Abstract
Ultramarathon-associated corneal edema is a rare phenomenon. We report a case of a patient who presented with bilateral corneal edema following an ultramarathon. The corneal edema resolved without sequelae 48 h later. The authors hypothesize that the additive effect of enhanced glycolysis, an increased lactate level in the aqueous humor, and oxidative stress alters the normal endothelial regulation of the cornea and leads to corneal edema.
Keywords: Corneal edema, Ultramarathon, Visual impairment
Introduction
Corneal edema is not commonly seen as a result of athletic activities. In a survey-based investigation, 173 ultramarathon runners described their visual impairment as painless blurred vision that resolved spontaneously 24–48 h after they stopped running. Corneal edema was confirmed via slit lamp examination in eight of the runners [1]. This phenomenon was also reported in a cyclist in a 161-km mountain bike race [2]. Long-distance endurance sports may have an impact on the cornea and affect its normal mechanism of maintaining transparency. For the purpose of this review, an ultramarathon is defined as any running competition longer than 26.2 miles (42.2 km), with most races falling between 40 and 100 miles (70–160 km). We present a case of a patient with bilateral corneal edema occurring immediately after an ultramarathon, and hypothesize on the possible underlying mechanisms.
Case Report
A 44-year-old white man experienced painless bilateral blurring of vision during and after an ultramarathon event in Park City, Utah, in April 2011. He noticed the visual impairment primarily in the right eye during the last few hours of the ultramarathon and presented to our clinic 5 h after completion of the event. This was his first ultramarathon and he had not had any similar episodes of visual impairment in previous athletic activities. Past medical history included hyperlipidemia, controlled by atorvastatin (Lipitor). Family, social, surgical and ophthalmologic histories were non-contributory. He presented to the clinic the evening after the event. The patient involved provided written informed consent to having his data used for research purposes, in accordance with the tenets of the Declaration of Helsinki.
On eye examination, the patient had visual acuity of 20/200 OD and 20/30 OS. Intraocular pressure was 17 mmHg OD and 18 mmHg OS. Extraocular muscle movements were intact. The orbits and eyelids revealed no evidence of trauma. On slit lamp examination, the right eye had diffuse 3+ corneal edema with a few Descemet’s folds (Figs. 1 and 2) while the left eye had trace to 1+ corneal edema located on the nasal periphery of the cornea and dissipated at the temporal side. The conjunctivae had no injection and there was no corneal epithelial abrasion in either eye. The anterior chamber, iris and lens were normal in both eyes. There was no evidence of pigment dispersion. A dilated pupil fundus exam revealed a normal optic nerve, vasculature and macula on the left side, and only red reflex was appreciated in the right eye due to corneal edema.
Fig. 1.
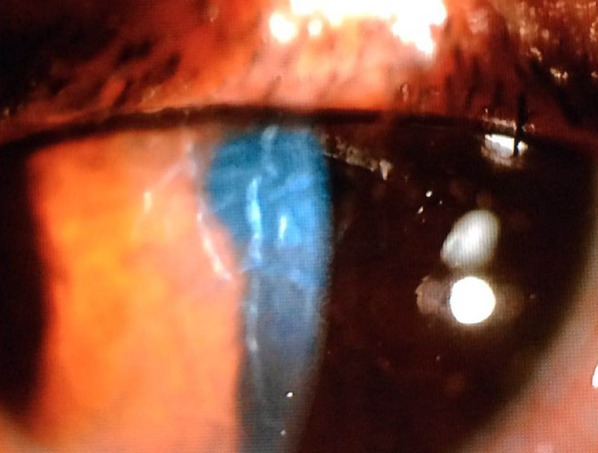
Diffuse corneal edema and Descemet’s folds in right eye
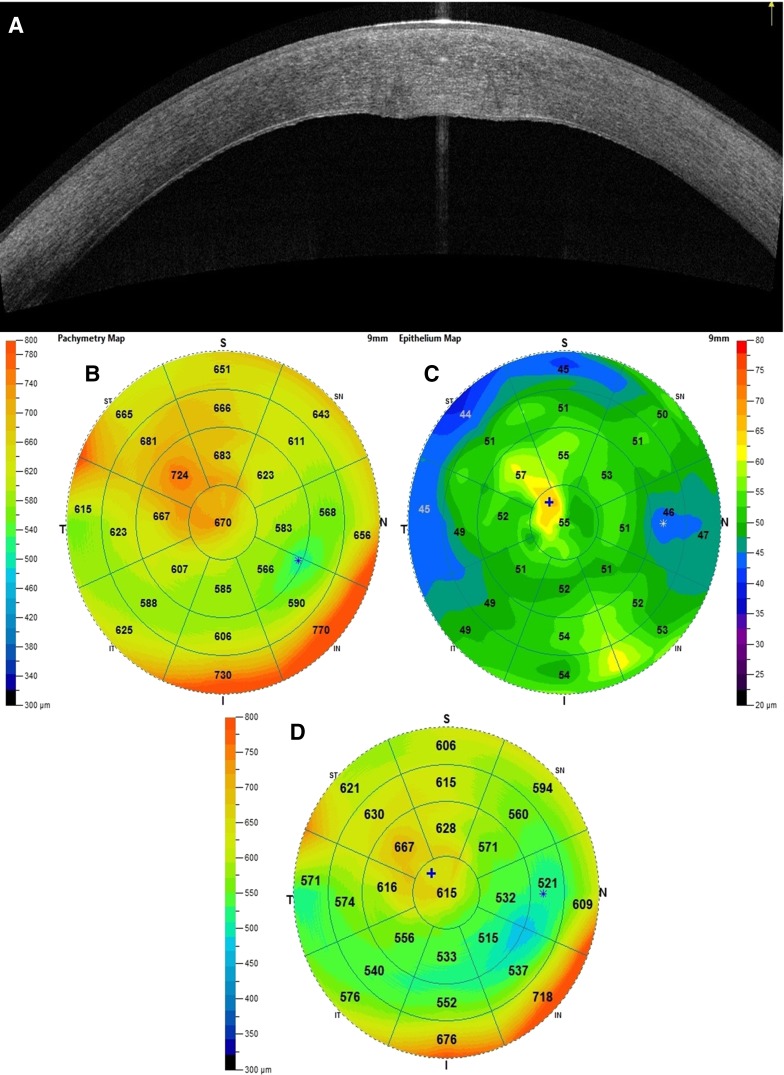
Fig. 2.
