distribution and a 21-day distributed lag function. The choice of lag period reflects that, while hot temperatures typically have a relatively immediate impact on morbidity and mortality, the impact of cold temperatures may persist over a period of weeks.11 We modeled mean daily temperature with a quadratic B-spline with three internal knots placed at the 25th, 50th, and 75th percentiles of mean temperature observed at each study site. We centered the B-spline at the location-specific minimum morbidity temperature for each model of emergency department visits and at the location-specific minimum mortality temperature for each model of deaths. We modeled the lag-response curve for temperature with a natural cubic B-spline with three internal knots placed at equally spaced values on the log scale. In each model we controlled for day of week, federal holidays, and seasonal and long-term time trends (natural cubic spline with 8 degrees of freedom per calendar year). To summarize the shape of the non-linear exposure-response curves, we estimated the percent difference (and 95% confidence interval [CI]) in the incidence rate of each outcome for a range of temperatures compared to the location-specific minimum morbidity or mortality temperature.
We calculated the fraction and annual number of emergency department visits and deaths attributable to deviations from the minimum morbidity or mortality temperature at each study site.28 To understand the relative importance of temperatures across the observed range, we present the fraction and annual number of emergency department visits and deaths attributable to temperature stratified by those attributable to extreme cold (less than the 2.5th percentile of location-specific temperature), moderate cold (2.5th percentile to the minimum morbidity or mortality temperature), moderate heat (minimum morbidity or mortality temperature to the 97.5th percentile), and extreme heat (greater than the 97.5th percentile).
Projected future change
We estimated the change in the annual number of emergency department visits and deaths attributable to heat (temperatures above the location-specific minimum morbidity or mortality temperature), cold (temperatures below the minimum morbidity or mortality temperature), and total temperature (any deviation from the minimum morbidity or mortality temperature), comparing the two future decades (2050 and 2090) to a baseline decade of 2005. In doing so, we used resampling methods to account for uncertainty in both the present-day exposure–response curves and in the projections of future temperatures across different climate models from the CMIP5 ensemble, as described previously.19 Briefly, we repeated the following process 5,000 times for each study site and health outcome. First, we randomly selected one set of parameters describing the lagged, non-linear relationship between temperature and the health outcome from the site-specific distributed lag model, assuming a multivariate normal distribution of those parameters. Next, using this set of parameters, we calculated the annual number of emergency department visits or deaths attributable to temperature28 under each RCP in three decades (2005, 2050, and 2090) using projected historical and future temperatures from one randomly selected climate model. Here, we conservatively applied the relative risk for the maximum temperature observed in the present day at each study site to days in future decades on which temperatures are projected to be even higher. Finally, we subtracted the annual number of temperature-related emergency department visits or deaths estimated for 2005 from the equivalent estimates for 2050 and 2090. By using climate model-projected temperatures to calculate temperature-attributable morbidity and mortality during 2005 and then subtracting this value from the future decade estimates, we correct for any potential differences between climate model projections and observed temperatures during the baseline period.
Iteration of the process described above yields a distribution from which we obtained a point estimate and 95% empirical CIs (eCI) for the net change in temperature-related morbidity and mortality. These numbers can be interpreted as the change (and 95% eCI) in the number of emergency department visits or deaths that would arise each year if the present-day population of each study site were exposed to the daily mean temperatures projected for 2050 and 2090 under each of the two RCPs, all other factors held constant. We repeated this process to estimate the change in morbidity and mortality attributable specifically to heat and cold.
We performed analyses in R version 3.3.129 using ‘dlnm’ package version 2.1.3.30
Results
The distribution of mean daily temperature was similar across study sites, with a mean of 11.2 °C (range: −17.0 °C to 31.7 °C) in RI and 10.7 °C (range: −16.7 °C to 31.4 °C) in Boston (Table 1). There were an average of 1,233 and 1,702 emergency department visits per day in RI and Boston, respectively, occurring predominantly among those under the age of 65. In RI, there were 26 deaths per day on average, the large majority of which (approximately 80%) occurred among individuals aged 65 years and older. In Boston, where data on deaths was limited to those aged 65 years and older, the daily death rate among this subpopulation was 31 deaths per day.
Table 1.
