Abstract
Collaborative Care is a comprehensive longitudinal care management strategy. The purpose of this pilot effectiveness-implementation hybrid study was to determine the feasibility of a Collaborative Care intervention initiated from the Emergency Department and proceeding longitudinally for six months for injured patients with prescription drug misuse (PDM). Adult patients presenting to an urban ED with an injury were screened for eligibility from 2/2015-8/2015. Eligible participants with a positive screen for PDM were enrolled in the ‘ED-LINC’ intervention which included the following elements: 1) active care coordination and linkage, 2) medication safety and utilization of opioid guidelines 3) longitudinal care management and 4) utilization of Electronic Medical Record (EMR) innovations such as the statewide Emergency Department Information Exchange (EDIE) and statewide prescription monitoring program information for assessment and follow-up. Baseline characteristics of the sample were assessed and regression models were used to evaluate longitudinal trajectories of risk for PDM. A total of 36 participants (56% of patients approached) had PDM and 30 participants were enrolled. Of those enrolled, 37% had prescription stimulant misuse, 20% with prescription sedative misuse and 97% had prescription opioid misuse. Follow-up rates at all time points were ≥ 83%. Baseline levels of comorbidity were high; 57% endorsed recent heroin use and 70% endorsed symptoms consistent with major depression. Over 50% had five or more statewide ED visits and 53% had used three or more different ED‘s in the past year. On average, participants received a total of 85 minutes of ED-LINC over six months with 90% of participants receiving all four intervention elements. All patients had care coordinated with new or existing primary care providers (PCP’s) and 23% were linked to a new PCP. A majority of patients (≥ 80%) reported receiving high quality, desired intervention services. There was no significant change in PDM over time. Collaborative Care initiated from the ED is feasible and acceptable to patients with trauma and PDM. Future directions could include effectiveness-implementation hybrid trials to study implementation barriers and strategies as well as patient-level outcomes of this intervention for this complex patient population.
Keywords: Emergency Medicine, prescription drug misuse, collaborative care
1. Introduction
In 2012 approximately 6.8 million Americans reported misuse of prescription drugs in the past month, which exceeds the number of Americans using cocaine, heroin, hallucinogens, and inhalants combined (Substance Abuse and Mental Health Services Administration, 2013b). The opioid epidemic in the United States continues with drug overdose deaths tripling from 1999-2014 and opioids being the most commonly implicated drug (Rudd, Aleshire, Zibbell, & Gladden, 2016). In addition to prescription opioid misuse, all types of prescription or pharmaceutical drug misuse is on the rise. In 2011, over half of all drug-related Emergency Department (ED) visits involved misuse of a pharmaceutical or prescription drug (e.g., opioid, sedative, stimulant) (Substance Abuse and Mental Health Services Administration, 2013a). Prescription drug misuse (PDM), defined as use of a prescription opioid, sedative or stimulant without a prescription, more than was prescribed or using to get high, is a serious public health problem that can lead to injection drug use, (Jones, 2013) addiction, (Bohnert et al., 2013) and fatal overdose (Jones, Mack, & Paulozzi, 2013).
The ED is a critical health care location to capture patients with PDM that may not otherwise access the health care system in a predictable, consistent way. Additionally, patients with substance use comorbidity utilize the ED for care more than patients without substance use comorbidity (Rockett, Putnam, Jia, Chang, & Smith, 2005). Behavioral-based interventions from the ED for substance use have typically focused on a brief intervention model and have provided mixed results. Specifically, screening brief intervention and referral to treatment (SBIRT) has been effective from the ED for patients with alcohol problems (D’Onofrio et al., 2012; Walton et al., 2010) and reduces overdose risk behaviors (Bohnert et al., 2016). SBIRT for drug use has provided mixed results. A large multi-site trial showed no effect of SBIRT for drugs from the ED, (Bogenschutz et al., 2014) while a recent study showed SBIRT to be effective from the ED in a population of patients with problematic drug use mostly related to marijuana (Blow et al., 2017). It is possible that SBIRT may not be sufficient for treating patients with substance use problems, which may require longitudinal coordinated care. While most ED’s have social workers that can provide substance use counseling and referral, only 30% of patients receive social work services while in the ED and these services rarely include longitudinal care coordination (Moore et al., 2016). Previous care coordination intervention studies from the ED have focused on reducing ED visits and opioid prescriptions for patients with disorders such as chronic pain without addressing comorbidity or providing evidence-based behavioral therapies (D. Neven et al., 2016; Olsen, Ogarek, Goldenberg, & Sulo, 2016).
Collaborative Care (CC) is a comprehensive patient-centered model of healthcare delivery targeting behavioral health or substance use that stems from the chronic care management framework (B. F. Miller, Kessler, Peek, & Kallenberg, 2011; Von Korff, Gruman, Schaefer, Curry, & Wagner, 1997; Wagner, Austin, & Von Korff, 1996). Elements central to CC can include brief behavioral intervention, team-based care for care coordination, evidence based pharmacotherapy guideline application and care management with coordinated longitudinal health care (Von Korff et al., 1997; Zatzick et al., 2014). A comprehensive care delivery system such as CC has produced effective treatment outcomes in primary care settings for complex heterogeneous patients with comorbid mental illness and medical problems (Dobscha et al., 2009; Katon et al., 2010; Richardson et al., 2014; Sharpe et al., 2014; Unutzer et al., 2002). In substance use treatment centers, integrated substance use and depression care improves outcomes for both comorbidities (Watkins et al., 2011). Such existing models are promising but are not directly applicable to patients in the ED with PDM as they require populations that are already engaged in a primary care practice or an existing health care system. Initial investigations of CC in acute care trauma center settings suggest that the model may be effective in linking patients to primary care services and community services. These CC interventions have effectively targeted PTSD and alcohol use for patients with serious injuries after acute trauma requiring inpatient care (Zatzick et al., 2013; Zatzick et al., 2014).
The complex comorbidity patterns in patients with PDM such as substance use disorders including stimulants, opioids, marijuana and alcohol, (Liebschutz et al., 2010) mental health diagnoses (Liebschutz et al., 2010; Zatzick et al., 2012) and other medical comorbidities including chronic pain (Morasco, Turk, Donovan, & Dobscha, 2013) are particularly challenging to address in the Emergency Medicine setting. Patients can develop chronic opioid use (Hoppe, Kim, & Heard, 2015) or misuse of prescription drugs after receiving a prescription from a health care provider (McCabe, West, Teter, & Boyd, 2012). Trauma patients in the ED may be a particularly important group to target for screening and longitudinal intervention for PDM as these patients have high rates of psychiatric and substance use comorbidity (Zatzick et al., 2012) and are in the ED for injury causing acute pain likely necessitating opioid medications. While Collaborative Care (CC) has been tested in primary care, outpatient and inpatient settings, the feasibility of a CC intervention aimed at PDM that is initiated from the ED and proceeds longitudinally has not been established.