a OCT of right eye showing diffuse thickening secondary to corneal edema, affecting the epithelium as well. b Total corneal thickness. c Epithelial corneal thickness. d Stromal corneal thickness
The patient was prescribed prednisolone acetate 1% ophthalmic suspension QID for both eyes. His vision subjectively recovered to his baseline 12 h later, and an eye exam performed 48 h after the episode showed complete recovery of both corneas without sequelae. Endothelial microscopy/counting was not performed.
Discussion
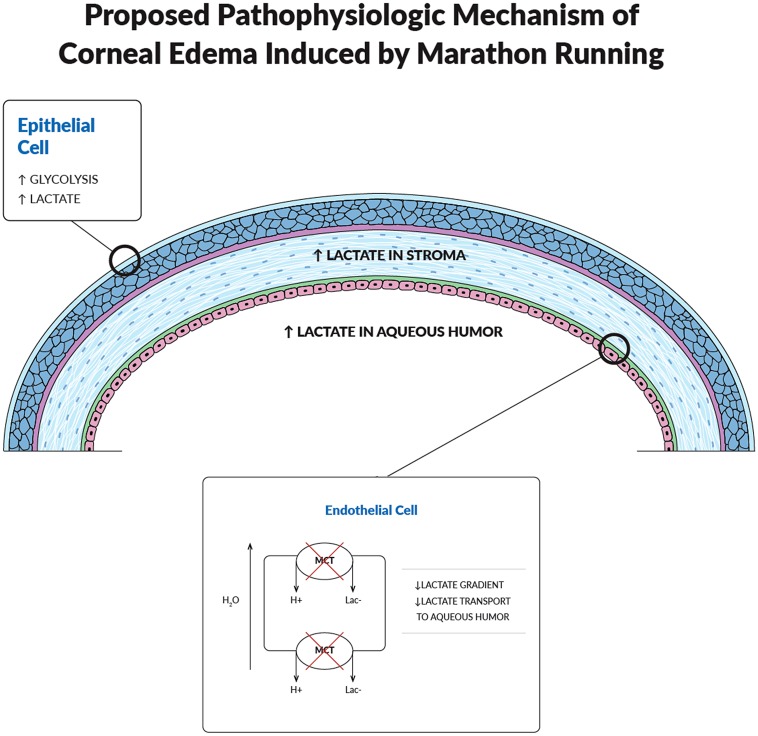
Ultramarathon events have been growing in popularity over the past decade [3]. These events usually take place in a mountainous area on a course mixed with trails, tough road and significant elevation changes [4]. Men’s and women’s records for the Western States Endurance Run, which is 161 km, are 14:46:44 and 16:47:19, respectively [5]. Many runners take 24–36 h to finish these races. As Hoeg et al. mentioned in their investigation, environmental stimuli increase the metabolic rate of the cornea [1]. During the race, the corneal epithelium must endure wind, temperature changes and enhanced ultraviolet (UV) light exposure, and cope with decreased oxygen tension at higher elevations. Unlike track runners, who anticipate no obstacles ahead, ultramarathon runners must constantly use their eyes to select the best path. This visual attention reduces the spontaneous blink rate [6], which intensifies the physical challenge to the corneal epithelium. Cells cope with environmental stress such as thermal changes with enhanced glycolysis [7]. Certain mechanisms involving cellular damage repair rely more upon glycolysis than upon oxidative phosphorylation [8]. When the corneal epithelium increases glycolysis in this constant running state, lactate production increases. Bonanno explained the movement of lactate across the epithelium to the aqueous humor in the following pattern [9]: (a) lactate is transferred to the stroma by the lactate-proton cotransporter located at the membrane of epithelial cells [10]; (b) lactate moves across the stroma by simple diffusion down the gradient to the membrane; (c) lactate-proton cotransporter and sodium-dependent lactate transporter facilitate the entry of lactate into endothelial cells; (d) lactate then exits the endothelial membrane by lactate-proton cotransporter to enter the anterior chamber [11]. Stromal lactate accumulation has been proven to be responsible for corneal edema, because increased osmolality attracts water [12]. Elevated lactate levels were detected in the blood of amateur ultramarathon runners during a 100-km run [13]. Elevation of blood lactate could cause increased lactate in the aqueous humor, which would in turn decrease the lactate gradient between endothelial cells and aqueous humor, thus impairing the facilitated transport of lactate to the anterior chamber. We agree with Hoeg et al. [1] that this accumulation of lactate caused by increased production and decreased excretion is one of the underlying mechanisms of the acute corneal edema induced by ultramarathon running (Fig. 3).
Fig. 3.
Possible pathophysiologic mechanisms that may result in corneal edema in individuals during an ultramarathon (MCT monocarboxylate cotransporter or lactate cotransporter, Lac- lactate, H+ hydrogen, H2O water)