Characteristics of the Rhode Island and Boston area study sites.
| Rhode Island | Boston area a | |
|---|---|---|
| 2010 population size [n] | 1,052,567 | 1,661,468 |
| Daily mean temperature [°C] b | ||
| Minimum | −17.0 | −16.7 |
| 2.5th percentile | −6.9 | −8.1 |
| Mean | 11.2 | 10.7 |
| 97.5th percentile | 26.1 | 26.7 |
| Maximum | 31.7 | 31.4 |
| Emergency department visits c | ||
| Years included | 2005–2014 | 2011–2015 |
| Emergency department visit rate [n/day] | 1,233 | 1,702 |
| Median (IQR d) age | 39 (22, 58) | 35 (21, 54) |
| % 65+ years old | 19.1 | 13.8 |
| % white | 72.3 | 71.5 |
| % female | 53.9 | 52.5 |
| Deaths e | ||
| Years included | 1999–2011 | 2000–2012 |
| Death rate [n/day] | 26 | 31 |
| Median (IQR) age | 80 (69, 88) | 84 (77, 90) |
| % 65+ years old | 79.9 | 100 |
| % white | 94.4 | 89.6 |
| % female | 53.7 | 57.9 |
Defined as a 10-mile radius around the Jamaica Plain weather station
1999–2015
All ages
IQR indicates interquartile range
Deaths among individuals of all ages in Rhode Island; deaths among individuals ≥ 65 years old in the Boston area
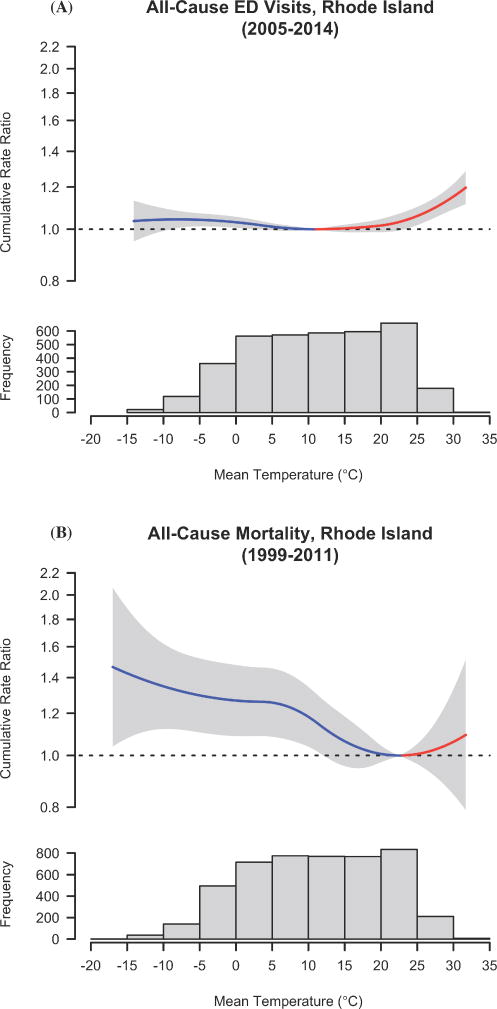
We observed a U-shaped relationship between temperature and emergency department visits in RI, with the minimum morbidity temperature located at 10.9 °C (Figure 1). For example, compared to the minimum morbidity temperature, the rate of emergency department visits was 15.2% (95% CI: 9.0, 21.7) and 4.3% (95% CI: −0.7, 9.5) higher on days with mean temperature of 30 °C and −10 °C, respectively (eTable 2). The relationship between temperature and deaths in RI was also U-shaped (Figure 1); however, the association between warm temperatures and deaths occurred over a relatively small range of observed temperatures due to the relatively higher minimum mortality temperature of 22.5 °C. The exposure–response curves for the association between temperature and both emergency department visits and deaths in Boston were similar to those observed in RI, with minima at 9.2 °C and 24.0 °C for emergency department visits and deaths, respectively (eFigure 1).
Figure 1.
Association between daily mean temperature and (A) cumulative 21-day all-cause emergency department (ED) visits relative to the location-specific minimum morbidity temperature, and (B) cumulative 21-day all-cause deaths relative to the location-specific minimum mortality temperature in Rhode Island.