Recent commentary has encouraged clinical trials to adopt effectiveness-implementation hybrid approaches resulting in more rapid widespread adoption of efficacious treatment models (Curran, Bauer, Mittman, Pyne, & Stetler, 2012). These hybrid trials allow for measurement of implementation outcomes such as patient and provider intervention acceptability and organizational sustainability (Proctor et al., 2011) as well as patient-level outcomes. These designs may also flexibly incorporate novel pragmatic trial methods including information technology and electronic medical record (EMR) innovations. Prior to a fully scaled effectiveness-implementation hybrid trial, it is logical to understand the feasibility of collaborative care initiated from the ED for both effectiveness and implementation (Leon, Davis, & Kraemer, 2011).
Therefore, the goal of this pilot effectiveness-implementation hybrid study was to establish the feasibility of a Collaborative Care intervention for injured patients with prescription drug misuse that will be initiated from the ED, include elements central to Collaborative Care, (B. F. Miller et al., 2011) and continue longitudinally for six months. The primary outcomes for this study are feasibility and acceptability of the Collaborative Care intervention and retention rates over time. Secondary outcomes include healthcare linkage and utilization and PDM over time. The results of this pilot study will inform future larger scale studies evaluating the effectiveness and implementation outcomes of Collaborative Care initiated in the ED for prescription drug misuse.
2. Material and Methods
Project ‘Emergency Department Longitudinal Integrated Care’ (ED-LINC) was a prospective, open feasibility pilot intervention trial of a Collaborative Care intervention using a sample of adult patients presenting to the Emergency Department (ED). Consistent with pilot study methodology, we aimed to recruit thirty participants to test feasibility and acceptability (Lancaster, Dodd, & Williamson, 2004). This study was approved by the University of Washington Institutional Review Board and all participants provided written informed consent. This trial is registered through ClinicalTrials.gov as NCT02804295.
2.1 Setting and Patient Population
The study was conducted at Harborview Medical Center (HMC) which is a large urban, academic Level 1 trauma center located in Seattle, Washington. Patients were recruited during the hours of 8:00 a.m. and 6:00 p.m. Monday through Friday between February 24th and August 17th, 2015. Eligible patients were English-speaking adults ages 18-65 who presented to the Emergency Department at HMC for an injury.
2.2.1 Screening: Electronic Medical Record (EMR) pre-screening procedure
Prior investigation by the study team has attempted EMR phenotyping procedures for common acute care medical, mental health and substance use comorbidities to quickly screen for study participants (Russo, Katon, & Zatzick, 2013). Similarly, methods were developed in this feasibility pilot study for the assessment of PDM. Prior to approach, the Research Assistant (RA) reviewed the EMR to identify patients with an injury and then determine if they had risk for prescription drug misuse (PDM). Based on an extensive literature review, risk factors for PDM included any of the following: history of opioid, sedative or stimulant abuse or dependence (Jones, 2013), history of opioid overdose (Silva, Schrager, Kecojevic, & Lankenau, 2013), current opioid prescription (Bohnert, Logan, Ganoczy, & Dowell, 2016; Bohnert et al., 2011), previous ED visit at HMC attributable to substance use (Agrawal, Lynskey, Madden, Bucholz, & Heath, 2007; Hall et al., 2008; Morasco et al., 2013), psychiatric disorder (Agrawal et al., 2007; Johnson et al., 2012) and more than five ED visits over the course of a year (Hall et al., 2008). All of the above elements were reviewed in the EMR for each possible participant and part of the EMR pre-screening procedure. Specifically, history of opioid, sedative or stimulant abuse or dependence and history of opioid overdose and previous ED visit attributable to substance use were obtained through any documented ICD-9 code related to abuse dependence or poisoning from these substances. A ‘current opioid prescription’ was defined as any prescription for opioids prescribed by a HMC provider within 3 months of the index ED visit. ED visits were reviewed from the statewide Emergency Department Information Exchange (EDIE) which was integrated with the EMR. Adult patients presenting to the ED with a trauma who had at least one risk factor for PDM based on the EMR pre-screening procedure were eligible for approach. Patients were excluded if they were incarcerated, required active resuscitation, were receiving care for a sexual assault, had a diagnosis of cancer or were receiving palliative care or hospice services, were in the ED for a primary psychiatric emergency (e.g. suicide attempt), lived beyond a 50 mile radius of HMC, were unable to provide two pieces of contact information including a phone number or were monolingual non-English speaking. All possible participants were approached in the ED clinical space or after admission to the inpatient unit from the ED.
2.2.2 Screening: In-Person Assessment
Eligible patients with at least one risk factor for PDM by EMR pre-screening criteria were approached and completed an in-person self-report assessment for PDM on a tablet computer. Self-report PDM was assessed using the NIDA-modified Alcohol Smoking and Substance Involvement Screening Test (NM-ASSIST) (Ali et al., 2002) and four questions from the Current Opioid Misuse Measure (COMM) (Butler et al., 2007). Specifically, prescription drug misuse was assessed by asking ‘have you ever used prescription opioids to ‘get high,’ or taken them when they were prescribed to someone else or taken more than what was prescribed to you?’ with analogous questions specific to prescription stimulants and prescription sedatives. Participants who completed the screening portion of the study were provided with $5 for their time. Participants with a positive self-report screen for prescription opioid misuse, prescription sedative misuse, or prescription stimulant misuse by the NM-ASSIST (Ali et al., 2002) (score ≥ 1) or by the four select questions from the COMM (Butler et al., 2007) (score ≥ 1) in the past 6 months had PDM and completed the baseline survey. Participants could screen-in for misuse of more than one prescription drug. Next, contact information including a primary phone contact, secondary contact information such as email or a secondary phone and family or friend contact information was collected. At this point, participants that did not have a phone were excluded due to the nature of the intervention.
2.3 The ED-LINC Intervention
‘Emergency Department Longitudinal Integrated Care’ or ED-LINC intervention development and implementation were derived by prior procedures described by the study team (Zatzick et al., 2013; Zatzick et al., 2014). Intervention team members included a board-certified emergency medicine physician (LKW), clinical psychologist trained in motivational interviewing and trauma care (DD), psychiatrist (DZ) and care manager (KJ). After the completion of the baseline survey, the study care manager contacted a member of the hospital-based study team (LW, DD and/or DZ) to have an initial case discussion which included review of the screening assessment, baseline assessment, the EMR and all prior ED and inpatient visits. This included review of a novel clinical health information exchange tool, Emergency Department Information Exchange (EDIE) (Collective Medical Technologies; D. E. Neven, Sabel, Howell, & Carlisle, 2012) which includes past 12 month ED utilization within all ED’s in the states of Washington and Oregon. The study care manager (KJ) was based at HMC and while all participants lived within 50 miles of the study site, it was not a requirement for participants to exclusively receive their care at HMC. However, most follow-up injury care occurred in outpatient clinics at HMC. As in previous similar trials (Zatzick et al., 2013; Zatzick et al., 2014), the care manager assisted with providing the ED-LINC intervention to all participants tailored to their specific concerns.
