Highlights
-
•
Gallbladder torsion is a rare condition of increasing prevalence in recent years.
-
•
Two types of anatomical predispositions have been described in gallbladder torsion.
-
•
Classically, a “triad of triads” has been described to aid in the clinical diagnosis of gallbladder torsion.
-
•
Delayed recognition and intervention can lead to fatal sequelae including gangrene and perforation.
Keywords: Case report, Hepatobiliary surgery, Cholecystitis, Acalculous cholecystitis, Cholecystectomy, Gallbladder torsion
Abstract
Introduction
Gallbladder torsion is a rare condition of increasing prevalence in recent years. It is often difficult to diagnose pre-operatively and delayed intervention can lead to significant complications.
Presentation of case
We present a case of an 81 year old lady who presented with symptoms of cholecystitis for 24 h with no evidence of cholelithiasis on imaging. She deteriorated within 24 h of admission despite intravenous antibiotics; Emergency laparoscopy was performed which showed the gallbladder malrotated 180 ° with features of necrosis. Laparoscopic cholecystectomy was performed without complications.
Discussion
The cause of gallbladder torsion are thought to be due to underlying anatomical variations or loss of elasticity associated with aging. Diagnosis is difficult clinically and radiologically, however, features such as “whirl sign” and “cystic duct knot sign” have been described. Due to ischemia associated with torsion, clinical vigilance and early intervention is recommended to prevent potential fatal sequelae particularly in the elderly population.
Conclusion
Gallbladder torsion is a rare finding that can be difficult to diagnose clinically, we are hoping to promote awareness to prevent complications associated with delayed therapy.
1. Introduction
This case report is in line with the SCARE criteria [1].
Gallbladder torsion is a rare condition which was initially described in 1898 and is of increasing prevalence in recent years. The cause of torsion is usually due to underlying anatomical variations along with the loss of elasticity associated with aging. Given its time-critical nature, we hope to promote awareness and encourage prompt surgical management in patients with suspected gallbladder torsion.
2. Case report
An 81 year old Caucasian lady with no previous medical or surgical history presented to the Emergency Department of a peripheral hospital. She complained of a 24 h history of severe, diffuse abdominal pain but was otherwise well. On initial assessment, patient was haemodynamically stable and apyrexial. Abdominal examination revealed a soft, non-distended abdomen with maximal tenderness over the right upper quadrant with no features of peritonism.
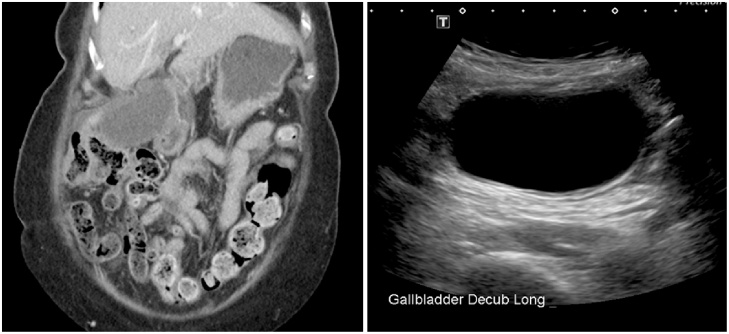
Her laboratory studies were re-assuring: Haemoglobin 133 g/L, leukocytes 9.2 × 109/L, CRP 2.4 mg/L with normal renal and hepatic functions. A Contrast enhanced CT of her abdomen demonstrated a distended gallbladder with no other findings to account for her symptoms. A subsequent ultrasound of her biliary system noted a distended gallbladder with increased wall thickness of 5 mm without hyperaemia or pericholecystic fluid [Fig. 1]. There were also no biliary calculi and the common bile duct was of normal calibre.
Fig 1.
CT Scan at time of admission demonstrates a large, distended gallbladder with normal wall thickness and common bile duct calibre. US scan demonstrating a mildly thickened gallbladder wall with no calculi.
The patient was admitted and commenced on intravenous antibiotics for presumed early acalculous cholecystitis. 24 h after admission, the patient developed abdominal distension with localised peritonism in the right upper quadrant. Her repeat laboratory studies showed a leucocyte count of 12.5 × 109/L with CRP trending up to 289U/L with no significant changes in her liver function tests.