In RI, 2.0% (95% eCI: 0.8%, 3.3%) of the emergency department visits occurring over the study period were attributable to deviations from the minimum morbidity temperature (10.9 °C), corresponding to an average of 8981 (95% eCI: 3383, 14557) temperature-related emergency department visits each year (Table 2). More emergency department visits were associated with moderate cold and heat, rather than with more extreme temperatures. For deaths, 12.1% (95% eCI: 3.8%, 19.7%) were attributable to deviations from the minimum mortality temperature (22.5 °C), a substantially larger fraction than we observed for emergency department visits. However, the annual average number of deaths attributable to temperature was comparatively smaller (1138 [95% eCI: 356, 1846]). In contrast to the results for morbidity, most temperature-attributable deaths in RI were related to moderate cold. We observed similar results in Boston (Table 2).
Table 2.
Mean (95% empirical confidence interval) fraction of emergency department visits and deaths attributable to deviations from the minimum morbidity or mortality temperature in Rhode Island and Boston. Extreme and moderate cold and heat are defined using the 2.5th and 97.5th percentiles of location-specific mean temperature and the location-specific minimum morbidity or mortality temperature.
| Attributable Fraction (%) | Attributable Number (n/year) | |||
|---|---|---|---|---|
|
| ||||
| Emergency department visits | Deaths | Emergency department visits | Deaths | |
| Rhode Island | ||||
| Total | 2.0% (0.8%, 3.3%) | 12.1% (3.8%, 19.7%) | 8981 (3382, 14557) | 1138 (356, 1846) |
| Extreme cold a | 0.1% (0.002%, 0.2%) | 0.7% (0.3%, 1.1%) | 445 (10, 863) | 70 (30, 104) |
| Moderate cold b | 0.8% (0.05%, 1.4%) | 11.3% (3.4%, 18.4%) | 3383 (220, 6320) | 1059 (316, 1721) |
| Moderate heat c | 0.9% (−0.2%, 2.0%) | 0.03% (−0.2%, 0.3%) | 4050 (−993, 8946) | 3 (−21, 26) |
| Extreme heat d | 0.2% (0.1%, 0.4%) | 0.1% (−0.2%, 0.3%) | 1103 (632, 1587) | 6 (−21, 29) |
| Boston | ||||
| Total | 2.1% (−0.3%, 4.3%) | 14.8% (6.0%, 22.4%) | 12928 (−1660, 26557) | 1646 (653, 2500) |
| Extreme cold a | 0.002% (−0.3%, 0.3%) | 0.8% (0.3%, 1.1%) | 10 (−1694, 1601) | 86 (39, 125) |
| Moderate cold b | 0.7 (−0.4%, 1.8%) | 14.0% (5.4%, 21.7%) | 4222 (−2518, 10786) | 1557 (604, 2425) |
| Moderate heat c | 1.2 (−0.9%, 3.2%) | 0.01% (−0.1%, 0.1%) | 7288 (−5435, 19382) | 1 (−12, 14) |
| Extreme heat d | 0.2 (0.1%, 0.4%) | 0.03% (−0.2%, 0.2%) | 1408 (419, 2369) | 3 (−22, 25) |
< 2.5th percentile of mean temperature
2.5th percentile of mean temperature to the location-specific minimum morbidity or mortality temperature
Location-specific minimum morbidity or mortality temperature to the 97.5th percentile of mean temperature
< 97.5th percentile of mean temperature
Under the lower greenhouse gas emissions scenario (RCP4.5), the CMIP5 model ensemble projects a median increase in mean daily temperature for RI of 1.5 °C (range: 0.3, 2.6) by 2050 and 2.2 °C (range: 0.6, 3.3) by 2090, relative to 2005 (eFigure 2). Median projected increases were larger under the higher greenhouse gas emissions scenario (RCP8.5): 2.0 °C (range 0.9, 3.6) by 2050 and 4.7 °C (range: 2.7, 6.5) by 2090. Projected increases in temperature were similar for Boston.