The ED-LINC intervention included the following elements: 1) active care coordination and linkage, 2) medication safety and utilization of opioid guidelines 3) longitudinal care management for six months after enrollment, and 4) utilization of EMR innovations such as EDIE and the prescription monitoring program (PMP) information for assessment and follow-up. The first three elements have been tested individually in efficacy-effectiveness spectrum studies (Zatzick et al., 2013; Zatzick et al., 2014).
As part of the active care coordination and linkage element, the study team used motivational interviewing (Miller & Rollnick, 2012) techniques at the time of enrollment or immediately after to assess patient motivation to link to outpatient healthcare services. Care linkage was defined as linking the patient to outpatient care which was tailored to the participants’ specific needs with a focus on primary care. However, care linkage also included subspecialty injury care, substance use and mental health services as indicated by the initial assessment of existing healthcare service use, the baseline survey and medical problems related to the index ED or hospital visit. We measured care linkage by noting care manager assistance with linking to existing care (e.g. help with making appointments) as well as linking to new providers (e.g. making appointment with a new provider) both within HMC and outside of HMC. The study care manager discussed appointments with each participant and would often be informed of the content of the appointment or if the appointment was missed. The care manager would assist with rescheduling any missed appointments.
A discussion of medication management and opioid medications took place during the longitudinal intervention with the RA and/or study PI as part of the medication safety and opioid guideline element of the intervention. A current medication list was reviewed by the study team physicians (LKW, DZ) after the initial assessment. As indicated, the team discussed safe opioid practices (e.g. no mixing with other opioids or with alcohol) and reviewed any instances of co-occurring prescriptions for benzodiazepines or sedatives which was defined as any prescription for an opioid and sedative prescribed on the same day or for the same range of days in the past six months. Additionally, the team emphasized the role of the ED in treating acute and chronic pain and prescribing opioids, which was informed by the Washington ED opioid prescribing guidelines (D. E. Neven et al., 2012). If indicated, this would include a discussion by the study team with participants’ existing care providers around medications opioids.
As part of the care management element, the RA performed longitudinal care management tasks tailored to each individual participant needs for six months. These tasks included calling or texting to remind the participant of existing appointments, referral to substance use treatment providers and discussing participant progress with existing care providers such as primary care providers, substance use providers, case managers or social workers. Importantly, many patients had substance use comorbidity and the care manager referred participants as needed to local substance use treatment providers both at HMC and in the community. As requested by participants, the care manager would coordinate care with existing substance use treatment providers including those providing medication assisted treatment for opioid use disorder.
EMR innovations were central to both initial assessments and obtaining information for follow-ups. EDIE was reviewed at the time of enrollment for ED utilization patterns as well as prescription information, which is provided on EDIE reports via the statewide PMP. To follow enrolled patients, EDIE was queried frequently to obtain information on ED visits within Washington and Oregon. Additionally, a real-time email notification was provided to the care manager via EDIE when any participant had an ED visit at HMC.
Consistent with Collaborative Care procedures (B. F. Miller et al., 2011), the care manager logged contact and services provided for each participant and had weekly meetings with the intervention team for supervision and to discuss active cases. As appropriate, the intervention physicians (LKW, DZ) would contact participant primary care providers or subspecialty mental health practitioners by phone during or after these meetings. Otherwise, these weekly meetings provided a framework for the care manger to complete tasks related to care coordination and care management. All participants were provided with the number to a study cell phone that was covered by members of the intervention team 24 hours a day, seven days a week to address any concerns real-time via phone or text. Additionally, this study cell phone allowed for care coordination with other existing service providers such as substance use, mental health, social work or other care managers.
2.4 Outcomes and Assessments
Participants completed self-report assessments at the point of recruitment and again at one-month, 3-months and 6-months during the intervention period. The baseline assessment was self-administered or administered with RA assistance on a tablet computer and the outcome assessments were completed in-person, over the phone or via email link. Multiple modalities to obtain outcome assessments were used as previous research has shown no difference in response between interviewer-administered assessments and web-based assessments (Fleming et al., 2013). Participants received increasing compensation for participation over the course of the study. Specifically, they received $15 for completion of the baseline up to $40 for completion of the six-month assessment for a total of $115 to complete the screen, baseline and all longitudinal assessments.
2.4.1 Feasibility outcomes: Effectiveness
Feasibility was assessed with recruitment rates and retention over time. Information on phone utilization and phone stability, defined as the number of participants that have a change in phone or phone number and method of contact, were provided via project contact logs.
2.4.2 Feasibility outcomes: Implementation
Fidelity to the intervention framework and acceptability including satisfaction are important implementation outcomes (Proctor et al., 2011). Treatment fidelity was defined by the proportion of participants that received each element of the ED-LINC intervention and care manager activities were carefully tracked and categorized into each element of ED-LINC over time. During the six month assessment, all participants completed the Client Satisfaction Questionnaire (CSQ-8) (Attkisson & Zwick, 1982) which is a validated instrument used to assess participant acceptability and satisfaction along with select questions from the Patient Assessment of Chronic Illness Care (PACIC) (Glasgow et al., 2005) to determine participant perspective of adherence to the Collaborative Care intervention framework.
2.4.3 Sociodemographic and Clinical Characteristics
During the screening survey, information on age, sex, education and employment status were obtained. Clinical characteristics such as injury type, length of stay, medication list and prescriptions provided at discharge were recorded via review of the EMR. Services provided to participants by social workers, chemical dependency counselors and psychiatry consult teams were also recorded to note the service delivery provided during their index ED visit or inpatient stay. HMC is a level one trauma center and SBIRT services are available to patients with a positive blood alcohol level at the time of admission to the hospital (Terrell et al., 2008). To ensure reliability of all chart review data, research staff abstracted data into a standardized database and discrepancies were assessed by two reviewers; a final decision was made by an Emergency Medicine physician (LKW) and audits were performed regularly (Gilbert, Lowenstein, Koziol-McLain, Barta, & Steiner, 1996).
2.4.4 Substance Use and Mental Health
The ten-item Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) was used to assess alcohol misuse or problem alcohol use using a cut-off of ≥ 8 to note hazardous drinking. The AUDIT has excellent validity and reliability and has previously been used in ED settings (Walton et al., 2010). The NM-ASSIST (Ali et al., 2002) was used to detect illicit drug use and misuse of prescription drugs. At baseline, participants were asked about past six-month use of specific substances including cannabis, cocaine, methamphetamine and heroin. At each subsequent outcome assessment, participants were asked about interval use of each substance. Further, participants who used heroin or opioid pain medications were provided with an overdose risk assessment (A.S. Bohnert et al., 2016). The 9-item Patient Health Questionnaire (PHQ-9) was used to assess DSM-IV symptoms consistent with a major depressive disorder; PHQ-9 item 9 assessed the presence or absence of suicidality (Kroenke, Spitzer, & Williams, 2001). The Generalized Anxiety Disorder-7 (GAD-7) was used to assess anxiety symptoms over the past two weeks(Spitzer, Kroenke, Williams, & Lowe, 2006). PHQ-9 and GAD-7 scores were dichotomized, with a score ≥ 10 indicating major depression or clinically significant anxiety, respectively.