There are other potential causes of corneal edema during ultramarathons. High altitude causes hypoxia and increased exposure to UV light, and is known to induce an increase in central corneal thickness [14]. Hypoxia-induced corneal edema has been shown quantitatively in multiple studies in contact lens wearers [15, 16]. In a study investigating how UVA-induced oxidation affects different corneal cells, Zinflou et al. found that corneal epithelial cells can adapt more quickly than endothelial cells [17]. The mechanism through which epithelial cells limit UVA-induced toxicity likely involves enhanced glycolysis to create more ATP. On the other hand, the susceptibility of endothelium to UVA can damage the pump function of the endothelium, which is the driving force in moving water out of the stroma [9]. Our patient experienced his event at high altitude (Park City, UT, USA, roughly 7000 feet elevation) and endured relatively distinct temperature changes (26.8–37.3 °C). Both could be contributing factors to the development of his corneal edema. The definite cause of the difference in severity of corneal edema in our patient’s eyes is unknown, but we suggest that it may be due to different degrees of exposure to external irritants such as UV light and wind.
Other contributing factors causing corneal edema could include (a) participants wearing soft contact lenses; (b) participants with prior corneal refractive surgery changing the original structure of the anterior layers of the cornea, which could affect the metabolism and excretion of lactate into the aqueous humor; and (c) corneal endothelial dystrophy altering the regulation of corneal hydration.
After reviewing limited literature concerning this matter, we hypothesize that patients who wear soft contact lenses (especially with higher correction), have silent guttata and subclinical endothelial dystrophies, have a history of corneal transplantation, suffer from dry eye, or have had corneal refractive surgery such as LASIK have a higher risk of developing corneal edema during ultramarathon events.
Eye protection should be the most effective method for preventing corneal edema during long-endurance sports, since it provides shielding from wind and UV light. Administration of topical 5% hypertonic sodium chloride can enhance corneal clarity in the event of corneal edema. Rest or closure of the eyes would be ideal but is probably not realistic during the competition. Since dehydration can further increase the blood lactate level, adequate hydration is advised.
Conclusion
Ultramarathon-induced corneal edema is a rare multifactorial phenomenon. The additive effect of enhanced glycolysis, decreased lactate excretion to the aqueous humor, ambient temperature changes, hypoxia, and oxidative stress caused by exposure to UV light can impact the normal endothelial regulation of the cornea and may lead to corneal edema. Inter-subject variability may be the result of varying metabolic rates and endothelial pump function, as well as membrane transporter efficiency.
Acknowledgements
Funding
This study was funded by an unrestricted grant from Research to Prevent Blindness (RPB), 360 Lexington Avenue, 22nd Floor, New York, NY, 10017. No support was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published.