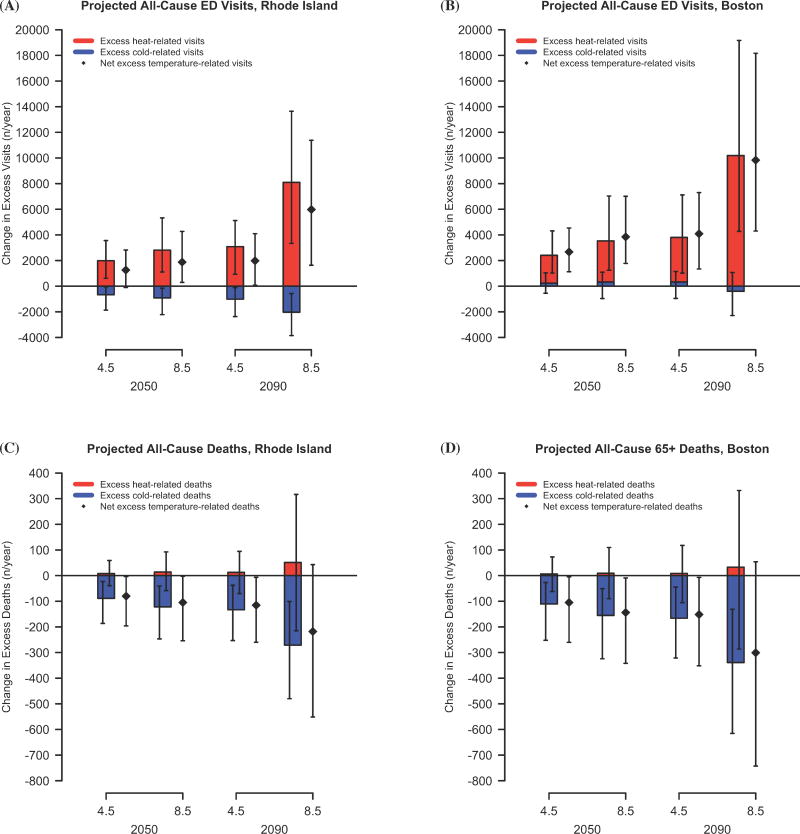
If the current RI population was exposed to the future temperatures projected for 2090 under RCP8.5, we project there would be 8099 (95% eCI: 3332, 13648) more heat-related emergency department visits, but 2032 (95% eCI: −3852, −575) fewer cold-related emergency department visits per year, relative to 2005. We further project that the combined impact of these changes would be a net increase of 5976 (95% eCI: 1630, 11379) temperature-related emergency department visits per year (Figure 2). In contrast, we project that the population of RI would experience 51 (95% eCI: −215, 316) more heat-related deaths and 271 (95% eCI: −480, −101) fewer cold-related deaths per year, resulting in a net decrease in annual temperature-related deaths of −218 (95% eCI: −551, 43). Results were qualitatively similar for Boston. For both sites, our projections for the net change were smaller but in the same direction in 2050 and under RCP4.5 (Tables S3, S4).
Figure 2.
Bar plots of the change (and 95% empirical confidence interval) in annual all-cause emergency department (ED) visits attributable to deviations from the minimum morbidity temperature in (A) Rhode Island and (B) Boston, and in annual all-cause deaths attributable to deviations from the minimum mortality temperature in (C) Rhode Island and (D) Boston, in 2045–2054 and 2085–2094 versus 2001–2010 under two emissions scenarios.
Discussion
Given the U-shaped association between temperature and morbidity and mortality10,31 as well as the general shift to higher daily temperatures projected through the end of the century1, continued climate change is expected to result in more heat-related, but fewer cold-related deaths and emergency department visits. However, whether the net change in temperature-related morbidity or mortality will be positive or negative in a given location remains largely unknown. Accordingly, we quantified the net impact of projected changes in temperature on the number of emergency department visits and deaths at two sites in southern New England through the end of the century.
Consistent with previous work, we found that present-day hot and cold temperatures are both associated with higher mortality rates.10,11 A large, international analysis reported similar U-shaped relationships with an minimum mortality temperature of 23.3 °C for Providence, RI and of 21.9 °C for Boston,10 similar to our observed minimum mortality temperatures of 22.5 °C for RI and 24.0 °C for Boston. The small differences in minimum mortality temperatures between studies may be explained by differences in the length and timing of the study period, the geographic boundaries of each study site, the age group examined, and the use of a meta-analytic model to determine the best linear unbiased prediction of the location-specific temperature-mortality association.