2.4.5 Health Services Utilization
ED utilization throughout Washington and Oregon in the previous 12 months and controlled substance prescriptions from Washington from the past 6 months were abstracted from the Emergency Department Information Exchange (EDIE). Information from the Washington Prescription Monitoring Program (PMP) is included in EDIE reports if one of the following criteria is met: more than three prescribers in 12 months, more than four controlled substance prescriptions within 12 months, more than two controlled substance prescriptions in the last 40 days, any prescription for long-acting opioids including buprenorphine, any overlapping prescriptions for opioids and benzodiazepines in the last six months and more than 100 morphine equivalents/day prescribed, averaged over the last 40 days. Self-report service utilization including primary care, substance use and mental health services was assessed at baseline using the substance abuse outcomes module (Smith et al., 2006). Specifically, participants were asked ‘In your lifetime have you ever attended a drug abuse or alcohol abuse treatment program (i.e. inpatient, outpatient or residential treatment program or a program where you detoxified from alcohol or drugs’. Those with a ‘yes’ response to this question were then asked the same question with a timeline of past six months.
2.5 Data Analysis
We examined descriptive statistics and characteristics of the ED-LINC intervention. Fisher’s exact test was used for categorical data and t-tests were performed for continuous variables. We performed an exploratory regression analysis to assess longitudinal changes in prescription opioid misuse, prescription sedative misuse and prescription stimulant misuse as measured by an NM-ASSIST (Ali et al., 2002) score ≥ 1 for each prescription drug using generalized mixed models. In the multivariate analysis the sample size at each time point corresponded to the response rate and there was no further missing data. These models were all adjusted for age and gender. All analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, NC).
3. Results
3.1 Study sample characteristics
A total of 233 injured trauma patients had a positive EMR pre-screen; 133 were approached to participate and of those approached, 37 were excluded, 22 declined, 10 were missed and 64 completed the in-person screening (Figure 1). All patients that consented to the study completed the screening and 36 (56%) screened positive for prescription drug misuse (PDM). Sixty-nine percent (n=40) of all participants that competed the in-person screening survey were discharged from the ED and there was no difference in admission rates among those that had a positive screen for PDM (n=36) compared to those without a positive screen for PDM (n=28) (p=0.68). Six participants with PDM were not eligible for enrollment after completion of the screen and baseline due to inadequate contact information and thus 30 participants were enrolled in the study and received the ED-LINC intervention. outcome assessment (Figure 1).
Figure 1.
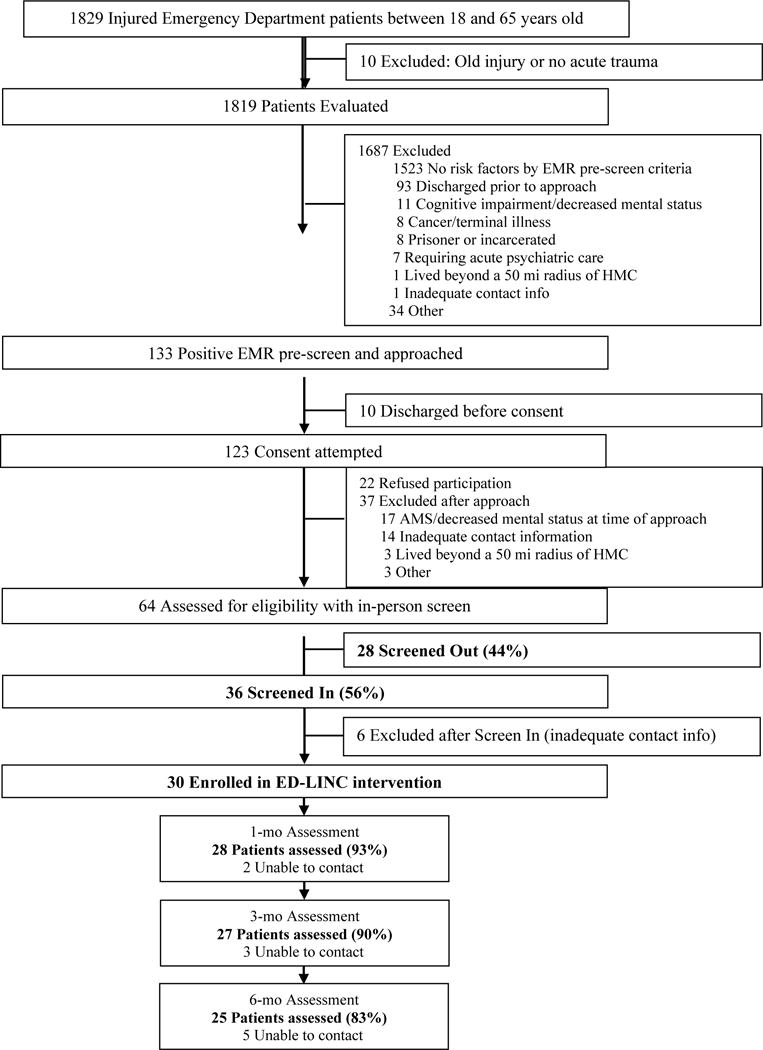
Flow of Patients and Consort Diagram
Among those enrolled in ED-LINC, the mean age was 44.6 years (SD 13.5), 33% were female, 27% were homeless or temporarily housed and the majority identified as white (60%). Additionally 37% of those with PDM were admitted to the hospital with four participants requiring care in the Intensive Care Unit (ICU) and five participants receiving surgery. Almost all of those enrolled had a positive screen for prescription opioid misuse (97%) while 20% had a positive screen for prescription sedative misuse and 37% had a positive screen for prescription stimulant misuse. At baseline, 20% of participants reported receiving methadone at an opioid treatment program for opioid addiction and one patient was receiving buprenorphine from a primary care provider for medication assisted treatment. At discharge from the ED or the hospital, 47% of participants received a prescription for opioids for treatment of pain, 47% were seen by social work and only 7% received SBIRT services or chemical dependency counseling (Table 1).
Table 1.