Disclosures
Majid Moshirfar, Yanning Ding, Yasmyne Ronquillo, Orry C. Birdsong, and Michael S. Murri have nothing to disclose.
Compliance with Ethics Guidelines
The patient involved provided written informed consent to having his data used for research purposes, in accordance with the tenets of the Declaration of Helsinki.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to 10.6084/m9.figshare.5938717.
References
- 1.Hoeg TB, Corrigan GK, Hoffman MD. An investigation of ultramarathon-associated visual impairment. Wilderness Environ Med. 2015;26(2):200–204. doi: 10.1016/j.wem.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Khodaee M, Torres DR. Corneal opacity in a participant of a 161-km mountain bike race at high altitude. Wilderness Environ Med. 2016;27(2):274–276. doi: 10.1016/j.wem.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Scott D. Number of ultramarathons has doubled in the last decade|Runner’s World [Internet]. 2014 [cited 2018 Jan 11]. p. para 1. https://www.runnersworld.com/newswire/number-of-ultramarathons-has-doubled-in-the-last-decade.
- 4.100 mile course description| run rabbit run| 50 &100 mile endurance races| Steamboat Springs, CO [Internet]. [cited 2018 Jan 11]. http://runrabbitrunsteamboat.com/courses/100-mile-course-description/.
- 5.Records—western states endurance run [Internet]. [cited 2018 Jan 11]. http://www.wser.org/records/.
- 6.De Jong PJ, Merckelbach H. Eyeblink frequency, rehearsal activity, and sympathetic arousal. Int J Neurosci. 1990;51(1–2):89–94. doi: 10.3109/00207459009000513. [DOI] [PubMed] [Google Scholar]
- 7.Jimenez AG, Williams JB. Rapid changes in cell physiology as a result of acute thermal stress house sparrows, Passer domesticus. J Therm Biol. 2014;46:31–39. doi: 10.1016/j.jtherbio.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Rybchyn MS, De Silva WGM, Sequeira VB, McCarthy BY, Dilley AV, Dixon KM, et al. Enhanced repair of UV-induced DNA damage by 1,25-dihydroxyvitamin D3 in skin is linked to pathways that control cellular energy. J Investig Dermatol. 2017 doi: 10.1016/j.jid.2017.11.037. [DOI] [PubMed] [Google Scholar]
- 9.Bonanno JA. Effects of contact lens-induced hypoxia on the physiology of the corneal endothelium. Optom Vis Sci. 2001;78(11):783–790. doi: 10.1097/00006324-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Bonanno JA. Lactate-proton cotransport in rabbit corneal epithelium. Curr Eye Res. 1990;9(7):707–712. doi: 10.3109/02713689008999587. [DOI] [PubMed] [Google Scholar]
- 11.Giasson C, Bonanno JA. Facilitated transport of lactate by rabbit corneal endothelium. Exp Eye Res. 1994;59(1):73–81. doi: 10.1006/exer.1994.1082. [DOI] [PubMed] [Google Scholar]
- 12.Klyce SD. Stromal lactate accumulation can account for corneal oedema osmotically following epithelial hypoxia in the rabbit. J Physiol. 1981;321:49–64. doi: 10.1113/jphysiol.1981.sp013971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jastrzebski Z, Zychowska M, Konieczna A, Ratkowski W, Radziminski L. Changes in the acid-base balance and lactate concentration in the blood in amateur ultramarathon runners during a 100-km run. Biol Sport. 2015;32(3):261–265. doi: 10.5604/20831862.1163372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris DS, Somner JE a, Scott KM, McCormick IJC, Aspinall P, Dhillon B. Corneal thickness at high altitude. Cornea [Internet]. 2007;26(3):308–11. http://www.ncbi.nlm.nih.gov/pubmed/23156091. [DOI] [PubMed]
- 15.Bonanno JA, Nyguen T, Biehl T, Soni S. Can variability in corneal metabolism explain the variability in corneal swelling? Eye Contact Lens. 2003;29(1 Suppl):S7-9-9, S192–4. [DOI] [PubMed]
- 16.Nguyen T, Soni PS, Brizendine E, Bonanno JA. Variability in hypoxia-induced corneal swelling is associated with variability in corneal metabolism and endothelial function. Eye Contact Lens. 2003;29(2):117–125. doi: 10.1097/01.ICL.0000062462.73172.18. [DOI] [PubMed] [Google Scholar]
- 17.Zinflou C, Rochette PJ. Ultraviolet A-induced oxidation in cornea: characterization of the early oxidation-related events. Free Radic Biol Med. 2017;108:118–128. doi: 10.1016/j.freeradbiomed.2017.03.022. [DOI] [PubMed] [Google Scholar]