A smaller number of studies have evaluated the impact of year-round temperatures on measures of morbidity such as emergency department visits. In RI, we found that both high and low temperatures were associated with higher rates of all-cause emergency department visits, and that the slope of the exposure-response function was steeper for high temperatures than for low temperatures. A study of Brisbane, Australia, reached similar conclusions regarding the relationship between daily mean temperature and pediatric emergency department visits,13 and a multi-city study in China documented U-shaped relationships between temperature and all-ages, non-external emergency department visits, although with a steeper slope for cold temperatures.14 The association between mean daily temperature and emergency department visits was similar in RI and Boston, although in Boston the shape of the curve at very cold temperatures (where uncertainty is highest) suggests a possible negative association. Additional large, multi-city analyses incorporating a meta-analytic approach would be useful in characterizing exposure-response curves for emergency department visits, particularly in locations where available time series data are limited either in time or in terms of a low number of events per day.
While extreme temperatures were associated with the largest relative rates of emergency department visits and deaths, moderate temperatures were more important in terms of the absolute number of events in both RI and Boston. For example, we found that 11.3% (95% eCI: 3.4, 18.4) of deaths in RI were attributable to moderate cold alone, compared to 12.1% (95% eCI: 3.8. 19.7) attributable to all deviations from the minimum mortality temperatures. Similarly, Gasparrini et al. estimated that 8.8% (95% eCI: 8.0, 9.5) of mortality in 135 US cities is attributable to deviations from city-specific minimum mortality temperatures, and that the large majority is attributable to moderate cold.10 We further found that 2.0% of emergency department visits in RI were attributable to deviations from the minimum morbidity temperature, with the majority attributable to moderate heat and cold. The importance of moderate heat in driving emergency department visits but not deaths may be due to the difference in the minimum morbidity versus minimum mortality temperature (e.g., 10.9 °C vs 22.5 °C in RI), as there are many more days above 10.9 °C than above 22.5 °C.
We project that if the current RI and Boston populations were exposed to the higher daily mean temperatures projected for 2050 and 2090, there would be more heat-related deaths but fewer cold-related deaths, and that the net change would be fewer temperature-related deaths relative to 2005. While several studies project a net increase in temperature-related mortality for various locations in the US,18,32 results from multi-city analyses suggest that the direction of the net change in temperature-related mortality may be depend on characteristics of specific populations or regions,15–17 potentially including air conditioning prevalence, activity patterns, local climate, and population demographics. For example, in a study of ten US metropolitan areas, eight were projected to experience a net increase in temperature-related mortality by 2090 under RCP8.5, while only two (including Boston) were projected to experience a net decrease.19
Contrary to our results for mortality, we found that large projected increases in heat-related emergency department visits will result in a net increase in projected temperature-related emergency department visits. These opposing results are likely driven by the difference between the observed minimum morbidity and mortality temperature. Two factors may contribute to this difference. First, southern New England residents who visited the emergency department were on average much younger than those that died. Accordingly, the minimum morbidity and mortality temperature may reflect age-related differences in susceptibility to the effects of temperature, which could arise from increased physiologic susceptibility to extreme temperatures among the elderly33 or differences in activity patterns by age group. Second, the temperature at which the risk of morbidity and mortality is lowest may differ across disease categories.34 As specific disease categories do not contribute equally to the burden of mortality and morbidity,35,36 the relative contributions of different diseases to temperature-related emergency department visits and deaths may have contributed to the difference in the minimum morbidity and mortality temperatures. Furthermore, the magnitude of the association between temperature and cause-specific health endpoints may also differ for emergency department visits and deaths. For example, warm temperatures are consistently associated with excess cardiovascular mortality, but typically not with excess cardiovascular morbidity.2,4
This study has several limitations. First, relatively low daily mortality rates resulted in limited precision around our estimates for the association between temperature and mortality, and consequently, around the projected future change in annual temperature-related deaths. However, the shape of our exposure–response curves is similar to those observed in southern New England over a longer time period (1985–2006),10 and the net change in temperature-related mortality we project is in the same direction as has been previously projected for Boston.19 Second, some authors have suggested that current modeling practices may overestimate temperature-attributable mortality at the long lag periods often used to look at the impact of cold,37,38 and this may be true for morbidity as well. However, a recent simulation demonstrated that distributed lag non-linear models provide unbiased estimates even when the lag period is as long as three weeks,39 such as in our study. Third, our exposure–response curves do not provide information on morbidity and mortality risk at temperatures higher than those observed during the present day. To estimate the future number of emergency department visits and deaths in 2050 and 2090, we applied the risk ratio for the highest temperature observed during the baseline period (e.g., 32 °C in RI) to days projected to exceed that value. While future temperatures even under the most extreme scenario (RCP8.5 in 2090) rarely exceed 32 °C (on average, fewer than three days per year in RI), this conservative approach may slightly underestimate the increase in heat-related morbidity and mortality.