Baseline Demographic Prescription Drug Misuse (PDM) screening results and clinical characteristics for participants enrolled in ED-LINC (n=30)
| Variable | n (%) |
|---|---|
| Demographics | |
| Age m(SD) | 44.6 (13.5) |
| Female | 10 (33) |
| Currently homeless or temporarily housed | 8 (27) |
| Race | |
| White | 18(60) |
| African-American | 6(20) |
| American Indian/Alaskan Native | 3(10) |
| Other | 3(10) |
| PDM Screening Results | |
| Risk for prescription stimulant misuse | 11 (37) |
| Risk for prescription sedative misuse | 6 (20) |
| Risk for prescription opioid misuse | 29 (97) |
| Clinical Characteristics at Baseline | |
| Opioid for pain management listed as home medication | 15 (50) |
| Sedative listed as home medication | 4 (14) |
| Stimulant listed as home medication | 0 (0) |
| Receiving Medication Assisted Treatment (MAT) for opioid use disorder | 7 (23) |
| Methadone | 6 (86) |
| Buprenorphine | 1 (14) |
| Admitted to the hospital | 11 (37) |
| Admitted to the ICU | 3 (27) |
| Received surgery | 4 (36) |
| Received social work services | 7 (64) |
| Received SBIRT as inpatient | 1 (9) |
| Seen by Anesthesia Pain Service | 2 (18) |
| Injury related to assault/violence | 3 (10) |
| Received prescription for opioids at discharge | 14 (47) |
| Received prescription for sedatives at discharge | 2 (7) |
| Received prescription for stimulants at discharge | 0 (0) |
| Received social work services in the ED | 7 (23) |
| Received chemical dependency services from ED | 1 (10) |
| Seen by Psychiatry | 0 (0) |
3.2 Baseline substance use, mental health comorbidity and health services utilization
ED-LINC intervention participants demonstrated high frequencies of substance use and mental health comorbidity (Table 2). Specifically, 83% used marijuana, 77% used cocaine, 63% used methamphetamine and 40% used heroin in the past six months. Overdose risk was high in the sample and 43% reported a history of lifetime overdose. Seventy percent of participants consumed alcohol with 43% having harmful or hazardous drinking in the past six months. Approximately one-third of participants had suicidal ideation based on a positive PHQ-9 (Kroenke et al., 2001) item 9 response at baseline, and 70% met DSM-IV symptomatic criteria for major depression. Lastly, over half (53%) had moderate or severe anxiety in the past two weeks. Despite this comorbidity, only 53% of participants had a primary care provider and only 43% of participants had received counseling in the past six months. On review of statewide ED visits through EDIE, over 50% of participants had at least five ED visits within Washington or Oregon in the past 12 months with 53% of participants visiting three or more ED’s.
Table 2.
Baseline Characteristics of Participants in the ED-LINC Intervention (n=30)
| Variable | n (%) or mean (SD) |
|---|---|
| Polysubstance use | |
| Past 6 month cannabis use | 25 (83) |
| Past 6 month cocaine use | 23 (77) |
| Past 6 month methamphetamine use | 19 (63) |
| Past 6 month heroin use | 17 (57) |
| Lifetime history of opioid overdose* | 12 (43) |
| Currently in medication assisted treatment * | 8 (29) |
| Past 6 month alcohol use | 21 (70) |
| AUDIT score | 9.9 (10.5) |
| AUDIT≥8 | 13 (43) |
| Mental Health | |
| PHQ-9 score in past month | 12.2 (5.8) |
| PHQ-9≥ 10 indicating major depression | 21 (70) |
| Suicidal ideation | 11 (37) |
| GAD-7 score over past 2 weeks | 10.7 (6.0) |
| GAD-7 ≥ 10 indicating moderate/severe anxiety | 16 (53) |
| Health Services Utilization | |
| Currently have a primary care physician | 16 (53) |
| Number of visits to physician in past year | 4.6 (10.1) |
| Attended substance abuse treatment in your lifetime | 22 (73) |
| Attended substance abuse treatment in the past 6 months@ | 11 (50) |
| Received counseling in the past 6 months | 13 (43) |
| Have a case manager # | 11 (38) |
| Statewide ED visits in past 12 months (mean, SD) | 10.7 (13.0) |
| Statewide ED visits in past 12 months ≥ 5 | 17 (57) |
| Number of different ED’s in past 12 months (mean, SD) | 3.3 (2.3) |
| Number of different ED’s in past 12 months ≥ 3 | 16 (53) |
28 participants answered the question and thus included in this item
22 participants answered the question and thus included in this item
29 participants answered the question and thus included in this item
3.3 Intervention Services
Review of the ED-LINC project notes revealed that 100% of participants received the ‘active care coordination and linkage’ element. All participants (n=30) received a discussion with a trained member of the study team about symptoms, medication management and/or motivation to link to services as part of the active care coordination piece of this intervention element. All participants were linked to new primary care or had care coordination to existing primary care over the course of the study including seven participants (23%) that were actively referred to a new primary care provider and five participants (17%) that were actively referred to new mental health or substance use service provider. As part of the ‘medication safety and utilization of opioid guidelines’ element to ED-LINC, the study team reviewed medications and had a discussion about medication management with 90% (n=27) of participants and discussed pain control and pain management with 90% (n=27) during the course of the study. The 10% (n=3) of patients that did not receive this intervention element had cell phone instability and reported homelessness or living in a shelter at some point during the course of the study. Longitudinal care management occurred for all participants and included direct coordination of services with existing primary care providers (17%), assistance with upcoming appointments (73%), referral to housing (83%) and other social services (20%), and bedside meetings during any subsequent ED visits or hospitalizations (73%). Additionally, the care management element included coordinating care for addiction or substance use services (83%) and over the course of the six-month intervention we were able to link one participant to methadone treatment with an opioid treatment program. We coordinated care with the seven participants already on medication assisted treatment by talking with case managers associated with their methadone program or with the primary care provider prescribing buprenorphine and set up appointments and established connections with several outpatient treatment providers such as chemical dependency counselors. Lastly, EDIE was reviewed for 100% of participants over the course of the study. At enrollment 27% (n=8) had PMP data available via EDIE. Over the course of the study 67% had a real-time email alert sent to the study care manager notifying them of a current HMC ED visit. Please see Table 3 for full details of ED-LINC elements and service provision for participants over the course of the study.
Table 3.
ED-LINC Elements and Service Provision for Participants over time (n=30)
| Participants who received this service over time | Received service ≥ 1 time | |||
|---|---|---|---|---|
| 0-1 month n (%) |
1-3 month n (%) |
3-6(+) month n (%) |
n (%) | |
| Active Care Coordination + Linkage | ||||
| Care Coordination: Initial assessment of existing healthcare service use and symptoms | 30 (100) | 0 (0) | 0 (0) | 30 (100) |
| Care Coordination: Review of primary care physician plan for subsequent care | 24 (80) | 13 (43) | 30 (100) | 30 (100) |
| Linkage: New primary care provider | 5 (17) | 1 (3) | 3 (10) | 7 (23) |
| Linkage: New mental health/substance abuse service | 4 (13) | 1 (3) | 1 (3) | 5 (17) |
| Linkage: Other healthcare needs (e.g. PT) | 1 (3) | 1 (3) | 3 (10) | 4 (13) |
| Linkage: Subsequent assessments | 15 (50) | 11 (37) | 19 (63) | 24 (80) |
| Medication Guideline Application | ||||
| Med List review and medication management | 19 (63) | 13 (43) | 17 (57) | 27 (90) |
| Pain management (symptoms, medication) | 25 (83) | 18 (60) | 21 (70) | 27 (90) |
| Longitudinal Care Management (post-ED visit and/or hospitalization) | ||||
| Direct coordination with existing PCP | 4 (13) | 0 (0) | 3 (10) | 5 (17) |
| Direct coordination with other existing service providers (e.g. mental health, social work, case manager) | 10 (33) | 5 (17) | 7 (23) | 12 (40) |
| Direct coordination with housing service, other | 4 (13.3) | 2 (6.7) | 3 (10.0) | 6 (20) |
| Provided referral and info for housing, other | 20 (67) | 13 (43) | 16 (53) | 25 (83) |
| Appointment reminder (primary care, mental health, subspecialty, etc.) | 14 (47) | 17 (57) | 14 (47) | 22 (73) |
| Care management for addiction/substance abuse | 21 (70) | 6 (20) | 20 (67) | 25 (83) |
| Other care management | 18 (60) | 12 (40) | 18 (60) | 23 (77) |
| Met patient in ED/inpatient, discussion about visit | 13 (43) | 10 (33) | 15 (50) | 22 (73) |
| Accompany to HMC appointment (assistance with check-in, wheelchair, etc.) | 3 (10) | 3 (10) | 4 (13) | 9 (30) |
| EMR Innovations | ||||
| EDIE reviewed | 30 (100) | 30 (100) | 30 (100) | 30 (100) |
| Prescription Monitoring Program information reviewed in EDIE upon enrollment | 8 (27) | n/a | n/a | 8 (27) |
| EDIE email alert regarding ED visit at HMC | 11 (37) | 11 (37) | 14 (47) | 20 (67) |
3.4 Feasibility Outcomes: Effectiveness
Over the course of the study, 93% (n=28) of the intervention patients completed the one-month outcome assessment, 90% (n=27) completed the three-month outcome assessment and 83% (n=25) completed the six-month. On average, enrolled participants (n=30) received a total of 85 minutes (SD 53.20 minutes) (range 15-221 minutes) of ED-LINC across six months, with 35% of the intervention time coming in the first month after enrollment (Table 3). Over the course of the intervention, 77% (n=23) had cell phone instability with 53% having a change in their phone and 70% having a phone number that became inactive.