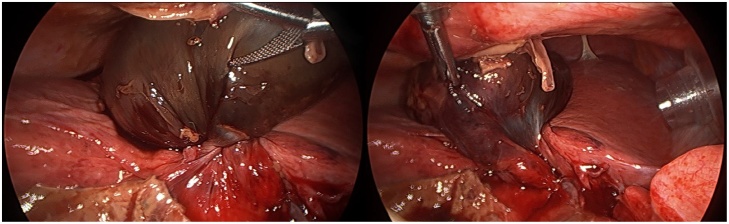
Decision was made for an emergency laparoscopic cholecystectomy given her clinical deterioration. Intra-operatively, the gallbladder was found to be loosely adherent to the inferior aspect of the liver and was malrotated 180 ° anticlockwise along the axis of the cystic duct and artery resulting in distension and gangrene [Fig. 2]. There was a moderate volume of free fluid with associated ileus of the small bowel. Total cholecystectomy was performed with relative ease due to very minimal connective tissue anchoring of the gallbladder to the gallbladder fossa. Intra-operative cholangiogram confirmed adequate intrahepatic and extrahepatic ductal flow without filling defect.
Fig. 2.
Left: Laparoscopic cholecystectomy: Intra-operative finding of a large, distended gangrenous gallbladder which has undergone a 180 ° anticlockwise torsion along the cystic duct and artery. Right: Laparoscopic cholecystectomy: Unwinding the torted gallbladder reveals a loose strand of mesentery as the only attachment for the gallbladder to the liver.
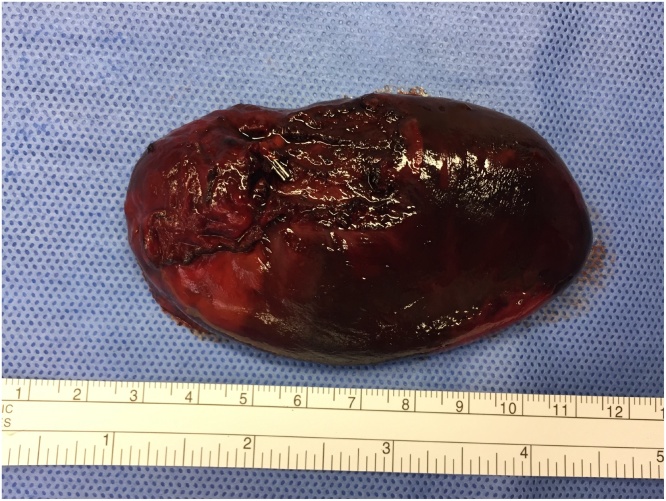
Histopathological assessment of the gallbladder demonstrated an intact gallbladder measuring 75 × 40 × 35 mm containing semisolid, thickened bile with no calculi. The wall thickness predominantly measured 1 mm with an area of congestion at the fundus measuring 5 mm [Fig. 3]. Microscopically, there was dense neutrophilic infiltrate with areas of haemorrhage and transmural necrosis consistent with acute gangrenous acalculous cholecystitis.
Fig. 3.
Post-operative examination of the resected specimen demonstrates a 75 mm long, thin walled gallbladder with extensive areas of necrosis.
There were no post-operative complications and the patient was discharged on post-operative day 4. Interestingly, it was noted retrospectively that her mother and all three of her sisters have undergone emergency cholecystectomies for what was described by the patient as “severe cholecystitis”.
3. Discussion
Gallbladder torsion was first described by Wendel in 1898–a case of a 23 year old female diagnosed with a “floating gallbladder.” The findings included an anomalous length of the cystic duct measuring three and a quarter inches with a mesentery anchoring the duct to the inferior aspect of the liver as the sole attachment for the gallbladder [2]. As of 2014, approximately 500 cases have been reported with a noted increase in incidence over the recent years [3].
The predisposing factors are congenital or acquired anatomical variations. Two types of congenital variants have been described: in one form, the gallbladder has a loose mesenteric attachment that is prone to torsion (as seen in our patient); in the other form, the gallbladder “floats” in the abdomen with the mesentery supporting only the cystic duct as described by Wendel. The presumed acquired risk factors are the loss of elasticity and visceral tissue as a result of aging which may explain the higher prevalence amongst elderly females [4]. The mechanisms of torsion are thought to be due to the presence of kyphoscoliosis, a tortuous and atherosclerotic cystic artery or intense peristalsis of the neighbouring bowel [5].