Additionally, the approach we used to quantify the net impact of projected future temperatures on morbidity and mortality assumes that all other factors remain constant over time, including population size, demographics, and underlying event rates. This approach also assumes that no adaptation or acclimatization to hotter temperatures occurs. Yet, heat-related mortality risk has declined in recent decades both in the US40,41 and abroad42, a trend that may be partially due to increased adaptation to heat. Should adaptation to heat continue, the future number of heat-related emergency department visits and deaths may be lower than the estimates we provide, although the magnitude of this impact will depend on the continued degree and pace of adaptation.43
On the other hand, strengths of this study include the use of an established approach for the estimation of exposure–response curves, the simultaneous assessment of the impact of both hot and cold temperatures in the present day and in future decades, and the evaluation of both morbidity and mortality in the same geographic locations. In addition, our approach for projecting future temperature-attributable morbidity and mortality allowed us to estimate the degree to which uncertainty in both the projections of future temperatures and the exposure–response curves affect our estimates.
In summary, our results confirm that both hot and cold temperatures are associated with emergency department visits and deaths in southern New England. Although current preventive strategies often focus on reducing health impacts at extreme temperatures, consistent with prior studies10,44 we find that moderate temperatures may be more important than extreme temperatures in driving the absolute number of events. Additionally, our results suggest that projected increases in temperature in southern New England may lead to a trade-off in which fewer temperature-related deaths, but more temperature-related emergency department visits are observed. However, in the absence of other changes, we project that there will still be an increase in the number of heat-related deaths, all of which are worth preventing. Furthermore, we project that the magnitude of the increase in temperature-related emergency department visits will be substantial.
Supplementary Material
Acknowledgments
Sources of financial support: The research reported in this publication was supported by grant 5UE1EH001040 from the Centers for Disease Control and Prevention. Dr. Weinberger was supported by a postdoctoral fellowship from the Institute at Brown for Environment and Society and by NIEHS grant F32 ES027742.
We acknowledge the World Climate Research Programme’s Working Group on Coupled Modeling, which is responsible for CMIP, and we thank the climate modeling groups (listed in Supplemental Material, Table S1 of this paper) for producing and making available their model output. For CMIP the U.S. Department of Energy’s Program for Climate Model Diagnosis and Intercomparison provides coordinating support and led development of software infrastructure in partnership with the Global Organization for Earth System Science Portals. We also thank Dr. Xavier Basagaña for critically reviewing an earlier draft of this manuscript, and Sylvia Hobbs, Anne Medinus and Fu Yaying from the Center for Health Information and Analysis in Boston for facilitating our access to emergency department visit data for Massachusetts.
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
Process for obtaining the data and code for replicating this analysis: The computing code and exposure data required to replicate the results reported in this manuscript can be obtained by contacting the corresponding author. The morbidity and mortality data can be obtained by making data requests to the Rhode Island Department of Health, the Massachusetts Center for Health Information and Analysis, and the Centers for Medicare and Medicaid Services.