3.6 Feasibility Outcomes: Implementation
Overall, participants were satisfied with the care they received through this intervention. A substantial majority of patients (80%) thought the quality of services they received during the intervention were ‘good’ or ‘excellent’ and 88% received the services they wanted through this intervention. Additionally, 84% thought the services they received helped them deal more effectively with their problems. Patient perception of chronic illness care provided ED-LINC was generally good. Specifically, 60% reported they were contacted after a visit to see how things were going and 50% perceived that they were encouraged to attend community programs that would benefit their wellness and health.
3.7 Prescription drug misuse over time
Generalized mixed models adjusted for age and gender revealed no significant change across time of prescription stimulant misuse, prescription sedative misuse or prescription opioid misuse (Table 4). While there was a trend in decrease of prescription opioid misuse and this was the most frequently misused prescription drug in the sample, this did not reach statistical significance.
Table 4.
Generalized Mixed Models predicting Prescription Drug Misuse over time adjusted for age and gender with baseline values as the reference.
| Prescription Drug Misuse category | One month RR and 95% CI |
3-months RR and 95% CI |
6-months RR and 95% CI |
|---|---|---|---|
| Prescription opioid misuse | 1.56 (0.74,3.29) | 1.02 (0.40,2.55) | 0.54 (0.20,1.44) |
| Prescription sedative misuse | 1.06 (0.30,3.74) | 1.16 (0.33,4.13) | 0.93 (0.24,3.57) |
| Prescription stimulant misuse | 0.71 (0.11,4.42) | 1.11 (0.22,5.73) | 0 (0.0) |
RR = relative risk
95% CI = 95% Confidence Interval
4. Discussion
To our knowledge, this is the first report of feasibility and acceptably of a Collaborative Care intervention in the Emergency Department service delivery context. A large literature base has established the feasibility, acceptability and effectiveness of the Collaborative Care model for patients with comorbid mental health and medical comorbidity treated in primary care and acute care trauma center inpatient settings (Katon et al., 2010; Richardson et al., 2014; Sharpe et al., 2014; Unutzer et al., 2002; Zatzick et al., 2013; Zatzick et al., 2014). The ED-LINC intervention was tailored for and initiated from the ED, used evidence-based elements and preceded longitudinally while incorporating EMR innovations as both assessment and follow-up tools.
These data also suggest the feasibility of simultaneous targeting of trauma, substance use and mental health comorbidity. Previous research suggests that over 80% of patients admitted for trauma have co-existing alcohol, drug use or psychiatric comorbidity (Zatzick et al., 2012). Interventions aimed at this population should be designed to address multiple conditions. Bogenshutz et al. (2014) recently completed a multi-site trial of SBIRT for patients with problematic drug use presenting to the ED (Bogenschutz et al., 2014). In this well done multi-site trial, there was no difference in drug use among patients randomized to brief intervention or usual care and only 25% of participants were linked to substance use treatment after referral to treatment. It is possible that a brief intervention is not enough for patients with substance use that have high levels of associated comorbidity. The ED is an important service delivery point for patients with unmet substance use and mental health needs (Rockett et al., 2005) and it is important that interventions for these participants address comorbidity.
For patients with PDM, ED-LINC shows promise as a feasible intervention. All eligible participants were enrolled in the intervention and retention rates were high over the course of the study. The importance of establishing sound and robust follow-up procedures in studies of substance use interventions from the ED cannot be overstated and are necessary to maintain internal validity (Cunningham et al., 2008). Interventions aimed at patients in the Emergency Department can often exclude patients that are difficult to follow, thus decreasing generalizability and external validity. These feasibility results indicate that with proper study protocols and resources, follow-up rates of over 80% are possible in urban safety-net settings.
Patients reported high rates of satisfaction with the ED-LINC intervention. Over 80% of patients reported that they received the services they desired and that services received were helpful in addressing their complex comorbidities. One of the benefits of Collaborative Care is coordinated care among providers. The ED can often act as a central health services access point for vulnerable populations and while the ED is the place for episodic acute care, it can also be a point where patients not engaged in primary care come for basic needs. Despite the large amount of comorbidity among study participants, almost half (47%) did not have a primary care provider and 57% report five or more ED visits in the past year. Additionally, 53% used three or more different ED’s in the past year suggesting fragmented health care which is a known risk factor for overdose and death in patients with misuse of prescription opioids (Hall et al., 2008; Johnson et al., 2012).
The ED-LINC intervention is feasible and linked patients to primary care, community mental health and subspecialty substance abuse care. Importantly, not all these linkages were within the same hospital or health system. A recent investigation showed that only 50% of ED patients referred to a transitional care clinic complete their follow-up appointment and substance use problem is a known risk for decreased linkage to outpatient care (Elliott, Klein, Basu, & Sabbatini, 2016). ED-LINC successfully linked all participants to outpatient care. Specifically, more than half of participants did not have a primary care provider at the baseline assessment and over the course of the study, all participants were actively referred to new providers and care was coordinated for patients with existing primary care providers. Care management tasks included providing reminders of upcoming appointments and discussing care with existing providers. Care coordination and longitudinal care management is not routinely part of care from the ED which likely contributed to the successful linkages. The Collaborative Care framework of ED-LINC allows for adapting the existing intervention and integrating evidence-based elements such as medication assisted treatment and utilization of prescribing guidelines. For example, initiating buprenorphine from the ED for patients with opioid use disorder (D’Onofrio et al., 2015) to the ED-LINC intervention would seamlessly fit into the Collaborative Care framework. (B. F. Miller et al., 2011; Von Korff et al., 1997; Wagner et al., 1996) centralizing healthcare services for this population and therefore improving engagement with subsequent primary care services.