Gallbladder torsion is a challenging pre-operative diagnosis. Our patient initially displayed clinical features to suggest cholecystitis but had very little biochemical and radiological evidence to confirm the diagnosis. This may be due to a partial torsion at presentation which progressed to a complete torsion 24 h later. Lau et al. in 1982 have suggested a “triad of triads” to aid the diagnosis of gallbladder torsion [6] and radiologically, there may be indirect signs of a gangrenous process or perforation to suggest torsion including pericholecystic fluid, gallbladder wall thickening, thumb printing of the gallbladder and avascularity of the gallbladder on ultrasound scans. Furthermore, an anterior, free-floating gallbladder may also be seen in gallbladder torsion and it has been suggested that “Whirl Sign” on CT scans [7] and “cystic duct knot sign” on ultrasound scans [8] may be pathognomonic for gallbladder torsion.
In summary, early recognition and surgical intervention are crucial in preventing potentially fatal sequelae of gallbladder torsion. Ironically, laparoscopic cholecystectomy in the setting of gallbladder torsion may be performed with relative ease due to the lack of mesenteric attachments.
Conflicts of interest
There are no conflicts of interest, financial, personal or otherwise which could influence bias.
Sources of funding
No funding was needed for this case report, except for the amount required if published.
Ethical approval
Ethical approval was not required for this case as it is exempted by our institution.
Consent
Written consent was from the patient to write this case report and accompanying images. Identifying details have been omitted.
Author contribution
Dr Jason Cui – corresponding author. Review of patient notes, drafted article and critically analysed and approved final submission.
Dr Mariya Abdullah – Critical analysis of draft and approved final submission.
Dr Iman Awan – Critical revision of draft and approved final submission.
Guarantor
Dr Daniel Mehanna.
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Wendel A.V. VI. A case of floating gall-bladder and kidney complicated by cholelithiasis, with perforation of the gall-bladder. Ann. Surg. 1898;27(2):199–202. [PMC free article] [PubMed] [Google Scholar]
- 3.Pu T.W., Fu C.Y., Lu H.E., Cheng W.T. Complete body-neck torsion of the gallbladder: a case report. World J. Gastroenterol. 2014;20(October (38)):14068–14072. doi: 10.3748/wjg.v20.i38.14068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsuhashi N., Satake S., Yawata K., Asakawa E., Mizoguchi T., Kanematsu M., Kondo H., Yasuda I., Nonaka K., Tanaka C., Misao A., Ogura S. Volvulus of the gallbladder diagnosed by ultrasonography, computed tomography, coronal magnetic resonance imaging and magnetic resonance cholangio-pancreatography. World J. Gastroenterol. 2006;12:4599–4601. doi: 10.3748/wjg.v12.i28.4599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Losken A., Wilson B.W., Sherman R. Torsion of the gallbladder: a case report and review of the literature. Am. Surg. 1997;63:975–978. [PubMed] [Google Scholar]
- 6.Lau W.Y., Fan S.T., Wong S.H. Acute torsion of the gallbladder in the aged: a re-emphasis on clinical diagnosis. Aust. N. Z. J. Surg. 1982;52:492–494. doi: 10.1111/j.1445-2197.1982.tb06036.x. [DOI] [PubMed] [Google Scholar]
- 7.Tajima Y., Tsuneoka N., Kuroki T. Clinical images. Gallbladder torsion showing a whirl sign on a multidetector computed tomography scan. Am. J. Surg. 2009;197(January (1)):e9–e10. doi: 10.1016/j.amjsurg.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Dasyam A.K., Koo J., Stahlfeld Miller M., Sell H.W., Jr., Tublin M.E. The cystic duct knot sign: case report with description of a new ultrasound sign of gallbladder torsion. Emerg. Radiol. 2015;22(August (4)):445–447. doi: 10.1007/s10140-015-1331-8. [DOI] [PubMed] [Google Scholar]