References
- 1.IPCC. Climate Change 2013: The Physical Science Basis. In: Stocker TF, Qin D, Plattner GK, Tignor M, Allen SK, Boschung J, Nauels A, Xia Y, Bex V, Midgley PM, editors. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2013. [Google Scholar]
- 2.D’Ippoliti D, Michelozzi P, Marino C, de’Donato F, Menne B, Katsouyanni K, Kirchmayer U, Analitis A, Medina-Ramon M, Paldy A, Atkinson R, Kovats S, Bisanti L, Schneider A, Lefranc A, Iniguez C, Perucci CA. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health. 2010;9:37. doi: 10.1186/1476-069X-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson GB, Bell ML. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ Health Perspect. 2011;119(2):210–8. doi: 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environmental Health Perspectives. 2014;122(11):1187–1192. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- 6.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. Jama. 2014;312(24):2659–67. doi: 10.1001/jama.2014.15715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kingsley SL, Eliot MN, Gold J, Vanderslice RR, Wellenius GA. Current and Projected Heat-Related Morbidity and Mortality in Rhode Island. Environ Health Perspect. 2016;124(4):460–7. doi: 10.1289/ehp.1408826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ostro B, Barrera-Gomez J, Ballester J, Basagana X, Sunyer J. The impact of future summer temperature on public health in Barcelona and Catalonia, Spain. Int J Biometeorol. 2012;56(6):1135–44. doi: 10.1007/s00484-012-0529-7. [DOI] [PubMed] [Google Scholar]
- 9.Peng RD, Bobb JF, Tebaldi C, McDaniel L, Bell ML, Dominici F. Toward a quantitative estimate of future heat wave mortality under global climate change. Environ Health Perspect. 2011;119(5):701–6. doi: 10.1289/ehp.1002430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, Tobias A, Tong S, Rocklov J, Forsberg B, Leone M, De Sario M, Bell ML, Guo YL, Wu CF, Kan H, Yi SM, de Sousa Zanotti Stagliorio Coelho M, Saldiva PH, Honda Y, Kim H, Armstrong B. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369–75. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, Lavigne E, de Sousa Zanotti Stagliorio Coelho M, Leone M, Pan X, Tong S, Tian L, Kim H, Hashizume M, Honda Y, Guo YL, Wu CF, Punnasiri K, Yi SM, Michelozzi P, Saldiva PH, Williams G. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25(6):781–9. doi: 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavigne E, Gasparrini A, Wang X, Chen H, Yagouti A, Fleury MD, Cakmak S. Extreme ambient temperatures and cardiorespiratory emergency room visits: assessing risk by comorbid health conditions in a time series study. Environmental Health. 2014;13(1):5. doi: 10.1186/1476-069X-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu Z, Hu W, Su H, Turner LR, Ye X, Wang J, Tong S. Extreme temperatures and paediatric emergency department admissions. J Epidemiol Community Health. 2014;68(4):304–11. doi: 10.1136/jech-2013-202725. [DOI] [PubMed] [Google Scholar]
- 14.Zhao Q, Zhang Y, Zhang W, Li S, Chen G, Wu Y, Qiu C, Ying K, Tang H, Huang J, Williams G, Huxley R, Guo Y. Ambient temperature and emergency department visits: time-series analysis in 12 Chinese cities. Environmental Pollution. 2017;224:310–316. doi: 10.1016/j.envpol.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Martin SL, Cakmak S, Hebbern CA, Avramescu ML, Tremblay N. Climate change and future temperature-related mortality in 15 Canadian cities. Int J Biometeorol. 2012;56(4):605–19. doi: 10.1007/s00484-011-0449-y. [DOI] [PubMed] [Google Scholar]
- 16.Vardoulakis S, Dear K, Hajat S, Heaviside C, Eggen B, McMichael AJ. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ Health Perspect. 2014;122(12):1285–92. doi: 10.1289/ehp.1307524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz JD, Lee M, Kinney PL, Yang S, Mills D, Sarofim MC, Jones R, Streeter R, Juliana AS, Peers J, Horton RM. Projections of temperature-attributable premature deaths in 209 U.S. cities using a cluster-based Poisson approach. Environ Health. 2015;14:85. doi: 10.1186/s12940-015-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mills D, Schwartz J, Lee M, Sarofim M, Jones R, Lawson M, Duckworth M, Deck L. Climate change impacts on extreme temperature mortality in select metropolitan areas in the United States. Climatic Change. 2015;131:83–95. [Google Scholar]
- 19.Weinberger KR, Haykin L, Eliot MN, Schwartz JD, Gasparrini A, Wellenius GA. Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environment International. 2017;107:196–204. doi: 10.1016/j.envint.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor KE, Stouffer RJ, Meehl GA. An overview of CMIP5 and the experiment design. Bulletin of the American Meteorological Society. 2012;93:485–498. [Google Scholar]
- 21.U.S. Census Bureau. 2010 Census of Population and Housing, Population and housing Unit Counts, CPH-2-31. Rhode Island. Washington, DC: 2012. [Google Scholar]
- 22.U.S. Census Bureau. [Accessed 22 September, 2016];TIGER/Line Shapefile, 2010, 2010 State, Massachusetts, 2010 Census Block State-Based. http://www.census.gov/geo/www/tiger.