Implementation of ED-LINC in real-world settings is an important consideration. While this investigation used research staff to recruit participants, deliver the intervention and complete follow-up assessments, several important implementation outcomes were obtained. First, EMR screening procedures are efficient, cost-effective and could be implemented across a variety of settings (Russo et al., 2013). Using the EMR to screen also broadens the population impact (Koepsell, Zatzick, & Rivara, 2011) of the screening procedure and allows for targeted in-person screening assessments. While the EMR pre-screen in this study was not automated, the EMR pre-screen procedure allowed for targeted approach of individuals at high risk for PDM, decreasing the number of in-person approaches needed to recruit the target population and thus increasing efficiency. Future trials should consider the benefits of utilizing EMR screening tools while balancing the limitations of using historical data within one health system to identify possible participants. Use of a statewide health information exchange such as EDIE is extremely promising due to the ability to share information across health systems. The use of EDIE, a novel integrated health-information exchange system which included automated emails to the care manager notifying them of an HMC ED visit in real-time, could be implemented in the work flow of existing ED staff such as case managers or social workers. On-going work could focus on organizational readiness for implementation and sustainment of this type of practice within a busy Emergency Department.
Participants reported high satisfaction with ED-LINC which is an important implementation outcome. Future fully-scaled effectiveness-implementation hybrid clinical trials (Curran et al., 2012) should include an assessment of the facilitators and barriers of implementation within the ED and within the healthcare system or organization for implementing this system of care. ED-LINC successfully linked participants with PCP’s and other health care providers within HMC but also within the community and outside the HMC system. Documenting the reach of the care manager will assist with understanding scope and scalability. The Consolidated Framework for Implementation Research (CFIR) (Damschroder et al., 2009) provides a structure for implementing complex interventions in the real-world and can guide evaluation of evidence-based interventions. The adaptability of ED-LINC could be assessed using this theoretical model. A fully-scaled effectiveness-implementation hybrid study (Curran et al., 2012) would allow for attention to both patient level outcomes such as substance use symptoms and participant health care utilization as well as organizational level outcomes such as adoption, cost and sustainability (Proctor et al., 2011) which would need to account for the time spent by the intervention team for activities such as weekly supervision and coverage of the intervention cell phone. Similarly, qualitative observations of the care manager would provide information relevant to adoption and sustainability.
While this investigation provides important information on the feasibility of initiating an intervention using principles of Collaborative Care from the ED, there are some important limitations to consider. The EMR pre-screen used to identify possible participants for approach was based on known risk factors for PDM, but has not been validated. The overall number of eligible patients approached that refused participation was small (n=22) but the reasons for refusal were not systematically collected. Future investigations should include this information, as it is important for implementation and generalizability. All participants approached completed a validated self-assessment for PDM, but it is possible the pre-screen criteria selected for participants with higher levels of comorbidity and ED utilization than the general population that uses the ED for care. This feasibility trial did not randomize patients to intervention and control conditions and the study was not powered to show a decrease of PDM over time. Future investigations should include appropriately powered randomized clinical trial designs that incorporate effectiveness and implementation outcomes. Also, this study was conducted in a single, large urban academic hospital and these results may not apply to other settings. PDM outcomes were assessed by self-report and not confirmed with biomarkers which could be perceived as a limitation. Previous work has documented the reliability of self-report for substance use in this context as well as the limitations for biomarkers for misuse of prescription drug misuse (Vitale, van de Mheen, van de Wiel, & Garretsen, 2006). A convenience sample of patients was recruited and future studies should consider systematic recruitment of evenings, nights and weekends to ensure generalizability to the ED population.
5. Conclusions
Collaborative Care initiated from the ED and progressing longitudinally for six months is feasible and acceptable to injured patients with prescription drug misuse. Participants in this study had high rates of substance use and mental health comorbidity and the elements of ED-LINC within the Collaborative Care framework can address this comorbidity while linking patients to subspecialty services. Future fully scaled effectiveness-implementation hybrid trials could address implementation and effectiveness outcomes of ED-LINC for the complex population of patients with PDM.
Acknowledgments
The authors acknowledge Leah Ingraham for excellent administrative and project support and special thanks is owed to the patients and staff of Harborview Medical Center.
This work was funded through the University of Washington Alcohol and Drug Abuse Institute (ADAI) small grants program and through the National Institute on Drug Abuse (K23DA039974). The preparation of this article was supported in part by the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (5R25MH08091607).
Footnotes
Poster presentation of findings at the University of Michigan Opioid Overdose Summit, Ann Arbor, MI, December, 2015; and the College on Problems of Drug Dependence, Palm Springs, CA, June, 2016.
References
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Ali R, Awwad E, Babor TF, Bradley F, Butau T, Farrell M, Grp, Who Assist Working The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Bohnert AS, Ignacio RV, Chermack S, Cunningham RM, Barry KL. A randomized controlled trial of brief interventions to reduce drug use among adults in a low-income urban emergency department: the HealthiER You study. Addiction. 2017 doi: 10.1111/add.13773. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Donovan DM, Mandler RN, Perl HI, Forcehimes AA, Crandall C, Douaihy A. Brief intervention for patients with problematic drug use presenting in emergency departments: a randomized clinical trial. JAMA Intern Med. 2014;174(11):1736–1745. doi: 10.1001/jamainternmed.2014.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Eisenberg A, Whiteside L, Price A, McCabe SE, Ilgen MA. Prescription opioid use among addictions treatment patients: nonmedical use for pain relief vs. other forms of nonmedical use. Addict Behav. 2013;38(3):1776–1781. doi: 10.1016/j.addbeh.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Logan JE, Ganoczy D, Dowell D. A Detailed Exploration Into the Association of Prescribed Opioid Dosage and Overdose Deaths Among Patients With Chronic Pain. Med Care. 2016;54(5):435–441. doi: 10.1097/MLR.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- Bohnert AS, Bonar EE, Cunningham R, Greenwald MK, Thomas L, Chermack S, Walton M. A pilot randomized clinical trial of an intervention to reduce overdose risk behaviors among emergency department patients at risk for prescription opioid overdose. Drug Alcohol Depend. 2016;163:40–47. doi: 10.1016/j.drugalcdep.2016.03.018. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Fernandez KC, Houle B, Benoit C, Katz N, Jamison RN. Development and validation of the Current Opioid Misuse Measure. Pain. 2007;130(1-2):144–156. doi: 10.1016/j.pain.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collective Medical Technologies. The Emergency Department Information Exchange. Retrieved April 11, 2016, from http://collectivemedicaltech.com/what-we-do-2/edie-option-2/
- Cunningham R, Walton MA, Tripathi SP, Outman R, Murray R, Booth BM. Tracking inner city substance users from the emergency department: how many contacts does it take? Acad Emerg Med. 2008;15(2):136–143. doi: 10.1111/j.1553-2712.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, Fiellin DA, Pantalon MV, Chawarski MC, Owens PH, Degutis LC, O’Connor PG. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Ann Emerg Med. 2012;60(2):181–192. doi: 10.1016/j.annemergmed.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, O’Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, Fiellin DA. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobscha SK, Corson K, Perrin NA, Hanson GC, Leibowitz RQ, Doak MN, Gerrity MS. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242–1252. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- Elliott K, Klein J, Basu A, Sabbatini AK. Transitional care clinics for follow-up and primary care linkage for patients discharged from the ED. Am J Emerg Med. 2016;34(7):1230–1235. doi: 10.1016/j.ajem.2016.03.029. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Marchesini G, Elgin J, Haggerty KP, Woodward D, Abbott RD, Catalano RF. Use of Web and Phone Survey Modes to Gather Data From Adults About Their Young Adult Children: An Evaluation Based on a Randomized Design. Field methods. 2013;25(4):388–404. doi: 10.1177/1525822X12466888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27(3):305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43(5):436–444. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015;65(5):493–499 e494. doi: 10.1016/j.annemergmed.2014.11.015. [DOI] [PubMed] [Google Scholar]
- Johnson EM, Lanier WA, Merrill RM, Crook J, Porucznik CA, Rolfs RT, Sauer B. Unintentional Prescription Opioid-Related Overdose Deaths: Description of Decedents by Next of Kin or Best Contact, Utah, 2008–2009. J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2225-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132(1-2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–659. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, McCulloch D. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koepsell TD, Zatzick DF, Rivara FP. Estimating the population impact of preventive interventions from randomized trials. Am J Prev Med. 2011;40(2):191–198. doi: 10.1016/j.amepre.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–312. doi: 10.1111/j..2002.384.doc.x. [DOI] [PubMed] [Google Scholar]
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebschutz JM, Saitz R, Weiss RD, Averbuch T, Schwartz S, Meltzer EC, Samet JH. Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. J Pain. 2010;11(11):1047–1055. doi: 10.1016/j.jpain.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ. Medical and nonmedical use of prescription opioids among high school seniors in the United States. Arch Pediatr Adolesc Med. 2012;166(9):797–802. doi: 10.1001/archpediatrics.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BF, Kessler R, Peek CJ, Kallenberg GA. In: A National Agenda for Research in Collaborative Care: Papers from the Collaborative Care Research Network Research Development Conference. Mullican C, editor. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd. Guilford Press; 2012. [Google Scholar]
- Moore M, Whiteside LK, Dotolo D, Wang J, Ho L, Conley B, Zatzick DF. The Role of Social Work in Providing Mental Health Services and Care Coordination in an Urban Trauma Center Emergency Department. Psychiatr Serv. 2016;67(12):1348–1354. doi: 10.1176/appi.ps.201500469. [DOI] [PubMed] [Google Scholar]
- Morasco BJ, Turk DC, Donovan DM, Dobscha SK. Risk for prescription opioid misuse among patients with a history of substance use disorder. Drug Alcohol Depend. 2013;127(1-3):193–199. doi: 10.1016/j.drugalcdep.2012.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neven DE, Sabel JC, Howell DN, Carlisle RJ. The development of the Washington State emergency department opioid prescribing guidelines. J Med Toxicol. 2012;8(4):353–359. doi: 10.1007/s13181-012-0267-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neven D, Paulozzi L, Howell D, McPherson S, Murphy SM, Grohs B, Roll J. A Randomized Controlled Trial of a Citywide Emergency Department Care Coordination Program to Reduce Prescription Opioid Related Emergency Department Visits. J Emerg Med. 2016;51(5):498–507. doi: 10.1016/j.jemermed.2016.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen JC, Ogarek JL, Goldenberg EJ, Sulo S. Impact of a Chronic Pain Protocol on Emergency Department Utilization. Acad Emerg Med. 2016;23(4):424–432. doi: 10.1111/acem.12942. [DOI] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C, Katon W. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809–816. doi: 10.1001/jama.2014.9259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockett IR, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann Emerg Med. 2005;45(2):118–127. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in Drug and Opioid Overdose Deaths–United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry. 2013;35(5):485–491. doi: 10.1016/j.genhosppsych.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sharpe M, Walker J, Holm Hansen C, Martin P, Symeonides S, Gourley C, Team, S. MaRT Oncology-2 Integrated collaborative care for comorbid major depression in patients with cancer (SMaRT Oncology-2): a multicentre randomised controlled effectiveness trial. Lancet. 2014;384(9948):1099–1108. doi: 10.1016/S0140-6736(14)61231-9. [DOI] [PubMed] [Google Scholar]
- Silva K, Schrager SM, Kecojevic A, Lankenau SE. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend. 2013;128(1-2):104–110. doi: 10.1016/j.drugalcdep.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, Grimes W. Reliability and validity of the substance abuse outcomes module. Psychiatr Serv. 2006;57(10):1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, editor. Substance Abuse and Mental Health Services Administration. Drug Abuse Warning Network 2011: National Estimates of Drug-Related Emergency Department Visits. Rockville, MD: 2013a. (HHS Publication No (SMA) 13-4760, DAWN Series D-39). [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Helath: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013b. [Google Scholar]
- Terrell F, Zatzick DF, Jurkovich GJ, Rivara FP, Donovan DM, Dunn CW, Gentilello LM. Nationwide survey of alcohol screening and brief intervention practices at US Level I trauma centers. J Am Coll Surg. 2008;207(5):630–638. doi: 10.1016/j.jamcollsurg.2008.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Treatment, Impact Investigators. Improving Mood-Promoting Access to Collaborative Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Vitale SG, van de Mheen H, van de Wiel A, Garretsen HFL. Substance use among emergency room patients: Is self-report preferable to biochemical markers? Addictive Behaviors. 2006;31(9):1661–1669. doi: 10.1016/j.addbeh.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127(12):1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. Jama. 2010;304(5):527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Hepner KA, Paddock SM, de la Cruz E, Zhou AJ, Gilmore J. An effectiveness trial of group cognitive behavioral therapy for patients with persistent depressive symptoms in substance abuse treatment. Arch Gen Psychiatry. 2011;68(6):577–584. doi: 10.1001/archgenpsychiatry.2011.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Donovan D, Dunn C, Russo J, Wang J, Jurkovich G, Gentilello L. Substance use and posttraumatic stress disorder symptoms in trauma center patients receiving mandated alcohol screening and brief intervention. J Subst Abuse Treat. 2012;43(4):410–417. doi: 10.1016/j.jsat.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Rivara FP, Russo J, Wagner A, Wang J, Katon W. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. 2013;257(3):390–399. doi: 10.1097/SLA.0b013e31826bc313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick D, Russo J, Lord SP, Varley C, Wang J, Berliner L, Rivara FP. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial. JAMA Pediatr. 2014;168(6):532–539. doi: 10.1001/jamapediatrics.2013.4784. [DOI] [PubMed] [Google Scholar]