- 23.NOAA. Climate Data Online. 2016. [Google Scholar]
- 24.Maurer EP, Brekke L, Pruitt T, Duffy PB. Fine-resolution climate projections enhance regional climate change impact studies. Eos, Transactions American Geophysical Union. 2007;88(47):504. [Google Scholar]
- 25.Bureau of Reclamation; U.S. Department of the Interior, Bureau of Reclamation, Technical Services Center, editor. Downscaled CMIP3 and CMIP5 Climate and Hydrology Projections: Release of Downscaled CMIP5 Climate Projections, Comparison with Preceding Information, and Summary of User Needs. Denver, Colorado: 2013. [Google Scholar]
- 26.van Vuuren DP, Edmonds J, Kainuma M, Riahi K, Thomson A, Hibbard K, Hurtt GC, Kram T, Krey V, Lamarque J-F, Masui T, Meinshausen M, Nakicenovic N, Smith SJ, Rose SK. The representative concentration pathways: an overview. Climatic Change. 2011;109:5–31. [Google Scholar]
- 27.Thomson AM, Calvin KV, Smith SJ, Kyle GP, Volke A, Patel P, Delgado-Arias S, Bond-Lamberty B, Wise MA, Clarke LE, Edmonds JA. RCP4. 5: a pathway for stabilization of radiative forcing by 2100. Climatic Change. 2011;109:77–94. [Google Scholar]
- 28.Gasparrini A, Leone M. Attributable risk from distributed lag models. BMC Med Res Methodol. 2014;14:55. doi: 10.1186/1471-2288-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 30.Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. Journal of Statistical Software. 2011;43(8):1–20. [PMC free article] [PubMed] [Google Scholar]
- 31.Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li T, Horton RM, Kinney P. Future projections of seasonal patterns in temperature-related deaths for Manhattan. Nat Clim Chang. 2013;3:717–721. doi: 10.1038/nclimate1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environmental Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kovats RS, Hajat S, Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, U. K Occup Environ Med. 2004;61:893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control. [Accessed 30 May 2016];Deaths, percent of total deaths, and death rates for the 15 leading causes of death: United States and each State. 2011 http://www.cdc.gov/nchs/data/dvs/lcwk9_2011.pdf.
- 36.Centers for Disease Control. [Accessed 30 May 2016];National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf.
- 37.Kinney PL, Schwartz J, Pascal M, Petkova E, Le Tertre A, Medina S, Vautard R. Winter season mortality: will climate warming bring benefits? Environmental Research Letters. 2015;10(064016) doi: 10.1088/1748-9326/10/6/064016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ebi KL, Mills D. Winter mortality in a warming climate: a reassessment. WIREs Climate Change. 2013;4(3):203–212. [Google Scholar]
- 39.Gasparrini A. Modelling lagged associations in environmental time series data: a simulation study. Epidemiology. 2016;27(6):835–842. doi: 10.1097/EDE.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Petkova EP, Gasparrini A, Kinney PL. Heat and mortality in New York City since the beginning of the 20th century. Epidemiology. 2014;25(4):554–60. doi: 10.1097/EDE.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bobb JF, Peng RD, Bell ML, Dominici F. Heat-related mortality and adaptation to heat in the United States. Environmental Health Perspectives. 2014;122(8):811–816. doi: 10.1289/ehp.1307392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, Zanobetti A, Schwartz JD, Tobias A, Leone M, Tong S, Honda Y, Kim H, Armstrong BG. Temporal variation in heat-mortality associations: a multicountry study. Environmental Health Perspectives. 2015;123(11):1200–1207. doi: 10.1289/ehp.1409070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Petkova EP, Vink JK, Horton RM, Gasparrini A, Bader DA, Frances JD, Kinney PL. Towards more comprehensive projections of urban heat-related mortality: estimates for New York City under multiple population, adaptation, and climate scenarios. Environmental Health Perspectives. 2016 doi: 10.1289/EHP166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wellenius GA, Eliot MN, Bush KF, Holt D, Lincoln RA, Smith AE, Gold J. Heat-related morbidity and mortality in New England: evidence for local policy. Environmental Research. 2017;156:845–853. doi: 10.1016/j.envres.2017.02.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.